- Clinical Pharmacy Department, College of Pharmacy, Taif University, Taif, Saudi Arabia
Background: Digital Health innovative technologies, encompassing eHealth, mHealth, e-learning, tele-health, artificial intelligence (AI), tele-medicine, tele pharmacy, virtual reality, and augmented reality, are increasingly incorporated into learning and pharmacy education to prepare students for a Digital healthcare environment. However, evidence on the impact and implementation of these technologies still needs to be explored.
Objective: The current scoping review collates and appraises the impact of Digital Health on pharmacy education, evaluating effects on learning outcomes, skill development, competencies, and readiness for tele pharmacy and Digital Health application transformations. The primary objective was to explore the impact of Digital Health (eHealth, mHealth, e learning, telehealth, AI, telemedicine, tele pharmacy, VR, ML, and AR) in pharmacy education via structured scoping review reporting.
Methods: A systematic search following PRISMA guidelines conducted across databases, including Cochrane Library, Google Scholar, PubMed, Scopus, and Web of Science for recent papers published on Digital Health in pharmacy education from 2019 to 2024. Post-screening, 47 studies met the final criteria.
Results: 47 studies were included in the current scoping review. Five themes emerged (1) Curriculum integration and transformation in pharmacy education; (2) Digital literacy (competency development); (3) Tele pharmacy (remote health services and AI) in education; (4) Practical skill development (interactive learning through Digital tools) and (5) Student and faculty perceptions, attitudes, and challenges in adopting Digital Health. Digital Health integration improves students’ Digital competence, engagement, and tele pharmacy readiness, though gaps remain in curriculum standardization. Regional disparities show integration, which more advanced in Western programs, while foundational efforts seen in Asian, Middle East and North Africa (MENA) regions. The current review emphasized the importance of faculty developing, workload integration, regional disparities, and ethical concerns with AI and challenges in hybrid learning.
Conclusion: Digital Health has been an innovator in pharmacy students’ education, equipping them with the skills and competences required in today’s healthcare environment. However, faculty development, curriculum gaps, workload integration, insufficient telehealth training, regional disparities, and inadequate AI ethics instruction all point to the need for adequate and relevant curriculum modifications to qualify graduates to deal with Digital healthcare challenges.
Highlights
• Digital Health tools are increasingly integrated into pharmacy education to prepare students for modern healthcare.
• Many pharmacy programs lack formal Digital Health training, revealing a substantial gap in student readiness.
• Students show varied Digital literacy levels, pointing to a need for targeted training in AI and Digital tools.
• While students generally have a positive view of Digital Health, concerns about AI ethics, data security, and hands-on skill retention suggest the need for balanced training approach.
1 Background
Digital Health encompassing eHealth, mHealth, e learning, tele-health, artificial intelligence (AI), tele-medicine, tele pharmacy, Machine Learning (ML), virtual reality (VR), and augmented reality (AR), and electronic health records (EHRs). These technologies contribute to attaining high-quality healthcare services and the objective of Universal health coverage (1, 2). Students believed that remote services improve patient care and appreciated by patients and clinicians. They were willing to include tele pharmacy services in their future pharmacy practice (3, 4). In the United Kingdom (UK), Digital literacy is becoming increasingly crucial in pharmacy education (5). Evidence on effectively incorporating tele-education into pharmacy curricula is scarce, partly because pharmacy education combines diverse methods: classroom-based learning, simulations, and practical training (6). Students expressed a need for enhanced tele pharmacy, pharmacy management training, and a more substantial alignment between academic content and practical application (3, 7). The epidemic of COVID-19 accelerated the Digital transition in pharmacy education, setting a foundation for sustainable Digital teaching and learning changes that could benefit pharmacy education beyond the crisis (6, 8). A global study revealed that 57% of pharmacy schools lack Digital Health content in their curricula, pointing to a considerable gap in preparing students for Digital Health’s role in modern healthcare (9). Tailored educational tools and supportive learning environments are critical in preparing pharmacy students for successful careers (10–12). The current review aims to gather and evaluate the impact of Digital Health on pharmacy education by examining current practices and identifying gaps to better prepare students for modern healthcare needs.
Pharmacy education and training have evolved with the expanded role of pharmacists to encompass individual patient-centered care and further optimization of therapy and disease management. Digital Health innovations such as tele-pharmacy, telemonitoring, and tele therapeutics places the pharmacy students and faculty to embrace and reflect the recent advancement in pharmacy practice. AI in pharmacy education is transforming how students learn and interact with the material. AI technologies can provide personalized learning experiences, adapt to individual student needs, and enhance the understanding of complex concepts. For example, AI-driven simulations and virtual patients allow students to practice clinical decision-making in a risk-free environment. Additionally, AI can assist in automating administrative tasks, giving educators more time to focus on teaching. This integration of technology not only improves educational outcomes but also prepares future pharmacists to effectively utilize AI in their practice.
1.1 What is known?
Pharmacy education now includes Digital tools like EHRs, AR, and tele pharmacy, enhancing student engagement and skills. While students view these tools positively, training in areas like tele pharmacy, mHealth, and AI still needs to be improved.
1.2 What is not known?
A standardized Digital Health curriculum needed to foster consistent Digital literacy. Critical gaps include training in AI ethics, data privacy, tele pharmacy, and research on the long-term effects of Digital Health education on clinical performance and patient readiness for tech-driven healthcare warranted.
1.3 What will the current study add?
The present scoping review examines the consequences of Digital Health on pharmacy education, identifying shortcomings in the curriculum and the approaches to uniform training of electronic literacy. It explores the assimilation of available technologies like AI, mHealth, and tele pharmacy and finds lacunae between the programs and suitable modes of training. The review emphasizes hands-on training to help students gain competence and confidence. It advocates long-term studies to evaluate real-world impacts and calls for ethics-focused training on AI, promoting better preparation for pharmacy students in Digital healthcare roles.
1.4 Rationale
Tele therapeutic, telemedicine, Telehealth, m-health, mobile-health, smart apps, e-health, tele pharmacy, and EHRs are examples of Digital Health technologies that are increasingly integrated into pharmacy education to prepare students for a Digital healthcare environment. While there is evidence of positive outcomes, such as improved clinical decision-making, the research on Digital Health in pharmacy education is scattered and lacks coherence. A scoping review is ideal for exploring this broad area, as it includes diverse study designs and methodologies.
1.5 Objective
The current scoping review collates and appraises the impact of Digital Health on pharmacy education, evaluating effects on learning outcomes, skill development, competencies, and readiness for tele pharmacy and Digital Health application transformations. The primary objective was to explore the impact of Digital Health (eHealth, mHealth, e learning, telehealth, AI, telemedicine, tele pharmacy, VR, ML, and AR) in pharmacy education via structured scoping review reporting.
2 Methods
The Protocol developed to conduct the current scoping review not registered in PROSPERO. Eligibility criteria the inclusion criteria for this review encompass studies published between 2019 and 2024, focusing on Digital Health interventions in pharmacy education (e-Health, mHealth, e-learning, mobile health, smart apps, telehealth, AI, telemedicine, tele pharmacy, VR, ML, and AR). Any type of study using Digital Health interventions compared to traditional learning methods in pharmacy education with population defined as pharmacy students were deemed eligible for inclusion. Restriction imposed to studies published in English language. The specific outcomes included increased student engagement, active learning, long-term knowledge retention, improved academic performance and high student satisfaction.
The selection period was limited to the past 5 years to capture the most recent developments in Digital pharmacy education. Studies lacking full-text availability or those from non-peer-reviewed sources excluded to ensure the inclusion of high-quality evidence. Studies with multiple outcomes and studies not specific to pharmacy education were excluded from the review.
The information sources for the current review included a comprehensive literature search across multiple databases: PubMed, Cochrane Library, Web of Science, Scopus, CINAHL, and Embase. The search process adhered to the PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist (Supplementary Appendix 1). Whereby a systematic approach applied to study identification, screening, and inclusion of relevant articles on Digital Health (smart apps, eHealth, mHealth, e learning, telehealth, AI, ML, telemedicine, tele pharmacy, VR, and AR). A detailed Search strategy applied in EMBASE, PubMed, Scopus, CINHAL, and Cochrane Library. The following keywords and BOOLEEN used (“Digital Health” OR “e-learning” OR “telehealth” OR “eHealth” OR “mHealth” OR “tele-pharmacy” OR “telemedicine” OR “artificial intelligence” OR “virtual reality” OR “augmented reality” OR “big data” OR “machine learning”) AND (“pharmacy education” OR “pharmacists” OR “pharmaceutical care” OR “students”) AND (“interventions” OR “implementation” OR “curriculum” OR “programs” OR “training”). The selection for sources of evidence involved two steps to select articles for the current scoping review. In the initial screening, the titles and abstracts of the included articles used to evaluate their relevance. In the second step, a complete reading of the paper to ensure the eligibility of each study based on the pre-identified inclusion and exclusion criteria. A standardized data charting form developed [using the Joanna Briggs Institute (JBI) data extraction tool] (Supplementary Appendix 2), was tested to ensure its effectiveness in systematically capturing relevant data encompassing smart apps, ML, Digital Health (e-Health, mHealth, e-learning, telehealth, AI, telemedicine, tele pharmacy, VR, and AR). The extracted variables for data items included: study characteristics (author, year, country), intervention details (type of Digital Health tool, duration), outcomes (learning outcomes, student satisfaction), and assessment of the impact on pharmacy education. The critical appraisal of individual sources of evidence (Supplementary Appendix 3) accomplished using the Mixed Methods Appraisal Tool (MMAT) to assess the methodological quality of the selected and included studies. The synthesis of results is performed by thematic analysis, grouping articles based on types of Digital Health interventions and their reported impact on pharmacy education.
3 Results
For the current review, 2077 identified from databases sources related to the impact of Digital Health in education and 86 from registers. Records removed before screening due to duplicate records (n = 334), marked as disqualified (n = 217), and (666) for other reasons. Records screened (n = 860) while (n = 392) records excluded. Reports sought retrieval (n = 468), deemed relevant and assessed for eligibility. Reports assessed for eligibility were (n = 116) while (n = 352) reports not retrieved. Reports excluded for lack of relevance (n = 54) and insufficient data (n = 22). Ultimately, 47 studies were included in the current scoping review. The others excluded due to lack of relevance or insufficient data or not specific to the impact of Digital Health on pharmacy education. Results of search depicted on the PRISMA flow chart for included studies (Figure 1). The characteristics of sources of evidence of the included articles charted based on crucial information such as the authors and publication year, the study design, the Digital Health interventions, and the outcome measures. A Critical appraisal within sources of evidence of the included articles, adapted for practice settings, the clarity of the Digital Health interventions, and the reliability of outcome assessments related to patient care. Twenty-eight out of forty-seven studies scored highly in participant selection and intervention clarity, while twenty had less clear outcome measures.
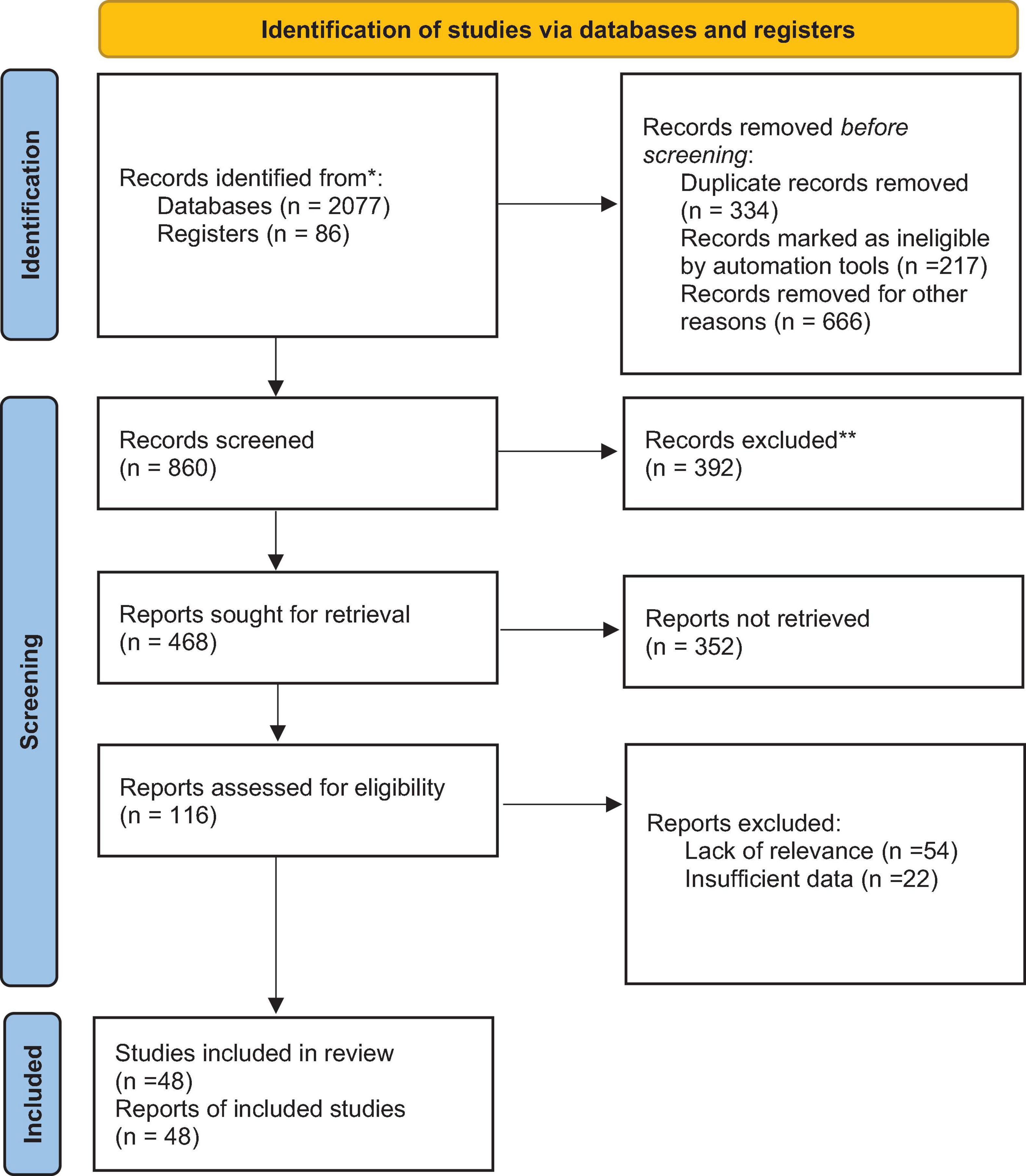
Figure 1. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
3.1 Results of individual sources of evidence
The results of individual sources of evidence comprehended that the review synthesizes findings on the integration of Digital Health tools in pharmacy education, organized under five thematic areas. The five thematic areas comprised curriculum integration and transformation in pharmacy education; Digital literacy (competency development); tele pharmacy (remote health services and AI) in education; practical skill development (interactive learning through Digital tools) and, student and faculty perceptions, attitudes, and challenges) in adopting Digital Health. Each theme is examined through observational and original studies.
3.2 Theme 1: curriculum integration and transformation in pharmacy education
A study on mHealth applications found that pharmacy students familiar with adherence apps demonstrated more excellent knowledge and acceptance of Digital Health, highlighting the benefits of curriculum alignment with Digital Health advancements (13). Blended learning preferences among pharmacy students in Ireland indicated a strong preference for recorded lectures, but challenges like social isolation highlighted the need for support in technology-enhanced learning (14). Faculty perspectives at United States of America (USA). Pharmacy schools emphasize the positive impact of telehealth integration on student engagement and support for Digital Health tools within the curriculum (15). Studies on curriculum transformation indicate the critical role of Digital Health tools, particularly during the COVID-19 pandemic, in enhancing curriculum flexibility and maintaining educational standards (8). A global survey revealed that only 43% of pharmacy programs offer formal Digital Health training, with those that do report positive impacts on students’ Digital readiness (16). A comparison of EHRs training approaches in USA schools revealed varying comfort levels among students, with extracurricular experience in EHRs further boosting confidence (4). Tele pharmacy readiness was explored at the University of Tennessee Health Science Center, where pharmacy students showed positive attitudes, albeit limited knowledge of tele pharmacy, indicating a need for further training (17). Variations in curriculum quality across Canada and the UK show that students seek more comprehensive Digital Health training to support their professional development (17). Applying the Taba model to rural health courses at the University of Wisconsin-Madison increased student engagement and competence in Digital Health skills, preparing them for rural healthcare (18) (Table 1). The topic of workload and curriculum overload concerns in the use of Digital technology in pharmacy education highlights the challenges faced by both educators and students. With the increasing integration of Digital tools and online resources, there is a risk of overwhelming students with excessive material and assignments. It’s crucial to strike a balance between embracing technology to enhance learning and ensuring that the curriculum remains manageable. Some potential concerns include: (1) Increased expectations: Digital platforms may lead to higher expectations for students to engage with Supplementary material, which could contribute to stress and fatigue. (2) Accessibility issues: Not all students may have equal access to technology, potentially widening the gap between those who can fully benefit from Digital resources and those who cannot. (3) Quality versus quantity: There’s a need to focus on the quality of educational content rather than just adding more resources, ensuring that each component serves a clear educational purpose. (4) Support for educators: Faculty members may require additional training to effectively integrate technology into their teaching strategies without creating an overwhelming workload. Addressing these concerns is essential for optimizing pharmacy education and ensuring that the incorporation of Digital technologies enhances, rather than detracts, the learning experience.
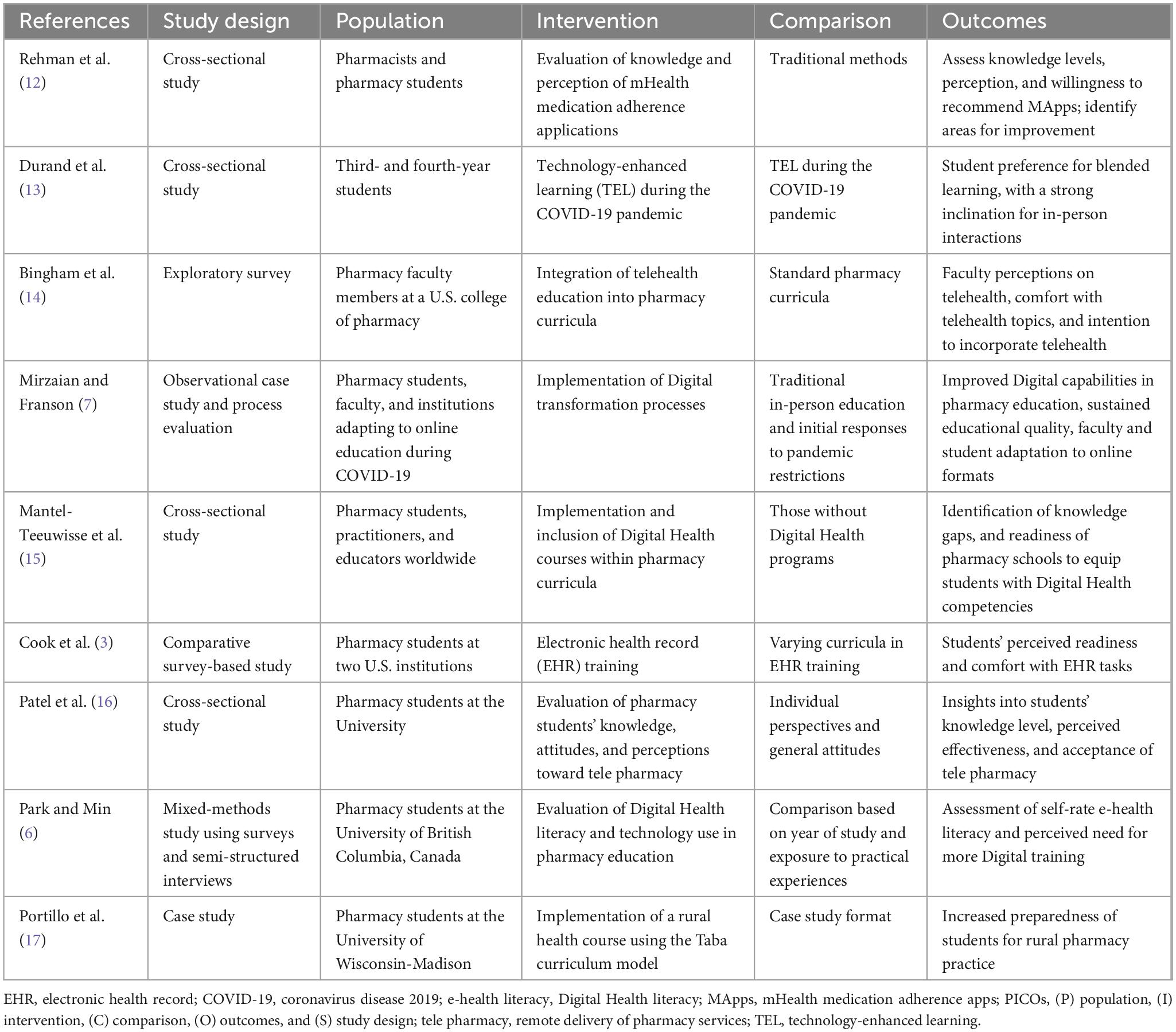
Table 1. P for population, I for intervention, C for comparison, O for outcomes, and S for study design (PICOs) of selected studies on curriculum integration and transformation in pharmacy education.
3.3 Theme 2: Digital literacy and competency development
Throughout countries, pharmacy students reported to have varying levels of Digital literacy. The South Indian pharmacy students who used AI for self-medication expressed concerns about the risks associated with self-prescribing, hence emphasizing the need for the provision of guidance on AI literacy in pharmacy education (19). Nottingham University’s co-creation of Digital learning resources with pharmacy and veterinary students enhanced Digital competencies and engagement in Digital Health education (20). Studies in Jordan, Palestine, and the broader Middle East and North Africa (MENA) region identified generally positive attitudes toward AI but noted concerns over data 0 security and ethical implications (21, 22). Malaysian pharmacy students exhibited strong electronic health (eHealth) literacy but expressed doubts about their ability to use Digital Health tools in clinical settings, highlighting the need for curriculum improvements (23). In Turkey, higher eHealth literacy observed among students who use mobile health apps frequently, which underlines the need for repeated engagement with Digital resources regarding Digital competencies (24) (Table 2). Digital literacy initiatives have shown promising results. A study using wearable devices like continuous glucose monitoring (CGM) and blood pressure (BP) monitors demonstrated that students improved significantly in interpreting health data, preparing them for modern Digital Health practices (25). A Digital pharmacy training program using AR significantly enhanced knowledge of diabetes management and practical Digital skills among pharmacy students in Indonesia (26). Digital skills training improved reading comprehension among Indonesian pharmacy students, significantly increasing proficiencies in browsing, presenting, and video conferencing (27). Training with EHRs improved Digital readiness and competency in navigating health records among pharmacy students, with students demonstrating heightened accuracy in clinical tasks, reinforcing the need for Digital training in core pharmacy curricula (28) (Table 2).
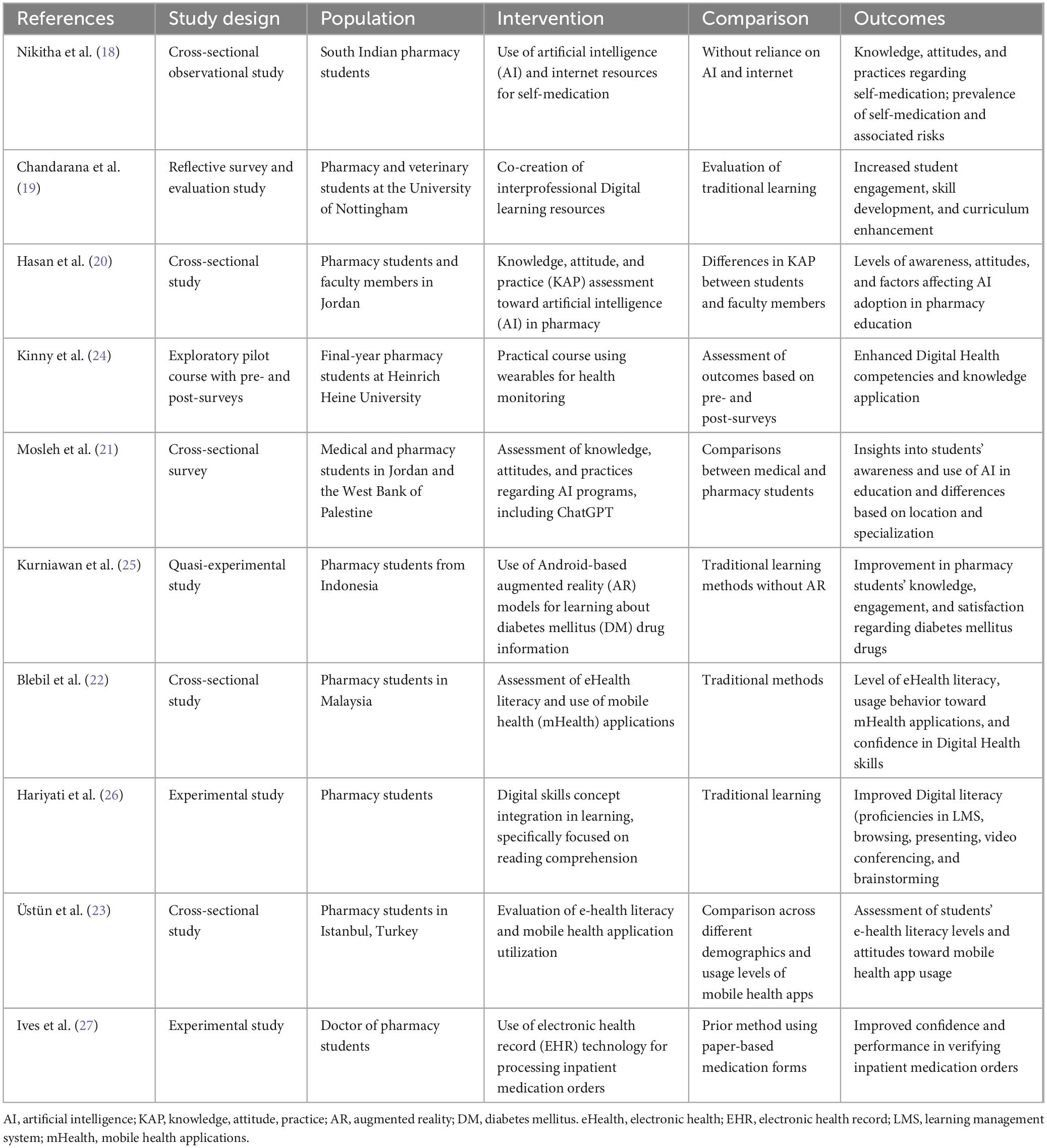
Table 2. P for population, I for intervention, C for comparison, O for outcomes, and S for study design (PICOs) of selected studies on Digital literacy and competency development.
3.4 Theme 3: tele pharmacy, remote health services, and AI in education
The tele pharmacy training in pharmacy programs positively perceived, though challenges remain. Pharmacy students in Saudi Arabia supported tele pharmacy education, though faculty limitations in expertise and resources posed difficulties (29). In the MENA region, students expressed concern over the ethical aspects of AI, primarily related to privacy and potential job displacement (30). A cross-sectional survey of Digital literacy among pharmacy students in Iraq showed that students found ChatGPT beneficial for academic tasks, though it posed concerns over critical thinking skills (31). Indonesian students studying tele pharmacy viewed it positively for improving access but noted that limited prior knowledge was a significant barrier to tele pharmacy adoption (32). A tele pharmacy module developed for pharmacy students in Malaysia enhanced students’ confidence in virtual healthcare, underscoring the value of practical tele pharmacy training (12). Malaysian students showed high awareness and positive attitudes toward tele pharmacy, though they expressed concerns over workload and necessary incentives (33) (Table 3). Original research studies validate the efficacy of tele pharmacy training. A non-inferiority trial in Germany found tele pharmacy training for inhaler techniques as effective as in-person training, with high student satisfaction reported (34). USA pharmacy students view the tele pharmacy as an effective tool to improve healthcare access in rural areas, although relationship building was a noted barrier (35). A study finding revealed that on-campus objective structured clinical examinations (OSCEs) are preferred for interaction and skill assessment. However, virtual OSCEs offer flexibility and could be improved for practical skill training (36). Pharmacy students in Iraq and the United Arab Emirates (UAE) highlighted the value of AI tools like ChatGPT in academic efficiency. However, they were concerned about the influence AI will have on traditional learning skills (37), (Table 3).
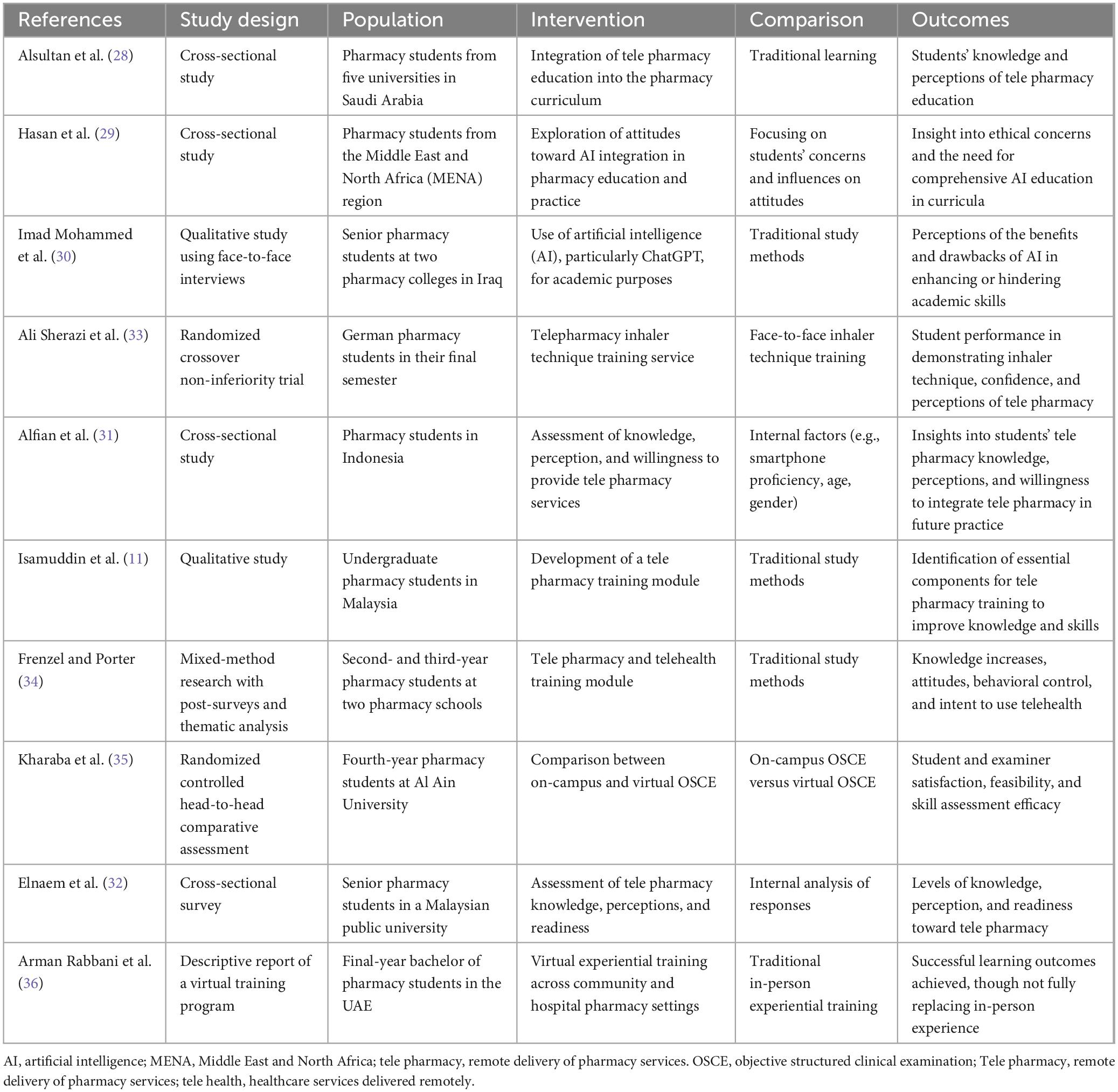
Table 3. P for population, I for intervention, C for comparison, O for outcomes, and S for study design (PICOs) of selected studies on tele pharmacy, remote health services, and AI in education.
3.5 Theme 4: practical skill development and interactive learning through Digital tools
The use of Digital tools has also contributed to the better development of practical skills. The tele pharmacy practice in Sweden positively supported, with students affirming its usefulness and expecting high technical competence standards in-patient care (3). The introduction of AI teaching tools enjoyed widespread acceptance in many regions, which gives an impression of positive performance when it comes to practical skill training (38). Interactive learning models, including group discussions and problem-solving, fostered better engagement and knowledge retention among pharmacy students in Macedonia (39) (Table 4). Interactive Digital tools have significantly enhanced student engagement in skill-based training. Pharmacy technicians in Spain who trained via Digital electronic learning (e learning) and simulations showed advanced competencies in sterile compounding and non-sterile preparation (40). AR-based diabetes education tools improved understanding and satisfaction among Indonesian students, showing the effectiveness of interactive technologies in pharmacy education (26). Pharmacy students in Germany improved their clinical pharmacy skills, particularly in diabetes management, by using Digital Health tools (41). A Digital pharmacy-training program conducted in Indonesia enhanced students’ practical skills and had high satisfaction rates, indicating the success of Digital tools in practical learning (9). USA pharmacy students in compounding labs using an AR application reported increased engagement and skill retention, demonstrating the value of Digital tools for experiential learning (42). AR and smart glasses in USA pharmacy labs increased student satisfaction and engagement, showing promise in supporting hands-on education (43). My Dispense virtual simulation in the USA effectively engaged students in self-care therapeutics, though no significant changes in confidence were reported (44). Remote experiential learning adaptations in Malaysia using My Dispense simulations helped retain dispensing skills, though face-to-face skills like communication were challenging to replicate (45) (Table 4).
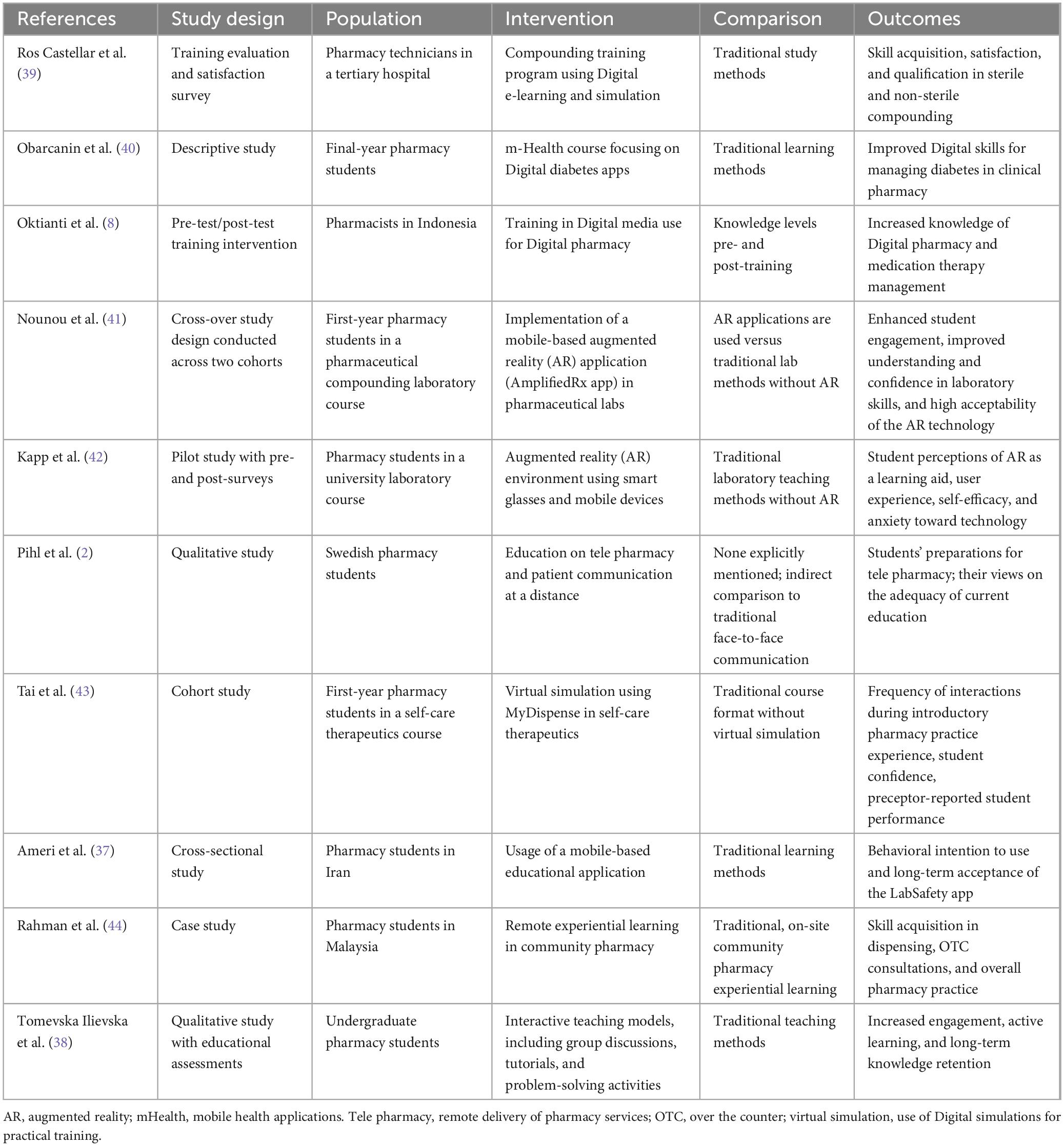
Table 4. P for population, I for intervention, C for comparison, O for outcomes, and S for study design (PICOs) of selected studies on practical skill development and interactive learning through Digital tools.
3.6 Theme 5: student and faculty perceptions, attitudes, and challenges in adopting Digital Health
Pharmacy students generally have an optimistic but cautious approach toward Digital Health. Students in 12 countries reported positive attitudes toward AI but were apprehensive about its potential impact on job security (46). In the U.K., pharmacy students recognized the importance of Digital literacy education in pharmacy curricula but noted the need for faculty development and curriculum enhancement (5). Pharmacy students in the USA using ChatGPT expressed high satisfaction but desired traditional learning to balance academic tasks (47). Virtual training feedback from Cairo University highlighted high student satisfaction, though session density needed adjustment to improve experiences (48). Digital versus printed poster preferences improved student engagement and accessibility, supporting Digital formats for learning (49). Electronic learning (e learning) well perceived in Mongolia as an alternative to traditional methods, though students preferred a hybrid approach combining Digital and hands-on experiences (50). A telehealth rotation study found that pharmacy students gained valuable experience in inter-professional telehealth collaboration (51). Students at a Virtual Annual Meeting liked the flexibility of Digital learning but preferred hands-on experience for skill building (10) (Table 5). Perception based studies offer solutions to the barriers that can hinder the use of Digital Health. A scoping review pinned 40 important Digital Health topics for medical students taught within knowledge, skills, and attitudes (52) (Table 5).
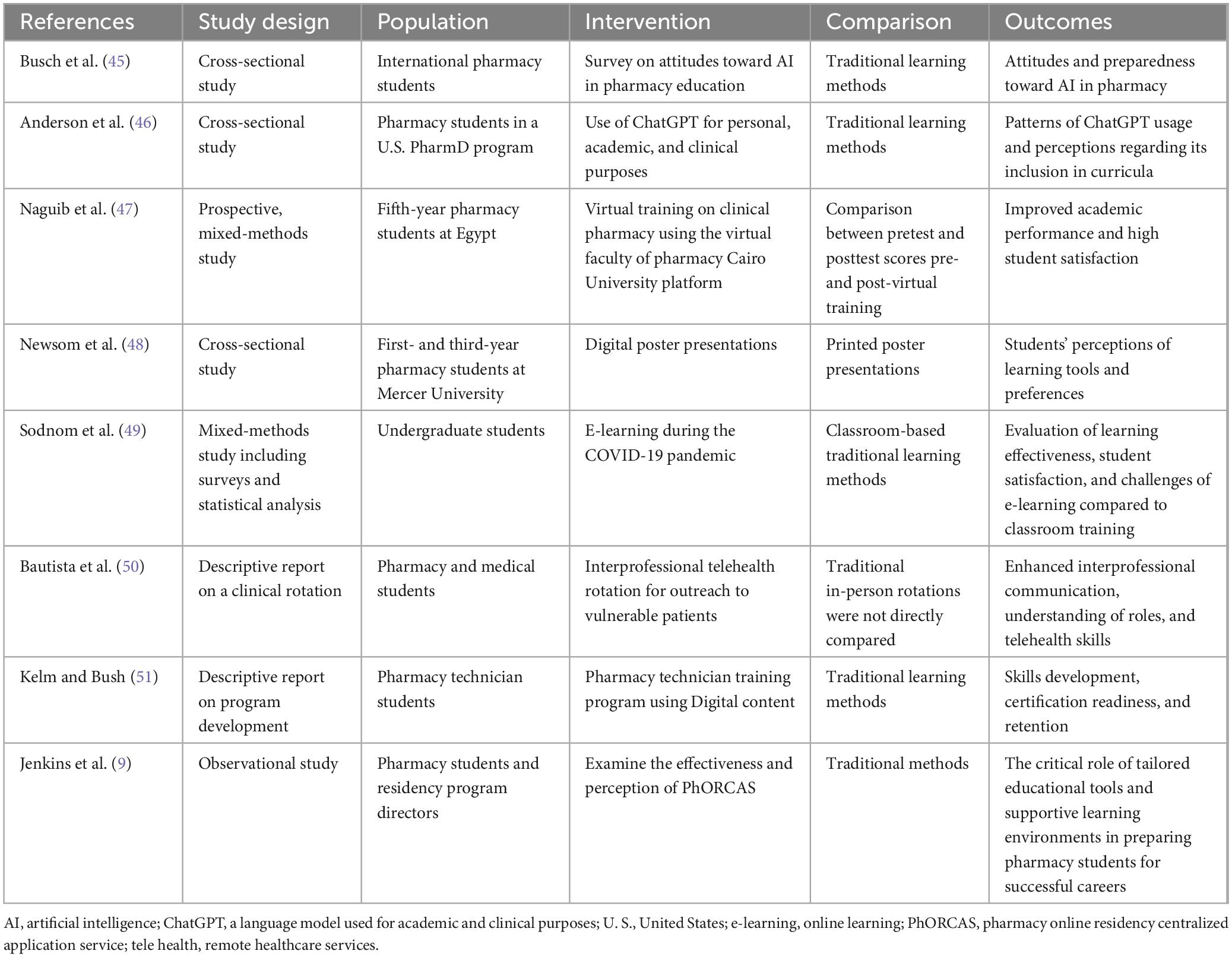
Table 5. P for population, I for intervention, C for comparison, O for outcomes, and S for study design (PICOs) of selected studies on student and faculty perceptions, attitudes, and challenges in adopting Digital Health.
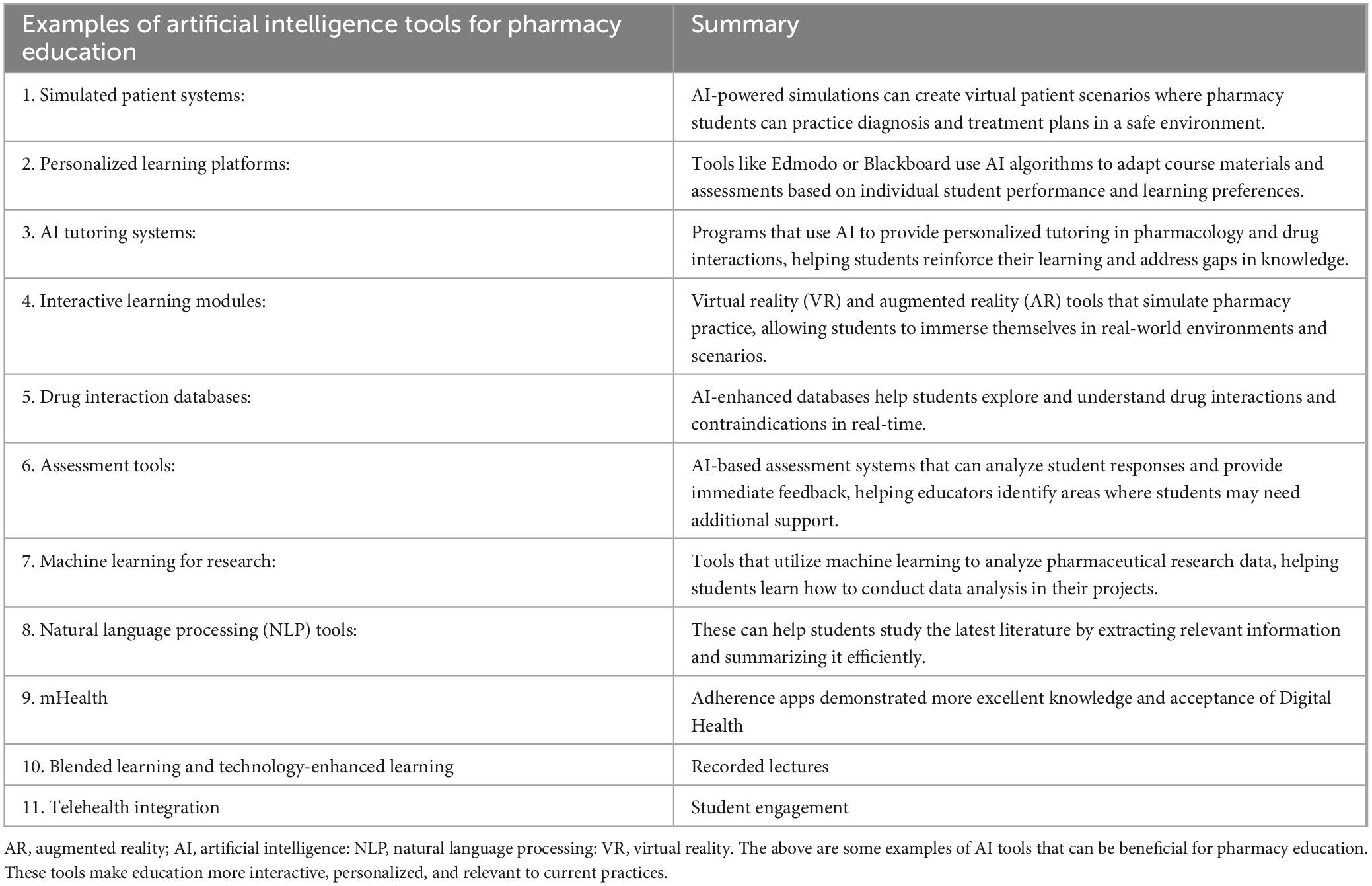
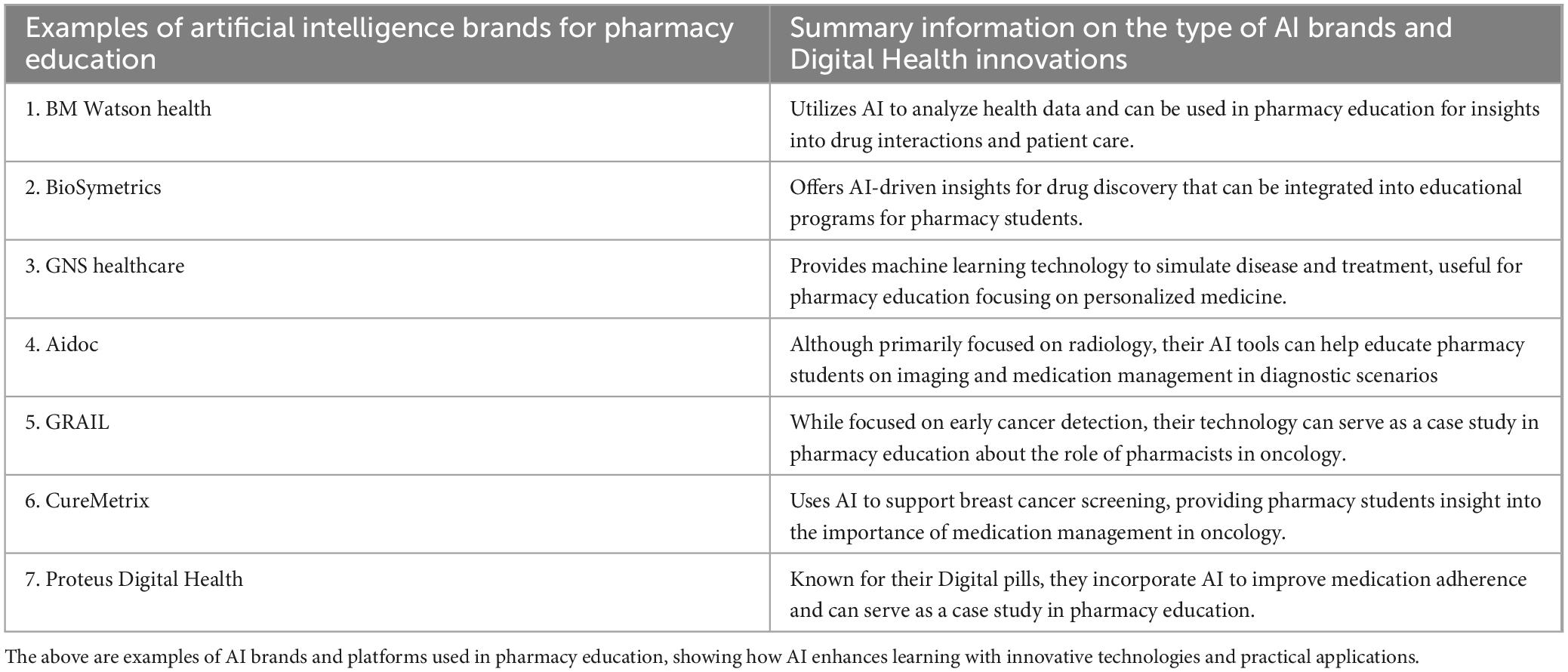
Table 6 depicted the advantages and disadvantages of Digital Health innovations in curriculum integration and transformation in pharmacy education. Further Table 7 have presented examples of AI tools for pharmacy education such as augmented reality (AR), Artificial Intelligence (AI), Natural Language Processing (NLP), Virtual reality (VR). These AI tools can be beneficial for pharmacy education that permit more interactive, personalized, and relevant learning to current practices. More examples of AI brands for Digital Health innovations in pharmacy education were exhibited in Table 8. These brands and platforms can be used in pharmacy education, showing how AI enhances learning with innovative technologies and practical applications.
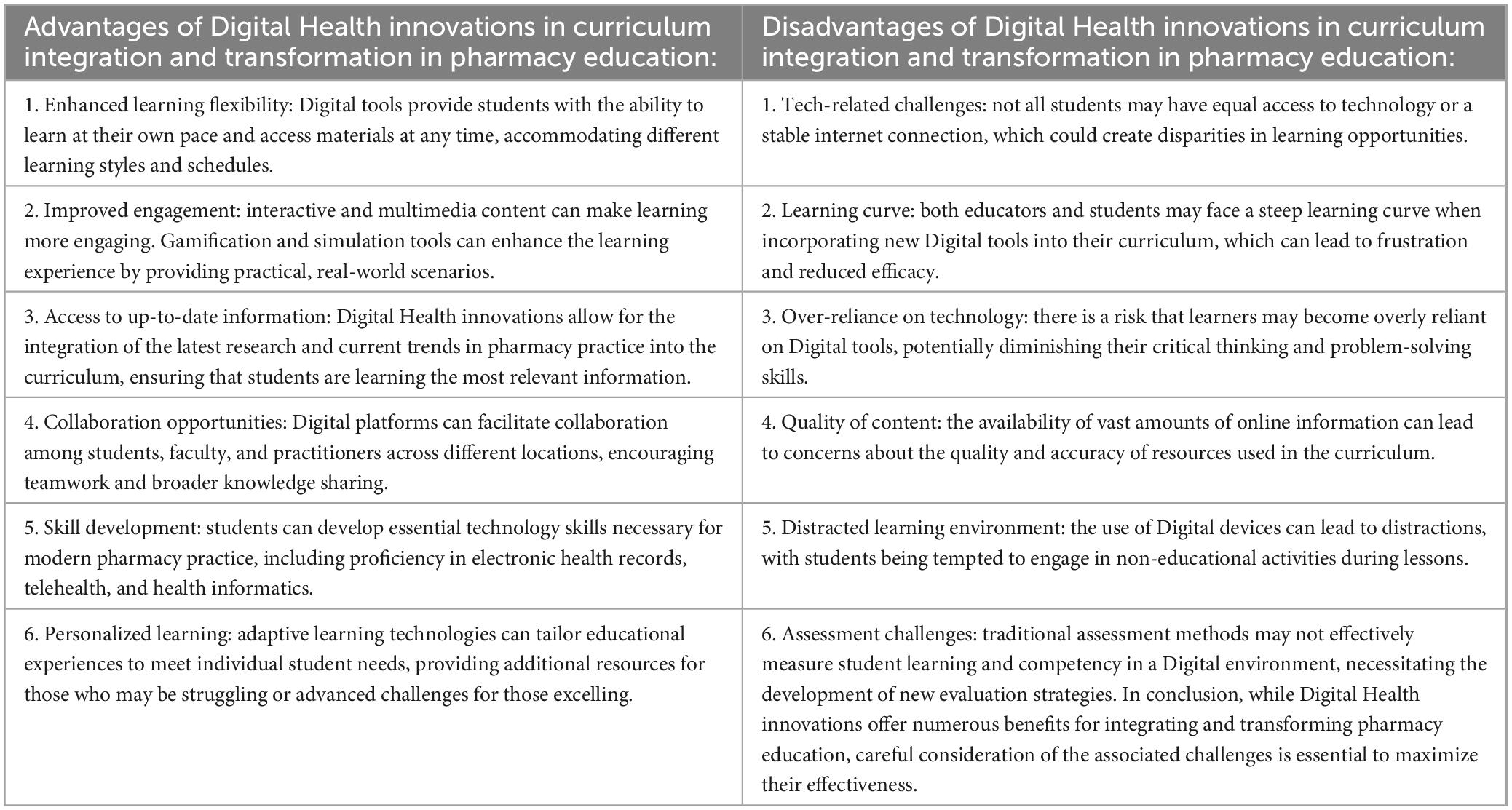
Table 6. The advantages and disadvantages of Digital Health innovations in curriculum integration and transformation in pharmacy education.
4 Discussions
4.1 Discussions and synthesis of results
In synthesizing these results, it became evident that Digital Health technologies are transforming pharmacy education. Digital Health enhances pharmacy education by improving skills, engagement, and confidence with tools like AI, AR, and EHRs. However, better curriculum integration, Digital literacy training, and ethical guidance are needed. Tele pharmacy and AI improve access but raise concerns about workload and critical thinking. Students value a mix of Digital and hands-on learning, calling for updated curricula and more robust faculty support. Some hands-on skills remain challenging to teach remotely.
4.1.1 Curriculum integration and transformation in pharmacy education (curriculum development)
The integration of Digital Health into pharmacy education curricula shows significant advancements, driven by responses to COVID-19 and the increasing demands of modern healthcare. Findings from studies across the USA, Malaysia, and Ireland illustrate a shared commitment to rapidly incorporating Digital Health tools like EHRs and tele pharmacy into pharmacy programs, albeit through differing approaches: the USA focus on meeting competency standards. At the same time, Malaysia and Ireland emphasize blended and fully remote models to address regional needs (8, 14, 45). Studies also reveal common challenges in maintaining interpersonal skill development in fully remote setups, highlighting the importance of hybrid learning approaches for skill retention (18).
4.1.2 Digital literacy and competency development (knowledge and competencies)
Digital literacy differs widely across pharmacy curricula, with research from Turkey, Malaysia, and MENA finding intermediate eHealth literacy levels among students, underscoring the importance of structured training (21, 23, 24). Notably, USA, and Indonesian studies demonstrate the successful use of AR and wearables to engage students in practical applications, bridging theory and real-world skills (25, 26). Hands-on EHR training also improves comprehension and data interpretation skills, showing that immersive Digital tools can effectively build essential pharmacy competencies (28). That aligns with previous reviews that examine Digital Health education, highlighting similar gaps in standardized curricula and calling for consistent competency frameworks (53, 54).
4.1.3 Tele pharmacy, remote health services, and AI in education (skills development)
Tele pharmacy and AI training are emerging areas, yet programs vary significantly in their adoption and focus. In Germany and the USA, tele pharmacy incorporated to prepare students for remote services, while Saudi Arabia and Indonesia show early interest with limited integration (29, 32, 34, 35). MENA region students express AI-related ethical concerns, contrasting with Western students who focus more on practical applications (30, 46). The findings underscore a gap, where Western programs lead Digital integration, while Middle Eastern and Asian programs prioritize foundational tele pharmacy education to address local needs (12, 36). The impact of Digital Health innovations on pharmacy education can be framed through the lens of several key concerns regarding artificial intelligence (AI), which can resonate as a unified theme across different regions.
The impact of Digital Health Innovations on pharmacy education concerns about AI (privacy, self-medication, overreliance) may provide some insights as unified strategy across regions. Firstly, the concern of privacy, as AI systems integrate into pharmacy practice, the handling of sensitive patient data becomes crucial. Pharmacy education must address the ethical implications and legal responsibilities surrounding patient privacy. Students should be taught the importance of data protection and the implications of breaches, emphasizing the need for robust systems to safeguard personal health information, regardless of regional regulations. Secondly, with the rise of Digital Health tools, patients increasingly engage in self-medication based on online information. Pharmacy education should highlight the role of pharmacists in guiding patients to make informed decisions about their health. A unified educational approach can cultivate a global understanding of the risks associated with self-medication and the pharmacist’s role in patient education, promoting safer practices internationally. Lastly, the convenience of AI and Digital Health tools may lead to overreliance on these technologies, potentially undermining clinical judgment and traditional pharmaceutical knowledge. Pharmacy curricula should balance Digital Health innovations with core competencies, ensuring that future pharmacists retain critical thinking skills and the ability to make informed decisions without solely depending on technology.
By addressing these concerns through a unified theme of education, pharmacy programs can prepare students to navigate the complexities of Digital Health innovations responsibly. This holistic approach fosters a global community of pharmacists equipped to adapt to technological advancements while prioritizing patient welfare and ethical practices.
4.1.4 Practical skill development and interactive learning through Digital tools (skills and competencies development)
Interactive Digital tools are increasingly integral to skill development in pharmacy education. In Germany and the USA, mHealth and AR used to enhance engagement, and similar successes reported with AR in Indonesia and Spain, particularly in compounding labs (26, 40, 41, 43). Malaysian remote experiential training highlights challenges in replicating interpersonal interactions, whereas AR-based training preserves hands-on learning benefits (45). These findings collectively support hybrid-learning models to achieve optimal skill acquisition.
4.1.5 Student and faculty perceptions, attitudes, and challenges in adopting Digital Health (student and faculty development)
Student and faculty perceptions reveal both enthusiasm and caution toward Digital Health technologies. Positive feedback includes increased engagement and skill development, especially with tools like ChatGPT and EHRs in USA, and Iraqi programs (28, 31). However, ethical and workload concerns regarding AI and tele pharmacy training in MENA and Southeast Asia highlight differing cultural perspectives on Digital Health adoption (21, 33). A previous review underscores ethical challenges in incorporating AI into pharmacy education, including tool generalizability and legal implications (54). Studies investigating a Digital and traditional learning approach in countries like Mongolia suggest that while Digital platforms offer theoretical learning comparable to a classroom, skills acquisition remains best in practical settings (50). These findings suggest that one potential way to increase the effectiveness of Digital Health training across several educational contexts is by using Digital and analogue tools simultaneously.
The benefits of Artificial Intelligence in pharmacy education are numerous and can significantly enhance the learning experience for students and improve the overall educational process. Via personalized learning AI can tailor educational content to meet individual students’ needs, helping them grasp complex concepts at their own pace. This customization can lead to improved understanding and retention of syllabi. Further, interactive learning environments provided by AI-powered tools can provide immersive simulations and interactive scenarios that make learning more engaging. This hands-on approach can help students apply theoretical knowledge in practical situations. AI can assist students in quickly finding relevant research papers, case studies, and clinical guidelines, enhancing their ability to stay updated with the latest developments in pharmacy (access to vast resources). AI can streamline the assessment process by providing instant feedback on quizzes and assignments (assessment and feedback). This timely information allows students to identify areas where they need improvement and foster continuous learning. AI can analyze trends and patterns in student performance, helping educators identify at-risk students early and implement targeted interventions to support their success (predictive analytics). AI can aid in drug discovery and pharmacological research, providing students with valuable insights into the latest technologies and methodologies being used in the field. AI can assist with administrative responsibilities, allowing educators to spend more time focusing on teaching and mentoring students. AI platforms can facilitate collaboration among students (collaborative learning), enabling them to work on group projects and share knowledge more effectively, regardless of their geographical locations. By integrating AI into pharmacy education, institutions can enhance educational experience, better prepare students for their careers, and ultimately improve healthcare outcomes (18, 20, 21, 29, 30, 33).
The benefits of telepharmacy in pharmacy education are numerous and impactful. First, tele pharmacy can enhance access to educational resources and expertise, allowing students in remote or underserved areas to connect with experienced pharmacists and educators. This can lead to a more comprehensive and varied learning experience. Additionally, tele pharmacy facilitates the use of technology and Digital tools, making pharmacy education more interactive and engaging. Students can participate in virtual simulations, webinars, and online discussions, which can help them develop critical thinking and problem-solving skills in real-time scenarios. Moreover, tele pharmacy can also promote flexibility in learning. Students can schedule their classes or meetings around their availability, making it easier for them to balance their studies with other commitments. Furthermore, this approach encourages collaboration among peers and professionals across various locations. Students can engage in group projects and discussions with individuals from diverse backgrounds, enriching their educational experience and preparing them for teamwork in their future careers. Lastly, tele pharmacy can improve patient care training by allowing students to observe and participate in consultations and medication management scenarios remotely. This exposure is invaluable as it reflects the changing landscape of pharmacy practice and prepares students for the realities of modern healthcare. Overall, the integration of tele pharmacy into pharmacy education is a promising development that can enhance learning, accessibility, and the overall quality of education for future pharmacists (11, 28, 31, 34).
In summary the current scoping review outlined the importance of Digital Health on pharmacy education, influence on learning outcomes, pertinent skill development, and deemed |competencies, for the transformations.
4.2 Implementing Digital Health innovations in pharmacy education
Implementing Digital Health innovations in pharmacy education presents several challenges that can be thought of for structured implementation process: (1) Curriculum Integration: One of the primary challenges is incorporating Digital Health technologies into the existing pharmacy curriculum. There needs to be an alignment between traditional pharmacy education and emerging Digital Health trends, which often require curriculum redesign and workload distribution. (2) Technological Infrastructure: Many educational institutions may lack the necessary technological infrastructure to support Digital Health innovations. This includes both hardware (e.g., computers, software) and reliable internet access. (3) Faculty Development and Training: Educators may not have the requisite knowledge or skills to teach Digital Health innovations effectively. Providing adequate training and resources for faculty members is crucial to ensure they can guide students in this area. (4) Funding and Resources: Implementing new Digital Health technologies often requires significant investment. Budget constraints can limit the ability of institutions to adopt and sustain these innovations. (5) Student Engagement: Engaging students with Digital Health tools can be challenging. It’s essential to ensure that students see the value of these innovations in their future practice to foster interest and participation. (6) Regulatory and Compliance Issues: Navigating the regulatory landscape associated with Digital Health can be complex. Pharmacy education programs need to stay updated with changes in laws, AI ethics, and regulations governing Digital Health practices. (7) Interprofessional Collaboration: Digital Health often requires collaboration across various healthcare disciplines. Facilitating interprofessional education to prepare pharmacy students for a collaborative healthcare environment can be difficult but is essential. (8) Assessment of Learning Outcomes: Developing appropriate metrics to assess the effectiveness of Digital Health training in pharmacy education can be challenging. Institutions need to ensure that learning outcomes are met and that students are adequately prepared for real-world applications and regional disparities. Addressing these challenges requires a concerted effort from educational institutions, healthcare organizations, and stakeholders in the pharmacy field to create an environment conducive to the successful implementation of Digital Health innovations.
4.3 Summary of evidence
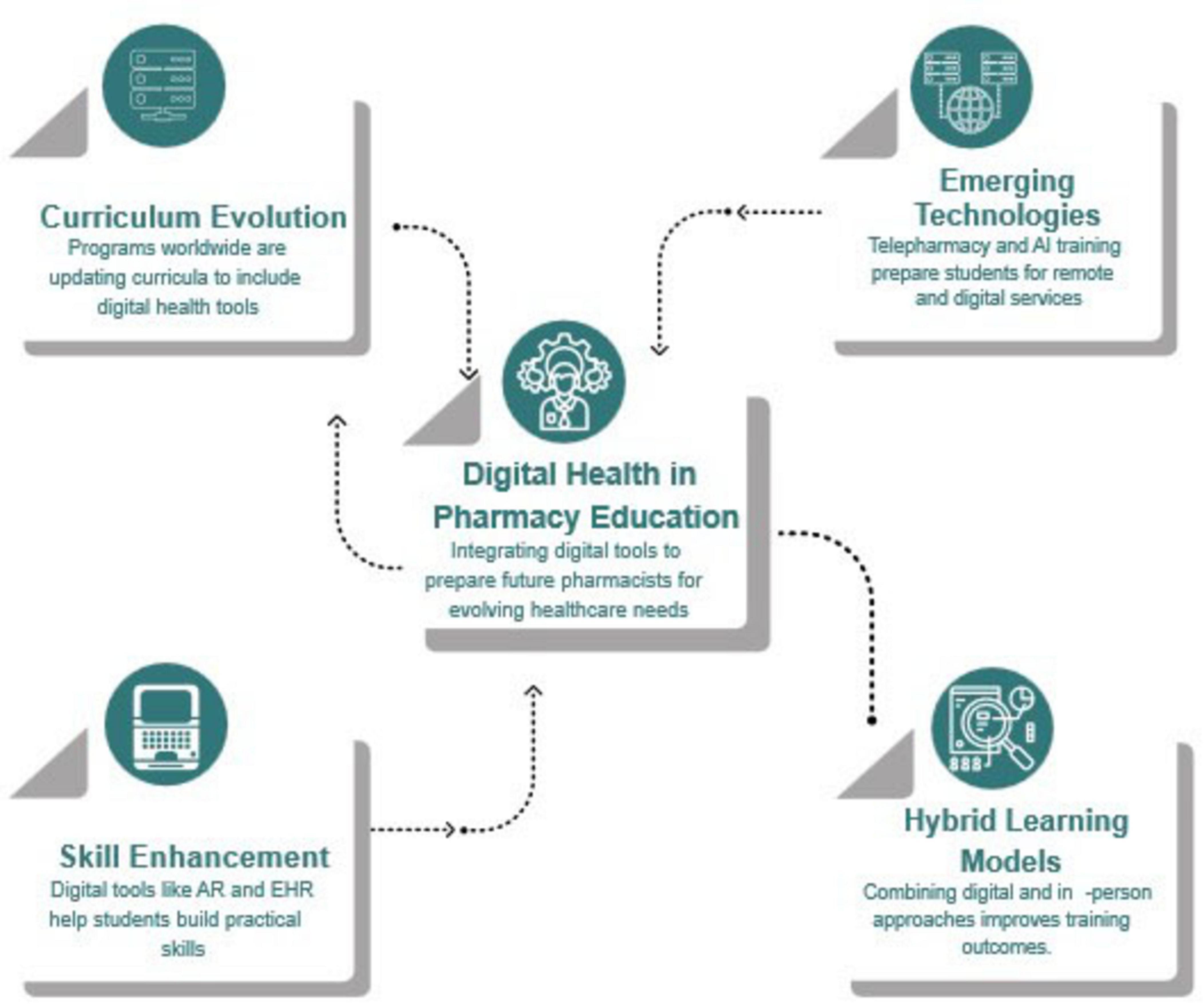
Students obtain excellent proficiency in tele pharmacy and Digital literacy due to the introduction of health technologies in pharmacy training. It is, above all, encouraging, but potential issues such as regional disparities, AI ethics, workload efficiency, energy and level of organization of students and teachers deserve further emphasis. The main key findings illustrated in (Figure 2). The structured results of the impact of Digital Health innovation on pharmacy education have led to significant advancements in the field. These innovations have not only enhanced the quality of education but have also instilled a strong sense of confidence in the findings derived from this research. By systematically analyzing the effects of Digital tools and technologies, educators and practitioners have been able to identify effective teaching methods, improve engagement, and ultimately prepare pharmacy students for the evolving landscape of healthcare. This quality work serves as a solid foundation for future studies and applications, ensuring that the integration of Digital Health in pharmacy education continues to yield positive outcomes (Tables 1–5).
The value added by the current scoping review versus prior reviews, contributes significantly to the existing literature on Digital Health innovation in pharmacy education by providing a comprehensive synthesis of recent advancements and trends. Unlike prior reviews, which may have focused on specific aspects or limited timeframes, this review encapsulates a broader range of studies and evidence, highlighting the evolving nature of Digital tools and their implications for educational practices. Additionally, this review addresses gaps identified in earlier works, such as the practical application of Digital Health innovations in curriculum development and student learning outcomes. By analyzing a wider variety of Digital Health technologies and their educational impacts, the current review offers a more nuanced understanding of how these innovations can enhance pharmacy education. Furthermore, it emphasizes the importance of interdisciplinary collaboration and the integration of Digital Health into pharmacy training, providing actionable insights for educators and policymakers. Overall, this scoping review not only updates the discourse but also sets the stage for future research in the field.
4.4 The significance for the impact of versatile Digital Health innovations on pharmacy education
The significance of versatile Digital Health innovations on pharmacy education is profound and multifaceted. As the healthcare landscape continues to evolve, pharmacy education must adapt to incorporate new technologies that enhance learning and improve patient care. The current review summarizes major significance in this context: (1) Enhanced Learning Opportunities: Digital Health innovations provide access to a wealth of resources and learning tools. This includes online courses, virtual simulations, and interactive platforms that engage students in real-world scenarios, making education more dynamic and accessible. (2) Inter-professional Collaboration: Digital Health tools often facilitate communication and collaboration among different healthcare professionals. Pharmacy education that incorporates these technologies prepares students to work effectively in interdisciplinary teams, essential for coordinated patient care. (3) Data-Driven Decision Making: With the rise of big data in healthcare, pharmacy education is increasingly integrating data analysis into curricula. Understanding how to interpret and leverage data is crucial for pharmacists to make informed clinical decisions and improve patient outcomes. (4) Remote Patient Monitoring: Innovations in telehealth and remote monitoring allow pharmacy students to understand modern patient management techniques. Learning to utilize these technologies prepares students to manage medication therapy and patient consultations effectively, regardless of location. (5) Focus on Personalized Medicine: Digital Health innovations are at the forefront of personalized medicine, which tailors’ treatment to individual patients. Pharmacy education that emphasizes these innovations helps students understand the importance of customizing medication regimens based on genetic, environmental, and lifestyle factors. (6) Adaptability to Change: The fast pace of technological advancements requires pharmacy students to be adaptable and agile learners. Incorporating these innovations into education fosters a mindset that embraces continual learning and adaptability in practice. Overall, the integration of versatile Digital Health innovations into pharmacy education not only enhances the learning experience but also ensures that future pharmacists are well equipped to thrive in a rapidly changing healthcare environment.
4.5 Limitations
Limitations included potential biases in the selection of studies and the included studies published only between 2019 and 2025, which may have missed other studies that would have affected the result. Further the challenge of measuring the long-term impact of Digital Health training on student outcomes and professional practice may limit the findings. As a scoping review, the assessment of methodological quality was limited. Generally, during conducting the current scoping review on the impact of versatile Digital Health innovations on pharmacy education, several limitations encountered. (1) Variability in Digital Health Innovations: The wide range of Digital Health tools and technologies can make it difficult to assess their specific impacts consistently. Variations in features, target populations, and usage can lead to inconsistent findings. (2) Limited Evidence Base: There may be a lack of empirical studies specifically focusing on the impact of Digital Health innovations on pharmacy education. Many tools have been evaluated in clinical settings rather than educational contexts. (3) Quality of Included Studies: The quality and rigor of the studies that are included in the review can vary significantly. Some may not adhere to strong methodological standards, affecting the overall reliability of findings. (4) Publication Bias: Studies with positive findings more likely published. This can skew the review results since it may not represent negative outcomes or the lack of impact. (5) Rapidly Evolving Field: Due to the fast-paced nature of technological advancements, findings can quickly become outdated. This poses challenges in ensuring that the review is current and relevant. (6) Diversity of Educational Contexts: Pharmacy education varies significantly across different institutions and regions, which can affect how Digital Health innovations are integrated and their subsequent impacts. (7) Stakeholder Perspectives: The review might not adequately capture the perspectives of all stakeholders involved in pharmacy education, such as educators, students, and practitioners, which can limit understanding of the full impact. (8) Integration Challenges: Identifying how Digital Health innovations integrated into existing curricula and the challenges faced during this process can be difficult to assess. (9) Longitudinal Effects: Understanding the long-term impact of Digital Health innovations may require longitudinal studies, which are often underrepresented in the literature. Addressing these limitations in future reviews is crucial for drawing meaningful conclusions about the role of Digital Health innovations in enhancing pharmacy education.
5 Conclusion
The current scoping review emphasized that the integration of Digital Health in pharmacy education enhances the students’ readiness to form future professional pharmacy careers. Further it emphasized the importance of faculty developing, workload integration, regional disparities, and ethical concerns with AI and challenges in hybrid learning. Digital Health has been an innovator in pharmacy students’ education, equipping them with the skills and competences required in today’s healthcare environment. However, faculty development, curriculum gaps, workload integration, insufficient telehealth training, regional disparities, and inadequate AI ethics instruction all point to the need for adequate and relevant curriculum modifications to qualify graduates to deal with Digital healthcare challenges. Critical gaps remain in standardized curricula for Digital Health in pharmacy profession, incorporating comprehensive telehealth training, and increasing the emphasis on emerging technologies such as AI, ML, Large language Models (LLMs) and versatile mHealth tools. Addressing these gaps will ensure pharmacy graduates are well equipped to navigate and lead in a digitally driven healthcare environment.
Author contributions
FA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by Taif University, Saudi Arabia, Project No. (TU-DSPP-2025-26).
Acknowledgments
We extends appreciation to Taif University, Saudi Arabia, for supporting this work through project number (TU-DSPP-2025-26).
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1577494/full#supplementary-material
Abbreviations
AI, artificial intelligence; AR, augmented reality; BP, blood pressure; CGM, continuous glucose monitoring; COVID-19, coronavirus disease 2019; DM, diabetes mellitus; EHR, electronic health record; eHealth, electronic health; e-learning, online learning; KAP, knowledge, attitude, practice; LLMs, Large language Models; LMS, learning management system; ML, machine learning; MApps, mHealth medication adherence apps; MMAT, Mixed Methods Appraisal Tool; MENA, Middle East and North Africa; mHealth, mobile health applications; OSCE, objective structured clinical examination; OTC, over the counter; PhORCAS, pharmacy online residency centralized application service; PICOs, P for population, I for intervention, C for comparison, O for outcomes, and S for study design; TEL, technology-enhanced learning; Tele health, healthcare services delivered remotely; Tele pharmacy, remote delivery of pharmacy services; UAE, United Arab Emirates; U. K., United Kingdom; U. S., United States; VR, virtual reality.
References
1. Digital Health. Available online at: https://www.who.int/health-topics/digital-health/#tab=tab_1recommendations on digital interventions for health system strengthening (accessed October 29, 2024).2024
2. Pihl R, Eriksson I, Sporrong S, Wettermark B. Are Swedish Pharmacy Students Prepared for Patient Communication at a Distance?: A Focus Group Study on Pharmacy Students’ Views and Opinions on Telepharmacy and Pharmacy Education, with a focus on communication at a distance. (2021). Available online at: https://urn.kb.se/resolve?urn=urn:nbn:se:uu:diva-446762 (accessed October 24, 2024).
3. Cook K, Cochran G, Gali H, Hatch T, Awdishu L, Lander L. Pharmacy students’ readiness to use the electronic health record: a tale of two institutions. Curr Pharm Teach Learn. (2021) 13:327–32. doi: 10.1016/j.cptl.2020.11.005
4. Alowais M, Nazar H, Tolley C. Digital literacy education for UK undergraduate pharmacy students: a mixed-methods study. Int J Pharm Pract. (2024) 32:413–9. doi: 10.1093/ijpp/riae040
5. Frenzel J, Porter A. The need to educate pharmacy students in telepharmacy and telehealth. Am J Pharm Educ. (2021) 85:8566. doi: 10.5688/ajpe8566
6. Park J, Min J. Exploring Canadian pharmacy students’ e-health literacy: a mixed method study. Pharm Pract. (2020) 18:1747. doi: 10.18549/PharmPract.2020.1.1747
7. Mirzaian E, Franson K. Leading a digital transformation in pharmacy education with a pandemic as the accelerant. Pharmacy. (2024) 9:19. doi: 10.3390/pharmacy9010019
8. Oktianti D, Bangsa J, Hati A. Training on the use of digital media for implementation digital pharmacy for pharmacist at Salatiga in supporting the industrial revolution 4.0. Community Empowerment. (2022) 7:2091–9. doi: 10.31603/ce.7939
9. Jenkins Z, Cole J, Chen A, Harper N, Krauss Z. The role of PhORCAS database functions vs. traditional curriculum vitae in the pharmacy residency application cycle. Am J Pharm Educ. (2020) 84:819. doi: 10.5688/ajpe8220
10. Chen J, Yang J. Development and application of workbook teaching materials – taking the curriculum construction of pharmacy and traditional chinese medicine pharmacy in higher vocational colleges of pharmaceutical specialty group as an example. Educ Reform Dev. (2021) 3:5–9. doi: 10.26689/erd.v3i1.2612
11. Isamuddin N, Elnaem M, Kamil T, Nazar N. Identification of teaching and learning components of a telepharmacy training module for undergraduate pharmacy students in Malaysia: a qualitative study. Pharm Educ. (2023) 23:505–13. doi: 10.46542/pe.2023.231505513
12. Rehman W, Thanganadar H, Idrees S, Mehmood A, Azeez F, Almaimani H, et al. Knowledge and perception of mHealth medication adherence applications among pharmacists and pharmacy students in Jazan, Kingdom of Saudi Arabia. PLoS One. (2024) 19:e0308187. doi: 10.1371/journal.pone.0308187
13. Durand E, Kerr A, Kavanagh O, Crowley E, Buchanan B, Bermingham M. Pharmacy students’ experience of technology-enhanced learning during the COVID-19 pandemic. Explor Res Clin Soc Pharm. (2023) 9:100206. doi: 10.1016/j.rcsop.2022.100206
14. Bingham J, Axon D. Telehealth integration into pharmacy practice curricula: an exploratory survey of faculty perception. Pharmacy. (2023) 11:110. doi: 10.3390/pharmacy11040110
15. Mantel-Teeuwisse A, Meilianti S, Khatri B, Yi W, Azzopardi L, Gómez J, et al. Digital health in pharmacy education: preparedness and responsiveness of pharmacy programmes. Educ Sci. (2021) 11:296. doi: 10.3390/educsci11060296
16. Patel K. Assessment of knowledge, attitude, perception of pharmacy students towards telepharmacy. Appl Res Projects. (2021) 75:72. doi: 10.21007/chp.hiim.0072
17. Portillo E, Look K, Mott D, Breslow R, Kieser M, Gallimore C. Intentional application of the taba curriculum model to develop a rural pharmacy practice course. Innov Pharm. (2020) 11:2089. doi: 10.24926/iip.v11i1.2089
18. Nikitha B, Roopa K, Kynshi S, Chauhan R, Girish B, Srinivasan R. Artificial intelligence and internet influence on drug utilization: exploring self-medication trends in South Indian pharmacy students. Intelligent Pharm. (2024) 2:814–20. doi: 10.1016/j.ipha.2024.06.001
19. Chandarana P, Rickaby R, Sonnex K, Allegrucci C, Garcia-Ara A. Student co-creation of digital learning resources: an evaluation and reflection of veterinary pharmacy and care home pharmacy interprofessional education packages. Student Engag High Educ J. (2024) 5:203–27.
20. Hasan H, Jaber D, Al Tabbah S, Lawand N, Habib H, Farahat N. Knowledge, attitude and practice among pharmacy students and faculty members towards artificial intelligence in pharmacy practice: a multinational cross-sectional study. PLoS One. (2024) 19:e0296884. doi: 10.1371/journal.pone.0296884
21. Mosleh R, Jarrar Q, Jarrar Y, Tazkarji M, Hawash M. Medicine and pharmacy students’ knowledge, attitudes, and practice regarding artificial intelligence programs: jordan and west bank of palestine. Adv Med Educ Pract. (2023) 14:1391–400. doi: 10.2147/AMEP.S433255
22. Blebil A, Dujaili J, Mohammed A, Loh L, Chung W, Selvam T, et al. Exploring the eHealth literacy and mobile health application utilisation amongst Malaysian pharmacy students. J Telemed Telecare. (2024) 29:58–71. doi: 10.1177/1357633X221077869
23. Üstün G, Söylemez S, Uçar N, Sancar M, Okuyan B. Assessment of the pharmacy students’ e-health literacy and mobile health application utilization. J. Res. Pharm. (2022) 24:23–9. doi: 10.35333/jrp.2020.125
24. Kinny F, Schlottau S, Ali Sherazi B, Obarcanin E, Läer S. Digital health in pharmacy education: elective practical course integrating wearable devices and their generated health data. Explor Res Clin Soc Pharm. (2024) 15:100465. doi: 10.1016/j.rcsop.2024.100465
25. Kurniawan A, Puspita N, Yusmaniar T, Rajendra F. The effectiveness of using digital applications for diabetes mellitus with augmented reality models as learning media in pharmacy education. Pharm Educ. (2023) 23:53–9. doi: 10.46542/pe.2023.232.5359
26. Hariyati N. Impact of the digital skills concept in society 5.0 on pharmacy students reading comprehension. Int Conf Government Educ Manag Tourism. (2022) 1.
27. Ives A, Tucker S, Trovato J. Using electronic health record technology to teach inpatient medication order verification to pharmacy students. Am J Pharm Educ. (2020) 84:aje7534. doi: 10.5688/ajpe7534
28. Alsultan M, Baraka M, Alahmari A, Elrggal M, Mahmoud M, Alrasheed M, et al. Knowledge and perception of pharmacy students toward telepharmacy education in Saudi Arabia. Healthcare. (2024) 12:1806. doi: 10.3390/healthcare12181806
29. Hasan H, Jaber D, Khabour O, Alzoubi K. Perspectives of pharmacy students on ethical issues related to artificial intelligence: a comprehensive survey study. Res Sq. (2024) rs.3.rs-4302115. doi: 10.21203/rs.3.rs-4302115/v1
30. Imad Mohammed S, Lateef Jasim A, Azeez Al-Jumaili A, Mudher Mikhael E, Zuhair Ali F. Perceptions of senior pharmacy students towards the impact of artificial intelligence on university education and scientific writing: a qualitative study. Al-Rafidain. J Med Sci. (2024) 6:142–6. doi: 10.54133/ajms.v6i1.538
31. Alfian S, Khoiry Q, Andhika A, Pratama M, Pradipta IS, Kristina SA, et al. Knowledge, perception, and willingness to provide telepharmacy services among pharmacy students: a multicenter cross-sectional study in Indonesia. BMC Med Educ. (2024) 23:800. doi: 10.1186/s12909-023-04790-4
32. Elnaem M, Akkawi M, Al-Shami A, Elkalmi R. Telepharmacy knowledge, perceptions, and readiness among future malaysian pharmacists amid the COVID-19 pandemic. Indian J Pharm Educ Res. (2022) 56:9–16. doi: 10.5530/ijper.56.1.2
33. Ali Sherazi B, Sayyed S, Möllenhoff K, Läer S. Telepharmacy versus face-to-face approach in providing inhaler technique training service: a non-inferiority assessment among German pharmacy students. Integr Pharm Res Pract. (2024) 13:165–80. doi: 10.2147/IPRP.S468881
34. Frenzel J, Porter A. Design and assessment of telepharmacy and telehealth training in two pharmacy programs. Am J Pharm Educ. (2023) 87:aje8800. doi: 10.5688/ajpe8800
35. Kharaba Z, AlAhmad M, Ahmed Elnour A, Abou Hajal A, Abumweis S, Ghattas M. Are we ready yet for digital transformation? Virtual versus on-campus OSCE as assessment tools in pharmacy education. a randomized controlled head-to-head comparative assessment. Saudi Pharm J. (2023) 31:359–69. doi: 10.1016/j.jsps.2023.01.004
36. Arman Rabbani S, Wadhwa T, Sridhar S, Shareef J, Anwer Ali A, Rao P. Experiential training during COVID-19 pandemic: a virtual attachment experience from a college of pharmaceutical sciences in the United Arab Emirates Background and context. Pharm Educ. (2021) 21:51–5. doi: 10.46542/pe.2021.211.5155
37. Ameri A, Khajouei R, Ameri A, Jahani Y. Acceptance of a mobile-based educational application (LabSafety) by pharmacy students: an application of the UTAUT2 model. Educ Inf Technol. (2020) 25:419–35. doi: 10.1007/s10639-019-09965-5
38. Tomevska Ilievska E, Tonic Ribarska J, Trajkovic Jolevska S, Ancevska Netkovska K, Tofovikj Kjamilova M. Interactive Models in University Teaching: Application in Pharmacy Education. (2019). Available from: https://repository.ukim.mk:443/handle/20.500.12188/9903 (accessed October 24, 2024).
39. Ros Castellar F, Ruano Encinar M, Pérez Robles T, García Vázquez N, Casado Abad G, Sánchez Rubio L, et al. Training program in compounding for pharmacy technicians through a digital platform and simulation techniques. Farm Hosp. (2024): doi: 10.1016/j.farma.2023.07.019 Online ahead of print.
40. Obarcanin E, Ali-Sherazi B, Dabidian A, Schlottau S, Deters M, Läer S. Introducing m-health and digital diabetes apps in clinical pharmacy education in Germany. J Diabetes Clin Res. (2022) 4:17–9. doi: 10.33696/diabetes.4.051
41. Nounou M, Eassa H, Orzechowski K, Eassa H, Edouard J, Stepak N, et al. Mobile-based augmented reality application in pharmacy schools implemented in pharmaceutical compounding laboratories: students’ benefits and reception. Pharmacy. (2024) 10:72. doi: 10.3390/pharmacy10040072
42. Kapp K, Sivén M, Laurén P, Virtanen S, Katajavuori N, Södervik I. Design and usability testing of an augmented reality (AR) environment in pharmacy education—presenting a pilot study on comparison between AR smart glasses and a mobile device in a laboratory course. Educ Sci. (2022) 12:854. doi: 10.3390/educsci12120854
43. Tai M, Rida N, Klein K, Diez H, Wells T, Kippes K, et al. Impact of virtual simulation in self-care therapeutics course on introductory pharmacy practice experience self-care encounters. Curr Pharm Teach Learn. (2020) 12:74–83. doi: 10.1016/j.cptl.2019.10.015
44. Rahman N, Nazar N, Elnaem M. Experiential learning in community pharmacy: online and remote teaching experience in Malaysian higher education. Pharm Educ. (2020) 20:29–30. doi: 10.46542/pe.2020.202.2930
45. Busch F, Hoffmann L, Truhn D, Palaian S, Alomar M, Shpati K, et al. International pharmacy students’ perceptions towards artificial intelligence in medicine-A multinational, multicentre cross-sectional study. Br J Clin Pharmacol. (2024) 90:649–61. doi: 10.1111/bcp.15911
46. Anderson H, Kwon S, Linnebur L, Valdez C, Linnebur S. Pharmacy student use of ChatGPT: a survey of students at a U.S. school of pharmacy. Curr Pharm Teach Learn. (2024) 16:102156. doi: 10.1016/j.cptl.2024.102156
47. Naguib S, AlSetohy W, Sabry N. Virtual clinical pharmacy training in the era of COVID-19: a report on undergraduate students’ perceptions and academic performance. Curr Pharm Teach Learn. (2023) 15:8–18. doi: 10.1016/j.cptl.2023.02.002
48. Newsom L, Miller S, Chesson M. Use of digital vs printed posters for teaching and learning in pharmacy education. Am J Pharm Educ. (2021) 85:8307. doi: 10.5688/ajpe8307
49. Sodnom B, Tudevdagva U, Luvsandorj T, Erdenechimeg S. Comparison of E-learning and classroom training for bachelor students of traditional medicine. Article Int J Integr Technol Educ. (2021) 10:55–64. doi: 10.5121/ijite.2021.10205
50. Bautista C, Huang I, Stebbins M, Floren L, Wamsley M, Youmans S, et al. Development of an interprofessional rotation for pharmacy and medical students to perform telehealth outreach to vulnerable patients in the COVID-19 pandemic. J Interprof Care. (2020) 34:694–7. doi: 10.1080/13561820.2020.1807920
51. Kelm M, Bush P. Digital content delivery in a pharmacy technician training program in a health system. Am J Health Syst Pharm. (2024) 77:295–9. doi: 10.1093/ajhp/zxz255
52. Khurana M, Raaschou-Pedersen D, Kurtzhals J, Bardram J, Ostrowski S, Bundgaard J. Digital health competencies in medical school education: a scoping review and Delphi method study. BMC Med Educ. (2022) 22:129. doi: 10.1186/s12909-022-03163-7
53. Permata Sari K, Maria N, Arrum Kusumawardani L, Wilda Risni H, Farhanah Syafhan N, Nur Fauziyyah A. Education and training for improving pharmacist’s telepharmacy competencies: a scoping review (Pendidikan dan pelatihan untuk peningkatan kompetensi apoteker terkait telefarmasi: scoping review). J Ilmu Kefarmasian Indonesia. (2023) 21: 293–9.
Keywords: Digital Health, health literacy, curriculum integration, telehealth training, pharmacy education, telepharmacy, artificial intelligence
Citation: Alsulami FT (2025) A scoping review on the impact of versatile Digital Health innovations on pharmacy education. Front. Med. 12:1577494. doi: 10.3389/fmed.2025.1577494
Received: 15 February 2025; Accepted: 29 September 2025;
Published: 17 October 2025.
Edited by:
Hosna Salmani, Iran University of Medical Sciences, IranReviewed by:
Vladimir Lj Jakovljevic, University of Kragujevac, SerbiaDesak Gede B. K., University of Indonesia, Indonesia
Copyright © 2025 Alsulami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fahad T. Alsulami, Zi5hbHN1bGFtaUB0dS5lZHUuc2E=
†ORCID: Fahad T. Alsulami, orcid.org/0000-0001-8989-7958
 Fahad T. Alsulami
Fahad T. Alsulami