- 1Department of Anesthesiology, Mianyang 404 Hospital, Mianyang, Sichuan, China
- 2Department of Anesthesiology, Sichuan Science City Hospital, Mianyang, Sichuan, China
Objective: This meta-analysis investigates the efficacy and safety of ultrasound-guided nerve block in geriatric surgical patients, a crucial endeavor for optimizing anesthetic protocols and enhancing perioperative medical outcomes and prognostic indices in this vulnerable patient cohort.
Methods: A comprehensive literature search was conducted in major bibliographic databases, including Web of Science, PubMed, The Cochrane Library, Embase, CNKI, Wan Fang, and VIP, to identify studies investigating the utilization of ultrasound-guided nerve blocks in elderly surgical patients. The search encompassed publications from database inception to January 2025. Two independent reviewers meticulously screened the retrieved literature, extracted relevant data, and assessed the risk of bias inherent in the included studies. Subsequently, a meta-analysis was performed to synthesize the findings.
Results: Twenty-five randomized trials were included in the analysis, The meta-analysis showed that, Compared with the control group, Ultrasound-guided nerve block Blocking effective rate ([RR = 1.21 (1.11, 1.31), P < 0.001], time of onset of sensory nerve block [SMD = −2.76 (−3.67, −1.85), P < 0.001] and Duration [SMD = 2.52 (1.86, 3.18), P < 0.01]; Time to onset of motor nerve block [SMD = −1.94 (−2.68,−1.19), P < 0.001], and Duration [SMD = 1.11 (0.24, 1.98), P = 0.01] has a good effect. After the ultrasound-guided nerve block group, 4 [SMD = −1.68 (−2.68, −0.68), P < 0.001], 8 [SMD = −0.99 (−1.66, −0.32), P < 0.001], 12 [SMD = −1.03 (−1.0.48, −0.58), P < 0.001], 24 [SMD = −1.56 (−2.36, −0.75), P < 0.001] hours had all lower VAS scores than the control group. The Adverse reaction rate in the experimental group was 0.35 times that of the control group [RR = 0.35 (0.23, 0.55), P < 0.001] and no significant difference between the operating groups [SMD = 0.25 (−0.36, 0.86), P = 0.43]. Significant publication bias was found except for the duration of the motor nerve block and surgery time. Sensitivity analysis confirmed the stability of the results.
Conclusion: Ultrasound-guided nerve blocks constitute an efficacious and safe anesthetic modality for elderly surgical patients. These findings have significant implications for the refinement of anesthetic protocols within the geriatric population, with the potential to enhance perioperative medical quality and patient outcomes. The evidence presented in this meta-analysis provides a robust foundation for the widespread adoption of ultrasound-guided nerve blocks in clinical practice for elderly surgical patients.
1 Introduction
The burgeoning elderly population has resulted in a significant increase in the number of geriatric surgical patients (1). Owing to their unique physiological characteristics, including organ system decline and the concomitant presence of multiple chronic diseases, elderly patients present heightened demands for anesthetic tolerance and safety (2, 3). The judicious selection of anesthetic techniques is paramount for optimizing perioperative outcomes, facilitating postoperative rehabilitation, and minimizing the incidence of complications in elderly surgical patients (4).
Nerve block, a widely employed anesthetic modality, constitutes a cornerstone of surgical anesthesia and postoperative pain management (5). Notably, elderly patients derive the greatest benefit from successful regional nerve blocks, as this approach markedly reduces the risk of postoperative delirium—a common and severe complication in this population associated with prolonged hospital stays, increased mortality, and long-term cognitive decline. Conventional nerve block techniques predominantly depend upon the identification of anatomical surface landmarks or the utilization of nerve stimulators (6). Nevertheless, these methodologies exhibit inherent limitations, including imprecise positioning and an inconsistent success rate (7). Notably, these challenges may be exacerbated in geriatric patients due to age-related alterations in anatomical structures and a concomitant decline in physiological function.
The advent of ultrasound-guided nerve block technology has ushered in a new era of innovation within the field of nerve block. This technique constitutes an anesthetic modality that enables the precise localization of analgesia through the real-time or visually guided administration of the anesthetic agent (8). This approach enables direct visualization of both the nerve and the puncture needle, thereby markedly enhancing puncture accuracy and mitigating the risks inherent in blind puncture procedures (9). For elderly patients, this precision is crucial not only for block success but also for avoiding complications that could precipitate delirium, such as excessive sedation or respiratory depression from rescue analgesics. This visualization facilitates the identification of perivascular anatomy, thereby preventing inadvertent needle penetration of blood vessels. This mitigates the risk of local anesthetic systemic toxicity and minimizes the likelihood of iatrogenic injury to vital structures, including nerves and blood vessels, ultimately enhancing patient safety (10). The ultrasound-guided nerve block technique has an extremely wide range of applications. It exhibits utility in both anesthetic and postoperative analgesic contexts for a diverse range of surgical procedures, encompassing upper extremity, lower extremity, and abdominal surgeries. Furthermore, it demonstrates efficacy in the management of various neuropathic pain conditions (11–13). Owing to its multifaceted benefits, this technique has found widespread application across diverse medical domains, with particularly promising outcomes observed in geriatric surgical patients (14, 15).
Nevertheless, despite the theoretical promise of ultrasound-guided nerve block technology in geriatric surgical patients, assessing its clinical efficacy presents a multifaceted and heterogeneous challenge. Some studies have demonstrated that ultrasound-guided nerve blocks can significantly reduce postoperative pain intensity in surgical patients, decrease opioid consumption, and lower the incidence of complications—including delirium, which is directly mitigated by reduced opioid use—thereby improving patient prognosis (1, 16); some studies point out that this technology may have some technical difficulties in practice, and the analgesic effect for some specific types of surgery or patient groups, the effect may not be ideal, and may even increase the risk of some complications (17, 18).
Therefore, a rigorous and comprehensive systematic review of relevant literature is imperative to accurately assess the efficacy and safety profile of ultrasound-guided nerve blocks in geriatric surgical patients. This meta-analysis endeavors to systematically synthesize and critically appraise the existing evidence pertaining to the safe and effective implementation of ultrasound-guided nerve blocks within the context of geriatric surgical procedures, thereby providing a more robust foundation for clinical decision-making.
2 Methods
2.1 Search strategies
This study was a systematic review and meta-analysis using the Preferred Reporting Project (PRISMA) report list (19). The meta-analysis was carefully constructed according to the PICO (Patient, Intervention, Comparison, Outcome) framework, describing the key aspects as follows: Patient (P) was a geriatric surgical patient. The intervention studied (I) was the ultrasound-guided nerve block. Comparison (C) relates to other forms of anesthesia other than ultrasound-guided nerve block. For outcome (O), our primary focus was on the effect on postoperative wound pain, as well as secondary outcomes such as the success rate of nerve blocks, time to onset, duration of analgesia, and frequency of complications.
We searched the relevant literature on 2 January 2025 in various electronic databases: PubMed, Web of Science, Cochrane Library, CNKI, Wang Fang, VIP, and Embase, without imposing any time limits. There are no restrictions on language. In addition, a manual review of the reference list of relevant articles was conducted to identify any further potential records. The search strategy incorporates key terms including: “Ultrasound-guided nerve block,” “US-guided SNB,” “nerve block,” “Ultrasound-guided scalp nerve block,” “Block,” “Nerve Blocks,” “Blockade,” “Elderly patients,” “old people,” “geriatrics,” “geriatrist,” “Geriatric Anesthesia.” These terms have been deliberately chosen to capture the broad scope of the PICO framework and to ensure a comprehensive compilation of relevant studies for this meta-analysis, for which specific search strategies are detailed in Supplementary Table 1 in Supplementary File 1.
2.2 Inclusion criteria and exclusion criteria
2.2.1 Inclusion criteria
1. Study Design: Randomized controlled trials (RCTs) and observational studies assessing the efficacy of ultrasound-guided nerve block.
2. Population: Elderly patients (age ≥=65 years or older).
3. Interventions: Studies must involve the use of ultrasound-guided nerve block as an intervention.
4. Comparison: Other forms of anesthesia other than ultrasound-guided nerve block.
5. Outcomes: The primary outcome must include the assessment of postoperative wound pain. Secondary outcomes should include the success rate of nerve block, onset time, duration of analgesia, and incidence of complications.
2.2.2 Exclusion criteria
1. Non-Clinical Studies: Laboratory-based or animal studies, case reports, reviews, editorials, and letters to the editor.
2. Non-Adult Population: Studies involving pediatric patients or patients under 65.
3. Non-Ultrasound-Guided Techniques: Studies that do not specifically use ultrasound guidance for the nerve block.
4. Incomplete Data: Studies with incomplete outcome data relevant to the primary and secondary outcomes as defined.
5. Duplicate Publications: Studies that are duplicate publications or sub-studies of included trials.
2.3 Data extraction
In our meta-analysis, literature screening and data extraction were rigorously performed by two independent evaluators, followed by a thorough cross-verification to ensure accuracy and precision. Discrepancies encountered during this process were resolved through collaborative discussions between the evaluators, with the involvement of a third-party reviewer when consensus could not be reached. The extracted data encompassed several key elements: the author(s) of each study, the publication year of the study, and specific characteristics of the included studies such as sample size, anesthesia methods, the site of nerve block, and the types and dosages of drugs used for the nerve block. The primary outcome measure extracted was the success rate of the nerve block within 30 min. Secondary outcome measures included the onset time of the block, the duration of the block’s effect, the duration of the block procedure, and the incidence rate of complications.
2.4 Quality of individual studies
The Cochrane Manual of Systematic Evaluators 5.1.0 (20) was used as the criterion for literature quality evaluation, which included random allocation methods, hiding of allocation schemes, implementation of blind methods, integrity of outcome data, selective reporting of findings, and other sources of bias. The judgments included “low risk of bias,” “unknown risk of bias,” and “high risk of bias.”
2.5 Statistical analyses
Statistical analysis was performed using Stata 16 software. The χ2 test was used to analyze the heterogeneity among the studies. If P > 0.1 and I2 < 50%, there was no statistical heterogeneity among the studies. A fixed-effects model was initially employed for the meta-analysis. However, evidence of significant heterogeneity among the included studies was observed. Consequently, a random-effects model was adopted to account for this between-study variability. Subgroup analyses were subsequently conducted to explore potential sources of heterogeneity. In the absence of identifiable sources of heterogeneity, descriptive analyses were performed to characterize the observed variability. Sensitivity analyses were then implemented to assess the robustness of the findings. Relative risk (RR) and 95% confidence intervals (CI) were used to estimate clinical efficacy, while continuous data were presented as Standardized Mean Difference (SMD) and 95% confidence intervals. An inverted funnel diagram and Begg’s test were used for publication bias analysis.
3 Results
3.1 Selected studies
A stepwise approach was employed to select eligible studies. All identified articles were exported to EndNote X9 Citation Manager. An initial screening of titles and abstracts resulted in the exclusion of 2,587 records. Furthermore, 338 duplicate entries were removed. Following a comprehensive evaluation of the remaining articles, 2,118 records were excluded. Ultimately, 25 articles met the inclusion criteria after a full-text review. The study selection process is depicted in Figure 1.
3.2 Study characteristics
The basic characteristics of the included works of literature are shown in Table 1. All the 25 included studies were retrospective studies or prospective studies. The inclusion and exclusion criteria and the evaluation criteria for each indicator are detailed in Supplementary Table 2 in Supplementary File 1.
3.3 Quality assessment
The quality assessment of this study is shown in Table 2.
3.4 Results of index meta-analysis
3.4.1 Blocking effective rate
The blocking effective rate was reported in all 10 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 58.8%. The meta-analysis using the random effects model showed that there was a statistically significant difference in the effective rate between the two groups [RR = 1.21 (1.11, 1.31), P < 0.001], and the effective rate of the experimental group was 1.21 times that of the control group (Figure 2 and Table 3).
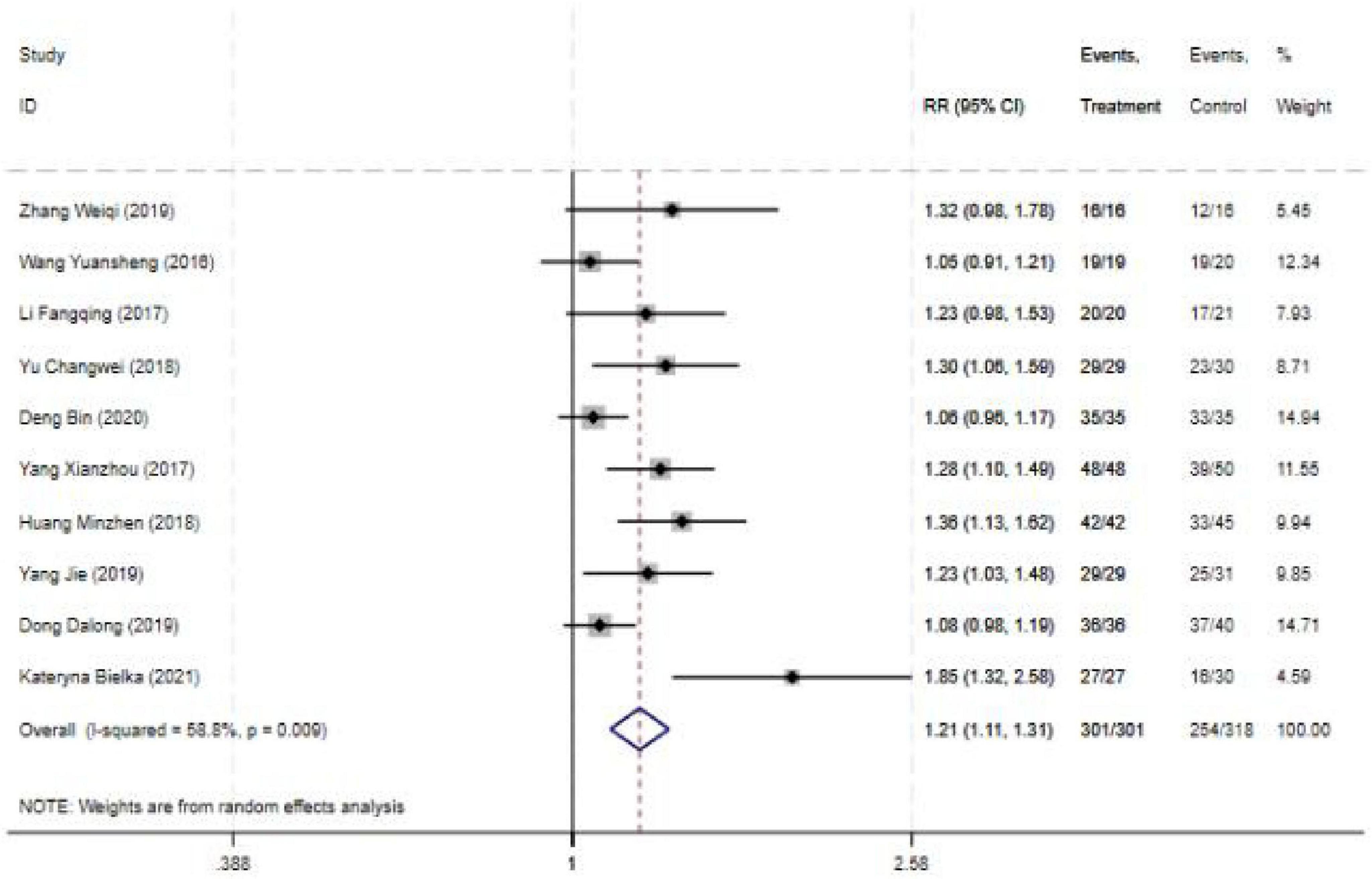
Figure 2. Forest plot comparing Blocking effective rate for ultrasound-guided nerve block vs. control group. RR: Relative risk; 95CI, 95% confidence intervals.
3.4.2 Sensory nerve block onset and duration time
The block onset time was reported in 13 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 97.5%. The meta-analysis using the random effects model showed that there was a statistically significant difference in sensory nerve block onset time between the two groups [SMD = −2.76 (−3.67, −1.85), P < 0.001], and the sensory nerve block onset time of the experimental group was shorter than that of the control group (Figure 3A and Table 3).
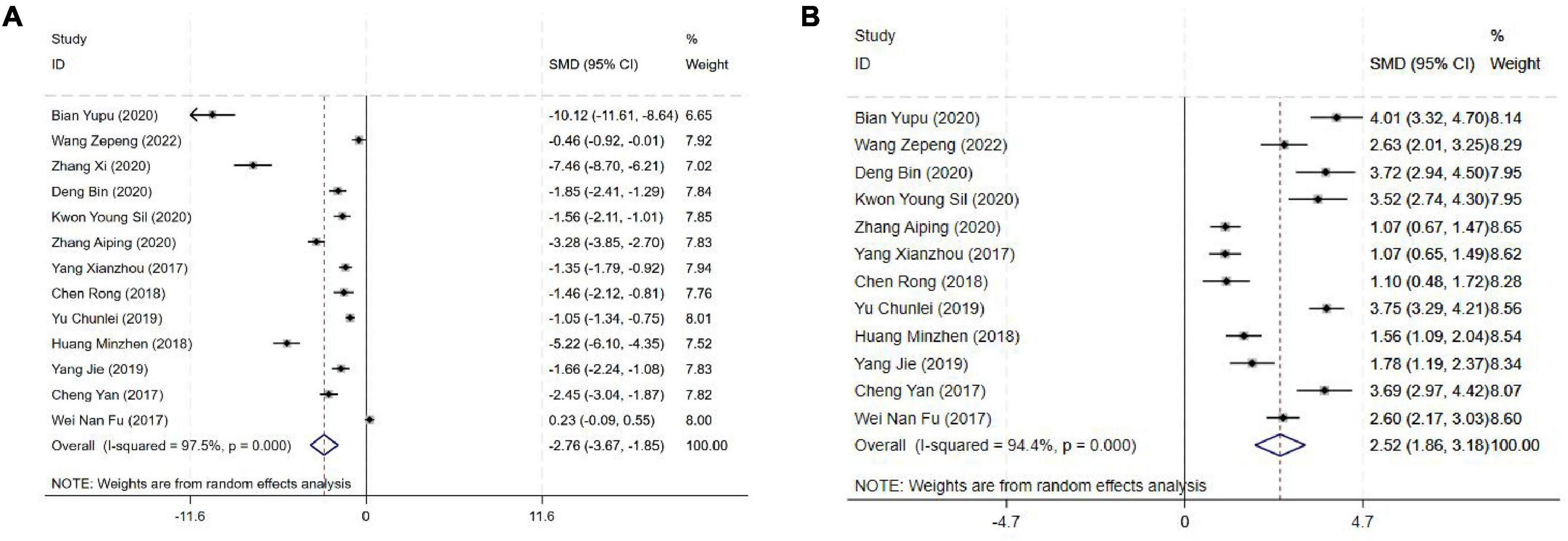
Figure 3. Forest plot comparing sensory nerve block. (A) Sensory nerve block onset time, (B) Sensory nerve block duration time. SMD, Standardized Mean Difference; 95%CI, 95% confidence intervals.
The block duration time was reported in 12 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 94.4%. A meta-analysis using a random effects model showed that sensory nerve block duration time difference between the two groups was statistically significant [SMD = 2.52(1.86,3.18), P < 0.01], and the sensory nerve block duration time of the experimental group was longer than that of the control group (Figure 3B and Table 3).
3.4.3 Motor nerve block onset and duration time
The motor nerve block onset time was reported in 12 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 96.4%. The meta-analysis using the random effects model showed that there was a statistically significant difference in motor nerve block onset time between the two groups [SMD = −1.94(−2.68, −1.19), P < 0.001], and the motor nerve block onset time of the experimental group was shorter than that of the control group (Figure 4A and Table 3).
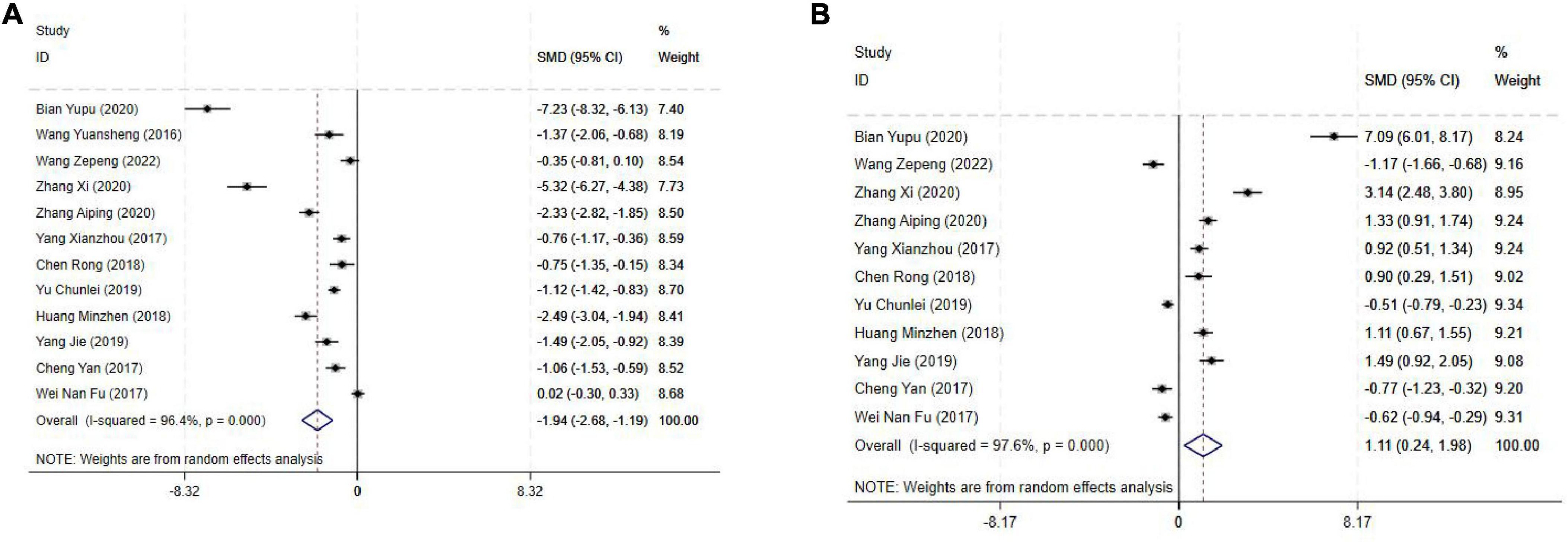
Figure 4. Forest plot comparing motor nerve block. (A) Motor nerve block onset time, (B) Motor nerve block duration time. SMD, Standardized Mean Difference; 95%CI, 95% confidence intervals.
The motor nerve block duration time was reported in 11 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 97.6%. A meta-analysis using a random effects model showed that motor nerve block duration time difference between the two groups was statistically significant [SMD = 1.11(0.24,1.98), P = 0.01], and the motor nerve block duration time of the experimental group was longer than that of the control group (Figure 4B and Table 3).
3.4.4 Analgesic effect
The VAS score post operation 4H was reported in six studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 94.80%. The meta-analysis using the random effects model showed that there was a statistically significant difference in the VAS score post operation 4H between the two groups [SMD = −1.68(−2.68, −0.68), P < 0.001] (Figure 5A and Table 3); The VAS score post operation 8H was reported in 5 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 89.30%. The meta-analysis using the random effects model showed that there was a statistically significant difference the VAS score post operation 8H between the two groups [SMD = −0.99(−1.66, −0.32), P < 0.001] (Figure 5B and Table 3); The VAS score post operation 12H was reported in 4 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 82.80%. The meta-analysis using the random effects model showed that there was a statistically significant difference in the VAS score post operation 12H between the two groups [SMD = −1.03(−1.48, −0.58), P < 0.001] (Figure 5C and Table 3); The VAS score post operation 24H was reported in 6 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 96.30%. The meta-analysis using the random effects model showed that there was a statistically significant difference in the VAS score post operation 24H between the two groups [SMD = −1.56(−2.36, −0.75), P < 0.001] (Figure 5D and Table 3).
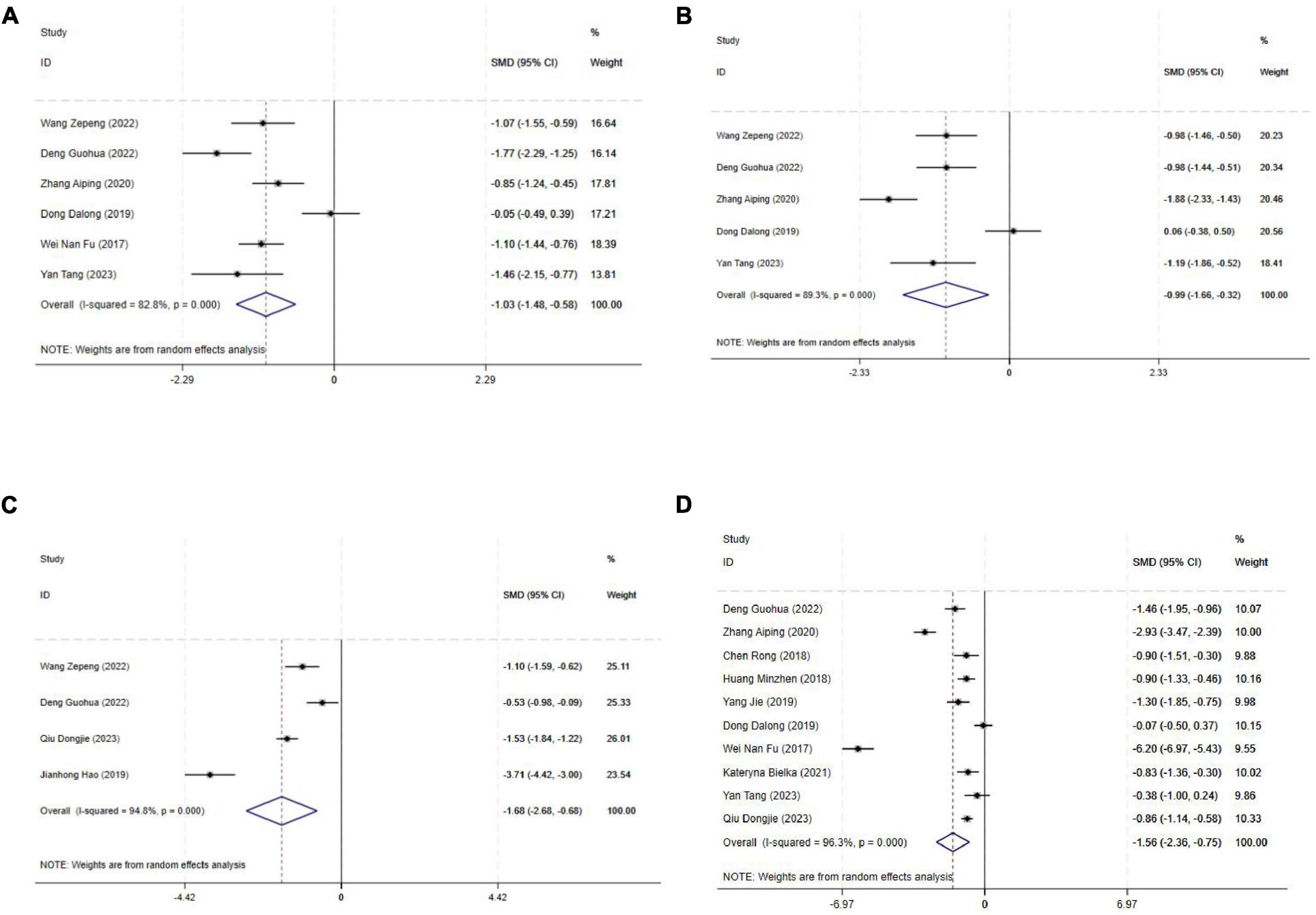
Figure 5. Forest plot comparing VAS score. (A) Post operation 4H, (B) post-operation 8H, (C) post-operation 12H, (D) post-operation 24H. SMD, Standardized Mean Difference; 95%CI, 95% confidence intervals.
The VAS scores of the ultrasound-guided nerve blocks were lower than those of the control group at 4, 8, 12, and 24 h after surgery.
3.4.5 Adverse reaction rate
The Adverse reaction rate was reported in 18 studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 74.40%. The meta-analysis using the random effects model showed that there was a statistically significant difference in the adverse reaction rate between the two groups [RR = 0.35(0.23,0.55), P < 0.001], and the adverse reaction rate of the experimental group was 0.35 times that of the control group (Figure 6 and Table 3).
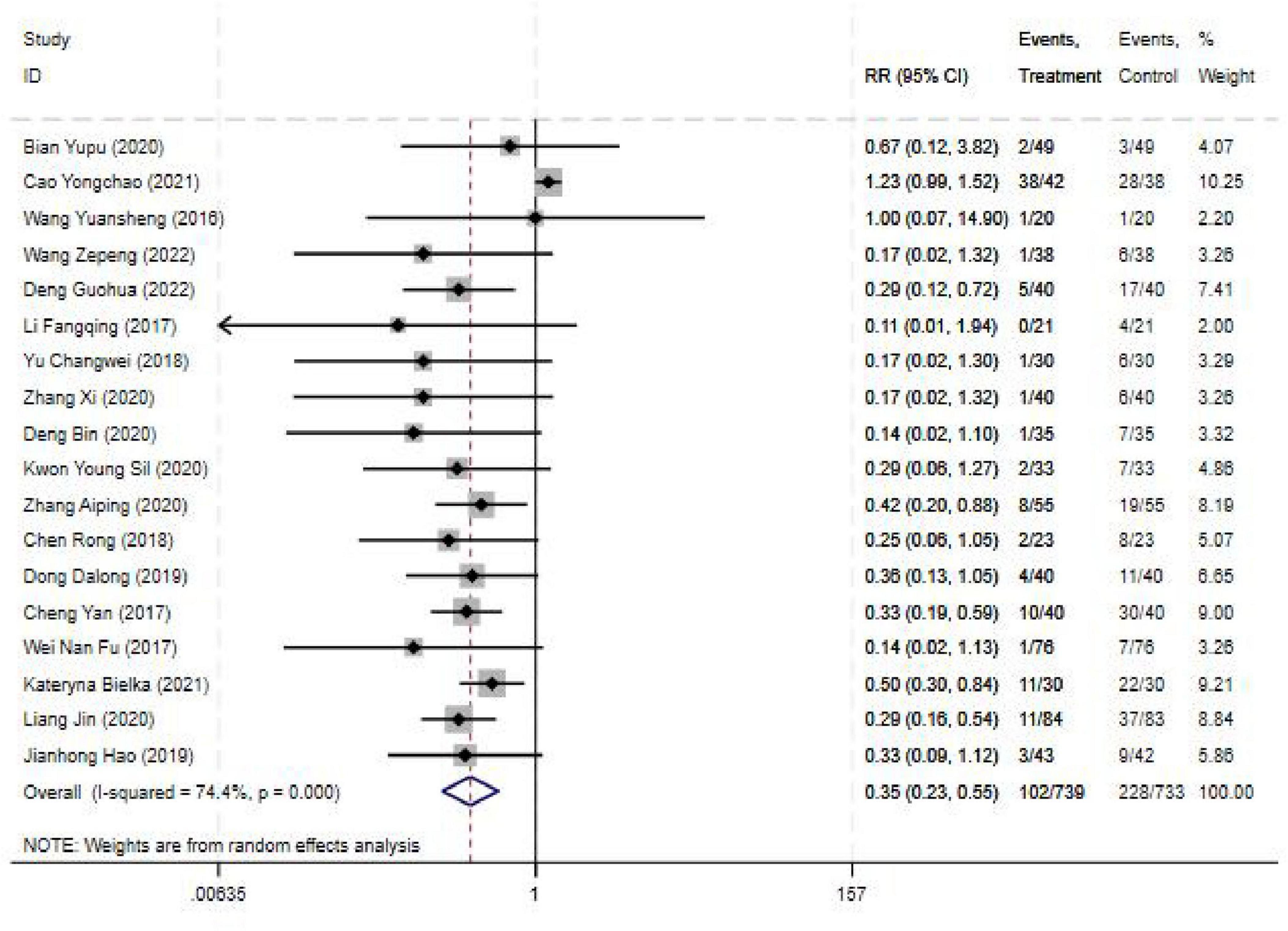
Figure 6. Forest plot comparing blocking effective rate for ultrasound-guided nerve block vs. control group. RR, Relative risk; 95%CI, 95% confidence intervals.
3.4.6 Operating time
The operating time was reported in five studies, and the results of an inter-study heterogeneity test were P < 0.001 and I2 = 92.80%. The meta-analysis using the random effects model showed that there was no significant difference in operating time between the two groups [SMD = 0.25(−0.36, 0.86), P = 0.43] (Figure 7 and Table 3).
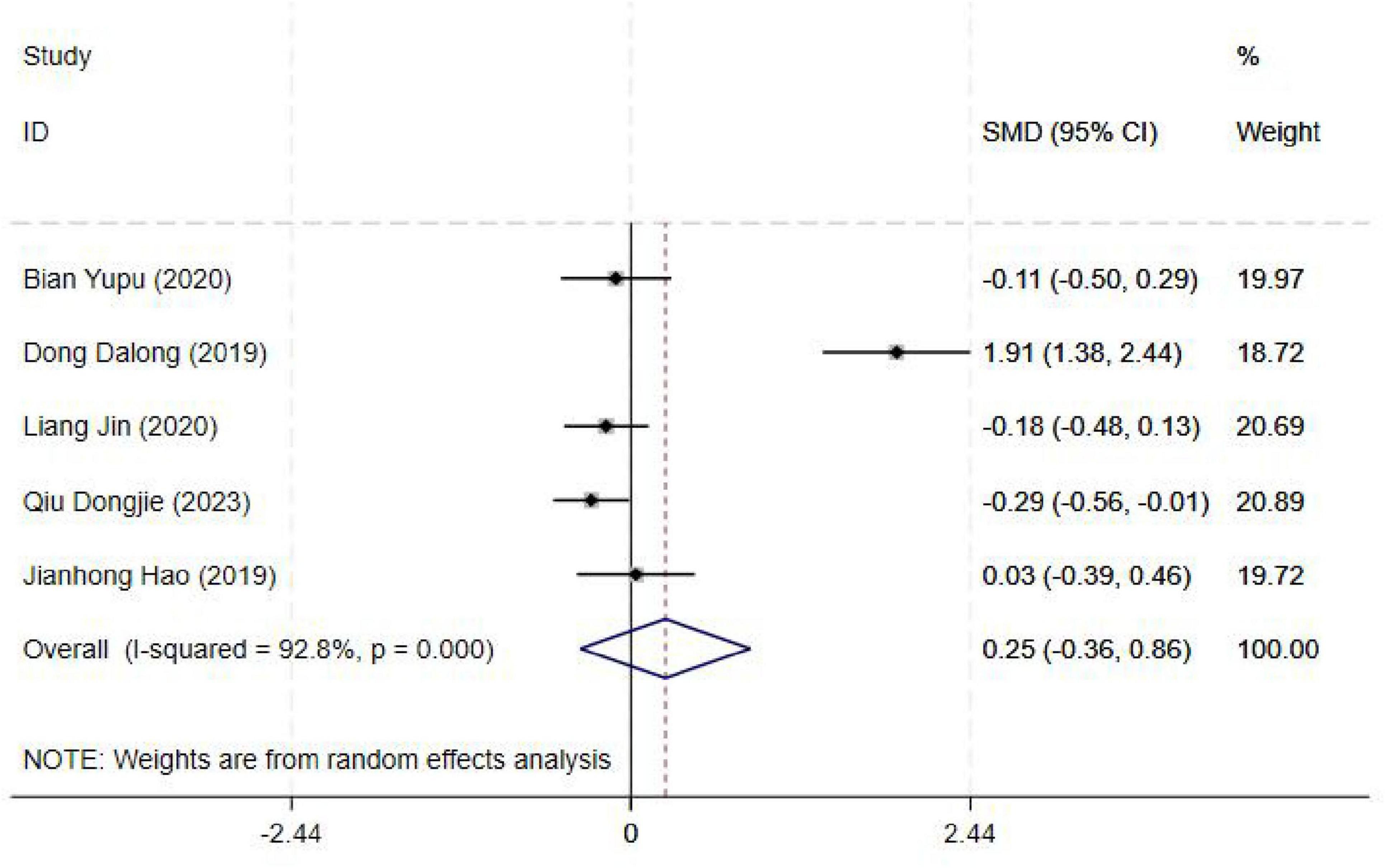
Figure 7. Forest plot comparing operating time for ultrasound-guided nerve block vs. control group. SMD, Standardized Mean Difference; 95%CI, 95% confidence intervals.
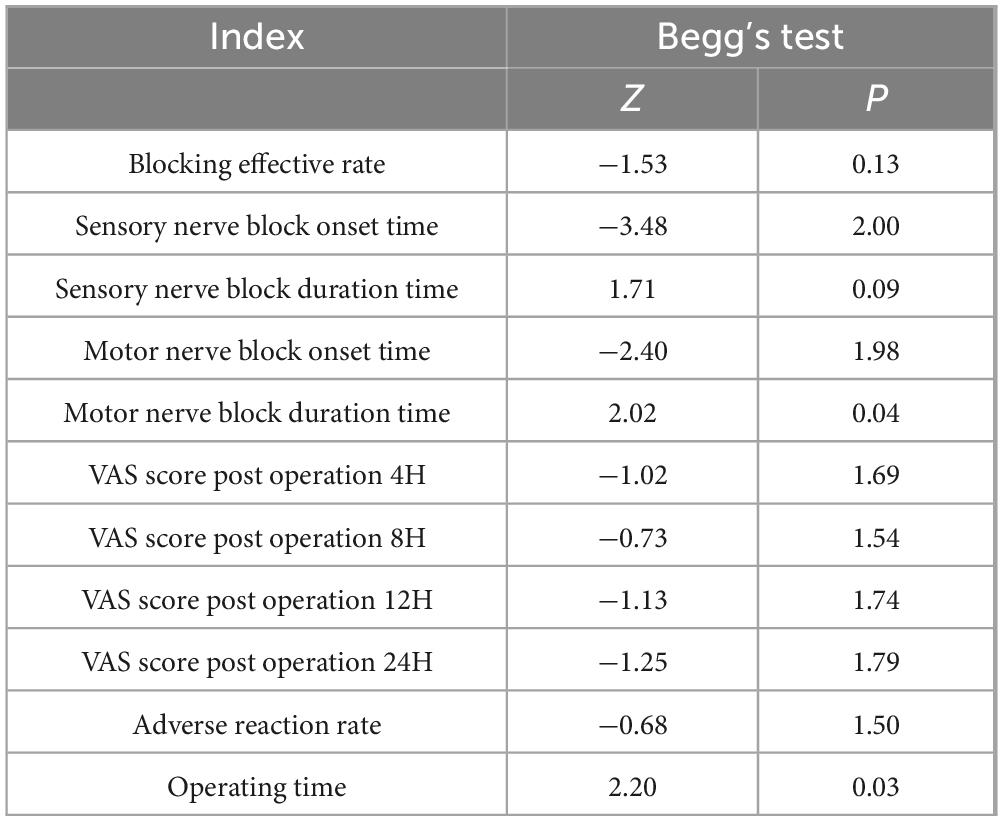
3.5 Publication bias
The Begg’s test results (Table 4) for the Blocking effective rate (z = −1.53, p = 0.13), Sensory nerve block onset time (z = −3.48, p = 2.00), Sensory nerve block duration time (z = 1.71, p = 0.09), Motor nerve block onset time (z = −2.40, p = 1.98), Motor nerve block duration time (z = 2.02, p = 0.04), VAS score post operation 4H (z = −1.02, p = 1.69), VAS score post operation 8H (z = −0.73, p = 1.79), VAS score post operation 12H (z = −1.13, p = 1.74), VAS score post operation 24H (z = −1.25, p = 0.13), Adverse reaction rate (z = −0.68, p = 1.50), Operating time (z = 2.20, p = 0.03) and the scatter distribution of each study was basically symmetrical (Supplementary Figures 1–10 in Supplementary File 2).
The results indicated that there was no publication bias except motor nerve block duration time, Operating time, and then the two indexes used the scissoring method. But the number of references was not filled after the scissoring method. So there may be a publication bias in the two indexes, the results of the meta-analysis of the two indexes should be interpreted with caution.
3.6 Sensitivity analysis
After deleting all studies one by one, the obtained 95% CI did not cross the invalid line, and the point of combined effect size was still within the original 95% CI, indicating that the results of this study were relatively robust (Supplementary Tables 1–11 in Supplementary File 2).
4 Discussion
The aging process is accompanied by the emergence of a diverse spectrum of both acute and chronic illnesses. This physiological decline manifests in a gradual deterioration of bodily functions and a diminishing organ reserve capacity, rendering elderly individuals less tolerant of surgical trauma. These factors present significant challenges to the advancement of surgical interventions in this patient population (46). These characteristics can significantly complicate upper limb, lower limb, abdominal, and thoracic surgical procedures. For instance, patients with hypertension exhibit blood pressure fluctuations during surgery, resulting in decreased vascular wall elasticity and increased fragility. This heightened susceptibility can readily lead to serious adverse events, such as cerebrovascular accidents and myocardial infarction (47, 48). To enhance the safety of surgical interventions, more nuanced anesthetic strategies are imperative. Scholars have demonstrated that in upper limb surgery, brachial plexus block can accurately block nerve conduction, effectively reduce the pain in the surgical area, reduce the number of general anesthesia drugs, and reduce the impact on cardiovascular, respiratory, and other systems, thus reducing the risk of surgery (49, 50). Therefore, it emerges as a crucial component in optimizing patient recovery and ensuring the quality of postoperative care.
This study undertook a rigorous systematic review and meta-analysis to comparatively assess the efficacy and safety of ultrasound-guided nerve block versus other anesthetic modalities in geriatric surgical patients. The ultrasound-guided nerve block technique exhibited a superior block success rate. Notably, the onset of sensory nerve block was more rapid in the experimental cohort compared to the control group, while the duration of sensory nerve block was prolonged. These findings underscore the unique advantages of ultrasound-guided nerve block in augmenting surgical safety and enhancing patient comfort within the clinical setting. This meta-analysis provides a novel perspective on the comparative evaluation of ultrasound-guided nerve block and alternative anesthetic approaches. Through a meticulous examination of key indicators, including block success rate, onset latency, analgesic duration, and complication incidence, this study offers a comprehensive assessment of these anesthetic techniques within the geriatric surgical patient population. The study findings emphasize the pivotal role of ultrasound-guided nerve blocks in contemporary clinical practice, particularly their exceptional efficacy in mitigating postoperative wound pain and enhancing surgical safety.
A meta-analysis of diverse efficacy indicators revealed that ultrasound-guided nerve blocks exhibit numerous advantages. Notably, the experimental group demonstrated superior block efficacy compared to the control group. This enhancement can be attributed to the inherent capacity of ultrasound imaging to delineate the intricate anatomical relationships between nerves and surrounding tissues. This real-time visualization enables anesthesiologists to precisely target the nerves for drug injection, thereby optimizing the blockade of neural conduction. Yu et al. (51) found that ultrasound-guided subsheath sciatic nerve block was more effective than rapidly and completely achieving tibial and foot surgical sensory block, with faster start time and comparable safety.
A noteworthy observation pertains to the relevant indicators of sensory and motor nerve blockade. Notably, the latency to onset of the block in the experimental cohort was significantly reduced compared to the control group, while the duration of the block was markedly prolonged. Consistent with these findings, Haley et al. (9) reported shorter onset times for sensory nerve block in a study of ultrasound-guided suprazygomatic nerve block to the pterygopalatine fossa compared to other anesthetic techniques. This rapid onset of anesthesia can expedite the provision of adequate pain control at the commencement of surgery, thereby mitigating patient discomfort. This finding carries significant implications for the peri-operative management of elderly surgical patients. Furthermore, a randomized, double-blind, placebo-controlled trial conducted by Rambhia et al. (52) investigating ultrasound-guided ganglion block following total knee arthroplasty demonstrated that prolonged block duration not only facilitated continuous postoperative analgesia but also mitigated the risk of various complications arising from pain-induced physiological stress responses, thereby accelerating patient recovery. Their findings align with the conclusions drawn from this study.
Analysis of the Visual Analog Scale (VAS) scores at various time points postoperatively revealed that the ultrasound-guided nerve block group exhibited significantly lower VAS scores at 4, 8, 12, and 24 h compared to the control group. This finding strongly suggests that this technique may confer more efficacious postoperative analgesia in elderly surgical patients. A study published in the American Journal of Emergency Medicine (53) corroborated these findings by comparing the analgesic efficacy of ultrasound-guided femoral nerve block (USFNB) in patients with both intracapsular and extracapsular hip fractures. This evidence underscores the critical importance of effective analgesia, particularly in geriatric patients. Adequate pain management mitigates the physiological stress response elicited by pain, thereby promoting improved sleep quality, dietary intake, and functional recovery.
Furthermore, regarding the incidence of adverse events, the experimental group exhibited a significantly lower rate, amounting to only 0.35 times that observed in the control group. This finding unequivocally demonstrates the enhanced safety profile of ultrasound-guided nerve block. This may be due to the real-time visual guidance of ultrasound. Bowness (54) posited that meticulous adjustment of image display parameters, including focus, depth, and gain (brightness), can effectively mitigate the risk of inadvertent injury to vital surrounding structures, such as blood vessels and nerves, during needle puncture. This optimization of image visualization is crucial in minimizing the likelihood of adverse events stemming from procedural errors.
This study, however, also identified several limitations. Notably, most heterogeneity tests revealed substantial heterogeneity among studies, likely attributable to variations in patient characteristics (e.g., age, comorbidities, physical condition), surgical procedures, anesthetic choices, ultrasound equipment, and operator expertise. The inconsistency of these factors may have introduced bias into the study results and limited the generalizability of the findings. Publication bias analysis indicated the absence of bias for most outcomes, with the notable exception of motor nerve block duration and operative time, which exhibited evidence of potential publication bias. Sensitivity analyses demonstrated that the study results were generally robust and reliable, with minimal influence from individual studies.
This study underscores the substantial advantages of ultrasound-guided nerve block in terms of both efficacy and safety within the elderly surgical population. However, recognizing the inherent heterogeneity of the existing evidence base and the potential for publication bias, further investigation is warranted. Specifically, larger, multi-center trials with rigorous methodology are required to elucidate the optimal application paradigm for ultrasound-guided nerve block in this patient cohort. Key areas for further exploration include: (1) the identification of appropriate patient selection criteria, (2) the refinement of operational protocols, and (3) the judicious selection of analgesic agents and their appropriate dosing regimens. These endeavors will contribute to a more robust evidence base to guide clinical practice.
4.1 Study limitation
While the scope of the literature search was not explicitly limited, the inclusion of publications in languages other than English was constrained by language barriers. Consequently, the included literature predominantly comprised Chinese publications, followed by English, raising concerns regarding potential selection bias. Furthermore, the possibility of publication bias cannot be entirely ruled out, as the search may not have encompassed all available gray literature, such as conference proceedings and supplements. Among the included studies, methodological limitations exist, particularly concerning the presence of random and blinded procedures, which significantly impact the overall quality of the evidence. The need for robust, high-quality evidence remains, specifically large-scale, multi-center, randomized controlled trials employing optimal study designs to investigate the efficacy and safety of ultrasound-guided nerve blocks in elderly surgical patients.
5 Conclusion
This meta-analysis provides a comprehensive exploration of ultrasound-guided nerve block utilization in elderly surgical patients, offering a nuanced understanding of its clinical significance. Our findings unequivocally demonstrate that ultrasound-guided nerve block confers substantial advantages. In terms of efficacy, it exhibits a superior block success rate, more rapid onset times for both sensory and motor nerve blockade, and prolonged block duration. These factors translate into efficient pain management during and after surgery, as evidenced by the lower VAS scores at multiple time points post-operation. This not only enhances patient comfort but also significantly mitigates the stress response associated with pain, thereby facilitating improved recovery trajectories in terms of sleep quality, dietary intake, and functional restoration.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Heterogeneity of Studies: The included studies in the meta-analysis may have significant differences in terms of study design (e.g., randomized controlled trials vs. observational studies), patient populations (varying ages, comorbidities, and types of surgeries among elderly patients), the specific techniques of ultrasound-guided nerve blocks used (different approaches, frequencies, etc.), and outcome measures. This heterogeneity can limit the generalizability of the pooled results and may introduce bias. Requests to access these datasets should be directed to d2FuZ3Jvbmc4NzEwQDE2My5jb20=.
Author contributions
RW: Data curation, Formal analysis, Funding acquisition, Software, Supervision, Validation, Writing – original draft. JJ: Conceptualization, Investigation, Methodology, Project administration, Resources, Visualization, Writing – review & editing. XP: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1580172/full#supplementary-material
References
1. Gu J, Wang E, Dai S, Dong R, Xu F, Shen Z, et al. Ultrasound-guided multiple nerve blocks: a safe and effective anesthetic modality in geriatric hip fracture patients. Clin J Pain. (2021) 37:881–6. doi: 10.1097/AJP.0000000000000988
2. Cao X, White PF, Ma H. Perioperative care of elderly surgical outpatients. Drugs Aging. (2017) 34:673–89. doi: 10.1007/s40266-017-0485-3
3. Hausman MS Jr, Jewell ES, Engoren M. Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg. (2015) 120:1405–12. doi: 10.1213/ANE.0000000000000574
4. Hazen S, Larsen P, Martin J. General anesthesia and elderly surgical patients. AORN J. (1997) 65:821–2. doi: 10.1016/s0001-2092(06)63005-6
5. Scurrah A, Shiner C, Stevens J, Faux S. Regional nerve blockade for early analgesic management of elderly patients with hip fracture - a narrative review. Anaesthesia. (2018) 73:769–83. doi: 10.1111/anae.14178
6. Kaçmaz M, Turhan Z. Spinal anesthesia versus combined sciatic nerve/lumbar plexus nerve block in elderly patients undergoing total hip arthroplasty: a retrospective study. Ann Saudi Med. (2022) 42:174–80. doi: 10.5144/0256-4947.2022.174
7. Desai N, Kirkham K, Albrecht E. Local anaesthetic adjuncts for peripheral regional anaesthesia: a narrative review. Anaesthesia. (2021) 76:100–9. doi: 10.1111/anae.15245
8. Smith L, Barrington M. Ultrasound-guided blocks for cardiovascular surgery: which block for which patient? Curr Opin Anaesthesiol. (2020) 33:64–70. doi: 10.1097/ACO.0000000000000818
9. Smith C, Dickinson K, Carrazana G, Beyer A, Spana J, Teixeira F, et al. Ultrasound-guided suprazygomatic nerve blocks to the pterygopalatine fossa: a safe procedure. Pain Med. (2022) 23:1366–75. doi: 10.1093/pm/pnac007
10. Salam A, Aamir R, Khan R, Ahmed A, Rehman A. Safety and effectiveness of ultrasound guided peripheral nerve blocks: audit at tertiary care hospital. J Pak Med Assoc. (2021) 71:1623–6. doi: 10.47391/JPMA.447
11. Priyadarshini K, Behera B, Tripathy B, Misra S. Ultrasound-guided transverse abdominis plane block, ilioinguinal/iliohypogastric nerve block, and quadratus lumborum block for elective open inguinal hernia repair in children: a randomized controlled trial. Reg Anesth Pain Med. (2022) 47:217–21. doi: 10.1136/rapm-2021-103201
12. Haley C, Beauchesne A, Fox J, Nelson A. Block time: a multispecialty systematic review of efficacy and safety of ultrasound-guided upper extremity nerve blocks. West J Emerg Med. (2023) 24:774–85. doi: 10.5811/westjem.56058
13. Li J, Szabova A. Ultrasound-guided nerve blocks in the head and neck for chronic pain management: the anatomy. Sonoanatomy, and Procedure. Pain Physician. (2021) 24:533–48.
14. Hao W, Zhang C, He J, Pei R, Huo H, Liu H. Effect of ultrasound-guided nerve blocks on anesthesia and pulmonary function in patients undergoing distal radius fracture surgery. Medicine. (2024) 103:e39436. doi: 10.1097/MD.0000000000039436
15. Nuthep L, Klanarong S, Tangwiwat S. The Analgesic effect of adding ultrasound-guided pericapsular nerve group block to suprainguinal fascia iliaca compartment block for hip fracture surgery: a prospective randomized controlled trial. Medicine. (2023) 102:e35649. doi: 10.1097/MD.0000000000035649
16. Beaudoin F, Nagdev A, Merchant R, Becker B. Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med. (2010) 28:76–81. doi: 10.1016/j.ajem.2008.09.015
17. Hayaran N, Malhotra R, Tyagi S, Jain A. Transversus abdominis plane block with ilioinguinal-iliohypogastric nerve a viable alternative to provide surgical anesthesia for cesarean delivery: a case report. A A Pract. (2019) 12:185–6. doi: 10.1213/XAA.0000000000000875
18. Diwan S, Nair A, Sancheti P, Zundert A. Does subepineural injection damage the nerve integrity? A technical report from four amputated limbs. Korean J Pain. (2021) 34:132–6. doi: 10.3344/kjp.2021.34.1.132
19. Elsman E, Butcher N, Mokkink L, Terwee C, Tricco A, Gagnier J, et al. Study protocol for developing, piloting and disseminating the PRISMA-COSMIN guideline: a new reporting guideline for systematic reviews of outcome measurement instruments. Syst Rev. (2022) 11:121. doi: 10.1186/s13643-022-01994-5
20. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. The Cochrane Collaboration. (2011).
21. Weiqi Z. Effect observation and safety analysis of ultrasound-guided lower back plexus sciatic nerve block anesthesia in elderly lower extremity orthopedic surgery. Electr J General Stomatol. (2019) 6:135–8. doi: 10.16269/j.cnki.cn11-9337/r.2019.13.097
22. Yupu B, Kun H. Application effect of ultrasound-guided lumbar plexus-sciatic nerve block anesthesia in artificial knee replacement in the elderly and its influence on complications. China Acad J Electronic Publishing House. (2022) 7:87–9. doi: 10.19347/j.cnki.2096-1413.202218024
23. Yongchao C. Clinical study of ultrasound-guided brachial plexus block for upper extremity anesthesia in elderly patients. Modern Diagnosis Treatment. (2021) 32:1092–3.
24. Yuansheng W, Lihui C. Application of ultrasound-guided intrascaline brachial plexus block. Int Med Health Guidance News. (2016) 22:3563–5. doi: 10.3760/cma.j.issn.1007-1245.2016.23.007
25. Zepeng W. The clinical value of ultrasound-guided femoral nerve block combined with lateral femoral cutaneous nerve block in the operation of patellar fracture in elderly patients. J Imaging Res Med Appl. (2022) 6:179–81.
26. Guohua D. Effect of ultrasound-guided femoral nerve block anesthesia on postoperative an-algesia in elderly patients with knee arthroplasty. World J Complex Med. (2022) 8:63–6.
27. Fangqing L. Value of ultrasound-guided intermuscular groove brachial plexus block in upper extremity operation in elderly patients. Heilongjiang Med J. (2017) 30:881–2. doi: 10.14035/j.cnki.hljyy.2017.04.089
28. Changwei Y, Jinbao C. Application effect of brachial plexus nerve block under ultrasonic guidance via interscalene combined with supraclavicular approach in upper -limb surgery of elderly patients. Anhui Med J. (2018) 39: 182–5.
29. Xi Z. Application of ultrasound-guided nerve block anesthesia in elderly patients undergoing unilateral lower extremity orthopedic surgery. Chin J Mod Drug Appl. (2020) 14:73–4. doi: 10.14164/j.cnki.cn11-5581/r.2020.06.033
30. Bin D. Application of ultrasound-guided nerve block anesthesia in elderly patients undergoing single upper extremity orthopedic surgery. Medical Diet and Health. (2020) 18:77–9.
31. Sil K, Won K. Application effect of ultrasound-guided nerve block anesthesia in elderly patients undergoing upper extremity orthopedic surgery. China Rural Health. (2020) 12:88.
32. Aiping Z, Yuxing Q. Application value of lumbar plexus combined with seiatic ner’ve block anesthesia guided by ultrasound in the operation of intertrochanterie fracture of the elderly patients. J Bengbu Med Coll. (2020) 45:592–5. doi: 10.13898/j.cnki.issn.1000-2200.2020.05.009
33. Xianzhou Y. Application effect of ultrasound-guided lumbar plexus combined with sciatic nerve block anesthesia in elderly patients with lower extremity orthopedic surgery. Chinese J Clin Rational Drug Use. (2017) 10:131–2. doi: 10.15887/j.cnki.13-1389/r.2017.18.066
34. Rong C, Ye Y. Application value of ultrasound-guided lumbar plexus combined with sciatic nerve block anesthesia in elderly patients with lower extremity orthopedic surgery. Chinese J Crit Care Med. (2018) 38:121. doi: 10.3969/j.issn.1002-1949.2018.z1.111
35. Chunlei Y. Observation on the effect of ultrasound-guided lower back plexus sciatic nerve block anesthesia in elderly lower extremity orthopedic surgery. China Reflexolocy. (2019) 28:96–7. doi: 10.19589/j.cnki.issn1004-6569.2019.24.096
36. Minzhen H, Qing L, Haifeng H. Application of ultrasound-guided lower back plexus sciatic nerve block anesthesia in elderly patients with lower extremity orthopedic surgery. Chinese J Trauma Disabil Med. (2018) 26:43–5. doi: 10.13214/j.cnki.cjotadm.2018.12.025
37. Jie Y, Jiming S, Hongzhuan H. Application of ultrasound-guided lower back plexus sciatic nerve block anesthesia in elderly lower extremity orthopedic surgery. J Imaging Res Med Appl. (2019) 3:212–3. doi: 10.3969/j.issn.2096-3807.2019.06.143
38. Dalong D, Mingming Z, Ankui W, Qun G, Shengfeng L, Zhihua M. AppHcation of ultrasound-gllided lumbosacral plexus nerve block combined with laryngeal mask general anesthesia in elderly patients with total hip joint replacement. J Clin Med Pract. (2019) 23:71. doi: 10.7619/jcmp.201902018
39. Yan C, Chen L. Application of ultrasound-guided lumbosacral plexus block in elderly patients undergoing hip replacement. Zhejiang J Traumatic Surg. (2017) 22:813–4. doi: 10.3969/j.issn.1009-7147.2017.04.096
40. Fu W, Cuibao W. Application of ultrasound-guided lower extremity nerve block in elderly critically ill patients undergoing femoral head replacement. J Med Theory Pract. (2017) 30:3364–5. doi: 10.19381/j.issn.1001-7585.2017.22.038
41. Bielka K, Kuchyn I, Tokar I, Artemenko V, Kashchii U. Psoas compartment block efficacy and safety for perioperative analgesia in the elderly with proximal femur fractures: a randomized controlled study. BMC Anesthesiol. (2021) 21:252. doi: 10.1186/s12871-021-01473-9
42. Tang Y, Zhang X, Yi S, Li D, Guo H, Liu Y, et al. Ultrasound-guided pericapsular nerve group (PENG) block for early analgesia in elderly patients with hip fractures: a single-center prospective randomized controlled study. BMC Anesthesiol. (2023) 23:383. doi: 10.1186/s12871-023-02336-1
43. Jin L, Yao R, Heng L, Pang B, Sun F, Shen Y, et al. Ultrasound-guided continuous thoracic paravertebral block alleviates postoperative delirium in elderly patients undergoing esophagectomy: a randomized controlled trial. Medicine. (2020) 99:e19896. doi: 10.1097/MD.0000000000019896
44. Dongjie Q, Longbiao Z, Peng L, Li J, Hongmeng X, Zhiyan C, et al. Effects of thoracic paravertebral nerve block on postoperative pain and postoperative delirium in elderly patients undergoing thoracoscopic lobectomy. Medicine. (2023) 102:e32907. doi: 10.1097/MD.0000000000032907
45. Hao J, Dong B, Zhang J, Luo Z. Pre-emptive analgesia with continuous fascia iliaca compartment block reduces postoperative delirium in elderly patients with hip fracture. A randomized controlled trial. Saudi Med J. (2019) 40:901–6. doi: 10.15537/smj.2019.9.24483
46. Luchette FA, Barraco RD. Nuances of surgical care for the elderly. Clin Geriatr Med. (2019) 35:xiii–xiv. doi: 10.1016/j.cger.2018.10.001
47. Duran-Salgado MB, Rubio-Guerra AF. Lifestyle changes and surgical treatment for hypertension in the elderly. Cardiovasc Hematol Agents Med Chem. (2015) 12:174–86. doi: 10.2174/1871525713666150310110650
48. Liu Y, Huang Y, Wang R, Zhai Y, Huang K, Ren Z. Sedation with a 1:1 mixture of etomidate and propofol for gastroscopy in hypertensive elderly patients. J Clin Hypertens. (2023) 25:778–83. doi: 10.1111/jch.14693
49. Xing T, Ge L. Ultrasound-guided brachial plexus block by costoclavicular space approach: a narrative review. Med Sci Monit. (2023) 29:e939920. doi: 10.12659/MSM.939920
50. Kirkham K, Albrecht E. Perineural or intravenous dexamethasone in interscalene brachial plexus block. Br J Anaesth. (2020) 124:15–7.
51. Yu D, Wang X, Jiang L, Wu Y, Han S, Li J. Evaluating the impact of ultrasound-guided subsheath versus extrasheath sciatic nerve block on postoperative wound pain in tibial and foot surgeries: a systematic review and meta-analysis. Int Wound J. (2024) 21:e14640. doi: 10.1111/iwj.14640
52. Rambhia M, Chen A, Kumar AH, Bullock WM, Bolognesi M, Gadsden J. Ultrasound-guided genicular nerve blocks following total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. (2021) 46:862–6. doi: 10.1136/rapm-2021-102667
53. Dickman E, Pushkar I, Likourezos A, Todd K, Hwang U, Akhter S, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Am J Emerg Med. (2016) 34:586–9. doi: 10.1016/j.ajem.2015.12.016
Keywords: elderly, clinical effects, safety, meta-analysis, ultrasound-guided nerve blocks
Citation: Wang R, Ju J and Pang X (2025) Efficacy and safety of ultrasound-guided nerve blocks in elderly surgical patients: a meta-analysis. Front. Med. 12:1580172. doi: 10.3389/fmed.2025.1580172
Received: 25 February 2025; Accepted: 21 July 2025;
Published: 18 August 2025.
Edited by:
Somchai Amornyotin, Mahidol University, ThailandReviewed by:
Christian Bohringer, UC Davis Medical Center, United StatesNada Pejcic, University Clinical Center Niš, Serbia
Copyright © 2025 Wang, Ju and Pang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoyi Pang, cHh5LTIwMDJAMTYzLmNvbQ==
 Rong Wang
Rong Wang Jinlong Ju2
Jinlong Ju2