- 1Division of Obstetrics & Gynecology, KK Women's and Children's Hospital, Singapore, Singapore
- 2Duke-National University of Singapore Graduate Medical School, Singapore, Singapore
- 3Department of Maternal Fetal Medicine, KK Women's and Children's Hospital, Singapore, Singapore
- 4Department of Psychological Medicine, KK Women's and Children's Hospital, Singapore, Singapore
Introduction: There is limited data on perinatal depression and anxiety rates, as well as on knowledge, attitudes, and practices related to perinatal mental health (PMH), particularly in an urban Southeast Asian population.
Methods: From September to December 2022, 446 antenatal and 150 postnatal participants completed a 38-item survey assessing depressive and anxiety symptoms, along with knowledge, attitudes, and practices regarding PMH. Probable depression was defined as an Edinburgh Postnatal Depression Scale (EPDS) score of ≥15 during pregnancy or ≥13 postnatal. Probable anxiety was defined using the EPDS anxiety subscale (EPDS-3A), which comprises items 3, 4, and 5, with a score of ≥5 indicating probable anxiety.
Results: The rates of probable depression were 11.9% antenatally and 23.7% postnatally, while anxiety rates were 48.4% and 56.7%, respectively. Only 63.8% of participants could identify symptoms of mental health disorders, and just 24.1% had received assessment or education from healthcare professionals. Although most women (57.0%) would seek support from their spouse or partner, only 15.5% indicated willingness to consult healthcare professionals. Most participants supported the need for mental health education (89.5%), screening (87.4%), and tailored guidelines (94.5%) for perinatal women.
Conclusion: High rates of probable depression and anxiety, coupled with low mental health literacy, highlight the urgent need for comprehensive PMH education and guidelines in Singapore.
Highlights
• Routine mental health screening: Integrate antenatal and postnatal mental health screening to detect and address the high rates of depression and anxiety early.
• Enhance mental health literacy: Implement targeted education programs to improve symptom recognition and encourage professional help-seeking.
• Engage partners in care: Involve spouses or partners in mental health support to strengthen family-centered care during the perinatal period.
Introduction
Perinatal mental health (PMH) is increasingly recognized as a significant global public health concern. The perinatal period—defined by the World Health Organization (WHO) as encompassing pregnancy and the first year after childbirth (1)—is a particularly vulnerable time for women. A 2018 systematic review estimated that ~10%−20% of women experience mental health disorders during this period (2). These disorders are concerning, not only because of their potential to affect the mother's long-term physical and mental wellbeing, but also due to their broader implications for the child, family, and society (3, 4). The impact of maternal depression and anxiety on fetal neurodevelopment (5–7), and their adverse consequences in the postnatal period (8–10) have been well documented.
A meta-analysis from high-income countries reported prevalence rates of 11% for antenatal depression, and 13% for postnatal depression (11). Another meta-analysis showed that the prevalence of maternal anxiety during pregnancy varies depending on the specific type of anxiety disorder studied, with estimates reaching up to 13% (12). The COVID-19 pandemic further intensified stressors affecting perinatal mental health. A systematic review and meta-analysis found that lockdown measures significantly increased mental health risks for pregnant and postnatal women (13), while comparative studies reported higher rates of perinatal depression during the pandemic compared to pre-pandemic periods (14–16). In Singapore, local data from the Postnatal Depression Intervention Programme similarly showed a statistically significant rise in screen-positive postnatal depression cases in 2021 (17). However, much of the existing evidence remains rooted in Western populations, with limited representation of Asian cohorts (11–13), underscoring the need for more context-specific data from diverse cultural settings.
Singapore is a multi-ethnic island city-state in Southeast Asia. As a highly developed and urbanized nation, it differs from many other Asian settings in terms of cultural practices, healthcare access, and societal norms (18). Culture plays a central role in shaping women's experiences during pregnancy and the postnatal period, influencing how emotional distress is perceived, expressed, and managed. Cultural beliefs and norms, particularly in Asian societies, can significantly affect attitudes toward mental health and influence help-seeking behaviors during this critical time. Compared to Western contexts, Asian perspectives on PMH often reflect lower awareness of the potential adverse effects of PMH conditions on both mother and child, as well as greater reluctance to seek mental health support (19, 20). Limited mental health literacy further compounds this issue and remains a key barrier to early screening and intervention (21). Despite the importance of addressing these challenges, there is a notable lack of evidence on maternal knowledge, attitudes, and help-seeking practices during the perinatal period in Asian populations.
This study aims to describe the prevalence of maternal depression and anxiety during pregnancy and the postnatal period, and to explore knowledge, attitudes, and practices related to PMH among a multicultural population of women in Singapore.
Methods
Study sample
Caregivers participating in this study were enlisted as part of the IPRAMHO survey on Integrated Maternal Perinatal Mental Health Care (IMUM). Survey data were collected using a convenience sampling method from eligible participants attending the outpatient Obstetrics & Gynecology Clinic at KK Women's and Children's Hospital (KKH) in Singapore. Eligible participants were Singaporean or permanent residents who were pregnant, and women up to 12 weeks' postnatal and possessed the ability to comprehend English. Before taking part, participants needed to provide witnessed verbal consent to the research team. Subsequently, they were given an electronic version of the survey through FormSG (https://form.gov.sg/) for completion. The research procedures for this study received formal approval for an exempt review from the SingHealth Centralized Institutional Review Board (CIRB Ref No.: 2022/2454). Clinical trial number: not applicable. All the authors and participants surveyed have provided consent for the publication of this manuscript.
Data collection
The survey of this study was administered between September 2022 and December 2022 when Singapore was still in the Disease Outbreak Response System Condition (DORSCON) framework level Yellow due to the COVID-19 outbreak (22), and a total of n = 602 survey responses were collected. The survey comprised 38 items that included data collected on participants' demographics, 10 items from the Edinburgh Postnatal Depression Scale (EPDS) (23), and nine items regarding the knowledge, attitudes, and practices of mental health during pregnancy and the postnatal period. The survey questionnaire was developed and reviewed by members of the Perinatal Mental Health Guidelines on Depression and Anxiety Committee, who were responsible for the development of the Singapore Perinatal Mental Health Guidelines on Depression and Anxiety (17). The development of the survey questionnaire went through an expert review and thorough literature review which establishes content validity (see Supplementary Data File 1). The survey took 10–15 min in total duration.
Assessment of probable depressive and anxiety during pregnancy and postnatal
Self-reported depressive and anxiety symptoms were assessed during pregnancy and up to 12 weeks postnatal using the Edinburgh Postnatal Depression Scale (EPDS), a widely validated 10-item screening tool for perinatal populations. A local Singapore cohort study has demonstrated good reliability of the EPDS, with a Cronbach's alpha of 0.82 (5). Participants with EPDS scores ≥15 during pregnancy or ≥13 postnatal, based on established normative values (24), were considered at high risk for probable depression.
Anxiety symptoms were assessed using the EPDS-3A, which comprises items 3, 4, and 5 of the EPDS. While two local unpublished studies found limited screening accuracy for perinatal anxiety, we conducted a preliminary analysis using the cut-off established by Smith-Nielsen et al., where a score of ≥5 demonstrated optimal sensitivity (70.9%), specificity (92.2%), and an AUC of 0.926—suggesting potential utility as a time-efficient screening tool for probable anxiety in both pregnant and postnatal women (25).
Prevalence rates of probable depressive and anxiety symptoms were calculated separately for antenatal and postnatal participants. Additionally, prevalence was examined by trimester (first: 0–12 weeks, second: 13–27 weeks, third: 28–40 weeks) and presented as Supplementary Data File 1.
Maternal knowledge, attitudes, and practices of PMH and guideline recommendations
To gauge participants' understanding of PMH, the survey included five key questions: (1) “Are you aware that mental health disorders, such as anxiety and depression, can occur during pregnancy or postnatal?” (2) “Do you know the symptoms or signs of mental health disorders (anxiety or depression) to watch for during pregnancy or postnatal?” (3) “Do you believe that mental health disorders (anxiety and depression) can have adverse consequences on your pregnancy outcomes and your child's health outcomes after birth?” (4) “Do you consider lifestyle habits (diet, exercise, and sleep) important for mental health before, during pregnancy, or postnatal?” (5) “During your pregnancy and postnatal, were you assessed or educated about mental health disorders (anxiety and depression) by your primary obstetrician or other healthcare professionals?” Additionally, one question focused on participants' attitudes toward seeking help for PMH symptoms: “If you were experiencing symptoms of anxiety or depression during your pregnancy or postnatal, who would you seek help from?” The final three questions aimed to understand participants' perceptions of PMH: (1) “Do you believe there are positive benefits to providing mental health education for pregnant mothers and mothers postnatal?” (2) “Do you think there are positive benefits to implementing mental health screening for pregnant mothers and mothers' postnatal?” (3) “Do you believe that mental health guidelines for pregnant mothers and mothers postnatal would be useful?”
Statistical analyses
In total, 602 women were recruited, of whom those with missing values for the gestational age during pregnancy or number of postnatal weeks (n = 6) were excluded, resulting in an analytical antenatal sample of 446 participants and postnatal sample of 150 participants for the calculation of prevalence rates.
Characteristics of all the 602 participants were presented with continuous datasets that were normally distributed are presented as the mean and standard deviation (SD), while frequencies and percentages were used to describe categorical variables between the antenatal and postnatal participants. In a supplementary analysis examining the comparison of categorical variables between probable depression and anxiety across trimesters in pregnancy, a chi-squared test was utilized. Statistically significant results were determined at 2-sided p < 0.05. All analyses were performed using STATA software version 18.0 (StataCorp, College Station, US).
Results
Caregiver characteristics
A total of 602 women participated in the IMUM study, and their characteristics were presented in Table 1. In summary, a majority of the women were of Chinese ethnicity (71.3%), employed (83.6%), with university-level education (69.9%), and approximately half were nulliparous (53.5%). On average the women were 32.0 (SD: 4.3) years old, with a pre-pregnancy BMI of 22.8 (SD: 4.8) kg/m2 (Table 2). Only 8.5% of the women had newborns with medical issues in their latest pregnancy, with 22.4% of them having previous pregnancies that ended in miscarriages, stillbirths, or early infant deaths. Among the majority of these women (72.8%), the most recent pregnancy was planned (Table 1). The average depression screening scores were 9.0 (SD: 4.8) and 9.5 (SD: 4.7) for antenatal and postnatal women, respectively. The average anxiety screening scores were 4.2 (SD: 2.1) and 4.5 (SD: 2.0) for antenatal and postnatal women, respectively.
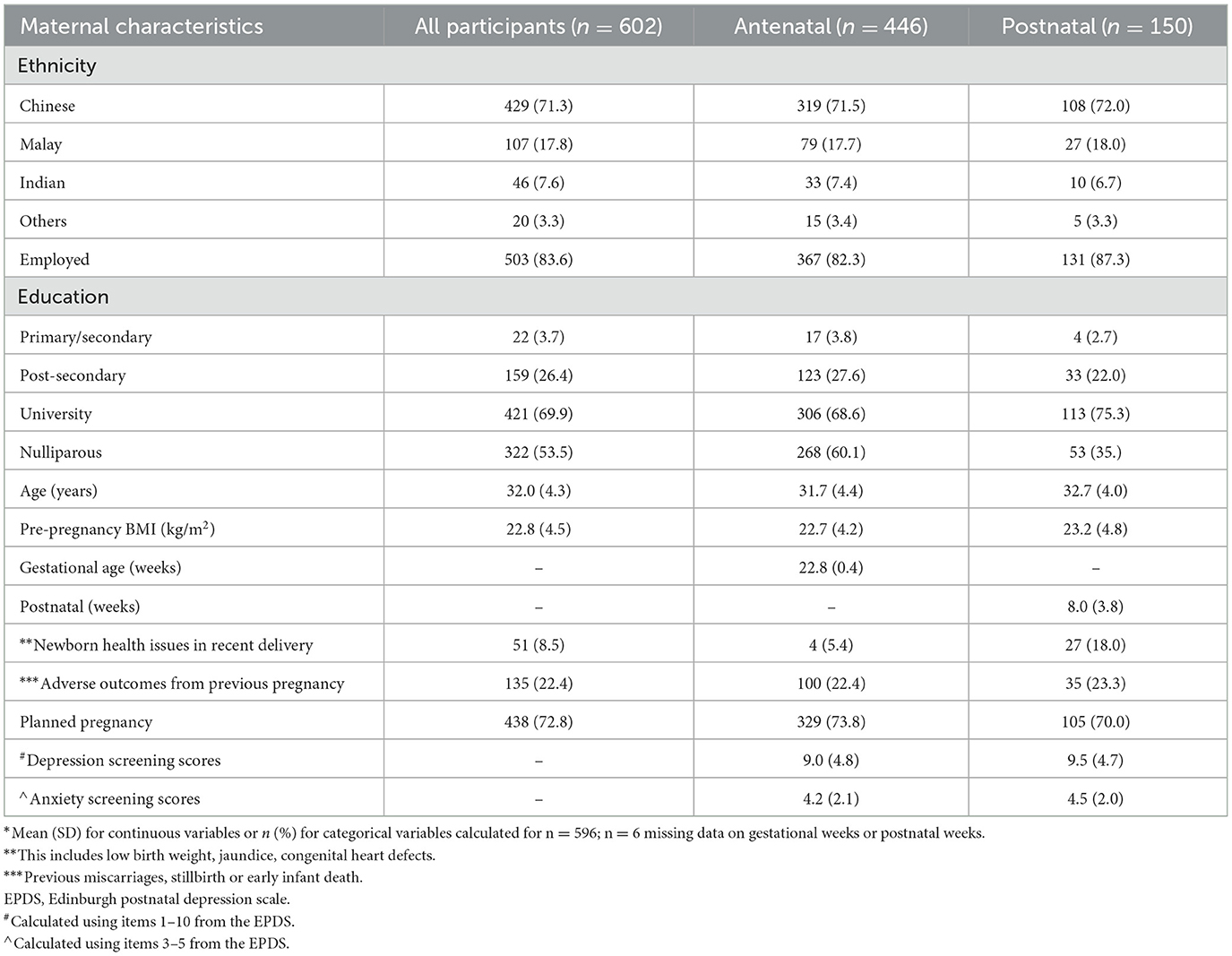
Table 1. *Baseline characteristics of the n = 446 antenatal and n = 150 postnatal study participants.
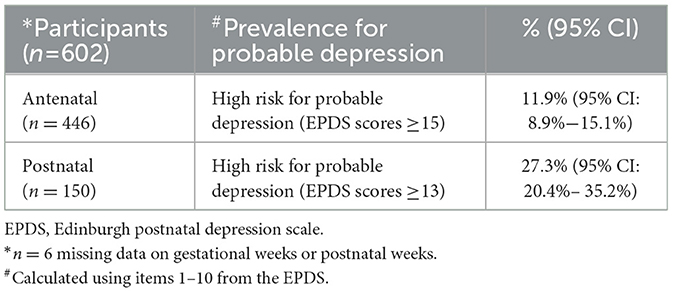
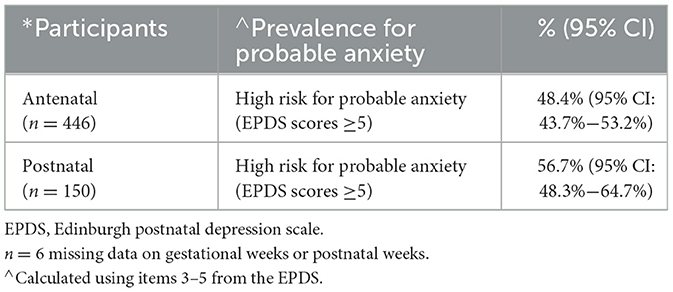
Prevalence of probable depression and anxiety
The proportions of probable antenatal and postnatal depression were 11.9% (95% CI: 8.9%−15.1%) and 23.7% (95% CI: 20.4%−35.2%), respectively (Table 2). For anxiety, the reported proportions were 48.4% (95% CI: 43.7%−53.2%) during the antenatal period, and 56.7% (95% CI: 48.3%−64.7%) during the postnatal period (Table 3). During pregnancy, the proportion of depression cases was 6.1% (95% CI: 1.4%−12.3%) in the first trimester, 12.6% (95% CI: 8.2%−18.7%) in the second trimester, and 13.8% (95% CI: 9.0%−19.2%) in the third trimester. Anxiety proportions were 46.3% (95% CI: 35.0%−57.8%) in the first trimester, 44.3% (95% CI: 37.2%−52.5%) in the second trimester, and 53.6% (95% CI: 45.2%−59.8%) in the third trimester. Statistical analysis showed no significant differences between trimesters (p > 0.05) (Supplementary Table 1).
Knowledge, attitudes, and practices of perinatal mental health
Table 4 presents data on women's knowledge, attitudes, and practices regarding perinatal mental health. A significant majority (96.8%) recognized that mental health disorders can occur during pregnancy or after childbirth, with 94.2% acknowledging the influence of lifestyle habits on mental health. While 77.4% were aware of potential adverse effects on pregnancy and child health, only 63.8% identified the signs and symptoms to watch for. Notably, 24.1% reported having received assessment or education about mental health disorders from their primary obstetrician or other healthcare professionals. Regarding help-seeking behavior for anxiety or depression symptoms during or after pregnancy, ~57.0% indicated they would turn to their spouse or partner, whereas only 15.5% were willing to seek help from healthcare professionals. Participants overwhelmingly recognized the value of mental health education (89.5%) and screening (87.4%), with 94.5% emphasizing the importance of mental health guidelines tailored for pregnant and postnatal women.
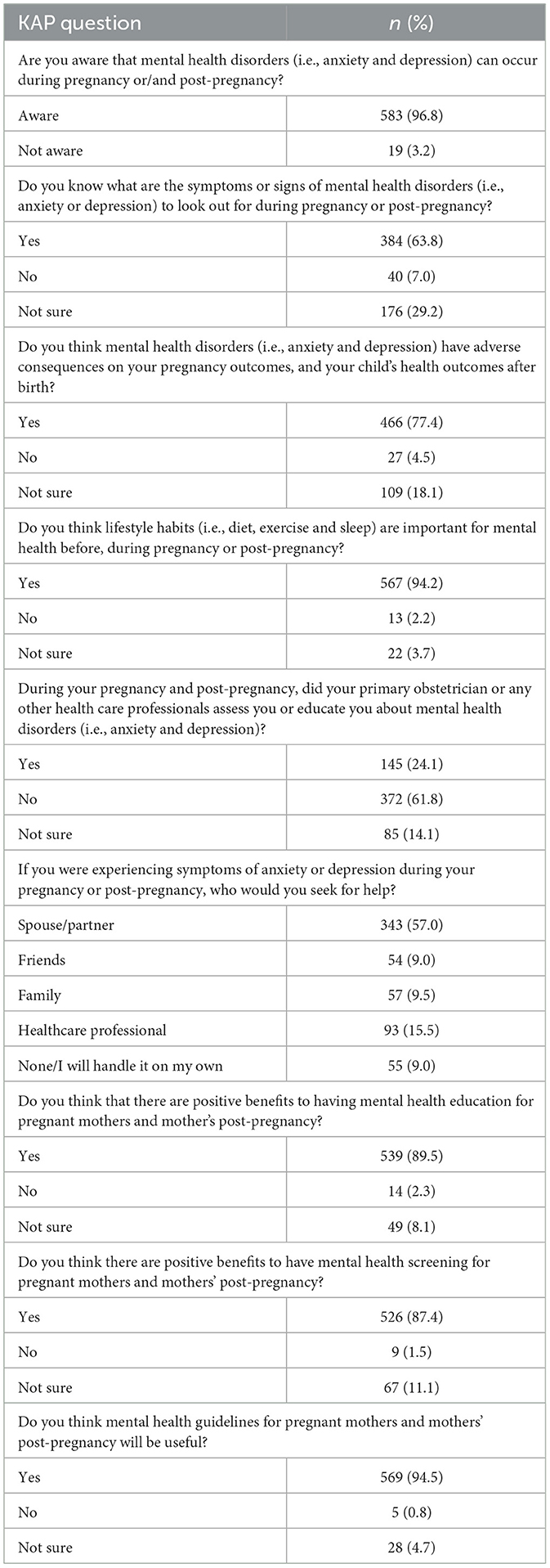
Table 4. Knowledge, attitudes, and practices of n = 602 study participants on perinatal mental health.
Discussion
Our study found that approximately one in 10 pregnant women and one in four women within 12 weeks postnatal reported symptoms indicative of probable depression. Notably, an even greater proportion of women were identified as experiencing probable anxiety, both during pregnancy (48.4%) and in the postnatal period (56.7%).
We observed a postnatal depression prevalence of 27.3%, as screened using the EPDS (cut-off ≥13), based on data collected in 2022. This rate is significantly higher than those reported in earlier years—4.9% in 2019 and 6.5% in 2021 (16)—based on data from outpatient clinic screening programs. As expected, cohort studies tend to report higher prevalence rates, likely due to self-selection bias and increased psychological awareness among participants. For example, postnatal depression rates in local cohort studies were 10.4% in 2014 (26), 17.0% in 2018 (27), and 9.8% (28), all using the same EPDS cut-off of ≥13.
Similarly, the prevalence of antenatal depression (EPDS >15) in our study (11.9%) exceeded earlier reports—7.3% in 2016 (29) and 9.0% in 2019 (30). While prevalence estimates for perinatal depression vary widely across studies due to methodological differences, our findings appear consistent with global trends showing an increase in postnatal depression. For instance, prevalence in the US rose from 16.9% in 2019 to 18.1% in 2020 (15), while in the UK it increased from 10.3% in 2014 to 23.9% in 2020 (31). Both studies attributed this rise, at least in part, to the impact of the COVID-19 pandemic on maternal mental health. Furthermore, the overall higher prevalence of probable perinatal depression observed in this cohort compared to previous local estimates may reflect both sample characteristics and methodological factors. A relatively high proportion of participants reported adverse pregnancy outcomes, which is associated with increased psychological vulnerability during the perinatal period. Methodological differences may also have contributed. While many previous local studies administered depression screening only once, often in mid-pregnancy and at month-3 postpartum (10, 26, 28, 29), our study assessed participants at multiple time points throughout pregnancy and up to 12 weeks postpartum. This extended follow-up period may have captured late-onset antenatal symptoms and postpartum onset, resulting in a higher overall prevalence.
We also found higher rates of probable perinatal anxiety (antenatal: 48.4%; postnatal: 56.7%), as assessed using the EPDS-3A (25), compared to a 2018 meta-analysis that reported pooled rates of 15.2% during pregnancy and 15.0% postnatal (32). In Singapore, earlier studies using the State-Trait Anxiety Inventory (STAI) reported lower antenatal anxiety rates of 17–19% in 2016 (8) and 29.5% in 2018 (33). A meta-analysis conducted during the COVID-19 pandemic found that anxiety symptoms in pregnant women exceeded rates of depression, with a pooled antenatal anxiety prevalence of 40% across 26 studies, primarily from Asia (34). Our findings of 48.4% are consistent with this upward trend and further supported by other studies linking heightened anxiety to the pandemic context (34–36).
An increase in antenatal depression from the first to the third trimester was also observed, with both depression and anxiety peaking in the third trimester. This aligns with prior systematic reviews and meta-analyses suggesting higher rates in the second and third trimesters (37, 38). However, not all studies observed similar trends. In Kenya (39), the highest depression prevalence occurred during the early second trimester, while in Bangladesh (40), depressive symptoms declined as pregnancy progressed. These differences may stem from variations in EPDS cut-offs > 12 in Kenya and > 10 in Bangladesh—vs. > 15 in our study. Unlike depression, trends in antenatal anxiety were less consistent across trimesters, possibly due to the lack of standardized diagnostic criteria. A review found pooled anxiety rates of 18.2% (first trimester), 19.1% (second), and 24.6% (third) (32), with other studies showing mixed trimester trends (39, 41).
Despite high overall awareness of perinatal mental health (PMH) disorders (96.8%), fewer women were aware of the adverse effects on pregnancy outcomes and child development (77.4%). Additionally, only 63.8% could recognize symptoms of PMH disorders—comparable to the 68.2% found in a Chinese study on postnatal literacy (42). A systematic review of studies in Western countries similarly highlighted poor symptom recognition among postnatal women (19). Since awareness and recognition are critical for timely help-seeking (43), the discrepancy is noteworthy.
Our findings show that women were more likely to seek support from their spouse (57%) than from healthcare professionals (15.5%). This pattern is consistent with both Western (21) and Chinese studies (42), which found a general preference for informal sources of help. For example, Gong et al. reported only 9.3% of women preferred seeking help from professionals (44), while Huang et al. noted that “knowledge and beliefs about professional help” scored lowest among literacy items (42). Cultural beliefs play a significant role in shaping attitudes toward mental health and help-seeking behaviors in Singapore (45). Among Chinese individuals, the concept of “face” and the perception of mental health struggles as a moral failing may contribute to stronger stigma and less social tolerance (46, 47). In contrast, while some Malay Muslim participants attributed mental health issues to spiritual possession—potentially delaying access to appropriate care—they also demonstrated greater acceptance of persons with mental health issues, possibly due to Islamic teachings that emphasize compassion, acceptance, and the divine purpose behind human suffering (48). Thus, our findings of low help-seeking from healthcare professionals align with existing evidence that stigma—rooted in conservative values, shame, loss of “face,” and cultural reluctance to discuss psychological distress—remains a major barrier to mental health care in Asian societies compared to Western populations (49).
Healthcare provider support for PMH also appears suboptimal. A recent local survey of 55 doctors found that 83.7% lacked confidence in managing PMH concerns, and 65.5% did not routinely screen for them (50). Similar patterns were reported in India, where 89% of providers did not screen for perinatal depression and less than half were familiar with the appropriate tools (51). A systematic review across 43 studies in Western countries also revealed only moderate PMH literacy among healthcare providers, with limited knowledge of symptoms and screening tools (52). This deficiency, observed among both women and providers (50, 52), poses a major barrier to delivering adequate PMH care. Encouragingly, 85% of women in our study endorsed the benefits of education and screening, and 94.5% agreed that PMH guidelines would be helpful.
Strengths and limitations
The study's strengths include a robust sample size (n = 602), which is comparable to previous local studies (10, 26, 29, 30). We also captured self-reported symptoms of both depression and anxiety during pregnancy and postnatal. Notably, this is the first study in Singapore to assess PMH literacy—including knowledge, attitudes, and help-seeking behaviors—among perinatal women.
However, several limitations must be acknowledged. First, we used the EPDS to screen for both depression and anxiety, which may limit comparability with studies using alternative tools such as the STAI (10, 26, 29). Second, the psychometric properties of the EPDS-3A for anxiety screening have not yet been validated in our local population. Therefore, the high prevalence of anxiety reported here warrants further investigation. Furthermore, there is low internal consistency (Cronbach's α = 0.40) of the 9-item KAP section of the survey. This may be attributed to the multidimensional nature of the KAP framework, the small number of items, and the inclusion of knowledge-based questions that do not reflect a single latent construct. Despite this, the items were developed by expert consensus to ensure content relevance and remain useful for capturing key aspects of perinatal mental health literacy and behaviors. Future work may involve separating the KAP domains into subscales, conducting factor analysis to explore dimensionality, or refining and expanding the item pool to improve internal consistency. Third, convenience sampling from the outpatient obstetrics clinic at KK Women's and Children's Hospital may reduce the generalizability of findings to the broader Singapore population. Finally, it is worth noting that the majority of participants in our study were of Chinese ethnicity, employed, and had attained university-level education, which may limit the generalizability of our findings to more diverse or less-advantaged Asian populations.
Conclusion
In conclusion, our study highlights high rates of perinatal depression and anxiety, alongside suboptimal mental health literacy among women. These findings, together with insights from a recent survey of healthcare professionals (50), informed the development of the Singapore Perinatal Mental Health Guidelines on Depression and Anxiety (17). In parallel, initiatives have been introduced to strengthen public education and outreach, as well as to enhance training within primary healthcare settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Human Ethics and Consent to Participate declarations. The research procedures for this study received formal approval for an exempt review from the SingHealth Centralized Institutional Review Board (CIRB Ref No. 2022/2454). All participants have provided consent to participate in this study. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
PQ: Formal analysis, Writing – original draft, Data curation, Methodology, Conceptualization, Writing – review & editing, Supervision. ZP: Writing – review & editing. HC: Writing – review & editing. T-EC: Writing – review & editing. LT: Writing – review & editing. KT: Resources, Writing – review & editing, Funding acquisition, Supervision, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Integrated Platform for Research in Advancing Metabolic Health Outcomes in Women and Children (IPRAMHO) - Singapore Ministry of Health's National Medical Research Council Centre Grant NMRC/CG/C008A/2017_KKH.
Acknowledgments
Perinatal Mental Health Guidelines On Depression & Anxiety Committee: Helen Chen, KK Women's and Children's Hospital; Tze-Ern Chua, KK Women's and Children's Hospital; Theresa LEE, KK Women's and Children's Hospital; Elizabeth Junpei SIAK, KK Women's and Children's Hospital; Lin Feng HONG, KK Women's and Children's Hospital; Ying Chia CH'NG, KK Women's and Children's Hospital; Yasmin HASSAN, KK Women's and Children's Hospital; Cornelia Yin Ing CHEE, National University Hospital; Yee Ming MOK, Institute of Mental Health; Say How ONG, Institute of Mental Health; Victor Samuel RAJADURAI, KK Women's and Children's Hospital; Tiong Ghee TEOH, KK Women's and Children's Hospital; Vasuki UTRAVARTHY, Health Promotion Board; Kok Hian Tan, KK Women's and Children's Hospital; and Lay Kok Tan, KK Women's and Children's Hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1623596/full#supplementary-material
References
1. World health organization. Guide for integration of perinatal mental health in maternal and child health services. (2022) Geneva: World Health Organization. Available online at: https://www.who.int/publications/i/item/9789240057142 (Accessed June 25, 2024).
2. Sambrook Smith M, Lawrence V, Sadler E, Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open. (2019) 9:e024803. doi: 10.1136/bmjopen-2018-024803
3. Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. (2020) 19:313–27. doi: 10.1002/wps.20769
4. Bauer A, Knapp M, Parsonage M. Lifetime costs of perinatal anxiety and depression. J Affect Disord. (2016) 192:83–90. doi: 10.1016/j.jad.2015.12.005
5. Rifkin-Graboi A, Bai J, Chen H, Hameed WB, Sim LW, Tint MT, et al. Prenatal maternal depression associates with microstructure of right amygdala in neonates at birth. Biol Psychiatry. (2013) 74:837–44. doi: 10.1016/j.biopsych.2013.06.019
6. Soh SE, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, et al. Cohort profile: growing up in Singapore towards healthy outcomes (GUSTO) birth cohort study. Int J Epidemiol. (2014) 43:1401–9.
7. Qiu A, Tuan TA, Ong ML, Li Y, Chen H, Rifkin-Graboi A, et al. COMT haplotypes modulate associations of antenatal maternal anxiety and neonatal cortical morphology. Am J Psychiatry. (2015) 172:163–72. doi: 10.1176/appi.ajp.2014.14030313
8. Chong SC, Broekman BF, Qiu A, Aris IM, Chan YH, Rifkin-Graboi A, et al. Anxiety and Depression during pregnancy and temperament in early infancy: findings from a multi-ethnic, asian, prospective birth cohort study. Infant Ment Health J. (2016) 37:584–98. doi: 10.1002/imhj.21582
9. Rifkin-Graboi A, Kong L, Sim LW, Sanmugam S, Broekman BF, Chen H, et al. Maternal sensitivity, infant limbic structure volume and functional connectivity: a preliminary study. Transl Psychiatry. (2015) 5:e668. doi: 10.1038/tp.2015.133
10. Law EC, Aishworiya R, Cai S, Bouvette-Turcot AA, Broekman BFP, Chen H, et al. Income disparity in school readiness and the mediating role of perinatal maternal mental health: a longitudinal birth cohort study. Epidemiol Psychiatr Sci. (2021) 30:e6. doi: 10.1017/S204579602000102X
11. Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. (2014) 384:1775–88. doi: 10.1016/S0140-6736(14)61276-9
12. Viswasam K, Eslick GD, Starcevic V. Prevalence, onset and course of anxiety disorders during pregnancy: a systematic review and meta analysis. J Affect Disord. (2019) 255:27–40. doi: 10.1016/j.jad.2019.05.016
13. Adrianto N, Caesarlia J, Pajala FB. Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis. Obstet Gynecol Sci. (2022) 65:287–302. doi: 10.5468/ogs.21265
14. Camoni L, Mirabella F, Gigantesco A, Brescianini S, Ferri M, Palumbo G, et al. The impact of the COVID-19 pandemic on women's perinatal mental health: preliminary data on the risk of perinatal depression/anxiety from a national survey in Italy. Int J Environ Res Public Health (2022) 19:14822. doi: 10.3390/ijerph192214822
15. Harrison S, Quigley MA, Fellmeth G, Stein A, Alderdice F. The impact of the Covid-19 pandemic on postnatal depression: analysis of three population-based national maternity surveys in England (2014-2020). Lancet Reg Health Eur. (2023) 30:100654. doi: 10.1016/j.lanepe.2023.100654
16. Chen KK, Umboh SJ, Chua T, Chua MS, Yik CM, Poon NY, et al. Impact of the COVID-19 pandemic on the prevalence of postnatal depression in Singapore. Proc Singap Healthcare. (2023) 32:1–3. doi: 10.1177/20101058231207691
17. Chen H, Chua TE, Lee TMY, Siak EJ, Hong LF, Ch'ng YC, et al. Consensus statement on Singapore perinatal mental health guidelines on depression and anxiety. Ann Acad Med Singap. (2023) 52:467–75. doi: 10.47102/annals-acadmedsg.2023148
18. Pang S, Subramaniam M, Lee SP, Lau YW, Abdin E, Chua BY, et al. The Singaporean public beliefs about the causes of mental illness: results from a multi-ethnic population-based study. Epidemiol Psychiatr Sci. (2018) 27:403–12. doi: 10.1017/S2045796017000105
19. Arifin SRM, Cheyne H, Maxwell M. Review of the prevalence of postnatal depression across cultures. AIMS Public Health. (2018) 5:260–95. doi: 10.3934/publichealth.2018.3.260
20. Cheng H, Wang C, McDermott RC, Kridel M, Rislin JL. Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J Couns Dev. (2018) 96:64–74. doi: 10.1002/jcad.12178
21. Daehn D, Rudolf S, Pawils S, Renneberg B. Perinatal mental health literacy: knowledge, attitudes, and help-seeking among perinatal women and the public - a systematic review. BMC Pregnancy Childbirth. (2022) 22:574. doi: 10.1186/s12884-022-04865-y
22. Further Easing of Community and Border Measures. Available online at: https://www.moh.gov.sg/news-highlights/details/further-easing-of-community-and-border-measures (Accessed April 6, 2024).
23. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
24. Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh postnatal depression scale in antepartum and postpartum women. Acta Psychiatr Scand. (2009) 119:350–64. doi: 10.1111/j.1600-0447.2009.01363.x
25. Smith-Nielsen J, Egmose I, Wendelboe KI, Steinmejer P, Lange T, Vaever MS. Can the Edinburgh postnatal depression scale-3A be used to screen for anxiety? BMC Psychol. (2021) 9:118. doi: 10.1186/s40359-021-00623-5
26. Chong MF, Wong JX, Colega M, Chen LW, van Dam RM, Tan CS, et al. Relationships of maternal folate and vitamin B12 status during pregnancy with perinatal depression: the GUSTO study. J Psychiatr Res. (2014) 55:110–6. doi: 10.1016/j.jpsychires.2014.04.006
27. Zhu CS, Tan TC, Chen HY, Malhotra R, Allen JC, Ostbye T. Threatened miscarriage and depressive and anxiety symptoms among women and partners in early pregnancy. J Affect Disord. (2018) 237:1–9. doi: 10.1016/j.jad.2018.04.012
28. Teo C, Chia AR, Colega MT, Chen LW, Fok D, Pang WW, et al. Prospective associations of maternal dietary patterns and postpartum mental health in a multi-ethnic asian cohort: the growing up in Singapore towards healthy outcomes (GUSTO) study. Nutrients. (2018) 10:299. doi: 10.3390/nu10030299
29. Padmapriya N, Bernard JY, Liang S, Loy SL, Shen Z, Kwek K, et al. Association of physical activity and sedentary behavior with depression and anxiety symptoms during pregnancy in a multiethnic cohort of Asian women. Arch Womens Ment Health. (2016) 19:1119–28. doi: 10.1007/s00737-016-0664-y
30. Lim HA, Chua TE, Malhotra R, Allen JC, Teo I, Chern BSM, et al. Identifying trajectories of antenatal depression in women and their associations with gestational age and neonatal anthropometry: a prospective cohort study. Gen Hosp Psychiatry. (2019) 61:26–33. doi: 10.1016/j.genhosppsych.2019.09.001
31. Waschmann M, Rosen K, Gievers L, Hildebrand A, Laird A, Khaki S. Evaluating the impact of the COVID-19 pandemic on postpartum depression. J Womens Health. (2022) 31:772–8. doi: 10.1089/jwh.2021.0428
32. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
33. Chua TE, Bautista DC, Tan KH, Yeo G, Chen H. Antenatal anxiety: prevalence and patterns in a routine obstetric population. Ann Acad Med Singap. (2018) 47:405–12. doi: 10.47102/annals-acadmedsg.V47N10p405
34. Shorey SY, Ng ED, Chee CYI. Anxiety and depressive symptoms of women in the perinatal period during the COVID-19 pandemic: a systematic review and meta-analysis. Scand J Public Health. (2021) 49:730–40. doi: 10.1177/14034948211011793
35. Moyer CA, Compton SD, Kaselitz E, Muzik M. Pregnancy-related anxiety during COVID-19: a nationwide survey of 2740 pregnant women. Arch Womens Ment Health. (2020) 23:757–65. doi: 10.1007/s00737-020-01073-5
36. Saccone G, Florio A, Aiello F, Venturella R, De Angelis MC, Locci M, et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol. (2020) 223:293–5. doi: 10.1016/j.ajog.2020.05.003
37. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. (2004) 103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f
38. Dlamini LP, Amelia VL, Shongwe MC, Chang PC, Chung MH. Antenatal depression across trimesters as a risk for postpartum depression and estimation of the fraction of postpartum depression attributable to antenatal depression: a systematic review and meta-analysis of cohort studies. Gen Hosp Psychiatry. (2023) 85:35–42. doi: 10.1016/j.genhosppsych.2023.09.005
39. Adina J, Morawska A, Mitchell AE, Haslam D, Ayuku D. Depression and anxiety in second and third trimesters among pregnant women in Kenya: a hospital-based prevalence study. J Affect Disord Rep. (2022) 10:100447. doi: 10.1016/j.jadr.2022.100447
40. Begum MR, Biswas SC. Changes in depressive symptoms during the antenatal period: a cohort study from Bangladesh. Indian J Psychol Med. (2020) 42:519–24. doi: 10.1177/0253717620954337
41. Zhou J, Zhang S, Teng Y, Lu J, Guo Y, Yan S, et al. Maternal pregnancy-related anxiety and children's physical growth: the Ma'anshan birth cohort study. BMC Pregnancy Childbirth. (2023) 23:384. doi: 10.1186/s12884-023-05711-5
42. Huang W, Li G, Wang D, Qu H, Tian M, Wang Y. Postpartum depression literacy in Chinese perinatal women: a cross-sectional study. Front Psychiatry. (2023) 14:1117332. doi: 10.3389/fpsyt.2023.1117332
43. Hu Y, Huang S, Xiao M, Fu B, Tang G, Lommel L, et al. Barriers and facilitators of psychological help-seeking behaviors for perinatal women with depressive symptoms: a qualitative systematic review based on the consolidated framework for implementation research. Midwifery. (2023) 122:103686. doi: 10.1016/j.midw.2023.103686
44. Gong W, Jin X, Cheng KK, Caine ED, Lehman R, Xu DR. Chinese women's acceptance and uptake of referral after screening for perinatal depression. Int J Environ Res Public Health. (2020) 17:8686. doi: 10.3390/ijerph17228686
45. Tan GTH, Shahwan S, Goh CMJ, Ong WJ, Wei KC, Verma SK, et al. Mental illness stigma's reasons and determinants (MISReaD) among Singapore's lay public - a qualitative inquiry. BMC Psychiatry. (2020) 20:422. doi: 10.1186/s12888-020-02823-6
46. Pang S, Liu J, Mahesh M, Chua BY, Shahwan S, Lee SP, et al. Stigma among Singaporean youth: a cross-sectional study on adolescent attitudes towards serious mental illness and social tolerance in a multiethnic population. BMJ Open. (2017) 7:e016432. doi: 10.1136/bmjopen-2017-016432
47. Yuan Q, Abdin E, Picco L, Vaingankar JA, Shahwan S, Jeyagurunathan A, et al. Attitudes to mental illness and its demographic correlates among general population in Singapore. PLoS ONE. (2016) 11:e0167297. doi: 10.1371/journal.pone.0167297
48. Hanafiah AN, Van Bortel T. A qualitative exploration of the perspectives of mental health professionals on stigma and discrimination of mental illness in Malaysia. Int J Ment Health Syst. (2015) 9:10. doi: 10.1186/s13033-015-0002-1
49. Shamblaw AL, Botha FB, Dozois DJ. Accounting for differences in depression stigma between Canadian Asians and Europeans. J Cross Cult Psychol. (2015) 46:597–611. doi: 10.1177/0022022115575076
50. Poo ZX, Quah PL, Chen H, Wright A, Teoh TG, Tan LK, et al. Knowledge, attitude and perceptions around perinatal mental health among doctors in an obstetrics and gynaecology academic department in Singapore. Cureus. (2023) 15:e38906. doi: 10.7759/cureus.38906
51. Gupta J, Kaushal S, Priya T. Knowledge, attitude, and practices of healthcare providers about perinatal depression in Himachal Pradesh-a cross-sectional study. J Family Med Prim Care. (2023) 12:478–83. doi: 10.4103/jfmpc.jfmpc_1170_22
Keywords: perinatal mental health, maternal mental health, perinatal depression, perinatal anxiety, Edinburgh Postnatal Depression Scale (EPDS), knowledge, attitudes, and practices (KAP), help-seeking behavior, prevalence
Citation: Quah PL, Poo ZX, Chen HY, Chua T-E, Tan LK and Tan KH (2025) Perinatal mental health in Singapore—prevalence, knowledge, attitudes, and practices. Front. Med. 12:1623596. doi: 10.3389/fmed.2025.1623596
Received: 06 May 2025; Accepted: 21 August 2025;
Published: 11 September 2025.
Edited by:
Tingyu Mu, Anhui Medical University, ChinaReviewed by:
Astrid Berg, Stellenbosch University, South AfricaPhyllis Ohene-Agyei, The University of Auckland, New Zealand
Haixia Feng, Shandong Public Health Clinical Center, China
Copyright © 2025 Quah, Poo, Chen, Chua, Tan and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Phaik Ling Quah, ZXFwbEBudXMuZWR1LnNn
 Phaik Ling Quah
Phaik Ling Quah Zi Xi Poo3
Zi Xi Poo3 Tze-Ern Chua
Tze-Ern Chua Kok Hian Tan
Kok Hian Tan