Abstract
Gallstone ileus is a rare but severe complication of gallstone disease and is typically caused by the formation of a fistula between the biliary and gastrointestinal systems. The conventional treatment approach is enterolithotomy with stone removal. However, for elderly patients or those with underlying comorbidities, surgical intervention poses significant risks. Therefore, exploring minimally invasive, nonsurgical treatment strategies holds critical clinical value. A 63-year-old female was admitted to the hospital due to abdominal pain, chills, and high fever. She was diagnosed with a large common bile duct stone (diameter 3.9 cm). During endoscopic retrograde cholangiopancreatography (ERCP), as the stone was too large to be removed directly, endoscopic sphincterotomy (EST) combined with the placement of a biliary plastic stent was performed. On the 7th postoperative day, the patient developed nausea, vomiting, and constipation. Laboratory tests revealed elevated inflammatory marker, pancreatic enzyme, bile enzyme, and bilirubin levels. Imaging studies revealed intestinal dilatation and a high-density shadow within the intestinal lumen, leading to the diagnosis of gallstone ileus. On postoperative day 11, biliary and pancreatic stents were placed. On postoperative day 16, endoscopic stone extraction was attempted, successfully relieving the obstruction. The patient recovered well postoperatively and experienced no recurrence during the 2-month follow-up. This case report describes the successful treatment of post-ERCP gallstone ileus using endoscopic stone extraction and fragmentation techniques.
1 Introduction
Gallstone ileus is a rare complication of gallstone disease. Its primary pathological mechanism involves chronic inflammation of the biliary tract, which leads to adhesions between the biliary and intestinal systems, resulting in pressure necrosis and the formation of a fistula, most commonly between the gallbladder and the duodenum. This pathological channel allows gallstones to enter the intestinal tract, causing mechanical bowel obstruction (1). The imaging findings typically exhibit the classic Rigler triad: ectopic gallstones, bowel obstruction, and pneumobilia (2). In rare cases, gallstones may pass directly into the duodenum through the common bile duct and an enlarged ampulla of Vater following ERCP and sphincterotomy, leading to bowel obstruction (3–6).
Although the incidence of gallstone ileus is low [accounting for less than 0.1% of cases of mechanical bowel obstruction (7)], its mortality rate is 5–10 times higher than that of other nonmalignant mechanical small bowel obstructions, with reported mortality rates ranging from 12 to 18% (8). It is a surgical emergency requiring significant attention (9). Common risk factors include female sex, age >65 years, a history of untreated cholecystitis, and large gallstones (>2.5 cm). Enterolithotomy is the current mainstay of treatment (10). However, the high risks and complication rates associated with surgical intervention (11) make it unsuitable for elderly patients with poor baseline health. In this context, exploring nonsurgical treatment approaches is critically important.
We report a case in which endoscopic stone extraction combined with mechanical lithotripsy was successfully used to treat ileal gallstone obstruction, providing valuable insights into the management of such patients.
2 Case presentation
A 63-year-old female (BMI = 15.79) presented to the hospital with a 3-day history of chills, high fever, and abdominal pain. Ultrasound examination revealed extrahepatic bile duct stones. Thirteen years earlier, she had undergone open cholecystectomy for gallbladder stones. On September 29, 2024, ERCP was performed. Given the large size of the common bile duct stone (approximately 3.9 cm in diameter), direct stone extraction was not feasible. Therefore, EST and biliary plastic stent placement were performed to drain bile and relieve obstruction. Postoperatively, the patient’s abdominal pain and fever subsided.
However, on the 4th postoperative day, the patient developed postprandial abdominal distension and nausea. By the 7th postoperative day, her condition worsened, with fever, vomiting, and difficulty passing stool. Emergency laboratory tests revealed elevated inflammatory markers, bilirubin, pancreatic enzymes and bile enzymes (Laboratory examination indicators are listed in Table 1). CT on October 8 revealed dilatation of the intrahepatic and extrahepatic bile ducts with the presence of pneumobilia, proximal bowel dilation, and high-density shadows of a gallstone and stent within the small intestine, suggesting that the gallstone and stent had migrated into the intestinal tract. These findings were consistent with retrograde biliary infection combined with intestinal obstruction, for which symptomatic medical treatment was administered.
Table 1
| Reference range | October 7 | October 12 | October 15 |
|---|---|---|---|
| Neutrophils (0.5–0.7) | 0.921 | 0.626 | 0.503 |
| White blood cells (3.5 × 109/L–10 × 109/L) | 16.37 × 109/L | 5.56 × 109/L | 5.48 × 109/L |
| Interleukin-6 (0–5.9 pg/mL) | 609.70 pg/mL | 5.79 pg/mL | <2.00 pg/mL |
| Total bilirubin (0–21.0 μmol/L) | 57.7 μmol/L | 17.5 μmol/L | 15.4 μmol/L |
| Direct bilirubin (0–8.6 μmol/L) | 39.5 μmol/L | 10.6 μmol/L | 10.4 μmol/L |
| Alkaline phosphatase (0–130 U/L) | 653.0 U/L | 269.9 U/L | 238.7 U/L |
| Gamma-glutamyl transferase (0–50 U/L) | 924.0 U/L | 343.9 U/L | 296.4 U/L |
| Amylase (0–150 U/L) | 2398.0 U/L | 219.1 U/L | 212.8 U/L |
| Lipase (13–60 U/L) | 7473.7 U/L | 194.0 U/L | 373.2 U/L |
| Blood culture | Enterococcus faecalis | – | – |
Laboratory examinations.
On October 11, ERCP was repeated, and biliary and pancreatic stents (for pancreatitis prevention) were placed. Postoperatively, the patient’s abdominal distension and fever improved. A follow-up abdominal CT on October 14 showed that the gallstone had migrated to the 5th–6th segment of the small intestine (the change in the position of the gallstone is shown in Figure 1). After thorough communication with the patient’s family, and considering her poor general condition and comorbid mild tricuspid and aortic valve regurgitation, surgical intervention was deemed high risk and was declined by the patient and her family. As the stone was located near the ileocecal region, endoscopic stone extraction combined with mechanical lithotripsy was considered a feasible option to relieve the intestinal obstruction.
Figure 1

Changes in gallstone location (A) October 1 (MRI); (B) October 8 (CT); (C) October 14 (CT).
On October 16, endoscopic treatment was performed. A colonoscope (OLYMPUS CF-H290I) was advanced through the ileocecal valve to the ileum, 50–70 cm beyond which a large gallstone was found to completely obstruct the intestinal lumen (Figure 2A). Because the outer layer of the gallstone was relatively soft, the stone was fragmented using repeated maneuvers with foreign body forceps, a snare (COOK ASJ-1-S), and a retrieval basket (COOK MWB-3X6) to grasp and pull back portions of the stone (Figure 2B). After the stone size was significantly reduced, the retrieval basket was used to encapsulate and drag the stone to the sigmoid colon. However, owing to the large size of the stone, it could not pass through the sigmoid colon. The scope was advanced to the descending colon, where the stone was completely fragmented using an emergency lithotripter (COOK SLH-1, TTCL-1 [8.5F]), and the larger fragments were extracted using a snare (Figure 2C). The entire procedure lasted approximately 4 hours.
Figure 2
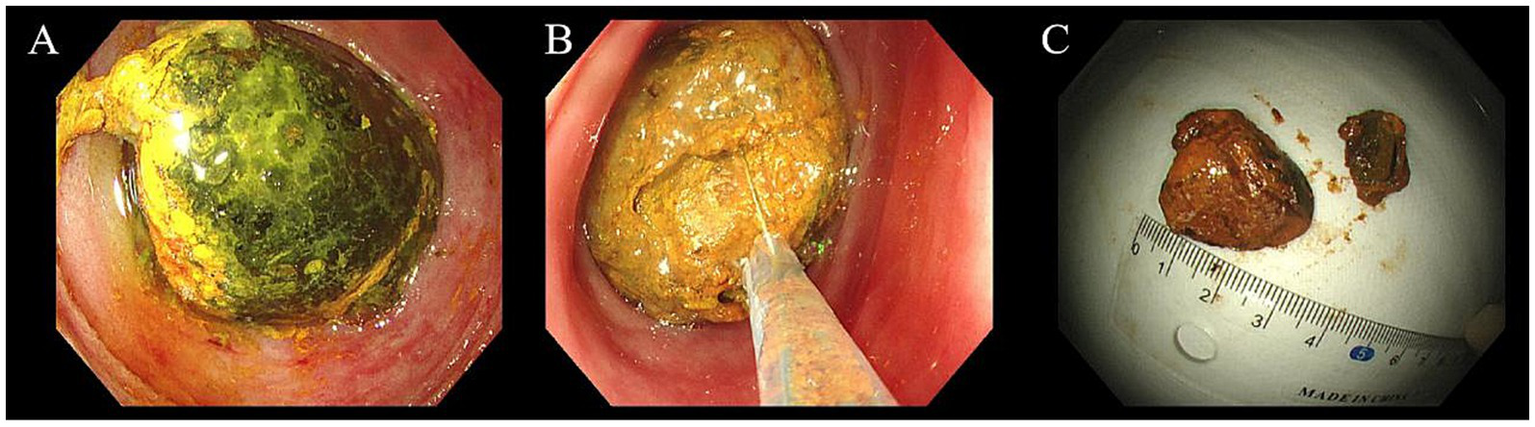
Endoscopic mechanical lithotripsy of gallstone ileus (A) large gallstone in the ileum, (B) fragmentation of the gallstone, (C) retrieved gallstone fragments and size measurement.
The patient was discharged on October 22. During the 2-month follow-up, no recurrence of symptoms was observed.
3 Discussion
According to the literature, it is extremely rare for gallstones to pass directly into the gastrointestinal tract through the ampulla of Vater after ERCP and EST, subsequently leading to gallstone ileus. The onset of this complication can range from 2 days to 7 months post-procedure (3, 6). Most reported cases eventually required surgical intervention; however, there has been one case where the gallstones were spontaneously expelled (6). Although gallstone ileus is an exceedingly rare complication of ERCP, clinicians should remain highly vigilant and closely monitor patients, particularly after the removal of large stones.
Hermosa et al. conducted a retrospective study of 40 patients over 21 years (1980–2000) and reported that the most common site of gallstone impaction in the gastrointestinal tract was the ileum (62.5%), followed by the jejunum (22.5%), duodenum (7.5%), and colon (2.5%). Although the ileum is a frequent site of gallstone ileus, reports of successful endoscopic treatment in this region are limited. Published case reports include Murray et al. (12), who used a large Olympus polypectomy snare to capture and retrieve a gallstone at the ileocecal valve during colonoscopy. De Palma et al. (13) successfully removed an impacted gallstone using a Roth net device. Heinzow et al. (14) was the first to perform single-balloon enteroscopy combined with extracorporeal shock wave, laser, and mechanical lithotripsy to fragment a stone. Shin et al. (15) reported Korea’s first case of a gallstone impacted at the ileocecal valve successfully treated with electrohydraulic lithotripsy.
Endoscopic treatment of gallstone ileus has mostly been reported in case studies, and its applicability should be individually evaluated based on the patient’s condition. Key considerations include the accessibility of the endoscope and instruments, procedural safety, and the patient’s willingness to undergo intervention. In this case, physical examination revealed no significant abdominal tenderness, and the small bowel showed no signs of ischemic necrosis or exudation, suggesting preserved intestinal perfusion. Under these conditions, colonoscopic intervention was considered relatively safe; otherwise, a more cautious approach would be warranted. Additionally, attention should be paid to the patient’s subjective symptoms, as severe complications such as perforation are often accompanied by marked discomfort.
The successful resolution of gallstone ileus may depend on the endoscopist’s selection of instruments and experience level, although these factors have not been systematically evaluated. Endoscopic tools commonly include foreign body forceps, snares, and stone retrieval baskets. Foreign body forceps are typically used to grasp small stone fragments or assist with fragmentation. Snares, although useful, may have issues such as slippage and insufficient gripping strength when dealing with stones. In contrast, stone retrieval baskets are preferred for removing large or irregularly shaped stones. The limited operational space often necessitates combining lithotripsy techniques for completely impacted stones. Laser lithotripsy offers the advantage of minimal trauma in gallstone management (16). However, its probes are prone to damage, and the procedure is expensive. Electrohydraulic lithotripsy is more cost-effective but carries risks such as perforation and bleeding. On the other hand, mechanical lithotripsy is simple to perform, cost-efficient, and has a relatively high success rate when used alone (17, 18). Importantly, most studies on lithotripsy have focused on managing bile duct stones, and sufficient data regarding the removal of gallstones in the intestinal environment are lacking.
A review of the literature identified 24 reported cases of gallstone ileus successfully treated with mechanical lithotripsy (Table 2). The average age of the patients was 78.92 years, with females accounting for 54.17% (13/24) and males accounting for 45.83% (11/24). The duodenum was the most common site of successful cases, accounting for 83.33% (20/24), followed by the colon (12.50%, 3/24) and the jejunum (4.17%, 1/24). The successful application of mechanical lithotripsy in the ileum, as reported in this case, provides an important addition to the data in the table.
Table 2
| Gender, age | Number, maximum size (mm), and location of stones | Stone entry route | Endoscopic treatment | Surgical treatment | Year | References |
|---|---|---|---|---|---|---|
| M, 71 | 1, NA, bulb | D1 has a large fistulous opening | – | Planned cholecystectomy | 2016 | Dumonceau and Deviere (18) |
| F, 83 | 1, NA, bulb | Cholecystoduodenal fistula | – | – | 2015 | |
| M, 78 | 1, NA, pylorus | Cholecystoenteric communication | – | – | 2015 | |
| M, 90 | 1, NA, pylorus | Cholecystoduodenal fistula | Endoscopic biliary sphincterotomy, common bile duct stone extraction | – | 2014 | |
| F, 62 | 1, 35 × 30, D3 | Cholecystoduodenal fistula | – | – | 2012 | |
| F, 81 | 1, 30, bulb | Cholecystoduodenal fistula | – | – | 2012 | |
| M, 84 | 1, 40, pylorus | Bilio-enteric fistula | – | Planned cholecystectomy | 2012 | |
| M, 80 | 1, 45 × 40, bulb | NA | – | – | 2011 | |
| F, 81 | 2, NA, pylorus | Cholecystoduodenal fistula | Extended cholecystectomy (incidental T1 adenocarcinoma) | 2010 | ||
| M, 86 | 1, 33, D2 | Cholecystoduodenal fistula | – | – | 2009 | |
| F, 93 | 1, 27 × 27, bulb | Cholecystoduodenal fistula | – | – | 2009 | |
| F, 76 | 1, NA, bulb | Cholecystoduodenal fistula | – | – | 2008 | |
| F, 76 | 1, 30, bulb | Possibility of cholecystoduodenal fistula | – | – | 2008 | |
| F, 65 | 1, 35 × 25, pylorus | Cholecystoduodenal fistula | – | – | 2007 | |
| M, 81 | 1, NA, bulb | Possibility of cholecystoduodenal fistula | – | – | 2006 | |
| F, 73 | 1, 40, bulb | Cholecystoduodenal fistula | – | Cholecystectomy, closure of the cholecystoduodenal fistula | 2005 | |
| M, 68 | 1, 25, bulb | NA | – | Cholecystectomy | 2002 | |
| M, 86 | 1, 25 × 30, bulb | Choledochoduodenal fistula | – | Cholecystectomy | 2017 | Hasan et al. (19) |
| F, 83 | 1, 35, D1 | Cholecystoduodenal fistula | – | – | 2022 | Sanyang et al. (20) |
| M, 61 | 1, 50, duodenum | The fistula was observed along the lateral duodenal wall | – | Planned outpatient cholecystectomy | 2023 | Bechara et al. (21) |
| F, 94 | 1, 35, sigmoid colon | Cholecystocolonic fistula | – | – | 2015 | Balzarini et al. (22) |
| F, 78 | 1, 30, sigmoid colon | NA | – | – | 2008 | Reiss et al. (23) |
| M, 73 | 1, 40 × 40, rectosigmoid level | Cholecystoenteric fistula | – | – | 2014 | Waterland et al. (24) |
| F, 91 | 1, 40, upper jejunum | Cholecystoduodenal fistula | – | – | 1999 | Lubbers et al. (25) |
Successful application of mechanical lithotripsy in gallstone ileus.
M, male; F, female; NA, not available; D1, first part of the duodenum; D2, second part of the duodenum; D3, third part of the duodenum.
Based on our procedural experience, we recommend first assessing the size of the gallstone to determine whether it can be directly retrieved. If the stone is large, its volume should be reduced in situ before attempting extraction. When sufficient operating space is available, a snare and retrieval basket can effectively fragment and remove the stone. However, if the stone is tightly adherent to the intestinal wall, preventing proper deployment of these devices, initial fragmentation using foreign body forceps may help create adequate space for subsequent instrument access and lithotripsy.
4 Conclusion
In gallstone ileus, stones are often impacted, significantly increasing the difficulty of treatment with a single instrument. In this case, multiple tools, including foreign body forceps, snares, stone retrieval baskets, and emergency lithotripters, were used to fragment and completely remove the stone gradually. This highlights the value of a multitool approach in managing complex cases.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
For the studies involving humans because waiver of ethical approval was granted; therefore, no IRB/ethics committee was involved. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JW: Writing – original draft. ZL: Writing – review & editing. BY: Supervision, Writing – review & editing. GS: Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This works was supported by the Defense Science and Technology Innovation Special Zone Project (Project No. 23-163-00-GZ-001-001-02-03) and the Top Discipline Talent Training Program under the Military High-Level Science and Technology Innovation Talent Initiative (GCCRC-2024-002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ERCP, endoscopic retrograde cholangiopancreatography; EST, endoscopic sphincterotomy.
References
1.
Matli VVK Marler KC Morgan A Pujala V Pandit S Morris J . Gallstone enteropathy: an unusual cause of bowel obstruction. Cureus. (2023) 15:e44707. doi: 10.7759/cureus.44707
2.
Lai YT Wu PH . Gallstone ileus. N Engl J Med. (2022) 387:924. doi: 10.1056/NEJMicm2204208
3.
Fedele S Lobascio P Carbotta G Balducci G Laforgia R Sederino MG et al . Gallstone ileus in a ninety-two years old colecistectomized patient after endoscopic biliary sphincterotomy: a case report. G Chir. (2017) 38:299–302. doi: 10.11138/gchir/2017.38.6.299
4.
Pittman MA Heath D McNair A . Gallstone ileus following endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy. Dig Dis Sci. (2007) 52:513–5. doi: 10.1007/s10620-006-9588-0
5.
Sivagnanam P Cheong E Rhodes M . Delayed gallstone ileus presentation after ERCP and sphincterotomy. Gastrointest Endosc. (2009) 69:156–8. doi: 10.1016/j.gie.2008.06.012
6.
Yamauchi Y Wakui N Asai Y Dan N Takeda Y Ueki N et al . Gallstone ileus following endoscopic stone extraction. Case Rep Gastrointest Med. (2014) 2014:271571. doi: 10.1155/2014/271571
7.
Halabi WJ Kang CY Ketana N Lafaro KJ Nguyen VQ Stamos MJ et al . Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. (2014) 259:329–35. doi: 10.1097/SLA.0b013e31827eefed
8.
Doko M Zovak M Kopljar M Glavan E Ljubicic N Hochstadter H . Comparison of surgical treatments of gallstone ileus: preliminary report. World J Surg. (2003) 27:400–4. doi: 10.1007/s00268-002-6569-0
9.
Roy A Phukan PD . Gallstone ileus: rare life-threatening disease. J Med Soc. (2020) 34:111. doi: 10.4103/jms.jms_86_18
10.
Alzerwi NAN Idrees B Alsareii S Aldebasi Y Alsultan A . The regularity of the site of impaction in recurrent gallstone ileus: a systematic review and meta-analysis of reported cases. Can J Gastroenterol Hepatol. (2021) 2021:5539789. doi: 10.1155/2021/5539789
11.
Mallipeddi MK Pappas TN Shapiro ML Scarborough JE . Gallstone ileus: revisiting surgical outcomes using National Surgical Quality Improvement Program data. J Surg Res. (2013) 184:84–8. doi: 10.1016/j.jss.2013.05.027
12.
Murray EL Collie M Hamer-Hodges DW . Colonoscopic treatment of gallstone ileus. Endoscopy. (2006) 38:197. doi: 10.1055/s-2006-925144
13.
De Palma GD Mastrobuoni G Benassai G . Gallstone ileus: endoscopic removal of a gallstone obstructing the lower ileum. Dig Liver Dis. (2009) 41:446. doi: 10.1016/j.dld.2008.06.017
14.
Heinzow HS Meister T Wessling J Domschke W Ullerich H . Ileal gallstone obstruction: single-balloon enteroscopic removal. World J Gastrointest Endosc. (2010) 2:321–4. doi: 10.4253/wjge.v2.i9.321
15.
Shin KH Kim DU Choi MG Kim WJ Ryu DY Lee BE et al . A case of gallstone ileus treated with electrohydraulic lithotripsy guided by colonoscopy. Korean J Gastroenterol. (2011) 57:125–8. doi: 10.4166/kjg.2011.57.2.125
16.
Nakai Y Sato T Hakuta R Ishigaki K Saito K Saito T et al . Management of difficult bile duct stones by large balloon, cholangioscopy, enteroscopy and endosonography. Gut Liver. (2020) 14:297–305. doi: 10.5009/gnl19157
17.
Yasuda I Itoi T . Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc. (2013) 25:376–85. doi: 10.1111/den.12118
18.
Dumonceau JM Deviere J . Novel treatment options for Bouveret’s syndrome: a comprehensive review of 61 cases of successful endoscopic treatment. Expert Rev Gastroenterol Hepatol. (2016) 10:1245–55. doi: 10.1080/17474124.2016.1241142
19.
Hasan S Khan Z Darr U Javaid T Siddiqui N Saleh J et al . Successful endoscopic treatment of Bouveret syndrome in a patient with choledochoduodenal fistula complicating duodenal ulcer. Case Rep Gastrointest Med. (2017) 2017:6918905. doi: 10.1155/2017/6918905
20.
Sanyang N Shanti H Patel AG . Successful endoscopic management of Bouveret syndrome. J Surg Case Rep. (2022) 2022:rjac484. doi: 10.1093/jscr/rjac484
21.
Bechara R Milne F Rai M . Treatment of Bouveret syndrome with stone fragmentation using an endoscopic submucosal dissection knife. VideoGIE. (2024) 9:82–3. doi: 10.1016/j.vgie.2023.09.016
22.
Balzarini M Broglia L Comi G Calcara C . Large bowel obstruction due to a big gallstone successfully treated with endoscopic mechanical lithotripsy. Case Rep Gastrointest Med. (2015) 2015:798746. doi: 10.1155/2015/798746
23.
Reiss G Gopi R Ramrakhiani S . Unusual cause of colonic obstruction: gallstone impaction requiring mechanical lithotripsy. Clin Gastroenterol Hepatol. (2009) 7:A20. doi: 10.1016/j.cgh.2008.07.034
24.
Waterland P Khan FS Durkin D . Large bowel obstruction due to gallstones: an endoscopic problem?BMJ Case Rep. (2014) 2014:bcr2013201652. doi: 10.1136/bcr-2013-201652
25.
Lubbers H Mahlke R Lankisch PG . Gallstone ileus: endoscopic removal of a gallstone obstructing the upper jejunum. J Intern Med. (1999) 246:593–7. doi: 10.1046/j.1365-2796.1999.00597.x
Summary
Keywords
gallstone ileus, mechanical lithotripsy, endoscopic retrograde cholangiopancreatography, endoscopic treatment, case report
Citation
Wang J, Luan Z, Yan B and Sun G (2025) Successful endoscopic mechanical lithotripsy for post-ERCP gallstone ileus: a case report. Front. Med. 12:1604835. doi: 10.3389/fmed.2025.1604835
Received
02 April 2025
Accepted
17 June 2025
Published
02 July 2025
Volume
12 - 2025
Edited by
Amit Kumar Dutta, Christian Medical College and Hospital, India
Reviewed by
Rahul Gupta, Synergy Institute of Medical Sciences, India
Noble Mathew, Christian Medical College and Hospital, India
Updates
Copyright
© 2025 Wang, Luan, Yan and Sun.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Yan, yanbin0108@163.com; Gang Sun, sunok301@126.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.