Abstract
A 35-year-old male was admitted with drowning-induced cardiorespiratory arrest. Initial assessment revealed acute respiratory distress syndrome (ARDS), pneumothorax and refractory hypoxemia. Despite mechanical ventilation and thoracostomy tube placement, his condition deteriorate. Prompting urgent initiating of veno-veous extracorporeal membrane oxygenation (V-V ECMO). Respiratory support was dynamically adjusted through sequential oxygen therapy, balancing oxygenation optimization with mitigation of ventilator-induced lung injury. Concurrent targeted antimicrobial therapy and intensive care management led to gradual clinical improvement, culminating in successful ECMO weaning and eventual recovery. This case highlights the potential of integrating ECMO with sequential oxygen therapy to address complex pathophysiological challenges in drowning-associated ARDS.
Introduction
Drowning, the third leading cause of unintentional injury-related deaths globally, poses significant challenges in emergency and critical care management (1). With an estimated 300,000 annual fatalities worldwide (WHO data) its pathophysiological complexity-characterized by hypoxic injury, non-cardiogenic pulmonary edema, multiorgan dysfunction—demands therapeutic strategies that reconcile rapid intervention with physiological precision (2, 3). Current guidelines emphasize the drowning survival chain, spanning prevention, prehospital resuscitation (e.g., prompt retrieval from water, high-quality CPR, airway clearance) (4); and hospital-based management targeting hypoxemia correction (via high-flow oxygen or mechanical ventilation), hemodynamic stabilization, and multiorgan monitoring (5). For refractory hypoxemia unresponsive to conventional therapies, extracorporeal membrane oxygenation (ECMO) may serve as a salvage intervention (6).
Drowning-induced lung injury arises from alveolar-capillary membrane disruption and pulmonary surfactant loss, precipitating acute respiratory distress syndrome (ARDS) (7). While the EOLIA trial subgroup analysis supports early ECMO initiation in severe ARDS to improve outcomes (8), recent retrospective data suggest lower survival rates in drowning patients receiving ECMO than previously reported, with uncertain mortality impacts of distinct ECMO modalities (9). Despite these insights, clinical decision-making remains constrained by limited high-quality evidence, as most drowning-related studies are observational and fail to address critical knowledge gaps (10), including optimal ECMO timing, configuration, and adjuvant therapies. Impact of ECMO treatment on resuscitation of drowning victims needs further research to assess it (11).
This case report details the successful management of drowning-induced ARDS through ECMO combined with sequential oxygen therapy—a strategy dynamically balancing oxygenation enhancement and ventilator-induced lung injury mitigation. Our approach may provide a clinical reference for this high-risk population.
Case report
Following retrieval from a 5-meter-deep swimming pool where the patient was found unresponsive with cardiopulmonary arrest (CPA), prompt CPR was initiated. During prehospital transport, oxygenation was sustained via a bag-valve-mask (BVM) device, accompanied by continuous norepinephrine infusion (0.4 μg/kg/min) to maintain hemodynamic stability.
Upon emergency department arrival, the patient presented comatose with perioral cyanosis, bilaterally diminished breath sounds, and SpO₂ 80% despite maximal oxygen supplementation. Emergent endotracheal intubation with mechanical ventilation was initiated. However, clinical deterioration ensued: chest X-ray demonstrated right-sided pneumothorax (>50% lung collapse, Figure 1A), necessitating immediate thoracostomy tube placement. The patient developed refractory hypotension requiring norepinephrine titration (0.2 μg/kg/min) and was subsequently transferred to the intensive care unit (ICU) for advanced hemodynamic monitoring and organ support.
Figure 1

Chest X-ray. (A) Pneumothorax, white arrows: absence of lung markings. (B) Marked resolution of pneumothorax after thoracostomy tube placement.
Admission examination
A 35-year-old male with an more than 10-min drowning-induced cardiorespiratory arrest presented comatose. Physical examination revealed bulbar conjunctival edema with petechial hemorrhages, sluggish pupillary light reflexes (bilateral), and abdominal distension. Vital signs included weight 60 kg, temperature 36°C, heart rate 125 bpm, and blood pressure 114/56 mmHg under norepinephrine infusion (0.2 μg/kg/min). Mechanical ventilation was ongoing, with a functional right-sided closed thoracostomy tube draining copious air (chest drainage system). Laboratory studies demonstrated hepatic dysfunction, acute kidney injury, and coagulopathy (Table 1). Bronchoscopy identified abundant bloody secretions in the bronchial tree (Figures 2A–C). No significant preexisting comorbidities were reported by the family. Initial diagnoses included acute respiratory distress syndrome (ARDS), pneumothorax, and refractory hypoxemia.
Table 1
| Variable | Reference range, this hospitala | Admission | ECMO 72 h | Discharge |
|---|---|---|---|---|
| Blood routine examination | ||||
| White blood cell (×109/L) | 3.50–9.50 | 22.83 | 15.98 | 4.53 |
| Red blood cell (×1012/L) | 4.3–5.8 | 3.71 | 3.21 | 3.11 |
| Hemoglobin (g/L) | 130–175 | 109 | 94 | 89 |
| Platelet (×109/L) | 125–350 | 115 | 79 | 193 |
| Absolute neutrophil count (×109/L) | 1.80–6.30 | 21.64 | 14.76 | 2.98 |
| Absolute lymphocyte count (×109/L) | 1.1–3.2 | 0.5 | 0.64 | 1.08 |
| Renal function | ||||
| Blood urea (mmol/L) | 3.1–8.0 | 10.6 | 9.9 | 7.9 |
| Serum creatinine (μmol/L) | 57–97 | 170 | 99 | 84 |
| Glomerular filtration rate (mol/min) | 80–120 | 44.1 | 84.8 | 103.4 |
| Uric acid (μmol/L) | 202–463 | 605 | 192 | 247 |
| Liver function | ||||
| Alanine aminotransferase (U/L) | 9.0–50.0 | 318.8 | 64.6 | 41.8 |
| Aspartate aminotransferase (U/L) | 15–40 | 293.8 | 36.2 | 32 |
| Total protein (g/L) | 65.0–85.0 | 53.1 | 63.4 | 58.6 |
| Albumin (g/L) | 40.0–55.0 | 37.8 | 43.0 | 36.8 |
| Globulin (g/L) | 20.0–40.0 | 15.3 | 21.6 | 21.8 |
| Coagulation function | ||||
| Prothrombin time activity (%) | 70.0–130.0 | 50.5 | 64.1 | 85.5 |
| Thrombin time (s) | 14–21 | 35.1 | 14.8 | 15.9 |
| Activated partial thromboplastin time (s) | 23.3–32.5 | 89.8 | 28.2 | 27.9 |
| Fibrinogen (g/L) | 1.8–3.5 | 1.26 | 3.08 | 3.74 |
| D-Dimer (mg/mL) | <0.55 | >80 | 7.48 | 6.21 |
| Other | ||||
| C-reactive protein (mg/L) | 0–8 | 30 | 16.4 | 2 |
| Procalcitonin (ng/mL) | <0.046 | 19.2 | 0.1 | 0.035 |
Laboratory examinations.
Serial monitoring of blood parameters showed initial abnormalities on admission and progressive normalisation by discharge.
Reference values are influenced by many variables, including the patient population and the laboratory methods used.
Figure 2
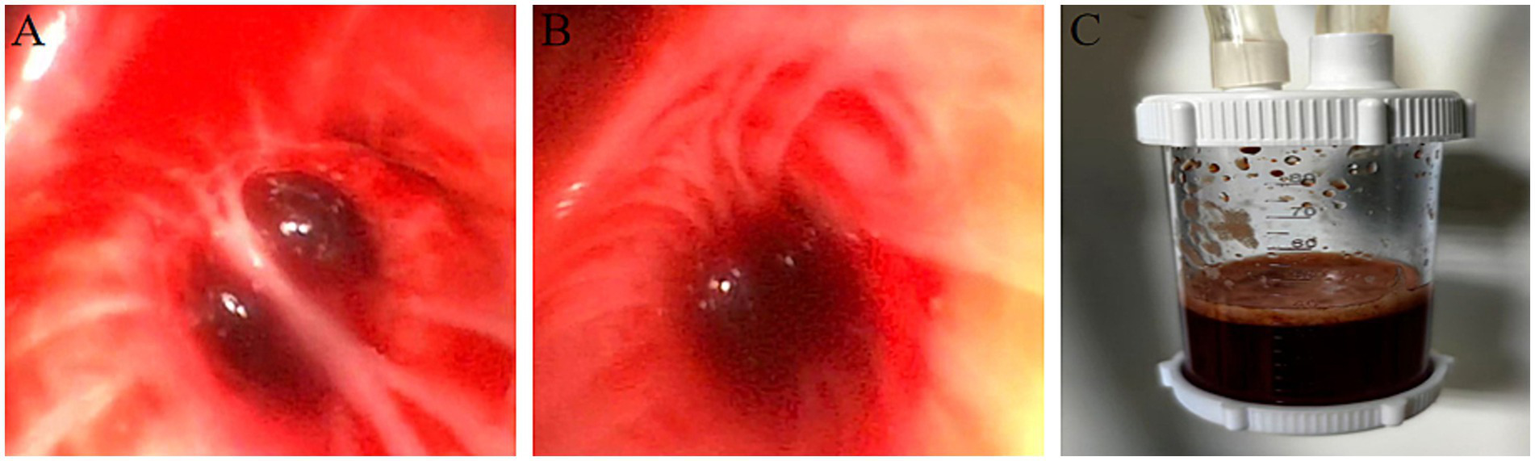
Bronchoscopic photos. (A–C) Copious blood-tinged fluid within the tracheal lumen.
Our therapeutic interventions are as follows:
-
Respiratory & hemodynamic support: Maintained closed thoracostomy drainage with analgesia-sedation; initiated double-lumen nasogastric tube insertion for gastrointestinal decompression.
-
Airway management: Performed therapeutic bronchoscopy, aspirating hemorrhagic secretions.
-
Coagulopathy correction: Administered fresh frozen plasma to restore coagulation homeostasis.
-
ECMO initiation: Despite 6 h of lung-protective mechanical ventilation (PEEP 12 cmH₂O, FiO₂ 100%), refractory hypoxemia persisted (PaO₂/FiO₂ ratio <80), prompting veno-venous ECMO (V-V ECMO) cannulation.
-
Adjunctive therapies: Implemented prone positioning (12 h/day) to enhance pulmonary recruitment; initiated targeted temperature management (36°C for 72 h) to mitigate hypoxic–ischemic brain injury.
-
Antimicrobial stewardship: Empirical meropenem combined with vancomycin was administered on admission. Fever (38.4°C) emerged on day 6, with bronchoalveolar lavage cultures and metagenomic next-generation sequencing (mNGS) identifying Pseudomonas aeruginosa, Klebsiella pneumoniae, and Candida glabrata. Antifungal therapy (caspofungin) and zavicefta were subsequently escalated (Figure 3). On day 17 sitafolxacin was de-escalated.
-
Supportive care: Enforced strict infection control protocols, normothermia maintenance, and enteral nutrition optimization via a standardized ICU bundle.
Figure 3

Therapeutic management flow chart. The upper panel delineates the chronological sequence of ECMO combined with stepwise oxygen therapy weaning, while the lower panel documents temporal adjustments in the antimicrobial stewardship regimen.
As the patient’s oxygenation improved, ECMO parameters were progressively weaned while ventilator support was concomitantly increased. By 72 h post-ECMO initiation, serial chest radiographs demonstrated marked resolution of the right pneumothorax (Figure 1B). Thoracic CT revealed persistent diffuse bilateral pulmonary edema with extensive ground-glass opacities and consolidative patches (Figures 4A,B). Concurrently, laboratory indices showed progressive normalization of hepatic and renal function (Table 1). Subsequently, the patient was successfully weaned from ECMO.
Figure 4
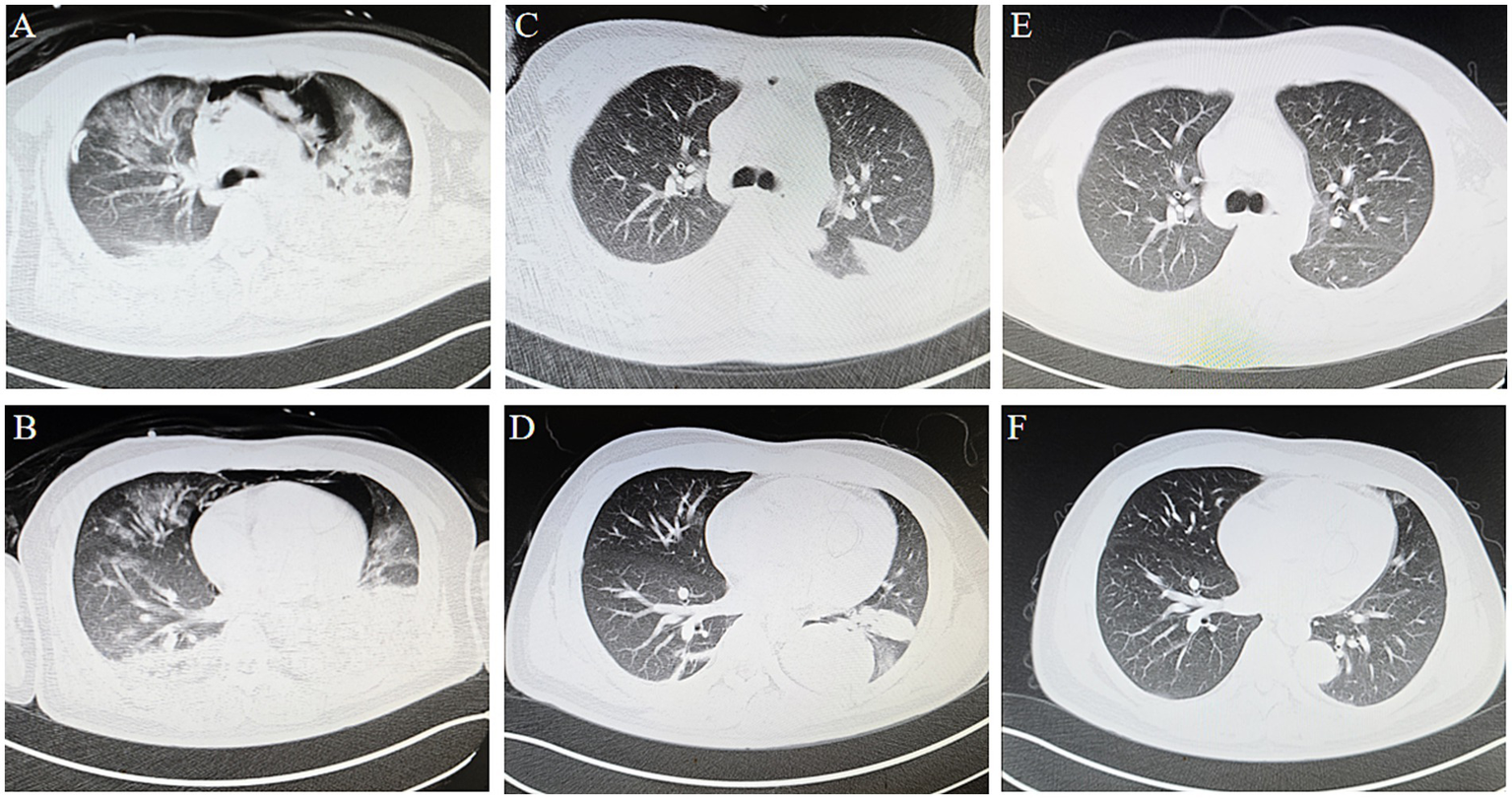
Thoracic CT. (A,B) At 72 h of ECMO, CT demonstrating bilateral pulmonary edema with extensive ground-glass opacities, patchy consolidations and pneumomediastinum. (C,D) Thoracic imaging demonstrated complete resolution of pulmonary edema, with residual consolidative opacities persisting in bilateral lower lobes. (E,F) The 3-month follow-up showed that the patchy shadows were significantly reduced, and had basically recovered.
Post-decannulation respiratory management included mechanical ventilation coupled with scheduled bronchoscopic airway clearance. During the 48-h post-decannulation period, the patient passed spontaneous breathing trials (SBTs) and cuff-leak tests, facilitating extubation. Oxygenation support was then transitioned to high-flow nasal cannula (Supplementary material) to promote alveolar recruitment, complemented by a structured pulmonary rehabilitation program. Sequential stepwise de-escalation to conventional nasal oxygen (2–3 L/min) was achieved by day 8, with complete oxygen independence documented on hospital day 16 (see Figure 3 for timeline). Parameter settings for ECMO, MV, etc. during salvage are shown in the Supplementary material.
By ICU day 23, follow-up thoracic CT demonstrated substantial pulmonary recovery with residual left lower lobe consolidative opacities (Figures 4C,D), paralleled by normalization of hepatic and renal function biomarkers (Table 1). These improvements prompted ICU discharge to general ward care. No ECMO-or ventilator-associated complications occurred during hospitalization.
At the 3-month outpatient follow-up, repeat imaging revealed near-complete resolution of consolidative lesions (Figures 4E,F). The patient reported full resumption of premorbid activities (6-min walk distance: 420 meters) without exertional dyspnea (mMRC grade 0). At the 9-month follow-up, the patient reported that tests at other hospitals showed that the indicators had returned to normal.
Discussion
Drowning as a critical global public health challenge, underscored by the United Nations’ inaugural World Drowning Prevention Day (July 2021) and a 38% decline in age-standardized drowning mortality since 2000. While these advances reflect progress in prevention strategies, achieving the SDG target (reducing unintentional injury deaths) demands accelerated multisectoral collaboration (3). Concurrently, optimizing resuscitation protocols for salvageable patients remains imperative.
This case exemplifies the intricate balance between aggressive intervention and iatrogenic risk mitigation in drowning-induced ARDS. Despite early lung-protective ventilation, refractory hypoxemia (PaO₂/FiO₂ <80) and barotrauma-related pneumothorax necessitated escalation to V-V ECMO—a decision aligned with recent ELSO guidelines prioritizing early ECMO for reversible respiratory failure (8). Our weaning protocol, characterized by synchronized ECMO flow reduction and incremental ventilator adjustments, achieved decannulation within 72 h—a timeframe associated with lower nosocomial infection risks compared to prolonged ECMO runs (12). Post-ECMO respiratory management leveraged sequential oxygen therapy (HFNC → NIV → conventional oxygen), which may attenuate reintubation rates (13).
Notably, the delayed febrile response (day 6) underscores drowning’s unique infection dynamics. Unlike typical aspiration pneumonitis, water immersion predisposes to polymicrobial infections with pathogens (14). Our antimicrobial approach—empirical treatment followed by culture-guided escalation—de-escalation. We believe that an appropriate antimicrobial stewardship strategy is also important, and therefore antibiotics were actively used in the management of this patient.
This case demonstrates ECMO’s viability as rescue therapy and offers valuable insights for analogous clinical scenarios. Yet three evidence gaps warrant prioritization: optimal ECMO initiation thresholds (EOLIA criteria vs. drowning-specific indices); standardized weaning biomarkers beyond PaO₂/FiO₂ (e.g., ventilatory ratio, dynamic compliance); cost-effectiveness of sequential oxygen modalities in resource-constrained settings. Prospective RCTs comparing ECMO timing strategies (EOLIA vs. RESCUE trials) and bundled rehabilitation protocols are urgently needed to establish drowning-specific care pathways.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YW: Data curation, Formal analysis, Investigation, Writing – original draft. RZ: Methodology, Validation, Visualization, Writing – review & editing. BW: Conceptualization, Investigation, Writing – original draft. PZ: Formal analysis, Resources, Writing – original draft. LZ: Project administration, Resources, Visualization, Writing – original draft. HC: Formal analysis, Investigation, Methodology, Writing – original draft. CC: Data curation, Methodology, Validation, Writing – original draft. MH: Project administration, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1609610/full#supplementary-material
References
1.
McCallin TE Dezfulian C Bierens J Dunne CL Idris AH Kiragu A et al . 2024 American Heart Association and American Academy of Pediatrics focused update on special circumstances: resuscitation following drowning: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2024) 150:e501–16. doi: 10.1161/CIR.0000000000001274
2.
Girela-López E Beltran-Aroca CM Dye A Gill JR . Epidemiology and autopsy findings of 500 drowning deaths. Forensic Sci Int. (2022) 330:111137. doi: 10.1016/j.forsciint.2021.111137
3.
Jagnoor J Kobusingye O Scarr JP . Drowning prevention: priorities to accelerate multisectoral action. Lancet. (2021) 398:564–6. doi: 10.1016/S0140-6736(21)01601-9
4.
Girasek DC Hargarten S . Prevention of and emergency response to drowning. N Engl J Med. (2022) 387:1303–8. doi: 10.1056/NEJMra2202392
5.
Szpilman D Morgan PJ . Management for the drowning patient. Chest. (2021) 159:1473–83. doi: 10.1016/j.chest.2020.10.007
6.
Andre MC Vuille-Dit-Bille RN Berset A Hammer J . Rewarming young children after drowning-associated hypothermia and out-of-hospital cardiac arrest: analysis using the CAse REport guideline. Pediatr Crit Care Med. (2023) 24:e417–24. doi: 10.1097/PCC.0000000000003254
7.
Thom O Roberts K Devine S Leggat PA Franklin RC . Treatment of the lung injury of drowning: a systematic review. Crit Care. (2021) 25:253. doi: 10.1186/s13054-021-03687-2
8.
Mi MY Matthay MA Morris AH . Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. (2018) 379:884–7. doi: 10.1056/NEJMclde1804601
9.
Jasny T Kloka J Old O Piekarski F Lotz G Zacharowski K et al . Results from 237 extracorporeal membrane oxygenation runs with drowned patients: a nationwide retrospective study. Crit Care. (2023) 27:293. doi: 10.1186/s13054-023-04580-w
10.
Bierens J Abelairas-Gomez C Barcala Furelos R Beerman S Claesson A Dunne C et al . Resuscitation and emergency care in drowning: a scoping review. Resuscitation. (2021) 162:205–17. doi: 10.1016/j.resuscitation.2021.01.033
11.
Jasny T Kloka J Old O Piekarski F Lotz G Zacharowski K et al . ECMO in resuscitated drowning patients: a propensity score matched sub-analysis—a response to Jouffroy et al. Crit Care. (2023) 27:409. doi: 10.1186/s13054-023-04705-1
12.
Hadaya J Benharash P . Extracorporeal membrane oxygenation. JAMA. (2020) 323:2536. doi: 10.1001/jama.2020.9148
13.
Yasuda H Okano H Mayumi T Narita C Onodera Y Nakane M et al . Post-extubation oxygenation strategies in acute respiratory failure: a systematic review and network meta-analysis. Crit Care. (2021) 25:135. doi: 10.1186/s13054-021-03550-4
14.
Metlay JP Waterer GW Long AC Anzueto A Brozek J Crothers K et al . Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. (2019) 200:e45–67. doi: 10.1164/rccm.201908-1581ST
Summary
Keywords
drowning, extracorporeal membrane oxygenation, sequential oxygen therapy, acute respiratory distress syndrome, case report
Citation
Wu Y, Zhai R, Wang B, Zhao P, Zhao L, Cui H, Chen C and Hu M (2025) ECMO combined with sequential oxygen therapy in drowning-induced ARDS: a case report. Front. Med. 12:1609610. doi: 10.3389/fmed.2025.1609610
Received
10 April 2025
Accepted
26 May 2025
Published
11 June 2025
Volume
12 - 2025
Edited by
Giuseppe Fiorentino, Colli Hospital, Italy
Reviewed by
Carmen Fierro, University of Studies G. d’Annunzio Chieti and Pescara, Italy
Fabrizio Tritapepe, University of Studies G. d’Annunzio Chieti and Pescara, Italy
Updates
Copyright
© 2025 Wu, Zhai, Wang, Zhao, Zhao, Cui, Chen and Hu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mei Hu, humei306@126.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.