Abstract
Purpose:
Low-dose propofol has a preventive effect on postoperative nausea and vomiting (PONV). Ciprofol is a new short-acting GABAA receptor agonist developed in China with a similar chemical structure to propofol, but its effect on PONV is unclear. This study examines whether administration of low-dose ciprofol immediately after the start of surgery reduces the incidence of PONV.
Patients and methods:
In this study, this study enrolled 75 patients undergoing gynecological ambulatory surgery under general anesthesia, and randomly divided the patients into ciprofol group and normal saline control group. Both groups received remimazolam (6 mg/kg/h) until asleep, then alfentanil (20 μg/kg) and mivacurium (0.2 mg/kg) intravenous, followed by maintenance infusions of remimazolam and alfentanil. Five minutes after the start of the surgery, the ciprofol group was given 2 mL of ciprofol (5 mg) and the control group was given 2 mL of normal saline. The primary outcome measure was the incidence of PONV in the PACU. Secondary outcomes included the incidence of emetic episodes or nausea in the PACU and within 24 h, anesthetic time, wake-up time, and administered doses of remimazolam and alfentanil. Safety outcomes encompassed hypotension, hypertension, bradycardia, and tachycardia.
Results:
The incidence of PONV in the PACU was significantly lower in the ciprofol group compared to the control group (16.2% vs 52.6%; RR=0.31; 95% CI, 0.14–0.68; ARR=0.364; p = 0.002). The ciprofol group also exhibited a lower incidence of emetic episodes (defined as retching, vomiting, or both) in the PACU (RR=0.27; 95% CI, 0.10–0.75; ARR=0.287; p = 0.005), as well as a lower incidence of nausea (RR=0.31; 95% CI, 0.14–0.68; ARR=0.364; p = 0.002). The frequency of emetic episodes or nausea within 24 h postoperatively was similar between the groups. There were no significant differences between the two groups regarding anesthesia time, wake-up time, remimazolam and alfentanil dosage, or safety indicators (p > 0.05).
Conclusion:
Low-dose ciprofol can effectively prevent PONV in PACU after gynecological day surgery under general anaesthesia remazolam combined with afentanil, but its effect is limited and cannot reduce the incidence of emetic episodes or nausea within 24 h after surgery.
Clinical trial registration:
https://www.chictr.org.cn, identifier ChiCTR2300077247.
1 Introduction
Day surgery has been widely used worldwide due to its advantages of quick recovery and short hospital stay. Postoperative nausea and vomiting (PONV) is one of the most common complications after day surgery, which seriously affects patients’ postoperative recovery and quality of life (1). Remimazolam is a new type of benzodiazepine with fast onset of action and rapid recovery and can be used for the induction and maintenance of general anaesthesia (2). Alfentanil has the advantages of short action time, fast elimination, no accumulation and low incidence of PONV, and is more suitable for day surgery anaesthesia than sufentanil and remifentanil (3). However, studies have shown that the incidence of nausea and vomiting after remimazolam combined with alfentanil anesthesia is relatively high (4, 5). PONV with this type of anesthesia remains a concern.
Ciprofol is a new type of intravenous anaesthetics researched. The core structure of classical short-acting intravenous anesthetics is 2,6-disubstituted phenol, which binds to GABAA receptors to produce an anesthetic effect, and propofol is the most widely used drug among these drugs (6). Ciprofol adds a cyclopropyl group to the chemical structure of propofol, which enhances its affinity with the GABAA receptor and shows higher lipid solubility and potency than propofol, with less lipids from ciprofol reaching the circulatory system compared to propofol for the same level of anaesthesia (7). Additionally, ciprofol demonstrates clinical advantages including a lower incidence of injection pain and a smooth onset of action (8). Studies have shown that low-dose propofol (when not used as the primary anesthetic) has a certain anti-nausea and vomiting effect, which can effectively prevent PONV under general anaesthesia of remimazolam (9). It is still unclear whether low-dose ciprofol (when not used as the primary anesthetic) has the effect of preventing PONV.
Therefore, we conducted this randomized, controlled study,the aim of this study is to observe the effect of low-dose ciprofol (when not used as the primary anesthetic) immediately after the start of surgery reduces the incidence of PONV, so as to provide a new and effective method of preventing PONV.
2 Methodology
The manuscript was written in accordance with the CONSORT statement guideline for a randomized controlled trial.
2.1 Ethical considerations
We conducted this study in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Weifang People’s Hospital (Ethics No. KYLL20231009-2) and registered with the China Clinical Trial Registry (ChiCTR2300077247; https://www.chictr.org.cn). From November, 2023 to January, 2024, the study was conducted in the department of anaesthesiology, Weifang People’s Hospital, Weifang City, China, where the registration was carried out and informed consent was signed with the patients.
2.2 Patient inclusion criteria
Patients undergoing gynecological day surgery in Weifang People’s Hospital were selected, and the inclusion criteria were ASAI-II, 18–65 years old, and BMI 18-28 kg/m2. Exclusion criteria were a history of preoperative sedation and analgesics, patients with allergies to the study drug, hearing abnormalities, patients with surgery time of less than 10 min or more than 1 h, patients with additional diploids after surgery, and patients with missing follow-up.
2.3 Randomization and blinding
Randomization was performed by an independent investigator using SPSS 25.0 software (IBM Corporation, New Orchard Road, Armonk, NY; https://www.ibm.com/products/spss-statistics) with a random number table method, allocating participants at a 1:1 ratio into either the ciprofol group or the saline control group. Patients were blinded to group assignment, while anesthesiologists were aware of their allocation. Data collection was performed by an anesthetist assistant blinded to group assignments. All anesthetic procedures were administered by the same anesthesia team.
2.4 Methods of anaesthesia
All patients complied with standardized preoperative fasting protocols: a minimum fasting duration of 6–8 h for solid foods and ≥ 2 h for clear fluids before anesthesia induction. Forearm venous access is established after the patient is admitted, and a multifunctional monitor (mindray BeneVision N17) was connected to monitor the electrocardiogram (ECG), noninvasive blood pressure (NIBP), heart rate (HR), pulse saturation (SpO2), and anaesthesia depth index (BIS). Dexamethasone 5 mg and flurbiprofen 50 mg were administered before induction of anaesthesia.
Both groups were induced by remimazolam 6 mg/kg/h infusion until falling asleep (call without opening eyes), followed by alfentanil 20ug/kg and mivacurium chloride 0.2 mg/kg injected slowly (30 s each). After 3 min of assisted respiration, a laryngeal mask was placed and mechanical ventilation maintained ETCO2 35–45 mmHg. Anaesthesia was maintained by continuous intravenous remimazolam 1 mg/kg/h and alfentanil 40ug/kg/h to maintain BIS values between 40 and 60. In the ciprofol group, 2 mL of ciprofol (5 mg) was given at 5 min after the start of surgery. In the control group, 2 mL of saline was given at 5 min after the start of surgery.
Bradycardia (HR < 50 beats min−1 for at least 1 min) and hypotension (SBP below <90 mmHg or ≥30% lower than preoperative or mean arterial pressure <60 mmHg) are treated symptomatically with atropine 0.3 mg or ephedrine 6 mg during surgery. Esmolol was given to treat tachycardia (HR > 100 beats min−1 for at least 1 min) and hypertension (SBP above >140 mmHg or ≥30% higher than preoperative or mean arterial pressure >110 mmHg) was decreased with urapidil. The drug was stopped at the end of the surgery, and When the patient wakes up, the laryngeal mask was removed, and the patient was sent to the post-anaesthesia care unit (PACU). Patients can be returned to the ward after being observed in the PACU for at least 30 min and having an Aldrete score of ≥ 9. Discharged after meeting the discharge criteria of PADS≥9.
All patients were followed up by a blinded evaluator on the second day after surgery through a questionnaire or a telephone form,and they need to answer two questions: Q1. Have you vomited or had dry-retching? Q2. Have you experienced a feeling of nausea (“an unsettled feeling in the stomachand slight urge to vomit”)? If yes, has your feeling of nausea interfered with activities of daily living, such as being able to get out of bed, being able to move about freely in bed, being able to walk normally, or eating and drinking (10)?
Basic information about the patients was obtained through preoperative anaesthesia clinic assessment, intraoperative anaesthesia monitoring, inpatient electronic medical records, and observation records in the PACU.
2.5 Observation indicators
The primary outcome was the incidence of PONV in the PACU. Secondary outcomes included the incidence of emetic episodes or nausea in the PACU and within 24 h, anesthetic time, wake-up time, and administered doses of remimazolam and alfentanil. Safety outcomes included hypotension (SBP below <90 mmHg or ≥30% lower than preoperative or mean arterial pressure <60 mmHg), hypertension (SBP above >140 mmHg or ≥30% higher than preoperative or mean arterial pressure >110 mmHg), bradycardia (HR < 50 beats min−1 for at least 1 min), tachycardia (HR > 100 beats min−1 for at least 1 min) during anaesthesia.
2.6 Sample size calculation
PASS 15.0 software (https://www.ncss.com/online-store/) was used for sample size calculation, assuming a typeIerror of 0.05 (bilateral) and a test efficacy of 90%. Based on preliminary trial results, 3 of 22 patients (13.6%) in the ciprofol group experienced nausea and vomiting, whereas 10 of 21 patients (47.6%) in the normal saline group developed these symptoms, and the sample size was calculated to be at least 34 cases in each group, taking into account a possible 15% loss to follow-up, resulting in the final inclusion of 80 patients, 40 cases in each group.
2.7 Statistical analysis
In this study, SPSS 25.0 software (IBM Corporation, New Orchard Road, Armonk, NY; https://www.ibm.com/products/spss-statistics) was used for statistical analysis of data. Data distribution was assessed using the ShapiroeWilk test. Continuous variables with a normal distribution are expressed as means (SD), non-normal variables are reported as medians [interquartile range (IQR)] and count data results are expressed as frequency (%). Comparisons between groups were performed using the chi-square test, Fisher’s exact test, or rank-sum test. The prophylaxis effect of ciprofol vs. control was assessed by Risk Ratio (RR) and its 95% confidence interval (CI). A two-sided p < 0.05 was considered as the difference was statistically significant.
3 Results
3.1 Patient condition
The recruitment period was from November 2023 to January 2024, a total of 80 patients were recruited (Figure 1), 2 patients were excluded (One patient was excluded due to analgesic use for lower abdominal pain, while another was excluded for regularly taking sedative medication before sleep to manage chronic insomnia), 78 patients were randomly included in the study, due to 3 patients lost follow-up, and finally 75 patients were included in the statistical analysis.
Figure 1

Flow chart of the experiment.
3.2 Baseline and perioperative characteristics
The baseline characteristics of the two subject groups were balanced in Table 1. The median age (IQR) was 40 (35.00–49.00) years in the ciprofol group and 41(35.25–48.00) years in the control group. Body weight and BMI were comparable between groups, with the ciprofol group showing a mean body weight of 59.97 kg and a median BMI (IQR) of 22.95 (22.03–24.14) kg/m2, while the control group had a mean body weight of 58.51 kg and a median BMI (IQR) of 22.24 (20.15–24.85) kg/m2. All subjects were classified as ASA class 1–2. Preoperative Apel scores were evenly distributed, with 21 patients scoring 1–2 points and 16 scoring 3–4 points in the ciprofol group, compared to 23 and 15 patients in the control group, respectively. Additionally, no significant difference was observed in surgical categories between the two groups.
Table 1
| Variables | Ciprofol group (n = 37) | Control group (n = 38) | P |
|---|---|---|---|
| Age [years, M (Q1 ~ Q3)] | 40 (35.00–49.00) | 41 (35.25 to 48.00) | 0.981 |
| Weight (kg, x ± S) | 59.97 (4.18) | 58.51 (6.84) | 0.272 |
| BMI [kg/m2, M(Q1 ~ Q3)] | 22.95 (22.03 to 24.14) | 22.24 (20.15 to 24.85) | 0.350 |
| ASA [example (%)] | |||
| I | 7 (18.9) | 8 (21.1) | 0.819 |
| II | 30 (81.1) | 30 (78.9) | |
| Apfel score [example (%)] | |||
| 1–2 | 21 (56.8) | 23 (60.5) | 0.742 |
| 3–4 | 16 (43.2) | 15 (39.5) | |
| Surgery category [example (%)] | |||
| Hysteroscopy | 29 (78.4) | 28 (73.7) | 0.636 |
| Conization | 8 (21.6) | 10 (26.3) |
General information of patients.
Data are presented as mean (SD), median (interquartile range), or n (%).
BMI, body mass index; ASA, American society of anesthesiologists; PONV, postoperative nausea and vomiting.
3.3 Primary outcome
The incidence of PONV in the PACU in the ciprofol group was 16.2% significantly lower than 52.6% in the control group [6 (16.2%) vs 20 (52.6%); RR = 0.31; 95% CI, 0.14–0.68; ARR = 0.364; p = 0.002] (Table 2).
Table 2
| Ciprofol group (n = 37) | Control group (n = 38) | Risk ratio (95% CI) | P | |
|---|---|---|---|---|
| Primary outcome | ||||
| PONV in the PACU [example (%)] | 6 (16.2) | 20 (52.6) | 0.31 (0.14 to 0.68) | 0.002* |
| Secondary outcomes | ||||
| Emetic episodes [example (%)] | ||||
| PACU | 4(10.8) | 15 (39.5) | 0.27 (0.10 to 0.75) | 0.005* |
| 0-24 h | 8(21.6) | 15 (39.5) | 0.55 (0.26 to 1.14) | 0.084 |
| Nausea [example (%)] | ||||
| PACU | 6 (16.2) | 20 (52.6) | 0.31 (0.14 to 0.68) | 0.002* |
| 0-24 h | 19 (51.4) | 21(55.3) | 0.93 (0.61 to 1.42) | 0.736 |
| Anaesthesia time [min, M (Q1 ~ Q3)] | 20.00 (14.00 to 28.00) | 23.00 (18.25 to 29.00) | - | 0.146 |
| Wake-up time [min, M (Q1 ~ Q3)] | 6.00 (5.00 to 7.00) | 6.00 (5.00 to 6.75) | - | 0.382 |
| Remimazolam dosage [mg, M (Q1 ~ Q3)] | 18.00 (11.00 to 27.80) | 16.50 (12.13 to 22.83) | - | 0.463 |
| Alfentanil dosage [mg, M (Q1 ~ Q3)] | 0.72 (0.44 to 1.04) | 0.56 (0.42 to 0.88) | - | 0.214 |
| Safety outcomes | ||||
| Hypotension [example (%)] | 8(21.6) | 7 (18.4) | 1.17 (0.47 to 2.91) | 0.781 |
| Hypertension [example (%)] | 2(5.4) | 0 | - | 0.149 |
| Bradycardia [example (%)] | 2(5.4) | 5 (13.2) | 0.41 (0.09 to 1.99) | 0.430 |
| Tachycardia [example (%)] | 1(2.7) | 1 (2.6) | 1.03 (0.07 to 15.82) | 1.000 |
Primary, secondary, and safety outcomes.
Data are median (interquartile range) or n (%). *Significance difference in comparison with control group (P < 0.05).
PONV, postoperative nausea and vomiting; CI, confidence interval.
3.4 Secondary outcomes
Outcomes for nausea or emetic episodes are shown in Table 2 and Figure 2. The occurrence frequency of emetic episodes in the ciprofol group was lower in the PACU [4 (10.8%) vs 15 (39.5%); RR = 0.27; 95% CI, 0.10–0.75, ARR = 0.287; p = 0.005], The occurrence frequency of nausea in the ciprofol group was lower in the PACU [6 (16.2%) vs 20 (52.6%); RR = 0.31; 95% CI, 0.14–0.68; ARR = 0.364; p = 0.002]. The frequency of nausea or emetic episodes was similar in the 24 h after surgery. There was no significant difference in anesthesia time, wake-up time, remimazolam and alfentanil dosage between the two groups (p > 0.05).
Figure 2
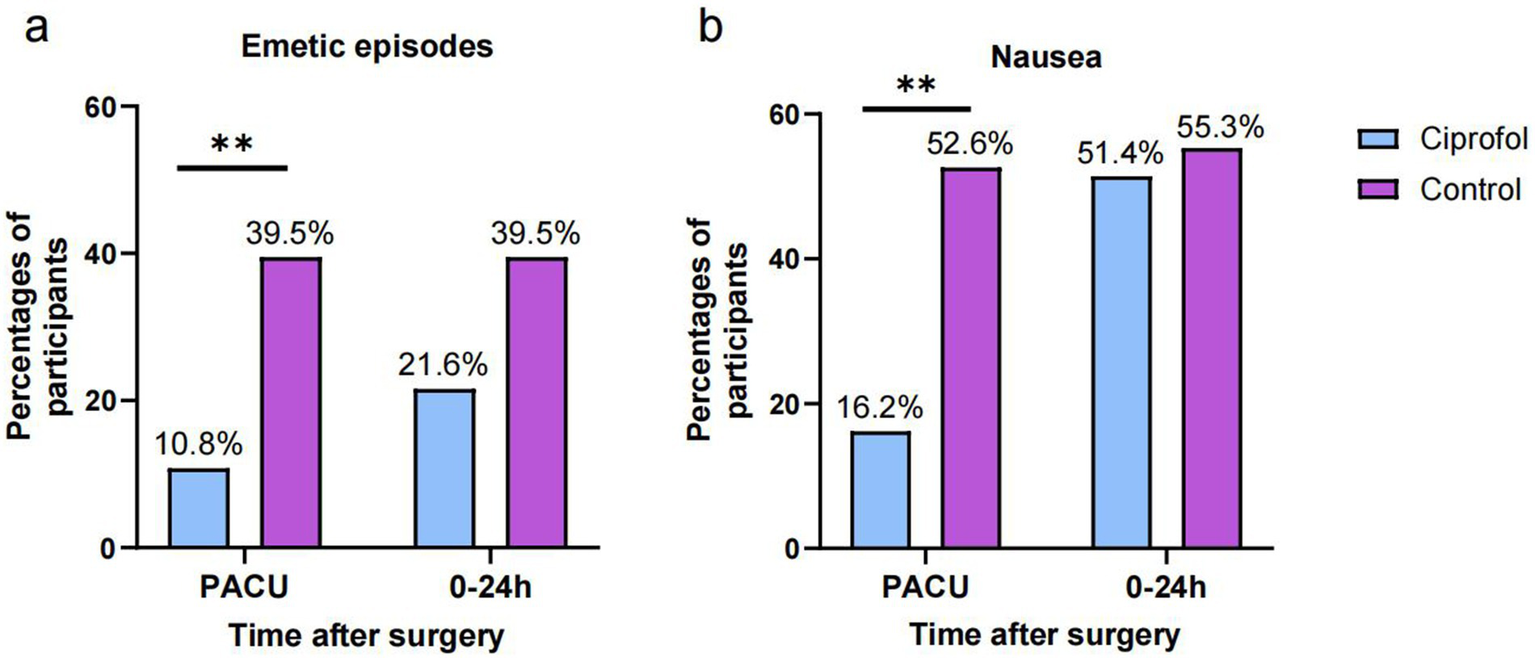
The rates of emetic episodes and nausea in the PACU and during 0–24 after surgery. (A) the rates of emetic episodes; (B) the rates of nausea; Significance was determined by two-tailed X2 test. *p < 0.05; **p < 0.01.
3.5 Safety outcomes
There was no significant difference in safety outcomes between the two groups (p > 0.05). Hypotension occurred in 8 cases (21.6%) in the ciprofol group and 7 cases (18.4%) in the control group. Hypertension and tachycardia are uncommon (Table 2).
4 Discussion
In adult patients undergoing gynecological ambulatory surgery, we report for the first time that adding low-dose ciprofol to remimazolam-alfentanil anesthesia significantly reduces both the incidence and severity of PONV in the PACU. However, no significant efficacy was observed for emetic episodes or nausea within 24 h postoperatively. These findings suggest that low-dose ciprofol provides short-term prophylaxis against PONV, offering clinical benefits in high-volume ambulatory centers with constrained PACU resources through accelerated turnover, optimized nursing allocation, and reduced hospitalization costs. The lack of sustained antiemetic effect beyond 24 h may be attributable to its pharmacokinetic profile. Sole reliance on low-dose ciprofol for PONV prophylaxis could compromise patient comfort, necessitating combination therapy with longer-acting antiemetics for extended protection.
PONV is one of the common complications after anaesthesia and surgery, and women are one of the important risk factors for the occurrence of PONV (11). Most patients undergoing hysteroscopy surgical treatment are young women, and the occurrence of PONV after hysteroscopy surgery may be related to the large release of neurotransmitters such as 5-hydroxytryptamine caused by postoperative uterine contraction pain and the use of intraoperative opioids, which can stimulate the body’s chemoreceptor trigger zone and vomiting centre, causing the nausea and vomiting reflex (12). Day surgery has a short duration, but adverse reactions such as PONV can affect patients’ postoperative recovery, and how to reduce the incidence of PONV is important for improving patient prognosis and patient recovery.
Remimazolam belongs to the new short-acting benzodiazepine sedatives, which are metabolized by non-specific plasma esterase hydrolysis, with a rapid onset of action, short half-life, and rapid awakening after discontinuation (13). However, Yuji Suzuki and colleagues in a single-centre retrospective cohort study found a higher incidence of PONV after remimazolam anaesthesia than propofol anaesthesia (5). Alfentanil is a fentanyl derivative acting at the μ receptor, a short-acting strong opioid analgesic with the advantages of fast onset, short duration of action, rapid elimination, and no accumulation, and it is suitable for use in gynaecological hysteroscopy surgery in which the operative time is short and the rhythm is fast, and it has a low incidence of PONV when compared with sufentanil and fentanyl (3).
Propofol is one of the most commonly used intravenous anaesthetics and can directly inhibit the vagal nucleus, the central emetic chemoreceptor area, and can also act as an antiemetic through the modulation of subcortical structures and pathways (14). Borgeat and colleagues concluded that the antiemetic effect of propofol can be exerted in concentrations lower than the sedative effect (15). A study of the Cechetto DF found that the reduced levels of serotonin in the area postrema and the cerebrospinal fluid may explain the antiemetic property of propofol, propofol may also directly act on area postrema neurons via a GABAA receptor to reduce their activity (16). Ciprofol is a new short-acting GABAA receptor agonist. The introduction of a cyclopropyl group to the chemical structure of propofol results in a chiral structure that increases the steric effect and thus enhances its affinity for the GABAA receptor (6). Ciprofol is approximately 4–6 times more potent than propofol, with a smooth onset of action, and a very low incidence of injection pain (8). Our team’s studies have confirmed that ciprofol has a similar anaesthetic effect in gynaecological day surgery compared to propofol, and that the incidence of adverse events was lower in the ciprofol group (17). This study revealed a 16.2% incidence of PONV in the PACU with low-dose ciprofol, aligning with our team’s prior findings demonstrating that low-dose propofol significantly reduces PACU PONV incidence (10.6%) following remimazolam-alfentanil anesthesia (9). Furthermore, an outpatient hysteroscopy study showed comparable PONV incidence between ciprofol and propofol groups at both 1 h and 24 h postoperatively (18). Collectively, these observations suggest ciprofol may share similar mechanisms with propofol for PONV prophylaxis, warranting further pharmacokinetic investigations to elucidate the underlying pharmacological basis.
In this study, we found that there was no significant difference in the incidence of emetic episodes or nausea within 24 h after surgery, and it can be inferred that ciprofol has a limited time to prevent emetic episodes or nausea and cannot effectively reduce the occurrence and severity of emetic episodes or nausea within 24 h. This is similar to the results of the study of Xiao HY in the study of low-dose propofol for the prevention of nausea or vomiting after general anaesthesia with remimazolam and alfentanil (9). This phenomenon may be attributed to ciprofol’s pharmacokinetics, characterized by triexponential elimination with corresponding half-lives of 2.0 min (t1/2,α), 34.9 min (t1/2,β), and 6.2 h (t1/2,γ). The clinical effects demonstrate dose dependency (19, 20). Potentially explaining why low-dose ciprofol provides only transient antiemetic efficacy. Clinically, proactive co-administration with antiemetics is warranted to prevent prolonged emetic episodes or nausea. Furthermore. The occurrence of emetic episodes or nausea may increase in patients due to the possibility of using transportation such as cars when they are discharged from the hospital within 24 h. This study also suggests that continued attention should be given to the prevention of emetic episodes or nausea in patients undergoing gynaecological day surgery. Further studies are needed to determine whether the mechanism of action of ciprofol in preventing emetic episodes or nausea is similar to that of propofol. There was no significantly difference in the wake-up time between the two groups, indicating that low-dose ciprofol given during surgery did not prolong the wake-up time.
This study still has some limitations. Firstly, this study was a single-centre study with a relatively small sample size, which may have some selection bias, and the influencing factors of PONV were not further analysis, and it is necessary to further validate the present results in a multi-centre, large-sample study. Secondly, this study had a relatively short observation period, and a longer follow-up observation period is needed, and patient satisfaction or recovery quality score surveys need to be increased to gain a more comprehensive understanding of patient recovery. Thirdly, we only recruited gynecological day surgery patients, which limits the universality,and it is necessary to expand the range of surgical types for further research. Fourth, while this study studies the short-term effects of a single dose of low-dose ciprofol administration, future systematic pharmacokinetic studies are warranted to comprehensively characterize its metabolic trajectory and elimination profile.
5 Conclusion
In conclusion,low-dose ciprofol can effectively prevent PONV in PACU after gynecological day surgery under general anaesthesia remazolam combined with afentanil, but its effect is limited and cannot reduce the incidence of emetic episodes or nausea within 24 h after surgery. This finding underscores the importance of implementing a full-period antiemetic strategy during day surgery. Future research should focus on clarifying its mechanism, exploring the synergistic effects with long-acting antiemetic drugs, and verifying their application value in a wider population.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Medical Research Ethics Committee of Weifang People’s Hospital/Weifang People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XS: Writing – original draft, Visualization, Conceptualization, Methodology, Project administration, Writing – review & editing, Investigation. ZQ: Writing – review & editing, Validation, Supervision, Investigation, Conceptualization. YW: Formal analysis, Investigation, Writing – review & editing, Data curation. HX: Methodology, Writing – review & editing, Project administration, Conceptualization. RZ: Writing – review & editing, Investigation, Formal analysis, Data curation. GZ: Supervision, Investigation, Writing – review & editing, Data curation. MZ: Data curation, Supervision, Conceptualization, Writing – review & editing. AM: Supervision, Investigation, Data curation, Writing – review & editing. FY: Conceptualization, Writing – review & editing, Software, Data curation. FJ: Writing – review & editing, Project administration, Conceptualization, Supervision. PN: Supervision, Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank all the subjects and their families, and all the investigators and site personnel for participating in this trial.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ASA, American Society of Anesthesiologists; PONV, postoperative nausea and vomiting; PACU, Postanesthesia care unit; BMI, Body Mass Index.
References
1.
Gran Bruun AM Svensen K Johansen E Halstensen TD Gustavsson A Leonardsen ACL . A quantitative, multicentre, longitudinal study of patient experiences after gynaecological day surgery. Nurs Open. (2023) 10:1536–44. doi: 10.1002/nop2.1403
2.
Schüttler J Eisenried A Lerch M Fechner J Jeleazcov C Ihmsen H . Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: part I. Pharmacokinetics and clinical pharmacodynamics. Anesthesiology. (2020) 132:636–51. doi: 10.1097/ALN.0000000000003103
3.
Li Z Xiao H Zhu T Yue F Fu M Ji T . Observation on the application effect of alfentanil compounded with propofol in anaesthesia for daytime hysteroscopy surgery. J Shandong Med. (2022) 62:72–5. doi: 10.3969/j.issn.1002-266X.2022.09.018
4.
Yi F Xiao H Zhu T Man Y Ji F . Prevention of postoperative nausea and vomiting after gynaecological day surgery under remimazolam general anesthesia: a randomized double-blind controlled study. BMC Anesthesiol. (2022) 22:2922022 Sep 15. doi: 10.1186/s12871-022-01835-x
5.
Suzuki Y Kawashima S Makino H Doi M Nakajima Y . Comparison of postoperative nausea and vomiting between remimazolam and propofol: a propensity score-matched, retrospective, observational, single-center cohort study. Korean J Anesthesiol. (2023) 76:143–51. doi: 10.4097/kja.22441
6.
Lu M Liu J Wu X Zhang Z . Ciprofol: A Novel Alternative to Propofol in Clinical Intravenous Anesthesia?Biomed Res Int. (2023) 2023:7443226. doi: 10.1155/2023/7443226
7.
Liao J Li M Huang C Yu Y Chen Y Gan J et al . Pharmacodynamics and pharmacokinetics of HSK3486, a novel 2,6-disubstituted phenol derivative as a general Anesthetic. Front Pharmacol. (2022) 13:830791. doi: 10.3389/fphar.2022.830791
8.
Chen BZ Yin XY Jiang LH Liu JH Shi YY Yuan BY . The efficacy and safety of ciprofol use for the induction of general anesthesia in patients undergoing gynecological surgery: a prospective randomized controlled study. BMC Anesthesiol. (2022) 22:245. doi: 10.1186/s12871-022-01782-7
9.
Xiao H Liu M Man Y Wei Y Ji F . Effect of low-dose propofol combined with dexamethasone on the prevention of postoperative nausea and vomiting in gynaecological day surgery under remimazolam-based general anesthesia. Medicine (Baltimore). (2023) 102:e33249. doi: 10.1097/MD.0000000000033249
10.
Myles PS Wengritzky R . Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br J Anaesth. (2012) 108:423–9. doi: 10.1093/bja/aer505
11.
Choy R Pereira K Silva SG Thomas N Tola DH . Use of Apfel simplified risk score to guide postoperative nausea and vomiting prophylaxis in adult patients undergoing same-day surgery. J Perianesth Nurs. (2022) 37:445–51. doi: 10.1016/j.jopan.2021.10.006
12.
Shaikh SI Nagarekha D Hegade G Marutheesh M . Postoperative nausea and vomiting: a simple yet complex problem. Anesth Essays Res. (2016) 10:388–96. doi: 10.4103/0259-1162.179310
13.
Hu Q Liu X Wen C Li D Lei X . Remimazolam: an updated review of a new sedative and anaesthetic. Drug Des Devel Ther. (2022) 16:3957–74. doi: 10.2147/DDDT.S384155
14.
Kampo S Afful AP Mohammed S Ntim M Buunaaim ADB Anabah TW . Sub-hypnotic dose of propofol as antiemetic prophylaxis attenuates intrathecal morphine-induced postoperative nausea and vomiting, and pruritus in parturient undergoing cesarean section - a randomized control trial. BMC Anesthesiol. (2019) 19:177. doi: 10.1186/s12871-019-0847-y
15.
Borgeat A Wilder-Smith OH Saiah M Rifat K . Subhypnotic doses of propofol possess direct antiemetic properties. Anesth Analg. (1992) 74:539–41. doi: 10.1213/00000539-199204000-00013
16.
Cechetto DF Diab T Gibson CJ Gelb AW . The effects of propofol in the area postrema of rats. Anesth Analg. (2001) 92:934–42. doi: 10.1097/00000539-200104000-00027
17.
Man Y Xiao H Zhu T Ji F . Study on the effectiveness and safety of ciprofol in anesthesia in gynecological day surgery: a randomized double-blind controlled study. BMC Anesthesiol. (2023) 23:92. doi: 10.1186/s12871-023-02051-x
18.
Zhang H Zhang M Hao L Li Q Li Q Yang J et al . Comparison of the effects of Ciprofol and propofol on postoperative nausea and vomiting in patients undergoing outpatient hysteroscopy. Drug Des Devel Ther. (2024) 18:5701–7. doi: 10.2147/DDDT.S489223
19.
Bian Y Zhang H Ma S Jiao Y Yan P Liu X et al . Mass balance, pharmacokinetics and pharmacodynamics of intravenous HSK3486, a novel anaesthetic, administered to healthy subjects. Br J Clin Pharmacol. (2021) 87:93–105. doi: 10.1111/bcp.14363
20.
Expert Panel . Clinical practice guidelines for ciprofol administration. Chin J Anesthesiol. (2021) 41:129–32. doi: 10.3760/cma.j.cn131073.20201011.00201
Summary
Keywords
ciprofol, remimazolam, alfentanil, day surgery, postoperative nausea and vomiting
Citation
Shi X, Qi Z, Wei Y, Xiao H, Zhang R, Zhuang G, Zhuang M, Mou A, Yue F, Ji F and Nie P (2025) Effect of low-dose ciprofol on postoperative nausea and vomiting following gynecologic day surgery: a randomized controlled trial. Front. Med. 12:1612322. doi: 10.3389/fmed.2025.1612322
Received
15 April 2025
Accepted
19 August 2025
Published
05 September 2025
Volume
12 - 2025
Edited by
Christian Bohringer, UC Davis Medical Center, United States
Reviewed by
Firoozeh Madadi, Shahid Beheshti University of Medical Sciences, Iran
Takehito Sato, Nagoya University Hospital, Japan
Kuo-Chuan Hung, Chi Mei Medical Center, Taiwan
Updates
Copyright
© 2025 Shi, Qi, Wei, Xiao, Zhang, Zhuang, Zhuang, Mou, Yue, Ji and Nie.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fanceng Ji, jifanceng@163.com; Peihe Nie, peihenie@126.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.