- 1The Second Affiliated Hospital of Zunyi Medical University, Zunyi, Guizhou, China
- 2Nursing School of Zunyi Medical University, Zunyi, Guizhou, China
- 3The Affiliated Hospital of Zunyi Medical University, Zunyi, Guizhou, China
- 4Department of Nursing, Zhejiang Cancer Hospital, Hangzhou, Zhejiang, China
Objectives: To evaluate the effects of a 2-week graded exercise rehabilitation program on respiratory function, exercise capacity, inflammatory markers, and immune function in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD).
Methods: This is a prospective randomized controlled trial aimed at evaluating the efficacy of the graded exercise rehabilitation therapy based on the GOLD guidelines in patients with AECOPD. We divided the patients into the intervention group and the control group using the random number table method, with 35 patients in each group. The control group received conventional symptomatic treatment and exercise rehabilitation, while the intervention group underwent graded exercise rehabilitation according to the GOLD guidelines, twice a day, each session lasting 30–45 min, for a total duration of 2 weeks. After the treatment, the main indicators included serum inflammatory factors and T lymphocyte subsets. Secondary indicators included exercise endurance (6MWT), disease symptom burden (CAT), dyspnea (mMRC), self-care ability (ADL), and psychological state (HADS). The hospitalization time, duration of non-invasive mechanical ventilation, and the overall incidence of related complications were also evaluated. All evaluations were conducted 2 weeks before and after the rehabilitation treatment.
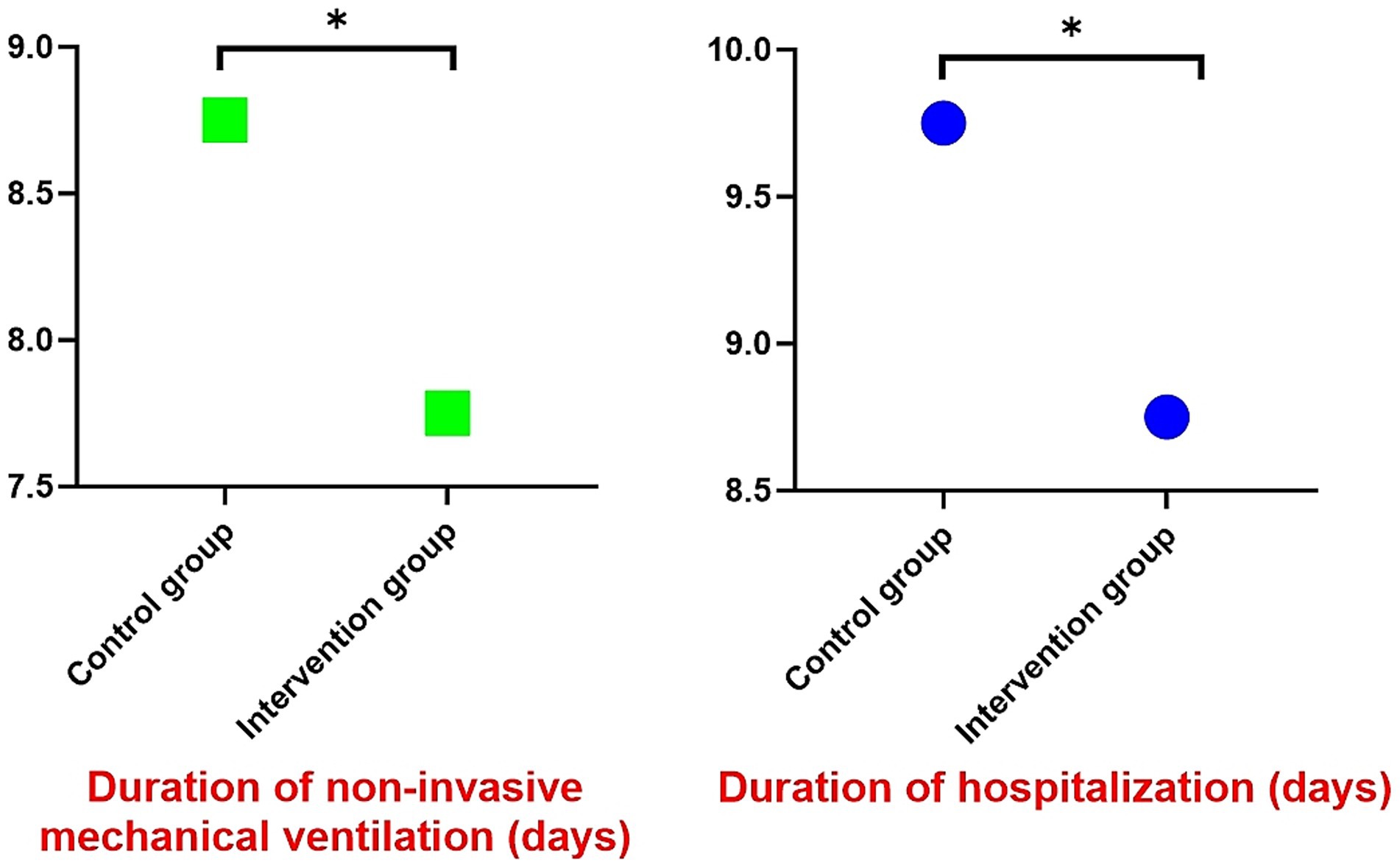
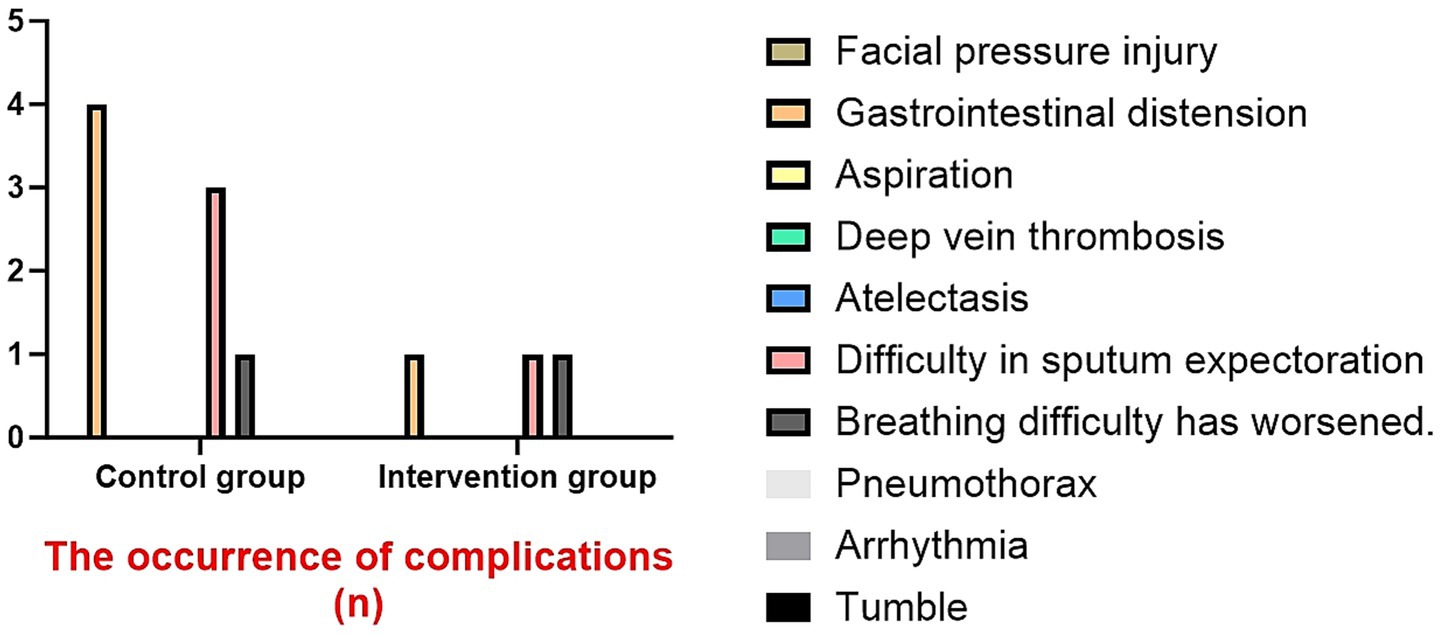
Results: Baseline characteristics were comparable between groups. Post-intervention, both groups showed significant improvements in all measured parameters (p < 0.05 vs. baseline), with superior outcomes in the intervention group: greater reductions in inflammatory markers (IL-6, IL-8, TNF-α, CRP; p < 0.05); more favorable immune profile (higher CD3+, CD4+, CD4+/CD8+ ratio; lower CD8+; p < 0.05); better functional outcomes (6MWT, mMRC, CAT, ADL, HADS; p < 0.05). The duration of non-invasive ventilation, the length of hospital stay, and the incidence of complications were all reduced.
Conclusion: The GOLD-based graded exercise rehabilitation demonstrates superior clinical efficacy compared to conventional rehabilitation for AECOPD patients, showing significant benefits in reducing systemic inflammation, improving immune function, and enhancing physical and psychological outcomes.
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic respiratory condition characterized by persistent airflow limitation, featuring progressive airflow obstruction and abnormal inflammatory responses of the lungs to noxious particles or gases (1, 2). Globally, COPD remains a leading cause of morbidity and mortality, ranking as the third most common cause of death worldwide according to WHO statistics, surpassed only by ischemic heart disease and stroke (3).
Acute exacerbations of COPD (AECOPD) are defined as acute worsening of respiratory symptoms including dyspnea, cough, and sputum production (4, 5). These exacerbations not only accelerate lung function decline but also increase risks of respiratory failure and mortality (6). Elderly AECOPD patients are particularly vulnerable due to age-related physiological decline and compromised immune function (7), necessitating special consideration during acute-phase management. However, current research has predominantly focused on pulmonary rehabilitation in stable COPD, with relatively limited evidence regarding rehabilitation during acute exacerbations.
As the cornerstone of pulmonary rehabilitation, exercise training has been proven to effectively improve patients’ respiratory function and exercise endurance (8), while reducing systemic inflammation and regulating immune responses (9). Meanwhile, studies have shown that early pulmonary rehabilitation initiated during hospitalization for AECOPD patients is beneficial, improving their quality of life, activity capacity, and reducing readmission rates and mortality (10–12). The therapeutic effect is influenced by multiple factors, including exercise mode, intensity, duration, and environment. The best outcome requires a precisely tailored and safely implemented program. Current rehabilitation programs mainly focus on exercise mode, timing, safety, and effectiveness, often neglecting the critical aspect of stratifying the severity of acute exacerbation. Based on our preliminary research, we have developed a personalized and graded exercise rehabilitation program according to the 2023 GOLD guideline classification system (13), categorizing the severity of AECOPD into three levels based on clinical manifestations and arterial blood gas analysis, thereby achieving truly dynamic and precise exercise therapy.
Emerging evidence highlights the prognostic value of inflammatory cytokines and T-cell subsets in predicting AECOPD recurrence and outcomes (14). To address current knowledge gaps, we conducted a randomized controlled trial to systematically evaluate the therapeutic effects of graded exercise rehabilitation in AECOPD patients, with particular focus on its impacts on inflammatory markers and T-lymphocyte subpopulations. This investigation aims to provide novel theoretical foundations and practical approaches for AECOPD rehabilitation, ultimately optimizing clinical management strategies and improving patients’ quality of life and long-term prognosis.
Materials and methods
Study design
This is a prospective, single-blind, randomized controlled clinical trial conducted in accordance with the CONSORT guidelines and the Helsinki Declaration. It was implemented in Guizhou, China from August 2024 to February 2025. The study has been registered in the Chinese Clinical Trial Registry (Registration Number: ChiCTR2300072409). The study has received ethical approval from the Medical Ethics Committee of the Second Affiliated Hospital of Zunyi Medical University (approval number: 2024-1-295). All participants and their families were informed of the study and signed informed consent forms.
Participants
The study population comprised patients aged 40–80 years with a confirmed COPD diagnosis per 2023 GOLD criteria, who were hospitalized for acute exacerbation (AECOPD). Eligible participants met the following criteria: (1) clear consciousness with unimpaired verbal communication; (2) no prior participation in structured exercise training programs.
Exclusion criteria: Severe cardiovascular diseases, acute exacerbation of bronchial asthma, pulmonary embolism, pneumothorax, hemoptysis, metastatic cancer, diseases affecting neuromuscular system or bone and joint disorders, limb impairments, deep vein thrombosis, immunodeficiency or low immunity patients, as well as those with poor compliance and unwillingness to cooperate.
Randomization and allocation
At baseline assessment, an independent researcher not involved in either evaluation or intervention procedures allocated participants using a computer-generated randomization table. This staff member prepared the randomization sequence in advance and assigned consecutive eligible patients according to their admission order—those corresponding to odd numbers were allocated to the control group while even numbers designated the intervention group.
Interventions
After completing the registration, eligible participants need to undergo a baseline assessment. After a rigorous evaluation, if the patient’s condition and vital signs are stable, exercise rehabilitation training will begin within 24 h after admission and will last for 2 weeks. Before each training session, vital signs and consciousness status will be evaluated.
Both groups of patients will receive the standard treatment protocol, which covers multiple aspects: For the use of antibiotics, based on the patient’s clinical symptoms, signs, and results of sputum culture and other examinations, targeted antibiotics are selected for anti-infection treatment. The treatment course is adjusted according to the severity of the condition and the treatment effect; The use of systemic corticosteroids follows relevant guidelines, and appropriate doses and treatment courses of oral or intravenous administration are given based on the patient’s condition to reduce airway inflammation. At the same time, conventional drugs such as bronchodilators, expectorants, etc. are also combined for comprehensive treatment, as well as necessary oxygen therapy and respiratory support measures.
Control group
Received standard rehabilitation comprising.
Pursed-lip breathing
Nasal inhalation followed by prolonged expiration through pursed lips (expiratory duration ≈2 × inspiratory time), administered twice daily (5–10 min/session).
Diaphragmatic breathing
Pursed-lip breathing: Performed in supine/sitting position with chest immobilization (abdominal retraction during inspiration/relaxation during expiration) at identical frequency/duration.
ADL training
Pursed-lip breathing: Self-care activities (feeding, dressing) and basic limb exercises (hand gripping, elbow flexion). Ambulatory patients progressed to walking (2 × daily, 8–12 reps/set, 2–3 sets).
Intervention group
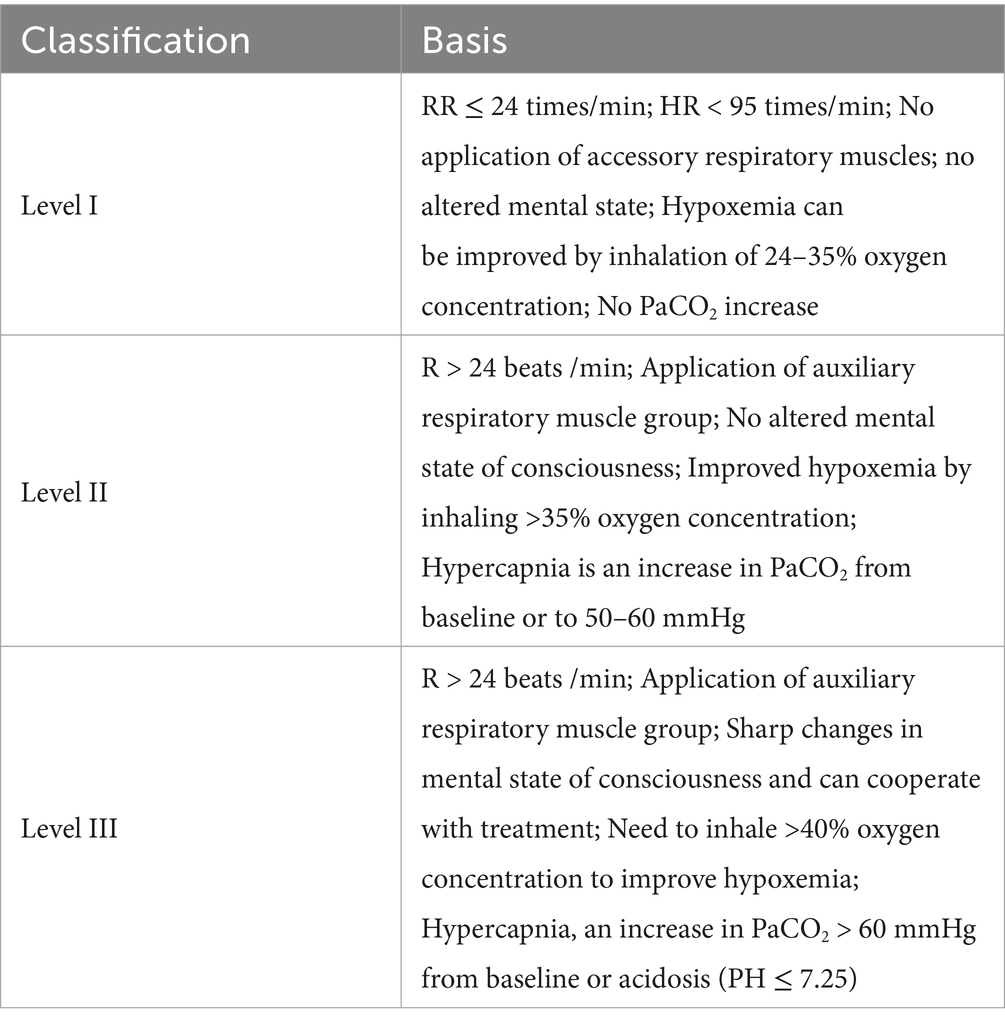
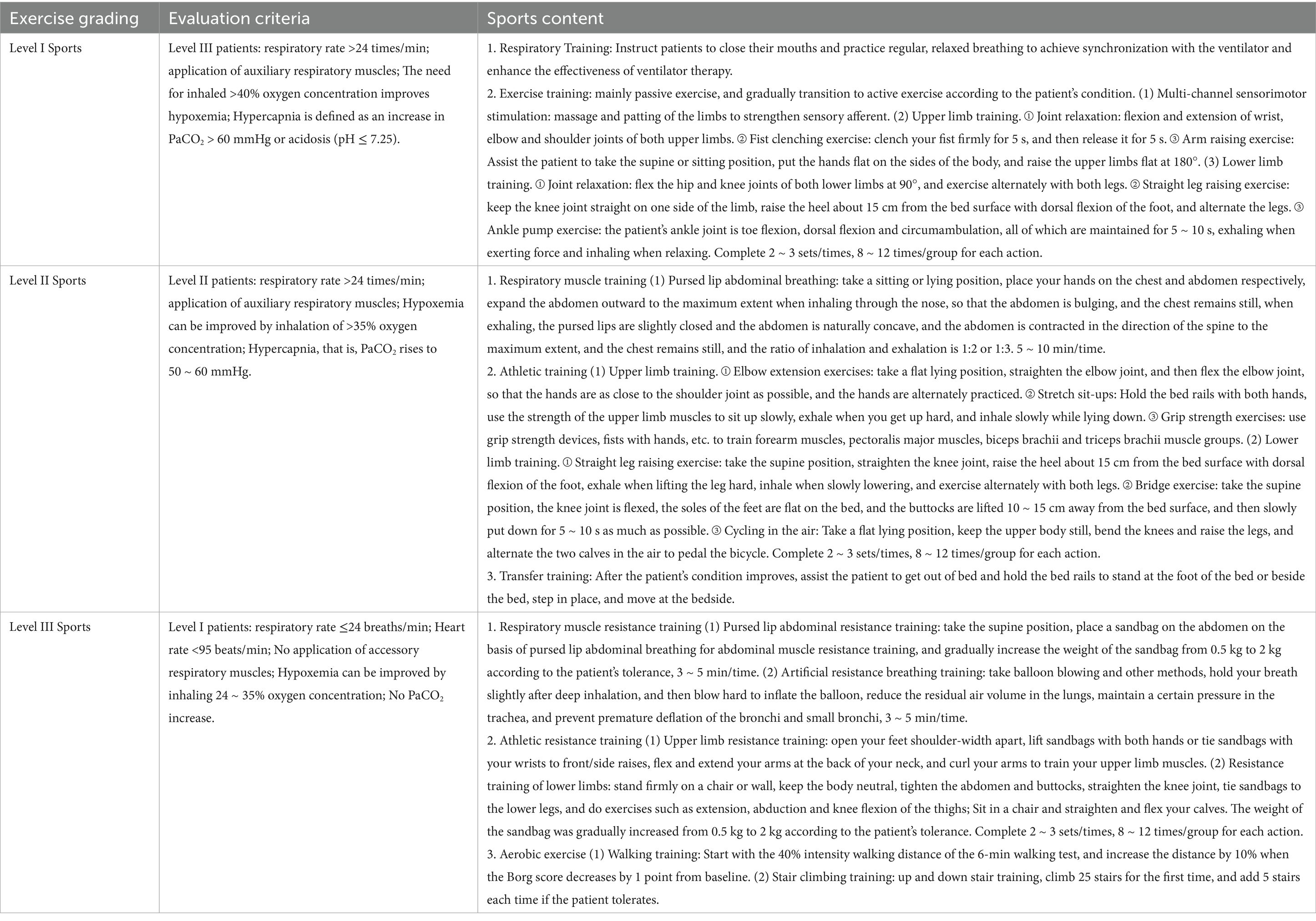
Received graded exercise rehabilitation training. The grading standard for the severity of AECOPD patients hospitalized is shown in Table 1. The specific plan is shown in Table 2.
Outcome measurement
Primary observation measures
Measurement of inflammatory markers
Fasting venous blood samples (3 mL) were collected from the antecubital vein pre- and post-intervention. Serum was isolated by centrifugation at 3000 rpm for 10 min. IL-6, IL-8, TNF-α, and hs-CRP levels were quantified using ELISA kits (Shanghai Jingkang Biological Engineering Co., Ltd.) with a Sunrise automated microplate reader (Tecan, Switzerland) via sandwich immunoassay. All procedures strictly adhered to manufacturer protocols and were performed by certified technicians.
Immunological function assessment
Fasting venous blood (5 mL) was collected in heparinized tubes and mixed thoroughly. T lymphocyte subsets (CD3+, CD4+, CD8+) and CD4+/CD8+ ratios were analyzed using a BriCyte E6 flow cytometer (Mindray, Shenzhen) with matched antibody kits (Mindray Bio-Medical Electronics Co., Ltd.). Standardized protocols were followed for.
Secondary observation measures
Exercise capacity
The 6-min walk test (6MWT) was performed along a 30-meter corridor, with continuous monitoring of walking distance, oxygen saturation (SpO2), heart rate, and exercise-induced symptoms.
Dyspnea severity
Assessed using the modified Medical Research Council (mMRC) (15) dyspnea scale (range: 0–4), where higher scores indicate greater dyspnea limitation.
Health status
The health status assessment was conducted using the Chronic Obstructive Pulmonary Disease Assessment Test (CAT) (16), with a score range of 0–40. This test mainly reflects the burden of symptoms for the patients, and the lower the score, the less the patient is affected by the disease.
Functional status
Activities of daily living (ADL) (17) were evaluated using the Barthel Index (range: 0–100), where higher scores denote greater independence.
Psychological assessment
The Hospital Anxiety and Depression Scale (HADS) (18) (range: 0–21 per subscale) evaluated. Anxiety (scores ≥8 suggestive, ≥11 diagnostic). Depression (scores ≥8 suggestive, ≥11 diagnostic).
Clinical outcomes
Duration of non-invasive ventilation (total hours), Length of hospitalization (days), Incidence of complications (%).
Statistical analysis
The data analysis was conducted by an independent statistician who was unaware of the grouping situation using SPSS 29.0. Continuous variables were expressed as mean ± standard deviation or median (quartile), and within-group comparisons were performed using paired t-test, while between-group comparisons were conducted using independent sample t-test; categorical variables were presented as number (percentage), and chi-square test was used for analysis. A difference was considered statistically significant when p < 0.05 (two-sided).
Results
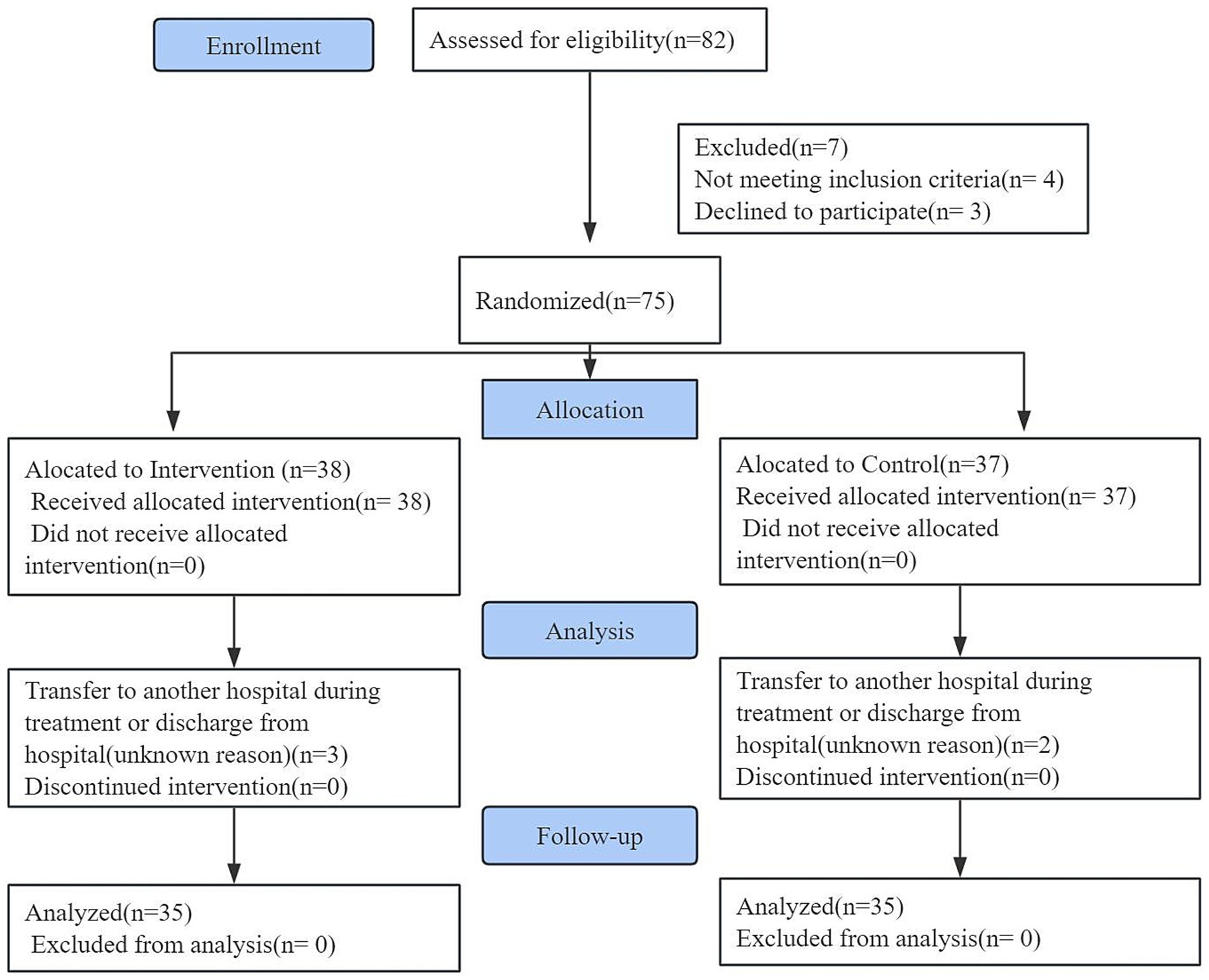
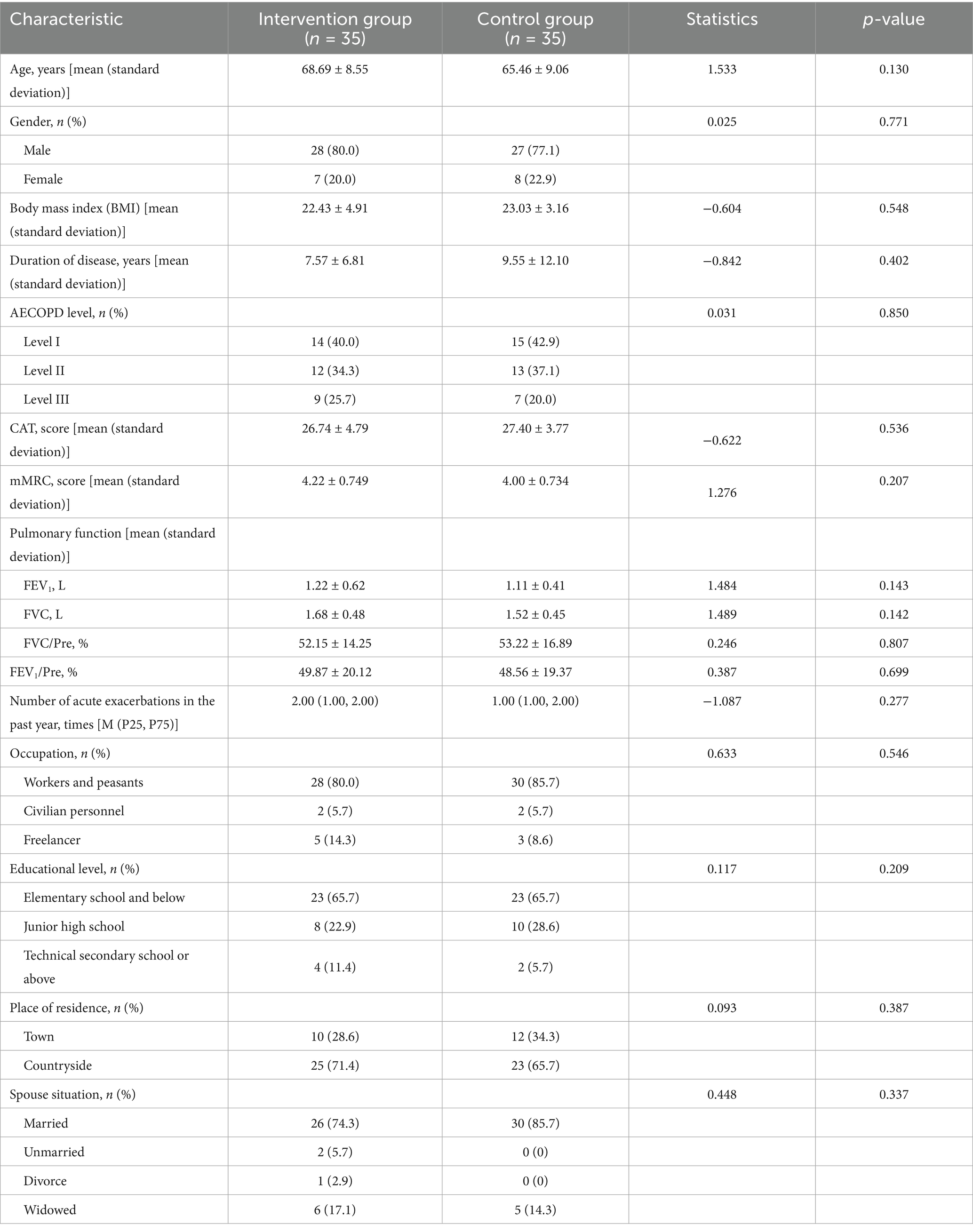
From August 2024 to February 2025, 82 patients were initially screened. After excluding 4 ineligible patients and 3 decliners, 75 participants were randomized to either the intervention (n = 38) or control group (n = 37). Five cases were subsequently lost to follow-up due to hospital transfer or discharge, yielding 35 analyzable cases per group (Figure 1). Baseline characteristics demonstrated balanced distribution between groups (p > 0.05, Table 3).
The main observation results are as follows
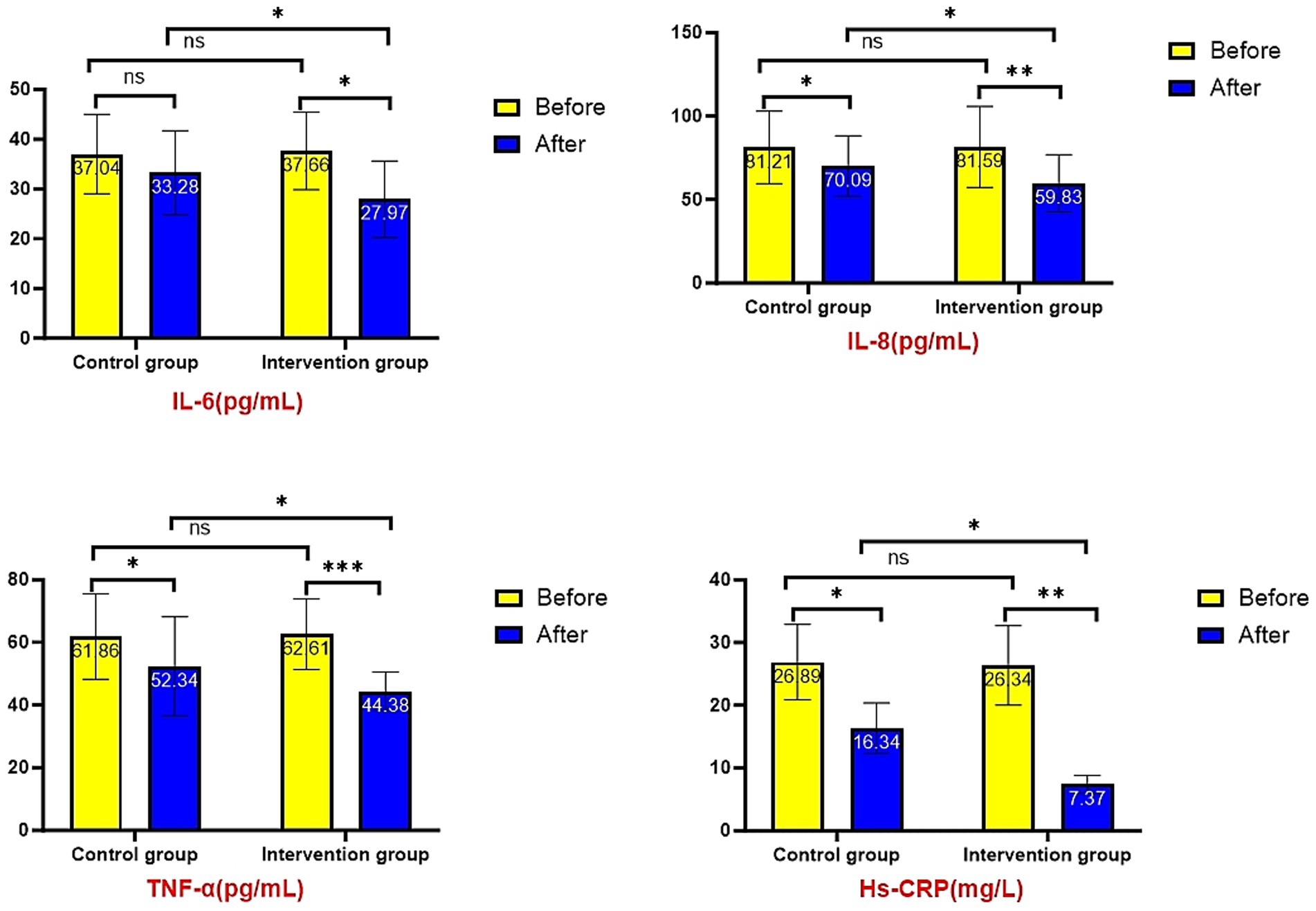
Serum inflammatory factor analysis revealed no significant intergroup differences at baseline (all p > 0.05). Post-intervention results demonstrated significantly lower levels of IL-6 (27.97 ± 7.64 vs. 33.28 ± 8.44 pg./mL, p = 0.012), IL-8 (59.83 ± 17.09 vs. 70.09 ± 18.12 pg./mL, p = 0.026), TNF-α (44.38 ± 6.14 vs. 52.34 ± 15.83 pg./mL, p = 0.016), and hs-CRP (7.37 ± 2.15 vs. 15.29 ± 4.62 mg/L, p = 0.042) in the intervention group compared to controls. Both groups showed significant improvements from baseline (p < 0.05), with greater reductions observed in the intervention group (Figure 2). (NS: not significant; *p < 0.05; **p < 0.01; ***p < 0.001. All the following expressions are like this.)
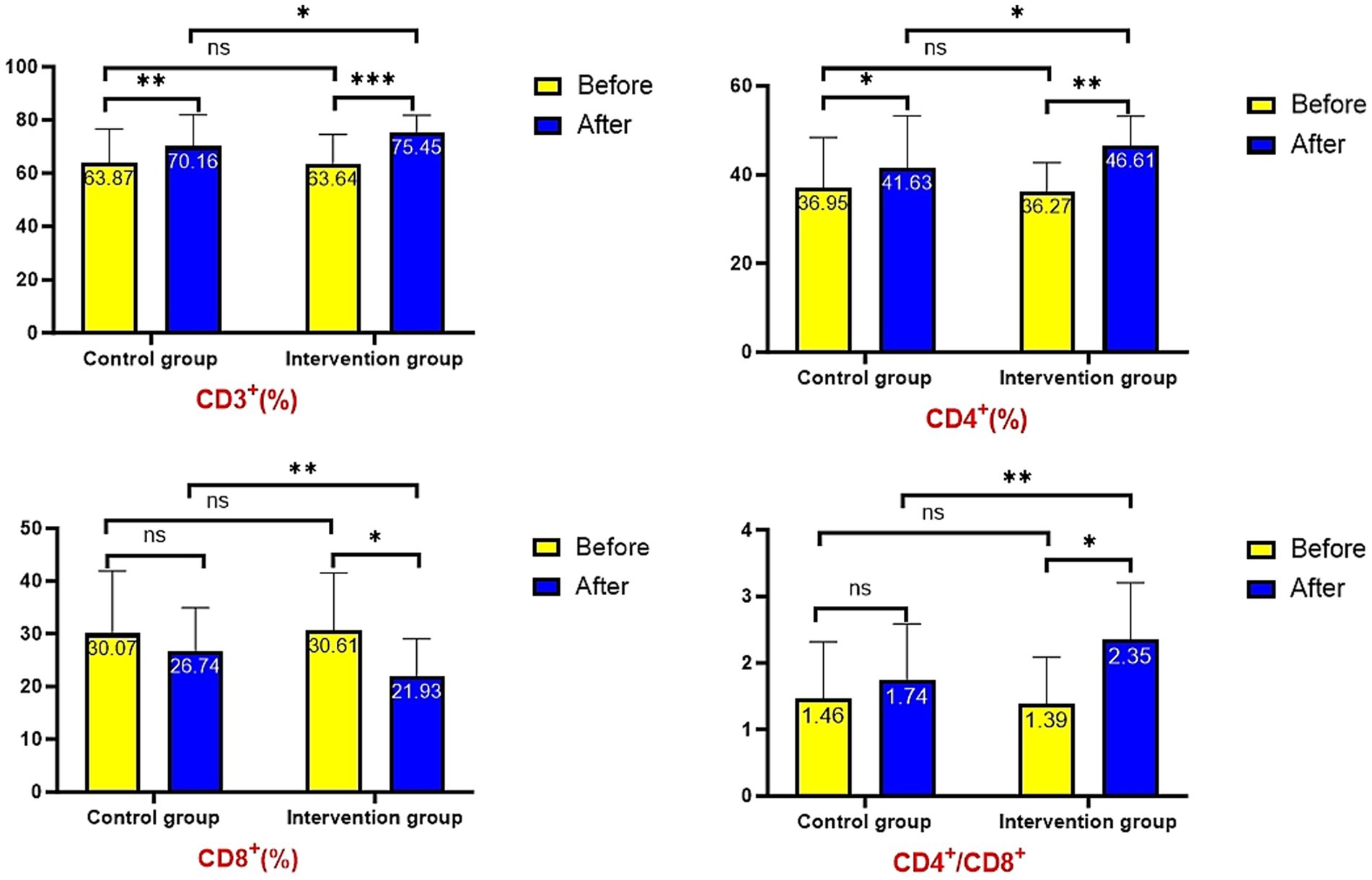
Baseline measurements showed no significant differences in T lymphocyte subsets (CD3+, CD4+, CD8+) or CD4+/CD8+ ratio between groups (p > 0.05). Post-intervention, the intervention group demonstrated significantly higher CD3+ (75.45 ± 6.37% vs. 70.16 ± 11.73%, p = 0.023), CD4+ (46.61 ± 6.57% vs. 41.63 ± 11.58%, p = 0.031), and CD4+/CD8+ ratio (2.35 ± 0.86 vs. 1.74 ± 0.85, p = 0.004), along with significantly lower CD8+ levels (21.93 ± 7.09% vs. 26.74 ± 8.18%, p = 0.011) compared to controls. Longitudinal analysis revealed significant increases in CD3+ and CD4+ levels from baseline in both groups (p < 0.05), while changes in CD8+ levels and CD4+/CD8+ ratio remained non-significant (p > 0.05, Figure 3).
The results of secondary observation indicators are as follows
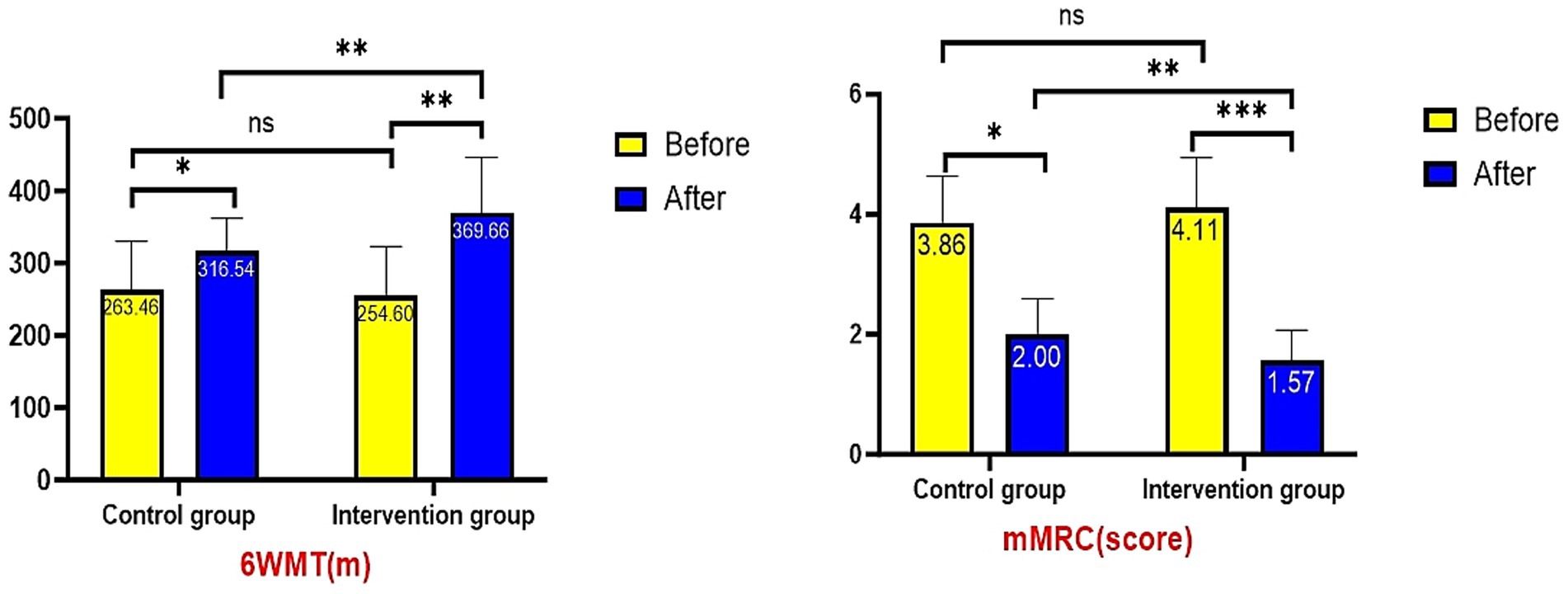
Exercise Capacity and Respiratory Function Outcomes: Post-intervention analysis revealed significantly better performance in the intervention group compared to controls for both 6-min walk test distance (369.66 ± 76.69 m vs. 316.54 ± 45.4 m, p = 0.001) and modified Medical Research Council (mMRC) dyspnea score (1.57 ± 0.5 vs. 2.00 ± 0.59, p = 0.002). Baseline measurements showed no significant differences between groups for either parameter (p > 0.05). Following treatment, both groups demonstrated significant improvements from baseline in 6WMT distance (p < 0.05) and mMRC scores (both p < 0.05), with the intervention group exhibiting greater magnitude of improvement (Figure 4).
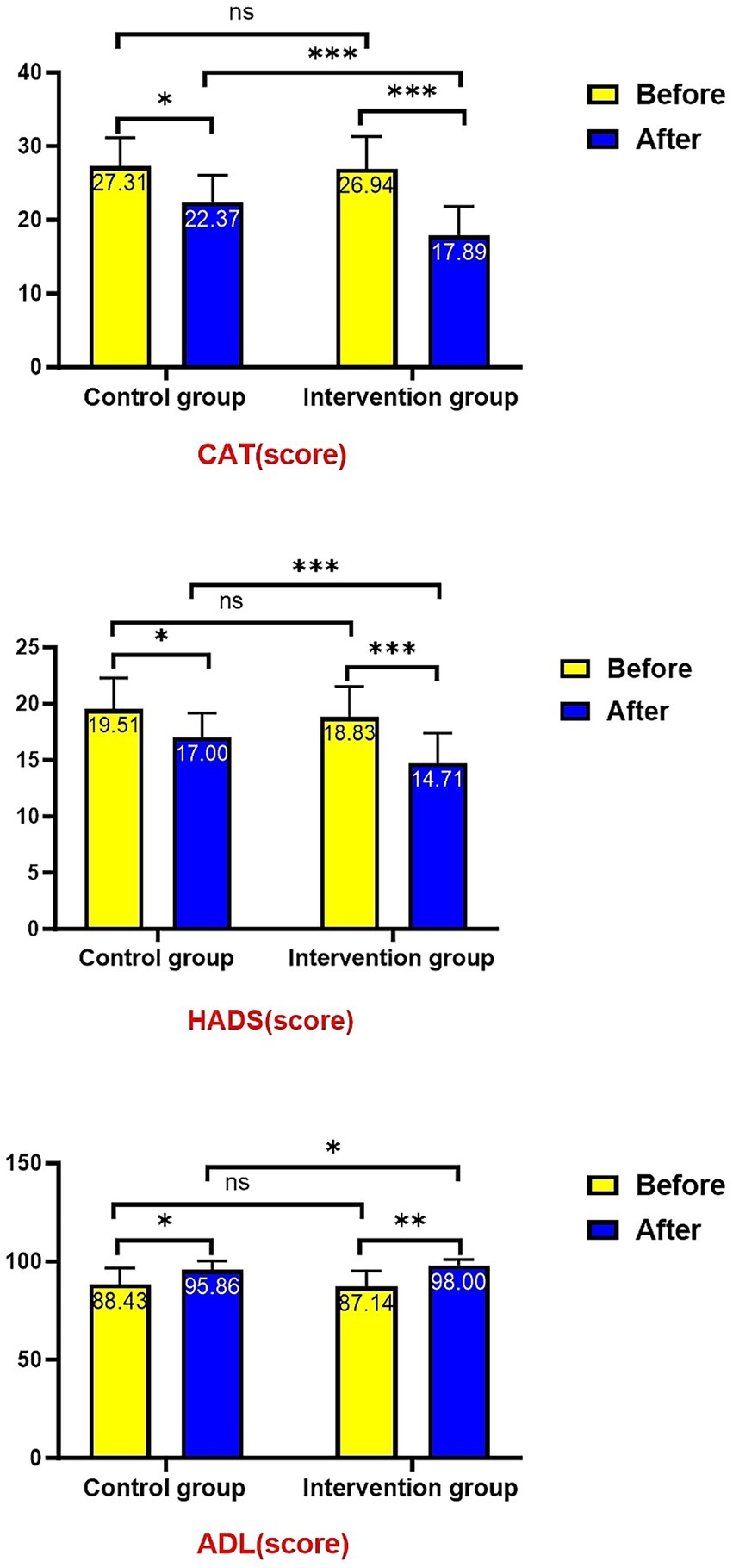
Post-treatment intergroup comparisons demonstrated significantly better outcomes in the intervention group across multiple key indicators: CAT score (17.89 ± 3.92 vs. 22.37 ± 3.68, p < 0.001), HADS score (14.71 ± 2.66 vs. 17.00 ± 2.17, p < 0.001), and ADL score (98.00 ± 3.02 vs. 95.86 ± 4.62, p = 0.025). Baseline measurements showed no significant differences between groups in CAT scores, HADS scores, or ADL scores (all p > 0.05). Following treatment, both groups exhibited significant improvements compared to baseline: CAT and HADS scores decreased significantly (both p < 0.05) while ADL scores increased significantly (both p < 0.05), with the intervention group showing more pronounced improvements (Figure 5).
The intervention group demonstrated significantly shorter durations of both non-invasive mechanical ventilation [7.75 (6.75–9.75) days vs. 9.75 (7.75–11.25) days, p = 0.034] and hospitalization [8.75 (7.50–10.00) days vs. 9.75 (8.50–11.75) days, p = 0.035] compared to the control group, with median differences of 2 days and 1 day respectively, showing statistically significant improvements (Figure 6).
The incidence of complications in the intervention group was lower than that in the control group. The incidence of gastrointestinal distension was 2.86% versus 11.43%, while the incidence of difficulty in expectoration was 2.86% versus 8.57%. The cases of exacerbated breathing difficulties in the intervention group were the same as those in the control group, both being 2.86%. It is worth noting that neither group experienced severe complications (such as aspiration, deep vein thrombosis, pneumothorax, etc.). Arrhythmias and falls were also rare, with only 1 case (2.86%) of fall in the control group. These results support the safety of early rehabilitation in this population (Figure 7).
Discussion
COPD is a highly prevalent global respiratory disorder, has emerged as one of the leading chronic conditions threatening human health. The disease not only causes progressive decline in lung function with symptoms including dyspnea, cough, and sputum production, but also severely restricts patients’ daily activities and social participation, imposing substantial economic and psychological burdens on families and society (19). During acute exacerbations (AECOPD), clinical deterioration accelerates pulmonary function impairment and may trigger life-threatening complications such as cor pulmonale and respiratory failure (20, 21). Epidemiological data indicate COPD patients experience 0.5–3.5 acute exacerbations annually, with increased frequency exacerbating healthcare burdens and significantly elevating mortality risk (22). Current pharmacological interventions demonstrate limited efficacy, while neglecting rehabilitation often leads to disease recurrence and further quality of life deterioration (23). The predominance of elderly individuals among AECOPD patients—who face compounded challenges from both physiological decline and immune dysfunction—renders their treatment and rehabilitation particularly demanding (24, 25). Our preliminary research and existing literature (13, 26) have confirmed that exercise rehabilitation significantly improves exercise tolerance, alleviates dyspnea, and enhances quality of life in AECOPD patients. Building upon this foundation, the present study specifically investigates the effects of graded exercise rehabilitation on immune function and inflammatory cytokine profiles in AECOPD patients.
The pathogenesis of AECOPD involves complex interactions, with most researchers attributing it to immune dysfunction mediated by T lymphocytes and their associated chemokine-induced inflammatory responses (27). Persistent airway inflammation in AECOPD patients is characterized by markedly elevated levels of inflammatory cytokines (IL-6, IL-8, TNF-α), which not only reflect disease severity but also perpetuate chronic inflammatory damage to airways, lung parenchyma, and vasculature through neutrophil activation (28). A prospective study of 1,755 patients demonstrated significantly higher serum levels of TNF-α, IL-6, and CRP in COPD patients compared to healthy controls, with longitudinal data revealing strong correlations between these inflammatory markers and frequency of exacerbations, degree of pulmonary function impairment, and mortality rates (29). Our results align with these established findings: both groups showed significant post-treatment reductions in serum IL-6, IL-8, TNF-α, and CRP levels compared to baseline (p < 0.05), with the intervention group demonstrating superior reductions versus controls (p < 0.05). These observations corroborate previous work by Dou Yu, Gaunaurd, and Fischer (30–32), collectively indicating that graded exercise rehabilitation effectively mitigates systemic inflammation in AECOPD patients.
Existing evidence indicates that AECOPD patients exhibit reduced cellular immunity, with T lymphocytes playing pivotal roles as both immunoregulators and effector cells (33). Among T-cell subsets, CD8+ cells recognize antigens and mediate cytotoxicity against altered host cells, while CD4+ helper T cells (B-cell inducing subset) express CD4+ antigens (34). A decreased CD4+/CD8+ ratio reflects impaired immune competence and elevated infection risk, establishing the clinical relevance of T-lymphocyte subset alterations in COPD (35, 36). Our results demonstrate that graded exercise rehabilitation significantly increased CD3+, CD4+ percentages and CD4+/CD8+ ratios while reducing CD8+ levels in both groups, with more pronounced improvements in the intervention group (p < 0.05). These findings indicate that structured exercise training effectively enhances immune function in AECOPD patients, potentially breaking the vicious cycle of inflammation-immunity imbalance.
Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) often leads to skeletal muscle dysfunction and muscle atrophy. The involvement of respiratory muscles can exacerbate the progression of the disease and increase the burden of disease symptoms, thus forming a vicious pathological cycle (37). Our study demonstrated that graded exercise rehabilitation significantly improved multiple functional parameters in both groups, including reductions in mMRC and CAT scores, increased 6-min walk distance, and enhanced ADL scores (p < 0.05 versus baseline), with superior improvements observed in the intervention group compared to controls (p < 0.05). These findings indicate that structured exercise training effectively enhances both respiratory and locomotor function in AECOPD patients. The therapeutic mechanisms likely involve professionally supervised training targeting both respiratory mechanics (improving inspiratory/expiratory muscle strength and preventing fatigue) and peripheral muscle function. Through individualized prescription of exercise frequency, intensity, and duration, early initiation of rehabilitation promotes pulmonary function recovery, increases exercise tolerance, and alleviates dyspnea severity.
However, rehabilitation treatment should attach importance to the psychological state of patients. Studies by Rahi et al. reported that the incidence of anxiety and depression in patients with COPD was 30 to 50% (38). Chen Hua-ping et al.’s investigation and research on 154 COPD patients showed that 40.3% of COPD patients had varying degrees of anxiety and depression (39). Negative emotions such as anxiety and depression not only reduce patients’ compliance with treatment and rehabilitation exercises, but also cause abnormal excitement of the sympathetic nerve, resulting in physiological and pathological changes, and affecting the quality of life and disease prognosis of patients. The results of this study showed that the anxiety and depression scores of COPD patients in both groups before treatment were higher than the normal level. After treatment, the anxiety and depression scores of the intervention group were lower than those of the control group, and the difference was statistically significant (p < 0.05), suggesting that scientific and effective rehabilitation training can significantly improve the negative emotions such as anxiety and depression of COPD patients.
The results of this study indicate that the hospitalization time, non-invasive mechanical ventilation time, and the incidence of complications in the intervention group were significantly lower than those in the control group. This suggests that implementing graded exercise rehabilitation can reduce the hospitalization time, non-invasive mechanical ventilation time, and the occurrence of complications in patients with AECOPD. The intervention group received graded exercise rehabilitation, while the control group only received conventional exercise rehabilitation. Due to the lack of personalized plans, the physical functions of the control group declined, making it difficult to effectively improve and maintain lung function. The body was more prone to being invaded by pathogens or experiencing physiological dysfunction, increasing the risk of complications. For example, long-term lack of exercise leads to slowed gastrointestinal peristalsis, which may cause gastrointestinal distension; weak respiratory muscles are unable to effectively expel phlegm, resulting in phlegm accumulation in the airways, which may lead to difficulties in expectoration and other related complications.
This study has confirmed that graded exercise rehabilitation provides an effective personalized treatment plan for patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD), significantly improving immune function, inflammatory response, respiratory capacity, exercise endurance and disease burden, while reducing the duration of mechanical ventilation and hospitalization. These findings offer novel theoretical foundations and practical guidance for AECOPD rehabilitation with substantial clinical applicability. Future investigations should elucidate the precise mechanistic pathways of graded exercise rehabilitation and evaluate its synergistic effects when combined with other therapeutic modalities to develop more comprehensive and optimized rehabilitation strategies.
Study limitations
This study has some limitations that need to be taken into account in future research: Firstly, the sample size is small and a single-center design is used, which may limit the statistical power and generalizability of the results. Moreover, due to potential selection bias in the recruitment of regional participants, the research results cannot be generalized to different medical environments. Secondly, although the two-week intervention period shows short-term therapeutic effects, it is unable to assess the long-term sustainability and prognostic impact because there is a lack of subsequent evaluation. Additionally, the study is a single-blind design (only the evaluators are blinded), which introduces potential execution bias because neither the participants nor the intervention providers are aware of the group allocation. Furthermore, potential confounding factors such as infection causes, comorbidities, and environmental factors (such as weather changes) were not adequately considered for their impact on the research results. Although efforts were made to maintain the relative balance of patients’ conditions and physical states during the study, these factors may still interfere and affect the accuracy of the conclusions. Future studies will take more rigorous measures to address this issue.
Conclusion
Grade-based exercise rehabilitation has significantly improved the inflammatory levels, immune function and exercise capacity of patients with AECOPD through personalized plans. At the same time, it has shortened the hospital stay and reduced complications. The mechanism of its effect may be related to regulating the immune-inflammation balance, enhancing respiratory muscle function and providing psychological support. In the future, it is necessary to expand the sample size and extend the follow-up time to verify the long-term efficacy and explore the synergistic effect with other treatments. This study provides evidence-based evidence for the rehabilitation treatment of AECOPD patients and supports the inclusion of grade-based exercise rehabilitation in clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the Second Affiliated Hospital of Zunyi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YC: Conceptualization, Methodology, Writing – review & editing, Project administration, Investigation, Validation, Writing – original draft, Software, Data curation. H-mR: Data curation, Project administration, Formal analysis, Investigation, Writing – review & editing, Conceptualization, Software, Writing – original draft. YW: Project administration, Validation, Visualization, Writing – review & editing, Writing – original draft, Supervision, Investigation. D-dF: Writing – original draft, Formal analysis, Data curation, Project administration, Methodology, Writing – review & editing, Supervision, Conceptualization. N-nY: Software, Writing – review & editing, Writing – original draft, Visualization, Data curation, Investigation, Project administration. C-lC: Project administration, Methodology, Writing – review & editing, Data curation, Writing – original draft, Software, Resources, Investigation. RL: Data curation, Validation, Project administration, Writing – review & editing, Methodology, Conceptualization, Writing – original draft, Investigation, Supervision. L-wL: Writing – original draft, Methodology, Data curation, Conceptualization, Project administration, Investigation, Writing – review & editing, Resources, Formal analysis. J-mL: Project administration, Validation, Resources, Data curation, Methodology, Writing – review & editing, Investigation, Writing – original draft, Conceptualization. L-nM: Software, Writing – original draft, Investigation, Visualization, Methodology, Writing – review & editing, Data curation, Project administration. HZ: Resources, Funding acquisition, Supervision, Writing – original draft, Project administration, Formal analysis, Writing – review & editing, Conceptualization, Visualization, Validation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Zunyi City-Hospital Joint Project of Guizhou Province, China (Grant No. Zunshi Kehe HZ Character (2025) 123), the Science and Technology Department of Guizhou Province, China (Grant No. Qian Ke He Cheng Guo - LC [2024] 035), the Science and Technology Department of Guizhou Province, China (Grant No. Qian Ke He Ji Chu - ZK [2022] General 645), the Science and Technology Fund Project of Guizhou Provincial Health Commission, China (Grant No. gzwkj2025-579), and the Guizhou Province Science and Technology Innovation Talent Team Construction Project for Smart Geriatric Care (Grant No. Qian Ke He Ping Tai Ren - CXTD[2023] 028; 202411). The funding agencies played no role in the design of the study, data collection, analysis, interpretation of data, or writing of the manuscript.
Acknowledgments
We would like to express our sincere gratitude to all the participants who have taken part in this randomized controlled trial.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yang, H, Huang, D, Luo, J, Liang, Z, and Li, J. The use of high-flow nasal cannula in patients with chronic obstructive pulmonary disease under exacerbation and stable phases: a systematic review and meta-analysis. Heart Lung. (2023) 60:116–26. doi: 10.1016/j.hrtlng.2023.02.016
2. Singh, D, Agusti, A, Anzueto, A, Barnes, PJ, Bourbeau, J, Celli, BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. (2019) 53:1900164. doi: 10.1183/13993003.00164-2019
3. Agustí, A, Celli, BR, Criner, GJ, Halpin, D, Anzueto, A, Barnes, P, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med. (2023) 207:819–37. doi: 10.1164/rccm.202301-0106PP
4. Hao, G, Qiu, Q, Hou, L, and Gu, F. The effect of symptom clusters and sleep disorder on quality of life among patients with chronic obstructive pulmonary disease. J Healthc Eng. (2021) 2021:1–8. doi: 10.1155/2021/1692480
5. Kim, SJ, Kwak, N, Choi, SM, Lee, J, Park, YS, Lee, CH, et al. Sleep duration and its associations with mortality and quality of life in chronic obstructive pulmonary disease: results from the 2007-2015 KNAHNES. Respiration. (2021) 100:1043–9. doi: 10.1159/000516381
6. Jurado Gámez, B, Feu Collado, N, Jurado García, JC, García Gíl, F, Muñoz Gomariz, E, Jiménez Murillo, L, et al. Home intervention and predictor variables for rehospitalization in chronic obstructive pulmonary disease exacerbations. Arch Bronconeumol. (2013) 49:10–4. doi: 10.1016/j.arbres.2012.08.003
7. Zhao, Y, and Wu, Z. TROP2 promotes PINK1-mediated mitophagy and apoptosis to accelerate the progression of senile chronic obstructive pulmonary disease by up-regulating DRP1 expression. Exp Gerontol. (2024) 191:112441. doi: 10.1016/j.exger.2024.112441
8. Xu, Y, Yang, D, Lu, B, Zhang, Y, Ren, L, and Shen, H. Efficacy of aerobic training and resistance training combined with external diaphragm pacing in patients with chronic obstructive pulmonary disease: a randomized controlled study. Clin Rehabil. (2023) 37:1479–91. doi: 10.1177/02692155231172005
9. Bowen, TS, Aakerøy, L, Eisenkolb, S, Kunth, P, Bakkerud, F, Wohlwend, M, et al. Exercise training reverses extrapulmonary impairments in smoke-exposed mice. Med Sci Sports Exerc. (2017) 49:879–87. doi: 10.1249/MSS.0000000000001195
10. Valenzuela, PL, Saco-Ledo, G, Rivas-Baeza, B, Martínez-Velilla, N, Izquierdo, M, and Lucia, A. Safety of in-hospital early rehabilitation in chronic obstructive pulmonary disease exacerbations: a systematic review and meta-analysis. Ann Phys Rehabil Med. (2022) 65:101528. doi: 10.1016/j.rehab.2021.101528
11. Ryrsø, CK, Godtfredsen, NS, Kofod, LM, Lavesen, M, Mogensen, L, Tobberup, R, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD-exacerbations: a systematic review and meta-analysis. BMC Pulm Med. (2018) 18:154. doi: 10.1186/s12890-018-0718-1
12. Machado, A, Matos Silva, P, Afreixo, V, Caneiras, C, Burtin, C, and Marques, A. Design of pulmonary rehabilitation programmes during acute exacerbations of COPD: a systematic review and network meta-analysis. Eur Respir Rev. (2020) 29:200039. doi: 10.1183/16000617.0039-2020
13. Yang, N, Zeng, H, Fu, D, Wang, Y, Cheng, CL, Liu, R, et al. Construction and application of a graded exercise rehabilitation program for patients with acute exacerbation of chronic obstructive pulmonary disease. Chin J Nurs. (2024) 59:773–81. doi: 10.3761/j.issn.0254-1769.2024.07.001
14. Deng, H, Zhu, S, Yu, F, Song, X, Jin, X, and Ding, X. Analysis of predictive value of cellular inflammatory factors and T cell subsets for disease recurrence and prognosis in patients with acute exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. (2024) 19:2361–9. doi: 10.2147/COPD.S490152
15. Sunjaya, A, Poulos, L, Reddel, H, and Jenkins, C. Qualitative validation of the modified Medical Research Council (mMRC) dyspnoea scale as a patient-reported measure of breathlessness severity. Respir Med. (2022) 203:106984. doi: 10.1016/j.rmed.2022.106984
16. Gil, HI, Zo, S, Jones, PW, Kim, BG, Kang, N, Choi, Y, et al. Clinical characteristics of COPD patients according to COPD assessment test (CAT) score level: cross-sectional study. Int J Chron Obstruct Pulmon Dis. (2021) 16:1509–17. doi: 10.2147/COPD.S297089
17. Qiu, YR, Wang, JW, Wu, HW, and Chen, GH. Practice and effect evaluation of constructing a graded service standard for nursing assistants using the activities of daily living scale. In: ZXDHLZ Zhi editor. (2020) 26:2858–62. doi: 10.3760/cma.j.cn115682-20190813-02899
18. Fomenko, A, Dümmler, D, Aktürk, Z, Eck, S, Teusen, C, Karapetyan, Y, et al. Hospital Anxiety and Depression Scale Anxiety subscale (HADS-A) for detecting anxiety disorders in adults. Cochrane Database Syst Rev. (2025) 7:CD015456. doi: 10.1002/14651858.CD015456
19. Vieira, CLZ, Koutrakis, P, Huang, S, Grady, S, Hart, JE, Coull, BA, et al. Short-term effects of particle gamma radiation activities on pulmonary function in COPD patients. Environ Res. (2019) 175:221–7. doi: 10.1016/j.envres.2019.05.032
20. Pei, Z, Sun, Y, Wang, S, Chen, Y, Yang, T, Huang, K, et al. Estimating mortality among inpatients with acute exacerbation of chronic obstructive pulmonary disease using registry data. NPJ Prim Care Respir Med. (2020) 30:28. doi: 10.1038/s41533-020-0186-y
21. Ruan, H, Zhang, H, Wang, J, Zhao, H, Han, W, and Li, J. Readmission rate for acute exacerbation of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Med. (2023) 206:107090. doi: 10.1016/j.rmed.2022.107090
22. Chronic Obstructive Pulmonary Disease Acute Exacerbation Diagnosis and Treatment Expert Group. Chinese expert consensus on the diagnosis and treatment of acute exacerbation of chronic obstructive pulmonary disease (AECOPD) (2017 updated version). Int J Respir Dis. (2017) 37:1041–57. doi: 10.3760/cma.j.cn131368-20171123-01066
23. Tan, D, Wang, B, Cao, P, Wang, Y, Sun, J, Geng, P, et al. High flow nasal cannula oxygen therapy versus non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease with acute-moderate hypercapnic respiratory failure: a randomized controlled non-inferiority trial. Crit Care. (2024) 28:250. doi: 10.1186/s13054-024-05040-9
24. Richardson, CR, Franklin, B, Moy, ML, and Jackson, EA. Advances in rehabilitation for chronic diseases: improving health outcomes and function. BMJ. (2019) 365:12191. doi: 10.1136/bmj.l2191
25. Nitta, Y, Ueda, Y, Ohira, S, Isono, M, Hirose, A, Inui, S, et al. Feasibility of a portable respiratory training system with a gyroscope sensor. Br J Radiol. (2024) 97:1162–8. doi: 10.1093/bjr/tqae085
26. Wouters, EF, Posthuma, R, Koopman, M, Liu, WY, Sillen, MJ, Hajian, B, et al. An update on pulmonary rehabilitation techniques for patients with chronic obstructive pulmonary disease. Expert Rev Respir Med. (2020) 14:149–61. doi: 10.1080/17476348.2020.1700796
27. Qi, Y, Yan, Y, Tang, D, Han, J, Zhu, X, Cui, M, et al. Inflammatory and immune mechanisms in COPD: current status and therapeutic prospects. J Inflamm Res. (2024) 17:6603–18. doi: 10.2147/JIR.S478568
28. Sahin, F, Kosar, AF, Aslan, AF, Yiğitbaş, B, and Uslu, B. Serum biomarkers in patients with stable and acute exacerbation of chronic obstructive pulmonary disease: a comparative study. J Med Biochem. (2019) 38:503–11. doi: 10.2478/jomb-2018-0050
29. Shao, S, Zhang, Z, Feng, L, Liang, L, and Tong, Z. Association of blood inflammatory biomarkers with clinical outcomes in patients with AECOPD: an 8-year retrospective study in Beijing. Int J Chron Obstruct Pulmon Dis. (2023) 18:1783–802. doi: 10.2147/COPD.S416869
30. Dou, Y, Zhang, CH, and Liu, XM. Effect of tiotropium bromide inhalation combined with pulmonary rehabilitation training in patients with chronic obstructive pulmonary disease. In: ZWYXY Jiu editor. (2023) 21:46–50. doi: 10.14033/j.cnki.cfmr.2023.05.01
31. Gaunaurd, IA, Gómez-Marín, OW, Ramos, CF, Sol, CM, Cohen, MI, Cahalin, LP, et al. Physical activity and quality of life improvements of patients with idiopathic pulmonary fibrosis completing a pulmonary rehabilitation program. Respir Care. (2014) 59:1872–9. doi: 10.4187/respcare.03180
32. Fischer, CP, Plomgaard, P, Hansen, AK, Pilegaard, H, Saltin, B, and Pedersen, BK. Endurance training reduces the contraction-induced interleukin-6 mRNA expression in human skeletal muscle. Am J Physiol Endocrinol Metab. (2004) 287:E1189–94. doi: 10.1152/ajpendo.00206.2004
33. Guo, F, Guo, Y, Feng, Q, Li, FS, Dong, B, Li, BP, et al. Clinical study of Qingfei Huatan Decoction in treating acute exacerbation of chronic obstructive pulmonary disease with phlegm-heat obstructing lung syndrome. Beijing J Tradit Chin Med. (2019) 42:430–5. doi: 10.3969/j.issn.1006-2157.2019.05.012
34. Zhang, Z, Jin, H, and Yu, X. Expression and significance of PD-1/PD-L1 in peripheral blood T cells of patients with acute exacerbation of chronic obstructive pulmonary disease. Chin J Gen Pract. (2020) 18:419–422+426. doi: 10.16766/j.cnki.issn.1674-4152.001262
35. Chatzileontiadou, DSM, Sloane, H, Nguyen, AT, Gras, S, and Grant, EJ. The many faces of CD4(+) T cells: immunological and structural characteristics. Int J Mol Sci. (2020) 22:73. doi: 10.3390/ijms22010073
36. Ma, Y, Chen, Y, Zhang, N, Xu, G, Wang, Y, Sun, Y, et al. Efficacy and safety of pulmonary rehabilitation training on lung function, quality of life, and T cell immune function in patients with stable chronic obstructive pulmonary disease: a randomized controlled trial. Ann Palliat Med. (2022) 11:1774–85. doi: 10.21037/apm-22-451
37. Cheng, YY, Lin, SY, Hsu, CY, and Fu, PK. Respiratory muscle training can improve cognition, lung function, and diaphragmatic thickness fraction in male and non-obese patients with chronic obstructive pulmonary disease: a prospective study. J Pers Med. (2022) 12:475. doi: 10.3390/jpm12030475
38. Rahi, MS, Thilagar, B, Balaji, S, Prabhakaran, SY, Mudgal, M, Rajoo, S, et al. The impact of anxiety and depression in chronic obstructive pulmonary disease. Adv Respir Med. (2023) 91:123–34. doi: 10.3390/arm91020011
Keywords: graded exercise rehabilitation, COPD exacerbation, immune function, inflammatory markers, T lymphocyte subsets
Citation: Chen Y, Ran H-M, Wang Y, Fu D-d, Yang N-n, Cheng C-l, Liu R, Luo L-w, Luo J-m, Ma L-n and Zeng H (2025) Effects of graded exercise rehabilitation on inflammatory factors and T-lymphocyte subsets in patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled trial. Front. Med. 12:1620577. doi: 10.3389/fmed.2025.1620577
Edited by:
Tzong-Shyuan Lee, National Taiwan University, TaiwanReviewed by:
Yi-Han Hsiao, Taipei Veterans General Hospital, TaiwanPhilippe Gosset, Institut National de la Santé et de la Recherche Médicale (INSERM), France
Copyright © 2025 Chen, Ran, Wang, Fu, Yang, Cheng, Liu, Luo, Luo, Ma and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Zeng, emVuZ2h1aS4xMjIxQDE2My5jb20=
†These authors have contributed equally to this work
 Yue Chen
Yue Chen Hong-Min Ran2†
Hong-Min Ran2†