Abstract
Introduction:
Ramadan fasting constitutes a form of intermittent fasting, and it is a religious obligation for healthy adult Muslims; however, there is a lack of comprehensive guidance for individuals diagnosed with sickle cell disease (SCD). This study seeks to identify predictors of fasting capability and investigate the effects of fasting among this patient population.
Participants and methods:
This cross-sectional study enrolled adult Muslim patients with SCD from Saudi Arabia. Data were collected through direct interviews using a structured questionnaire with four sections.
Results:
A total of 320 patients with SCD were evaluated, with a mean age of 32.6 years (SD ± 11.01) and the majority were females (63.1%). Among these participants, 214 (66.9%) observed Ramadan intermittent fasting (RIF) while 106 (33.1%) did not observe the fasting month or had interrupted fasting. Participants having secondary and university education were nearly twice as likely to fast the entire Ramadan (p = 0.025 and p = 0.003, respectively). History of SCD crises, emergency visits, acute chest syndrome, and intensive care unit admission were all significantly associated with lower odds of fasting the entire month (OR = 0.25, p = 0.019; OR = 0.25, p = 0.001; OR = 0.57, p = 0.035; and OR = 0.46, p = 0.003, respectively). Participants with more than four SCD episodes or more than four emergency room visits had significantly higher odds of experiencing complications within 30 days following Ramadan (OR = 3.31, p < 0.001 and OR = 2.55, p = 0.004, respectively).
Conclusion:
The effects of observing RIF on individuals with SCD are generally subtle during the month but more significant in the post-fasting phase. The capacity to predict an individual’s ability to fast and likelihood of post-fasting complications is substantially influenced by a range of sociodemographic factors such as education level as well as clinical variables, including frequency of annual hospitalizations, emergency room visits, intensive care unit admissions, occurrences of acute chest syndrome, and the presence of thrombocytosis. A Comprehensive evaluation of these factors will provide enhanced guidance for medical practitioners, facilitating more informed and insightful decisions regarding patient fasting recommendations.
Introduction
Sickle cell disease (SCD) is considered the most frequent genetic disease throughout the world. It is a chronic blood disorder that significantly impacts patients’ lives across clinical, economic, psychological, and psychosocial dimensions (1–4). This inherited hemoglobinopathy results from a single mutation in the β-globin gene, which leads to the production of abnormal hemoglobin S (HbS). Significant changes in the properties and morphology of red blood cells result as a consequence of HbS deoxygenation and subsequent polymerization of hemoglobin molecules (5, 6). Disease phenotype varies greatly between SCD genotypes, and is characterized by a myriad of acute and chronic events ranging from painful vaso-occlusive crises and acute chest syndrome (ACS) to chronic complications including organ failure, life-threatening infections, stroke, and a limited life expectancy (5, 7).
Each year, there are about 300,000 new cases of SCD globally. In Saudi Arabia, approximately 4.2% of the population possesses the sickle-cell trait, while 0.26% has SCD. The Eastern province exhibits the highest prevalence, with roughly 17% of the population carrying the gene and 1.2% affected by SCD (8, 9).
Muslims account for almost a quarter of the world’s population, with an estimated 2 billion Muslims (10). In Islam, Ramadan is the holy month of fasting, during which all healthy adult Muslims are obligated to fast every day from dawn to sunset, refraining from smoking, food, drink, and oral medication (11). Fasting duration varies from year to year, ranging from 10 to 21 h a day depending on geographical location and solar seasons, and the lunar month of Ramadan coincides with. However, there are several exemptions to fasting this month, including children, pregnant and breastfeeding women, during menstruation, travelers, and people with acute or chronic conditions for whom fasting would be risky. Additionally, Muslims are allowed to break their fast if they feel ill, and they can resume their fast once they have fully recovered (12–14).
Ramadan intermittent fasting (RIF) is considered a unique model of intermittent daytime fasting. In humans, the three most widely studied intermittent fasting (IF) regimens are alternate-day fasting, 5:2 IF (fasting 2 days each week), and daily time-restricted eating, such as the 16/8 approach (15). RIF is compatible with the last, as it involves fasting for 16 h per day for a complete month (29–30 days) (16). However, RIF might be more difficult than other kinds of IF, as it demands abstaining from all fluids (intermittent dry fasting), and the majority of the fasting occurs during the waking hours (11). Beyond its spiritual benefits, RIF has been shown through systematic reviews and meta-analyses to produce notable metabolic and physiological effects. These include improvements in glucose regulation, body weight and composition, and liver function. Moreover, RIF has been linked to reductions in key inflammatory and oxidative stress markers, contributing to better cardiometabolic health (17–21). Several guidelines and recommendations have been developed to improve chronic illness awareness, knowledge, and management during Ramadan, such as for diabetes mellitus, renal disease and cardiac disease (11, 12, 22, 23). Evidence regarding fasting practices among adult patients with SCD remains limited in both local and global contexts. Consequently, established protocols and directives are lacking, and clinicians are unable to provide definitive guidance concerning fasting to SCD patients. To date, only one study has specifically investigated the impact of RIF on individuals with SCD (24). However, this study was limited in scope as it did not examine the predictors that influence whether patients choose to observe RIF. Therefore, the primary objective of this study is to explore the effects of RIF on SCD patients and to identify the factors that influence an individual’s ability to fast. The findings of this research are anticipated to enhance management strategies and reduce risks associated with fasting periods for these patients.
Methodology
Study population
A cross-sectional study was conducted on SCD patients at the Blood Disease Center in Alahsa, Saudi Arabia, from October 2022 to October 2023. The included participants comprised Saudi Muslim SCD patients aged 18 to 65 years. The exclusion criteria included pregnancy for women, having the sickle cell trait, a history of chronic kidney disease, or a history of diabetes. The target sample size was calculated using the Cochrane equation for a finite population (N = 2,313) with a margin error of 5% and a confidence interval of 95%, which yielded an estimate of 330 participants. The study was approved by the Ethical Committee of King Fahad Hospital (H-05-HS-065). Participants were informed of the purpose of the study and the confidentiality of the data before giving their consent.
Data collection
Data were collected by trained research members through direct interviews with patients using a structured questionnaire with four sections. The first section covered sociodemographic data such as age, sex, marital status, education level, and history of chronic disease. The second section incorporated SCD baseline characteristics including the annual frequency of crises, annual frequency of emergency room (ER) visits, previous history of acute chest syndrome, previous history of intensive care unit (ICU) admission, previous history and frequency of blood transfusions, history of hydroxyurea administration (duration and dose), and history of surgical intervention related to SCD complications such as cholecystectomy, hip replacement surgery and splenectomy. The third section covered Ramadan-related data such as fasting status (fasting the entire month (30 days), not fasting at all, or interrupted fasting due to SCD complications) and SCD characteristics during Ramadan (hydroxyurea use, hospital admission, ICU admission, and blood transfusion). Finally, the fourth section concerned post-Ramadan data, specifically SCD characteristics within 30 days after Ramadan (SCD crises, hospital admission, ICU admission, ER visits, and blood transfusion).
Statistical analysis
Collected data were analyzed using SPSS version 27. Categorical data were presented as numbers and percentages while continuous data were summarized using the mean, median, range, and standard deviation (SD). After performing normality tests, differences in SCD characteristic distribution according to RIF pattern were assessed using the chi-square test for categorical variables and the Kruskal-Wallis test for continuous variables.
Predictors of successful fasting were analyzed using binary logistic regression. The primary outcome was defined as fasting the entire Ramadan month (1) versus not fasting the entire Ramadan month (0). Predictors of complications within 30 days after Ramadan among SCD participants who fasted the entire month were likewise analyzed by binary logistic regression, with the primary outcome being the occurrence of any SCD-related complication (SCD crisis, ER visit, hospital admission, ICU admission, or blood transfusion) within 30 days after Ramadan. The results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). A p-value <0.05 was considered statically significant.
Results
Participant characteristics
The study included 320 patients with SCD with an age range of 18 to 76 years and mean age of 32.6 years (SD 11.01). The majority were females (63.1%) and were married (52.8%). Regarding baseline SCD complications, almost all participants (91.6%) reported the occurrence of yearly SCD crises (range 1 to 50), with a median of four crises/year and mean ± SD of 6.70 ± 7.43 crises. Also, most participants (83.1%) reported annual emergency visits (range 1 to 60), with a median value of four visits/year and a mean of 7.19 ± 8.36 visits/year. Two-thirds of participants (66.6%) reported a history of ACS, and more than half (58.1%) reported a history of ICU admission. In addition, the great majority of participants (80.6%) reported a history of blood transfusion during their lives, with a wide range of 1 to 120 transfusions, an average of 9.66 ± 16.02, and a median of four. Regarding hydroxyurea use, more than a third of participants (n = 118, 36.9%) were currently taking it; however, only about half of them (50.8%, n = 60) were on the optimal dose. The average hydroxyurea dosage was 15.80 ± 4.70 mg/kg (median 14.52), with a range of 2.23–28.57 mg/kg. Notably, only 35.6% of participants reported using hydroxyurea during Ramadan. All collected demographic and health characteristic data are summarized in Table 1.
Table 1
| Characteristic | Total (n = 320) n (%) |
Fasting all Ramadan month (n = 214) n (%) |
Not fasting at all (n = 20) n (%) |
Interrupted fasting (n = 86) n (%) |
p value |
|---|---|---|---|---|---|
| Age in years (Mean±SD)& | 32.62 ± 11.01 | 32.17 ± 11.01 | 35.3 ± 13.09 | 33.18 ± 10.22 | 0.523 |
| Sex | |||||
| Male | 118 (36.9) | 78 (66.1) | 3 (2.5) | 37 (31.4) | 0.063 |
| Female | 202 (63.1) | 136 (67.3) | 17 (8.4) | 49 (24.3) | |
| Marital status | |||||
| Single | 151 (47.2) | 108 (71.5) | 10 (6.6) | 33 (21.9) | 0.160 |
| Married | 169 (52.8) | 110 (62.7) | 10 (5.9) | 53 (31.4) | |
| Education level | |||||
| Lower than secondary | 72 (22.4) | 38 (52.8) | 9 (12.5) | 25 (34.7) | 0.020* |
| Secondary | 124 (38.8) | 85 (68.5) | 5 (4.0) | 34 (27.4) | |
| University and higher | 124 (38.8) | 91 (73.4) | 6 (4.8) | 27 (21.8) | |
| Chronic diseases | |||||
| Yes | 69 (21.6) | 41 (59.4) | 8 (11.6) | 20 (29.0) | 0.086 |
| No | 251 (78.4) | 173 (68.9) | 12 (4.8) | 66 (26.3) | |
| History of SCD crises | |||||
| Yes | 293 (91.6) | 190 (64.9) | 18 (6.1) | 85 (29.0) | 0.017* |
| No | 27 (8.4) | 24 (88.9) | 2 (7.4) | 1 (3.7) | |
| Average annual SCD crises& | 6.70 ± 7.43 (n = 293) |
5.86 ± 6.28 (4) (n = 190) |
6.11 ± 3.39 (5.5) (n = 18) |
8.64 ± 9.67 (6) (n = 85) |
<0.001* |
| History of emergency visits | |||||
| Yes | 266 (83.1) | 167 (62.8) | 16 (6.0) | 83 (31.2) | 0.001* |
| No | 54 (16.9) | 47 (87.0) | 4 (7.4) | 3 (5.6) | |
| Average annual ER visits& | 7.19 ± 8.36 (n = 266) |
5.92 ± 6.69 (4) (n = 167) |
8.50 ± 8.84 (6) (n = 16) |
9.53 ± 10.54 (6) (n = 83) |
<0.001* |
| Previous history of acute chest syndrome | |||||
| Yes | 213 (66.6) | 134 (64.9) | 14 (6.6) | 65 (30.5) | 0.093 |
| No | 107 (33.4) | 80 (74.8) | 6 (5.6) | 21 (19.6) | |
| Previous history of ICU admission | |||||
| Yes | 186 (58.1) | 112 (60.2) | 15 (8.1) | 59 (31.7) | 0.010* |
| No | 134 (41.9) | 102 (76.1) | 5 (3.7) | 27 (20.1) | |
| Previous history of blood transfusion | |||||
| Yes | 258 (80.6) | 169 (65.5) | 17 (6.6) | 72 (27.9) | 0.564 |
| No | 62 (19.4) | 45 (72.6) | 3 (4.8) | 14 (22.6) | |
| Average no. blood transfusion& | 9.66 ± 16.02 (n = 258) |
8.45 ± 14.89 (3) (n = 169) |
14.18 ± 15.61 (10) (n = 17) |
11.42 ± 18.35 (3) (n = 72) |
0.076 |
| Previous history of surgery | |||||
| Yes | 203 (63.4) | 139 (68.5) | 13 (6.4) | 51 (25.1) | 0.648 |
| No | 117 (36.6) | 75 (64.1) | 7 (6.0) | 35 (29.9) | |
| Current use of hydroxyurea | |||||
| Yes | 118 (36.9) | 82 (96.5) | 9 (7.6) | 27 (22.9) | 0.393 |
| No | 202 (63.1) | 132 (65.3) | 11 (5.4) | 59 (29.2) | |
| Using of hydroxyurea during Ramadan | |||||
| Yes | 114 (35.6) | 79 (69.3) | 9 (7.9) | 26 (22.8) | 0.366 |
| No | 206 (64.4) | 135 (65.6) | 11 (5.3) | 60 (29.1) | |
| Blood parameters (Mean± SD)& | |||||
| WBC | 8.21 ± 4.38 | 7.94 ± 4.15 | 9.75 ± 4.03 | 8.50 ± 4.92 | 0.081 |
| Hemoglobin | 9.84 ± 1.43 | 9.92 ± 1.39 | 9.42 ± 1.72 | 9.72 ± 1.47 | 0.086 |
| Platelet | 298.38 ± 185.89 | 293.07 ± 169.34 | 374.50 ± 144.95 | 293.88 ± 227.32 | 0.015* |
| MCV | 78.06 ± 11.29 | 77.77 ± 11.39 | 81.64 ± 12.65 | 77.82 ± 10.58 | 0.340 |
| MCH | 27.20 ± 4.71 | 27.10 ± 4.80 | 28.85 ± 4.99 | 27.28 ± 4.36 | 0.208 |
| Hb A | 3.9713 ± 12.08 | 3.48 ± 11.67 | 8.77 ± 16.24 | 4.10 ± 11.87 | 0.197 |
| Hb A2 | 3.28 ± 1.80 | 3.20 ± 1.08 | 4.91 ± 5.87 | 3.10 ± 0.88 | 0.585 |
| Hb F | 15.98 ± 7.40 | 16.20 ± 7.44 | 14.57 ± 7.71 | 15.75 ± 7.25 | 0.720 |
| Hb S | 76.66 ± 11.51 | 76.88 ± 11.52 | 72.65 ± 13.47 | 77.03 ± 10.95 | 0.498 |
Demographic and health characteristics of the participants according to Ramadan fasting pattern.
&Test of Significance performed is the Kruskal Wallis (K-W) test.
WBC, white blood cells; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; Hb A, hemoglobin A; Hb A2, hemoglobin A2; Hb F, hemoglobin F; and Hb S, hemoglobin S. *p < 0.05 (significant).
Ramadan fasting pattern
Participants were classified into three groups based on RIF pattern: fasting every day (n = 214, 66.9%), not fasting at all (n = 20, 6.3%), or interrupted fasting (n = 86, 26.9%). On average, participants in the interrupted group broke fasting on 7.06 ± 6.50 days, with a median of 5 days (range 1–29 days) (Table 1). Interruptions were due to SCD complications, of which 32.6% (n = 28) required hospitalization, primarily for a painful SCD crisis, followed by blood transfusion (Figure 1). The remaining 67.4% (n = 58) of participants in the interrupted group experienced complications that did not require hospitalization; of these, 55.2% broke their fast based on personal preference, while only 10.3% did so following physician recommendation.
Figure 1

Reasons for hospital admission during Ramadan among SCD patients with interrupted fasting (n = 28).
Comparative statistical tests revealed significant differences in RIF pattern in relation to participant level of education, history of SCD crises, history of ER visits, and history of ICU admission. Among participants with university-level education, those who did not report any SCD crises, and those who reported no ER visits, a higher proportion successfully fasted the entire month (p = 0.020, p = 0.017, and p = 0.001, respectively). Conversely, participants with interrupted fasting had significantly more SCD crises, a higher mean number of ER visits, and higher ICU admissions (p < 0.001, p < 0.001, and p = 0.010, respectively). Meanwhile, there was no statistically significant difference between the three groups in terms of mean age, sex distribution, marital status, chronic diseases, ACS history, blood transfusion history, or use of hydroxyurea (either current or during Ramadan). In addition, blood parameters did not exhibit statistically significant differences in relation to fasting pattern, except for the mean platelet count, where higher platelet count was observed among non-fasting SCD patients (p = 0.015) (Table 1).
Table 2 presents the binary logistic regression results for predictors of fasting the entire month of Ramadan (Table 2). Participants having completed secondary education were nearly twice as likely to fast the entire month, and those with a university education 2.538 times more likely, both of which findings are statistically significant (p = 0.025 and p = 0.003, respectively).
Table 2
| Variables | p value | Odds ratio | 95% CI |
|---|---|---|---|
| Age | 0.281 | 0.99 | 0.97–1.01 |
| Sex (Ref: Female) | 0.822 | 0.95 | 0.58–1.53 |
| Marital (Ref: Single) | 0.173 | 0.72 | 0.42–1.07 |
| Education (Ref: Lower than secondary) | |||
| Secondary | 0.025 | 1.99 | 1.07–3.55 |
| University | 0.003 | 2.54 | 1.34–4.54 |
| Chronic diseases | 0.070 | 0.60 | 0.38–1.14 |
| History of SCD Crises | 0.019 | 0.25 | 0.07–0.75 |
| No. of SCD episodes (n = 293) | 0.017 | 0.96 | 0.93–0.99 |
| Number of SCD episodes (n = 293) Ref. median or less ≤ 4 | 0.001 | 0.45 | 0.28–0.74 |
| History of emergency visits | 0.001 | 0.25 | 0.11–0.58 |
| No. ER visits (n = 266) | 0.003 | 0.95 | 0.92–0.98 |
| Number of ER visits (n = 266) Ref. median or less ≤ 4 |
0.002 | 0.45 | 0.27–0.75 |
| Previous history of acute chest syndrome | 0.035 | 0.57 | 0.34–0.96 |
| Previous history of ICU Admission | 0.003 | 0.46 | 0.29–0.78 |
| Previous history of blood transfusion | 0.289 | 0.72 | 0.39–1.33 |
| Average no. blood transfusion (n = 258) | 0.105 | 0.99 | 0.97–1.00 |
| Previous history of surgery | 0.443 | 1.21 | 0.75–1.96 |
| Current use of hydroxyurea | 0.576 | 1.15 | 0.74–1.97 |
| Optimal dose of hydroxyurea (n = 118) | 0.781 | 0.89 | 0.41–1.96 |
| The use of hydroxyurea during Ramadan | 0.619 | 1.13 | 0.73–1.94 |
| WBC | 0.154 | 0.10 | 0.91–1.01 |
| Hemoglobin | 0.271 | 1.69 | 0.95–1.34 |
| Platelets | 0.678 | 1.00 | 0.10–1.00 |
| HBA | 0.269 | 0.99 | 0.98–1.01 |
| HBA2 | 0.262 | 0.92 | 0.81–1.07 |
| HBF | 0.605 | 1.01 | 0.98–1.04 |
| HBS | 0.450 | 1.01 | 0.98–1.02 |
Predictors of fasting capability among participants with SCD.
On the other hand, history of SCD crises, emergency visits, acute chest syndrome, and ICU admission were all significantly associated with lower odds of fasting the entire Ramadan (OR = 0.25, p = 0.019; OR = 0.25, p = 0.001; OR = 0.57, p = 0.035; and OR = 0.46, p = 0.003, respectively). For each new SCD crisis or ER visit, the odds of fasting the entire month decreased by approximately 4.0 and 5.0%, respectively, (OR = 0.96, p = 0.017 and OR = 0.95, p = 0.003), and having more than four of either was significantly associated with lower likelihood of month-long fasting (OR = 0.45, p = 0.001; OR = 0.45, p = 0.002, respectively). In addition, older age, male sex, having a blood transfusion history, and having a chronic disease all trended with lower likelihood of month-long fasting; however, none of these parameters achieved significance (p > 0.05). No hematological parameters were found to significantly predict fasting the entire Ramadan (p > 0.05).
Impact on health within 30 days after Ramadan
Among patients who fasted for the whole month of Ramadan (n = 214), around half (41.1%, n = 88) reported experiencing at least one SCD complication within 30 days following the fast. SCD crises accounted for 39.7% of all reported complications, with ER visits coming in second at 25% (Figure 2).
Figure 2
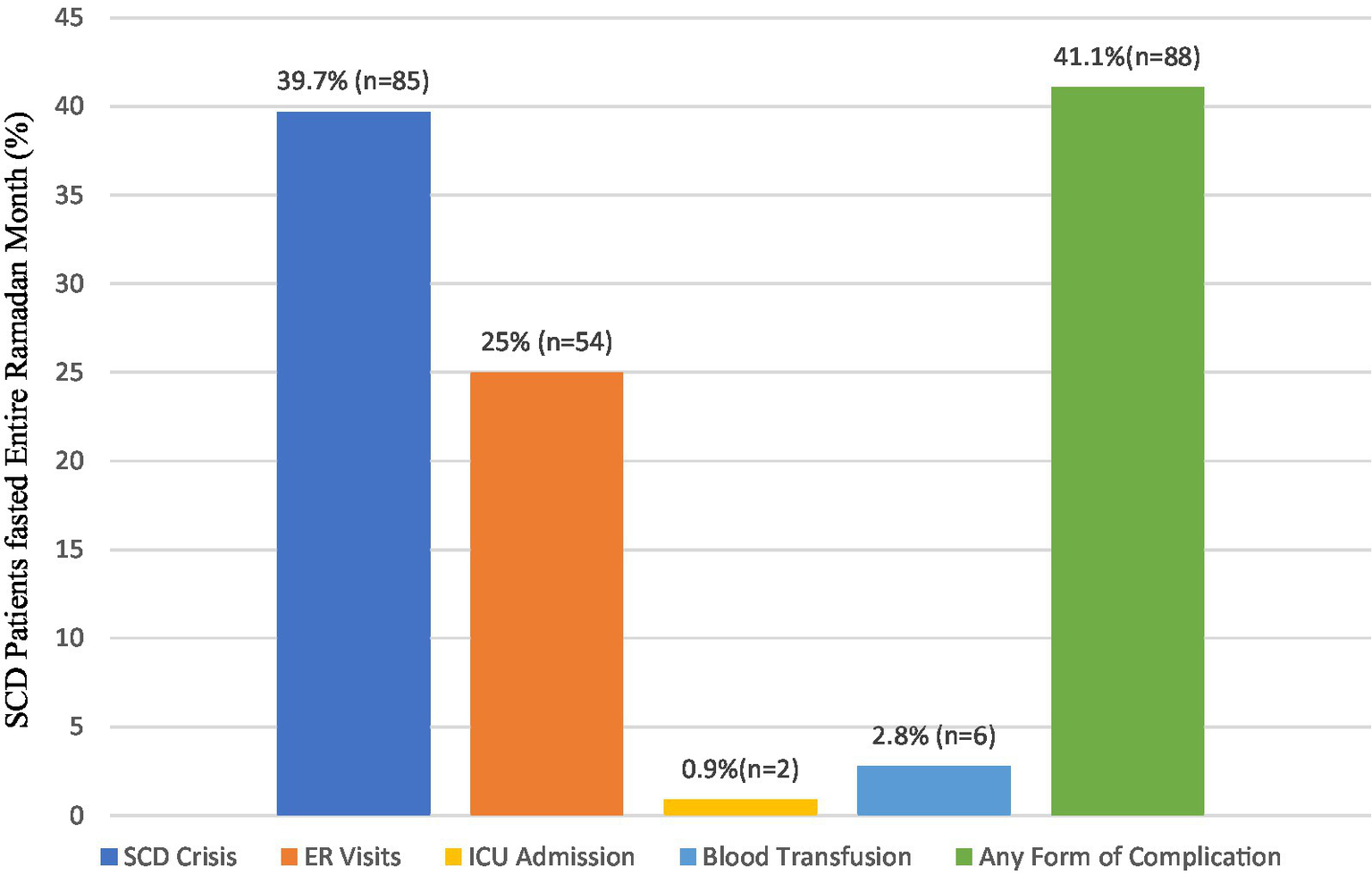
SCD complications within 30 days after Ramadan among SCD patients fasted entire Ramadan month (n = 214).
Table 3 presents the regression results concerning predictors of post-Ramadan complications among participants who complete the entire Ramadan fasting (n = 214). Participants having secondary and university education exhibited significantly lower likelihood of developing complications (OR = 0.36, p = 0.011 and OR = 0.41, p = 0.023). Meanwhile, the frequency of SCD crises was a statistically significant predictor of complications (OR = 1.14, p < 0.001), with each new crisis increasing the likelihood of complications by approximately 13.6%. Furthermore, participants with more than four SCD episodes had significantly higher odds of complications than those with four or fewer episodes (OR = 3.31, p < 0.001). Similarly, participants with a history of emergency visits had more than three times the odds of experiencing complications within 30 days following Ramadan (OR = 3.24, p = 0.002), and number of ER visits was a statistically significant predictor, with each additional visit increasing the odds of complications by approximately 8.9% (p = 0.005) and participants with more than four ER visits showing significantly higher odds of complications than those with four or fewer visits (OR = 2.55, p = 0.004). None of the examined hematological parameters, nor the remaining demographic and health characteristics, significantly predicted the occurrence of post-Ramadan complications (p > 0.05).
Table 3
| Variables | p value | Odds ratio | 95% CI |
|---|---|---|---|
| Age | 0.578 | 1.007 | 0.98–1.03 |
| Sex (Female) | 0.399 | 1.275 | 0.72–2.40 |
| Marital (Single) | 0.870 | 0.956 | 0.55–1.65 |
| Education (Lower than secondary) | 0.011 | 0.356 | 0.16–0.78 |
| Secondary university | 0.023 | 0.408 | 0.19–0.88 |
| Chronic diseases | 0.451 | 1.302 | 0.66–2.58 |
| Number of SCD episodes (n = 190) | <0.001 | 1.136 | 1.06–1.21 |
| Number of SCD episodes (n = 190) Ref. median or less ≤ 4 | <0.001 | 3.312 | 1.81–6.05 |
| History of emergency visits | 0.002 | 3.243 | 1.51–6.95 |
| Number of ER Visits (n = 167) | 0.005 | 1.089 | 1.03–1.05 |
| Number of ER Visits (n = 167) Ref. median or less ≤ 4 | 0.004 | 2.547 | 1.35–4.78 |
| Previous history of acute chest syndrome | 0.406 | 1.272 | 0.72–2.24 |
| Previous history of ICU admission | 0.413 | 1.256 | 0.73–2.17 |
| Previous history of blood transfusion | 0.394 | 1.345 | 0.68–2.66 |
| Previous history of surgery | 0.160 | 1.517 | 0.85–2.71 |
| Current use of hydroxyurea | 0.349 | 1.306 | 0.75–2.28 |
| Optimal dose of hydroxyurea (n = 82) | 0.502 | 1.345 | 0.56–3.22 |
| The use of hydroxyurea during Ramadan | 0.469 | 1.231 | 0.70–2.16 |
| WBC | 0.762 | 1.010 | 0.95–1.08 |
| Hemoglobin | 0.124 | 0.855 | 0.70–1.04 |
| Platelets | 0.790 | 1.000 | 0.10–1.00 |
| HBA | 0.589 | 0.993 | 0.97–1.02 |
| HBA2 | 0.362 | 1.123 | 0.87–1.44 |
| HBF | 0.273 | 0.979 | 0.94–1.02 |
| HBS | 0.463 | 1.009 | 0.98–1.03 |
Predictors of complications within 30 days after Ramadan among participants with SCD who fasted the entire Ramadan month (n = 214).
Discussion
All Muslims globally practice a form of diurnal IF during the month of Ramadan (14). Deciding not to fast during Ramadan or to break your fast mid-day is a serious matter in Islam and should be approached with knowledge, and often consultation. In the current study, majority of the interrupted-fasting group broke their fast based on personal decision, while only a few were medically advised not to complete fasting. These findings highlight a critical need to establish guidelines to assist medical practitioners in providing appropriate fasting recommendations for SCD patients. Furthermore, because many people will fast despite their doctors’ advices, health care professionals and religious/community leaders must collaborate to address these contemporary medical concerns (12).
Despite the fact that inadequate fluid and nutrition intake can trigger SCD symptoms flare-ups, a study from Qatar found that RIF did not impact the frequency of vaso-occlusive or hemolytic crises in these patients (16, 24, 25). Similarly, a case series of four patients practicing different types of IF including complete abstinence from food and/or water, reported no definitive impact on vaso-occlusive pain episodes (aside from one patient who discontinued fasting due to symptom worsening) (26). In line with these findings, not all participants in our study completed the entire month of fasting (averaging 14 h per day). However, our results revealed that RIF had a negative impact on the clinical course of SCD within 30 days following Ramadan. These discrepancies in results regarding the influence of fasting on SCD course might be attributed to various variables, such as the type of fasting used in each study and the variations in participants’ lifestyles. Key lifestyle factors, including hydration, diet, physical activity, rest, and managing stress which can all play significant roles in minimizing symptoms and preventing complications.
SCD presents significant variability among patients, with outcomes ranging from mortality in childhood to the potential for a relatively symptom-free life extending into the eighth decade. The interplay of genetic, environmental, and socioeconomic factors is critical in influencing patient outcomes; however, the precise effects of these variables can be difficult to predict (27, 28). Although there is no correlation between SCD incidence and sex, there have been reports of variations in SCD outcomes among adult patients based on biological sex. Male sex is linked to poorer outcomes in the majority of indicators, such as blood transfusions, hospital admissions, and cerebrovascular complications (29). Furthermore, a recent systematic review by Roky et al. highlighted notable differences in diseases frequency and incidence between both sexes during Ramadan (30). The sex-based difference may account for the female ability to fast for an entire month in the current study. In addition, it might be linked to the fact that women are exempt from fasting during their menstruation, which can last up to 7 days and is equivalent to the average number of interruptions. Moreover, our findings indicate that education level significantly influences safe and effective fasting, and potentially reducing complications. Higher levels of education, particularly secondary school qualifications and above, were more likely to fast the entire month without interruption and to have no post-fasting complications. This result aligns with Shdaifat et al. study, which found that higher education levels are associated with lower management costs for SCD, emphasizing the importance of education in reducing the disease’s overall burden (31). This link is expected, as higher education typically enhances self-management skills, treatment adherence, and symptom control.
Since there is no national or international registry to define or classify the severity of SCD, and lab-based genotyping and phenotyping alone do not reflect clinical severity, assessing the number of complications is essential for evaluating patient risk before fasting and predicting outcomes (32). The current study found that patients with a history of hospitalization or emergency department visits related to SCD crises, particularly those with more than four annual emergency department visits or hospitalization, exhibited higher propensity for interrupted fasting and higher risk of complications within the 30 days following fasting. Individuals with a past incidence of ICU admissions or acute chest syndrome likewise demonstrated decreased likelihood of fasting for the entire month, although the associated risks for post-fasting complications in these groups appear to be negligible.
It is also noteworthy that while hydroxyurea and blood transfusions are well-established therapeutic interventions for SCD patients (28, 33), neither administration of optimal hydroxyurea dose nor history of previous transfusions showed significant correlation with ability to maintain fasting among our patients. This might be because the majority of our patients either not using hydroxyurea or were taking suboptimal doses, preventing optimal treatment benefits.
With regard to hematological parameters, fetal hemoglobin and leukocytosis have been recognized as good indicators of SCD severity and outcomes, but have limited ability in predicting fasting capability (34, 35). A recent study by Ahmed et al. in Qatar demonstrated that fasting results in temporary decreases in platelet and reticulocyte counts, as well as a reversible decline in kidney function during the fasting period. Nevertheless, that study did not succeed in identifying individuals who may be at increased risk for negative outcomes (24). In the current study, only elevated platelet count exhibited close correlation with fasting interruption. This might reflect the baseline thromboinflammatory process in these patients, as thrombocytosis is considered an inflammatory marker with a significant role in some major SCD complications (6, 36).
The results of this study contribute significantly to the literature and highlight that despite the important beneficial impacts of RIF on human health in general, a comprehensive guide is crucial for patients with SCD. Not everyone with SCD should be advised to fast, and decisions should be based on risk categories. The constellation of contributing factors identified in this work could be translated into a scoring system and used to identify a high-risk group and provide proper guidance to the Muslim community suffering from SCD. Furthermore, as fetal hemoglobin level did not show evident impact on fasting success, the findings could be extended to other communities where Arab Indian haplotypes are uncommon (37).
Based on existing literature, this is the first study worldwide to explore the factors influencing RIF among patients with SCD, and the first to assess the health effects of RIF specifically in Saudi SCD patients. Despite that, it has some limitations that should be considered. First, this is a cross-sectional study that can identify associations but cannot prove causality. In addition, participants were from a single center in Saudi Arabia and did not include non-Saudi Muslim patients which may restrict the results’ generalizability. Furthermore, there is the lack of comparison between laboratory markers during and after fasting. Fundamentally, fasting duration is changeable from one country to another and might be affected by seasonal variations, which could also influence guidance. Importantly, the findings of our study apply to adult patients with SCD above the age of 18, while fasting may be undertaken at ages as early as 14 years old. Future studies remain needed for more detailed elucidation of variables and the determination of precise recommendations, as is collaboration between Muslim and non-Muslim countries where SCD is endemic and fasting is a common practice.
In summary, the Ramadan fast serves as a variant of IF that is adopted by adult Muslims globally. The physiological effects of fasting on individuals with SCD are initially subtle but become markedly evident during the post-fasting phase. The ability to predict fasting tolerance and potential complications in the post-fasting period is significantly influenced by a range of sociodemographic factors such as education level as well as clinical variables, including frequency of hospitalizations, emergency department visits, intensive care unit admissions, occurrences of acute chest syndrome, and presence of thrombocytosis. Careful consideration of this clinical profile will enable healthcare providers to offer more informed guidance and optimize fasting decisions for patients.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by King Fahad Hospital’s Ethical Committee (H-05-HS-065). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
MHA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MMA: Writing – original draft, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. JA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZSA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KAA: Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources. HB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KBA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia [Grant No.KFU 251839].
Acknowledgments
We would like to thank all participants for their collaboration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Piel FB Patil AP Howes RE Nyangiri OA Gething PW Dewi M et al . Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet. (2013) 381:142–51. doi: 10.1016/S0140-6736(12)61229-X
2.
Modell B Darlison M . Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. (2008) 2008:480–7. doi: 10.2471/BLT.06.036673
3.
Holdford D Vendetti N Sop DM Johnson S Smith WR . Indirect economic burden of sickle cell disease. Value Health. (2021) 24:1095–101. doi: 10.1016/j.jval.2021.02.014
4.
Essien EA Winter-Eteng BF Onukogu CU Nkangha DD Daniel FM . Psychosocial challenges of persons with sickle cell anemia: A narrative review. Medicine (Baltimore). (2023) 102:e36147. doi: 10.1097/MD.0000000000036147
5.
Tebbi CK . Sickle cell disease, a review. Hemato. (2022) 3:341–66. doi: 10.3390/hemato3020024
6.
Conran N De Paula EV . Thromboinflammatory mechanisms in sickle cell disease - challenging the hemostatic balance. Haematologica. (2020) 105:2380–90. doi: 10.3324/haematol.2019.239343
7.
Brousse V Bernaudin F Melaine A Goguillot M Gallagher M Benard S et al . Severity and burden of sickle cell disease in France: a nationwide real-world study. Haematologica. (2023) 108:2476–86. doi: 10.3324/haematol.2022.282098
8.
Jastaniah W . Epidemiology of sickle cell disease in Saudi Arabia. Ann Saudi Med. (2011) 31:289–93. doi: 10.5144/0256-4947.2011.289
9.
Alsalman M Alkhalifa H Alkhalifa A Alsubie M AlMurayhil N Althafar A et al . Hydroxyurea usage awareness among patients with sickle-cell disease in Saudi Arabia. Health Sci Rep. (2021) 4:e437. doi: 10.1002/hsr2.437
10.
World Population Review . (2025). Muslim majority countries 2025. Available online at: https://worldpopulationreview.com/country-rankings/muslim-majority-countries (Accessed January 15, 2025).
11.
Al-Arouj M Assaad-Khalil S Buse J Fahdil I Fahmy M Hafez S et al . Recommendations for management of diabetes during Ramadan: update 2010. Diabetes Care. (2010) 33:1895–902. doi: 10.2337/dc10-0896
12.
Akhtar AM Ghouri N Chahal CAA Patel R Ricci F Sattar N et al . Ramadan fasting: recommendations for patients with cardiovascular disease. Heart. (2022) 108:258–65. doi: 10.1136/heartjnl-2021-319273
13.
Emara MH Soliman HH Elnadry M Mohamed Said E Abd-Elsalam S Elbatae HE et al . The “Egyptian Ramadan fasting, liver diseases interest group”; “Egyptian Ramadan fasting, liver diseases interest group”. Ramadan fasting and liver diseases: A review with practice advices and recommendations. Liver Int. (2021) 41:436–48. doi: 10.1111/liv.14775
14.
Patterson RE Sears DD . Metabolic effects of intermittent fasting. Annu Rev Nutr. (2017) 37:371–93. doi: 10.1146/annurev-nutr-071816-064634
15.
de Cabo R Mattson MP . Effects of intermittent fasting on health, aging, and disease. N Engl J Med. (2019) 381:2541–51. doi: 10.1056/NEJMra1905136
16.
Purnell MC Rayborn M . Novel hydration and nutritional strategies for sickle cell disease. EJHaem. (2020) 1:230–4. doi: 10.1002/jha2.9
17.
Jahrami HA Faris ME Janahi IA Janahi IM Abdelrahim DN Madkour MI et al . Does four-week consecutive, dawn-to-sunset intermittent fasting during Ramadan affect cardiometabolic risk factors in healthy adults? A systematic review, meta-analysis, and meta-regression. Nutr Metab Cardiovasc Dis. (2021) 31:2273–301. doi: 10.1016/j.numecd.2021.05.002
18.
Jahrami HA Alsibai J Clark CCT Faris MAE . A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. (2020) 59:2291–316. doi: 10.1007/s00394-020-02216-1
19.
Faris MA Jahrami H BaHammam A Kalaji Z Madkour M Hassanein M . A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res Clin Pract. (2020) 165:108226. doi: 10.1016/j.diabres.2020.108226
20.
Faris M Jahrami H Abdelrahim D Bragazzi N BaHammam A . The effects of Ramadan intermittent fasting on liver function in healthy adults: A systematic review, meta-analysis, and meta-regression. Diabetes Res Clin Pract. (2021) 178:108951. doi: 10.1016/j.diabres.2021.108951
21.
Madkour MI El-Serafi A T Jahrami HA Sherif NM Hassan RE Awadallah S et al . Ramadan diurnal intermittent fasting modulates SOD2, TFAM, Nrf2, and sirtuins (SIRT1, SIRT3) gene expressions in subjects with overweight and obesity. Diabetes Res Clin Pract. (2019) 155:107801. doi: 10.1016/j.diabres.2019.107801
22.
Hassanein M Afandi B Yakoob Ahmedani M Mohammad Alamoudi R Alawadi F Bajaj HS et al . Diabetes and Ramadan: practical guidelines 2021. Diabetes Res Clin Pract. (2022) 185:109185. doi: 10.1016/j.diabres.2021.109185
23.
Boobes Y Afandi B AlKindi F Tarakji A al Ghamdi SM Alrukhaimi M et al . Consensus recommendations on fasting during Ramadan for patients with kidney disease: review of available evidence and a call for action (RaK initiative). BMC Nephrol. (2024) 25:84. doi: 10.1186/s12882-024-03516-y
24.
Ahmed K Abdu Y Khasawneh S Shukri A Adam E Mustafa S et al . The effect of intermittent fasting on the clinical and hematological parameters of patients with sickle cell disease: A preliminary study. Front Med. (2023) 10:1097466. doi: 10.3389/fmed.2023.1097466
25.
Brugnara C . Sickle cell dehydration: pathophysiology and therapeutic applications. Clin Hemorheol Microcirc. (2018) 68:187–204. doi: 10.3233/CH-189007
26.
Syed R Rizvi I Hussain F Farooqui M . Intermittent fasting in sickle cell disease: case series and review of literature. J Sick Cell Dis. (2024) 1:41. doi: 10.1093/jscdis/yoae002.041
27.
Rees DC Brousse VAM Brewin JN . Determinants of severity in sickle cell disease. Blood Rev. (2022) 56:100983. doi: 10.1016/j.blre.2022.100983
28.
Alsalman M Alsalman Z Alkhalifa HA Alfaraj AN Alkhalifah A Almulihi Q . Predictors of intensive care admission among adult patients with sickle cell disease in Eastern Province of Saudi Arabia. J Blood Med. (2023) 14:671–80. doi: 10.2147/JBM.S435861
29.
Di Mauro M El Hoss S Nardo-Marino A et al . Males with sickle cell disease have higher risks of cerebrovascular disease, increased inflammation, and a reduced response to hydroxyurea. Am J Hematol. (2023) 98:E341–4. doi: 10.1002/ajh.27074
30.
Roky R Aadil N Krami AM Benaji B Errabih I Abdelrahim DN et al . Sex as a biological factor in the changes in disease patients during Ramadan intermittent fasting: A systematic review. Front Nutr. (2022) 9:908674. doi: 10.3389/fnut.2022.908674
31.
Shdaifat E Abu-Sneineh F Alsaleh N Ibrahim A . Economic burden of sickle cell disease in Saudi Arabia. Value Health Reg Issues. (2025) 45:101038. doi: 10.1016/j.vhri.2024.101038
32.
Shah N Beenhouwer D Broder MS Bronte-Hall L de Castro LM Gibbs SN et al . Development of a severity classification system for sickle cell disease. Clinicoecon Outcomes Res. (2020) 12:625–33. doi: 10.2147/CEOR.S276121
33.
Ward J Lewis N Tsitsikas DA . Improving routine outpatient monitoring for patients with sickle-cell disease on hydroxyurea. BMJ Open Qual. (2018) 7:e000218. doi: 10.1136/bmjoq-2017-000218
34.
Steinberg MH Chui DH Dover GJ Sebastiani P Alsultan A . Fetal hemoglobin in sickle cell anemia: a glass half full?Blood. (2014) 123:481–5. doi: 10.1182/blood-2013-09-528067
35.
Alsalman M . Laboratory predictors of sickle cell disease severity: a cross-sectional study. J Med Life. (2024) 17:63–6. doi: 10.25122/jml-2023-0397
36.
Pillai K Premarajan S Parvathy V . Platelet indices as an acute phase reactant. J Pediatr Crit Care. (2019) 6:15. doi: 10.21304/2019.0602.00483
37.
Habara AH Shaikho EM Steinberg MH . Fetal hemoglobin in sickle cell anemia: the Arab-Indian haplotype and new therapeutic agents. Am J Hematol. (2017) 92:1233–42. doi: 10.1002/ajh.24872
Summary
Keywords
sickle cell disease, intermittent fasting, vaso-occlusive crisis, Ramadan, fasting recommendations
Citation
Alsalman MH, Alsalman Z, Alshams MM, Aljasem JM, Alsindi ZS, Almutairi AA, Alsunaikh KA, Buali HH, Algadeeb KB, Mohammed NEO, Bushehab AA and Shafey MM (2025) Predictors and health impacts of Ramadan intermittent fasting among patients with sickle cell disease. Front. Med. 12:1584795. doi: 10.3389/fmed.2025.1584795
Received
27 February 2025
Accepted
08 May 2025
Published
29 May 2025
Volume
12 - 2025
Edited by
Hassane Zouhal, University of Rennes 2 – Upper Brittany, France
Reviewed by
MoezAlIslam Ezzat Faris, Applied Science Private University, Jordan
Sio Mui Chong, The First Affiliated Hospital of Jinan University, China
Updates
Copyright
© 2025 Alsalman, Alsalman, Alshams, Aljasem, Alsindi, Almutairi, Alsunaikh, Buali, Algadeeb, Mohammed, Bushehab and Shafey.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zaenb Alsalman, Alsalman.zainab@hotmail.com; zalsalman@kfu.edu.sa
†ORCID: Zaenb Alsalman, https://orcid.org/0000-0002-1008-7977
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.