Abstract
Global disparities in access to radiation medicine are driven not only by infrastructure deficits but also by shortages of trained medical physicists. To address these gaps, RAD-AID International implemented four virtual educational initiatives in Kenya, Guyana, and Türkiye, along with a global lecture series, each aimed at strengthening local capacity in medical physics. Implementing such programs across diverse low- and middle-income country (LMIC) contexts presents significant challenges, particularly with regard to adaptability, engagement, and sustainability. To evaluate these efforts, we applied the Consolidated Framework for Implementation Research (CFIR) and the CFIR Expert Recommendations for Implementing Change (ERIC) Matching Tool to retrospectively identify barriers and recommend strategies to strengthen future initiatives. Stakeholders across all programs consistently cited limited access to knowledge and information as a key barrier. In response, the ERIC strategy “Conduct Educational Meetings” was highly endorsed, with 79% of experts identifying it as a top recommendation. Additional barriers, such as adaptability, planning, and responsiveness to patient needs, were matched with strategies including promoting adaptability, developing formal implementation blueprints, and engaging patients and families. By linking CFIR constructs to concrete examples, this study demonstrates the utility of structured implementation frameworks in radiological education and underscores the need for contextual sensitivity in resource-limited settings.
Introduction
Radiation medicine is fundamental to modern cancer care; however, access to radiotherapy remains profoundly unequal. In LMICs, over 90% of the population lacks access to basic radiotherapy services (1). Radiological imaging is similarly essential, supporting cancer detection, staging, treatment planning, and disease monitoring, with an estimated 3.2% of global cancer deaths attributable to insufficient imaging access (2). The global cancer burden is expected to increase by 77% from 2022 to 2050, disproportionately affecting LMICs and placing increasing pressure on diagnostic and therapeutic infrastructure (3). Radiological services such as computed tomography (CT), magnetic resonance imaging (MRI), and nuclear medicine also support the diagnosis and management of cardiovascular disease, tuberculosis, and maternal complications. However, disparities remain stark: LMICs often have fewer than one CT scanner per million people compared to nearly 40 per million in high-income countries (4). In recognition of this, the World Health Assembly recently issued a resolution calling for the global expansion of diagnostic imaging capacity, emphasizing workforce development as a central pillar (5).
These disparities are not solely infrastructural but also reflect critical workforce shortages. Medical physicists play an essential role in ensuring the safe and effective delivery of radiological care, yet many LMICs lack accredited training programs altogether. This has led to underutilized equipment and acute shortages of qualified personnel (23). Despite their importance, medical physicists are often overlooked in global health initiatives, which tend to focus more broadly on service delivery or infrastructure expansion. In addition, continuing education opportunities in medical subspecialties also remain fragmented or inaccessible in many LMICs (6).
To help address these gaps, RAD-AID International, a non-profit organization that works to improve access to medical imaging and radiology services (21), launched four virtual educational initiatives. These initiatives included the following: (1) a global medical physics education lecture series; (2) a diagnostic and therapeutic physics course for radiation oncology residents in Kenya; (3) a medical imaging physics course for radiology residents in Guyana; and (4) a comprehensive MRI course in Türkiye. The Global Medical Physics Education Lecture Series (GMPELS), delivered between 2022 and 2024, enrolled 226 participants, more than half of whom were practicing clinical medical physicists. The Guyana initiative, established in 2021 at Georgetown Public Hospital, was designed for radiology residents with limited prior exposure to physics (7). In Kenya, the program supported 26 residents at the University of Nairobi and aligned with national efforts aimed at staffing 12 new radiotherapy centers (8). The Turkish MRI course introduced 160 learners to foundational and advanced imaging principles over 9 weeks. Each initiative was tailored to meet local needs but differed in delivery format, audience, and content focus. Table 1 summarizes the design and characteristics of each program.
Table 1
| Program | Location | Audience | Number of participants | Duration | Focus |
|---|---|---|---|---|---|
| Kenya | University of Nairobi | Radiation oncology residents | 26 | 1 year | Introduction to diagnostic and therapeutic medical physics, covering radiation production and detection, imaging modalities (X-ray, CT, MRI, ultrasound, nuclear medicine), radiation safety, treatment planning, brachytherapy, quality assurance, and advanced techniques, such as IMRT and stereotactic procedures |
| Guyana | University of Georgetown | Radiology residents with limited physics background | 4 | 5 weeks | Medical imaging modalities (X-ray, CT, MRI, ultrasound, fluoroscopy, mammography, and nuclear medicine) with a focus on basic physics, image quality, safety, and informatics |
| Türkiye MRI Course | Türkiye | General medical imaging learners(??) | 160 | 9 weeks | Introduction to medical imaging principles (NMR, spatial encoding, agentic relaxation, sequence design, quality assurance, MRI safety) |
| Global Medical Physics Education Lecture Series (GMPELS) | Virtual | Medical physicists, medical physics students, and individuals engaged in academic medical physics work | 226 | Ongoing monthly presentations | A mix of radiotherapy and diagnostic imaging topics, including ultrasound and MRI physics, brachytherapy, modern linear accelerator and proton therapy techniques, treatment planning, dosimetry, imaging modalities, motion management, surface guidance, safety, and anatomy |
An overview of virtual medical physics initiatives sponsored by RAD-AID.
This table provides a comparative overview of each course design, each tailored to specific learner needs and regional contexts.
These initiatives reflect a broader shift toward technology-mediated health education as a means of improving professional capacity at scale. Online platforms offer cost-effective and flexible mechanisms for delivering specialized content across geographic and resource constraints. One illustrative example is Brazil’s Virtual Learning Environment of the Unified Health System (AVASUS), which is among the largest public health education platforms in the world. With more than 2 million registered learners, AVASUS has demonstrated success in expanding access to continuing professional development and improving readiness for health system service delivery (9). Similar digital platforms have been shown to improve health workforce performance, particularly when tailored to local needs and paired with sustained engagement strategies (20).
Despite these advantages, virtual education initiatives face meaningful implementation challenges. These challenges include difficulties in adapting content to local clinical contexts, engaging participants over time, and ensuring sustainability beyond the initial training period. Programs that span diverse LMIC settings must also contend with variability in infrastructure, staffing, institutional priorities, and learner needs (10–12). Understanding how these factors influence program outcomes is essential for optimizing educational investments.
To evaluate these dimensions, we applied the Consolidated Framework for Implementation Research (CFIR), a comprehensive implementation science model that identifies barriers and facilitators across five domains: intervention characteristics, outer setting, inner setting, characteristics of individuals, and implementation process (13, 19). In addition, we used the CFIR Expert Recommendations for Implementing Change (ERIC) Matching Tool, which links each identified barrier to expert-endorsed implementation strategies based on established consensus (14–16). The matching tool enables users to retrospectively evaluate implementation efforts and identify strategies likely to improve adoption, fidelity, and sustainability.
This study aims to assess the implementation of RAD-AID’s four educational programs using CFIR and the ERIC Matching Tool. Specifically, we sought to answer two research questions: (1) What implementation barriers were encountered across the four programs? and (2) Which ERIC strategies were most frequently matched to these barriers? We hypothesized that, although challenges would differ across programs, certain strategies would emerge as broadly applicable and that linking CFIR constructs to recommended actions would provide insight into strengthening future initiatives.
Methods
To evaluate the implementation of four educational initiatives, we administered a structured questionnaire to stakeholders involved in the design and delivery of each program. The questionnaire was organized by the five domains of the Consolidated Framework for Implementation Research (CFIR) and asked respondents to select two perceived barriers from each domain. This yielded a total of 10 barrier selections per stakeholder. Participants included instructors, evaluators, and course organizers from Kenya (n = 3), Guyana (n = 3), Türkiye (n = 4), and the Global Medical Physics Education Lecture Series (GMPELS; n = 2). Although the total sample size was small, it reflected complete participation from all individuals directly engaged in each program and represented the complete set of available implementation stakeholders.
Once selected, CFIR barriers were entered into the CFIR Expert Recommendations for Implementing Change (ERIC) Matching Tool (14). This tool links each barrier to a list of 73 evidence-based implementation strategies developed through a consensus process involving 169 researchers, practitioners, and administrators. These experts identified and ranked the strategies they believed were most effective for overcoming specific CFIR-defined barriers (15, 16). For each queried barrier, the matching tool provides a list of strategies accompanied by the percentage of experts who endorsed each one among their top seven choices.
Barrier identification and strategy matching were conducted separately for each of the four programs. To interpret the outputs, we applied two complementary approaches. First, we calculated the cumulative percentage of expert endorsements for each strategy across all barriers within a program, which allowed us to identify those strategies most broadly applicable. Second, we highlighted the highest-ranked strategy for each specific barrier, enabling a more context-sensitive understanding of implementation needs. Because the study relied on a structured selection of pre-defined CFIR constructs rather than open-ended qualitative responses, thematic coding and inter-rater validation were not applied. The focus of the analysis was not on generating emergent themes but on mapping stakeholder-selected barriers to existing constructs in the CFIR framework and linking them to implementation strategies. All data were processed using Microsoft Excel, and no additional analytic software was used. De-identified questionnaire responses, CFIR-ERIC Matching Tool outputs, and related supporting materials are available from the corresponding author upon request.
Results
Table 2 summarizes the distribution of identified barriers by stakeholders across the five CFIR domains for each educational program. The domain-level percentages reflect the extent to which barriers in each domain were perceived by stakeholders as relevant to implementation. The Outer Setting domain accounted for the highest proportion of barriers in Türkiye (100%) and Kenya (75%), suggesting that external influences were dominant challenges in these contexts. Characteristics of Individuals were most prominent in Guyana (75%) and Türkiye (75%), reflecting challenges related to Individual Knowledge and Beliefs, or Readiness for Implementation. Barriers within the Inner Setting domain were less frequently selected across all programs, ranging from 21% (GMPELS) to 36% (Kenya), while Process barriers were moderately represented across all programs.
Table 2
| CFIR Domain | Kenya | Guyana | Türkiye | GMPELS |
|---|---|---|---|---|
| Intervention Characteristics | 38% | 50% | 38% | 38% |
| Outer Setting | 75% | 50% | 100% | 50% |
| Inner Setting | 36% | 29% | 29% | 21% |
| Characteristics of Individuals | 50% | 75% | 75% | 50% |
| Process | 44% | 44% | 67% | 33% |
Distribution of selected barriers across the five CFIR domains for each respective program.
This is expressed as a percentage of the total barriers identified within each domain.
The program-specific strategies are shown in Figures 1A–D. Across the four programs, several recurring implementation challenges were identified by stakeholders for each respective initiative. Strategies to address these barriers provided by the CFIR-ERIC Matching Tool are also visualized in Figures 1A–D. The ERIC strategies with the highest cumulative percentage match value for each intervention are displayed. The cumulative percentages exceed 100% because implementation experts of the CFIR-ERIC tool endorse the same strategy for multiple barriers independently. Notably, barriers related to external technical support, costs, or policy constraints generated the lowest cumulative percentage match values, reflecting the strong collaborative and logistical groundwork of these initiatives.
Figure 1

(A–D) ERIC strategies with the highest match value to the combination of identified barriers. Cumulative percentages represent the sum of expert endorsements across all selected CFIR barriers.
Tables 3–6 presents the most salient implementation barriers identified in each respective program, as organized by the CFIR construct. Each barrier is paired with an ERIC strategy that is most strongly endorsed by expert respondents (n = 169) as effective for addressing that specific barrier. The percentages reflect the number of experts selecting the strategy among their top seven for an indicated barrier. The suggested ERIC strategy output is dependent on the specific combination of topics indicated by the stakeholders from each initiative.
Table 3
| CFIR construct | Barrier description | Matched ERIC strategy | % experts endorsing strategy for barrier |
|---|---|---|---|
| Readiness for implementation | There are a few tangible and immediate indicators of organizational readiness and commitment to implement the innovation. | Assess for readiness and identify barriers and facilitators | 81% |
| Access to knowledge and information | Stakeholders do not believe that the innovation can be sufficiently adapted, tailored, or reinvented to meet local needs. | Conduct educational meetings | 79% |
| Patient needs and resources | Patient needs, including barriers and facilitators to meet those needs, are not accurately known, and/or this information is not a high priority for the organization. | Obtain and use patients/consumers and family feedback | 76% |
| Adaptability | Stakeholders do not believe that the innovation can be sufficiently adapted, tailored, or reinvented to meet local needs. | Promote adaptability | 73% |
| Patient needs and resources | Patient needs, including barriers and facilitators to meet those needs, are not accurately known and/or this information is not a high priority for the organization. | Involve patients/consumers and family members | 71% |
Top expert-endorsed ERIC strategies matched to CFIR-identified barriers in Kenya.
Table 4
| CFIR construct | Barrier description | Matched ERIC strategy | % experts endorsing strategy for barrier |
|---|---|---|---|
| Readiness for implementation | There are a few tangible and immediate indicators of organizational readiness and commitment to implement the innovation. | Assess for readiness and identify barriers and facilitators | 81% |
| Access to knowledge and information | Stakeholders do not have adequate access to digestible information and knowledge about the innovation, nor do they know how to incorporate it into work tasks. | Conduct educational meetings | 79% |
| Adaptability | Stakeholders do not believe that the innovation can be sufficiently adapted, tailored, or reinvented to meet local needs. | Promote adaptability | 73% |
| Champions | Individuals acting as champions who support, market, or ‘drive through’ implementation in a way that helps to overcome indifference or resistance from key stakeholders who are not involved or supportive. | Identify and prepare champions | 67% |
| Cosmopolitanism | The organization is not well networked with external organizations. | Build a coalition | 62% |
Top expert-endorsed ERIC strategies matched to CFIR-identified barriers in Guyana.
Table 5
| CFIR construct | Barrier description | Matched ERIC strategy | % experts endorsing strategy for barrier |
|---|---|---|---|
| Access to knowledge and information | Stakeholders do not have adequate access to digestible information and knowledge about the innovation, nor how to incorporate it into work tasks. | Conduct educational meetings | 79% |
| Patient needs and resources | Patient needs, including barriers and facilitators to meet those needs, are not accurately known, and/or this information is not a high priority for the organization. | Obtain and use patients/consumers and family feedback | 76% |
| Adaptability | Stakeholders do not believe that the innovation can be sufficiently adapted, tailored, or reinvented to meet local needs. | Promote adaptability | 73% |
| Planning | A scheme or sequence of tasks necessary to implement the intervention has not been developed, or the quality is poor. | Develop a formal implementation blueprint | 73% |
| Patient needs and resources | Patient needs, including barriers and facilitators to meet those needs, are not accurately known, and/or this information is not a high priority for the organization. | Involve patients/consumers and family members | 71% |
Top expert-endorsed ERIC strategies matched to CFIR-identified barriers in Turkish MRI course.
Table 6
| CFIR construct | Barrier description | Matched ERIC strategy | % experts endorsing strategy for barrier |
|---|---|---|---|
| Access to knowledge and information | Stakeholders do not have adequate access to digestible information and knowledge about the innovation, nor how to incorporate it into work tasks. | Conduct educational meetings | 79% |
| Adaptability | Stakeholders do not believe that the innovation can be sufficiently adapted, tailored, or reinvented to meet local needs. | Promote adaptability | 73% |
| Planning | A scheme or sequence of tasks necessary to implement the intervention has not been developed or the quality is poor. | Develop a formal implementation blueprint | 73% |
| Key stakeholders | Multi-faceted strategies to attract and involve key stakeholders in implementing or using the innovation (e.g., through social marketing, education, role modeling, and training) are ineffective or non-existent. | Identify and prepare champions | 63% |
| Goals and feedback | Goals are not clearly communicated or acted upon, nor do stakeholders receive feedback that is aligned with goals. | Audit and provide feedback | 61% |
Top expert-endorsed ERIC strategies matched to CFIR-identified barriers in the global medical physics education lecture series (GMPELS).
One prominent construct was Adaptability, the ability to tailor educational interventions to fit local needs and resources. For example, in Kenya, while the radiation oncology residents appreciated the didactic sessions, some of the material focused on advanced radiotherapy technologies, such as stereotactic radiosurgery, that were not available in their clinical setting. This technological mismatch occasionally limited the perceived immediate applicability of the content, suggesting opportunities to enhance contextual tailoring in future iterations. The construct Planning also appeared in both Kenya and Guyana, where it was recommended to be addressed with Develop a Formal Implementation Blueprint (73%), reflecting a shared gap in the formalized implementation process (Tables 3, 4; Figure 2).
Figure 2
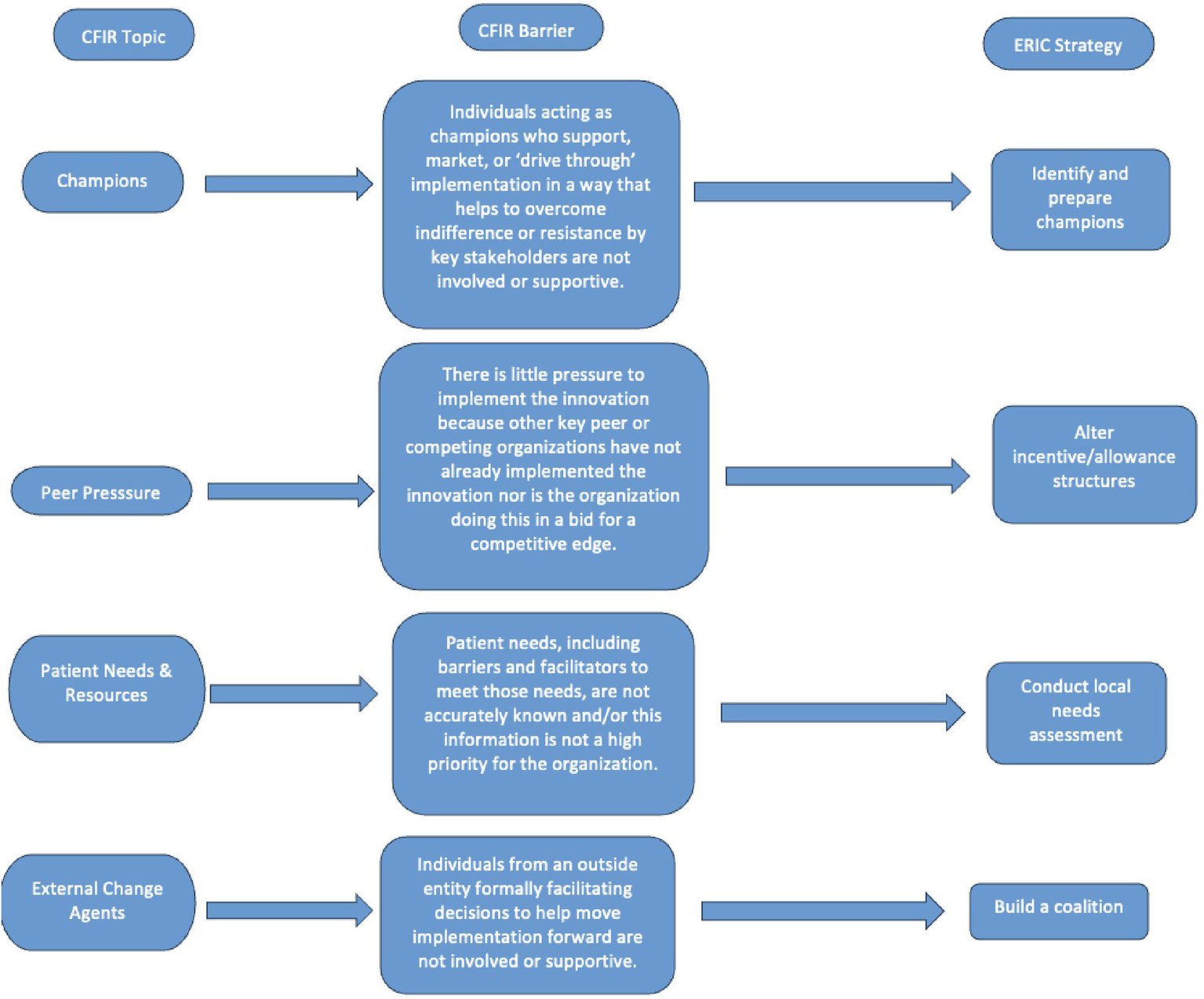
Process flowchart of salient CFIR barriers matched to corresponding ERIC strategy.
Another strategy that commonly emerged was the importance of identifying and preparing local champions or individuals who supported the intervention to help sustain momentum. In Guyana, there has historically been limited integration of physics expertise into the residents’ education, as there are only two medical physicists present within the health system as of June 2024. Strengthening the alignment between physics leadership and clinical training could help amplify the long-term impact of educational efforts. Identify and Prepare Champions also appeared in Türkiye under a slightly different construct (Champions), reinforcing the broader relevance of internal leadership development.
The limited role of Peer Pressure was also noted, particularly in Türkiye, where the MRI course was among the first of its kind. Of the four total stakeholders, three identified Peer Pressure as a barrier within the CFIR Outer Setting. Within the CFIR framework, Peer Pressure refers to the pressure exerted by external organizations having already implemented said intervention. Without comparable local or regional programs to serve as benchmarks or sources of professional momentum, there was relatively less institutional incentive to formalize or expand the course beyond its initial offering. Addressing this may require building professional networks or creating institutional recognition to reinforce the perceived value of such an initiative.
While individual programs presented unique implementation contexts, several core strategies recurred across sites, including promoting adaptability through the development of locally relevant case materials and strengthening leadership capacity by supporting local champions. This convergence suggests that, although tailoring to context remains essential, there is value in leveraging shared evidence-based strategies to address common challenges in an underemphasized medical subspeciality.
Discussion
This study offers insight into the implementation of four virtual educational initiatives designed to strengthen radiological capacity in LMIC settings. While each program operated within a distinct institutional and geographic context, several recurring barriers and corresponding strategies emerged. One of the most prominent constructs was Adaptability, which underscores the importance of aligning educational content with local clinical practice and technological availability. In Kenya, for example, the inclusion of advanced radiotherapy techniques, such as stereotactic radiosurgery, was perceived as less relevant, given that such technologies were not yet in use. Matching content to local resources may improve engagement and applicability, and the strategy “Promote Adaptability” was consistently endorsed for this barrier.
Another recurring barrier was planning. Both Kenya and Türkiye reported limited use of structured protocols to guide implementation. This gap was addressed through the ERIC strategy “Develop a Formal Implementation Blueprint,” which provides a framework for sequencing tasks, defining roles, and clarifying program goals. The absence of formal planning may undermine continuity and limit scalability, particularly for resource-constrained institutions seeking to replicate or sustain such programs.
Local leadership also played a significant role in influencing implementation outcomes. In Guyana, the limited integration of physics instruction into radiology residency training reflected both a structural gap and a lack of internal advocacy. At the time of the initiative, only two medical physicists were employed nationally, which constrained the visibility and influence of the discipline. This led stakeholders to identify “Champions” as a barrier, which matched the strategy “Identify and Prepare Champions.” In the CFIR framework, champions are individuals who actively promote and drive implementation, helping to overcome resistance and maintain momentum. In the context of medical physics, champions may serve as advocates for curricular inclusion, faculty support, or cross-disciplinary collaboration.
The absence of external reference points also emerged as a barrier in Türkiye. The construct “Peer Pressure” was identified by most stakeholders in reference to the MRI course, which was among the first of its kind in the country. In the absence of comparable programs to benchmark against, the course lacked institutional incentives for formalization or expansion. While CFIR defines peer pressure in a neutral sense, as the influence of external organizations implementing similar innovations, it may be useful to frame this concept more broadly as stakeholder alignment or sectoral signaling. Strategies such as building coalitions with professional societies or linking courses to certification pathways may help address this type of barrier.
While the primary focus of this study was identifying barriers, several supporting factors also became apparent. In the GMPELS initiative, for instance, the program evolved over time in response to participant feedback. Early sessions were sometimes misaligned with learner expectations, but adjustments were made to include topics such as proton therapy and MRI-guided radiotherapy (17). This iterative responsiveness strengthened the program’s reach and relevance. Similar adaptations may improve sustainability across settings.
Several limitations should be acknowledged. First, data were collected retrospectively and relied on stakeholder recall, which may introduce bias. Future studies could reduce this limitation through prospective data collection or triangulation with participant-level outcomes. Second, although the stakeholder sample represented all individuals directly involved in implementation, the small number of respondents limits the generalizability of findings. Third, while CFIR offers a useful framework for categorizing implementation factors, it does not completely account for broader structural determinants such as national workforce shortages, health financing, or regulatory frameworks. Recent proposals to expand CFIR with a sixth domain, Characteristics of Systems, may better capture these macro-level influences (18).
Despite these constraints, this study demonstrates how structured implementation frameworks can be applied to educational initiatives in radiological health. By linking CFIR constructs to targeted strategies, implementers can move beyond intuitive decision-making and adopt evidence-informed approaches that are responsive to local needs (22). The results suggest that, although contextual tailoring is essential, certain strategies, such as promoting adaptability, preparing local champions, and conducting structured educational meetings, may be broadly effective across settings.
Conclusion
Virtual education offers a scalable means of strengthening the medical physics workforce in LMICs, but successful implementation depends on careful alignment with the local context. By applying the Consolidated Framework for Implementation Research and the ERIC Matching Tool, this study identified recurring barriers and mapped them to evidence-based strategies across four distinct programs. Despite differences in geography and institutional structure, constructs such as Adaptability, Planning, and Access to knowledge appeared consistently, along with strategies that emphasized educational meetings, local leadership, and structured implementation planning. These findings support the utility of implementation science frameworks in designing and sustaining global health education efforts and point to a core set of strategies that may improve uptake, engagement, and long-term impact. Future research should continue to refine these approaches through prospective evaluation and integration with broader health system strengthening initiatives.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
NF: Writing – original draft, Writing – review & editing. EA: Writing – original draft, Writing – review & editing. JW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Atun R de Jongh T Secci F Ohiri K Adeyi O . Integration of targeted health interventions into health systems: a conceptual framework for analysis. Health Policy Plan. (2010) 25:104–11. doi: 10.1016/S1470-2045(15)00222-3
2.
Hricak H Abdel-Wahab M Atun R Lette MM Paez D Brink JA et al . Medical imaging and nuclear medicine: a lancet oncology commission. Lancet Oncol. (2021) 22:e136–72. doi: 10.1016/S1470-2045(20)30751-8
3.
World Health Organization . Global Cancer burden growing amidst mounting need for services. WHO News Release. (2024)
4.
Frija G Blažić I Frush DP Hierath M Kawooya M Donoso-Bach L et al . How to improve access to medical imaging in low- and middle-income countries?EClinicalMedicine. (2021) 38:101034. doi: 10.1016/j.eclinm.2021.101034
5.
World Health Organization. WHA78 . Resolution on strengthening medical imaging capacity. Geneva: World Health Assembly (2025).
6.
Merry L Castiglione SA Rouleau G Létourneau D Larue C Deschênes M-F et al . Continuing professional development (CPD) system development, implementation, evaluation and sustainability for healthcare professionals in low- and lower-middle-income countries: a rapid scoping review. BMC Med Educ. (2023) 23:498. doi: 10.1186/s12909-023-04427-6
7.
Maharaj RG Maharaj P . Internal medicine residency program in Guyana: a collaborative model for sustainable graduate medical education in resource-limited settings. Front Public Health. (2017) 5:112. doi: 10.3389/fpubh.2017.00112
8.
Weygand J Hao Y Awol M Joseph AO Kibudde S Malloum A et al . Evaluating the readiness for ultra-hypofractionated prostate and breast radiotherapy in sub-Saharan Africa: a strategic needs-assessment of six leading African institutions. E-cancer Medical Sci. (2025) 19:1853. doi: 10.3332/ecancer.2025.1853
9.
Valentim RAM de Oliveira CAP Oliveira ESG Ribeiro EL da Costa SM Morais IRD et al . Virtual learning environment of the Brazilian health system (AVASUS): efficiency of results, impacts, and contributions. Front Med. (2022) 9:896208. doi: 10.3389/fmed.2022.896208
10.
Kumwembe M Tembo E Sakwiya L Nyirenda R Chaphuka C Weygand J . Building radiation therapy technologist capacity in Malawi: overcoming challenges and expanding roles. J Med Imag Radiation Sci. (2025) 56:101905. doi: 10.1016/j.jmir.2025.101905
11.
Munkhtuvshin T Shagdarsuren B Bold B Khurelsukh K Myagmarsuren D Bryant JM et al . Cultivating expertise in MRI physics in Mongolia through international collaboration. J Med Imag Radiation Sci. (2025) 56:101897. doi: 10.1016/j.jmir.2025.101897
12.
Tazeh S Mbakwa R Tambe J Ali I Titi M Betifang M et al . A roadmap for expanding access to affordable diagnostic imaging services in west and Central Africa: lessons from Cameroon. J Med Imag Radiation Sci. (2025) 56:101977. doi: 10.1016/j.jmir.2025.101977
13.
Damschroder LJ Aron DC Keith RE Kirsh SR Alexander JA Lowery JC . Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
14.
CFIR-ERIC . Matching Tool v1.0. (2019). Available online at: https://cfirguide.org/choosing-strategies/ (Accessed May 15, 2025).
15.
Powell BJ Waltz TJ Chinman MJ Damschroder LJ Smith JL Matthieu MM et al . A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. (2015) 10:21. doi: 10.1186/s13012-015-0209-1
16.
Waltz TJ Powell BJ Matthieu MM Chinman MJ Smith JL Proctor EK . Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the expert recommendations for implementing change (ERIC) study. Implement Sci. (2015) 10:109. doi: 10.1186/s13012-015-0295-0
17.
Bryant JM Weygand J Keit E Cruz-Chamorro R Sandoval ML Oraiqat IM et al . Stereotactic magnetic resonance-guided adaptive and non-adaptive radiotherapy on combination MR-linear accelerators: current practice and future directions. Cancer. (2023) 15:2081. doi: 10.3390/cancers15072081
18.
Means AR Kemp CG Gwayi-Chore M-C Soi C Sherr K Wagenaar BH et al . Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. (2020) 15:17. doi: 10.1186/s13012-020-0977-0
19.
Damschroder LJ Reardon CM Opra Widerquist MA Lowery J . Conceptualizing outcomes for use with the consolidated framework for implementation research (CFIR): the CFIR outcomes addendum. Implement Sci. (2020) 15:23. doi: 10.1186/s13012-021-01181-5
20.
Jalloul M Miranda-Schaeubinger M Noor AM Stein JM Amiruddin R Derbew HM et al . MRI scarcity in low- and middle-income countries. NMR Biomed. (2023) 36:e5022. doi: 10.1002/nbm.5022
21.
Lugossy A-M Anton K Dako F Dixon RG DuCharme PA Duggan C et al . Building radiology equity: themes from the 2023 RAD-AID conference on international radiology and global health. J Am Coll Radiol. (2024) 21:1194–200. doi: 10.1016/j.jacr.2024.04.025
22.
Nilsen P . Making sense of implementation theories, models and frameworks. Implement Sci. (2015) 10:53. doi: 10.1186/s13012-015-0242-0
23.
Parker SA Weygand J Bernat BG the American Association of Physicists in Medicine Global Needs Assessment Committee . Assessing radiology and radiation therapy needs for cancer care in low- and middle-income countries: insight from a global survey of departmental and institutional leaders. Adv Radiat Oncol. (2024) 9:101615. doi: 10.1016/j.adro.2024.101615
Summary
Keywords
global health, medical physics, implementation sceince, education, training
Citation
Fedor N, Abrahamson EA and Weygand J (2025) A retrospective assessment of the implementation of virtual medical physics educational initiatives using the consolidated framework for implementation research. Front. Med. 12:1625455. doi: 10.3389/fmed.2025.1625455
Received
08 May 2025
Accepted
07 July 2025
Published
29 July 2025
Volume
12 - 2025
Edited by
Aimee Campbell, Columbia University, United States
Reviewed by
Talia Tene, Universidad Técnica Particular de Loja, Ecuador
Tom Clarijs, Belgian Nuclear Research Centre (SCK CEN), Belgium
Updates
Copyright
© 2025 Fedor, Abrahamson and Weygand.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: E. Axel Abrahamson, axel.abrahamson.27@dartmouth.edu
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.