Abstract
Purpose:
This study aims to provide a systematic review and meta-analysis of Pulse Indicator Continuous Cardiac Output (PICCO) compared with conventional central venous pressure (CVP) monitoring in the treatment of traumatic shock.
Methods:
A systematic literature retrieval was conducted in databases including PubMed, Web of Science, Cochrane Library, Embase, and China National Knowledge Infrastructure (CNKI) from database inception to October 22, 2024. Keywords such as “PICCO,” “traumatic shock,” and “hemorrhagic shock” were used. Retrieved studies were screened according to pre-determined inclusion and exclusion criteria. The methodological quality and risk of bias were assessed using the Newcastle-Ottawa Scale (NOS) for cohort studies and the Cochrane “risk of bias” tool for randomized controlled trials (RCTs). Outcomes, including mortality, duration of mechanical ventilation, and length of ICU stay, were extracted and meta-analyzed.
Results:
A total of 15 studies comprising 1,188 patients were included, with 597 monitored by PICCO and 591 by routine CVP. The risk of bias was assessed as low for all studies. PICCO-monitored patients showed a significantly shorter duration of mechanical ventilation compared to the control group [SMD in random effects model: −1.66; 95% CI: (−2.38, −0.94)]. However, no significant differences were found in mortality or length of ICU stay.
Conclusion:
PICCO monitoring can improve the prognosis of traumatic shock patients by shortening the duration of mechanical ventilation, but it does not significantly affect mortality or length of ICU stay. Given the limitations of the included studies, further exploration is warranted to verify these conclusions.
Introduction
Traumatic shock is a life-threatening subset of hypovolemic shock primarily caused by acute hemorrhage combined with major soft tissue injury, leading to a critical reduction in circulating blood volume and impaired tissue perfusion in intensive care unit (ICU) (1). Specifically, traumatic shock includes two closely related entities: traumatic hemorrhagic shock, which results from acute blood loss accompanied by extensive soft tissue damage and subsequent inflammatory and coagulopathic responses, and traumatic hypovolemic shock, characterized by significant fluid loss without active hemorrhage but with soft tissue injury and immune activation (2, 3). Severe trauma-hemorrhage and coagulation disorder are major cause of death. Effective management of traumatic shock relies heavily on accurate hemodynamic monitoring to guide fluid resuscitation and vasoactive therapy. The monitoring method commonly used in current is central venous pressure (CVP) monitoring, which is a traditional hemodynamic parameter that does not directly measure cardiac output (CO) and has recently been reported to have several limitations, including inefficiently response to hemodynamic changes and frequent fluctuations in measurements (4–6). Consequently, the development of innovative monitoring techniques is likely to enhance the therapeutic outcomes for patients with traumatic shock.
Pulse indicator continuous cardiac output (PICCO) system is a hemodynamic monitoring method technology that combines transpulmonary thermodilution (TPTD) for volumetric calibration with continuous arterial pulse contour analysis to assess cardiac function and fluid status (7). By using these techniques, PICCO allows for monitoring of numerous physiological variables including global end diastolic volume, intrathoracic blood volume (ITBV), and cardiac index (CI). With these measurements, PICCO can accurately reflect the hemodynamic status of a patient. Several studies have evaluated the clinical efficacy of PICCO. However, the conclusions in them exhibited inconsistent. One study compared treatment based on either PICCO-derived physiological values or CVP monitoring and found that PICCO was not able to reduce the 28-day mortality risk (8). In contrast, another study demonstrated that PICCO system can improve clinical outcomes in critically ill patients with acute respiratory distress syndrome (ARDS) (9). Taken together, systematic analysis of the clinical efficacy of PICCO on traumatic shock patients is still under-investigated.
This study aims to investigate the efficacy or futility of PICCO-based hemodynamic monitoring in patients with traumatic shock and hemorrhagic shock. While the PICCO system has been widely evaluated and shown to improve outcomes in septic shock patients, such as reducing mortality and shortening ICU stay and mechanical ventilation duration (10), evidence concerning its effectiveness in traumatic or hemorrhagic shock remains limited. By capitalizing on meta-analytic techniques, the current study examined the relationship between PICCO monitoring and clinical outcomes—namely, mortality, duration of mechanical ventilation, and length of ICU stay—in patients with traumatic or hemorrhagic shock, compared with conventional CVP monitoring. By analyzing the clinical efficacy of PICCO specifically in this population, our study provides new evidence and insights for fluid management in critical care settings where traumatic or hemorrhagic shock is prevalent.
Materials and methods
Following the Cochrane Handbook and PRISMA guidelines, we prospectively registered our systematic review and meta-analysis protocol (registration number: CRD420251138853).
Search strategy and eligible criteria
A literature search in various databases (Pubmed, Web of Science, Cochrane Library, Embase and China National Knowledge (CNKI)) was conducted on October 22nd, 2024 by using keywords such as “pulse index contour continuous cardiac output (PiCCO),” “traumatic shock,” and “hemorrhagic shock.” The detailed search strategy used for each database were listed in Supplementary Table S1.
Studies were included if they met the following criteria:
-
(1) The study was conducted on patients with traumatic shock, defined as a form of hypovolemic shock caused primarily by acute hemorrhage and major soft tissue injury, resulting in reduced circulating blood volume and impaired tissue perfusion (1).
-
(2) The study was a comparative one, in which the intervention group adopted PICCO, while the control group used conventional monitoring measures;
-
(3) The study contained indicators to assess the efficacy, including mean arterial pressure (MAP), CVP, blood lactate value, etc.;
-
(4) Full text was available.
Studies were excluded based on the following criteria:
-
(1) Review/meeting/case report;
-
(2) Animal/cellular studies;
-
(3) PICCO technology was not applied in the study;
-
(4) Studies with patient populations not limited to traumatic shock.
For studies reporting mortality as an outcome, we extracted the specific definition of mortality used in each study (e.g., 28-day mortality, ICU mortality, in-hospital mortality). In this meta-analysis, “28-day mortality” refers to deaths from any cause within 28 days after randomization or admission, while “ICU mortality” refers to deaths occurring during the index ICU stay.
Data acquisition and quality assessment
For potentially eligible studies, two reviewers independently check the eligibility of full-text articles using standard forms after title and abstract screening and extracted the following data from each eligible study: mortality, duration of mechanical ventilation, and length of ICU stay. For cohort study, the methodological quality and risk of bias was evaluated by the Newcastle-Ottawa Scale (NOS) tool; for RCT study, the methodological quality and risk of bias was assessed by using the Cochrane “risk of bias” tool. Conflicts between the 2 reviewers were resolved by a third reviewer.
Statistical analysis
Three outcomes were considered for meta-analysis: (a) mortality, (b) duration of mechanical ventilation, and (c) length of ICU stay. Meta-analysis was performed with the use of the meta package in Review Manager version 5.3. The results were illustrated as forest plots. p < 0.05 was considered as statistical significance. Risk ratio (RR) and 95% confidence interval (CI) were calculated to assess binary data, while standard mean difference (SMD) and 95% CI were calculated for continuous data. Statistical heterogeneity between the included studies was evaluated using the I2 and Tau2 statistic. Significant heterogeneity was defined as p < 0.05. I2 values of 25, 50, and 75% are considered low, moderate, and high estimates, respectively. Results were analyzed using a fixed-effect model when heterogeneity estimates were low, and a random-effects model was employed when heterogeneity estimates were moderate or high. Funnel plots were used to evaluate publication bias based on standard errors (SE) and corresponding measures. p < 0.05 was considered statistically significant. Sensitivity analysis was adopted by sequentially omitting each included study and estimating the overall impact of the study on the pooled results.
Results
Characteristics and quality assessment of the included studies
The current study identified a total of 1,290 results, of which 15 studies published between 2013 and 2023 met the inclusion criteria (Figure 1) (8, 11–27). Among these, 7 were RCTs, 1 was prospective cohort study, and 7 were retrospective cohort studies. A total of 1,188 patients were enrolled in the meta-analysis, including 597 individuals that monitored by PICCO, which provides continuous CO monitoring, and 591 individuals by routine CVP monitoring, a traditional method that does not directly measure CO. However, none of the studies specified the exact duration of PiCCO catheter insertion or monitoring time. The patients included 747 male patients and 441 female patients with an average age from 32.0 to 70.6 years. The outcomes measures including length of ICU stay, duration of mechanical ventilation, 28-day mortality and other indexes were analyzed (Table 1). The risk of bias was judged as low for all studies, although several studies displayed high risk of selection bias due to random sequence generation and performance bias due to blinding of participants and personnel (Supplementary Figure S1).
Figure 1

Flow diagram of the literature retrieve and selection.
Table 1
| Author year | Country | Study design | Shock type | Patients number | Gender (M/F) | Mean Age (Years) | APACHE II | Outcome measures | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PICCO | Control | PICCO | Control | PICCO | Control | PICCO | Control | |||||
| Yu et al. (2021) (24) | China | Retrospective cohort | Traumatic shock | 15 | 18 | 13/2 | 14/4 | 43 | 39 | NR | NR | Fluid resuscitation volume; Lac; BE; oxygen index |
| Lin (2018) (12) | China | RCT | Traumatic shock | 38 | 38 | 19/19 | 20/18 | 42.2 | 42.3 | 19.1 | 18.7 | Cardiac index; HR; APACHE II; MAP |
| Yang (2021) (22) | China | RCT | Traumatic shock | 43 | 43 | 22/21 | 20/23 | 47.1 | 46.4 | NR | NR | Lac; Cardiac index; EVLW |
| Zhang (2021) (25) | China | Retrospective cohort | Traumatic shock | 111 | 105 | 65/46 | 63/42 | 48.5 | 49 | 26.5 | 26.6 | 1*; 2*; 3*; APACHE II; fluid resuscitation volume; CVP; MAP; LAC |
| Lin (2021) (14) | China | RCT | Traumatic shock | 50 | 50 | 27/23 | 28/22 | 48.7 | 48.9 | NR | NR | 1*; 2*; MAP; CVP; HR |
| Xue et al. (2013) (21) | China | Retrospective cohort | Traumatic shock | 21 | 21 | 14/7 | 16/5 | 45.7 | 46.8 | 31.1 | 30.2 | 2*; APACHE II; MAP; LAC |
| Fang and Tang (2016) (11) | China | Retrospective cohort | Traumatic shock | 18 | 18 | 13/5 | 12/6 | 43.87 | 45.32 | 20.8 | 24.7 | 2*; APACHE II; MAP; LAC |
| Shi et al. (2017) (20) | China | RCT | Traumatic shock | 50 | 51 | 41/9 | 40/11 | 34 | 32 | 12 | 11 | Mortality; APACHE II; fluid resuscitation volume; CVP; MAP; LAC |
| Meng et al. (2019) (18) | China | RCT | Traumatic shock | 40 | 40 | 24/16 | 23/17 | 70.6 | 69.9 | NR | NR | 1*; fluid resuscitation volume; HR; CVP; MAP; LAC |
| Lin (2018) (13) | China | Retrospective cohort | Traumatic shock | 30 | 30 | 18/12 | 17/13 | 45.28 | 45.59 | NR | NR | MAP; Lactate clearance rate |
| Bian et al. (2021) (27) | China | Retrospective cohort | Traumatic shock | 42 | 42 | 28/14 | 27/15 | 60.24 | 60.13 | NR | NR | 1*; fluid resuscitation volume; HR; CVP; MAP; LAC |
| Zhu et al. (2017) (40) | China | Retrospective cohort | Traumatic shock | 45 | 41 | 29/16 | 31/10 | 41.8 | 43.1 | 16.5 | 17.1 | 1*; fluid resuscitation volume; HR; CVP; MAP; LAC; BE |
| Ma (2020) (17) | China | RCT | Traumatic shock | 35 | 35 | 20/15 | 22/13 | 46.74 | 46.88 | NR | NR | MAP; Lactate clearance rate |
| Ni (2022) | China | Prospective cohort | Traumatic shock | 39 | 39 | 27/12 | 25/14 | 49.29 | 48.27 | 24.39 | 25.37 | 1*; 2*; 3*APACHE II; CVP; MAP |
| Yuan (2015) | China | RCT | Traumatic shock | 20 | 20 | 14/6 | 15/5 | 60.7 | 59.2 | 21.65 | 21.8 | 1*; 2*; APACHE II; fluid resuscitation volume; CVP; MAP; LAC; HR |
Characteristics of the included studies.
1*: length of ICU stay; 2*: duration of mechanical ventilation; 3*: 28-day mortality; 4: fluid resuscitation volume; RCT, randomized controlled trial; NR, not reported, missing values are indicated as “NR”; PICCO, pulse indicator continuous cardiac output; APACHE, Acute Physiology and Chronic Health Evaluation; SOFA, Sequential Organ Failure Assessment; CVP, central venous pressure; MAP, mean arterial pressure; BE, XXXX; LAC, lactate; HR, heart rates.
The impact of PICCO monitoring on mortality of traumatic shock patients
To assess the impact of PICCO monitoring on mortality of traumatic shock patients, 4 studies (9, 19, 25, 28) comprising 221 cases in PICCO group and 214 cases in control group were analyzed, including 2 RCTs, 1 prospective cohort study and 1 retrospective cohort study. As shown in the forest plot in Figure 2, although the risk of mortality in PICCO group was lower when compared with the control group, the difference between the two groups was not significant [RR in random effects model: 0.62; 95% CI: (0.26, 1.45)]. The I2 = 56% indicated moderate heterogeneity in the meta-analysis. The funnel plot was created to identify the publication bias. The symmetry of the plot indicated the meta-analysis did not exhibit significant publication bias (Figure 3). The result of the influence analysis demonstrated the robustness of the analysis (Figure 4).
Figure 2
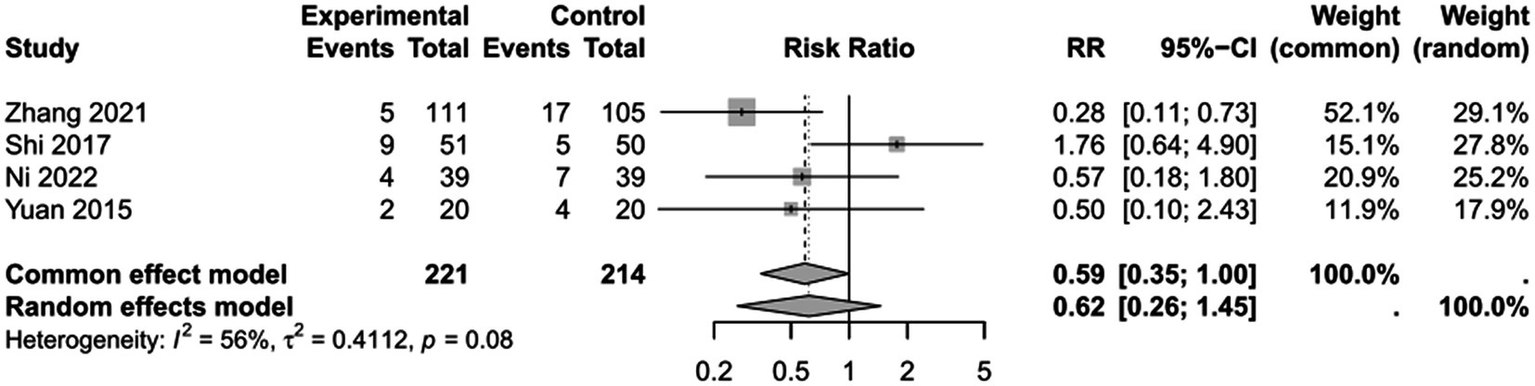
Forest plot: comparison of mortality.
Figure 3

Funnel plot of mortality.
Figure 4
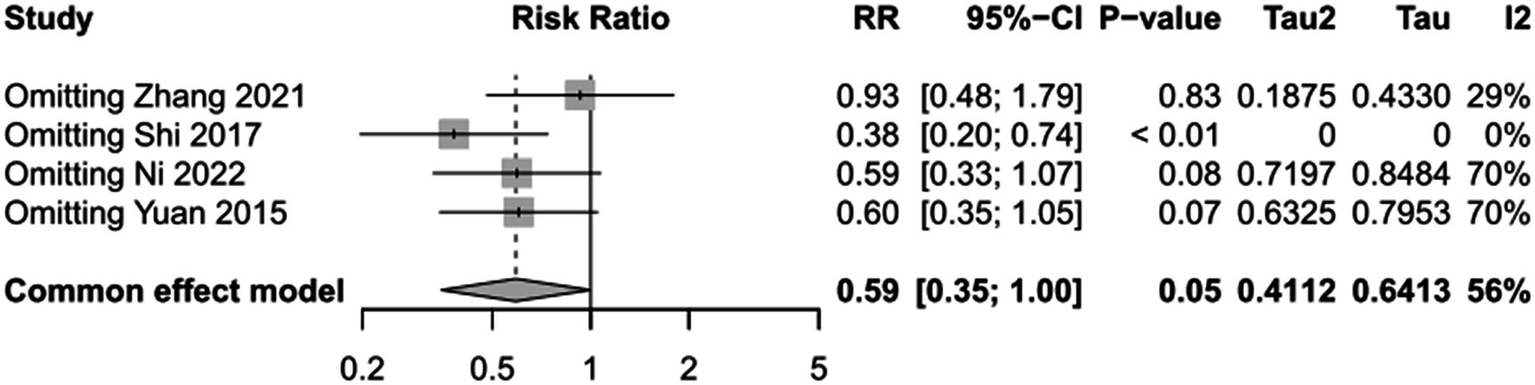
Sensitivity analysis of mortality.
The impact of PICCO monitoring on duration of mechanical ventilation of traumatic shock patients
To assess the impact of PICCO monitoring on duration of mechanical ventilation of traumatic shock patients, 6 studies (9, 19, 25, 26, 29, 30) comprising 265 cases in PICCO group and 255 cases in control group were analyzed, including 2 RCTs and 4 retrospective cohort studies. The forest plot in Figure 5 showed that the duration of mechanical ventilation in PICCO group was significantly lower than that in control group [SMD in random effects model: −1.66; 95% CI: (−2.38, −0.94)]. The I2 = 87% indicated obvious heterogeneity in the meta-analysis. The symmetry of the funnel plot indicated no obvious publication bias in the meta-analysis (Figure 6). Finally, the robustness of the analysis was examined by sensitivity analysis, and exclusion of any study at one time did not materially alter the overall estimates (Figure 7).
Figure 5
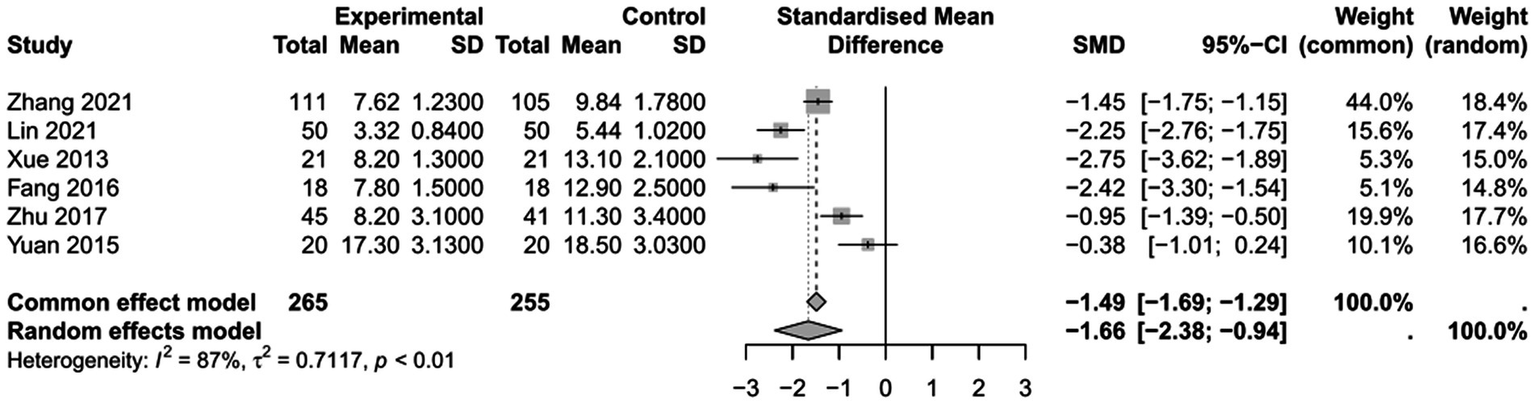
Forest plot: comparison of duration of mechanical ventilation.
Figure 6
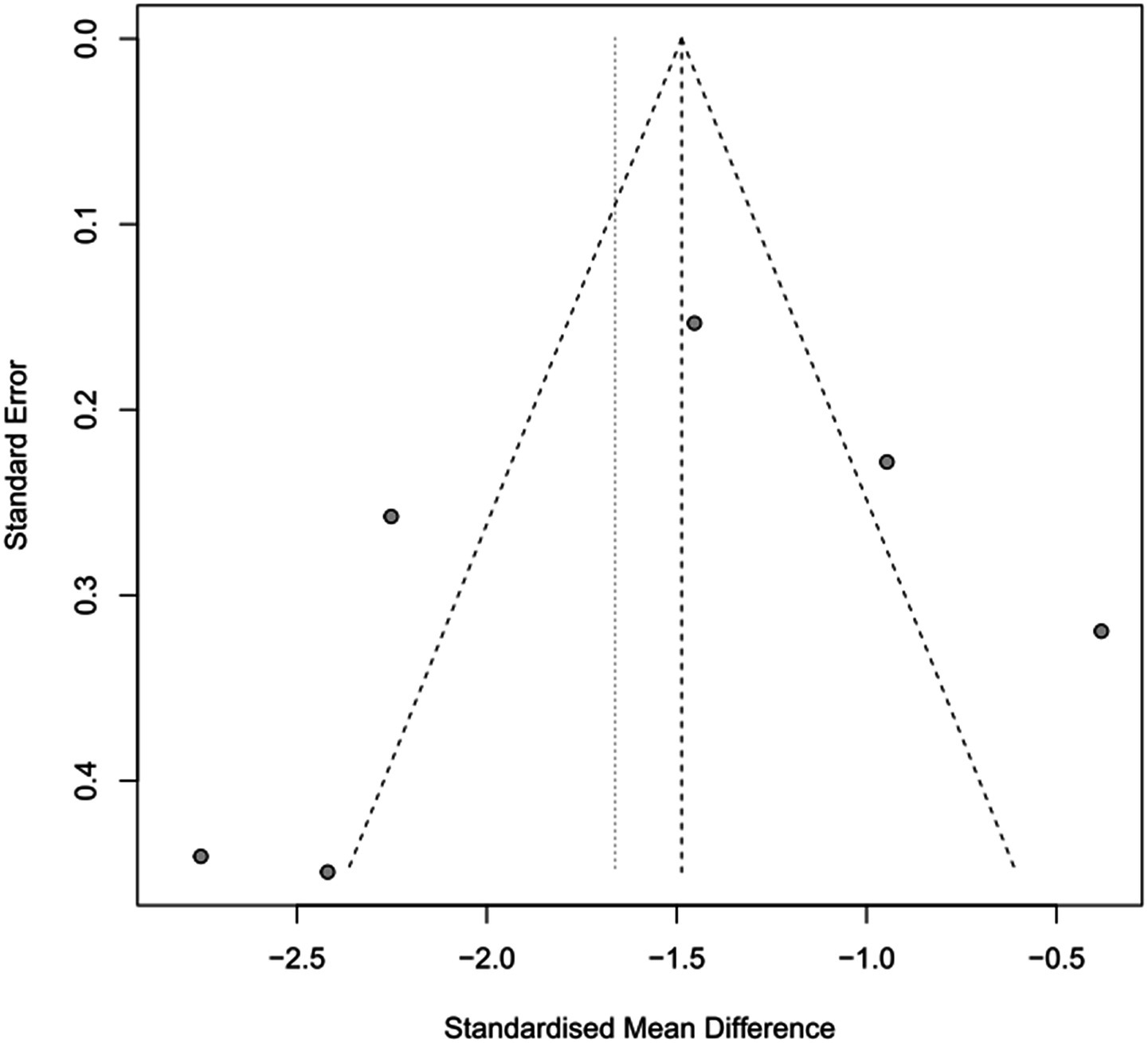
Funnel plot of duration of mechanical ventilation.
Figure 7
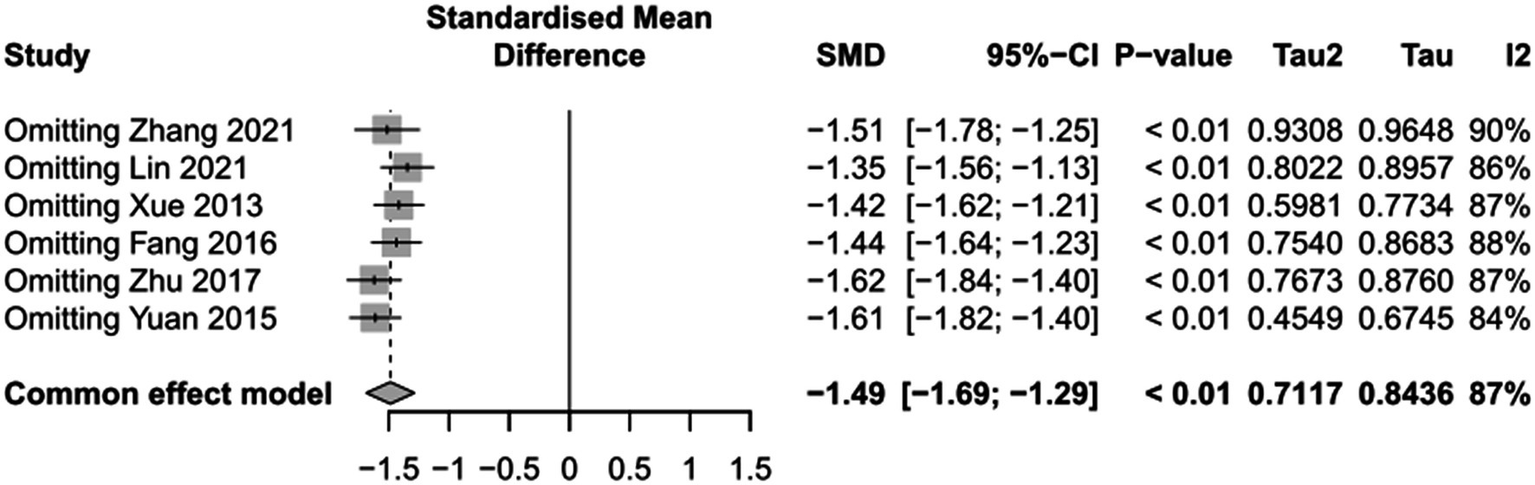
Sensitivity analysis of duration of mechanical ventilation.
The impact of PICCO monitoring on length of ICU stay of traumatic shock patients
To assess the the impact of PICCO monitoring on length of ICU stay of traumatic shock patients, 5 studies (9, 25, 26, 29, 31)comprising 266 cases in PICCO group and 256 cases in control group were analyzed, including 3 RCTs and 2 retrospective cohort studies. As shown in the forest plot, treatment based on PICCO displayed beneficial effect when compared with the control group, but the difference between the two groups was not significant [SMD in random effects model: −0.57; 95% CI: (−1.38, 0.25)]. To enhance interpretability, the SMD value was translated into clinical units: based on the pooled standard deviation of ICU stay (approximately 2.3 days across studies), this corresponds to an average reduction of about 1.3 days in ICU stay for the PICCO group compared to the control group. The I2 = 95% indicated significant heterogeneity in the meta-analysis (Figure 8). The funnel plot in Figure 9 demonstrated a moderate publication bias in the meta-analysis. The sensitivity analysis further demonstrated the robustness of the meta-analysis results, confirming that the overall conclusions were not significantly affected by the exclusion of individual studies (Figure 10).
Figure 8
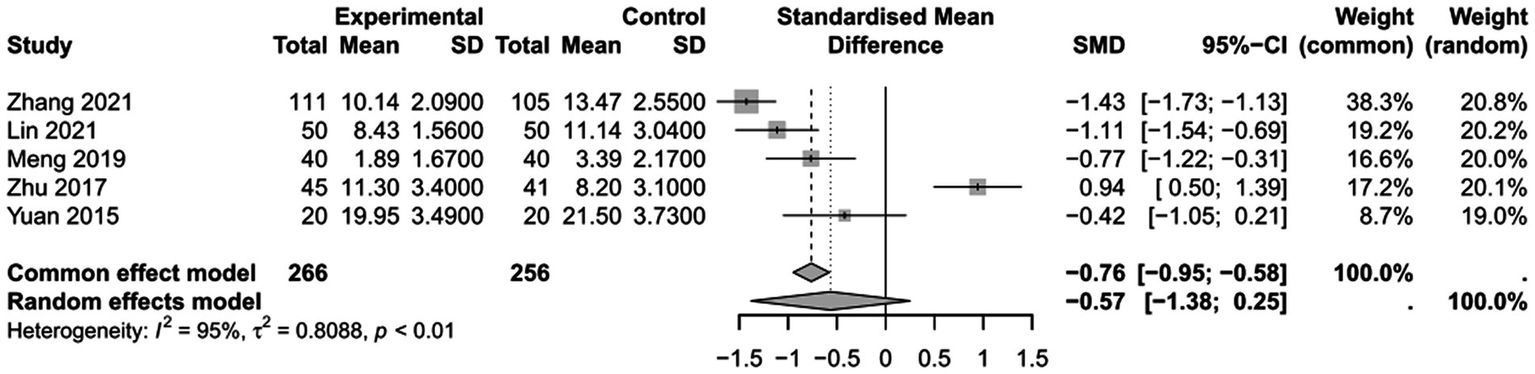
Forest plot: comparison of length of ICU stay.
Figure 9
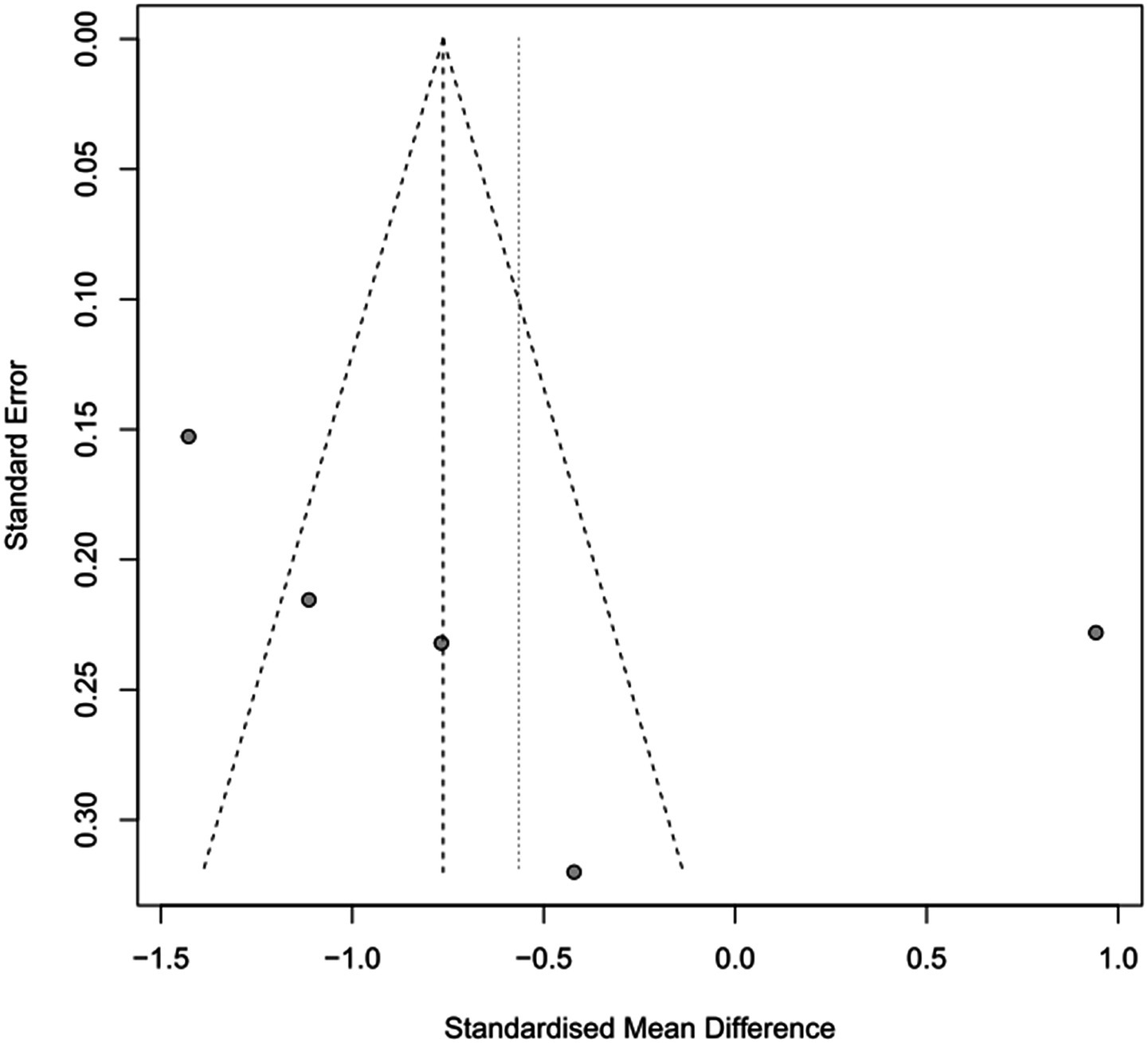
Funnel plot of duration of length of ICU stay.
Figure 10
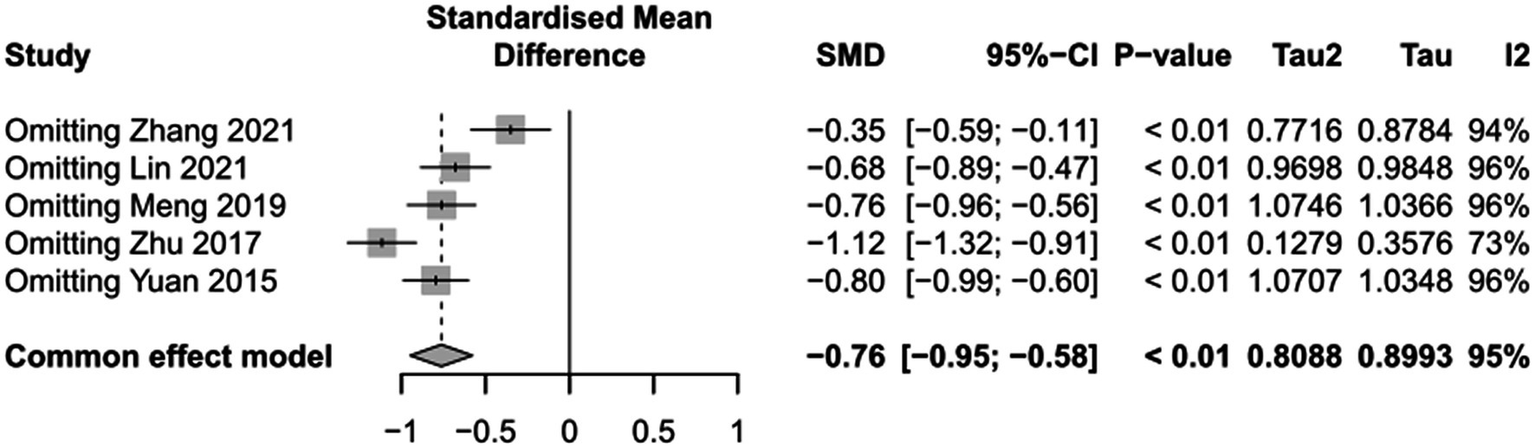
Sensitivity analysis of length of ICU stay.
Meta regression
Meta-regression analyses were conducted for these three outcomes. Based on the availability of relevant data across included studies, meta-regression for 28-day mortality and duration of mechanical ventilation was performed according to study design and APACHE II stratification, while the analysis for length of ICU stay was conducted based solely on study design. The results indicated that neither study design nor APACHE II stratification accounted for the observed heterogeneity in any of the outcomes, suggesting that these factors were not significant sources of heterogeneity in our meta-analysis (Supplementary Figures S2–S4).
Discussion
In this systematic review, a total of 1,290 studies were identified and 15 studies were included in the analysis. Based on these 15 studies, this systematic review revealed that traumatic shock patients monitored with PICCO exhibited lower mortality, reduced duration of mechanical ventilation, and shorter ICU stay. However, although a significant shorter duration of mechanical ventilation was observed, the difference between PICCO group and control group (CVP) in mortality and length of ICU stay was not statistically significant, suggesting that PICCO monitoring may improve the prognosis of traumatic shock to a certain extent. This study increases the understanding of the therapeutic effects of PICCO monitoring on traumatic shock patients through meta-analyzing the data of mortality, duration of mechanical ventilation, length of ICU stay. To our knowledge, this study represents the largest systematic review and meta-analysis of published studies of PICCO monitoring on traumatic shock population.
PICCO is one of the five most popular systems for arterial pulse contour analysis. The other four systems include FloTrac/Vigileo(®), LiDCO/PulseCO(®), PRAM/MostCare(®), and Modelflow (32–35). Several previous systematic reviews have demonstrated the benefits of PICCO monitoring, particularly in septic shock patients. For example, a meta-analysis in 2022 reported that PICCO monitoring can improve the prognosis of septic shock patients by shortening the duration of mechanical ventilation and ICU stay, and reducing 28-day mortality (36). Another 2014 study compared different arterial pulse contour analysis systems and found that PICCO showed acceptable accuracy during hemodynamically stable conditions (37). More recently, a 2023 meta-analysis demonstrated that PICCO monitoring in septic shock patients with ARDS resulted in improved oxygenation, shorter ICU stays and mechanical ventilation duration, fewer complications, and lower mortality rates (38). Additional evidence from a 2023 meta-analysis recommended clinical use of PICCO based on reduced use of vasopressors in purulent septic shock patients (39), and an earlier meta-analysis supported that PICCO monitoring was associated with shorter ICU stays and lower ICU and 28-day mortality in septic shock patients (40). However, in our current meta-analysis focusing on traumatic shock patients, only the duration of mechanical ventilation was significantly reduced in the PICCO group compared to the control group, while differences in mortality and ICU stay between groups were not statistically significant. This suggests that while PICCO monitoring may improve certain aspects of critical care, such as ventilatory support, its impact on overall survival and ICU length of stay in traumatic shock patients remains uncertain and may differ from its effects in septic shock.
Although based on these reported results, clinicians may be aware of the use of PICCO to improve prognosis of shock patients in ICU, the current study intend to explore the efficacy of PICCO in treatment of traumatic shock population. Studies have revealed that the intricate hemochemical makeup and changes during these shock states is exemplified in shock whether induced by infection or hemorrhage (41). PICCO can overcome the drawbacks of traditional CVP monitoring by continuously monitoring haemodynamics and providing a more comprehensive relevant parameters to guide the entire process of fluid resuscitation. PICCO’s impact on reducing the duration of mechanical ventilation may reflect better hemodynamic optimization, which potentially minimizes ventilator-associated complications by ensuring more precise fluid management and improved organ perfusion (42). This reduction in ventilation duration may be attributed to several mechanisms. First, PICCO allows for improved preload optimization by accurately assessing cardiac filling and guiding individualized fluid resuscitation, which helps avoid both hypovolemia and fluid overload (43). By preventing excessive fluid administration, PICCO can reduce the risk of pulmonary edema--a major contributor to prolonged mechanical ventilation in critically ill patients (44). Additionally, optimized fluid management via PICCO can enhance oxygen delivery to tissues, promoting faster recovery of organ function and reducing the need for prolonged ventilatory support (9). Collectively, these effects contribute to a more favorable respiratory profile, facilitating earlier liberation from mechanical ventilation. This aligns with the concept of protective hemodynamics, where continuous and comprehensive monitoring with PiCCO enables tailored interventions that support lung function and reduce the risk of ventilator-induced lung injury, thereby enhancing patient outcomes (45).
There are several possible explanations for why PICCO monitoring did not result in statistically significant reductions in mortality or ICU length of stay in our analysis. First, the presence of confounding variables--such as differences in baseline patient characteristics, variations in standard care across centers, and the use of concomitant therapies may have diluted the observable impact of PICCO on these outcomes. Second, the timing of intervention may play a crucial role; if PICCO monitoring is not initiated early enough in the course of shock, its potential benefits in preventing irreversible organ dysfunction or death may be limited. Third, many included studies enrolled patients with a wide range of illness severity, and PICCO’s advantages may be most pronounced in specific subgroups (e.g., those with more severe or refractory shock), which could have attenuated the overall effect in a heterogeneous population. Finally, mortality and ICU stay are influenced by numerous factors beyond hemodynamic monitoring, such as underlying comorbidities, complications, and institutional protocols, making it challenging to isolate the effect of PICCO alone on these endpoints.
Despite these promising findings, the study has several important limitations. First, all included studies were conducted in China, which limits generalizability due to global differences in trauma systems, ICU protocols, staffing, and resource availability. Second, key details regarding PICCO implementation—such as catheter duration and monitoring frequency—were frequently missing, limiting interpretation and reproducibility. Third, several studies lacked blinding, introducing potential performance and detection bias. Fourth, as most studies were observational, the risk of confounding and observational fallacy remains, since causality cannot be definitively established (46). Additionally, substantial heterogeneity was present among studies due to differences in shock definitions, patient selection, and study design. Finally, the small number of included studies makes it difficult to reliably assess publication bias. Collectively, these limitations underscore the need for more high-quality, multicenter randomized controlled trials (RCTs) in diverse healthcare settings to clarify the efficacy of PICCO monitoring in traumatic shock patients.
In conclusion, this systematic review and meta-analysis found that PICCO monitoring was associated with a significantly shorter duration of mechanical ventilation in patients with traumatic shock. However, no statistically significant difference was observed in mortality or ICU length of stay between the PICCO and control groups. While there appeared to be a trend toward improved prognosis with PICCO, further high-quality studies with larger sample sizes are needed to clarify its impact on mortality and other key clinical outcomes in this patient population. This meta-analysis provides preliminary evidence and highlights areas for future research regarding the use of PICCO monitoring in traumatic shock patients in the ICU.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AL: Data curation, Investigation, Writing – original draft, Writing – review & editing. ZL: Formal analysis, Resources, Writing – original draft, Writing – review & editing. KX: Investigation, Resources, Writing – original draft, Writing – review & editing. JC: Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. XN: Conceptualization, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study is supported by the Suqian City science and technology Bureau mandatory planning subject (S202012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1578348/full#supplementary-material
References
1.
Health Emergency Committee of CHINESE Research Hospital, Cardiopulmonary Resuscitation Specialized Committee of Chinese Research Hospital, Cardiopulmonary Resuscitation Specialized Committee of Henan Hospital . Chinese expert consensus on the clinical application of innovative first-aid resuscitation Technology for Traumatic Shock in 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2019) 31:257–63. doi: 10.3760/cma.j.issn.2095-4352.2019.03.001
2.
Dufour-Gaume F Frescaline N Cardona V Prat NJ . Danger signals in traumatic hemorrhagic shock and new lines for clinical applications. Front Physiol. (2022) 13:999011. doi: 10.3389/fphys.2022.999011
3.
Higashi H Kanki A Watanabe S Yamamoto A Noda Y Yasokawa K et al . Traumatic hypovolemic shock revisited: the spectrum of contrast-enhanced abdominal computed tomography findings and clinical implications for its management. Jpn J Radiol. (2014) 32:579–84. doi: 10.1007/s11604-014-0354-5
4.
Xia B Shi S . Application effect of pulse index continuous cardiac output monitoring in the fluid management of infectious shock patients complicated with acute respiratory distress syndrome. Pract J Cardiac Cerebral Pneumal Vascular Dis. (2016) 24:100–2.
5.
Association EMBoCMD . Expert consensus on acute circulatory failure: clinical practice of Chinese emergency physicians. Chin J Emerg Med. (2016) 25:146–52.
6.
Delgado-Serrano JF Torres-Cordón M Duarte H Peña-Rangel MA Serrano-Gómez S Torres-Dueñas D et al . Myocardial dysfunction and its prognostic utility in sepsis and septic shock. Rev Med Inst Mex Seguro Soc. (2021) 59:300–5.
7.
Herold IH Soliman Hamad MA van Assen HC Bouwman RA Korsten HH Mischi M . Pulmonary blood volume measured by contrast enhanced ultrasound: a comparison with transpulmonary thermodilution. Br J Anaesth. (2015) 115:53–60. doi: 10.1093/bja/aeu554
8.
Zhang Z Ni H Qian Z . Effectiveness of treatment based on Picco parameters in critically ill patients with septic shock and/or acute respiratory distress syndrome: a randomized controlled trial. Intensive Care Med. (2015) 41:444–51. doi: 10.1007/s00134-014-3638-4
9.
Yuanbo Z Jin W Fei S Liangong L Xunfa L Shihai X et al . ICU management based on PiCCO parameters reduces duration of mechanical ventilation and ICU length of stay in patients with severe thoracic trauma and acute respiratory distress syndrome. Ann Intensive Care. (2016) 6:113. doi: 10.1186/s13613-016-0217-6
10.
Wang L Liu H Wang L Zhang Y Guo W Wu P et al . Evaluating an oral health programme for the prevention of dental decay among school-aged children in China: protocol for a mixed-methods study based on the re-aim framework. BMJ Open. (2022) 12:e061601. doi: 10.1136/bmjopen-2022-061601
11.
Fang H Tang H . Analysis of the value of PICCO monitoring in the treatment of patients with hemorrhagic shock combined with pulmonary edema. For All Health. (2016) 10:75–6.
12.
Lin A . Application of PiCCO in treatment of traumatic shock. China Foreign Med Treat. (2018) 37:47–9. doi: 10.16662/j.cnki.1674-0742.2018.08.047
13.
Lin A . The role of PiCCO in the management of traumatic shock. Chin J Crit Care Med. (2018) 38:44. doi: 10.3969/j.issn.1002-1949.2018.z1.034
14.
Lin W . A study of the value of guided fluid resuscitation under PICCO monitoring techniques in patients with hemorrhagic shock due to chest trauma. Pract Clin J Integr Trandit Chin West Med. (2021) 21:118–9.
15.
Liu X Ji W Wang J Pan T . Application strategy of PiCCO in septic shock patients. Exp Ther Med. (2016) 11:1335–9. doi: 10.3892/etm.2016.3040
16.
Lu NF Zheng RQ Lin H Shao J Yu JQ Yang DG . Improved Sepsis bundles in the treatment of septic shock: a prospective clinical study. Am J Emerg Med. (2015) 33:1045–9. doi: 10.1016/j.ajem.2015.04.031
17.
Ma Y . The value of cardiorespiratory volume monitoring (Picco) in the treatment of traumatic shock. Contin Med Educ. (2020) 34:78–9. doi: 10.3969/j.issn.1004-6763.2020.06.043
18.
Meng D Yang Y Chu X . Evaluation of Picco-oriented fluid resuscitation strategies in the acute phase of traumatic shock. J Prev Med Chin Peoples Liberation Army. (2019) 37:130–1.
19.
Ni X Liu XJ Ding TT . The application of Picco-guided fluid resuscitation in patients with traumatic shock. Am Surg. (2023) 89:4431–7. doi: 10.1177/00031348221087898
20.
Shi C Wang Z Sun L Li Y Guo Q Qiao W et al . Transpulmonary thermodilution technique in application of traumatic shock. Chin J Med. (2017) 52:65–8.
21.
Xue F Chen Z Wang X Liu C Wang L . The value of PiCCO monitoring in the management of patients with hemorrhagic shock combined with pulmonary edema. Shandong Med J. (2013) 53:57–8.
22.
Yang X . Analysis of the effect of fluid resuscitation guided by the PiCCO technique on ci, blood lactate and evlwi levels in patients with emergency traumatic shock. Modern Diagnosis Treatment. (2021) 32:3432–3.
23.
Yi M Me G Guo X . Value of pulse indicator continuous cardiac output monitoring of cardiac function in septic shock patients: a prospective study. Chin Crit Care Med. (2015) 27:22–7. doi: 10.3760/cma.j.issn.2095-4352.2015.01.006
24.
Yu H Zhu P Chen L Zhu F Hu R Li X . Application of pulse contour cardiac output monitoring technology in fluid resuscitation of severe burn patients in shock period. Chin J Burns Wounds. (2021) 37:136–42. doi: 10.3760/cma.j.cn501120-20200908-00403
25.
Zhang C Su J . Application of PiCCO-guided limited fluid resuscitation in rescue of severe traumatic hemorrhagic shock. Hainan Yi Xue Yuan Xue Bao. (2021) 32:42–5.
26.
Zhuge J . Clinical study on the application of PiCCO in the liquid resuscitation in patients with chest trauma. Chin Gen Pract. (2017) 20:146–8.
27.
Bian G . An observational study on the treatment methods and effects of fluid resuscitation strategies in patients with traumatic shock. Doctor. (2021) 6:116–8.
28.
Chun-zhi S . Transpulmonary thermodilution technique in application of traumatic shock. Chin Med J. (2017) 52:65–8.
29.
Wen-qing L . Study on the application value of PICCO monitoring technology in guiding fluid resuscitation in patients with hemorrhagic shock caused by chest trauma. Pract Clin Appl Integrated Tradit Chin Western Med. (2021) 21:118–9.
30.
Feng X . The application value of PICCO monitoring in the treatment of patients with hemorrhagic shock complicated with pulmonary edema. Shandong Med. (2013) 53:57–8.
31.
Wei-de M . Evaluation of PiCCO-guided fluid resuscitation strategy in the acute phase of traumatic shock. J Mil Prev Med. (2019) 37:130–1.
32.
Oh C Lee S Oh P Chung W Ko Y Yoon SH et al . Comparison between fourth-generation Flotrac/Vigileo system and continuous Thermodilution technique for cardiac output estimation after time adjustment during off-pump coronary artery bypass graft surgery: a retrospective cohort study. J Clin Med. (2022) 11:6093. doi: 10.3390/jcm11206093
33.
Hadian M Kim HK Severyn DA Pinsky MR . Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care. (2010) 14:R212. doi: 10.1186/cc9335
34.
Saxena R Durward A Puppala NK Murdoch IA Tibby SM . Pressure recording analytical method for measuring cardiac output in critically ill children: a validation study. Br J Anaesth. (2013) 110:425–31. doi: 10.1093/bja/aes420
35.
Smorenberg A Cherpanath TGV Geerts BF de Wilde RBP Jansen JRC Maas JJ et al . A Mini-fluid challenge of 150ml predicts fluid responsiveness using Modelflow(R) pulse contour cardiac output directly after cardiac surgery. J Clin Anesth. (2018) 46:17–22. doi: 10.1016/j.jclinane.2017.12.022
36.
Wang B Cai L Lin B He Q Ding X . Effect of pulse Indicator continuous cardiac output monitoring on septic shock patients: a meta-analysis. Comput Math Methods Med. (2022) 2022:1–9. doi: 10.1155/2022/8604322
37.
Schlöglhofer T Gilly H Schima H . Semi-invasive measurement of cardiac output based on pulse contour: a review and analysis. Can J Anesth/J Can Anesth. (2014) 61:452–79. doi: 10.1007/s12630-014-0135-8
38.
Liu Z Zhang L Wang L Li Z Yuan M Li E et al . Evaluation of the efficacy of PICCO monitoring for fluid resuscitation in septic shock patients with ARDS: a meta-analysis. Med J Wuhan Univ. (2023) 44:1361–70. doi: 10.14188/j.1671-8852.2023.0042
39.
Pan Z , editor. Meta-analysis of PICCO monitoring and guiding the use of vasoactive drugs in the treatment of septic shock patients. Proceedings of 2nd International Conference on Biomedical Engineering, Healthcare and Disease Prevention (BEHDP 2022) (2023); Xiamen, Fujian, China.
40.
Zhu Y Shen X Jiang Q Cai Y Guo N Zhao H . Efficacy of pulse indicating continuous cardiac output monitoring on the treatment guidance of patients with septic shock: a meta-analysis. Chin J Evid Based Med. (2017) 17:934–40.
41.
Bunch CM Chang E Moore EE Moore HB Kwaan HC Miller JB et al . Shock-induced Endotheliopathy (Shine): a mechanistic justification for Viscoelastography-guided resuscitation of traumatic and non-traumatic shock. Front Physiol. (2023) 14:1094845. doi: 10.3389/fphys.2023.1094845
42.
D'Amico F Marmiere M Monti G Landoni G . Protective hemodynamics: CLEAR!J Cardiothorac Vasc Anesth. (2025) 39:13–9. doi: 10.1053/j.jvca.2024.10.021
43.
La Via L Vasile F Perna F Zawadka M . Prediction of fluid responsiveness in critical care: current evidence and future perspective. Trends Anaesth Crit Care. (2024) 54:101316. doi: 10.1016/j.tacc.2023.101316
44.
Martin ND Codner P Greene W Brasel K Michetti C . Contemporary hemodynamic monitoring, fluid responsiveness, volume optimization, and endpoints of resuscitation: an AAST critical care committee clinical consensus. Trauma Surg Acute Care Open. (2020) 5:e000411. doi: 10.1136/tsaco-2019-000411
45.
D'Amico F Landoni G . Protective hemodynamics: a novel strategy to manage blood pressure. Curr Opin Crit Care. (2024) 30:629–36. doi: 10.1097/mcc.0000000000001205
46.
D'Amico F Marmiere M Fonti M Battaglia M Belletti A . Association does not mean causation, when observational data were misinterpreted as causal: the observational interpretation fallacy. J Eval Clin Pract. (2025) 31:e14288. doi: 10.1111/jep.14288
Summary
Keywords
pulse indicator continuous cardiac output, traumatic shock, hemorrhagic shock, meta-analysis, central venous pressure
Citation
Lin A, Lin Z, Xu K, Chen J and Ni X (2025) The impact of PICCO monitoring on traumatic shock: a systematic review and meta-analysis. Front. Med. 12:1578348. doi: 10.3389/fmed.2025.1578348
Received
17 February 2025
Accepted
21 October 2025
Published
14 November 2025
Volume
12 - 2025
Edited by
Alessandro Belletti, IRCCS San Raffaele Scientific Institute, Italy
Reviewed by
Diamanto Aretha, General University Hospital of Patras, Greece
Shahzad Raja, Harefield Hospital, United Kingdom
Bassem Nashaat Beshey, Alexandria Faculty of Medicine, Egypt
Updates
Copyright
© 2025 Lin, Lin, Xu, Chen and Ni.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xun Ni, n18751086362@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.