- Department of Vascular Surgery, The Second Affiliated Hospital of Xi'an Jiaotong University, Xi'an, Shaanxi, China
The recent research entitled “Trends and benefits of early hip arthroplasty for femoral neck fracture in China: a national cohort study” demonstrates the great clinical benefit of early total hip arthroplasty (THA) in elderly patients with femoral neck fractures (FNFs) (1). In particular, early THA gains distinctly competitive advantages over delayed surgery in the field of the prevention of pulmonary embolism (PE) and deep vein thrombosis (DVT). Unfortunately, according to the data from Chinese national electronic inpatient database, <20% of patients received early THA therapy. Nonetheless, delayed THA does not mean the catastrophic outcomes. Based on the perspective of vascular surgery, we argue that the preoperatively accurate assessment of venous thromboembolism (VTE) risk and reasonable strategy of DVT prevention will greatly reduce the risk of PE and DVT in patients receiving delayed THA, thereby mitigating the adverse effects brought by delayed surgery (Figure 1).
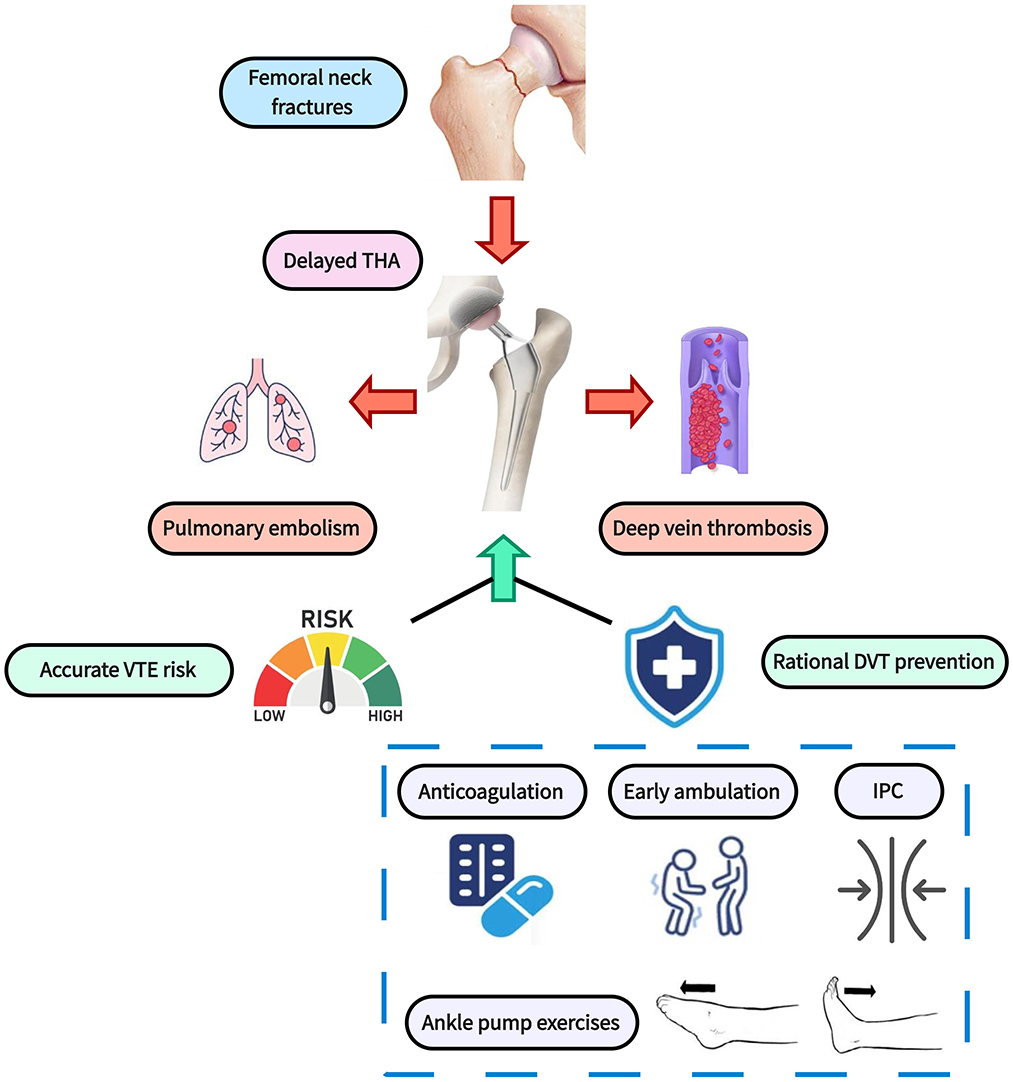
Figure 1. Perioperative rational thromboprophylaxis strategy for patients receiving delayed THA. THA, total hip arthroplasty; VTE, venous thromboembolism; DVT, deep vein thrombosis; IPC, intermittent pneumatic compression.
Emphasize preoperative VTE risk assessment
PE and DVT are crucial factors that affect the prognosis of FNFs patients. According to statistics, over 9.4% of inpatients are accompanied by DVT and thus face the threat of PE. Therefore, it is important to conduct timely and precise assessments of VTE risk and use it as the foundation for developing a reasonable prevention program. There are two critical decision points in this procedure. First, Caprini score should be performed on all FNFs patients prior to surgery. Currently, this grading scale is the most commonly used system for assessing thrombotic risk in surgical inpatients, with higher scores denoting greater DVT risks (2). Luksameearunothai et al. (3) demonstrated that FNFs patients with a Caprini score higher than 12 had a 7.56 times greater risk of DVT than patients with a score lower than 12. For elderly FNFs patients, they are commonly concomitant with advanced age (2 points), prolonged immobilization (2 points), long operation time (2 points), and broken hip or pelvis (5 points), totaling 11 points. Therefore, patients require extra concern when they simultaneously present with other common risk factors, such as obesity, chronic obstructive pulmonary disease, active cancer, atrial fibrillation, and varicose veins in the lower extremities, as these cases would have the scores >12. These patients should be defined as high-risk for VTE and appropriate thrombus prophylaxis needs to be taken into account.
Secondly, greater focus should be placed on the dynamic assessment and re-scoring of patients with delayed THA. The alterations of D dimer, leg circumference, and respiratory status of FNFs patients, especially for those receiving delayed surgery, deserve extra attention. For instance, if a patient manifests with a high or persistently elevated D dimer level during waiting times to surgery, prompt anticoagulation is generally beneficial. Recently, Li et al. (4) developed a model based on D-dimer levels and platelet distribution width for predicting the incidence of DVT in patients with femoral neck. In this predictive model, the odd ratio (OR) of high D-dimer levels (Age*0.02 mg/L) was as high as 2.718, highlighting the potential significance of early anticoagulant interventions.
Preoperative reasonable DVT prophylaxis
Anticoagulation is fundamental and critical to DVT prevention. Nevertheless, balancing the benefits of anticoagulation and the risk of bleeding in clinical practice remains a challenging endeavor. As for patients with high risk for VTE, preoperative anticoagulation is commonly safe and essential. For instance, the 2024 edition of the guideline for perioperative cardiovascular management for non-cardiac surgery based on American Heart Association pinpoints that patients with high risk for thrombotic complications should be treated with preoperative bridging of anticoagulant therapy (5). Moreover, a study from Mayo Clinic revealed that only 0.3% of surgical patients who received preoperative anticoagulation suffered from fatal bleeding events (6). Of course, the risk of bleeding associated with anticoagulation is an issue that cannot be ignored. Although controversial, a study indicated that perioperative antithrombotic drugs had a greater than two-fold increased likelihood of developing a significant postoperative bleed (7). Therefore, the development of an anticoagulation regimen for patients receiving delayed THA should be based on an accurate VTE risk assessment, and multidisciplinary collaboration from vascular surgery is particularly important.
Notably, except for anticoagulant therapy, early ambulation, ankle pump exercises, and intermittent pneumatic compression (IPC) are also essential parts for DVT prevention. For instance, a meta-analysis confirmed that although IPC combined with pharmacologic prophylaxis was not more preferable in DVT prevention than single pharmacologic prophylaxis, was superior in bleeding prevention (OR = 0.17). These non-anticoagulant approaches are especially important for patients with a high risk of bleeding (8).
Conclusions
Due to insufficient healthcare resources and the limitations of medical technology, most elderly patients with FNFs in China are unable to receive THA intervention at the early stage, and delayed treatment exposes these patients to the threat of DVT and PE, which greatly and adversely affects the prognosis of these elderly trauma patients. Faced with this grim situation, timely and accurate VTE risk assessment and a rational anticoagulation prophylaxis regimen based on it will hopefully alleviate the thrombotic risk associated with delayed THA.
Author contributions
FX: Funding acquisition, Visualization, Writing – original draft, Writing – review & editing. ZL: Writing – original draft. HG: Writing – original draft. JM: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Natural Science Foundation of Shaanxi Province (S2024-JC-QN-1771).
Acknowledgments
All authors would like to thank Second Affiliated Hospital of Xi'an Jiaotong University for its support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang Y, Jiang Q, Long H, Chen H, Wei J, Li X, et al. Trends and benefits of early hip arthroplasty for femoral neck fracture in China: a national cohort study. Int J Surg. (2024) 110:1347–55. doi: 10.1097/JS9.0000000000000794
2. Cronin M, Dengler N, Krauss ES, Segal A, Wei N, Daly M, et al. Completion of the Updated Caprini Risk Assessment Model (2013 Version). Clin Appl Thromb Hemost. (2019) 25:1076029619838052. doi: 10.1177/1076029619838052
3. Luksameearunothai K, Sa-Ngasoongsong P, Kulachote N, Thamyongkit S, Fuangfa P, Chanplakorn P, et al. Usefulness of clinical predictors for preoperative screening of deep vein thrombosis in hip fractures. BMC Musculoskelet Disord. (2017) 18:208. doi: 10.1186/s12891-017-1582-5
4. Li Y, Cao P, Zhu T, Wang Y, Wang F, Li L, et al. Combination of age-adjusted d-dimer, platelet distribution width and other factors predict preoperative deep venous thrombosis in elderly patients with femoral neck fracture. BMC Surg. (2024) 24:426. doi: 10.1186/s12893-024-02724-5
5. Thompson A, Fleischmann KE, Smilowitz NR, de Las Fuentes L, Mukherjee D, Aggarwal NR, et al. 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM guideline for perioperative cardiovascular management for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. (2024) 84:1869–969.
6. Zhang C, Bews K, Klemen ND, Etzioni D, Habermann EB, Thiels C. Thrombotic and hemorrhagic outcomes after elective surgery in preoperatively anticoagulated patients. Mayo Clinic Proceed. (2024) 99:1038–45. doi: 10.1016/j.mayocp.2023.12.010
7. Wiegmann AL, Khalid SI, Coogan AC, Xu TQ, DeCesare LA, Skertich NJ, et al. Antithrombotic prescriptions for many general surgery patients significantly increases the likelihood of post-operative bleeding complications. Am J Surg. (2020) 219:453–9. doi: 10.1016/j.amjsurg.2019.10.001
Keywords: femoral neck fracture, total hip arthroplasty, deep vein thrombosis, venous thromboembolism, anticoagulation
Citation: Xu F, Li Z, Guan H and Ma J (2025) Perioperative rational thromboprophylaxis strategy contributes to reduce adverse clinical effects of delayed total hip arthroplasty. Front. Med. 12:1602605. doi: 10.3389/fmed.2025.1602605
Received: 31 March 2025; Accepted: 04 June 2025;
Published: 04 July 2025.
Edited by:
Stefano Marco Paolo Rossi, Fondazione Poliambulanza Istituto Ospedaliero, ItalyReviewed by:
Corrado Ciatti, Guglielmo da Saliceto Hospital, ItalyCopyright © 2025 Xu, Li, Guan and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiancang Ma, bWFqaWFuY2FuZ3hqdHVAMTYzLmNvbQ==
 Fangshi Xu
Fangshi Xu Zongyu Li
Zongyu Li Jiancang Ma
Jiancang Ma