- Department of Gastroenterology, Shenzhen Luohu People’s Hospital, Shenzhen, China
Idiopathic Mesenteric Phlebosclerosis Colitis (IMP) is indeed a rare and potentially life-threatening condition characterized by chronic ischemic changes in the colon, primarily due to calcification of the mesenteric veins. This disease is often associated with long-term use of certain herbal medicines, particularly in Asian populations, where its prevalence is notably higher. This report describes a 55-year-old male patient who has been taking Chinese patent medicine orally for an extended period to treat prostatitis. His primary symptom is diarrhea. Imaging studies revealed multiple linear calcifications in the mesenteric veins surrounding the ascending and transverse colon. Colonoscopic findings showed bluish-purple discolored mucosa and multiple ulcers of the colonic and rectal mucosa. Pathological biopsy indicated fibrous tissue proliferation in the mucosal lamina propria and thickening of some blood vessel walls accompanied by hyaline degeneration. Based on clinical presentation, CT, colonoscopy, and histopathological findings, the final diagnosis was confirmed as IMP.
Introduction
Idiopathic Mesenteric Phlebosclerosis Colitis (IMP) is a rare form of ischemic colitis that primarily impacts the right hemicolon, characterized by the thickening of the colonic wall and calcification of the mesenteric veins. This condition is particularly prevalent in East Asia (1, 2), where there is a notable association with the long-term use of traditional herbal medicines, especially those containing geniposide, which may contribute to the disease’s pathogenesis (3, 4). Guo et al. (1) suggested that the use of herbal medicine might be linked to the development of IMP. A 2021 retrospective review of 240 individuals, predominantly of East Asian descent, conducted by Wang et al. (5) found that 78.7% of those diagnosed with IMP had used herbal medicines. The ileocecum and ascending colon are primary sites for absorbing water, nutrients, and toxins, which may explain why IMP typically affects the right colon and can extend to the descending colon, sigmoid colon, or rectum (6).
The clinical manifestations of IMP often include abdominal pain, diarrhea, and weight loss, which can lead to misdiagnosis as inflammatory bowel disease or other gastrointestinal disorders (7, 8). Diagnosis of IMP typically relies on imaging techniques such as computed tomography (CT) and colonoscopy. CT scans reveal characteristic features such as tree-like mesenteric venous calcifications and colonic wall thickening, while colonoscopy may show a dark purple discoloration of the mucosa along with erosions and ulcerations (6, 9). The histopathological examination often reveals fibrosis and calcification in the veins, which are critical for confirming the diagnosis (10, 11).
In this paper, we describe a case of IMP involving the entire colorectum, attributed to the prolonged oral intake of Chinese patent medicine. Although the disease was not identified in its early stages, several characteristic features of its progression are highlighted.
Treatment options for IMP remain controversial and vary based on the severity of the disease. While conservative management is often sufficient for asymptomatic patients or those with mild symptoms, surgical intervention, such as colectomy, may be necessary for patients presenting with severe symptoms or complications like intestinal obstruction (12, 13). A systematic review of cases indicates that a significant proportion of patients experience good recovery following conservative treatment, although some may require surgical intervention due to the severity of their condition (5, 14). In summary, idiopathic mesenteric phlebosclerosis is a complex condition that necessitates a high index of suspicion, particularly in patients with a history of herbal medicine use. Early diagnosis through appropriate imaging and histopathological evaluation is crucial for effective management and improved patient outcomes (15, 16).
Case report
A 55-year-old male visited the Department of Gastroenterology at our hospital with a 2-year history of diarrhea. More than 2 years prior, the patient had diarrhea without obvious cause and passed yellow watery stools 6–8 times a day, more than 10 times a day. The patient’s medical history includes chronic prostatitis for over 10 years, for which he had been taking “Shubitong Capsules, Longjintonglin Capsules, Prostatitis Relief Capsules, and Qinglin Granules” as traditional Chinese medicine. He also had a 10-year history of hypertension, treated with oral metoprolol succinate. No obvious abnormality was found by physical examination.
Laboratory tests indicated hypokalemia (K 3.4 mmol/L), hyponatremia (NA 136 mmol/L), hypoalbuminemia (ALB 38.9 g/L), and positive fecal occult blood test (OB). The T cells spot test (T-Spot TB) was positive, while EB virus antibodies (anti-EB-IgM) and cytomegalovirus antibodies (anti-CMV-IgG and anti-CMV-IgM) were all negative. No significant abnormalities were found in erythrocyte sedimentation rate, C-reactive protein, complete blood count, coagulation profile, liver and kidney function tests, D-dimer, urinalysis, immunoglobulins, Immunoglobulin G4 (IgG4), gastrointestinal tumor markers, fasting blood glucose, stool bacterial cultures, anti-nuclear antibodies, antibody spectrum, anticardiolipin antibodies (ACA), β2-glycoprotein 1, antineutrophil cytoplasmic antibody (ANCA), and lupus anticoagulative substance.
CT demonstrated an increased number of mesenteric vein branches surrounding the ascending colon, transverse colon, and left small intestine (Figure 1). Multiple short, linear calcifications were observed in the mesenteric veins around the ascending and transverse colon (Figure 1). CTE demonstrates thickening of the colonic wall in the right hemicolon, with multiple short linear calcifications in the branches of the mesenteric veins (Figure 2).
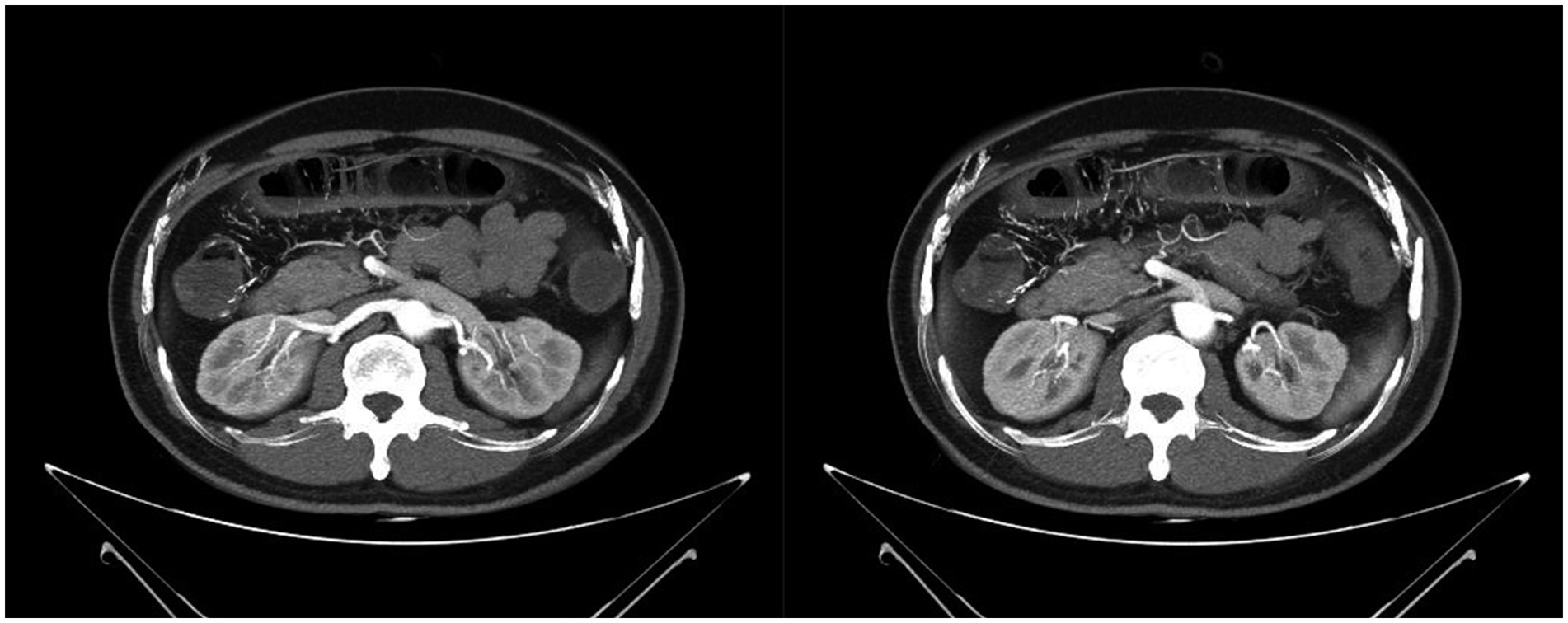
Figure 1. Computed tomography showed a thickened bowel wall with edema of the colonic wall in the right hemicolon, accompanied by multiple calcifications in the surrounding vasculature.
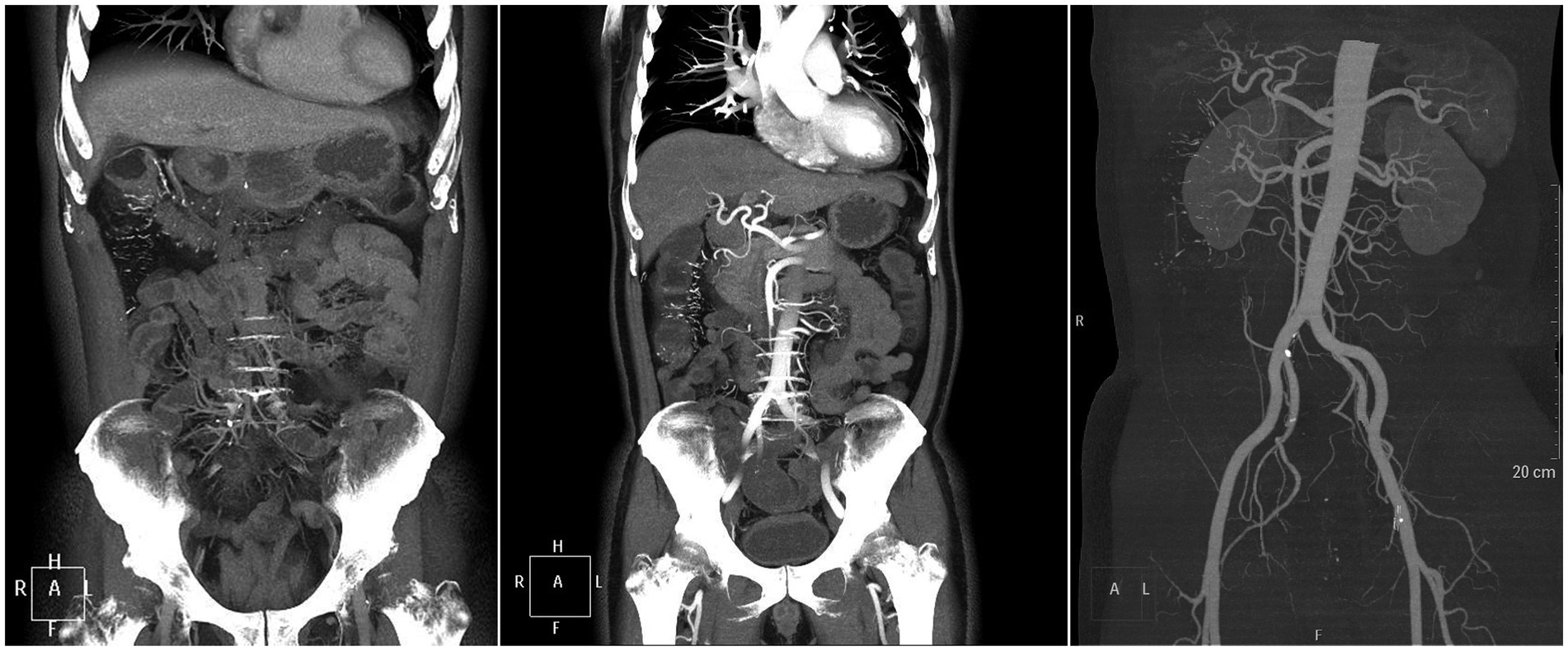
Figure 2. CTE demonstrates thickening of the colonic wall in the right hemicolon, with multiple short linear calcifications in the branches of the mesenteric veins.
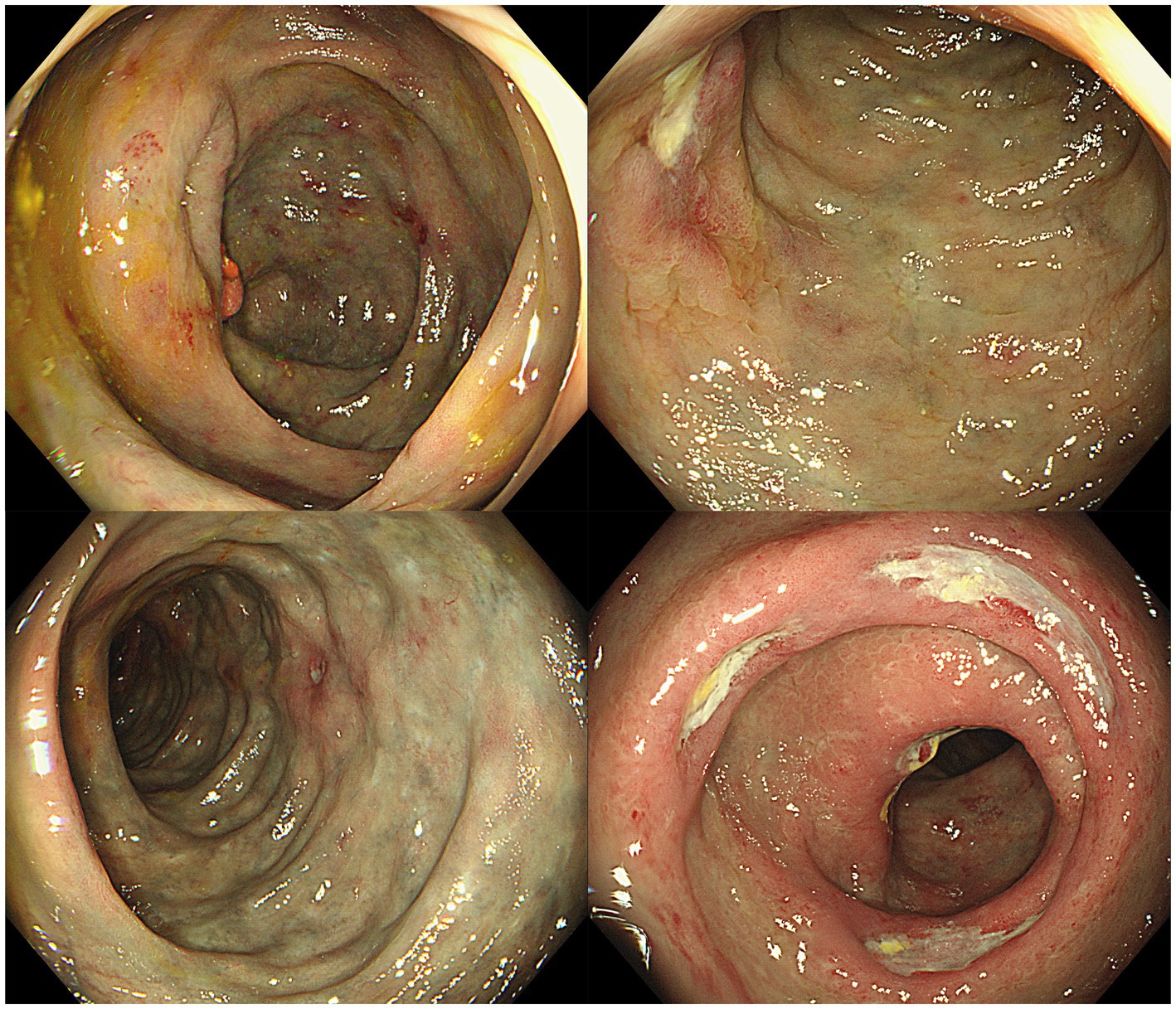
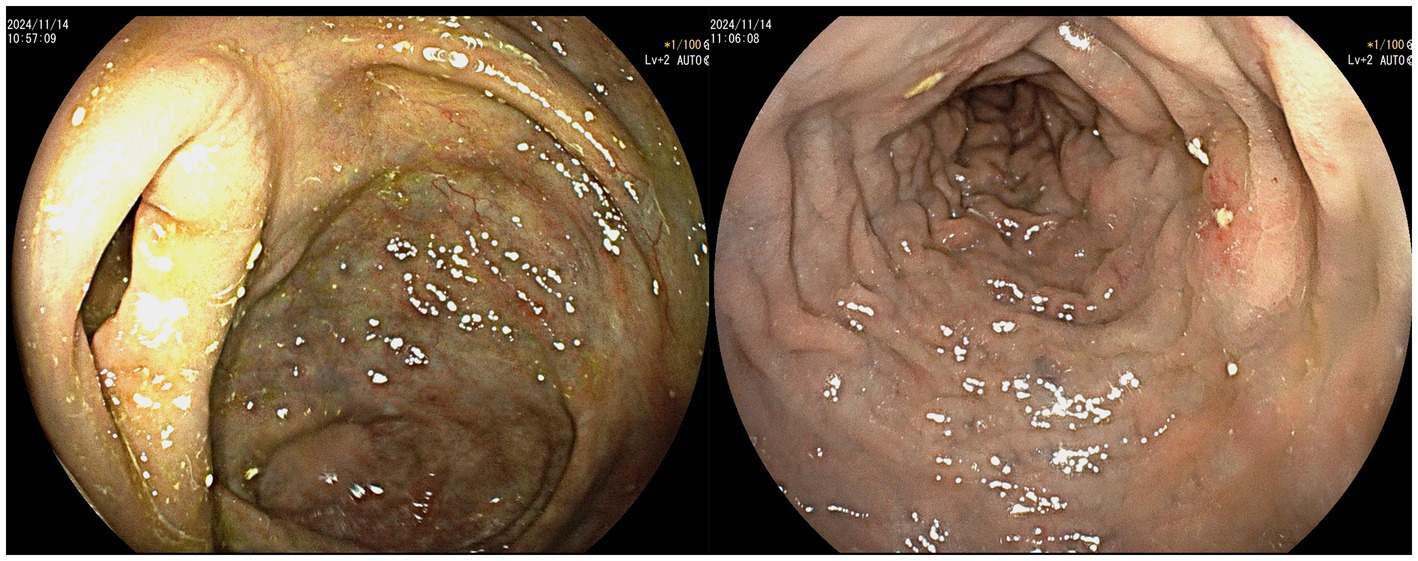
Colonoscopy revealed that the mucosa of the entire colon and rectum was congested, edematous, and had a bluish-purple discoloration, accompanied by multiple ulcers. The surface of the ulcers was covered with a white necrotic tissue (Figure 3).
Pathological results indicated fibrous tissue proliferation in the mucosal lamina propria, with some blood vessel walls showing thickening and hyaline degeneration under microscopy. A small infiltration of lymphocytes and plasma cells was observed in the stroma. The crypt glands varied in size, but no structural abnormalities were noted. Immunohistochemistry (IHC) results were: Actin(−), Desmin(−), SMA(−). Special staining showed: Masson(+), Congo Red(−) (Figure 4).
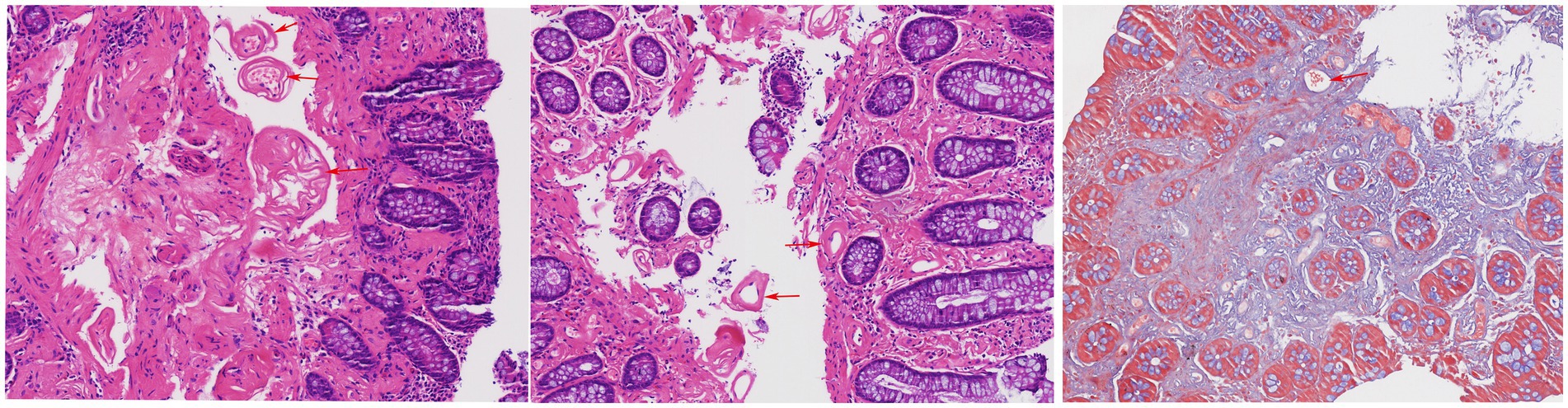
Figure 4. Thickening of blood vessel wall and hyalinization (indicated by red arrows). Masson’s trichrome stain demonstrates perivascular fibrosis (indicated by red arrows).
A final diagnosis of IMP was reached by integrating clinical characteristics with results from CT scans, colonoscopy, and histopathological analysis. The treatment plan stopped the patient’s use of traditional Chinese medicine and included mesalazine for intestinal inflammation, probiotics for gut health, aspirin for antiplatelet therapy, and atorvastatin for lowering lipids. The patient was discharged once diarrhea subsided. A follow-up colonoscopy 3 months later showed improved colorectal mucosal changes (Figure 5).
Discussion
IMP is a rare form of chronic ischemic colitis with an unclear etiology. This disease primarily manifests as sclerosis of the mesenteric veins and their branches, leading to fibrosis, hyalinization, calcification, and thickening of the colonic wall (17). The pathogenesis of IMP may involve chronic injury to venous smooth muscle and endothelium, leading to progressive fibrosis and calcification of the vessel walls, and even gradual venous occlusion. Impaired venous return causes chronic ischemia of the intestinal wall, which in turn can induce dense fibrous connective tissue proliferation, resulting in intestinal lumen narrowing and bowel obstruction (18, 19). Radiologically, IMP typically presents with calcification of the colonic wall, especially in the right colon, a feature more commonly observed in Asian populations (20). The proposed hypothesis is that ingested toxins and biochemicals are predominantly absorbed from the right colon. Chronic stasis within the lumen leads to cephalad migration, and along with increased intraluminal pressure, causes prolonged venous return reduction, resulting in impaired venous drainage and hemorrhagic infarction of the affected colonic wall (21). Few cases have documented the pathology extending to involve the transverse colon or even the entire colon. One confirmed case involved only the left colon, with the right colon remaining unaffected (21). Although the exact etiology of IMP remains unknown, studies have suggested that prolonged use of herbal medicine, particularly those containing geniposide (22), licorice (glycyrrhizin), Scutellaria baicalensis (baicalin), Poria cocos, and alcohol may be associated with its development (17, 20, 23, 24). The consumption of herbal medicine with sanshishi as an ingredient has shown a strong correlation with IMP (25).
The current pathological mechanism primarily revolves around the toxic metabolite hypothesis: After being absorbed into the mesenteric veins, geniposide can induce intimal hyperplasia, thickening, and fibrosis of the venous walls, leading to the obstruction of the venous lumen and impaired intestinal venous return. This results in intestinal wall thickening and edema. Geniposide can also directly damage the intestinal wall, causing ulcer formation and fibrosis of the lamina propria. Moreover, when interacting with amino acids and/or proteins in the intestinal wall, it transforms into a dark blue pigment, which is likely responsible for the dark blue or purple discoloration of the mucosa observed during colonoscopy.
In this case, the patient took various traditional Chinese medicines orally during the period of chronic prostatitis, most of which contained geniposide. Additionally, the patient consumed these medications in doses exceeding the recommended levels for an extended period. Clinically, the symptoms of IMP are varied and non-specific, primarily including abdominal pain, bloating, and diarrhea (13). The primary clinical manifestation in this case was diarrhea, which is consistent with this condition. In the early stages, some patients might not have symptoms, but those with advanced disease could develop intestinal obstructions and even perforations (23, 26). The diagnosis of IMP primarily relies on abdominal CT and colonoscopy. Abdominal CT is crucial in identifying the characteristic tortuous thread-like calcifications in the mesenteric veins, which are indicative of IMP. These calcifications are typically seen in the right hemicolon and can extend to other parts of the colon (1, 27).
CT findings primarily include extensive punctate and linear calcifications in the areas traversed by the mesenteric veins and their branches, with the linear calcifications perpendicular to the intestinal wall. Mesenteric CTV (CT venography) more clearly demonstrates the relationship between the calcifications and the mesenteric veins. Additionally, the involved intestinal wall shows swelling and thickening, with mild uniform enhancement on contrast-enhanced scans. Some researchers have found that patients without a history of herbal medicine use exhibit slightly different features, with calcifications confined to the submucosal veins of the colonic wall rather than the mesenteric veins (12). In this case, the patient only had calcifications in the branches of the mesenteric veins, without involvement of the main trunk, which is consistent with the literature. Studies have also indicated that the extent of mesenteric venous calcification is related to the severity of the disease (6). Abdominal CT for this patient revealed diffuse thickening and edema of the entire colon and rectal walls, with visible stratification changes. Multiple calcifications were observed in the mesenteric venous routes around the ascending and transverse colon. Abdominal CTV showed increased branches of mesenteric veins around the ascending colon, transverse colon, and left small intestine, with multiple short linear calcifications seen in the mesenteric veins around the ascending and transverse colon. There were no abnormalities in the superior mesenteric vein, splenic vein, portal vein, or inferior vena cava. CT indicated multiple calcifications in the branches of the superior mesenteric vein around the ascending and transverse colon, while no significant calcifications were found in the branches of the inferior mesenteric vein. However, considering the overall edema of the colon, it is believed that the branches of the inferior mesenteric vein also had varying degrees of wall thickening and lumen narrowing, but without calcification.
The endoscopic features of IMP are characteristic and can assist in diagnosing the condition when biopsy results are inconclusive. On colonoscopy, the colonic mucosa affected by IMP displays a distinct dark purple color. Additional colonoscopic observations consist of erythema, colonic lumen narrowing, mucosal swelling, erosion, ulceration and increased rigidity of the colonic wall (26). Nonetheless, some patients may have normal colonoscopy results (28). In this case, the patient’s colonoscopy revealed that the mucosa of the entire colon and rectum was congested, edematous, and had a bluish-purple discoloration. Such cases involving the entire colon and rectum are rarer and are considered to be related to the patient’s prolonged and high-dose consumption of herbal medicines. Additionally, the patient has experienced diarrhea for many years without undergoing colonoscopic examinations or clinical treatments, leading to extensive involvement of the disease.
Due to the limited understanding of IMP, it is often challenging to distinguish it from inflammatory bowel disease and other non-neoplastic intestinal diseases in the early stages (17). Currently, there is no standard treatment regimen for IMP, with most medical centers opting for conservative management. However, for patients with recurrent symptoms who do not respond well to conservative treatment, surgical resection may be necessary (13). In some cases, postoperative pathological results confirm the diagnosis of IMP, and patients typically recover well without recurrence of IMP (13). By summarizing and analyzing the clinical and pathological features of IMP, clinicians and pathologists can improve their recognition of the disease and reduce misdiagnosis (17).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LL: Writing – original draft. R-yG: Writing – original draft. X-qY: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. X-qY is supported by Shenzhen Science and Technology Research and Development Fund, No. JSGG20210802153548040.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Guo, F, Zhou, YF, Zhang, F, Yuan, F, Yuan, YZ, and Yao, WY. Idiopathic mesenteric phlebosclerosis associated with long-term use of medical liquor: two case reports and literature review. World J Gastroenterol. (2014) 20:5561–6. doi: 10.3748/wjg.v20.i18.5561
2. Iwashita, A, Yao, T, Schlemper, RJ, Kuwano, Y, Iida, M, Matsumoto, T, et al. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. (2003) 46:209–20. doi: 10.1007/s10350-004-6526-0
3. Wen, Y, Chen, YW, Meng, AH, Zhao, M, Fang, SH, and Ma, YQ. Idiopathic mesenteric phlebosclerosis associated with long-term oral intake of geniposide. World J Gastroenterol. (2021) 27:3097–108. doi: 10.3748/wjg.v27.i22.3097
4. Wen, Y, Zhao, M, Huang, W, Fang, S, and Lin, C. Idiopathic mesenteric phlebosclerosis associated with use of Chinese herbal medicine: two case reports. Medicine (Baltimore). (2020) 99:e22813. doi: 10.1097/MD.0000000000022813
5. Wang, J, Shao, J, Lu, H, Wang, B, and Chen, J. Idiopathic mesenteric phlebosclerosis: one case report and systematic literature review of 240 cases. Am J Transl Res. (2021) 13:13156–66.
6. Ding, J, Zhang, W, Wang, L, Zhu, Z, Wang, J, and Ma, J. Idiopathic mesenteric phlebosclerosis: clinical and CT imaging characteristics. Quant Imaging Med Surg. (2021) 11:763–71. doi: 10.21037/qims-20-301
7. Kelly Wu, W, Tombazzi, CR, Howe, CF, Kendall, MA, Walton, DB, Washington, MK, et al. Idiopathic myointimal hyperplasia of the mesenteric veins: a rare imitator of inflammatory bowel disease. Am Surg. (2023) 89:1141–3. doi: 10.1177/0003134820973390
8. Sze, SF, Lam, PWY, Lam, JTW, Chung, CCC, and Lee, YT. Idiopathic mesenteric phlebosclerosis: a rare cause of chronic diarrhea. JGH Open. (2020) 4:769–70. doi: 10.1002/jgh3.12335
9. Chou, JW, Chang, CH, Wu, YH, Chang, KC, Cheng, KS, and Huang, PJ. Idiopathic mesenteric phlebosclerosis: a single-institute experience in Taiwan. Turk J Gastroenterol. (2023) 34:483–9. doi: 10.5152/tjg.2023.22335
10. Chi, J, Ji, Y, Qiao, Z, and Qian, J. Phlebosclerotic colitis: an unusual cause of abdominal pain and hematochezia. Rev Esp Enferm Dig. (2021) 113:218–9. doi: 10.17235/reed.2020.7358/2020
11. Wang, M, Wan, YX, Liao, JW, and Xiong, F. Idiopathic mesenteric phlebosclerosis missed by a radiologist at initial diagnosis: a case report. World J Clin Cases. (2024) 12:1810–6. doi: 10.12998/wjcc.v12.i10.1810
12. Sakurai, Y, Watanabe, K, Hayashi, T, Sato, K, and Sugano, I. Widespread mesenteric phlebosclerosis presenting as intestinal obstruction due to stenosis of the right-sided colon. Clin J Gastroenterol. (2022) 15:717–21. doi: 10.1007/s12328-022-01637-1
13. Liu, S, Tong, Y, Shi, R, Zeng, X, Luo, H, Yang, P, et al. Case report and literature review: laparoscopic extended right hemicolectomy for a 55-year-old patient with idiopathic mesenteric phlebosclerosis. Front Med (Lausanne). (2024) 11:1382475. doi: 10.3389/fmed.2024.1382475
14. Bowee, S, Matter, SB, Dawson, H, and Inglin, RA. Enterocolic phlebitis: a rare cause of bowel ischemia and review of the literature. Gastroenterol Rep (Oxf). (2023) 11:goad002. doi: 10.1093/gastro/goad002
15. Nishiwaki, R, Inoue, Y, Sugao, M, Sugimasa, N, Hamaguchi, T, Noji, M, et al. Hangeshashinto-associated mesenteric Phlebosclerosis and highly atypical adenoma requiring laparoscopic right hemicolectomy. Diagnostics (Basel). (2024) 14:565. doi: 10.3390/diagnostics14050565
16. Chen, S, Zhu, Y, Wu, B, and Xie, X. Idiopathic mesenteric phlebosclerotic colitis associated with Chinese herbal medicine. Rev Esp Enferm Dig. (2024) 116:170–1. doi: 10.17235/reed.2023.9641/2023
17. Deng, X, Tang, X, Yao, H, and Wang, Y. Severe venous calcifications in phlebosclerotic colitis and significantly decreased expression in betaine. Int J Surg Pathol. (2024):10668969241246475. doi: 10.1177/10668969241246475
18. Wang, X, Li, H, Xu, Z, Zhang, JY, and Huang, WF. An unusual cause of diarrhea: phlebosclerotic colitis. Am J Med Sci. (2023) 366:e3–4. doi: 10.1016/j.amjms.2023.02.008
19. Tong, T, Fu, J, and Kong, Y. Recurrent abdominal pain in a 61-year-old woman. Gastroenterology. (2023) 164:887–90. doi: 10.1053/j.gastro.2022.10.032
20. Lee, SM, and Seo, JW. Phlebosclerotic colitis: case report and literature review focused on the radiologic findings in relation to the intake period of toxic material. Jpn J Radiol. (2015) 33:663–7. doi: 10.1007/s11604-015-0467-5
21. Klein, S, Buchner, D, Chang, DH, Büttner, R, Drebber, U, and Fries, JW. Exclusive phlebosclerosis of submucosal veins leading to ischemic necrosis and perforation of the large bowel: first European case. Case Rep Gastroenterol. (2018) 12:137–42. doi: 10.1159/000488195
22. Minh, ND, Hung, ND, Huyen, PT, van Anh, NT, Lanh, NS, Anh, PQ, et al. Phlebosclerotic colitis with long-term herbal medicine use. Radiol Case Rep. (2022) 17:1696–701. doi: 10.1016/j.radcr.2022.02.069
23. Chang, YY, Lin, HH, and Lin, CC. Phlebosclerotic colitis presenting as intestinal obstruction. Clin Gastroenterol Hepatol. (2014) 12:e81–2. doi: 10.1016/j.cgh.2014.02.018
24. Fang, YL, Hsu, HC, Chou, YH, Wu, CC, and Chou, YY. Phlebosclerotic colitis: a case report and review of the literature. Exp Ther Med. (2014) 7:583–6. doi: 10.3892/etm.2014.1492
25. Shimizu, S, Kobayashi, T, Tomioka, H, Ohtsu, K, Matsui, T, and Hibi, T. Involvement of herbal medicine as a cause of mesenteric phlebosclerosis: results from a large-scale nationwide survey. J Gastroenterol. (2017) 52:308–14. doi: 10.1007/s00535-016-1218-9
26. Chen, W, Zhu, H, Chen, H, Shan, G, Xu, G, Chen, L, et al. Phlebosclerotic colitis: our clinical experience of 25 patients in China. Medicine (Baltimore). (2018) 97:e12824. doi: 10.1097/MD.0000000000012824
27. Sasaki, Y, Saito, M, Koshiba, Y, Zai, H, and Urita, Y. Idiopathic mesenteric phlebosclerosis associated with herbal drugs presenting with asymptomatic fecal occult blood. J Gen Fam Med. (2017) 18:475–6. doi: 10.1002/jgf2.122
Keywords: idiopathic mesenteric phlebosclerotic colitis, Chinese patent medicine, colonoscopy, case report, colon
Citation: Lv L, Gao R-y and Yu X-q (2025) Idiopathic mesenteric phlebosclerosis associated with use of Chinese patent medicine: a case report and literature review. Front. Med. 12:1583341. doi: 10.3389/fmed.2025.1583341
Edited by:
Andee Dzulkarnaen Zakaria, Universiti Sains Malaysia, MalaysiaReviewed by:
Monjur Ahmed, Thomas Jefferson University, United StatesKostas Tepelenis, University Hospital of Ioannina, Greece
Copyright © 2025 Lv, Gao and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi-qiu Yu, eGlxaXV5dTEyM0AxNjMuY29t
†These authors have contributed equally to this work
 Li Lv
Li Lv Ruo-yu Gao
Ruo-yu Gao Xi-qiu Yu
Xi-qiu Yu