Abstract
Background:
Androgenic alopecia (AGA) is the most common hair loss disease, caused by a combination of genetic factors and hormonal imbalances. Platelet-rich plasma (PRP) therapy has gained significant recognition in treating AGA, but optimal treatment protocol regarding centrifugation techniques has yet to reach a standardized consensus. We aim to conduct a systematic review and meta-analysis of randomized controlled trials (RCTs) to compare the efficacy of single-spin versus double-spin centrifugation protocols for PRP in patients with AGA.
Methods:
We searched PubMed, Embase, and Cochrane for RCTs comparing single-spin to double-spin PRP in AGA patients. The primary endpoint was the final platelets count after centrifugation. Secondary endpoints included improvement in hair density, as well as terminal and vellus hair rate. Statistical analysis was performed using RStudio software. Heterogeneity was assessed with I2 statistics.
Results:
We included 90 participants with AGA from three RCTs. The pooled mean difference (MD) for platelets concentration was 66.14 in single-spin compared to double-spin PRP (95% CI: −372.96 to 505.25; p = 0.77; I2 = 83.5%). The MD for change in hair density was 4.10% in single versus double-spin (95% CI: −4.74 to 12.93; p = 0.36; I2 = 0%). Moreover, the MD for terminal and vellus hair after single-spin versus double-spin PRP was 1.16 (95% CI: −3.34 to 5.66; p = 0.61; I2 = 0%), and −3.59 (95% CI: −12.49 to 5.30; p = 0.45; I2 = 4.8%), respectively.
Conclusion:
Our study suggests that single-spin PRP centrifugation is better in treating AGA patients compared to double-spin PRP.
Systematic review registration:
https://www.crd.york.ac.uk/PROSPERO/view/CRD42025643296, identifier CRD42025643296.
1 Introduction
Androgenic alopecia (AGA), the most common type of hair loss, is driven by a combination of genetic factors and hormonal imbalances (1). Increased levels of dihydrotestosterone (DHT), along with upregulated androgen receptors and caspases, contribute to cellular apoptosis and progressive hair thinning (1, 2). As DHT levels rise, the anagen phase of hair growth becomes shorter, while hair follicles in androgen-sensitive areas undergo miniaturization. Consequently, the hair becomes thinner, loses its pigment, and eventually transforms into vellus hair (1, 3).
Platelet-rich plasma (PRP) therapy has gained significant recognition in many fields, particularly in the treatment of AGA. Platelets are known to release multiple growth factors (GFs), such as platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and transforming growth factor beta (TGF-β), which facilitate cell proliferation, collagen synthesis, and angiogenesis (4, 5). It is suggested that PRP promotes the hair growth cycle, leading to increased hair density and shaft diameter, specifically promoting the growth of terminal hair, which is thick and pigmented (4, 6).
One of the key variables in PRP preparation is the centrifugation protocol. PRP can be prepared using either a single-spin or double-spin method, each yielding products with different cellular compositions. Single-spin techniques are simpler and quicker, typically resulting in higher platelet recovery but may retain more leukocytes. In contrast, double-spin protocols are designed to concentrate platelets while reducing leukocyte content, making them the preferred choice when leukocyte-poor PRP is desired – such as in aesthetic and dermatologic applications to minimize pro-inflammatory effects (7, 8).
Beyond AGA, the effects of centrifugation technique on PRP quality and clinical outcomes have been studied in various fields including orthopedics, dentistry, and sports medicine. These studies demonstrate that centrifugation strategy can significantly influence platelet concentration, GFs levels, and therapeutic efficacy depending on the clinical context (9–11). Despite the growing use of PRP in AGA, the efficacy and optimal treatment protocol regarding centrifugation techniques have yet to reach a standardized consensus, largely due to the insufficiency of comparative data on different centrifugation protocols (8, 12). We hypothesized that the choice of centrifugation method – single-spin versus double-spin – affects both platelet concentration and clinical outcomes in patients with AGA, with potential implications for therapeutic efficacy.
To our knowledge, this is the first systematic review and meta-analysis focusing specifically on randomized controlled trials (RCTs) comparing the efficacy of single-spin versus double-spin centrifugation protocols for PRP in patients with AGA. By providing a focused, evidence-based comparison, our study addresses a significant gap in the literature and contributes to the ongoing effort to standardize PRP protocols in hair restoration.
2 Methods
This Meta-Analysis and Systematic Review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under registration number (CRD42025643296), performed under the Cochrane Handbook for Systematic Reviews of Interventions, and reported adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines (13).
2.1 Eligibility criteria
Studies that met the following eligibility criteria were included: (1) RCTs; (2) comparing single-spin to double-spin centrifugation methods for PRP; (3) reporting the results in patients with AGA; and (4) reporting at least one clinical outcome of interest. No restrictions were applied to follow-up time or language. We excluded studies with: (1) overlapping patient populations; (2) observational design or of within-person RCT design; (3) had overlapping patient populations; (4) had no control group; (4) were performed in animals; (5) did not include patients with alopecia; and (7) with missing data on the interventional therapy used.
2.2 Search strategy and data extraction
We systematically searched PubMed, Embase, and Cochrane Central Register of Controlled Trials from inception to February 2025, using the following search terms: “alopecia,” “hair,” “baldness,” “platelet-rich plasma,” “platelet-enriched plasma,” “thrombocyte-rich plasma,” “autologous conditioned plasma,” “PRP,” “spin,” “spinning,” “centrifugation,” “centrifugal,” “centrifuge,” “separation,” “single-spin,” “one-spin,” “double-spin,” and “two-spin.” Boolean operators like “OR” and “AND” were used to optimize the search results. The complete search strategy can be found in the Supplementary Appendix 1. The references from all included studies, previous systematic reviews, and meta-analyses were also searched manually for any additional studies. Two authors (L.G. and N.K.) independently extracted the data following predefined search criteria and quality assessment. Disagreements were resolved by consensus among the two authors (L.G. and N.K.).
2.3 Endpoints
The primary endpoint was final platelet counts after centrifugation. Secondary endpoints were the percentage of change in hair density, the rate of final terminal hair, and the rate of vellus hair. The methods used for hair evaluation included standardized digital photography and analysis tools such as the Canon EOS 50D SLR with dermatoscope and NEO Image Analysis Software (14), and the FotoFinder® medicam 1000s, trichoscopy, and TrichoScan (15). In the study by Moftah et al. (16), we excluded group IV (single-spin) because it used a digital centrifuge, unlike the other three groups in that study, which used an electronic centrifuge. We made this exclusion to minimize heterogeneity due to differences in centrifuge settings and potential confounding factors. Moreover, we kept group II (double-spin) for comparison with group I (single-spin), as its second spin at 2,000 rpm was closer to the centrifugation speed used in the other included RCTs (16).
2.4 Statistical analysis
Mean difference (MD) and SD with 95% confidence intervals were used to compare the efficacy of single-spin PRP with double-spin PRP in AGA. Heterogeneity was assessed with I2 statistics and Cochran Q test; p values < 0.10 and I2 > 25% were considered significant for heterogeneity. For continuous outcomes, the inverse-variance method (IV) with REML was applied (17). A random-effects model was used for forest plots that included three studies, while a fixed-effects model was applied for forest plots that included two studies (18). We used RStudio software (version 2024.09.1+394) for statistical analysis.
2.5 Quality assessment
Cochrane Collaboration’s tool for assessing risk of bias in randomized trials (RoB 2) was used to assess the quality of individual RCTs (19). Two independent authors completed the risk of bias assessment (M.C.-C. and G.A.). Disagreements were resolved through a consensus after discussing reasons for the discrepancy.
3 Results
3.1 Study selection and baseline characteristics
The initial search yielded 197 results. After removal of duplicate records and ineligible studies, 13 remained and were fully reviewed based on inclusion criteria. Of these, a total of three RCTs were included in this meta-analysis, comprising a total of 90 participants diagnosed with AGA (Figure 1). Among the participants, 70 were male (77.8%). The baseline characteristics of the included studies, including PRP centrifugation parameters, alopecia classification systems, and follow-up durations, are summarized in Table 1. The follow-up periods ranged from 6 weeks to 12 months, providing a comprehensive view of short- and long-term outcomes.
FIGURE 1

PRISMA flow diagram of study screening and selection.
TABLE 1
| Study | Volume of PRP drawn per patient (ml) | Platelet activator | Single-spin (speed/time) | Double-spin (speed/time) | Follow-up (months) | No. of patients, n | No. of male patients, n (%) | Age (years), range, SD | Platelet count (thousand/μ l), mean | Alopecia classification | PRP regimen |
| Ince et al. (14) | 4–5 | Calcium chloride | 3,000 rpm for 15 min | 1st spin at 3,000 rpm for 15 min 2nd spin at 2,000 rpm for 5 min |
12 | 40 | 40 (100) | 29.95 | 272.5 | Type 2–4 (Hamilton-Norwood) | 1, 2, and 6 months after 1st injection |
| Moftah et al. (16) | 10 | None | 900 or 3,000 rpm for 10 min | 1st spin at 1,500 rpm for 10 min 2nd spin at 2,000 or 3,000 rpm for 5 min |
4 | 40 | 0 (0) | 25.75 ± 4.61 | 284.35 | Grade I and II (Ludwig) | 1 and 2 months after 1st injection |
| Legiawati et al. (15) | 13.5 | Calcium chloride or calcium gluconate | 3,000 rpm for 15 min | 1st spin at 1,500 rpm for 6 min 2nd spin at 2,500 rpm for 5 min |
1.5 | 30 | 30 (100) | 34.57 ± 7.53 | 307.66 | Stages III and VI (Hamilton–Norwood) | 2 and 4 weeks after 1st injection |
Baseline characteristics of included studies.
rpm, revolutions per minute; PRP, platelet-rich plasma; SD, standard deviation. Definitions of alopecia classification type varied between studies. The study by Moftah et al. (16), which included only female patients, used the Ludwig scale ranging from I to III. Grade I: perceptible thinning of the hair on the crown, limited in the front by a line situated 1–3 cm behind the frontal hairline. Grade II: pronounced rarefaction of the hair on the crown within the area seen in grade I. Grade III: full baldness (total denudation) within the area seen in grades I and II (33). On the other hand, the two other studies (14, 15) that included only male patients, used the Hamilton–Norwood scale ranging from I to VII. Stage II: the frontotemporal recession of the hairline does not extend further than 2 cm anterior to the mid-coronal line. Stage III: the frontotemporal recession of the hairline extends further than type II and may reach the midcoronal line. Stage IV: the frontotemporal recession of the hairline has receded beyond the mid-coronal line. Stage VI: the frontotemporal and vertex regions of the alopecia have become confluent, and the area of alopecia has increased laterally and posteriorly (34–36).
3.2 Pooled analysis of all studies
3.2.1 Platelet concentration
The three studies provided data on final platelet counts after centrifugation (14–16). A high degree of heterogeneity (I2 = 83.5%) was observed, likely attributable to differences in centrifuge settings and protocols across studies. The pooled MD for platelets concentration in single-spin versus double-spin centrifugation method was 66.14 (95% CI: −372.96 to 505.25; p = 0.77; Figure 2) (all values expressed in × 109/L), indicating no significant differences between single-spin and double-spin methods.
FIGURE 2

Final platelets count after centrifugation (all values expressed in ×109/L. SD, standard deviation; MD, mean difference; CI, confidence interval; IV, inverse variance.
3.2.2 Hair density improvement
The pooled analysis of hair density improvement included two studies (14, 15). The pooled MD for percentage change in hair density in single versus double-spin PRP was 4.10 (95% CI: −4.74 to 12.93; p = 0.36; Figure 3), with no significant heterogeneity (I2 = 0%). These results suggest no statistically significant difference in hair density improvement between single-spin and double-spin PRP centrifugation methods.
FIGURE 3

Percentage of change in hair density after PRP. SD, standard deviation; MD, mean difference; CI, confidence interval; IV, inverse variance.
3.2.3 Terminal hair count and vellus hair count
For terminal hair count differences, two studies were analyzed (15, 16). The pooled MD for the percentage change in terminal hair count in single-spin PRP, compared to double-spin PRP was 1.16 (95% CI: −3.34 to 5.66; p = 0.61; Figure 4A), with no heterogeneity detected (I2 = 0%).
FIGURE 4

Percentage of change in terminal (A) and vellus hair count (B) after PRP. SD, standard deviation; MD, mean difference; CI, confidence interval; IV, inverse variance.
For vellus hair count also reported by two studies, the pooled MD was −3.59 (95% CI: −12.49 to 5.30; p = 0.45; Figure 4B), with negligible heterogeneity (I2 = 4.8%) in single-spin versus double-spin PRP (15, 16). These findings suggest that neither centrifugation method had a statistically significant advantage in improving terminal or vellus hair counts.
3.3 Quality assessment
The risk of bias assessment, performed using the RoB 2 tool, is summarized in Figure 5. Two studies were rated as having a low risk of bias across all domains (14, 15). Moftah et al. (16) had some concerns regarding the “bias in the selection of the reported result” domain, as the trial was not registered on an official registry prior to initiation, despite obtaining ethical approval. However, the study was otherwise assessed as having a low risk of bias (16).
FIGURE 5
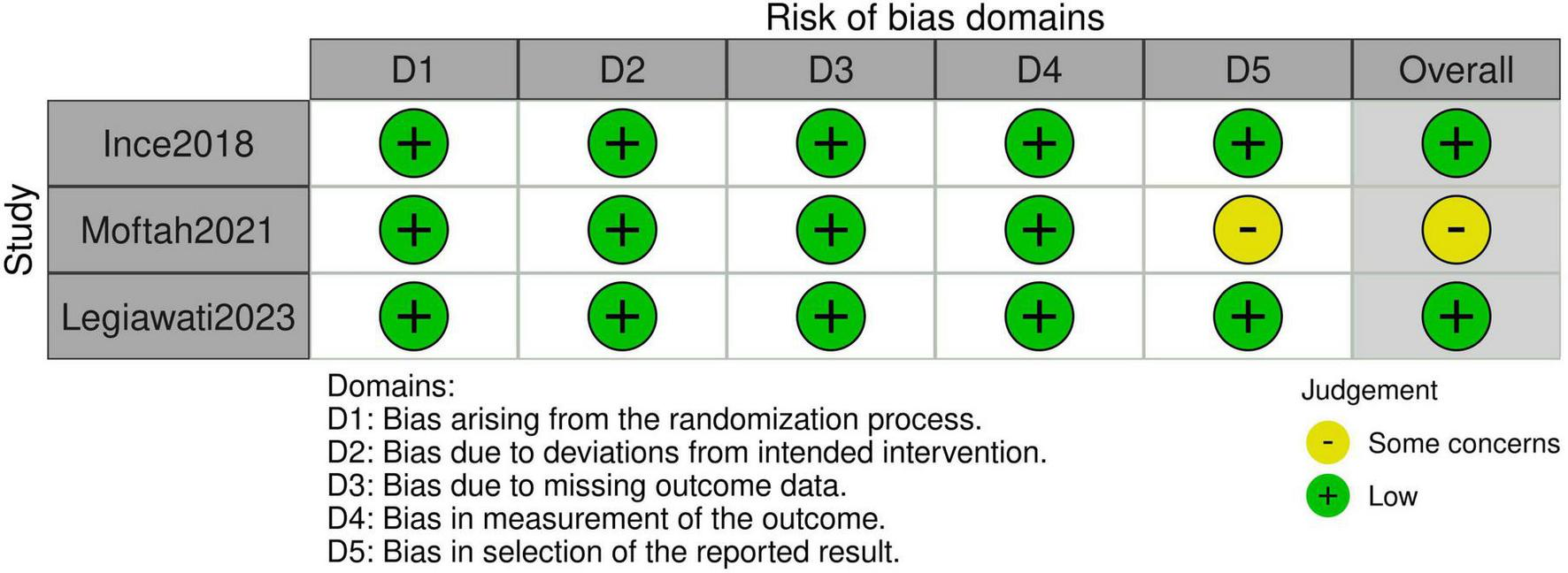
Risk of bias assessment per RoB 2.
4 Discussion
In this meta-analysis of three studies, we compared single-spin to double-spin PRP centrifugation methods in patients with AGA. Key findings include: (i) higher platelets count with single-spin PRP; (ii) higher hair density improvement in the single-spin group; (iii) slightly higher terminal hair count with one-spin centrifugation; and (iv) a lower vellus hair count with single-spin PRP. Our findings favor single-spin PRP over double-spin PRP showing a consistent trend of increased hair density, terminal hair growth and reduction in vellus hair, however the results were not statistically significant.
Platelet-rich plasma plays a crucial role in hair restoration by leveraging the regenerative properties of platelets and its rich concentration of GFs and cytokines. These factors include PDGF, VEGF, TGF-β, fibroblast growth factor (FGF), epidermal growth factor (EGF), and insulin-like growth factor 1 (IGF-1). Upon activation, platelets release bioactive proteins that target and bind to receptors on stem cells, triggering intracellular pathways in the hair follicle bulge. This enhances GF activity in dermal papilla cells, prolongs the growth phase, known as the anagen phase, stimulates bulge cell differentiation, and activates the Wingless/Integrated and β-catenin (Wnt/β-catenin) and extracellular signal-regulated kinase/protein kinase B/Akt (ERK/PKB/Akt) signaling pathways, which support follicle development and prevent apoptosis, through B-cell lymphoma 2 (Bcl-2) expression. PRP also enhances anagen-associated angiogenesis, driven by VEGF secreted by keratinocytes and dermal papilla fibroblasts (20, 21).
A within-person RCT, where one half of the scalp received single-spin PRP and the other half received double-spin PRP, demonstrated superior hair regrowth with the double-spin technique, as confirmed by trichoscopic assessment (22). However, we excluded this study from our meta-analysis due to significant methodological concerns highlighted in a systematic review by Leducq et al. (23). Notably, the risk of carry-across effects, where treatment on one site may inadvertently influence adjacent or contralateral areas, posed a major confounding factor. To ensure methodological rigor and data reliability, we included only traditional parallel-group RCTs in our analysis, allowing for independent comparisons of interventions.
The Indian Association of Dermatologists, Venereologists, and Leprologists (IADVL) developed standardized guidelines from 45 studies. The consensus supports the double-spin manual method, recommending centrifugation parameters of 100–300 g for 5–10 min in the first spin and 400–700 g for 10–17 min in the second. However, the review highlights inconsistencies in existing methodologies and the need for standardization to ensure reproducibility and efficacy in PRP treatments (8).
Despite the widely reported effectiveness of PRP therapy for AGA, significant clinical benefits have not been well established in the current literature, highlighting inconsistencies in treatment outcomes. For instance, a study was conducted on 50 patients [38 males with grade II–V (Norwood–Hamilton) and 12 females with grade II–III (Ludwig)], who underwent PRP treatment with a double-spin centrifugation method injected. Evaluation through photography follow-ups and patient satisfaction surveys revealed that 19 patients were unsatisfied and only 8 found the treatment satisfactory (24). Similarly, a trial comparing double-spin PRP to placebo on 26 females with Ludwig II AGA, failed to demonstrate PRP’s efficacy, with therapeutic benefits reported in patient surveys but not supported by objective hair count data or the hair mass index (HMI) (25). Additionally, a pilot study involving 19 males with AGA grade IV–VI (Norwood classification), used a two-step centrifugation process that increased platelet concentration by threefold. There was no increase in hair count, and conversion of vellus hair to terminal hair was not observed (26).
Notably, these three studies comparing double-spin PRP to placebo showed no benefit, suggesting its inefficacy may stem from centrifugation methodology—especially as our meta-analysis favored single-spin PRP. However, given the lack of statistical significance, further studies directly comparing both methods are needed. Establishing a standardized PRP protocol is crucial to optimizing outcomes and ensuring patient-centered care.
The activation state of PRP, whether in its natural or activated form, significantly influences its therapeutic efficacy. Activated PRP (A-PRP), induced by thrombin or calcium chloride, provides a controlled and sustained release of GFs, optimizing regenerative outcomes. By contrast, exogenously activated PRP (AA-PRP) results in a rapid but short-lived release, potentially limiting long-term effectiveness. This study further emphasized the superior outcomes of A-PRP in improving hair density and follicular activity, mediated by pathways such as Bcl-2, Akt signaling, and FGF-7 activation (27). Future trials comparing single-spin and double-spin PRP should prioritize A-PRP to standardize protocols, as it has demonstrated superior efficacy. This approach will help refine treatment guidelines and optimize clinical outcomes.
Platelet-rich plasma therapy has demonstrated efficacy not only in AGA but also in challenging hair conditions such as cicatricial centrifugal alopecia, including central centrifugal cicatricial alopecia (CCCA), and chronic telogen effluvium (CTE). Case studies on CCCA revealed temporary improvements in follicular density during monthly PRP sessions. However, sustained efficacy remains uncertain, underscoring the need for shorter maintenance intervals (28). In cases of CTE, PRP therapy improved hair density, thickness, and trichoscopy findings, regardless of the type of PRP tube used. Notably, no significant differences were observed between single-spin and double-spin methods (29). Given these findings, further RCTs are essential to compare single-spin versus double-spin PRP centrifugation techniques. Establishing optimal protocols for PRP regimens across these populations would further enhance clinical outcomes.
Combining PRP therapy with standard alopecia treatments – such as minoxidil, oral medications, microneedling, and non-cross-linked hyaluronic acid – has demonstrated synergistic effects on hair regrowth and scalp health. Studies indicate that PRP enhances follicular stimulation, while microneedling improves drug absorption, and hyaluronic acid provides hydration, collectively increasing hair density and thickness (30, 31). These findings underscore that PRP not only enhances the effectiveness of traditional treatments but also offers a safe, minimally invasive solution with minimal side effects. However, the development of a standardized protocol remains critical to optimize these results and ensure consistent therapeutic outcomes for patients. Therefore, we recommend further trials comparing combined PRP with standard treatments, considering centrifugation protocols to optimize patient outcomes.
This study has several limitations. Firstly, the sample size was relatively small, resulting in statistically non-significant findings, thereby affecting the power and robustness of our conclusions. Web of Science and Scopus were not included in the search, which could represent a minor limitation in study inclusion. Additionally, only three studies met our inclusion criteria, with a single common outcome reported across all three RCTs. Forest plots were generated using data from only two studies due to the limited availability of outcomes. Moreover, variability in centrifugation speed and duration, PRP regimen, and follow-up periods across studies may have introduced confounding factors. However, we sought to mitigate this by including only RCTs, ensuring that both comparison groups within each study received the same PRP regimen and were followed up for the same duration; and we excluded within-person RCTs to enhance comparability. Another limitation is the absence of reported measures of dispersion for platelet count outcomes in the study by Ince et al. (14). To address this, we imputed the standard deviation using data from Legiawati et al., following Cochrane’s guidelines (15, 32). Furthermore, we did not evaluate other important factors such as PRP activation methods or the combination of PRP with other treatment modalities, which are increasingly used in clinical practice. These aspects were beyond the scope of the current review and should be addressed in future research.
5 Conclusion
In conclusion, this systematic review and meta-analysis based on available evidence suggest that the single-spin centrifugation method for PRP has better outcomes than double-spin PRP increasing hair density, terminal hair, and platelets while decreasing thin unpigmented hair, known as vellus hair.
Statements
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LG: Writing – review and editing, Investigation, Software, Formal Analysis, Methodology, Data curation, Visualization, Project administration, Conceptualization. NK: Formal Analysis, Writing – original draft, Methodology, Data curation, Investigation. MP-O: Writing – original draft, Investigation. MC-C: Writing – original draft, Investigation, Formal Analysis. DM-M: Writing – original draft, Investigation. GA: Formal Analysis, Writing – original draft. VV-T: Formal Analysis, Validation, Supervision, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1631087/full#supplementary-material
Abbreviations
A-PRP, activated PRP; AA-PRP, exogenously activated PRP; AGA, androgenic alopecia; Bcl-2, B-cell lymphoma 2; CCCA, central centrifugal cicatricial alopecia; CI, confidence interval; CTE, chronic telogen effluvium; DHT, dihydrotestosterone; EGF, epidermal growth factor; ERK/PKB/Akt, extracellular signal-regulated kinase/protein kinase B/Akt; FGF, fibroblast growth factor; GF, growth factor; HMI, hair mass index; IADVL, Indian Association of Dermatologists, Venereologists, and Leprologists; IGF-1, insulin-like growth factor 1; IV, inverse variance; MD, mean difference; PDGF, platelet-derived growth factor; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PRP, platelet-rich plasma; RCT, randomized controlled trial; SD, standard deviation; TGF-β, transforming growth factor beta; VEGF, vascular endothelial growth factor; Wnt, Wingless/Integrated.
References
1.
Bazmi S Sepehrinia M Pourmontaseri H Bazyar H Vahid F Farjam M et al Androgenic alopecia is associated with higher dietary inflammatory index and lower antioxidant index scores. Front Nutr. (2024) 11:1433962. 10.3389/fnut.2024.1433962
2.
Dohan Ehrenfest D Rasmusson L Albrektsson T . Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF).Trends Biotechnol. (2009) 27:158–67. 10.1016/j.tibtech.2008.11.009
3.
Li Z Choi H Choi D Sohn K Im M Seo Y et al Autologous platelet-rich plasma: A potential therapeutic tool for promoting hair growth. Dermatol Surg. (2012) 38:1040–6. 10.1111/j.1524-4725.2012.02394.x
4.
Kieling L Konzen A Zanella R Valente D . Is autologous platelet-rich plasma capable of increasing hair density in patients with androgenic alopecia? A systematic review and meta-analysis of randomized clinical trials.An Bras Dermatol. (2024) 99:847–62. 10.1016/j.abd.2024.01.002
5.
Rodriguez M Mayrovitz H . The history and current status of platelet-rich plasma therapy in dermatology.Cureus. (2024) 16:e68306. 10.7759/cureus.68306
6.
Tanaka Y Aso T Ono J Hosoi R Kaneko T . Androgenetic alopecia treatment in Asian Men.J Clin Aesthet Dermatol. (2018) 11:32–5.
7.
Yin W Xu H Sheng J Zhu Z Jin D Hsu P et al Optimization of pure platelet-rich plasma preparation: A comparative study of pure platelet-rich plasma obtained using different centrifugal conditions in a single-donor model. Exp Ther Med. (2017) 14:2060–70. 10.3892/etm.2017.4726
8.
Dashore S Chouhan K Nanda S Sharma A . Preparation of platelet-rich plasma: National IADVL PRP Taskforce Recommendations.Indian Dermatol Online J. (2021) 12:S12–23. 10.4103/idoj.idoj_269_21
9.
Gupta P Jamra A Prakash S Gupta S Bharti A . Evaluating the efficacy of platelet-rich plasma in treating primary knee osteoarthritis: A prospective interventional study.Cureus. (2024) 16:e71415. 10.7759/cureus.71415
10.
Shrivastava S Patel S Pundkar A Jaiswal A Shrivastava P . Decoding the decade: Exploring the Efficacy of Platelet-Rich Plasma (PRP) in complex wound management - a comprehensive study.Indian J Orthop. (2024) 58:1043–52. 10.1007/s43465-024-01212-5
11.
Dubey D Raghuwanshi B . The efficacy of local autologous platelet-rich plasma prepared by single and double spin methods in the treatment of chronic ulcer.Cureus. (2024) 16:e61366. 10.7759/cureus.61366
12.
Rahman E Rao P Abu-Farsakh H Thonse C Ali I Upton A et al Systematic review of platelet-rich plasma in medical and surgical specialties: Quality, evaluation, evidence, and enforcement. J Clin Med. (2024) 13:4571. 10.3390/jcm13154571
13.
Moher D Liberati A Tetzlaff J Altman D Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. (2009) 339:b2535. 10.1136/bmj.b2535
14.
Ince B Yildirim M Dadaci M Avunduk M Savaci N . Comparison of the efficacy of homologous and autologous platelet-rich plasma (PRP) for treating androgenic alopecia.Aesthetic Plast Surg. (2018) 42:297–303. 10.1007/s00266-017-1004-y
15.
Legiawati L Yusharyahya S Bernadette I Novianto E Priyanto M Gliselda K et al Comparing Single-spin Versus Double-spin Platelet-rich Plasma (PRP) centrifugation methods on thrombocyte count and clinical improvement of androgenetic alopecia: A preliminary, randomized, double-blind clinical trial. J Clin Aesthet Dermatol. (2023) 16:39–44.
16.
Moftah N Taha N Alhabibi A Hamdino M . Different platelet-rich plasma preparation protocols in Female pattern hair loss: Does it affect the outcome? A pilot study.J Cosmet Dermatol. (2022) 21:3316–26. 10.1111/jocd.14648
17.
Cochrane. Chapter 10: Analysing Data and Undertaking Meta-Analyses. (2025). Available online at: https://training.cochrane.org/handbook/current/chapter-10 (accessed May 13, 2025).
18.
Cochrane. Performing Meta-Analyses in the Case of Very Few Studies | Cochrane Training. (2025). Available online at: https://training.cochrane.org/resource/performing-meta-analyses-very-few-studies (accessed February 6, 2025).
19.
Sterne J Savović J Page M Elbers R Blencowe N Boutron I et al RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. 10.1136/bmj.l4898
20.
Alexander S Horo I Johnson S Daniel S . Platelet-rich plasma in hair loss-Mechanism, preparation, and classification.J Cosmet Dermatol. (2022) 21:970–8. 10.1111/jocd.14662
21.
Almohanna H Ahmed A Griggs J Tosti A . Platelet-rich plasma in the treatment of alopecia areata: A review.J Investig Dermatol Symp Proc. (2020) 20:45–9. 10.1016/j.jisp.2020.05.002
22.
El-Husseiny R Saleh H Moustafa A Salem S . Comparison between single- versus double-spin prepared platelet-rich plasma injection in treatment of female pattern hair loss: Clinical effect and relation to vascular endothelial growth factor.Arch Dermatol Res. (2021) 313:557–66. 10.1007/s00403-020-02134-6
23.
Leducq S Dugard A Allemang-Trivalle A Giraudeau B Maruani A . Design and methodological issues of within-person (split-body) randomized controlled trials evaluating a topical treatment: A systematic review.Dermatology. (2023) 239:720–31. 10.1159/000530149
24.
Agarwal P Gajjar K Jagati A Chaudhari S Rathod S . Platelet-rich plasma in androgenetic alopecia: Is it really worth the hype?Int J Trichol. (2023) 15:98–104. 10.4103/ijt.ijt_31_21
25.
Puig C Reese R Peters M . Double-blind, placebo-controlled pilot study on the use of platelet-rich plasma in women with female androgenetic alopecia.Dermatol Surg. (2016) 42:1243–7. 10.1097/DSS.0000000000000883
26.
Mapar M Shahriari S Haghighizadeh M . Efficacy of platelet-rich plasma in the treatment of androgenetic (male-patterned) alopecia: A pilot randomized controlled trial.J Cosmetic Laser Therapy. (2016) 18:452–5. 10.1111/srt.13315
27.
Gentile P Cole J Cole M Garcovich S Bielli A Scioli M et al Evaluation of not-activated and activated PRP in hair loss treatment: Role of growth factor and cytokine concentrations obtained by different collection systems. Int J Mol Sci. (2017) 18:408. 10.3390/ijms18020408
28.
Larrondo J Petela J McMichael A . Transitory hair growth using platelet-rich plasma therapy in stabilized central centrifugal cicatricial alopecia.Dermatol Ther. (2022) 35:e15798. 10.1111/dth.15798
29.
El-Dawla R Abdelhaleem M Abdelhamed A . Evaluation of the safety and efficacy of platelet-rich plasma in the treatment of female patients with chronic telogen effluvium: A randomised, controlled, double-blind, pilot clinical trial.Indian J Dermatol Venereol Leprol. (2023) 89:195–203. 10.25259/IJDVL_1011_20
30.
Wei W Zhang Y Long B Zhang Y Zhang C Zhang S . Injections of platelet-rich plasma prepared by automatic blood cell separator combined with topical 5% minoxidil in the treatment of male androgenetic alopecia.Skin Res Technol. (2023) 29:e13315. 10.1111/srt.13315
31.
Wang S Li D Zou M Wu J Wang X Yang Y et al Efficacy of autologous platelet-rich plasma combined with a non-cross-linked hyaluronic acid compound in the treatment of female androgenetic alopecia: A retrospective, case-series study. J Cosmet Dermatol. (2023) 22:3268–75. 10.1111/jocd.15861
32.
Cochrane. Chapter 6: Choosing Effect Measures and Computing Estimates of Effect. (2025). Available online at: https://training.cochrane.org/handbook/current/chapter-06 (accessed February 10, 2025).
33.
Dinh Q Sinclair R . Female pattern hair loss: Current treatment concepts.Clin Interv Aging. (2007) 2:189–99.
34.
Henne S Nöthen M Heilmann-Heimbach S . Male-pattern hair loss: Comprehensive identification of the associated genes as a basis for understanding pathophysiology.Med Genet. (2023) 35:3–14. 10.1515/medgen-2023-2003
35.
Norwood O . Male pattern baldness: Classification and incidence.South Med J. (1975) 68:1359–65. 10.1097/00007611-197511000-00009
36.
Wirya C Wu W Wu K . Classification of male-pattern hair loss.Int J Trichol. (2017) 9:95–100. 10.4103/ijt.ijt_46_17
Summary
Keywords
androgenic alopecia, platelet-rich plasma, centrifugation, single-spin, double-spin
Citation
Ghanem L, Kirmani N, Palacios-Ortiz MP, Cevallos-Cueva M, Mendoza-Millán DL, Almeida Nascimento GV and Velasco-Tamariz V (2025) Comparison of single-spin to double-spin platelet-rich plasma centrifugation methods in the treatment of androgenic alopecia: a systematic review and meta-analysis of randomized controlled trials. Front. Med. 12:1631087. doi: 10.3389/fmed.2025.1631087
Received
19 May 2025
Accepted
30 June 2025
Published
21 July 2025
Volume
12 - 2025
Edited by
Alba Gomez Zubiaur, Ricart Medical Institute, Spain
Reviewed by
Feza Korkusuz, Hacettepe University, Türkiye
Ana Rodríguez-Villa Lario, Prince of Asturias University Hospital, Spain
Manuel Ballesteros Redondo, University of Valencia, Spain
Updates
Copyright
© 2025 Ghanem, Kirmani, Palacios-Ortiz, Cevallos-Cueva, Mendoza-Millán, Almeida Nascimento and Velasco-Tamariz.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Virginia Velasco-Tamariz, virginia.velasco@salud.madrid.org
†ORCID: Laura Ghanem, orcid.org/0009-0009-7918-0107; Najwaa Kirmani, orcid.org/0009-0006-4936-7008; María Paula Palacios-Ortiz, orcid.org/0009-0002-3589-4318; Martin Cevallos-Cueva, orcid.org/0000-0002-6737-9305; Daniela Lucía Mendoza-Millán, orcid.org/0000-0003-1481-5166; Gabriel Victor Almeida Nascimento, orcid.org/0009-0003-4611-963X; Virginia Velasco-Tamariz, orcid.org/0000-0003-4009-0525
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.