- 1Faculty of Mathematics and Computer Science, University of Bremen, Bremen, Germany
- 2Lebanese American University Medical Center –Rizk Hospital, Beirut, Lebanon
- 3Faculty of Medicine of Tishreen University, Latakia, Syria
Cervicovaginal anomalies are rare and form 4–7% of the Müllerian anomalies. Traditionally, cervicovaginal agenesis/dysgenesis had been treated by hysterectomy due to the high risks of restenosis and sepsis which are associated with cervical canalization. In this work, we report the case of a 14-year-old patient who presented with amenorrhea and cyclic abdominal pain. The patient had normal secondary sexual development. Magnetic resonance imaging revealed hematometra and bilateral hematosalpinx. Laparoscopic exploration identified an obstructed cervix and blunt vagina. The patient underwent direct cervicovaginal anastomosis under laparoscopic guidance. After 1 month of follow-up, the patient had normal menstruation and a healthy uterine cavity and cervical canal upon hysteroscopy.
1 Introduction
The Müllerian anomalies are relatively rare with a prevalence of 1 per 4,000–10,000 women (1). Cervicovaginal anomalies, on the other hand, are an even rarer subtype of the Müllerian malformations with a reported prevalence between 4–7% (2). The cervicovaginal anomalies result from a defective lengthening or vacuolization of the Müllerian ducts (3, 4). On this basis, Cervicovaginal anomalies are broadly classified into cervical agenesis and cervical dysgenesis (5). Cervical agenesis refers to the complete absence of the uterine cervix and cervical canal, whereas cervical dysgenesis refers to the presence of an abnormal cervix or cervical canal. Cervical dysgenesis is further subclassified into 4 subtypes, these are namely: cervical obstruction, a cervical body consisting of a fibrous band, cervical fragmentation, and stricture of the mid-portion of the uterine cervix (6). It is noteworthy that vaginal aplasia coexists with cervicovaginal anomalies in nearly 39% of cases (7).
Affected patients typically present with primary amenorrhea and cyclic abdominal pain (4). Such cases were classically treated by hysterectomy due to the high complication rate of cervical drilling and the associated morbidity and mortality risks (8). However, a general tendency to adopt conservative management strategies has been observed in recent years due to the increased experience with and improved technologies of laparoscopic surgery (9, 10). Uterovaginal and utero-vestibular anastomosis are conservative reconstructive procedures that aim to restore the continuity of the reproductive tract via direct suturing (4). In this case, we demonstrate the surgical management of an adolescent with cervicovaginal dysgenesis along with her follow-up results.
2 Case description
A 14-year-old adolescent girl presented with primary amenorrhea and cyclic abdominal pain. The gynecologic examination revealed normally developed external genitalia and a partially aplastic vagina measuring 4 cm in length and 2 cm in width. Magnetic resonance imaging (MRI) revealed an enlarged uterus with hematometra and bilateral hematosalpinx (Figure 1). The radiologists were unable to decide on the presence or absence of the cervical tissue based on the MRI images. The MRI did not show any urologic abnormality. After careful discussion with the patient and her parents, the patient was scheduled to undergo laparoscopic surgery to better assess her condition and treat the underlying obstructive anomalies.
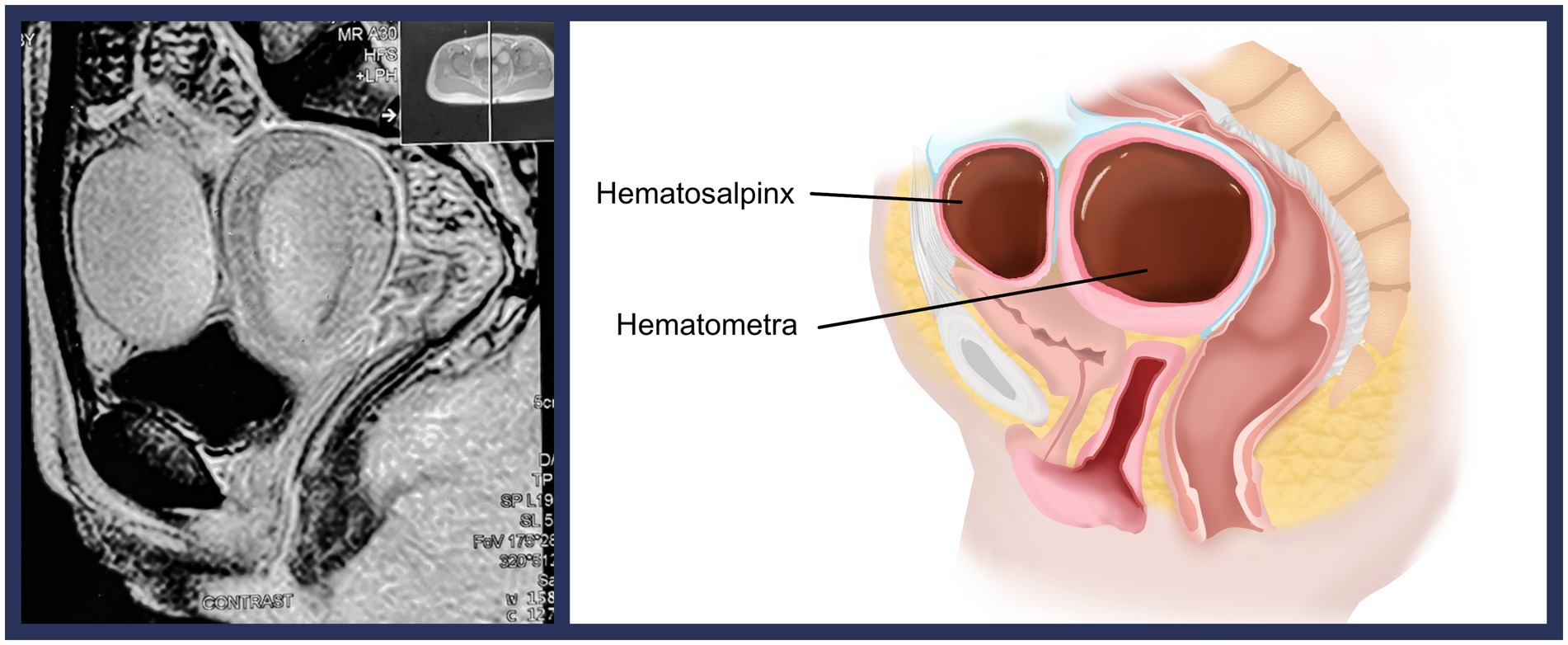
Figure 1. Magnetic resonance imaging demonstrating the hypertrophic uterus with the hematometra and the left hematosalpinx (left). Additionally, a visual demonstration of the malformation is presented (right).
The patient was placed in the dorsal lithotomy position. Under general anesthesia and after achieving proper intra-abdominal pressure, standard trocar placement took place. A 12-mm umbilical trocar for the laparoscope and two working 10-mm trocars at the level of the anterior superior iliac spines were placed via the direct entry method.
Initial exploration of the pelvic cavity revealed bilateral hematosalpinx. Moreover, the cervical tissue could be observed but it was discontinued with the vagina. Endometriosis lesions and intrapelvic adhesions were absent.
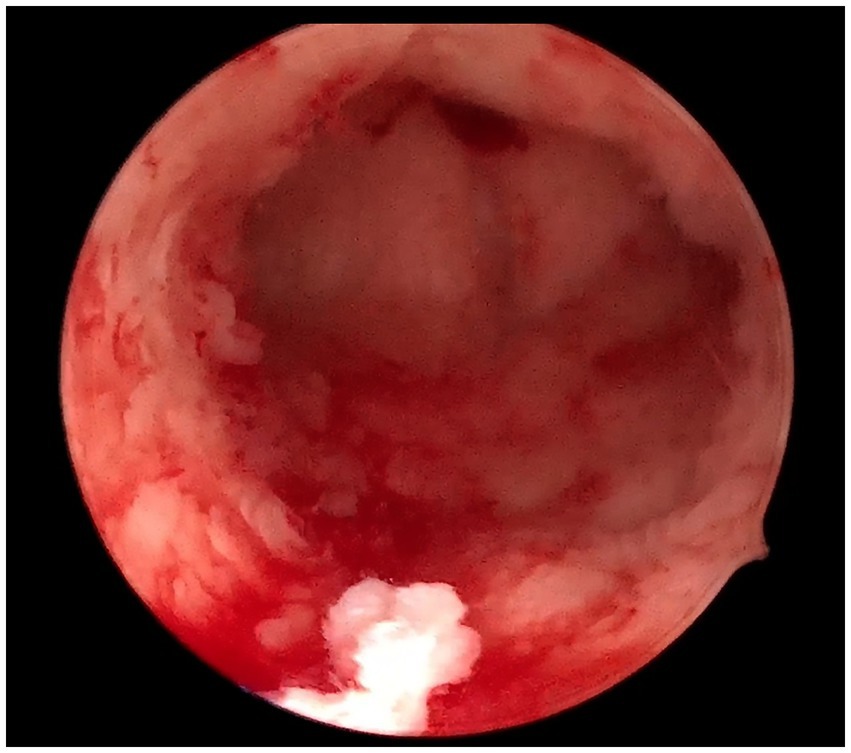
Firstly, bilateral salpingectomies were performed laparoscopically. To minimize bleeding, bilateral clipping of the uterine arteries was done. Afterward, the uterine fundus was incised vertically with a monopolar hook. The hematometra was drained using the suction cannula. Under laparoscopic guidance, the cannula was driven through the endocervical canal toward the vaginal dome. This step aims to better identify the uterovaginal axis and canalize the obstructed endocervical canal. The cannula was palpated transvaginally at the top of the vaginal dome, where a small horizontal incision was made. The uterine cervix was dilated gradually with Hegar dilators until a dilator size of 8 was reached. The uterine cervix was then sutured to the vagina with 2–0 Vicryl stitches. Thereafter, a 17F Foley catheter was introduced to the uterine cavity in the railroad fashion. Eventually, the hysterotomy incision was closed and the uterine arteries were unclipped. The surgical procedure is summarized in Figure 2 and detailed with a video footage in Supplementary Video 1. No intra-or postoperative complications occurred. The intrauterine catheter was kept for 2 weeks to prevent cervical stenosis. After 4 weeks of the initial operation, an exploratory hysteroscopy revealed a healthy cervical canal and uterine cavity. In addition, the patient had normal menstruation by the time of follow-up, and she was symptom-free (Figure 3).
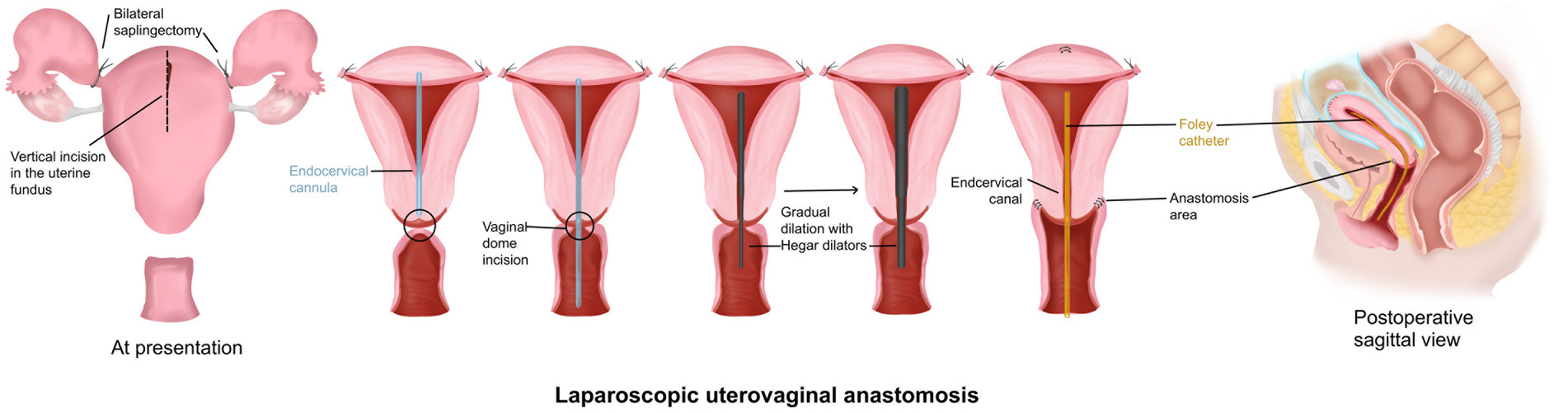
Figure 2. Laparoscopy-assisted uterovaginal anastomosis. A summary of the key surgical steps is illustrated.
3 Discussion
We presented a case of cervical atresia and partial vaginal aplasia in a 14-year-old patient. The patient was managed laparoscopically with a uterine-sparing reconstructive technique. At follow-up, the patient was symptom-free with an anatomically normal uterine cavity. In our opinion, successful management of cervicovaginal anomalies should relieve the patient’s symptoms and restore the continuity between the uterine cavity, cervical canal, and vagina in order to preserve the patient’s fertility. Nevertheless, an early diagnosis is crucial to achieve a successful surgical outcome and to avoid the psychological burden of this entity on the patient. A recent study by Liu et al. (11) demonstrated that half of the patients with cervicovaginal malformations suffer from depressive symptoms and 58.7% of them exhibit anxiety symptoms. This study also revealed that patients with depression were older and had longer preoperative pain periods compared to non-depressed patients, which encourages an early diagnosis and management (11).
A functional uterine cavity is present in 2–7% of patients with Müllerian anomalies (1). Considering that orthograde menstruation begins at menarche, delayed diagnosis and treatment theoretically increase the risk of endometriosis, intrapelvic adhesions, and inflammation (4). The key to an early diagnosis is keeping a high level of suspicion of cervicovaginal agenesis/dysgenesis and discriminating it from other pathologies that share the same presentation, such as imperforated hymen and obstructive transvaginal septum. Most patients with cervicovaginal anomalies present with primary amenorrhea and cyclic abdominal pain (2). In such cases, transabdominal -or when applicable, transvaginal- ultrasonography and MRI are valuable to determine the level of obstruction. An MRI is also useful to detect most coexisting urologic anomalies since it was reported in 15–20% of patients with cervicovaginal malformations (3).
Due to the complexity of the surgical reconstruction of these malformations, a direct intervention after the diagnosis may not be feasible. Therefore, some authors recommend hormonal suppression with oral contraceptives or Gonadotropin-releasing Hormone (GnRH) agonists to stop orthograde menstruation and associated etiologic processes (4).
A standardized surgical intervention for cervicovaginal anomalies is hard to determine owing to the vast heterogeneity of these malformations. Fedele et al. (4) indicated that the type of surgical intervention should be determined based on the cervical anomaly type and the presence or absence of the vagina. In fact, an earlier systematic review demonstrated that regardless of the surgical approach, the presence of a congenitally healthy vagina improved the postoperative pregnancy chances (2). Furthermore, Mikos et al. (2) suggested that a practical and comprehensive classification of uterovaginal anomalies should take into account the presence or absence of a normal vagina, which is unfortunately not explicitly implemented in some current classification systems of the Müllerian anomalies. The joint classification of Müllerian anomalies by the European Society of Human Reproduction and Embryology and the European Society of Gynecologic Endoscopy (ESHRE/ESGE) (12) covers the possible vaginal malformations but unfortunately misses many cervical malformations that were mentioned by Rock et al. (6). In our opinion, a revised ESHRE/ESGE classification of the Müllerian anomalies that covers all potential uterocervical malformations would be of great clinical value.
Many authors had recommended hysterectomy to be the treatment of choice for patients with cervicovaginal anomalies due to the elevated risk of restenosis and sepsis (8). Interestingly, the first attempt to conservatively repair a cervicovaginal anomaly dates to 1900 (13). Recent studies demonstrated the safety and effectiveness of surgical reconstructions for patients with Müllerian anomalies. The conservative surgical management of uterovaginal agenesis/dysgenesis could be broadly classified into 3 groups: cervical canalization, uterovaginal or utero-vestibular anastomosis, and transplantation of homologous or heterologous grafts (4). In the systematic review of Mikos et al. (2), the anastomotic procedures were the most commonly implemented. Most of the patients who underwent uterovaginal anastomosis had either cervical agenesis or cervical obstruction. The postoperative menstruation rate was 93.3%. Additionally, the authors reported a postoperative pregnancy rate of 14.1% (2). These results elucidate the effectiveness of this procedure for the treatment of cervical malformations.
Direct comparisons between these techniques are not available due to the scarcity of cervicovaginal agenesis/dysgenesis cases. However, it is our belief that comparisons have little to no value at all, due to the heterogenous spectrum of cervicovaginal anomalies and associated malformations. The surgical intervention should be as personalized as possible and tailored to the patient’s initial presentation.
4 Conclusion
The cervicovaginal anomalies are a rare clinical entity that has severe consequences on the patient’s mental and physical health. Laparoscopic cervicovaginal anastomosis is a feasible technique that restores the continuity between the cervix and the vagina and preserves the patient’s fertility with an acceptable safety profile. Conservative reconstructive surgeries should be considered as a first treatment in patients with cervicovaginal agenesis or dysgenesis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AN: Conceptualization, Writing – original draft. GM: Writing – review & editing. SS: Visualization, Writing – review & editing. ZS: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor GB declared a past co-authorship with the authors AN, ZS, and GM.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1604463/full#supplementary-material
References
1. Ludwin, A, and Pfeifer, SM. Reproductive surgery for Müllerian anomalies: a review of Progress in the last decade. Fertil Steril. (2019) 112:408–16. doi: 10.1016/j.fertnstert.2019.07.005
2. Mikos, T, Lantzanaki, M, Anthoulakis, C, and Grimbizis, GF. Functional and reproductive outcomes following surgical Management of Congenital Anomalies of the cervix: a systematic review. J Minim Invasive Gynecol. (2021) 28:1452–61.e16. doi: 10.1016/j.jmig.2020.10.030
3. Fujimoto, VY, Miller, JH, Klein, NA, and Soules, MR. Congenital cervical atresia: report of seven cases and review of the literature. Am J Obstet Gynecol. (1997) 177:1419–25. doi: 10.1016/s0002-9378(97)70085-1
4. Fedele, F, Parazzini, F, Vercellini, P, Bergamini, V, and Fedele, L. Reconstructive surgery for congenital atresia of the uterine cervix: a systematic review. Arch Gynecol Obstet. (2023) 308:685–700. doi: 10.1007/s00404-022-06825-5
5. Grimbizis, GF, Camus, M, Tarlatzis, BC, Bontis, JN, and Devroey, P. Clinical implications of uterine malformations and Hysteroscopic treatment results. Hum Reprod Update. (2001) 7:161–74. doi: 10.1093/humupd/7.2.161
6. Rock, JA, Roberts, CP, and Jones, HW Jr. Congenital anomalies of the uterine cervix: lessons from 30 cases managed clinically by a common protocol. Fertil Steril. (2010) 94:1858–63. Epub 20091125. doi: 10.1016/j.fertnstert.2009.10.024
7. Deffarges, JV, Haddad, B, Musset, R, and Paniel, BJ. Utero-vaginal anastomosis in women with uterine cervix atresia: long-term follow-up and reproductive performance. A study of 18 cases. Hum Reprod. (2001) 16:1722–5. doi: 10.1093/humrep/16.8.1722
8. Buttram, VC Jr. Müllerian anomalies and their management. Fertil Steril. (1983) 40:159–63. doi: 10.1016/s0015-0282(16)47230-4
9. Keepanasseril, A, Saha, SC, Bagga, R, Vyas, S, and Dhaliwal, LK. Uterovaginal anastomosis for the management of congenital atresia of the uterine cervix. Gynecol Surg. (2011) 8:161–4. doi: 10.1007/s10397-010-0640-x
10. Zhou, Q, Chen, X, Luo, X, Ding, J, Zhang, G, Ren, Y, et al. Laparoscopic-assisted Uterovaginal anastomosis for uterine cervix atresia with vaginal aplasia using a silicone stent lined with acellular porcine small intestinal submucosa graft inserted using a 16f Foley catheter. J Minim Invasive Gynecol. (2013) 20:710–3. doi: 10.1016/j.jmig.2013.03.010
11. Liu, X, Ding, J, Li, Y, Hua, K, and Zhang, X. An investigation of depressive symptoms in patients with congenital cervical and vaginal aplasia: a cross-sectional study. Int J Women's Health. (2022) 14:1621–7. doi: 10.2147/ijwh.S384339
12. Grimbizis, GF, Gordts, S, Di Spiezio Sardo, A, Brucker, S, De Angelis, C, Gergolet, M, et al. The eshre/Esge consensus on the classification of female genital tract congenital anomalies. Hum Reprod. (2013) 28:2032–44. doi: 10.1093/humrep/det098
Keywords: anastomosis, cervicovaginal agenesis, fertility preservation, laparoscopy, Müllerian anomalies, reconstructive surgery, uterine-sparing
Citation: Naem A, Moufawad G, Sultan S and Sleiman Z (2025) Laparoscopy-assisted uterovaginal anastomosis in a patient with atypical cervicovaginal malformation: a case report. Front. Med. 12:1604463. doi: 10.3389/fmed.2025.1604463
Edited by:
Giovanni Buzzaccarini, Vita-Salute San Raffaele University, ItalyReviewed by:
Ani Amelia Zainuddin, National University of Malaysia, MalaysiaDharmendra Kumar Pipal, All India Institute of Medical Sciences Gorakhpur, India
Copyright © 2025 Naem, Moufawad, Sultan and Sleiman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antoine Naem, YW50b2luZS5uYWVtQGdtYWlsLmNvbQ==
 Antoine Naem
Antoine Naem Graziella Moufawad
Graziella Moufawad Suzana Sultan3
Suzana Sultan3 Zaki Sleiman
Zaki Sleiman