Abstract
Background:
Elevated blood pressure (BP) in acute ischemic stroke (AIS) significantly impacts clinical outcomes, yet optimal BP management remains contentious due to patient heterogeneity. Traditional Chinese medicine (TCM) constitution theory categorizes individuals into distinct physiological patterns, offering a novel framework to address this variability. This study integrates TCM constitutional theory into modern AIS care to propose a personalized BP management hypothesis.
Methods:
A systematic review and meta-analysis were conducted across nine databases, including PubMed, Web of Science, Scopus, the Cochrane Library, ScienceDirect, the Chinese National Knowledge Infrastructure, Wanfang Data, VIP Database, and China Biology Medicine, covering publications up to January 2025. We analyzed TCM constitution distributions in AIS, hypertension, hypotension, AIS with hypertension, ischemic stroke (IS) with hypertension, and ischemic cerebrovascular disease with hypoperfusion, correlating constitutional types with clinical outcomes. We employed the Agency for Healthcare Research and Quality (AHRQ) checklist to evaluate the methodological quality of cross-sectional studies and utilized the Newcastle-Ottawa Scale (NOS) for quality assessment of cohort and case–control studies. Subgroup and sensitivity analyses were performed, and publication bias was assessed. A constitution-guided framework for BP management was developed through evidence synthesis.
Results:
Fifty-four studies were included in the study, with the majority being of moderate-to-high quality. The findings demonstrated that Phlegm-dampness, Qi-deficiency, Yin-deficiency, and Blood-stasis constitutions predominated in AIS patients with hypertension. Subgroup and sensitivity analyses confirmed the robustness of the results. Most analyses demonstrated no evidence of publication bias. Although several analyses indicated potential publication bias, the primary conclusions withstood the trim-and-fill adjustment and remained robust. A TCM constitution-based BP management hypothesis was proposed: patients with Phlegm-dampness or Blood-stasis constitutions may benefit from intensive BP control, whereas Qi-deficiency and Yin-deficiency types may require conservative strategies to mitigate hypoperfusion risks.
Conclusion:
This integration of TCM constitutional theory into AIS BP management provides a potential framework for advancing precision care to improve clinical outcomes in AIS patients. Further validation in multicenter cohorts and mechanistic exploration is warranted to enhance clinical applicability (Registration information: https://www.crd.york.ac.uk/PROSPERO2/view/CRD420250655689).
1 Introduction
Acute ischemic stroke (AIS) remains a leading cause of global morbidity and mortality (1, 2). Elevated blood pressure (BP) at onset, observed in approximately 75% of AIS patients (3), is strongly linked to adverse outcomes such as hemorrhagic transformation, cerebral edema, and long-term disability (4, 5). Current guidelines emphasize cautious BP management during the acute phase of AIS to balance cerebral perfusion and secondary injury risks (6–8). However, optimal BP targets remain contentious, as evidenced by conflicting results from landmark trials (e.g., ENCHANTED, OPTIMAL-BP) comparing intensive versus standard strategies (9–12). This ambiguity stems from marked patient heterogeneity in cerebral autoregulation, comorbid conditions, and therapeutic response, factors that remain inadequately addressed by conventional demographic or clinical stratification methods.
Traditional Chinese Medicine (TCM) constitution theory offers a novel framework to address this heterogeneity. Rooted in millennia of clinical observation, TCM constitution classification identifies distinct physiological and pathological patterns (nine TCM constitutions) that influence disease susceptibility and treatment efficacy (13). This study pioneers the integration of TCM constitution theory into modern BP management of AIS. By leveraging meta-analysis as an analytical tool, we systematically evaluate the distribution of TCM constitution types across AIS patients, hypertensive/hypotensive populations, and ischemic cerebrovascular cohorts with BP abnormalities. Through an extensive literature review and a step-by-step logical analysis, this investigation not only elucidates constitution-specific pathophysiological mechanisms underlying AIS with hypertension but also proposes a potential framework for personalized therapeutic strategies.
2 Methods
This meta-analysis was registered on the Prospective Register of Systematic Reviews (PROSPERO) under the code CRD420250655689 and conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.1 Deductive framework and analytical rationale
To systematically elucidate the constitutional characteristics of AIS patients with hypertension and establish targeted BP management strategies, we developed a stepwise analytical framework grounded in evidence synthesis (Figure 1). First, we characterized TCM constitution distributions in foundational populations (AIS and hypertensive cohorts) to identify baseline traits linked to cerebrovascular pathology. Due to limited direct evidence in AIS with hypertensive population, we expanded analyses to broader ischemic stroke (IS) with hypertensive population. To address the risks of hypotension/hypoperfusion from aggressive BP lowering, we further examined TCM constitution patterns in hypotensive and ischemic cerebrovascular disease with hypoperfusion cohorts, identifying vulnerability traits. By synthesizing these findings and relevant research, we mapped the constitutional profiles in AIS with hypertensive patients and correlated them with clinical outcomes such as recurrence and hypoperfusion risks. This integrative approach enabled us to make targeted hypotheses: considering which TCM constitutions are, respectively, suitable for intensive BP control and conservative strategies.
Figure 1

A TCM constitutions-guided framework for personalized BP management in AIS with hypertension.
2.2 Eligibility criteria
Studies were eligible for inclusion if they met the following criteria: (1) studies using the standardized TCM Constitution Classification and Determination criteria published by the China Association of Chinese Medicine (CACM) (14); (2) cohort studies, case–control studies, or cross-sectional studies; (3) studies providing sufficient data for calculating TCM constitution distribution in patients with AIS, hypertension, hypotension, AIS with hypertension, IS with hypertension, or ischemic cerebrovascular disease with hypoperfusion. Exclusion criteria were: (1) studies involving populations with other comorbidities; (2) studies analyzing only a single constitution type; (3) duplicate publications or secondary analyses of the same population; (4) reviews, commentaries, case reports, or animal studies; (5) studies with incomplete data reporting or inaccessible full texts.
2.3 Outcome measure
The outcome measure was the distribution of TCM constitution types in patients with AIS, hypertension, hypotension, AIS with hypertension, IS with hypertension, or ischemic cerebrovascular disease with hypoperfusion. To quantify this outcome, prevalence was used to describe the proportion of each constitution type within the study population, while odds ratios (ORs) were employed to compare the occurrence of specific constitution types between different patient groups. TCM constitution types were classified using the validated TCM Constitution Classification and Determination Criteria (ZYYXH/T157-2009) published by the CACM (14). (Supplementary material 1). This standardized tool defines nine constitution types: Balanced constitution (Type A) and eight unbalanced constitution types (Type B-I), including Qi-deficiency (Type B), Yang-deficiency (Type C), Yin-deficiency (Type D), Phlegm-dampness (Type E), Dampness-heat (Type F), Blood-stasis (Type G), Qi-stagnation (Type H), and Special Diathesis (Type I). Each participant completed the TCM Constitution Classification and Determination Questionnaire (Supplementary material 1), which consists of Likert-scale questions (5-point scoring) corresponding to the nine constitution domains. Raw scores were calculated by summing item responses for each constitution type. Conversion scores were derived using the formula:
A Balanced constitution was defined as having a conversion score of ≥60, with all eight unbalanced constitution types simultaneously scoring <30, while unbalanced constitutions were categorized into three levels: “yes” for conversion scores ≥40, “tendency” for scores ranging from 30 to 39, and “no” for scores <30. The detailed questionnaire items and criteria for constitution classification are presented in Supplementary material 1.
2.4 Retrieval methods and screening process
A comprehensive search was conducted across nine electronic databases, including China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP Database, China Biology Medicine (CBM), PubMed, Web of Science, Scopus, the Cochrane Library, and ScienceDirect. The search encompassed articles published in both Chinese and English languages up to January 2025. The included research types comprised cross-sectional study, case–control study, and cohort study. The search strategy employed a combination of Medical Subject Headings (MeSH) terms and free-text keywords, including but not limited to “acute ischemic stroke,” “acute cerebral infarction,” “constitution,” “ischemic stroke,” “cerebral infarction,” “hypertension,” “low blood pressure,” “hypoperfusion,” “traditional Chinese medicine,” “cohort study,” “case–control study,” and “cross-sectional study,” along with their respective Chinese equivalents. Complete search syntax exemplifying the PubMed strategy is detailed in Supplementary Tables 1–6 (Supplementary material 2), with database-specific adaptations implemented accordingly. The reference management process was implemented using EndNote 20 software. Two investigators independently performed a two-stage screening procedure involving sequential evaluation of titles, abstracts, and full-text documents. All stages of the literature search and selection process were subjected to reciprocal verification to determine eligible records. Any discrepancies were adjudicated through consensus discussions with senior reviewers.
2.5 Data extraction
The following information was systematically extracted from eligible studies: first author, publication year, study population, sample size, research design type, country of origin, and patient distribution across TCM constitution types. Two investigators independently performed data extraction using a pretested form and cross-checked the results for consistency, with discrepancies resolved through discussions.
2.6 Quality assessment
Quality assessment was conducted using standardized tools appropriate to each study design: cross-sectional studies were evaluated with the Agency for Healthcare Research and Quality (AHRQ) checklist (15), while cohort and case–control studies were appraised using the Newcastle-Ottawa Scale (NOS) (16). For the AHRQ checklist, each of the 11 items (e.g., clarity of data sources, inclusion/exclusion criteria, handling of confounding factors) was evaluated as “Yes,” “No,” “Unclear,” or “Not Applicable.” Scoring criteria were defined as follows: “Yes” responses were assigned 1 point, while “No,” “Unclear,” and “Not Applicable” received 0 point. For cross-sectional studies, Item 11 about follow-up was deemed “Not Applicable” due to the inherent design of such studies. Consequently, this item was excluded from the total score calculation, resulting in a maximum achievable score of 10. Study quality was classified based on established thresholds in the literature (17) studies fulfilling ≥7 scores were categorized as high quality, those scoring 4–6 as moderate quality, and those with ≤3 points as low quality.
The NOS evaluates studies across eight domains (e.g., cohort selection, comparability, outcome assessment), with a maximum score of 9. Quality classification followed established thresholds: studies scoring ≥7 points were classified as high quality, those with 5–6 points as moderate quality, and those with ≤4 points as low quality (18). Two researchers independently conducted quality assessments, followed by cross-verification of all entries. Any discrepancies were resolved through consensus discussions or, when necessary, adjudication by a third reviewer.
2.7 Statistical analysis
All statistical analyses were performed using Review Manager 5.3 and Stata software (version 14.0). Two types of analyses were conducted: (1) pooled prevalence estimates for single-group proportions, and (2) comparative analyses between groups using ORs. For synthesizing single-group prevalence estimates (e.g., TCM constitution distributions), pooled proportions were calculated using the logit transformation to stabilize variances of proportional data. Results were back-transformed to the original proportion scale via the inverse logistic transformation and reported as proportions (%) with 95% confidence intervals (CIs). Heterogeneity across studies was assessed using Cochran’s Q test (p-value) and the I2 statistic. A random-effects model was applied if significant heterogeneity was detected (p < 0.1 or I2 ≥ 50%); otherwise, a fixed-effects model was used. Comparative effect analyses (e.g., AIS with hypertension population vs. AIS without hypertension population) employed the inverse variance method for effect size calculation. Heterogeneity assessment and model selection criteria followed the same approach as described for prevalence analyses. All comparative results are expressed as ORs with 95% CIs.
Sensitivity analyses using leave-one-out cross-validation and subgroup analyses stratified by clinically relevant covariates were conducted to investigate potential sources of heterogeneity. When more than 10 studies were included in the analysis, funnel plots, Egger’s test, and Begg’s test would be employed to assess publication bias (19). If publication bias was detected, the trim-and-fill method would be applied to examine its impact (20).
3 Results
3.1 Literature selection and study characteristics
Fifty-four studies were ultimately included for analysis. The literature selection flowcharts are provided in Supplementary Figures 1–6 (Supplementary material 2). The characteristics of the studies are summarized in Table 1. The studies were conducted in China, with publication years spanning from 2009 to 2024, and sample sizes ranging from 9 to 26,579 participants. Research design types included cross-sectional (n = 40), cohort (n = 4), and case–control (n = 10). 28 studies have analyzed the distribution characteristics of TCM constitution in the AIS population. 13 studies focused on individuals with hypertension, three on those with hypotension, two on AIS patients with hypertension, 10 on IS with hypertension, and two on ischemic cerebrovascular disease with hypoperfusion. The distribution characteristics of the nine TCM constitutions for each population were also recorded in detail, respectively.
Table 1
| Study ID | Research type | Study population | Sample size | Number of patients in each TCM constitution type | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Balanced | Phlegm-dampness | Blood-stasis | Damp-heat | Qi-stagnation | Qi-deficiency | Yin-deficiency | Yang-deficiency | Special Diathesis | ||||
| Li (21) | Cross-sectional | AIS | 193 | 26 | 53 | 18 | 11 | 17 | 28 | 23 | 14 | 3 |
| Cai (22) | Cohort | AIS | 202 | 4 | 66 | 36 | 4 | 1 | 31 | 59 | 1 | 0 |
| Liu (23) | Cross-sectional | AIS | 120 | 16 | 17 | 4 | 8 | 6 | 33 | 17 | 18 | 1 |
| Yang (24) | Cross-sectional | AIS | 696 | 170 | 101 | 78 | 92 | 18 | 93 | 70 | 68 | 6 |
| Yang (25) | Cross-sectional | AIS | 120 | 2 | 31 | 9 | 1 | 4 | 41 | 25 | 7 | 0 |
| Zhang et al. (26) | Cohort | AIS | 168 | 14 | 32 | 5 | 8 | 8 | 57 | 34 | 10 | 0 |
| Zhou et al. (27) | Cross-sectional | AIS | 303 | 4 | 115 | 42 | 3 | 4 | 42 | 78 | 12 | 3 |
| Yuan (28) | Cross-sectional | AIS | 72 | 0 | 16 | 20 | 1 | 1 | 20 | 11 | 3 | 0 |
| Huang (29) | Cross-sectional | AIS | 180 | 11 | 55 | 38 | 7 | 5 | 36 | 13 | 15 | 0 |
| Li (30) | Cross-sectional | AIS | 248 | 26 | 183 | 146 | 40 | 108 | 94 | 49 | 33 | 18 |
| Wang 2012 (31) | Cross-sectional | AIS | 142 | 30 | 12 | 5 | 6 | 7 | 36 | 32 | 14 | 0 |
| Li (32) | Cross-sectional | AIS | 399 | 108 | 63 | 43 | 19 | 19 | 61 | 38 | 45 | 3 |
| Cui (33) | Cross-sectional | AIS | 153 | 42 | 21 | 7 | 12 | 15 | 18 | 11 | 19 | 8 |
| Shi (34) | Cross-sectional | AIS | 95 | 7 | 18 | 13 | 8 | 14 | 7 | 8 | 20 | 0 |
| Liu (35) | Cohort | AIS | 125 | 0 | 91 | 57 | 4 | 19 | 62 | 47 | 29 | 5 |
| Zhen (36) | Case–control | AIS | 237 | NR | 39 | NR | NR | NR | 69 | 46 | NR | NR |
| Fu (37) | Cross-sectional | AIS | 176 | 19 | 129 | 107 | 32 | 71 | 67 | 31 | 29 | 10 |
| Qiu (38) | Cross-sectional | AIS | 87 | 3 | 23 | 9 | 2 | 2 | 20 | 18 | 9 | 1 |
| Yan (39) | Cross-sectional | AIS | 289 | 16 | 56 | 55 | 21 | 21 | 43 | 40 | 29 | 8 |
| Gao (40) | Cohort | AIS | 302 | 18 | 67 | 43 | 19 | 31 | 58 | 35 | 22 | 9 |
| Liang et al. (41) | Cross-sectional | AIS | 116 | 17 | 17 | 3 | 8 | 6 | 30 | 17 | 16 | 2 |
| Xu 2015 (42) | Cross-sectional | AIS | 500 | 10 | 243 | 117 | 91 | 77 | 147 | 59 | 120 | 9 |
| Li et al. (43) | Cross-sectional | AIS | 178 | 5 | 20 | 61 | 4 | 10 | 62 | 19 | 29 | 1 |
| Dong (44) | Cross-sectional | AIS | 140 | 0 | 92 | 12 | 0 | 0 | 32 | 4 | 0 | 0 |
| Zhang et al. (45) | Cross-sectional | AIS | 124 | 15 | 19 | 4 | 8 | 6 | 34 | 19 | 18 | 1 |
| Zou et al. (46) | Case–control | AIS | 40 | 6 | 4 | 3 | 3 | 5 | 7 | 11 | 1 | 0 |
| Li and Huang (47) | Cross-sectional | AIS | 106 | 1 | 33 | 23 | 6 | 9 | 18 | 11 | 4 | 1 |
| Li et al. (48) | Cross-sectional | AIS | 200 | 12 | 46 | 36 | 37 | 16 | 15 | 29 | 9 | 0 |
| Lin et al.(51) | Cross-sectional | Hypertension | 322 | 80 | 87 | 18 | 14 | 8 | 45 | 30 | 34 | 6 |
| Yang et al. (52) | Cross-sectional | Hypertension | 1923 | 774 | 778 | 60 | 8 | 4 | 27 | 158 | 99 | 15 |
| Li et al. (53) | Cross-sectional | Hypertension | 2,592 | 449 | 138 | 889 | 78 | 36 | 109 | 471 | 377 | 45 |
| Xiao et al.(54) | Cross-sectional | Hypertension | 26,579 | 6,726 | 12,278 | 1,399 | 740 | 320 | 3,192 | 2,429 | 2,483 | 78 |
| Lin et al. (55) | Case–control | Hypertension | 300 | 47 | 34 | 4 | 41 | 9 | 74 | 15 | 70 | 6 |
| Chen (56) | Cross-sectional | Hypertension | 197 | 39 | 47 | 2 | 10 | 6 | 24 | 36 | 32 | 1 |
| Zhang (57) | Case–control | Hypertension | 174 | 65 | 71 | 4 | 2 | 6 | 8 | 6 | 10 | 2 |
| Jin (58) | Case–control | Hypertension | 250 | 36 | 68 | 48 | NR | NR | NR | 34 | 31 | NR |
| Fan et al. (59) | Case–control | Hypertension | 500 | 115 | 93 | 19 | 32 | 21 | 46 | 65 | 79 | 30 |
| Zhang 2022 (60) | Cross-sectional | Hypertension | 695 | 411 | 119 | 10 | 1 | 16 | 33 | 33 | 63 | 9 |
| Wang and Hu 2023 (61) | Cross-sectional | Hypertension | 515 | 134 | 217 | 3 | 17 | 12 | 21 | 55 | 54 | 2 |
| Gao et al. (62) | Case–control | Hypertension | 51 | 2 | 13 | 3 | 3 | 6 | 3 | 18 | 3 | 0 |
| Li (63) | Case–control | Hypertension | 1,041 | 35 | 305 | 49 | 130 | 11 | 50 | 272 | 189 | NR |
| Zhou et al. (27) | Cross-sectional | AIS/IS with hypertension | 227 | 3 | 89 | 30 | 1 | 4 | 31 | 58 | 8 | 3 |
| Li (64) | Case–control | AIS/IS with hypertension | 114 | 6 | 24 | 28 | 5 | 7 | 14 | 22 | 8 | 0 |
| Yu et al. (65) | Cross-sectional | IS with hypertension | 162 | 8 | 36 | 27 | 13 | 9 | 32 | 24 | 11 | 2 |
| Wang (66) | Cross-sectional | IS with hypertension | 139 | 6 | 47 | 18 | 8 | 9 | 28 | 10 | 11 | 2 |
| Wang (67) | Case–control | IS with hypertension | 47 | 2 | 16 | 11 | 1 | 0 | 13 | 2 | 2 | 0 |
| Li (68) | Cross-sectional | IS with hypertension | 527 | 0 | 182 | 54 | 5 | 9 | 160 | 98 | 19 | 0 |
| Li (69) | Cross-sectional | IS with hypertension | 224 | 3 | 43 | 65 | 30 | 0 | 76 | 5 | 1 | 1 |
| Han (70) | Cross-sectional | IS with hypertension | 215 | 15 | 45 | 7 | 23 | 17 | 46 | 58 | 4 | NR |
| Song (71) | Cross-sectional | IS with hypertension | 137 | 8 | 72 | 38 | 24 | 12 | 57 | 37 | 11 | 0 |
| Wu (72) | Cross-sectional | IS with hypertension | 273 | 13 | 53 | 37 | 22 | 28 | 63 | 29 | 17 | 11 |
| Liu (73) | Cross-sectional | Hypotension | 53 | 18 | 2 | 0 | 1 | 1 | 9 | 0 | 1 | 0 |
| Wang and Miao (74) | Cross-sectional | Hypotension | 210 | 8 | 57 | 29 | 19 | 26 | 162 | 46 | 128 | 6 |
| Zhang (75) | Cross-sectional | Hypotension | 108 | 0 | 13 | 0 | 1 | 0 | 7 | 83 | 4 | 0 |
| Qiu (38) | Cross-sectional | Ischemic cerebrovascular disease with hypoperfusion | 59 | 2 | 12 | 7 | 4 | 1 | 20 | 8 | 4 | 1 |
| Chen (76) | Cross-sectional | Ischemic cerebrovascular disease with hypoperfusion | 9 | 0 | 1 | 1 | 3 | 2 | 0 | 1 | 1 | 0 |
The characteristics of the included studies.
AIS, acute ischemic stroke; IS, ischemic stroke; TCM, traditional Chinese medicine; NR, not reported.
3.2 Quality evaluation of the included studies
We assessed the quality of 40 cross-sectional studies using the AHRQ measurement tool (Figure 2). The results showed that 11 studies had a total score of 7 to 10 points and were considered to be of high quality. 28 studies had a total score of 4 to 6 points and were regarded as of moderate quality, and one study had a total score of 3 points and was considered to be of low quality. The majority of score deductions stemmed from insufficient reporting of consecutive enrollment status in non-population designs, unverified blinding procedures for subjective assessments, undocumented quality control measures for primary outcomes, or incomplete documentation of participant response rates and data completeness. The detailed scores for items of each study are presented in Supplementary Table 7 (Supplementary material 2).
Figure 2
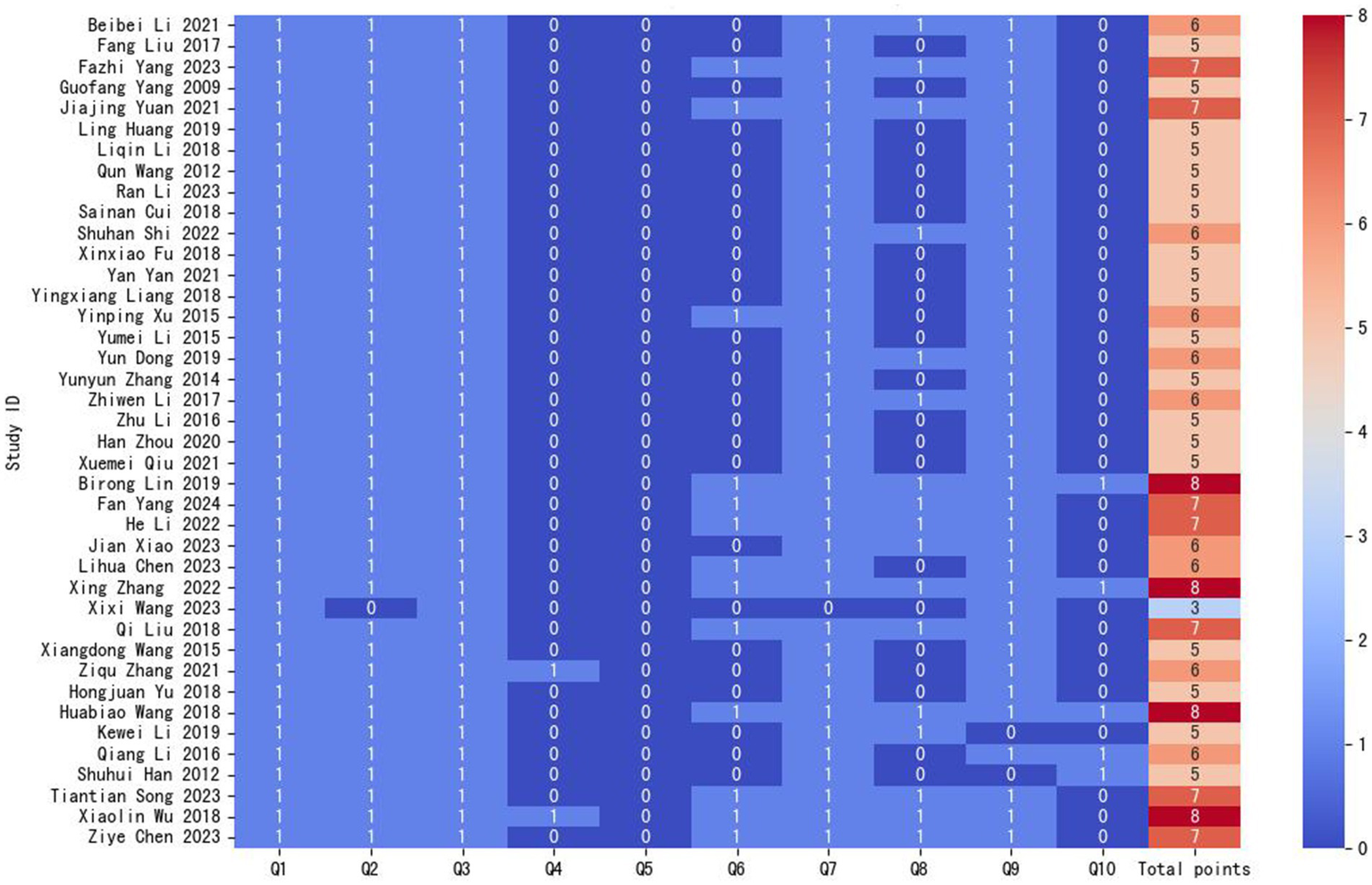
Results of the AHRQ scale assessment for cross-sectional studies. Q, question.
The NOS scale was used to assess the quality of four cohort studies and 10 case–control studies (Figure 3). 10 studies scored 7–9 points (classified as high-quality), while 4 studies scored 5–6 points (categorized as moderate-quality). The primary reasons for score deductions across most studies included inadequate follow-up duration, failure to describe follow-up completeness, and insufficient documentation of non-exposed group recruitment sources. The detailed scores for 8 items of each study are presented in Supplementary Table 8 (Supplementary material 2).
Figure 3

Results of the NOS scale assessment for cohort and case–control studies. V, variable.
3.3 Meta-analysis of TCM constitution patterns in study populations
Table 2 presents the meta-analysis results of TCM constitution distribution, whereas Table 3 compares TCM constitution types between the studied populations and other populations. The forest plots for the AIS population are presented in Figures 4, 5, with corresponding subgroup analysis forest plots provided in Figure 6. The forest plots for other meta-analyses and their subgroup analyses are presented in Supplementary Figures 7–19 (Supplementary material 2).
Table 2
| Metrics | Balanced constitution | Phlegm-dampness constitution | Blood-stasis constitution | Damp-heat constitution | Qi-stagnation constitution | Qi-deficiency constitution | Yin-deficiency constitution | Yang-deficiency constitution | Special Diathesis constitution | |
|---|---|---|---|---|---|---|---|---|---|---|
| AIS Population | Number of Studies | 24 | 28 | 27 | 26 | 26 | 28 | 28 | 26 | 17 |
| Cumulative Cases | 582 | 1,662 | 994 | 455 | 500 | 1,261 | 854 | 594 | 89 | |
| Cumulative Sample Size | 5,137 | 5,711 | 5,474 | 5,334 | 5,334 | 5,711 | 5,711 | 5,334 | 4,115 | |
| Proportion | 9% | 36% | 16% | 7% | 7% | 28% | 18% | 11% | 2% | |
| 95% CI | [0.06, 0.13] | [0.25, 0.51] | [0.11, 0.24] | [0.05, 0.09] | [0.05, 0.12] | [0.23, 0.35] | [0.15, 0.22] | [0.09, 0.14] | [0.01, 0.03] | |
| Q Value | 320.36 | 821.19 | 606.21 | 186.04 | 469.8 | 287.3 | 189.96 | 168.7 | 53.82 | |
| I2/% | 93 | 97 | 96 | 87 | 95 | 91 | 86 | 85 | 70 | |
| Hypertensive Population | Number of Studies | 13 | 13 | 13 | 12 | 12 | 12 | 13 | 13 | 10 |
| Cumulative Cases | 8,913 | 14,248 | 2,508 | 1,076 | 455 | 3,632 | 3,622 | 3,524 | 194 | |
| Cumulative Sample Size | 35,139 | 35,139 | 35,139 | 34,889 | 34,889 | 34,889 | 35,139 | 35,139 | 33,797 | |
| Proportion | 28% | 33% | 4% | 4% | 2% | 7% | 13% | 13% | 1% | |
| 95% CI | [0.20, 0.39] | [0.22, 0.52] | [0.02, 0.09] | [0.02, 0.06] | [0.01, 0.03] | [0.05, 0.11] | [0.09, 0.18] | [0.10, 0.17] | [0.01, 0.03] | |
| Q Value | 878.67 | 1532.45 | 2294.48 | 396.64 | 98.57 | 415.19 | 547.87 | 277.67 | 235.84 | |
| I2/% | 99 | 99 | 99 | 97 | 89 | 97 | 98 | 96 | 96 | |
| Hypotensive Population | Number of Studies | 2 | 3 | 1 | 3 | 2 | 3 | 2 | 3 | 1 |
| Cumulative Cases | 26 | 72 | 29 | 21 | 27 | 178 | 129 | 133 | 6 | |
| Cumulative Sample Size | 263 | 371 | 210 | 371 | 263 | 371 | 318 | 371 | 210 | |
| Proportion | 14% | 15% | 16% | 3% | 7% | 37% | 96% | 11% | 3% | |
| 95% CI | [0.01, 1.78] | [0.05, 0.43] | [0.11, 0.24] | [0.01, 0.17] | [0.01, 0.44] | [0.03, 4.88] | [0.09, 10.82] | [0.01, 2.53] | [0.01, 0.07] | |
| Q Value | 30.71 | 16.68 | N/A | 7.38 | 3.74 | 115.41 | 76.44 | 65.5 | N/A | |
| I2/% | 97 | 88 | N/A | 73 | 73 | 98 | 99 | 97 | N/A | |
| AIS with hypertension Population | Number of Studies | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 |
| Cumulative Cases | 9 | 113 | 58 | 6 | 11 | 45 | 80 | 16 | 3 | |
| Cumulative Sample Size | 341 | 341 | 341 | 341 | 341 | 341 | 341 | 341 | 227 | |
| Proportion | 3% | 42% | 22% | 2% | 4% | 15% | 31% | 5% | 1% | |
| 95% CI | [0.01, 0.12] | [0.18, 1.00] | [0.11, 0.47] | [0.00, 0.16] | [0.01, 0.13] | [0.11, 0.21] | [0.24, 0.40] | [0.03, 0.11] | [0.00, 0.04] | |
| Q Value | 3.94 | 10.94 | 6.73 | 4.51 | 4.12 | 0.13 | 1.64 | 1.99 | N/A | |
| I2/% | 75 | 91 | 85 | 78 | 76 | 0 | 39 | 50 | N/A | |
| IS with hypertension Population | Number of Studies | 9 | 10 | 10 | 10 | 8 | 10 | 10 | 10 | 5 |
| Cumulative Cases | 64 | 607 | 315 | 132 | 95 | 520 | 343 | 92 | 19 | |
| Cumulative Sample Size | 1,538 | 2065 | 2065 | 2065 | 1794 | 2065 | 2065 | 2065 | 1,025 | |
| Proportion | 5% | 40% | 19% | 6% | 6% | 31% | 17% | 5% | 2% | |
| 95% CI | [0.04, 0.06] | [0.29, 0.56] | [0.13, 0.28] | [0.04, 0.11] | [0.04, 0.09] | [0.23, 0.41] | [0.12, 0.25] | [0.04, 0.07] | [0.01, 0.04] | |
| Q Value | 12.97 | 89.66 | 83.59 | 61.32 | 32.53 | 65.84 | 77.66 | 21.11 | 8.44 | |
| I2/% | 38 | 90 | 89 | 85 | 78 | 86 | 88 | 57 | 53 | |
| Ischemic cerebrovascular disease with hypoperfusion | Number of Studies | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 |
| Cumulative Cases | 2 | 13 | 8 | 7 | 3 | 20 | 9 | 5 | 1 | |
| Cumulative Sample Size | 59 | 68 | 68 | 68 | 68 | 59 | 68 | 68 | 59 | |
| Proportion | 4% | 24% | 13% | 18% | 8% | 51% | 15% | 8% | 2% | |
| 95% CI | [0.01, 0.14] | [0.13, 0.44] | [0.06, 0.28] | [0.03, 1.18] | [0.00, 1.17] | [0.30, 0.88] | [0.08, 0.31] | [0.03, 0.20] | [0.00, 0.12] | |
| Q Value | N/A | 0.41 | 0 | 4.84 | 4.75 | N/A | 0.04 | 0.21 | N/A | |
| I2/% | N/A | 0 | 0 | 79 | 79 | N/A | 0 | 0 | N/A | |
Meta-analysis results of TCM constitution distribution in AIS, BP abnormalities, and ischemic cerebrovascular diseases with BP abnormalities populations.
N/A, not applicable; AIS, acute ischemic stroke; IS, ischemic stroke.
Table 3
| Metrics | Balanced constitution | Phlegm-dampness constitution | Blood-stasis constitution | Damp-heat constitution | Qi-stagnation constitution | Qi-deficiency constitution | Yin-deficiency constitution | Yang-deficiency constitution | Special Diathesis constitution | |
|---|---|---|---|---|---|---|---|---|---|---|
| AIS Population VS General Population | Number of Studies | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 3 | 1 |
| Heterogeneity (I2/%) | 80 | 46 | 0 | 68 | 56 | 79 | 55 | 63 | N/A | |
| Model | Random | Fixed | Fixed | Random | Random | Random | Random | Random | Fixed | |
| Pooled OR | 0.11 | 3.27 | 2.28 | 0.8 | 1 | 1.35 | 1.2 | 0.52 | 0.27 | |
| 95% CI | [0.05, 0.25] | [2.43, 4.40] | [1.69, 3.07] | [0.25, 2.60] | [0.33, 3.04] | [0.57, 3.19] | [0.68, 2.09] | [0.22, 1.24] | [0.02, 4.42] | |
| Z | 5.09 | 7.79 | 5.41 | 0.37 | 0 | 0.67 | 0.63 | 1.48 | 0.92 | |
| P | <0.00001 | <0.00001 | <0.00001 | 0.71 | 1 | 0.5 | 0.53 | 0.14 | 0.36 | |
| Hypertensive Population VS Non-hypertensive Population | Number of Studies | 13 | 13 | 13 | 12 | 12 | 12 | 13 | 13 | 9 |
| Heterogeneity (I2/%) | 97 | 86 | 53 | 12 | 28 | 64 | 84 | 83 | 46 | |
| Model | Random | Random | Random | Fixed | Fixed | Random | Random | Random | Random | |
| Pooled OR | 0.39 | 1.81 | 1.26 | 1.06 | 1.25 | 1.2 | 1.41 | 1.14 | 1.01 | |
| 95%CI | [0.28, 0.56] | [1.48, 2.21] | [1.03, 1.53] | [0.97, 1.16] | [1.09, 1.43] | [0.96, 1.51] | [1.09, 1.81] | [0.90, 1.44] | [0.69, 1.47] | |
| Z | 5.26 | 5.75 | 2.28 | 1.36 | 3.15 | 1.59 | 2.66 | 1.07 | 0.05 | |
| P | < 0.00001 | < 0.00001 | 0.02 | 0.18 | 0.002 | 0.11 | 0.008 | 0.28 | 0.96 | |
| Hypotensive Population VS Normal BP Population | Number of Studies | 1 | 2 | N/A | 1 | 1 | 2 | 1 | 2 | N/A |
| Heterogeneity (I2/%) | N/A | 90 | N/A | N/A | N/A | 45 | N/A | 28 | N/A | |
| Model | Fixed | Random | N/A | Fixed | Fixed | Fixed | Fixed | Fixed | N/A | |
| Pooled OR | 0.88 | 1.29 | N/A | 0.4 | 0.46 | 3.06 | 3.24 | 1.26 | N/A | |
| 95%CI | [0.48, 1.64] | [0.02,69.40] | N/A | [0.05, 3.07] | [0.06, 3.65] | [1.41, 6.65] | [1.89, 5.55] | [0.37, 4.28] | N/A | |
| Z | 0.39 | 0.13 | N/A | 0.89 | 0.73 | 2.83 | 4.29 | 0.37 | N/A | |
| P | 0.7 | 0.9 | N/A | 0.38 | 0.47 | 0.005 | < 0.0001 | 0.71 | N/A | |
| AIS with hypertension Population VS AIS without hypertension Population | Number of Studies | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | N/A |
| Heterogeneity (I2/%) | 0 | 0 | 69 | 0 | N/A | 0 | 63 | 0 | N/A | |
| Model | Fixed | Fixed | Random | Fixed | Fixed | Fixed | Random | Fixed | N/A | |
| Pooled OR | 0.49 | 1.13 | 1.3 | 0.4 | 0.45 | 0.85 | 1.4 | 0.85 | N/A | |
| 95%CI | [0.19, 1.23] | [0.74, 1.71] | [0.52, 3.26] | [0.14, 1.10] | [0.17, 1.18] | [0.50, 1.45] | [0.62, 3.16] | [0.38, 1.90] | N/A | |
| Z | 1.52 | 0.56 | 0.56 | 1.78 | 1.62 | 0.61 | 0.8 | 0.39 | N/A | |
| P | 0.13 | 0.57 | 0.57 | 0.08 | 0.11 | 0.54 | 0.42 | 0.7 | N/A | |
| IS with hypertension Population VS IS without hypertension Population | Number of Studies | 8 | 8 | 8 | 7 | 5 | 8 | 8 | 8 | 3 |
| Heterogeneity (I2/%) | 57 | 87 | 72 | 53 | 44 | 84 | 91 | 12 | 0 | |
| Model | Random | Random | Random | Random | Fixed | Random | Random | Fixed | Fixed | |
| Pooled OR | 0.5 | 2.15 | 1.1 | 1.18 | 1.26 | 1.05 | 0.66 | 0.66 | 0.78 | |
| 95%CI | [0.24, 1.03] | [1.02, 4.55] | [0.67, 1.81] | [0.62, 2.23] | [0.76, 2.08] | [0.57, 1.95] | [0.25, 1.73] | [0.45, 0.97] | [0.32, 1.89] | |
| Z | 1.88 | 2.01 | 0.37 | 0.51 | 0.9 | 0.16 | 0.84 | 2.1 | 0.55 | |
| P | 0.06 | 0.04 | 0.71 | 0.61 | 0.37 | 0.88 | 0.4 | 0.04 | 0.58 | |
| Ischemic cerebrovascular disease with hypoperfusion VS Ischemic cerebrovascular disease with normoperfusion | Number of Studies | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | N/A |
| Heterogeneity (I2/%) | N/A | 0 | 68 | 0 | N/A | N/A | 0 | 30 | N/A | |
| Model | Fixed | Fixed | Random | Fixed | Fixed | Fixed | Fixed | Fixed | N/A | |
| Pooled OR | 1.93 | 0.7 | 0.95 | 1.69 | 0.98 | 1.95 | 0.48 | 1.01 | N/A | |
| 95%CI | [0.17, 21.90] | [0.30, 1.66] | [0.07, 12.30] | [0.35, 8.26] | [0.06, 16.09] | [0.63, 5.99] | [0.19, 1.17] | [0.24, 4.19] | N/A | |
| Z | 0.53 | 0.81 | 0.04 | 0.65 | 0.01 | 1.16 | 1.62 | 0.01 | N/A | |
| P | 0.6 | 0.42 | 0.97 | 0.52 | 0.99 | 0.24 | 0.11 | 0.99 | N/A | |
Comparison of TCM constitution types between study populations and other populations.
N/A, not applicable; AIS, acute ischemic stroke; IS, ischemic stroke.
Figure 4

The forest plots of Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions in the AIS population.
Figure 5
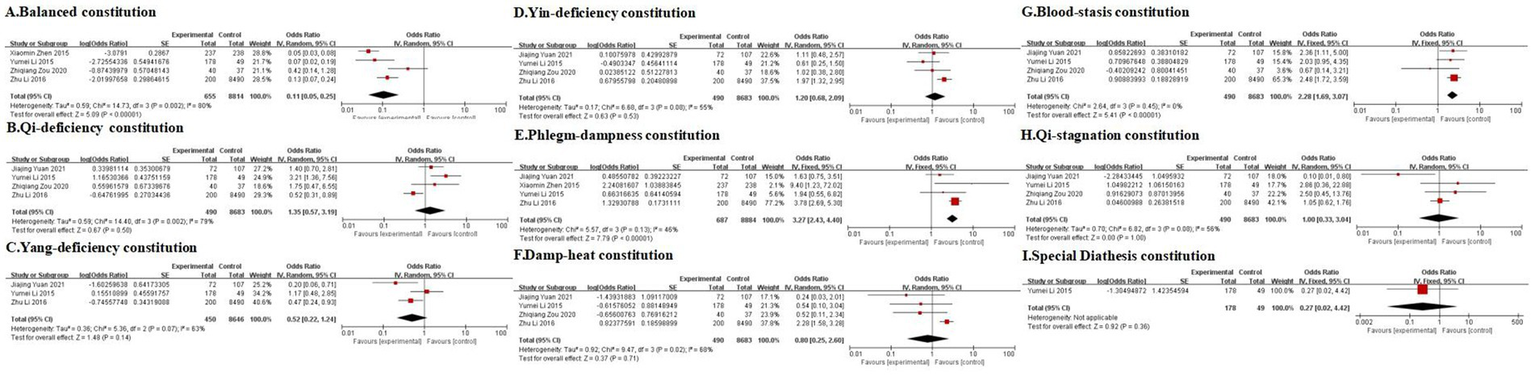
The forest plots comparing Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions between the AIS population and the general population.
Figure 6
The subgroup analysis for Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions in the AIS population according to the study design.
3.3.1 Meta-analysis of TCM constitution patterns in the AIS population
3.3.1.1 Main findings
A total of 28 studies (21–48) were included in the analysis (Table 2, Figure 4). Due to significant heterogeneity among studies, a random-effects model was used for the meta-analysis. The results revealed that Phlegm-dampness (Figure 4E), Qi-deficiency (Figure 4B), Yin-deficiency (Figure 4D), and Blood-stasis constitutions (Figure 4G) predominated among AIS patients, each accounting for ≥15% of the study population. Five studies compared the distribution of TCM constitution types between AIS patients and the general population (Table 3, Figure 5), with a total sample size of 9,648 cases (727 AIS patients and 8,921 controls). The meta-analysis demonstrated that Phlegm-dampness constitution (OR = 3.27, 95% CI [2.43, 4.40], p < 0.00001) (Figure 5E) and Blood-stasis constitution (OR = 2.28, 95% CI [1.69, 3.07], p < 0.00001) (Figure 5G) were more prevalent in AIS patients. In contrast, the Balanced constitution (Figure 5A) was more common in the general population and served as a protective factor against AIS (OR = 0.11, 95% CI [0.05, 0.25], p < 0.00001). No statistically significant differences were observed in the distribution of other constitutional types between the two groups.
3.3.1.2 Subgroup analysis
We conducted a subgroup analysis stratifying the 28 included studies by study design type (cross-sectional, cohort, and case–control). (Figure 6). Following subgroup analysis, heterogeneity decreased for seven of the nine TCM constitutions examined (Figures 6A,B,D–F,H,I). This suggests that the study design contributed to the observed high heterogeneity. While the proportion of specific constitutions within the AIS population varied across study types, the Phlegm-dampness (Figure 6E), Qi-deficiency (Figure 6B), Yin-deficiency (Figure 6D), and Blood-stasis constitutions (Figure 6G) consistently each accounted for ≥15% of cases across most studies. Conversely, the other five constitutions each represented <15% in most design categories. This confirms that Phlegm-dampness, Blood-stasis, Qi-deficiency, and Yin-deficiency constitutions are the predominant constitutions in AIS patients, aligning with the pooled meta-analysis results.
Considering the potential influence of disease severity and stroke subtype on TCM constitution distribution, we analyzed these factors. Only one study (21) reported on disease severity, specifically including mild-to-moderate AIS patients with a National Institutes of Health Stroke Scale (NIHSS) score <15. The prevalent constitutions identified—Phlegm-dampness (27.46%), Qi-deficiency (14.51%), Yin-deficiency (11.92%), and Blood-stasis (9.33%)—were consistent with the pooled meta-analysis findings. Similarly, only one study (44) assessed stroke subtypes, focusing exclusively on the large artery atherosclerosis (LAA) subtype. The top four constitutions were Phlegm-dampness (65.71%), Qi-deficiency (22.86%), Blood-stasis (8.57%), and Yin-deficiency (2.86%), again mirroring the primary meta-analysis results.
Collectively, these subgroup analyses reinforce the robustness of the conclusion that Phlegm-dampness, Blood-stasis, Qi-deficiency, and Yin-deficiency are the most prevalent constitutions in AIS across diverse study designs. It further suggests this pattern holds within the limited available data for mild-to-moderate disease severity and the LAA stroke subtype.
3.3.2 Meta-analysis of TCM constitution patterns in the hypertensive population
3.3.2.1 Main findings
Two studies have explored the distribution patterns of TCM constitutions among hypertensive populations (49, 50). A meta-analysis of 10 studies published before May 31, 2018, was conducted (49), revealing significant associations between hypertension and specific constitutional types. The analysis demonstrated a higher prevalence of Phlegm-dampness, Yin-deficiency, Qi-deficiency, and Blood-stasis constitutions in the hypertensive population, while a Balanced constitution showed protective effects (p < 0.05). These findings were further corroborated by another study (50), which included 13 case–control studies published before January 2019. The study identified constitutional profiles where Phlegm-dampness, balanced, Yin-deficiency, and Qi-deficiency types each accounted for >15% of cases. Compared with the general population, Phlegm-dampness, Qi-deficiency, and Yin-deficiency were found to be risk factors for hypertension, while the Balanced constitution was a protective factor, with all differences being statistically significant (p < 0.05).
To update and extend these findings, we performed a supplementary meta-analysis incorporating studies published between January 2019, and January 2025. Thirteen studies (51–63) revealed that Phlegm-dampness, balanced, Yin-deficiency, Qi-deficiency, and Yang-deficiency constitutions were prevalent in hypertensive individuals (Table 2, Supplementary Figure 7). These studies also compared the TCM constitution distribution between hypertensive (n = 35,139) and non-hypertensive (n = 40,003) populations. The meta-analysis showed that hypertensive individuals were more likely to exhibit Phlegm-dampness (OR = 1.81, 95% CI [1.48, 2.21], p < 0.00001), Yin-deficiency (OR = 1.41, 95% CI [1.09, 1.81], p = 0.008), Blood-stasis (OR = 1.26, 95% CI [1.03, 1.53], p = 0.02), and Qi-stagnation constitutions (OR = 1.25, 95% CI [1.09, 1.43], p = 0.002). In contrast, the Balanced constitution (OR = 0.39, 95% CI [0.28, 0.56], p < 0.00001) was more common in non-hypertensive individuals. No statistically significant differences were observed in the distribution of other constitutions between the two groups (Table 3, Supplementary Figure 8). These findings demonstrate remarkable consistency with previous meta-analyses (49, 50), confirming the protective role of the Balanced constitution and the susceptibility patterns associated with Phlegm-dampness, Yin-deficiency, Qi-deficiency, and Blood-stasis constitutions in hypertension.
3.3.2.2 Subgroup analysis
We stratified the 13 included studies by study design type (cross-sectional and case–control) for subgroup analysis (Supplementary Figure 9). Following subgroup analysis, heterogeneity decreased for Yang-deficiency (Supplementary Figure 9C), Dampness-heat (Supplementary Figure 9F), Qi-stagnation (Supplementary Figure 9H), and Special Diathesis constitutions (Supplementary Figure 9I), indicating that study design partially accounted for the high heterogeneity. Although the proportional distribution of TCM constitutions varied across study types, it is evident that the Phlegm-dampness, Balanced, Qi-deficiency, Yin-deficiency, and Yang-deficiency constitutions consistently emerged as the most prevalent in hypertensive population across all design categories. These findings align with the pooled results described above.
3.3.3 Meta-analysis of TCM constitution patterns in AIS with hypertension population
3.3.3.1 Main findings
The meta-analysis included two studies (27, 64) examining TCM constitution in AIS patients with hypertension (Table 2, Supplementary Figure 10). The results indicated that Phlegm-dampness, Qi-deficiency, Yin-deficiency, and Blood-stasis constitutions each accounted for ≥15% of cases, confirming their prevalence in this population. The two studies also compared the distribution of TCM constitution types between AIS patients with hypertension (n = 341) and those without (n = 179). No statistically significant differences were observed in constitutional distribution patterns between groups. This finding, while preliminary due to the limited sample size, suggests the need for further investigation into the role of constitutional factors in AIS patients with hypertension (Table 3, Supplementary Figure 11).
3.3.3.2 Subgroup analysis
Studies were categorized by study design type (cross-sectional or case–control) for subgroup analysis. (Supplementary Figure 12). The limited number of included studies precluded a definitive assessment of whether study design influenced heterogeneity. However, it was noteworthy that the Phlegm-dampness, Blood-stasis, Qi-deficiency, and Yin-deficiency constitutions each accounted for ≥15% of cases in the majority of studies within both design categories. Conversely, the remaining five constitutions consistently each represented <15% across subgroups. This pattern confirms these four constitutions as predominant in the AIS with hypertension population, concordant with the pooled findings.
3.3.4 Meta-analysis of TCM constitution patterns in IS with hypertension population
3.3.4.1 Main findings
A total of 10 studies (27, 64–72) were identified and included in the meta-analysis. The findings showed that Phlegm-dampness, Qi-deficiency, Yin-deficiency, and Blood-stasis constitutions each constituted ≥15% of cases, highlighting their prominence among IS patients with hypertension (Table 2, Supplementary Figure 13). Eight studies investigated the distribution of TCM constitution types in a cohort of 1,955 IS patients, comprising 1,323 with hypertension and 632 without. The results revealed that the Phlegm-dampness constitution (OR = 2.15, 95% CI [1.02, 4.55], p = 0.04) was significantly more prevalent in IS patients with hypertension. Conversely, the Yang-deficiency constitution was less common in the hypertensive group (OR = 0.66, 95% CI [0.45, 0.97], p = 0.04). These differences were statistically significant (Table 3, Supplementary Figure 14).
3.3.4.2 Subgroup analysis
Studies were classified by study design type (cross-sectional or case–control) for subgroup analysis. (Supplementary Figure 15). After stratification, heterogeneity decreased substantially and was eliminated (I2 = 0%) in the case–control subgroups for the following constitutions: Balanced constitution (Supplementary Figure 15A), Yang-deficiency constitution (Supplementary Figure 15C), Dampness-heat constitution (Supplementary Figure 15F), and Blood-stasis constitution (Supplementary Figure 15G). These findings identified study design as a primary driver of the observed heterogeneity. Despite variations in the proportional distribution of constitutions across study types, the Phlegm-dampness, Blood-stasis, Qi-deficiency, and Yin-deficiency constitutions each comprised ≥15% of cases in the majority of studies within both design categories. The remaining five constitutions consistently each accounted for <15% across subgroups. This confirms these four as core TCM constitutions in the IS with hypertension population, consistent with the pooled results.
We further assessed the potential influences of disease severity and stroke subtypes on TCM constitution distribution. No studies addressed associations with disease severity. However, one study (68) examined stroke subtypes, specifically including patients with LAA and/or small artery occlusion (SAO). In this cohort, the predominant constitutions were: Phlegm-dampness, Qi-deficiency, Yin-deficiency, and Blood-stasis—aligning with the meta-analysis results for IS patients with hypertension (Table 2).
3.3.5 Meta-analysis of TCM constitution patterns in hypotensive population
The analysis incorporated three eligible studies (73–75). Significant heterogeneity among studies necessitated the application of random-effects models. The findings revealed that Phlegm-dampness, Qi-deficiency, Yin-deficiency, and Blood-stasis constitutions each accounted for ≥15% of the cases in individuals with hypotension (Table 2, Supplementary Figure 16). Two studies (73, 75) compared TCM constitution types in 635 participants, including 161 with hypotension and 474 with normal BP. The meta-analysis demonstrated that Yin-deficiency (OR = 3.24, 95% CI [1.89, 5.55], p < 0.0001) and Qi-deficiency (OR = 3.06, 95% CI [1.41, 6.65], p = 0.005) were more prevalent among hypotensive individuals compared to the controls (Table 3, Supplementary Figure 17). All three eligible studies employed cross-sectional designs, precluding subgroup analysis by study type due to homogeneity.
3.3.6 Meta-analysis of TCM constitution patterns in ischemic cerebrovascular diseases with hypoperfusion populations
The meta-analysis incorporated two studies (38, 76) demonstrating that Qi-deficiency, Phlegm-dampness, Damp-heat, and Yin-deficiency constitutions each accounted for at least 15% of cases (Table 2, Supplementary Figure 18). The two studies also evaluated the differences in TCM constitution types between ischemic cerebrovascular patients with hypoperfusion (n = 68) and those with normoperfusion (n = 56). Due to the limited sample size, the meta-analysis did not identify any significant differences in TCM constitution distribution between the two groups (Table 3, Supplementary Figure 19). Subgroup analysis by study type was inapplicable as all two studies shared identical cross-sectional designs.
3.4 Sensitivity analysis
Sensitivity analyses were performed by sequentially excluding each included study. In the meta-analysis of the Special Diathesis constitution among IS with hypertension population, the exclusion of the study by Wu et al. (72) substantially reduced heterogeneity (I2 decreased from 53% [p = 0.08] to 0% [p = 0.78]). However, the pooled estimate was not statistically distinct (pre-exclusion: 2% [0.01, 0.04] vs. post-exclusion: 1% [0.01, 0.02]), confirming the low distribution of Special Diathesis constitution in this population. For the remaining five population subgroups, sequential exclusion of individual studies demonstrated no material alteration in heterogeneity indices or effect sizes, indicating robust primary findings.
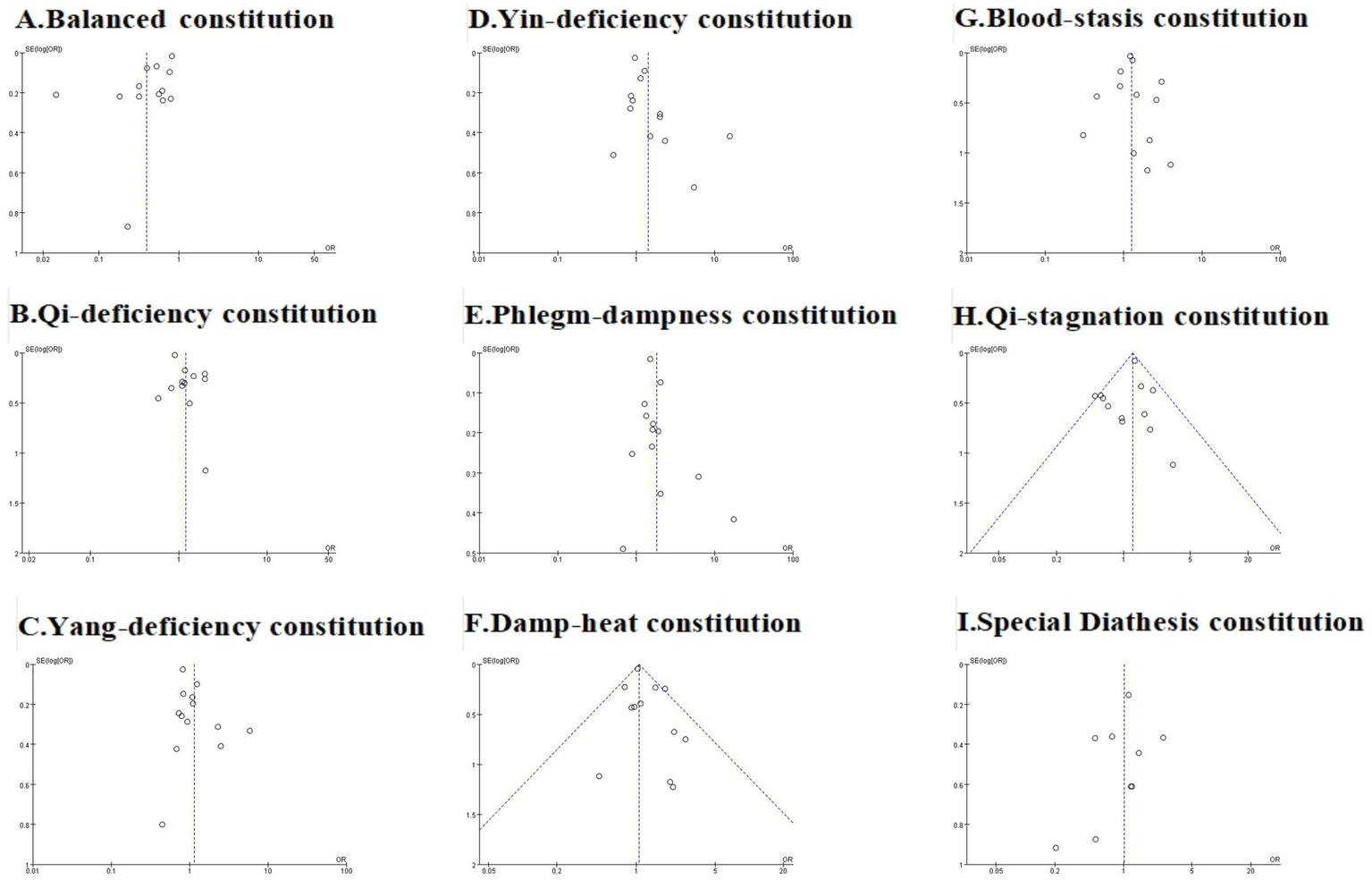
3.5 Publication bias assessment
We assessed publication bias for analyses incorporating more than 10 studies, including meta-analyses of TCM constitution distributions in the AIS population, hypertensive population, and comparative analyses of hypertensive versus non-hypertensive population. Trim-and-fill analysis was performed where publication bias was detected. The overall assessment indicated that while some analyses exhibited publication bias, the original conclusions remained robust after trim-and-fill correction. Funnel plots are presented in Figures 7–9, with Egger’s test, Begg’s test, and trim-and-fill results detailed in Table 4.
Figure 7
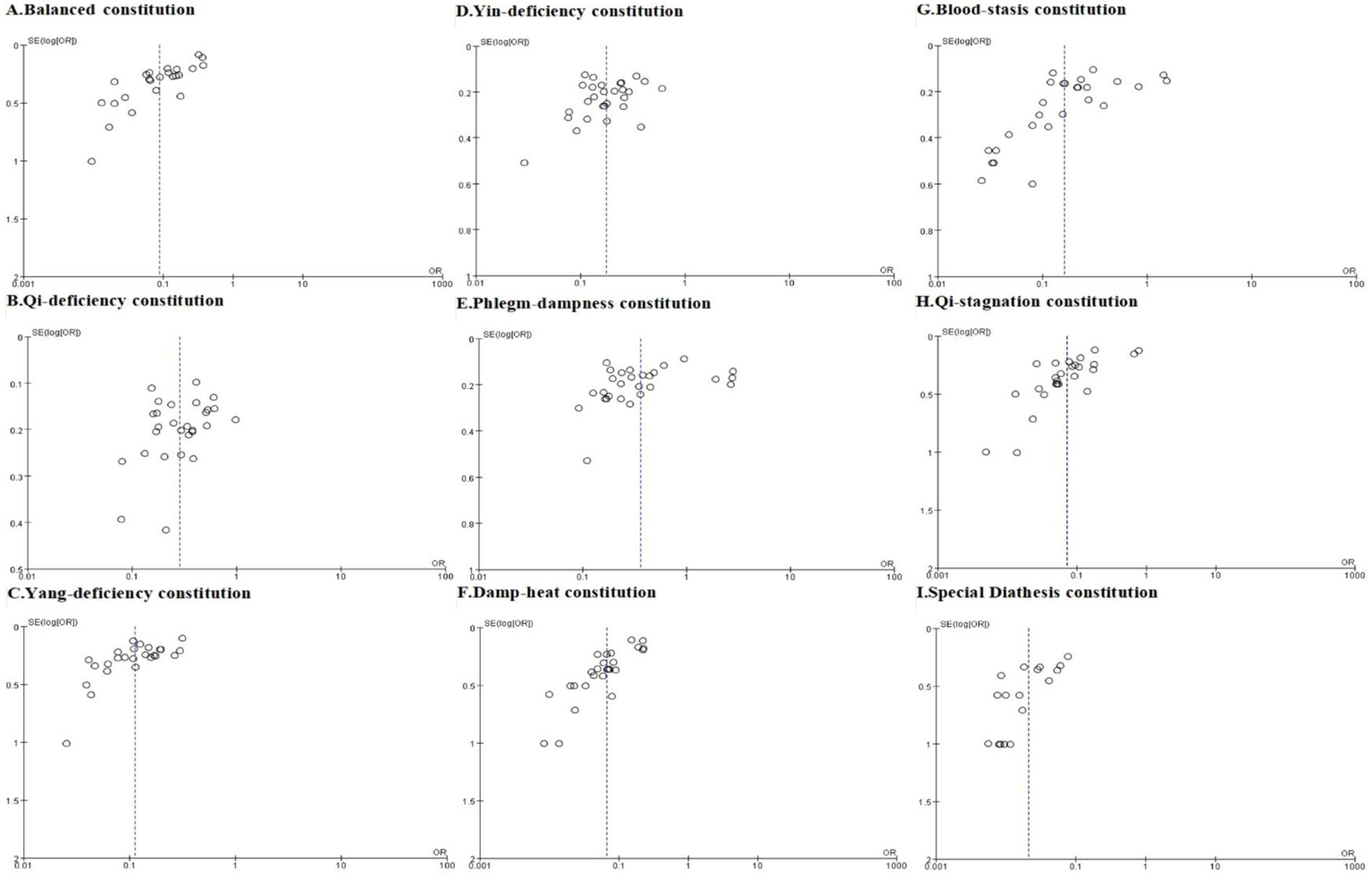
The funnel plots of Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions in the AIS population.
Figure 8

The funnel plots of Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions in the hypertensive population.
Figure 9
The funnel plots comparing Balanced constitution (A), Qi-deficiency constitution (B), Yang-deficiency constitution (C), Yin-deficiency constitution (D), Phlegm-dampness constitution (E), Damp-heat constitution (F), Blood-stasis constitution (G), Qi-stagnation constitution (H), and Special Diathesis constitution (I) distributions between the hypertensive population and the non-hypertensive population.
Table 4
| Population | TCM constitution | Egger’s test | Begg’s test | Trim and fill method | |||
|---|---|---|---|---|---|---|---|
| Intercept | P | Kendall’s tau | P | Number of imputed studies | Pooled proportion after trim and fill [95% CI], P | ||
| AIS Population | Yin-deficiency constitution | −2.207 | 0.187 | −0.159 | 0.236 | N/A | N/A |
| Phlegm-dampness constitution | −4.691 | 0.139 | −0.175 | 0.192 | N/A | N/A | |
| Qi-deficiency constitution | −2.393 | 0.256 | −0.196 | 0.144 | N/A | N/A | |
| Blood-stasis constitution | −5.549 | 0.008 | −0.345 | 0.012 | 0 | Data unchanged | |
| Balanced constitution | −6.089 | <0.0001 | −0.449 | 0.002 | 0 | Data unchanged | |
| Damp-heat constitution | −4.317 | <0.0001 | −0.366 | 0.009 | 0 | Data unchanged | |
| Qi-stagnation constitution | −6.397 | <0.0001 | −0.280 | 0.045 | 0 | Data unchanged | |
| Yang-deficiency constitution | −3.852 | <0.0001 | −0.372 | 0.008 | 0 | Data unchanged | |
| Special Diathesis constitution | −3.032 | 0.002 | −0.250 | 0.161 | 0 | Data unchanged | |
| Hypertensive Population | Yin-deficiency constitution | 2.041 | 0.449 | −0.051 | 0.807 | N/A | N/A |
| Phlegm-dampness constitution | −9.853 | 0.005 | −0.026 | 0.903 | 2 | 0.28 [0.14, 0.58], p = 0.001 | |
| Qi-deficiency constitution | −3.866 | 0.074 | −0.091 | 0.681 | N/A | N/A | |
| Blood-stasis constitution | −2.433 | 0.637 | 0.205 | 0.329 | N/A | N/A | |
| Balanced constitution | −0.775 | 0.812 | −0.231 | 0.272 | N/A | N/A | |
| Damp-heat constitution | 1.348 | 0.592 | −0.212 | 0.337 | N/A | N/A | |
| Qi-stagnation constitution | 2.394 | 0.054 | 0.182 | 0.411 | N/A | N/A | |
| Yang-deficiency constitution | 1.996 | 0.294 | −0.077 | 0.714 | N/A | N/A | |
| Special Diathesis constitution | 2.170 | 0.489 | −0.111 | 0.655 | N/A | N/A | |
| Hypertensive Population VS Non-hypertensive Population | Yin-deficiency constitution | 1.691 | 0.043 | 0.231 | 0.272 | 0 | Data unchanged |
| Phlegm-dampness constitution | 1.041 | 0.244 | 0.231 | 0.272 | N/A | N/A | |
| Qi-deficiency constitution | 1.172 | 0.030 | −0.273 | 0.217 | 0 | Data unchanged | |
| Blood-stasis constitution | 0.127 | 0.810 | 0.077 | 0.714 | N/A | N/A | |
| Balanced constitution | −4.937 | 0.012 | 0 | 1 | 4 | 0.28 [0.15,0.54], P<0.0001 | |
| Damp-heat constitution | 0.504 | 0.204 | 0.152 | 0.493 | N/A | N/A | |
| Qi-stagnation constitution | −0.460 | 0.347 | 0.061 | 0.784 | N/A | N/A | |
| Yang-deficiency constitution | 1.570 | 0.059 | 0 | 1 | N/A | N/A | |
| Special Diathesis constitution | −0.725 | 0.440 | −0.333 | 0.211 | N/A | N/A | |
Publication bias assessment with Egger’s test, Begg’s test, and Trim-and-fill analysis.
N/A, not applicable; AIS, acute ischemic stroke; TCM, traditional Chinese medicine.
For the AIS population, funnel plots for Yin-deficiency, Phlegm-dampness, and Qi-deficiency constitutions were symmetrical (Figure 7), with both Egger’s and Begg’s tests yielding p > 0.05, indicating no significant publication bias. However, funnel plots for Blood-stasis, Balanced, Damp-heat, Qi-stagnation, Yang-deficiency, and Special Diathesis constitutions demonstrated slight asymmetry, with either Egger’s or Begg’s test showing p ≤ 0.05, suggesting potential publication bias. Trim-and-fill analysis revealed no studies requiring addition or removal, confirming the robustness of original findings and indicating that publication bias did not substantively impact conclusions.
In the meta-analysis of TCM constitution distribution among hypertensive populations, funnel plots for all nine constitutions appeared generally symmetrical (Figure 8). With the exception of the Phlegm-dampness constitution which demonstrated significant asymmetry on Egger’s test (p = 0.005), both Egger’s and Begg’s tests for the remaining eight constitutions yielded non-significant results (p > 0.05), indicating no substantial evidence of publication bias. Trim-and-fill analysis for Phlegm-dampness constitution identified two missing studies. After imputation, the pooled prevalence estimate was 28% [0.14, 0.58]—closely aligned with the original effect size in Table 2—thereby reinforcing that Phlegm-dampness is among the most prevalent TCM constitutions in hypertension.
Regarding comparative analyses between hypertensive and non-hypertensive populations, funnel plots demonstrated symmetry for Phlegm-dampness, Blood-stasis, Damp-heat, Qi-stagnation, Yang-deficiency, and Special Diathesis constitutions (Figure 9), with non-significant Egger’s and Begg’s tests (p > 0.05), indicating no publication bias. Although Yin-deficiency (Egger’s test: p = 0.043; Begg’s test: p = 0.272) and Qi-deficiency (Egger’s test: p = 0.030; Begg’s test: p = 0.217) constitutions showed minor asymmetry, trim-and-fill analysis required no study imputation, confirming minimal bias impact. Balanced constitution exhibited significant funnel plot asymmetry (Egger’s test: p = 0.012; Begg’s test: p < 0.0001). Trim-and-fill imputation added four studies, yielding a corrected effect size of 0.28 [0.15, 0.54] (p < 0.0001). This result remained consistent with the original conclusion that Balanced constitution prevalence is significantly lower in the hypertensive population, affirming its role as a protective factor against hypertension.
4 Discussion
4.1 Summary of the findings
Approximately 75% of AIS patients present with elevated BP, mediated by neurological injury, autonomic dysfunction, and pre-existing hypertension (3, 4). In addition, acute disruption of cerebral autoregulation after AIS impairs cerebrovascular adaptability to BP fluctuations, exacerbating ischemic tissue vulnerability to both hypoperfusion and hyperperfusion (77). This creates a therapeutic paradox: aggressive early BP reduction may jeopardize penumbral perfusion (78, 79), while sustained hypertension elevates hemorrhagic transformation and reperfusion injury risks, particularly in thrombolysis recipients (80, 81). Large-scale trials (e.g., ENCHANTED, and BEST-II) comparing intensive versus standard BP strategies, have yielded inconclusive results (9–12) due to marked patient heterogeneity. Beyond CA impairment, BP regulation in AIS involves complex interactions among cerebral vasculature pathology, systemic hemodynamics, and endocrine responses, rendering conventional demographic-based stratification inadequate for capturing physiological and pathological variability. This underscores the necessity to transcend numerical BP targets by integrating individualized physiological profiling. Emerging frameworks, including TCM constitutional theory, may enhance precision in predicting antihypertensive responses and tailoring therapeutic strategies.
We therefore systematically investigated TCM constitutional distributions across relevant populations of AIS with hypertension to determine whether these patterns correlate with disease characteristics and therapeutic heterogeneity. Hypertensive and AIS populations share common constitutional patterns, with Phlegm-dampness, Yin-deficiency, Qi-deficiency, and Blood-stasis constitutions being the most prominent. In AIS/IS with hypertensive individuals, the overlap of constitutional profiles, dominated by Phlegm-dampness, Yin-deficiency, Qi-deficiency, and Blood-stasis constitutions, further underscores the shared pathophysiological mechanisms linking hypertension and AIS. These consistent patterns emphasize the fundamental role of the four TCM constitutions in AIS with hypertension, further large-scale studies are warranted to verify these findings. In contrast, the hypotensive population and those with ischemic cerebrovascular hypoperfusion display a unique constitutional distribution. While the Phlegm-dampness, Qi-deficiency, and Yin-deficiency constitutions remain prominent, the Yin-deficiency and Qi-deficiency constitutions are significantly more prevalent compared to normotensive individuals. This distinct constitutional divergence from hypertension and AIS profiles suggests a pathophysiological propensity toward hemodynamic instability, particularly manifesting as hypotension or ischemic cerebrovascular hypoperfusion in individuals with Yin-deficiency and Qi-deficiency constitutions.
The majority of included studies demonstrated moderate-to-high methodological quality as evaluated by standardized tools (AHRQ for cross-sectional studies and NOS for cohort/case–control studies). Subgroup analyses demonstrated that study design constituted a key source of heterogeneity; nevertheless, most subgroups consistently revealed that Phlegm-dampness, Blood-stasis, Qi-deficiency, and Yin-deficiency constitutions persisted as the predominant types across design categories. Sensitivity analyses employing leave-one-out cross-validation confirmed the robustness of primary findings. Publication bias assessments via funnel plots, Egger’s test, and Begg’s test indicated generally symmetrical distributions, with minimal evidence of bias for most constitutions. Where publication bias was detected (e.g., for Phlegm-dampness constitution in hypertensive population), trim-and-fill imputation demonstrated a negligible impact on the original effect sizes, reinforcing the robustness of the primary conclusions. Collectively, these analytical approaches substantiated the reliability and consistency of the identified TCM constitutional patterns underlying the proposed framework.
4.2 Targeted BP management in AIS with hypertension based on the TCM constitution
Extensive research has confirmed that distinct TCM constitutional types are associated with unique pathophysiological characteristics and prognostic implications, offering a framework for individualized BP management in AIS with hypertension. Patients with the Phlegm-dampness constitution often present with metabolic abnormalities such as hyperlipidemia and obesity, predisposing them to atherosclerosis (82–84) and elevating risks of BP irregularities and stroke. Mechanistic studies indicated intestinal microbiota imbalance (characterized by elevated Firmicutes/Bacteroidetes ratio), chronic inflammation, and metabolic dysregulation in these patients (85–88). These processes promoted vascular endothelial dysfunction (89), contributing to vascular-related diseases like hypertension and AIS. Regarding Blood-stasis constitution, several clinical studies revealed altered hemorheological parameters and heightened thrombogenic potential (37, 90), resulting in microcirculatory dysfunction and elevated vascular stenosis risk. Modern pathological studies further demonstrated that these abnormalities directly promote atherosclerosis, thrombosis, and endothelial dysfunction (91, 92). From a TCM perspective, both constitutions involve impeded circulation of Qi, blood, and fluids, leading to pathogenic accumulation within vessels. Consequently, elevated BP in these individuals may impose excessive mechanical stress on already compromised vasculature, significantly increasing the risk of acute vascular events, including plaque rupture, thrombosis, and recurrent stroke (93, 94). Intensive BP control may be warranted for patients with these constitutions to optimize cerebral hemodynamics and mitigate their inherently elevated stroke risk associated with vascular vulnerability.
Conversely, Qi-deficiency and Yin-deficiency constitutions pose unique challenges for BP regulation due to compromised autonomic function and diminished compensatory capacity. This renders patients highly susceptible to BP fluctuations and hypoperfusion events (38, 74, 76, 95). TCM pathology attributes Qi deficiency to the depletion of “vital energy” (Qi), manifesting as impaired functional activity that undermines blood circulation regulation. Yin deficiency, characterized by insufficient fluid nourishment, compromises vascular tone and perfusion pressure. Modern studies linked Qi-deficiency to cellular energy metabolism disorders (notably mitochondrial dysfunction) (96, 97), which impair adenosine triphosphate (ATP)-dependent vascular autoregulation and repair mechanisms. Yin deficiency was associated with chronic inflammation and oxidative stress (98, 99), exacerbating endothelial dysfunction and reducing vascular elasticity and reserve (100). These impairments weaken compensatory responses to BP fluctuations, increasing vulnerability to hypoperfusion, especially in critical organs like the brain. Consequently, a conservative BP management strategy may be more appropriate for them to avoid iatrogenic hypoperfusion while managing risks from sustained hypertension.
Taken together, these findings support a hypothesis for TCM constitution-targeted BP management in AIS patients. Patients with Phlegm-dampness or Blood-stasis constitutions, characterized by vascular stenosis, thrombosis propensity, and metabolic dysregulation, likely benefit from intensive BP control to reduce stroke recurrence risk (101). In contrast, those with Qi-deficiency or Yin-deficiency constitutions exhibit hemodynamic fragility and diminished vascular reserve, suggesting that more conservative BP management strategies could potentially be appropriate to help reduce the risk of hypoperfusion complications.
4.3 Challenges and opportunities for TCM constitution-based BP management
4.3.1 Limitations
The present meta-analysis provides novel insights into TCM constitution-based BP management in AIS. However, several limitations warrant consideration. Firstly, all studies originated from Chinese populations, potentially introducing cultural and regional biases that limit extrapolation to diverse ethnic groups. Secondly, the limited sample size, particularly for AIS patients with hypertension, underscores the need for larger, multicenter cohorts to validate these preliminary associations. Finally, many studies did not report data on associations between relevant factors (such as stroke subtypes) and TCM constitution distributions. This lack of data precluded subgroup analyses, thereby limiting our ability to perform more detailed characterization of population-specific constitutional profiles.
4.3.2 Clinical implications
The integration of TCM constitutional theory into AIS care might introduce a paradigm shift toward personalized BP management. By categorizing AIS patients into distinct constitutional profiles, such as Phlegm-dampness, or Qi-deficiency, clinicians might better predict hemodynamic vulnerabilities and therefore tailor different therapeutic strategies. This approach not only refines acute care protocols by aligning BP-lowering strategies but also enhances long-term secondary prevention through targeted interventions, such as lifestyle modifications. While rooted in TCM, this framework aligns with global precision medicine initiatives, offering a low-cost, non-invasive tool adaptable to diverse populations.
4.3.3 Future directions
To translate these findings into practice, the following priorities must be addressed: (1) Standardization: Developing internationally recognized criteria for TCM constitution classification, supported by objective biomarkers (e.g., inflammatory markers, hemodynamic parameters) to reduce subjectivity. (2) Mechanistic Exploration: Investigating the biological underpinnings of constitutional types using omics technologies (genomics, proteomics) to elucidate their interactions with cerebral autoregulation and BP homeostasis. (3) Interventional Trials: Designing adaptive trials comparing constitution-guided BP management versus standard care, with endpoints including functional outcomes, complication rates, and quality of life. Subgroup analyses should explicitly incorporate key clinical variables such as disease severity and stroke subtype to assess their association with the TCM constitution and evaluate the differential efficacy of intensive versus conservative strategies across constitutional profiles. (4) Global Collaboration: Establishing multinational registries to evaluate the cross-cultural applicability of TCM constitutional theory and address ethnic/geographic variability in stroke pathophysiology. (5) Technology Integration: Leveraging artificial intelligence to automate constitutional assessments using clinical, imaging, and laboratory data, thereby enhancing scalability and precision.
5 Conclusion
This study proposes a targeted BP management hypothesis for AIS patients by integrating TCM constitution theory with modern medical practices. Through systematic meta-analyses, we identified distinct constitutional patterns and their specific therapeutic requirements in AIS patients with hypertension. Our findings reveal that Phlegm-dampness and Blood-stasis constitutions may benefit from intensive BP management, while Qi-deficiency and Yin-deficiency constitutions may require conservative approaches. By addressing patient-specific needs, the study highlights the potential of integrating the TCM constitution and modern medicine to optimize recovery, lower stroke recurrence risk, and advance personalized healthcare.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XZ: Formal analysis, Methodology, Writing – original draft, Data curation, Conceptualization, Writing – review & editing, Investigation, Validation. KC: Conceptualization, Supervision, Writing – review & editing, Project administration, Funding acquisition. LZ: Conceptualization, Validation, Supervision, Writing – review & editing. JL: Writing – original draft, Investigation, Formal analysis, Data curation. YD: Software, Writing – original draft, Data curation, Methodology.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The work was funded by the Modernization of Traditional Chinese Medicine Special Project (2022YFC3501101), Capital’s Funds for Health Improvement and Research (2024-2-4193) and Dongzhimen Hospital Talent Cultivation Program (Grant Number: DZMG-LJRC0003). The sponsors were not involved in any aspect of the research design, data collection and analysis, manuscript preparation, revision, and publication decisions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1602274/full#supplementary-material
- AHRQ
Agency for Healthcare Research and Quality
- AIS
Acute Ischemic Stroke
- ATP
Adenosine Triphosphate
- BP
Blood Pressure
- CACM
China Association of Chinese Medicine
- CBM
China Biology Medicine
- CI
Confidence Interval
- CNKI
China National Knowledge Infrastructure
- IS
Ischemic Stroke
- LAA
Large Artery Atherosclerosis
- MeSH
Medical Subject Headings
- NIHSS
National Institutes of Health Stroke Scale
- NOS
Newcastle-Ottawa Scale
- NR
Not Reported
- N/A
Not Applicable
- OR
Odds Ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
Prospective Register of Systematic Reviews
- SAO
Small Artery Occlusion
- TCM
Traditional Chinese Medicine
Glossary
References
1.
Owolabi MO Thrift AG Mahal A Ishida M Martins S Johnson WD et al . Primary stroke prevention worldwide: translating evidence into action. Lancet Public Health. (2022) 7:e74–85. doi: 10.1016/S2468-2667(21)00230-9
2.
GBD 2019 Stroke Collaborators . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
3.
Qureshi AI Ezzeddine MA Nasar A Suri MF Kirmani JF Hussein HM et al . Prevalence of elevated blood pressure in 563,704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med. (2007) 25:32–8. doi: 10.1016/j.ajem.2006.07.008
4.
Gąsecki D Kwarciany M Kowalczyk K Narkiewicz K Karaszewski B . Blood pressure management in acute ischemic stroke. Curr Hypertens Rep. (2020) 23:3. doi: 10.1007/s11906-020-01120-7
5.
Willmot M Leonardi-Bee J Bath PM . High blood pressure in acute stroke and subsequent outcome: a systematic review. Hypertension. (2004) 43:18–24. doi: 10.1161/01.HYP.0000105052.65787.35
6.
Powers WJ Rabinstein AA Ackerson T Adeoye OM Bambakidis NC Becker K et al . Guidelines for the early Management of Patients with Acute Ischemic Stroke: 2019 update to the 2018 guidelines for the early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
7.
Sandset EC Anderson CS Bath PM Christensen H Fischer U Gąsecki D et al . European stroke organisation (ESO) guidelines on blood pressure management in acute ischaemic stroke and intracerebral hemorrhage. Eur Stroke J. (2021) 6:98. doi: 10.1177/23969873211026998
8.
Li G Zhao X . Interpretation of the 2023 Chinese guidelines for diagnosis and treatment of acute ischemic stroke. Chin J Stroke. (2024) 19:956–61.
9.
Green CR Hemphill JC . Blood pressure in acute stroke and secondary stroke prevention. Curr Neurol Neurosci Rep. (2022) 22:143–50. doi: 10.1007/s11910-022-01169-8
10.
Bath PM Song L Silva GS Mistry E Petersen N Tsivgoulis G et al . Blood pressure Management for Ischemic Stroke in the first 24 hours. Stroke. (2022) 53:1074–84. doi: 10.1161/STROKEAHA.121.036143
11.
Nam HS Kim YD Heo J Lee H Jung JW Choi JK et al . Intensive vs conventional blood pressure lowering after endovascular Thrombectomy in acute ischemic stroke: the OPTIMAL-BP randomized clinical trial. JAMA. (2023) 330:832–42. doi: 10.1001/jama.2023.14590
12.
Mistry EA Hart KW Davis LT Gao Y Prestigiacomo CJ Mittal S et al . Blood pressure management after endovascular therapy for acute ischemic stroke: the BEST-II randomized clinical trial. JAMA. (2023) 330:821–31. doi: 10.1001/jama.2023.14330
13.
Wang Q . Discussion on three key issues in TCM constitution research (part 1). J Tradit Chin Med. (2006) 4:250–2. doi: 10.13288/j.11-2166/r.2006.04.003
14.
CAoTC . Classification and determination of traditional Chinese medicine constitution (ZYYXH/T157-2009). World J Integr Tradit West Med. (2009) 4:303–4.
15.
Rostom A Dubé C Cranney A Garritty NSC Sampson M . Celiac disease. Rockville, MD: Agency for Healthcare Research and Quality (2004).
16.
Stang A . Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
17.
Ye Y Wang Y Li S Guo J Ding L Liu M . Association of Hypothyroidism and the risk of cognitive dysfunction: a Meta-analysis. J Clin Med. (2022) 11:6726. doi: 10.3390/jcm11226726
18.
Qi X Qiu L Wang S Chen X Huang Q Zhao Y et al . Non-thyroidal illness syndrome and the prognosis of heart failure: a systematic review and meta-analysis. Endocr Connect. (2023) 12:e230048. doi: 10.1530/EC-23-0048
19.
Jin ZC Zhou XH He J . Statistical methods for dealing with publication bias in meta-analysis. Stat Med. (2015) 34:343–60. doi: 10.1002/sim.6342
20.
Shi L Lin L . The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine (Baltimore). (2019) 98:e15987. doi: 10.1097/MD.0000000000015987
21.
Li B. (2021) Study on the correlation of early cognitive impairment with traditional Chinese medicine constitution and syndrome types in patients with acute ischemic stroke. Nanjing: Nanjing University of Traditional Chinese Medicine
22.
Cai B. (2020) Study on the correlation between treatment outcomes of acute cerebral infarction and traditional Chinese medicine constitution types and risk factors. Changsha: Hunan University of Traditional Chinese Medicine.
23.
Liu F Zhou D He H . Study on the correlation between recurrence and traditional Chinese medicine constitution in patients with ischemic stroke. World Chin Med. (2017) 12:1014–7.
24.
Yang F . Study on a predictive model for recurrence risk of acute cerebral infarction based on the distribution of traditional Chinese medicine constitution. Jinan: Shandong University of Traditional Chinese Medicine (2023).
25.
Yang G . Study on the correlation between common traditional Chinese medicine constitution types and syndromes in ischemic strokeHenan University of Traditional Chinese Medicine (2009).
26.
Zhang H Zhang Y Guo D Hu W Cheng Z . Study on the clinical characteristics of ischemic stroke patients with different constitution types. Liaoning J Tradit Chin Med. (2010) 37:1409–12.
27.
Zhou H Ma Z Zhou D Deng Y . Study on the correlation between traditional Chinese medicine constitution and risk factors in 303 patients with acute cerebral infarction. J Hunan Univ Tradit Chin Med. (2020) 40:54–8.
28.
Yuan J . Study on the correlation between risk factors of cerebral infarction in elderly patients and traditional Chinese medicine constitution. Jinan: Shandong University of Traditional Chinese Medicine (2021).
29.
Huang L. (2019) Study on the correlation of constitution, syndromes, and APOE gene polymorphism in patients with acute ischemic stroke. Nanchang: Jiangxi University of Traditional Chinese Medicine
30.
Li L . Study on the correlation between lesion locations on head MRI and constitution in acute cerebral infarction based on association rules. Changchun: University of Traditional Chinese Medicine (2018).
31.
Wang Q . Study on the relationship between syndrome types and constitution classification in acute ischemic stroke. Jinan: Shandong University of Chinese Medicine (2012).
32.
Li R . Study on the distribution of traditional Chinese medicine constitution and inflammatory factors in patients with acute ischemic stroke. Jinan: Shandong University of Traditional Chinese Medicine (2023).
33.
Cui S . Clinical study on the correlation between traditional Chinese medicine constitution, CISS etiological classification, and Apo E polymorphism in cerebral infarction. Jinan: Shandong University of Chinese Medicine (2018).
34.
Shi S . Study on the correlation between progressive ischemic stroke and traditional Chinese medicine constitution and its risk factors. Jinan: Shandong University of Traditional Chinese Medicine (2022).
35.
Liu X. (2016) Study on the correlation between traditional Chinese medicine constitution and short-term prognosis in patients with ischemic stroke. Beijing: Beijing University of Traditional Chinese Medicine.
36.
Zhen X Chen X Guo D Zhang H Ma J Zhang Y . Study on the correlation between traditional Chinese medicine constitution and ischemic stroke. J Emerg Tradit Chin Med. (2015) 24:650–2.
37.
Fu X . Correlation analysis between TCD changes and constitution in patients with acute ischemic stroke. Changchun: Changchun University of Chinese Medicine (2018)
38.
Qiu X . Study on the correlation between 3D-ASL perfusion imaging and the distribution of traditional Chinese medicine constitution in patients with acute cerebral infarction. Chengdu: Chengdu University of Traditional Chinese Medicine (2021).
39.
Yan Y . Study on the correlation between constitution and brain MRI in acute ischemic stroke. Jinan: Shandong University of Traditional Chinese Medicine (2021).
40.
Gao Y. (2022) The correlation study of serum inflammatory factors IL-6, TNF-α, CRP, and traditional Chinese medicine constitution on the prognosis of acute ischemic stroke. Zhengzhou: Henan University of Traditional Chinese Medicine.
41.
Liang Y Liang Y Feng M . Study on the correlation between traditional Chinese medicine constitution types and the recurrence of ischemic stroke. Shenzhen J Integr Tradit Chin West Med. (2018) 28:52–4.
42.
Xu Y Yu C Shen B . Investigation on the distribution patterns of traditional Chinese medicine constitution in 500 patients with acute ischemic stroke in Pinggu District, Beijing. Beijing J Tradit Chin Med. (2015) 34:1.
43.
Li Y Song Y Y Y . A study on the TCM constitution types in 178 elderly patients with ischemic stroke. J Yunnan Univ Tradit Chin Med. (2015) 38:62–76.
44.
Dong Y. (2019) Study on the correlation between clinical risk factors and phlegm-dampness constitution in patients with LAA-type ischemic stroke. Hohhot: Inner Mongolia Medical University.
45.
Zhang Y Yan F Long X Chen X Ma J . Comparison of traditional Chinese medicine constitution between high-risk and low-risk patients with recurrent ischemic stroke. J Emerg Tradit Chin Med. (2014) 23:846–8.
46.
Zou Z Zeng Z Zhong X Meng X . Study on lipoprotein (a) and traditional Chinese medicine constitution identification in patients with acute cerebral infarction and high-risk stroke populations. China Pract Med. (2020) 15:143–6.
47.
Li Z Huang H . Study on the correlation between traditional Chinese medicine constitution and plasma homocysteine and fibrinogen in patients with acute stroke. J Sichuan Trad Chinese Med. (2017) 35:64–6.
48.
Li Z Wang Q Wu Y Ni J Xue G Sun H et al . Study on the correlation between traditional Chinese medicine syndromes and constitution identification in 200 patients with acute ischemic stroke (meridian). Clin J Chin Med. (2016) 8:15–7.
49.
Zeng Y Liang H Jian W Liu W Hu Z . Meta-analysis on the correlation between hypertension and traditional Chinese medicine constitution. Modern Trad Chinese Med Mater. (2019) 21:1731–7.
50.
Li H Zhang R Yang Q Xie Y Yu B Xie R . Meta-analysis of the association between TCM constitution types and hypertension. J Jining Med Univ. (2020) 43:54–8.
51.
Lin B Lu X Y W . A study on the distribution characteristics of TCM constitution types in patients with primary hypertension in Luzhou area. Integr Trad Chinese Wes Med Nurs. (2019) 5:45–9.
52.
Yang F Tan H Peng Y Wang P . Analysis of the correlation between body mass index, TCM constitution, and hypertension in the elderly. Integr Trad Chinese Western Med Res. (2024) 16:1–5.
53.
Li H. (2022) Analysis of the distribution pattern of TCM constitution types and the correlation with risk factors in elderly hypertensive patients in the suburban areas of Zhengzhou. Zhengzhou: Henan University of Traditional Chinese Medicine.
54.
Xiao J Geng S Su D Cui Y Cheng Y Shi F et al . Analysis of the factors influencing TCM constitution in elderly hypertensive patients in Xinzheng City. Res Orient Hosp China. (2023) 10:45–9.
55.
Lin J Zhang L B L . Epidemiological study on the heredity of TCM constitution in hypertension. J China Prescript Drug. (2021) 19:126–8.
56.
Chen L . A survey and analysis of TCM constitution in patients with primary hypertension in Sixian community, Qingxiu district, Nanning city. Sci Health. (2023) 2:125–8.
57.
Zhang M. (2019) Study on the correlation between hypertension, multiple risk factors, and TCM constitution types in middle-aged and young adults. Beijing: Beijing University of Traditional Chinese Medicine.
58.
Jin S . Study on the association between hypertension and TCM constitution in community populations. Suzhou: Soochow University (2019).
59.
Fan S Chen H Chen S Hong J Hou X Yang Y . The correlation between TCM constitution types and primary hypertension in Sanshui District. Smart Healthcare. (2020) 6:178–80.
60.
Zhang X . Investigation of TCM constitution in elderly residents of Shuangzhao subdistrict, Xianyang city, and analysis of the therapeutic effects of constitution-based intervention for phlegm-dampness hypertension. Xianyang: Shaanxi University of Chinese Medicine (2022).
61.
Wang X S H . Study on the physical characteristics of elderly residents in the community and their correlation with hypertension. J Jiangxi Univ Tradit Chin Med. (2023) 35:53–6.
62.
Gao Y Wang Y Y S . Study on the correlation between TCM constitution types and elderly primary hypertension based on logistic regression analysis. Special Health. (2022) 14:94–6.
63.
Li Y. (2019) Study on the distribution of TCM constitution and related factors in hypertension patients based on regression analysis. Nanning: Guangxi University of Traditional Chinese Medicine.
64.
Li J. (2020) Distribution of traditional Chinese medicine constitution and analysis of risk factors in patients with acute ischemic stroke combined with hypertension. Jinan: Shandong University of Traditional Chinese Medicine.
65.
Yu H Shao H Gong M . Investigation and analysis of constitution in 252 patients with cerebral infarction during rehabilitation. Pract Med J. (2018) 35:152–4.
66.
Wang H . Clinical study on traditional Chinese medicine constitution in patients with ischemic stroke in Shijiazhuang region. Zhangjiakou: Hebei North University (2018).
67.
Wang K . Investigation and analysis of traditional Chinese medicine constitution types in 78 patients with cerebral infarction. Wuhan: Hubei University of Chinese Medicine (2012).
68.
Li K. (2019) Study on the adherence to ASA treatment regimen and analysis of traditional Chinese medicine constitution in patients with recurrent cerebral infarction. Wuhan: Hubei University of Traditional Chinese Medicine.
69.
Li Q . Cerebral infarction (stroke-meridian) and TCM constitution correlation analysis. Xianyang: Shaanxi University of Chinese Medicine (2016).
70.
Han S. (2012) Study on the characteristics of traditional Chinese medicine constitution types in patients with hypertension and comorbid stroke. Fuzhou: Fujian University of Traditional Chinese Medicine.
71.
Song T (2023) A cross-sectional study on traditional Chinese medicine etiology and constitution characteristics in patients with asymptomatic cerebral infarction. Zhengzhou: Henan University of Traditional Chinese Medicine.
72.
Wu X. (2018) Study on the current status of secondary prevention of stroke and traditional Chinese medicine constitution based on a healthy rural demonstration community in Beijing. Beijing: Beijing University of Traditional Chinese Medicine.
73.
Liu Q. (2018) Analysis of pulse frequency domain characteristics in prehypertensive individuals in Hunan region. Changsha: Hunan University of Traditional Chinese Medicine.
74.
Wang X Miao Q . Study on the correlation between primary hypotension and traditional Chinese medicine constitution. Shaanxi J Tradit Chin Med. (2015) 36:44–6.
75.
Zhang Z. (2021) Study on the relationship among immune mechanisms, cytokines, blood pressure, traditional Chinese medicine syndromes, and constitution in patients with primary hypotension. Chengdu: Chengdu University of Traditional Chinese Medicine.
76.
Chen Z. Correlation study between 3D-ASL imaging features of chronic cerebral ischemia and traditional Chinese medicine constitution types. Chengdu: Chengdu University of Traditional Chinese Medicine (2023).
77.
Bulwa Z Gomez CR Morales-Vidal S Biller J . Management of Blood Pressure after Acute Ischemic Stroke. Curr Neurol Neurosci Rep. (2019) 19:29. doi: 10.1007/s11910-019-0941-z
78.
Nogueira RC Beishon L Bor-Seng-Shu E Panerai RB Robinson TG . Cerebral autoregulation in ischemic stroke: from pathophysiology to clinical concepts. Brain Sci. (2021) 11:511. doi: 10.3390/brainsci11040511
79.
Dawson SL Panerai RB Potter JF . Serial changes in static and dynamic cerebral autoregulation after acute ischaemic stroke. Cerebrovasc Dis. (2003) 16:69–75. doi: 10.1159/000070118
80.
Waltimo T Haapaniemi E Surakka IL Melkas S Sairanen T Sibolt G et al . Post-thrombolytic blood pressure and symptomatic intracerebral hemorrhage. Eur J Neurol. (2016) 23:1757–62. doi: 10.1111/ene.13118
81.
Zubair AS Sheth KN . Hemorrhagic conversion of acute ischemic stroke. Neurotherapeutics. (2023) 20:705–11. doi: 10.1007/s13311-023-01377-1
82.
Zhai C Rong C Liu L Zhao D . Study on the correlation between atherosclerotic plaques and traditional Chinese medicine constitution. Jilin J Chin Med. (2020) 40:910–2.
83.
Wu J. (2019) Analysis of risk factors, traditional Chinese medicine constitution, and syndrome elements in patients with symptomatic vertebrobasilar atherosclerotic stenosis. Wuhan: Hubei University of Traditional Chinese Medicine.
84.
Luo H Wang Q . Systematic review and meta-analysis of the association between TCM constitution types and metabolic syndrome. J Beijing Univ Tradit Chin Med. (2016) 39:325–34.
85.
Li L Li T Liang X Zhu L Fang Y Dong L et al . A decrease in Flavonifractor plautii and its product, phytosphingosine, predisposes individuals with phlegm-dampness constitution to metabolic disorders. Cell Discov. (2025) 11:25. doi: 10.1038/s41421-025-00789-x
86.
Liu Y Sun Z Dong R . Rutin ameliorated lipid metabolism dysfunction of diabetic NAFLD via the AMPK/SREBP1 pathway. Phytomedicine. (2024) 126:155437. doi: 10.1016/j.phymed.2024.155437
87.
Huang L Rao Q Wang C Mou Y Zheng X Hu E et al . Multi-omics joint analysis reveals that the Miao medicine Yindanxinnaotong formula attenuates non-alcoholic fatty liver disease. Phytomedicine. (2024) 135:156026. doi: 10.1016/j.phymed.2024.156026
88.
Duan Y Guo F Li C Xiang D Gong M Yi H et al . Aqueous extract of fermented Eucommia ulmoides leaves alleviates hyperlipidemia by maintaining gut homeostasis and modulating metabolism in high-fat diet-fed rats. Phytomedicine. (2024) 128:155291. doi: 10.1016/j.phymed.2023.155291
89.
Linghui Z Ziwei S Yuanyuan G Meiyi L Yi Z Ruoxi YU et al . Differences in vascular endothelial function and serum proteome between obese people with phlegm-dampness constitution and balanced constitution. J Tradit Chin Med. (2024) 44:188–96. doi: 10.19852/j.cnki.jtcm.20231110.005
90.
Guo X Liu Y Yang Q Wang Q Li Z Wan L et al . Meta-analysis of the correlation between TCM constitution types and ischemic stroke. Clin J Chin Med. (2021) 13:129–33.
91.
Bochenek ML Schäfer K . Role of endothelial cells in acute and chronic thrombosis. Hamostaseologie. (2019) 39:128–39. doi: 10.1055/s-0038-1675614
92.
Badimon L Vilahur G Rocca B Patrono C . The key contribution of platelet and vascular arachidonic acid metabolism to the pathophysiology of atherothrombosis. Cardiovasc Res. (2021) 117:2001–15. doi: 10.1093/cvr/cvab003
93.
Gao F Liang N Chen J Yu S . Clinical distribution characteristics and risk factor analysis of traditional Chinese medicine constitution in 237 patients with recurrent cerebral infarction. Inner Mongolia J Tradit Chin Med. (2023) 42:135–8.
94.
Wang G Xie Y Yi D Zhang Y Gao Y Li Y et al . Study on the establishment of a constitution-based risk assessment model for ischemic stroke recurrence. China J Tradit Chin Med Pharm. (2019) 34:4860–6.
95.
Luo H Li L Wang Q . Correlation between Qi-deficiency constitution and diseases: a bibliometric analysis of 332 clinical studies. Tianjin J Tradit Chin Med. (2019) 36:625–30.
96.
Tran MN Kim S Nguyen QHN Lee S . Molecular mechanisms underlying Qi-invigorating effects in traditional medicine: network pharmacology-based study on the unique functions of Qi-invigorating Herb Group. Plants. (2022) 11:2470. doi: 10.3390/plants11192470
97.
Liu WJ Xu XZ Duan ZY Liang XC Ma D Li GG et al . Efficacy of Sijunzi decoction on limb weakness in spleen Qi deficiency model rats through adenosine monophosphate-activated protein kinase/unc-51 like autophagy activating kinase 1 signaling. J Tradit Chin Med. (2021) 41:617–23. doi: 10.19852/j.cnki.jtcm.2021.03.014
98.
Li J Zhai Y Cao Y Xia Y Yu R . Development of an interpretable machine learning model associated with genetic indicators to identify yin-deficiency constitution. Chin Med. (2024) 19:71. doi: 10.1186/s13020-024-00941-x
99.
Zhang C Tam CW Tang G Chen Y Wang N Feng Y . Spatial transcriptomic analysis using R-based computational machine learning reveals the genetic profile of Yang or yin deficiency syndrome in Chinese medicine theory. Evid Based Complement Alternat Med. (2022) 2022:5503181. doi: 10.1155/2022/5503181
100.
Higashi Y . Roles of oxidative stress and inflammation in vascular endothelial dysfunction-related disease. Antioxidants. (2022) 11:1958. doi: 10.3390/antiox11101958
101.
Bergmann F Prager M Pracher L Sawodny R Steiner-Gager GM Richter B et al . Systolic blood pressure targets below 120 mm hg are associated with reduced mortality: a meta-analysis. J Intern Med. (2025) 297:479–91. doi: 10.1111/joim.20078
Summary
Keywords
acute ischemic stroke, blood pressure management, TCM constitution, personalized medicine, hypothesis and theory
Citation
Zhang X, Cao K, Zhou L, Liu J and Ding Y (2025) Bridging tradition and innovation: a constitution-guided framework for personalized blood pressure management in acute ischemic stroke. Front. Med. 12:1602274. doi: 10.3389/fmed.2025.1602274
Received
22 April 2025
Accepted
12 June 2025
Published
02 July 2025
Volume
12 - 2025
Edited by
Thao Thi Phuong Nguyen, Vinmec Research Institute of Stem Cell and Gene Technology, Vietnam
Reviewed by
Vu Kim-Duy, Hanoi Medical University, Vietnam
Rui Fang, Hunan Academy of Chinese Medicine, China
Yufei Wei, Capital Medical University, China
Updates
Copyright
© 2025 Zhang, Cao, Zhou, Liu and Ding.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kegang Cao, bucm123@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.