Abstract
Introduction:
India has systematically integrated Indian traditional medicine systems Ayurveda, Yoga, Unani, Siddha, Sowa-rigpa including Homeopathy —collectively known as ‘Ayush’ into its public healthcare delivery. Since upgrading the Department of Ayush to a dedicated Ministry of Ayush in the year 2014, several landmark initiatives have been launched, including the National Ayush Mission (NAM), the establishment of Ayush Health and Wellness Centres under Ayushman Bharat, and the creation of the Ayushman Arogya Mandirs network. These efforts reflect a strategic commitment to enhance primary health care (PHC) by promoting culturally relevant, preventive, and affordable services.
Methods:
This practice and policy review employed a systematic approach to analyze the integration of Ayush into India’s PHC system. Primary and secondary source of data was drawn from national health policies, government reports, international frameworks, and official statistics between 2014 and 2024. Data was analyzed in detail to assess implementation status, infrastructure, global positioning, education, digital integration, and policy challenges.
Observations:
India’s traditional medicine sector includes 12,500 Ayushman Arogya Mandir led by qualified doctors of Ayurveda, Unani, Siddha, Sowarigpa and homeopathy doctors, 750,000 registered institutionally qualified practitioners, more than 700 Ayush medical colleges and attached hospitals, around 9,000 Ayush drug manufacturing industries, dedicated research councils for ewach of the Ayush system with their peripheral centers, a Pharmacopoeia Commission of Indian systems of Medicine and Homeopathy etc. Moreover, Ayush systems are integrated in 26,636 Primary Health Centres (PHCs), 6,155 Community Health Centres (CHCs), and 759 Districts Hospitals (DH) in the country. Ayush systems are also integrated in health infrastructure under Ministry of Defense, Ministry of Labour Welfare, Ministry of Railways etc. Public health programs targeting maternal health, geriatric care, and non-communicable diseases have incorporated Ayush-based approaches. Internationally, India has established academic collaborations and information cells across 42 countries and academic chairs across 38 countries, while domestic initiatives focus on digital health (Ayush Grid), education reform (NEP 2020), quality assurance, and cross-referral pathways.
Inference:
India’s integrative approach demonstrates how traditional medicine can enhance PHC delivery, particularly in underserved settings. With continued investment in evidence-based practices, regulatory alignment, and inclusive models, Ayush can play a pivotal role in achieving Universal Health Coverage and informing global traditional medicine strategies.
1 Introduction
India’s traditional medicine systems—Ayurveda, Yoga and Naturopathy, Unani, Siddha and Sowa rigpa have been an integral part of primary healthcare in households of Indians for centuries while Homeopathy is often considered alongside Traditional Indian system of Medicine and has been integrated and adopted into the country’s healthcare landscape for over two centuries—all of which have been regulated under the ambit of Ministry of Ayush. Each of these systems brings distinct epistemological frameworks and therapeutic approaches, collectively contributing to the landscape of primary health care (PHC) in the country. While Ayurveda has historically dominated scholarly and clinical attention, other Ayush systems are also accepted by the community, particularly in certain geographic regions Under the leadership of the Ministry of Ayush, the National Ayush Mission is taking this legacy forward by establishing Ayush health and wellness centers, co-locating Ayush services in existing health facilities, and supporting infrastructure, manpower, and medicine supply to ensure holistic and accessible healthcare.
In India formal education in traditional medicine evolved over thousands of years shifting from the Gurukul system (mentor-mentee training system, where knowledge was passed down orally or via apprenticeships within families) (1) to world class ancient Universities, e.g., Nalanda, Taksheela, Vikram Sheela in 3rd century BC to institutionalized university schooling system starting in the early 20th century. In the 20th century, the establishment of the first Ayurveda college in 1908, followed by the creation of regulatory bodies which are formal and legalized by the Act of parliament to bring uniformity in Ayush education system through NCISM and NCH (formerly known as CCIM and CCH).
Simultaneously, research ecosystem is fostered by establishing research councils such as CCRAS, (Central Council for Research in Ayurvedic Sciences), CCRH (Central council for Research in Homeopathy), CCRUM (Central council for Research in Unani Medicine), CCRS (Central council for Research in Siddha), and CCRYN (Central council for Research in Yoga and Naturopathy), and launched digital knowledge platforms like the Ayush Research Portal (2). Along with the extensive number of studies available, it was observed that corrective measures are being taken by the councils to upgrade research methodologies and their outcomes as per international standards.
In recent years, the Government of India has strategically boosted up efforts of harnessing the potential of Ayush systems into mainstream primary healthcare activities including creating separate Ayush infrastructure, optimizing Ayush trained HR and ensuring availability of therapies and medicines at grassroot level integrating with PHC network to contribute to prevention, health promotion, cultural relevance, and low-cost interventions, especially in underserved regions. This integration process involves both opportunities and challenges, including validation through scientific research, the development of collaborative models with biomedicine, and concerns about quality assurance and equitable access.
Globally, the World Health Organization (WHO) recognizes Traditional, Complementary, and Integrative Medicine (TCIM) as experience-based health systems that can be aligned with national healthcare frameworks when implemented safely and evidence-based. India’s Ayush integration efforts align with WHO’s Traditional Medicine Strategy 2025–2034, which advocates for rigorous evidence, quality standards, and equitable implementation (3).
To collate all the efforts of Ayush system towards Primary Health Care as a recognized healthcare system. This review was envisioned to analyze the implementation, scope, and outcomes of Ayush integration into India’s PHC from 2014 to 2024. It aims to evaluate both achievements and gaps by synthesizing data from national health programs, international collaborations, institutional developments, and public health indicators relevant to traditional medicine. An infographic summarizing the overall concept and flow of this manuscript is presented in Figure 1.
Figure 1

Infographic illustrating the overall structure and flow of this review, outlining the key sections and concepts discussed throughout the manuscript.
2 Methods
This review adopted a systematic, mixed-methods approach to examine the integration of Ayush systems into India’s primary health care (PHC) framework from 2014 to 2024. The study was collaboratively conducted by a multi-disciplinary team comprising researchers, Ayush clinicians, and policy analysts.
We employed a policy and program analysis framework based on the WHO’s health system building blocks (service delivery, health workforce, information systems, access to medicines, financing, and governance). The team conducted an iterative search and synthesis of national and international policy documents, government program reports, and academic literature.
2.1 Data sources and search strategy
Relevant data were sourced from the following platforms:
-
Government repositories: Ministry of Ayush website, Press Information Bureau (PIB), and Ministry of Statistics and Programme Implementation (MOSPI), National Health Policy 2017
-
International databases: WHO IRIS and WHO Traditional Medicine publications
-
Academic databases: Google Scholar and PubMed
-
Inclusion Criteria:
-
Timeframe: 2014 to 2024
-
Type of Sources: Peer-reviewed publications, national and international policy documents, official Ayush statistics, and validated institutional reports
-
Scope: Ayush integration in healthcare systems, education, globalization, and digital infrastructure
-
Language: English only
-
2.2 Review process
Each source was independently screened by at least two reviewers for relevance and quality. Discrepancies were resolved through discussion and consensus. Thematic coding was conducted using manual methods to group information under key domains such as policy implementation, service delivery models, education and regulation, public health outreach, digital innovations, and global engagement.
A data triangulation strategy was employed to validate findings across multiple sources. In cases where quantitative data were ambiguous or inconsistent, corroboration was sought from alternate repositories or direct institutional reports. Limitations in data availability or consistency are noted. The details of the sources reviewed are given in Table 1.
Table 1
| Source/Platform | Type of document | Access URL | Focus/Use in review |
|---|---|---|---|
| Ministry of Ayush Annual Reports (2014–2024) | Government reports | http://www.dbtayush.gov.in/resources/pdf/annualReport/AR_2024_2025.pdf | Programmatic coverage, service delivery models |
| Ayush Decade Growth Report (2014–2024) | Decadal summary report | https://aiia.gov.in/wp-content/uploads/2024/03/AyushDecadeGrowthReport-Eng-Final.pdf | Sector-wide achievements, schemes, reforms |
| WHO Traditional Medicine Strategy 2014–2023 | Global policy document | https://www.who.int/publications/i/item/9789241506096 | Global integration strategy, UHC alignment |
| WHO SEARO Traditional Medicine Progress | Regional review report | https://iris.who.int/handle/10665/340393 | South-East Asia regional progress 2014–2019 |
| NSSO 79th Round Report (2022–2023) | National Health Survey | https://www.mospi.gov.in | Ayush utilization, health-seeking behavior |
| Press Information Bureau (PIB) | Press releases | https://www.pib.gov.in/PressReleasePage.aspx?PRID=1740732 | Trade, global presence, export council |
| National Education Policy (NEP) 2020 | National policy document | https://www.education.gov.in/sites/upload_files/mhrd/files/NEP_Final_English_0.pdf | Education reforms and digital pedagogy for Ayush |
Tabulated summary of key sources consulted.
3 Observations
Observations for this policy review were derived from both primary and secondary data sources, enabling a comprehensive analysis. The findings are organized under six thematic subheadings: policy framework, infrastructure and manpower, public health initiatives and outreach, digital integration, and global outreach. The cumulative data from major sections is summarized in Figure 2.
Figure 2
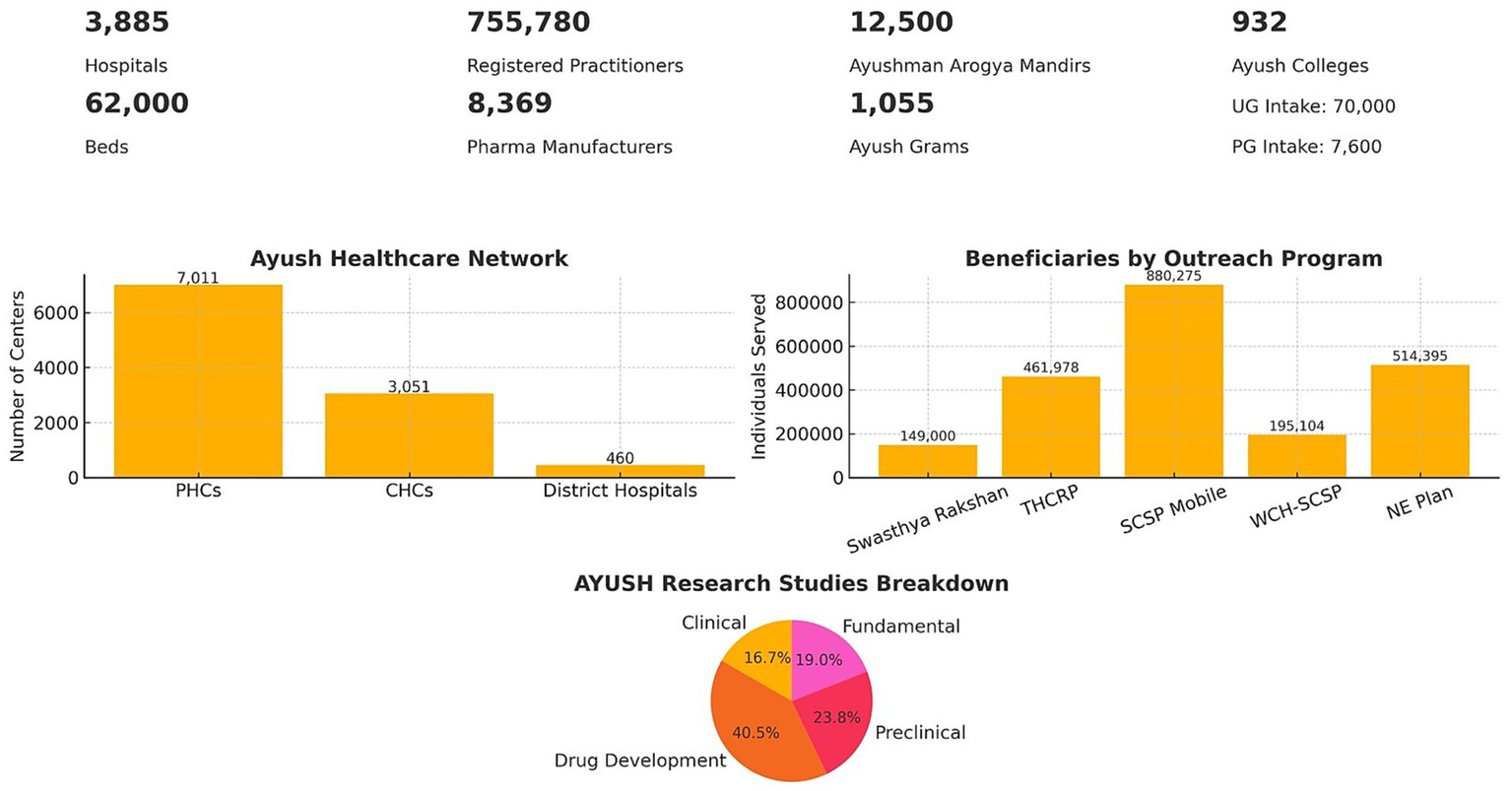
Overview of the AYUSH healthcare landscape in India. The infographic summarizes key statistics including the number of hospitals, beds, registered practitioners, pharmaceutical manufacturers, Ayushman Arogya Mandirs, Ayush Grams, and AYUSH colleges with their intake capacity. Bar graphs depict the AYUSH healthcare network (Primary Health Centres, Community Health Centres, and District Hospitals) and beneficiaries served through major outreach programs (Swasthya Rakshan, THCRP, SCSP Mobile, WCH-SCSP, and NE Plan). A pie chart illustrates the distribution of AYUSH research studies across drug development, preclinical, clinical, and fundamental categories.
3.1 Policy framework for Ayush integration into PHC (primary health care)
3.1.1 Healthcare
India’s commitment to mainstreaming Ayush into public health has been guided by evolving national policies. The National Health Policy (NHP) 2002 initiated efforts to incorporate Indian Systems of Medicine into health delivery, emphasizing access, affordability, and pluralism. The updated NHP 2017 advanced this vision by explicitly endorsing medical pluralism—defined as the coexistence and integration of multiple systems of healthcare—and by proposing structured, evidence-based inclusion of Ayush into Primary Health Care (PHC) (
4,
5). The 2017 policy outlines a three-dimensional strategy for Ayush mainstreaming (
6).
Service delivery through co-location in PHCs (Primary Health Centres) and CHCs (Community Health Centres), the backbone of India’s rural health infrastructure.
Research and evidence generation, particularly for prevention and chronic care management.
Education and human resource development
Complementing this policy vision, India’s leadership during its G20 presidency in 2023 culminated in the Gujarat Declaration, a high-level strategic document calling for the global integration of traditional medicine into PHC systems. This further enhanced India’s visibility in international health policy discussions (7). Hence for effective implementation efforts are being made through capacity building, quality assurance, and stakeholder collaboration across sectors (8).
In addition, the National List of Essential Medicines (NLEM), which guides the availability of key drugs in public health facilities and has traditionally focused on conventional (allopathic) medicines (9) has been recently updated now including Ayush formulations. Additionally, the Ministry of Ayush has created system-specific Lists of Essential Medicines (LEMs) for Ayurveda, Unani, Siddha, and Homoeopathy. These lists define which classical formulations should be prioritized for procurement and rational use in government-run Ayush hospitals (10).
Ayush services are now covered under India’s national health insurance scheme (PM-JAY) through 172 treatment packages offered by 27 insurers. In addition to insurance inclusion, the Ministry of Ayush is strengthening integration through policy reforms, sensitization of stakeholders, cross-referral pathways, digital health systems, and clinical protocol harmonization. These measures aim to enable accountable, interoperable healthcare while ongoing discussions with Insurance Regulation Authority of India (IRDAI) seek to incorporate Ayush more comprehensively under India’s ₹5 lakh (USD 5,850) family health coverage, promoting a holistic and inclusive care model (11–13).
3.1.2 Education and research
Significant governance reforms have taken place in Ayush education and regulation. The older regulatory bodies—the Central Council of Indian Medicine (CCIM) and the Central Council for Homoeopathy—were replaced in 2020 by:
NCISM: National Commission for Indian System of Medicine
NCH: National Commission for Homoeopathy
The NCISM and NCH regulate curricula and enforce ethical standards across the country. With NEP 2020, Ayush education now incorporates Indian Knowledge Systems (IKS), digital tools, interdisciplinary learning, and international fellowships. The institutions also offer doctoral and international fellowship programs in coordination with International Council for cultural Relations (ICCR) and Ministry of External Affairs, hosting students from 32 countries.
Policy reforms in Ayush research have focused on enhancing scientific rigor and ethical integrity through standardized guidelines and regulatory frameworks. Research must comply with OECD principles for preclinical studies, CTRI registration and IEC approval for clinical trials, and follow reporting standards like ARRIVE, STROBE, PRISMA, and CONSORT. Additionally, the ICMR’s Ethical Guidelines and its specific addendum for Ayush research provide a robust framework to ensure ethical conduct and quality in traditional medicine research.
Together, these institutions enable Ayush systems to not only expand service delivery but also generate evidence needed for mainstream health policy and international credibility.
3.1.3 Quality control and standardization
On the pharmaceutical side, in addition to GMP certification given to Ayush pharma manufacturing companies, the Pharmacopoeia Commission for Indian Medicine and Homoeopathy (PCIM&H) has been established as the apex body to develop quality standards for drugs. The One Herb, One Standard initiative—launched jointly with the Indian Pharmacopoeia Commission—aims to harmonize the standards used for identifying and testing medicinal plants across systems and agencies. Drug safety is regulated under the Drugs and Cosmetics Act, ensuring centralized oversight. India is also an active participant in the WHO’s International Regulatory Cooperation for Herbal Medicines (IRCH) and aligns with WHO Good Manufacturing Practices (GMP) to strengthen quality assurance and global credibility of its traditional medicine products. On the services part National Accreditation Board for Hospitals and Healthcare providers (NABH) for hospitals and National Assessment and Accreditation Council (NAAC) for educational institutions are implemented on par with Standards.
These policy, institutional, and regulatory mechanisms create an enabling ecosystem for Ayush to function as a co-equal component of India’s public health system. They also align with international goals of promoting culturally sensitive, inclusive, and evidence-informed healthcare models.
3.2 Sectoral infrastructure and workforce
In order to implement the policies made the next immediate requirement is infrastructure and Ayush Workforce.
3.2.1 Healthcare
As of 2024, India’s Ayush public health infrastructure includes 3,885 hospitals with over 62,000 beds and more than 755,780 registered Ayush practitioners. Ayush services have been co-located in 460 District Hospitals, 3,051 Community Health Centres (CHCs), 7,011 Primary Health Centres (PHCs), and over 3,000 additional health facilities under the National Health Mission (NHM). This widespread deployment underscores the increasing institutionalization of traditional medicine in India’s Primary Health Care (PHC) system (14).
Under the National Ayush Mission (NAM), over 12,500 Ayush Health and Wellness Centres (AHWCs) have been established. These centers provide preventive, promotive, and curative care, including yoga sessions, consultations, non-communicable disease (NCD) screenings, and dietary counselling. These centers known as Ayushman Arogya Mandirs serve as flagship AHWCs.
The Directorate General of Health Services (DGHS) now hosts a dedicated Ayush vertical. Indian Public Health Standards (IPHS) guidelines have been updated to include Ayush. Essential medicine lists have been issued, that allow to stock Ayush medicines at Jan Aushadhi Kendras (Public medicine stores). A separate Ayush sub-sector skill council is established for training of existing HR by upskilling, new skilling and re skilling programs.
3.2.2 Education and research
India’s Ayush education ecosystem includes 932 colleges and an annual intake of nearly 70,000 undergraduates and 7,600 postgraduate students. All India NEET and PG entrance examinations for traditional medicine, and skill development courses specifically targeting paramedical staff such as traditional medicine therapists and nurses have been introduced.
In parallel, India has built a substantial institutional research ecosystem. The Institute of Research and Training in Ayurveda (ITRA), Jamnagar an Institute of National Imminence, the All India Institute of Ayurveda (AIIA) in New Delhi and Goa, and the National Institute of Ayurveda, Jaipur as well as some other institutions under the Ministry of Ayush serve as the apex institutions for advanced education, clinical care, and integrative research in Ayurveda. Similarly, Institutes like National Institute of Homeopathy, Narela, National Institute of Siddha, Chennai serve as apex institutes of Homeopathy and Siddha traditional medicines. Additionally, Research council ecosystem has a top down model reaching the most remote areas. These centers are regionally distributed to study diverse health needs and traditional practices, and contribute significantly to the documentation, validation, and application of classical and local health traditions. Similarly, for all traditional medicine branches, the research councils work through their peripheral institutes and several other regional institutes established all over the country.
3.2.3 Quality control and standardization
The Ayush sector is progressively building its human resource capacity in the areas of quality control and standardization to ensure the safety, efficacy, and credibility of traditional medicine. Currently, India has over 8,369 licensed ASU&H drug manufacturing units, supported by 29 State Drug Testing Laboratories and several central and private labs approved under the Drugs & Cosmetics Act. However, the workforce dedicated to regulatory and quality assurance roles remains limited, with small number of Ayush drug inspectors.
To address this, the Ministry of Ayush and affiliated institutions like the Pharmacopoeial Commission for Indian Medicine & Homoeopathy (PCIM&H) offer specialized training programs. These include the Certificate Course in Quality Control of ASU&H Drugs, along with modules on GMP, phytochemical analysis, and drug testing protocols. Such capacity-building initiatives aim to equip technical personnel—pharmacists, analysts, and regulatory staff—with the necessary skills to uphold high standards in Ayush drug manufacturing and ensure compliance with national and international quality norms. There are more than 300 NABH accredited Ayush facilities in India as of 2025.
3.3 Public health outreach and awareness
As of the most recent National Sample Survey Office (NSSO) survey (2022–2023), awareness of Ayush systems stands at 94–96%, with usage rates exceeding 50% nationally (52.9% urban, 46.3% rural) (15–17). Which clearly demonstrates the position of Ayush systems in India. The outreach can be broadly understood in various contexts as following:
3.3.1 Integrating traditional medicine into primary health care in India
India’s integration of Ayush into Primary Health Care (PHC) is driven by a global and national recognition of the value of holistic, person-centered healthcare. This model, which emphasizes physical, mental, emotional, and spiritual well-being, is increasingly aligned with the principles of general practice and community-based healthcare. Ayush systems are not only deeply rooted in India’s cultural history but have now been systematically integrated into the country’s public health infrastructure. This integration enhances healthcare access, especially in rural and tribal areas where traditional medicine is often the first point of care (18, 19).
Several initiatives have been undertaken by various ministries, institutes, and organizations in India to strengthen the integration of Ayush into primary healthcare. The Ministry of Ayush has launched numerous programs, under the initiative called NAM and the integration of Ayush services into the National Programs (7). Notably, the Central Council for Research in Siddha (CCRS) has successfully deployed a traditional Siddha formulation, Nilavembu Kudineer for the prevention and management of dengue and chikungunya. Yoga has also been promoted through initiatives like the establishment of Preventive Health Care Units by the Morarji Desai National Institute of Yoga (MDNIY) in CGHS wellness centers across Delhi and National Capital Region. The Ministry of Defence has also established Ayurveda OPDs in Armed Forces Medical Services hospitals and Cantonment Board hospitals. These efforts collectively signify the government’s commitment to fostering an inclusive, multi-faceted healthcare system that marries traditional practices with contemporary healthcare delivery (20).
3.3.2 Flagship national health integration programs
The initiative NAM, launched in 2014, has facilitated a network of Integrated Ayush Hospitals, dispensaries, and co-located services across 7,011 PHCs, 3,051 CHCs, and 460 District Hospitals. Community outreach has extended to over 1,055 villages through the Ayush Grams initiative. The Ayush health and wellness centers called Ayushman Arogya Mandirs, 12,500 in number—serve as Ayush-led primary care centers delivering yoga, NCD screening, dietary counselling, and health education. These centers are distinct from allopathic facilities and emphasize preventive, promotive, and participatory healthcare.
Ayush interventions have been integrated into national health programs such as the NPCDCS, where over 1.89 million patients were screened and 175,000 enrolled in three pilot districts. Programs like the National Program for Musculoskeletal Disorders, Supraja (a program for maternal health), Vayo Mitra (a program for geriatric care), Ayurvidya (introduced for school health), and mobile medical units (MMUs) further demonstrate wide adoption (9).
3.3.3 Integration into other national programs
The Ministry of Ayush, has executed several outreach programs aimed at enhancing access to Ayush-based healthcare among underserved populations. While these efforts represent significant progress, they remain focused on targeted regions and subsets of the total eligible populations, highlighting the need for continued scale-up and systematic evaluation (
21).
Swasthya Rakshan Programme: A health promotion and disease prevention initiative implemented in selected regions to spread awareness about Ayush-based preventive care. It served over 149,000 individuals with services including lifestyle counseling, seasonal health advisories, and local herbal remedy promotion.
Tribal Health Care Research Programme (THCRP): This program addresses the health needs of indigenous (tribal) communities. It has reached over 461,978 individuals and documented 878 Local Health Traditions (LHTs), showcasing India’s vast ethnomedical knowledge systems. However, with India’s tribal population exceeding 104 million, further expansion remains a priority.
Scheduled Caste Sub Plan (SCSP) – Mobile Health Care Program: Provides mobile Ayush healthcare services to Scheduled Caste communities, serving 880,275 individuals. These programs are tailored to promote equity in healthcare delivery among historically disadvantaged groups.
Women and Child Health (WCH) under SCSP: Targets maternal and child health within Scheduled Caste populations, having served 195,104 patients. The initiative includes antenatal care, child nutrition, and Ayurvedic postpartum therapies.
Ayush Centres under North East Plan: Established in remote and geographically challenging regions of Northeast India, 19 centers have provided primary Ayush healthcare to over 514,395 people. These centers serve as models for integrative healthcare in difficult-to-reach areas.
In addition, select components of the Reproductive and Child Health (RCH) program have incorporated Ayush systems with promising results. The Central Council for Research in Ayurvedic Sciences (CCRAS) piloted the integration of Ayurvedic antenatal care protocols—particularly a classical pregnancy care regimen (Garbhini Paricharya)—at the primary health centre (PHC) level in regions like Gadchiroli, Maharashtra and Himachal Pradesh, yielding encouraging results in maternal health. These efforts reflect a growing institutional commitment to evidence-informed integrative healthcare.
Furthermore, CCRAS and other Ayush research councils operate peripheral institutes across India that combine structured outreach, clinical services, and health systems research. Many of these centers offer outpatient (OPD) services, and select ones also run inpatient (IPD) units, providing accessible Ayush-based care. While some are disease-specific (e.g., for cardiovascular diseases in New Delhi), others focus on therapeutic modalities (e.g., Panchakarma in Kerala) or broader thematic areas. This dual role enhances both research capacity and access to traditional medicine within the primary care ecosystem.
CCRAS has also collaborated with tertiary care institutions like Safdarjung Hospital in New Delhi to build integrative models for managing conditions such as osteoarthritis. At the national level, the Ayush-ICMR Advanced Centre for Integrative Health Research (AI-ACIHR) at AIIMS aims to build rigorous scientific foundations for such integrative care practices under the Indian Council of Medical Research (ICMR) umbrella. Together, these initiatives reflect India’s strategic emphasis on scalable, evidence-based integration of traditional systems into modern public health frameworks (22).
3.3.4 Malnutrition free India (Kuposhan Mukt Bharat) and Ayush-based nutritional strategies
Ayush plays an active role in India’s public health nutrition efforts through its engagement with the “Kuposhan Mukt Bharat” (Malnutrition-Free India) initiative. The Ministry of Ayush has released dietary advisories that align traditional Ayurvedic nutritional principles with contemporary public health standards. These guidelines are seasonally and regionally adapted and offer age- and condition-specific dietary recommendations for children, pregnant and lactating women, and individuals with anemia and undernutrition (23).
To reinforce community-level implementation, four targeted yoga modules—designed for children (ages 3–6), adolescent girls, pregnant women, and lactating mothers—were developed and disseminated through the Integrated Child Development Services (ICDS) platform via Anganwadi (community health) workers. These modules were jointly supported by the Ministries of Ayush and Women and Child Development under the broader scheme of “Suposhit Bharat” (Well nourished India) through well balanced Ayurveda diet (24).
The Ministry of Ayush also contributed traditional knowledge inputs to the revision of nutrition guidelines under the National Food Security Act (NFSA), 2013 (23). Ayurveda-inspired dietary counselling is a key service at Ayush Health and Wellness Centres (HWCs) established under NAM.
Additionally, research and field-level applications are underway to explore Rasayana-based dietary formulations and Ayurveda-inspired recipes for managing nutritional deficiencies such as childhood malnutrition and anemia (25). These initiatives emphasize preventive, promotive, and culturally contextual approaches to nutrition-sensitive healthcare.
Complementary efforts include the establishment of Poshan Vatikas (gardens with nutritional fruit bearing plants) and Ayurveda Nutrigardens in schools and communities, integration of Ayurveda-based dietary education in Ekalavya Model Residential Schools through collaborations with the Ministry of Tribal Affairs (MoTA) and the Ministry of Women and Child Development (WCD), and dissemination of Ayurveda Aahar (Ayurveda based diet) guidelines to promote sustainable, locally sourced, and culturally relevant nutrition practices.
These programs are executed jointly by Ayush research councils, state health departments, and local health workers. Through these, cost effective Ayush products and services are made available to everyone’s doorstep.
India’s model of Ayush integration in PHC serves as a replicable framework for culturally contextual, affordable, and scalable traditional medicine deployment worldwide. With its deep institutional foundations, cross-sectoral engagement, and global vision, the Ayush ecosystem is poised to become a cornerstone of both national health planning and global public health innovation.
These descriptions have been simplified into a flowchart illustrating how Traditional Medicine can be integrated across PHC levels (Figure 1).
3.4 Digital integration and information systems
The Ayush Grid (26)—a comprehensive digital health initiative—includes platforms such as A-HMIS (Ayush Hospital Management Information System), e-Aushadhi (digital supply chain), NAMASTE Portal (terminology and morbidity reporting), e-Charak (herbal networks), and Tools like eSanjeevani allow remote Ayush consultations.
Research tools such as the Ayush Research Portal, Traditional Knowledge Database Library (TKDL), Research Management Information System (RMIS), and e-Grantha (library automation and networking) facilitate transparency and access to clinical and traditional knowledge repositories.
Pharmacovigilance and adverse drug reaction (ADR) reporting are supported through tools like Ayush Suraksha portal and Suraksha Ayush application. Further to these advancements, interoperability with mainstream health IT systems under the Ayushman Bharat Digital Mission (ABDM) has started evolving.
A recent WHO technical brief, Mapping the Application of Artificial Intelligence in Traditional Medicine, developed with input from Ministry of Ayush, highlighted the potential of AI to enhance traditional medicine practices while underscoring ethical considerations such as data bias, patient privacy, informed consent, and safeguarding cultural heritage, reinforcing the importance of responsible digital integration (27).
3.5 Global positioning and collaborations
Traditional medicine systems are gaining renewed global relevance as countries seek to build more culturally appropriate, preventive, and cost-effective health systems. According to the WHO Global Report on Traditional and Complementary Medicine (TCM) 2019, 88% of WHO Member States (170 countries) report using some form of Traditional, Complementary and Integrative Medicine (TCIM), with 107 countries having national offices and 75 maintaining dedicated research institutes (25). The WHO Traditional Medicine Strategy 2025–2034 further emphasizes the importance of integrating TCIM into national health systems in an evidence-based, safe, and equitable manner.
At the global market level, the demand for herbal medicines—a core component of many TCIM systems—is projected to grow from USD 233 billion in 2024 to over USD 437 billion by 2032 (28). In many developed countries, use of TCIM is substantial: an estimated 24–71% of Europeans in different countries and 40% of US adults report having used some form of TCIM in recent years (29, 30).
India hosts the WHO Global Centre for Traditional Medicine (GCTM) in Jamnagar. International campaigns such as “Heal in India” and Ayush visas for Medical Value Travel (MVT) enhance India’s soft power. India has 42 Ayush Information Cells across 38 countries and 15 academic Chairs at global universities (31).
Formal recognition of Ayurveda systems exists in Sri Lanka, UAE, Oman, Malaysia, Nepal, Colombia, Tanzania, Hungary, Serbia, and others. Siddha is recognized in Sri Lanka and Malaysia; Sowa Rigpa in Bhutan and Mongolia. These recognitions result from diplomatic efforts by the Ministry of Ayush (32). Also, some Ayush practices, training courses and some forms of practice have been recognized in various countries across the globe like Switzerland, Australia, etc. (33).
Academic Collaboration and Trade Promotion: India has launched the Ayush Export Promotion Council (Ayushexcil) to boost global trade, regulatory cooperation, and academic partnerships (34). In fiscal year 2023–24, India’s exports of Ayush and herbal products grew by 3.6%, rising from USD 628.54 million to USD 651.17 million within a year (35). A dedicated IC scheme provides support to drug manufacturers/service providers to boost export.
Despite these significant strides in global outreach and recognition, strategic efforts are still needed to position India as the global leader in traditional medicine. Strengthening regulatory harmonization, evidence-based validation, and international collaborations will be key to realizing this potential.
4 Strategic future directions for global integration of Ayush
Looking forward, India’s traditional medicine sector can play a pivotal role in shaping the future of integrative healthcare — both domestically and globally. Several strategic directions can guide this evolution:
Digital Education Ecosystem: Establish dedicated centers for Ayush educational technology and innovation, including simulation-based Panchakarma labs, virtual learning platforms, and AI-driven pedagogy. Integration with NEP 2020 will ensure global competitiveness and skill-based training (36).
Policy-Oriented Implementation Science: Develop collaborations between Ayush institutions and public health bodies to evaluate the scalability, fidelity, and cost-effectiveness of Ayush Health & Wellness Centres under the National Ayush Mission. This will help generate implementation evidence to inform health policy and financing.
Global Harmonization of Quality Standards: Work closely with WHO, ISO, and partner countries to harmonize protocols, safety standards, and pharmacopoeial specifications. This is essential for enabling cross-border regulatory acceptance and scaling integrative care models (37).
Artificial Intelligence in Clinical Decision Support: Leverage AI tools trained on Ayush clinical data to enhance diagnosis, patient stratification, and treatment personalization — especially in the domains of non-communicable diseases and mental health.
Transdisciplinary Medical Education: Embed comparative modules on Ayush and biomedicine into MBBS, BAMS, and allied health curricula. This supports NEP 2020’s call for transdisciplinary and integrative education and promotes mutual understanding among systems.
One Health Integration via Ayush-Biodiversity Interface: Position Ayush systems within One Health frameworks, particularly for addressing zoonotic disease prevention, antimicrobial resistance (AMR), and climate-sensitive health challenges through sustainable, plant-based solutions.
All the strategic plans require a strong evidence informed research backup therefore Research methodologies become and integral part of Primary Healthcare Integration.
5 Research perspectives and methodologies in traditional medicine (TM) within primary healthcare
India’s primary healthcare system, particularly in rural and semi-urban areas, encounters diverse challenges that conventional biomedical approaches alone cannot fully address. Integrating Traditional Medicine (TM)—including codified systems like Ayurveda, Yoga, Unani, Siddha, and Homeopathy, along with local ethnomedical practices—has opened avenues for inclusive and culturally grounded healthcare delivery, offering new research frontiers.
5.1 Ethnomedical documentation and preservation
Community-based ethnographic studies have helped document region-specific health practices and therapies. Programs like the Tribal Health Care Research Programme (THCRP) have recorded 878 Local Health Traditions, while the Medico-Ethno Botanical Survey (MEBS) led by CCRAS collects and validates folklore-based health claims (38, 39). Although concerns persist about the marginalization of non-codified systems, including tribal medicine (40, 41), they are being addressed through safeguards focused on preserving indigenous knowledge and ensuring equitable benefit-sharing.
5.2 Public health, phytopharmacology, and clinical validation
TM research increasingly addresses lifestyle disorders, immunity, and preventive care—especially post-COVID-19. Phytopharmacological studies led by Council of Scientific and Industrial Research (CSIR) and collaborative missions with Ayush have advanced herbal drug development and standardization. Successful examples include development of Ayush-64 for malaria, which was later repurposed for COVID-19, and validation of classical formulations like Ashwagandha (Withania somnifera), Guduchi (Tinospora cordifolia), and Pippali (Piper longum) in scientifically designed studies (42). Examples of promising research outputs include clinical studies on Terminalia arjuna in cardiovascular diseases (43, 44). Guduchi (Tinospora cordifolia) for immunomodulation (45), and Ashwagandha (Withania somnifera) for stress reduction and mental well-being (46, 47). However, there remains a need for larger, multi-center trials to validate such findings at scale.
Randomized controlled trials (RCTs), though still limited in number, have evaluated TM therapies in conditions like psoriasis and osteoarthritis. Pragmatic and adaptive trials are gaining favor, given the multi-component nature of TM. Pragmatic controlled trials like the German RCT comparing Ayurvedic treatments with conventional care, and longitudinal studies at SDM Ayurveda Hospital, exemplify context-sensitive trial models (48, 49).
5.3 Personalized and genomic research
Ayurvedic concepts such as Prakriti (constitutional types) are now being explored through modern genomic research. Studies in Ayurgenomics are validating traditional classifications by linking them to molecular and genetic markers, enabling a new paradigm of personalized healthcare aligned with behavioral and metabolic traits (50–52).
5.4 Community participation and digital innovation
Community-Based Participatory Research (CBPR) models help ensure ethical and culturally appropriate research. By involving local stakeholders, these approaches promote trust and sustainability. Concurrently, digital health tools, telemedicine, AI-driven analysis, and mobile applications are improving monitoring, accessibility, and pharmacovigilance in TM research.
Despite substantial progress in the outreach and recognition, critical gaps remain that warrant systematic evaluation and strategic planning—paving the way for informed integration of Ayush into primary healthcare systems, as discussed in the following section.
6 Critical reflections on integrating Ayush into primary healthcare
India has made remarkable progress in integrating Ayush into its primary healthcare system, supported by strong policy frameworks and robust institutional mechanisms. Diverse models across states, expanding cross-referral pathways, and a steadily growing workforce reflect this momentum. The Ayush Research Portal now houses over 43,000 studies, spanning clinical research (~7,000), drug development (~17,000), preclinical research (~10,000), and fundamental studies (~8,000), offering a rich evidence base to inform clinical guidelines, academic curricula, and frontline practice. Looking ahead, emphasis on developing customized R&D protocols for Traditional Medicine, global harmonization of pharmacopoeial standards, innovative supply chain models for improved medicine accessibility, and expanded cultivation of medicinal plants will further strengthen integration. Conducive IPR policies that promote research while safeguarding the rights of knowledge holders will be crucial. Promising initiatives such as ICD-TM2 implementation through the Ayush Health Information Management System (AHIMS), responsible integration of AI in TM research and practice, advanced “Ayurveda Biology” projects including metabolomics studies, and personalized predictive–preventive healthcare models are emerging frontiers. How Ayush shapes and leads these developments will be pivotal to building a sustainable, globally relevant, and inclusive healthcare ecosystem.
7 Future possibilities for traditional medicine in primary health care interventions
Traditional Medicine (TM) is increasingly recognized as a valuable component of primary health care (PHC), offering cost-effective, culturally acceptable, and patient-centered approaches. The World Health Organization (WHO) has emphasized integrating TM into national health systems to address gaps in preventive, promotive, and curative care, particularly in low- and middle-income countries (53, 54). TM’s strength lies in its holistic and personalized framework, which addresses physical, mental, and social dimensions of health, making it well-suited for non-communicable disease (NCD) prevention, mental health promotion, and lifestyle modification (55, 56).
For instance, during the influenza outbreaks in early 20th century, Ayurvedic interventions such as fumigation therapy (Dhoopana) and the oral administration of herbal decoctions were widely adopted. These practices not only supported individual immunity but also contributed to community-level disease prevention and health promotion (57). During the COVID-19 pandemic, Ayush-based preventive and supportive strategies were widely implemented. These included usage of prophylactic formulations like herbal decoctions (Ayush Kadha), immunomodulatory formulations and medicinal oils for nasal therapy. A prominent example was the AYURAKSHA kit—developed by the All India Institute of Ayurveda, Delhi—which reported reduced COVID-19 incidence among Delhi Police personnel in a non-randomized trial (58). Similarly, systems such as Siddha and Unani contributed region-specific prophylactic and therapeutic protocols, while Yoga and Naturopathy approaches were integrated into mental health and well-being initiatives during COVID pandemic. The pluralistic nature of Ayush thus offers diverse tools for enhancing population health, but also highlights the need for robust evaluation frameworks that respect system-specific methodology.
The COVID-19 pandemic underscored the limitations of conventional PHC in managing chronic conditions, mental health burdens, and emerging challenges such as antimicrobial resistance (AMR) (59–61). Evidence suggests that TM interventions—such as Ayurveda’s Rasayana therapy, —can complement conventional strategies in immune modulation, stress reduction, and infection control (62, 63). Additionally, TM’s emphasis on diet, daily routines, and seasonal adaptation aligns with modern preventive health paradigms.
Looking forward, TM could play a transformative role through:
Integrative PHC Models – Combining evidence-based TM with biomedical protocols for prevention/wellness, addressing chronic disease management including NCD and mental health care from grass-root level. TM approaches such as personalized dietary guidance, detoxification, and herbal therapies offer supportive care for NCDs, which account for 74% of global deaths annually (64). Rasayana therapies like Triphala, Ashwagandha, and Amalaki show neuroprotective and immunomodulatory benefits in the elderly (65–68).
Addressing new health care challenges (AMR Mitigation) – Promoting rational research, creating evidence in exploring utility of traditional medicine in primary health care addressing latest health care challenges using antimicrobials and immunomodulators against the growing challenge that needs to be redressed. Herbal formulations with immunomodulatory and antimicrobial potential—like Ocimum sanctum, Tinospora cordifolia, Curcuma longa, and Withania somnifera—lowers AMR risk (69).
Community-Based Health Promotion – Empowering TM practitioners as frontline PHC providers. With Strategic policy support, rigorous research, and capacity building will ensure safe, effective, and equitable integration into future Public health frameworks. Ayush systems offer interventions such as Ashwagandha for anxiety (70), Bacopa monnieri, Shirodhara, and yoga-meditation programs for cognitive well-being (71–76). Ayush systems offer interventions such as Ashwagandha for anxiety (73), Bacopa monnieri, Shirodhara, and yoga-meditation programs for cognitive well-being (71–76), which are testaments of possibilities.
Digital Health Platforms – Delivering personalized TM-based lifestyle interventions and tele consultations making the reach of traditional medicine beyond and far across rural population.
Going forward, integration of TM into PHC will require investment in implementation science, interprofessional education, and robust regulatory frameworks. Strategic alignment with WHO and global policy directions will enhance TM’s contributions to an equitable, person-centered healthcare future.
8 Conclusion
India’s efforts to integrate Ayush systems into primary healthcare reflect a broader attempt to balance tradition with innovation in public health delivery. While significant progress has been made through service expansion, research, policy support, and global partnerships, active efforts are being implemented for overcoming challenges for ensuring consistent quality, workforce capacity, and evidence-based practice. The growing body of research, digital innovation, and community outreach are promising trends, thus are being met with rigorous evaluation and adaptive implementation models. The comprehensive roadmap for integrating traditional medicine into primary healthcare, along with the key implementation strategies, is summarized in Figure 3.
Figure 3

Flowchart illustrating key components essential for integrating Traditional Medicine into primary healthcare, including policy support, infrastructure, education, pharmaceutical standardization, digital systems, and pharmacovigilance mechanisms (Generated with the assistance of Napkin AI).
A balanced path forward would involve sustained investment in health systems research, capacity building, and participatory governance to ensure Ayush systems complement rather than compete with existing services. With equitable integration, grounded in public health priorities and responsive to community needs, Ayush can meaningfully contribute to India’s goals for universal health coverage and to the global discourse on integrative, person-centered care.
Statements
Author contributions
TN: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MN: Conceptualization, Investigation, Resources, Supervision, Validation, Writing – original draft. GR: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. RY: Methodology, Writing – original draft, Supervision. VH: Writing – original draft, Conceptualization. PD: Writing – original draft, Conceptualization. SGh: Methodology, Writing – original draft, Writing – review & editing. PG: Conceptualization, Writing – original draft, Methodology. VG: Conceptualization, Writing – original draft, Writing – review & editing. PS: Conceptualization, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. SGo: Data curation, Writing – original draft, Writing – review & editing. RK: Investigation, Writing – original draft, Writing – review & editing, Data curation, Resources. DP: Writing – review & editing, Data curation, Methodology, Formal analysis, Validation, Resources, Software.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors of the manuscript acknowledge the Ministry of Ayush for providing the data on policies and programs conducted nationwide.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. Chatgpt was used for language remodeling only.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The authors are affiliated with institutions under the Ministry of Ayush, Government of India, and this affiliation has informed their access to data and understanding of Ayush integration policies. The views expressed in this article are those of the authors and do not necessarily represent the official position of the Ministry of Ayush or the Government of India.
References
1.
Manohar PR . Ayurvedic education: where to go from here?Anc Sci Life. (2014) 33:143–5. doi: 10.4103/0257-7941.144615
2.
Ayush research portal . Available online at: https://ayushportal.nic.in (Accessed July 4, 2025)
3.
WHO global report on traditional and complementary medicine 2019. World Health Organization; (2019). Available online at: https://www.who.int/publications/i/item/978924151536 (Accessed May 16, 2025)
4.
Thyagarajan SP . Integration of Ayush within national health care systems: Challenges and the way forward. J Res Ayurvedic Sci. (2023) 7:59–64. doi: 10.4103/jras.jras_166_22
5.
Shankar D Patwardhan B . AYUSH for new India: vision and strategy. J Ayurveda Integr Med. (2017) 8:137–9. doi: 10.1016/j.jaim.2017.09.001
6.
Mohanty PC Sharma K . Households’ responses on medical pluralism: dynamics and determinants of access to traditional medicines in India. Clin Epidemiol Glob Health. (2021) 12:100880. doi: 10.1016/j.cegh.2021.100880
7.
Singh PA Bajwa N Hazra S Chandan A . Mapping out a direction: India’s G20 1447 presidency propels global promotion of traditional medicine. World Med Health Policy. (2024) 16:783–94. doi: 10.1002/wmh3.634
8.
Gautam M Sharma K Choudhary SK Anand A . Traditional Medicine as a part of Indian healthcare system: Challenges and Recommendations. Integrative Medicine Case Reports (2023) 4:71.
9.
Satheesh G Unnikrishnan MK Jha V Salam A . India’s latest essential medicines 1450 list: gaps, strengths and opportunities in evidence-based decision -making. BMJ Evid Based Med. (2023) 28:303–5. doi: 10.1136/bmjebm-2022-112171
10.
List of essential medicines. Available online at: https://namayush.gov.in/content/list-essential-medicines (Accessed April 4, 2025)
11.
Ministry of Ayush organises sensitisation event for insurance companies and Ayush hospital owners. (2024). Available online at: https://www.pib.gov.in/PressReleasePage.aspx?PRID=2021850 (Accessed June 15, 2025)
12.
Parveen A . Health insurance in India: a look into Ayushman Bharat- Pradhan Mantri Jan Arogya Yojana. Int J Multidisciplin Res. (2023) 5:1–5. doi: 10.36948/ijfmr.2023.v05i06.10519
13.
AYUSH under PM-JAY, Press Information bureau. Avaialble online at: https://www.pib.gov.in/PressReleaseIframePage.aspx?PRID=2043759 (Accessed May 16, 2025).
14.
IPHS of Ayushman Arogya Mandir. Available online at: https://ayush.karnataka.gov.in/storage/pdf-files/FinalAyushmanArogyaMandir.pdf (Accessed August 11, 2025)
15.
Survey on AYUSH 2022-23. Fact sheet. Available online at: https://www.mospi.gov.in/sites/default/files/publication_reports/Fact_sheet-Survey_on-Ayush.pdf (Accessed May 15, 2025)
16.
Rana MJ Kumar M Rahaman M Rahman MHU . Awareness, preference, and utilisation of Ayush in India: evidence from national sample survey, 2022-23. Adv Integr Med. (2025). doi: 10.1016/j.aimed.2025.03.006
17.
Srinivasan R Sugumar VR . Spread of traditional medicines in India: results of national sample survey organization’s perception survey on use of AYUSH. J Evid Based Complementary Altern Med. (2017) 22:194–204. doi: 10.1177/2156587215607673
18.
Das J Daniels B Ashok M Shim E-Y Muralidharan K . Two Indias: the structure of primary health care markets in rural Indian villages with implications for policy. Soc Sci Med. (2022) 301:112799. doi: 10.1016/j.socscimed.2020.112799
19.
Sen S Chakraborty R . Revival, modernization and integration of Indian traditional herbal medicine in clinical practice: importance, challenges and future. J Tradit Complement Med. (2017) 7:234–44. doi: 10.1016/j.jtcme.2016.05.006
20.
Saxena V Misra P Naveen KH Sumanth MM Das A Jain V . Strengthening AYUSH integration with preventive medicine. Indian J Community Med. (2024) 49:S183–90. doi: 10.4103/ijcm.ijcm_748_24
21.
Outreach activities/public health . Central Council for Research in Ayurvedic Sciences. (2021). Available online at: https://ccras.nic.in/services/outreach-activities-ccras/ (Accessed June 8, 2025)
22.
Ayush - ICMR Advanced Centre for Integrative Health Research (AI-ACIHR) at select AIIMS across the nation. Available online at: https://sansad.in/getFile/annex/267/AU3361_W0dMGQ.pdf?source=pqars#:~:text=The (Accessed June 15, 2025)
23.
Integration of Ayush in Lifestyle . (2022). Available online at: https://www.pib.gov.in/PressReleasePage.aspx?PRID=1810914 (Accessed June 12, 2025)
24.
Srikanth N . Global positioning and branding of Ayush food. J Drug Res Ayurvedic Sci. (2021) 6:119–21. doi: 10.4103/jdras.jdras_2_22
25.
Ayurvedic interventions for malnutrition: enhancing India’s nutrition programs for children . International journal of pharmaceutical sciences and research | IJPSR; (2025). Available online at: https://ijpsr.com/bft-article/ayurvedic-interventions-for-malnutrition-enhancing-indias-nutrition-programs-for-children/ (Accessed June 12, 2025)
26.
Available online at: https://journals.lww.com/ijar/fulltext/2023/04000/ayush_grid__digital_health_platform.2.aspx (Accessed August 11, 2025)
27.
Available online at: https://iris.who.int/bitstream/handle/10665/381769/9789240107663-eng.pdf?sequence=1 (Accessed August 11, 2025)
28.
Herbal medicine market size, share, growth analysis, 2032. Available online at: https://www.fortunebusinessinsights.com/herbal-medicine-market-106320# (Accessed September 15, 2025)
29.
Ventola CL . Current issues regarding complementary and alternative medicine (CAM) in the United States: part 1: the widespread use of CAM and the need for better-informed health care professionals to provide patient counseling. PT. (2010) 35:461–8.
30.
Lee EL Richards N Harrison J Barnes J . Prevalence of use of traditional, complementary and alternative medicine by the general population: a systematic review of national studies published from 2010 to 2019. Drug Saf. (2022) 45:713–35. doi: 10.1007/s40264-022-01189-w
31.
Available online at: https://aiia.gov.in/wp-content/uploads/2024/03/AyushDecadeGrowthReport-Eng-Final.pdf (Accessed cited June 12, 2025)
32.
Available online at: https://iris.who.int/bitstream/handle/10665/340393/9789290228295-eng.pdf?sequence=1&isAllowed=y (Accessed June 12, 2025)
33.
Yeola G Shirkande A Shirkande A Wele A . International delegate assembly: an overview of two decades. J Ayurveda Integr Med. (2024) 15:100892. doi: 10.1016/j.jaim.2024.100892
34.
AYUSH system of medicine become popular in many countries . Available online at: https://www.pib.gov.in/PressReleasePage.aspx?PRID=1740732 (Accessed June 12, 2025)
35.
Available online at: https://fitm.ris.org.in/sites/fitm.ris.org.in/files/Publication/Vaibhav (Accessed August 11, 2025)
36.
Available online at: https://www.education.gov.in/sites/upload_files/mhrd/files/NEP_Final_English_0.pdf (Accessed June 12, 2025)
37.
WHO Traditional Medicine Strategy, 2014-23. Available online at: https://iris.who.int/bitstream/handle/10665/92455/9789241506090_eng.pdf [cited (Accessed June 12, 2025)
38.
Doddamani SH Naik R Vendrapati RR Nagayya S Dixit AK Bhat S et al . Documentation and validation of local health traditions of Hassan district, Karnataka. J Drug Res Ayurvedic Sci. (2023) 8:19–25. doi: 10.4103/jdras.jdras_18_22
39.
Available online: https://www.researchgate.net/publication/339781532_Drug_Development_from_Ethno-medical_claims_and_Local_Health_Traditions_CCRAS_Initiatives#fullTextFileContent (Accesed June 8, 2025)
40.
Albert S Porter J . Is “mainstreaming AYUSH” the right policy for Meghalaya, Northeast India?BMC Complement Altern Med. (2015) 15:288. doi: 10.1186/s12906-015-0818-x
41.
Ijaz N Boon H . Statutory regulation of traditional medicine practitioners and practices: the need for distinct policy making guidelines. J Altern Complement Med. (2018) 24:307–13. doi: 10.1089/acm.2017.0346
42.
Sattigeri V . Council of Scientific and Industrial Research-AYUSH initiatives towards creating benchmarks. Int J Ayurveda Res. (2022) 3:48. doi: 10.4103/ijar.ijar_12_22
43.
Rastogi S Pandey MM Rawat AKS . Traditional herbs: a remedy for cardiovascular disorders. Phytomedicine. (2016) 23:1082–9. doi: 10.1016/j.phymed.2015.10.012
44.
Maulik SK Katiyar CK . Terminalia arjuna in cardiovascular diseases: making the transition from traditional to modern medicine in India. Curr Pharm Biotechnol. (2010) 11:855–60. doi: 10.2174/138920110793262051
45.
Verma M Rawat N Rani R Singh M Choudhary A Abbasi S et al . Adhatoda vasica and Tinospora cordifolia extracts ameliorate clinical and molecular markers in mild COVID-19 patients: a randomized open-label three-armed study. Eur J Med Res. (2023) 28:556. doi: 10.1186/s40001-023-01507-7
46.
Fanibunda SE Kukkemane K Ghai U Kolthur-Seetharam U Hingorani L Vaidya ADB et al . Withania somnifera regulates mitochondrial biogenesis and energetics in rat cortical neurons: role of BDNF and SIRT1. Mol Neurobiol. (2025). doi: 10.1007/s12035-025-04920-7
47.
Pandit S Srivastav AK Sur TK Chaudhuri S Wang Y Biswas TK . Effects of Withania somnifera extract in chronically stressed adults: a randomized controlled trial. Nutrients. (2024) 16. doi: 10.3390/nu16091293
48.
Witt CM Michalsen A Roll S Morandi A Gupta S Rosenberg M et al . Comparative effectiveness of a complex Ayurvedic treatment and conventional standard care in osteoarthritis of the knee--study protocol for a randomized controlled trial. Trials. (2013) 14:149. doi: 10.1186/1745-6215-14-149
49.
Sahu N Kamath S K P Sridhar Holla VK Sahu N Kamath S et al . Open pragmatic clinical trial evaluating the effect of virechana open pragmatic clinical trial evaluating the effect of virechana open pragmatic clinical trial evaluating the effect of virechana karma and tuvaraka rasayana in ekakushta/ psoriasis karma and tuvaraka rasayana in ekakushta/ psoriasis karma and tuvaraka rasayana in ekakushta/ psoriasis [internet]. Available online at: https://www.iamj.in/posts/images/upload/2776_2785.pdf (Accessed Augut 11, 2025).
50.
Prasher B Negi S Aggarwal S Mandal AK Sethi TP Deshmukh SR et al . Whole genome expression and biochemical correlates of extreme constitutional types defined in Ayurveda. J Transl Med. (2008) 6:48. doi: 10.1186/1479-5876-6-48
51.
Rani R Rengarajan P Sethi T Khuntia BK Kumar A Punera DS et al . Heart rate variability during head-up tilt shows inter-individual differences among healthy individuals of extreme Prakriti types. Physiol Rep. (2022) 10:e15435. doi: 10.14814/phy2.15435
52.
Aggarwal S Gheware A Agrawal A Ghosh S Prasher B Mukerji M et al . Combined genetic effects of EGLN1 and VWF modulate thrombotic outcome in hypoxia revealed by Ayurgenomics approach. J Transl Med. (2015) 13:184.
53.
WHO Traditional Medicine Strategy, 2014-23. Available online at: https://iris.who.int/bitstream/handle/10665/92455/9789241506090_eng.pdf?sequence=1 (Accessed August 11, 2025)
54.
Xu J Yang Y . Traditional Chinese medicine in the Chinese health care system. Health Policy. (2009) 90:133–9. doi: 10.1016/j.healthpol.2008.09.003
55.
Patwardhan B Mutalik G Tillu G . Integrative approaches for health. San Diego, CA: Academic Press (2015). 382 p.
56.
Bodeker G Kronenberg F . A public health agenda for traditional, complementary, and alternative medicine. Am J Public Health. (2002) 92:1582–91. doi: 10.2105/AJPH.92.10.1582
57.
Bhatwalkar SB Shukla P Srivastava RK Mondal R Anupam R . Validation of environmental disinfection efficiency of traditional Ayurvedic fumigation practices. J Ayurveda Integr Med. (2019) 10:203–6. doi: 10.1016/j.jaim.2019.05.002
58.
Nesari T Kadam S Vyas M Huddar VG Prajapati PK Rajagopala M et al . AYURAKSHA, a prophylactic Ayurvedic immunity boosting kit reducing positivity percentage of IgG COVID-19 among frontline Indian Delhi police personnel: a non-randomized controlled intervention trial. Front Public Health. (2022) 10:920126. doi: 10.3389/fpubh.2022.920126
59.
Kim JK Kim KH Shin YC Jang B-H Ko S-G . Utilization of traditional medicine in primary health care in low- and middle-income countries: a systematic review. Health Policy Plan. (2020) 35:1070–83. doi: 10.1093/heapol/czaa022
60.
Holmes EA O’Connor RC Perry VH Tracey I Wessely S Arseneault L et al . Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
61.
Singha B Singh V Soni V . Alternative therapeutics to control antimicrobial resistance: a general perspective. Front Drug Discov (Lausanne). (2024) 4. doi: 10.3389/fddsv.2024.1385460
62.
Tillu G Chaturvedi S Chopra A Patwardhan B . Public health approach of Ayurveda and yoga for COVID-19 prophylaxis. J Altern Complement Med. (2020) 26:360–4. doi: 10.1089/acm.2020.0129
63.
Luo E. Zhang D. Luo H. et al . Treatment efficacy analysis of traditional Chinese medicine for novel coronavirus pneumonia (COVID-19): an empirical study from Wuhan, Hubei Province, China. Chin Med (2020) 15. doi: 10.1186/s13020-020-00317-x
64.
Noncommunicable diseases. Available from: https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1 (Accesed September 25, 2025)
65.
Ahmed S Ding X Sharma A . Exploring scientific validation of Triphala Rasayana in ayurveda as a source of rejuvenation for contemporary healthcare: an update. J Ethnopharmacol. (2021) 273:113829. doi: 10.1016/j.jep.2021.113829
66.
Speers AB Cabey KA Soumyanath A Wright KM . Effects of Withania somnifera (Ashwagandha) on stress and the stress- related neuropsychiatric disorders anxiety, depression, and insomnia. Curr Neuropharmacol. (2021) 19:1468–95. doi: 10.2174/1570159X19666210712151556
67.
Bargale SS Shashirekha HK Baragi UC . Anti-aging effect of Amalaki rasayana in healthy elderly subjects. J Ayurveda Holistic Med. (2014) 2:10–8. doi: 10.70066/jahm.v2i1.138
68.
Baliga MS Meera S Rai MP Saldanha E Pais S Jayachander D et al . Use of the ayurvedic drug triphala in medical conditions afflicting older adults In: Foods and dietary supplements in the prevention and treatment of disease in older adults: Elsevier (2015). 135–42.
69.
Gupta PD Birdi TJ . Development of botanicals to combat antibiotic resistance. J Ayurveda Integr Med. (2017) 8:266–75. doi: 10.1016/j.jaim.2017.05.004
70.
Akhgarjand C Asoudeh F Bagheri A Kalantar Z Vahabi Z Shab-Bidar S et al . Does Ashwagandha supplementation have a beneficial effect on the management of anxiety and stress? A systematic review and meta-analysis of randomized controlled trials. Phytother Res. (2022) 36:4115–24. doi: 10.1002/ptr.7598
71.
Mathur D Goyal K Koul V Anand A . The molecular links of re-emerging therapy: a review of evidence of Brahmi (Bacopa monniera). Front Pharmacol. (2016) 7:44. doi: 10.3389/fphar.2016.00044
72.
Sardeshmukh S Deshmukh V Godse V Pathrikar A Joshi A Gujar S et al . Mind relaxation effect of Jatamansi Taila Shirodhara on psychological distress in triple negative breast Cancer patients - results of an open-labelled, randomised controlled clinical trial. J Ayurveda Integr Med. (2025) 16:101069. doi: 10.1016/j.jaim.2024.101069
73.
Rajan S Shamkuwar MK Tanwar AK . Impact of Shirodhara on biological markers of stress: a case study. J Ayurveda Integr Med. (2021) 12:178–81. doi: 10.1016/j.jaim.2021.01.008
74.
Thimmapuram J Patel K Madhusudhan DK Deshpande S Bouderlique E Nicolai V et al . Health-related quality of life outcomes with regular yoga and Heartfulness meditation practice: results from a multinational, cross-sectional study. JMIR Form Res. (2022) 6:e37876. doi: 10.2196/37876
75.
Tulloch A Bombell H Dean C Tiedemann A . Yoga-based exercise improves health-related quality of life and mental well-being in older people: a systematic review of randomised controlled trials. Age Ageing. (2018) 47:537–44. doi: 10.1093/ageing/afy044
76.
Gautam S Kumar M Kumar U Dada R . Effect of an 8-week yoga-based lifestyle intervention on psycho-neuro-immune axis, disease activity, and perceived quality of life in rheumatoid arthritis patients: a randomized controlled trial. Front Psychol. (2020) 11:2259. doi: 10.3389/fpsyg.2020.02259
Summary
Keywords
traditional medicine, Ayush systems, primary health care (PHC), integrative healthcare, universal health coverage (UHC), evidence-based Ayurveda, National Ayush Mission, health policy and systems integration
Citation
Nesari T, Nesari M, Ruknuddin G, Yadava RK, Huddar V, Dharmarajan P, Ghildiyal S, Gupta PK, Kumar R, Gupta V, Punera DS, Shetty P S and Goel S (2025) India’s journey in mainstreaming Ayush in primary health care—from tradition to integration. Front. Med. 12:1629515. doi: 10.3389/fmed.2025.1629515
Received
15 May 2025
Accepted
16 September 2025
Published
28 October 2025
Volume
12 - 2025
Edited by
Christian S. Kessler, Immanuel Hospital Berlin, Germany
Reviewed by
B. Ravishankar, Sri Sri College of Ayurvedic Science and Research, India
Parvathy Unnikrishnan, Amrita Vishwa Vidyapeetham University, India
Updates
Copyright
© 2025 Nesari, Nesari, Ruknuddin, Yadava, Huddar, Dharmarajan, Ghildiyal, Gupta, Kumar, Gupta, Punera, Shetty P and Goel.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tanuja Nesari, tnesari@hotmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.