Abstract
Background:
Preoperative anxiety is common. To date, no randomized controlled trial has examined the effectiveness of reflexology in reducing preoperative anxiety in patients undergoing elective laparoscopic cholecystectomy.
Methods:
A randomized, single blinded, interventional trial was conducted with 300 patients undergoing elective laparoscopic cholecystectomy, comparing the following three groups: controls receiving standard-of-care (SoC) only (group 1); intervention group receiving reflexology and SoC (group 2); and a group receiving sham reflexology and SoC (group 3). The primary outcome was the mean difference between the three groups in visual analog scale for anxiety (VAS-A). The secondary outcome was a similar analysis confined to patients experiencing baseline moderate-to-high anxiety. In all groups, level of preoperative anxiety was evaluated at entry and exit from the holding room area (HRA). The evaluation was carried out using the VAS-A questionnaire. The study was registered at clinicaltrials.gov (NCT01733771).
Results:
101 patients were randomly assigned to the reflexology group, 99 to the sham reflexology arm, and 100 received SoC alone. In all groups, SoC included anxiolytics in 25% of patients received about 2 h before the operation. Baseline anxiety (at entry to HRA) was similar in all groups, averaging 5.3. Between-group analysis comparing the reflexology and sham groups detected 0.8 point difference on 0–10 VAS scale in favor of the reflexology group (p = 0.022). Subgroup analysis of patients with moderate to high level of anxiety (VAS-A>4) at baseline (consisting of 75% of study participants), indicated 1.3 points difference (p = 0.023).
Conclusions:
The study findings suggest that reflexology treatments have a small, yet significant advantage over sham reflexology and over standard-of-care in reducing preoperative anxiety, in patients with moderate-to-high levels of anxiety.
Clinical trial registration:
https://clinicaltrials.gov/study/NCT01733771?tab=results, Identifier: NCT01733771.
1 Background
Cholecysectomy due to gallstones is one of the most common operations in general surgery (1). Nowadays, this type of surgery is usually done electively in the laparoscopic method laparoscopic cholecystectomy (LC), in Israel and worldwide (2). In recent years, enhanced recovery after surgery (ERAS), an international association of experts in the fields of surgery, anesthesia, and other allied health professions, has led a process of formulating guidelines, based on research evidence, in order to improve peri-operative care (3). This trend reflects an interventionist approach and a global perspective on the public health level in the context of surgery which, among others, highlights the need to address peri-operative symptoms.
The state of preoperative anxiety may affect the course of surgery usage of anesthetics (4), and the recovery period that follows in different aspects, such as pain (5, 6), wound healing (7), nausea and vomiting (8), duration of hospitalization and recovery (9), immune system status (10). Preoperative anxiety is usually evaluated using the visual analog scale for anxiety (VAS-A) questionnaire, which is based on the patient's own reporting and is a reliable, simple and quick method, particularly when the time available for interaction with the subject is limited, as is the case in the holding room area (HRA), a waiting room in which patients stay for 15–50 min before surgery (11–14).
Between 11 and 80% of adult patients undergoing surgery, report experiencing significant (moderate-to-high) preoperative anxiety (15, 16). A controlled, randomized clinical trial on 360 surgical patients showed that 70% of the subjects experienced moderate-to-high levels of anxiety ~1 h before the surgery, despite being treated with the standard-of-care (SoC), which involves administering anxiolytics prior to the surgery at the discretion of the anesthesiologist (17).
Anxiolytics are often administered before surgery, either orally or by intravenous injection. Several studies have proven the efficacy of using anxiolytics as part of premedication before surgery, including midazolam (18), gabapentin (19), diazepam (20) and oxazepam (21). However, data obtained from several other studies cast doubt on their effectiveness (22, 23). Several studies have demonstrated the effectiveness of different complementary medicine treatments, including reflexology, in reducing preoperative anxiety and anxiety before other medical procedures (17, 24, 25).
Reflexology is a touch treatment method which is based on the theory that the entire body is represented in reflex points located on the soles of the feet (or the palms of the hands). A number of studies have examined the impact of reflexology treatments on indices of stress, anxiety and relaxation (17, 26, 27).
A handful of studies compared reflexology treatments with sham reflexology treatments (general foot massage without applying direct pressure to formal reflex points), to counteract the expected placebo effect (28, 29). Such studies are important in order to isolate the treatment's placebo effect and highlight the specific effect, if any, of real reflexology.
Since elective LC is a very common operation, and due to the significance of preoperative anxiety in the context of potential post-operative complications and morbidity, we have examined the effect of reflexology as well as sham reflexology in parallel with SoC treatment which currently involves administration of anxiolytics, on this issue.
2 Methods
2.1 Type of study and study population
We conducted a single-blinded clinical intervention randomized controlled trial. Trial methods and results were reported according to the 2010 guidelines for consolidated standards of reporting trials (CONSORT) for non-pharmacologic interventions (30).
The trial involved 300 patients awaiting an elective LC, who agreed to participate in the trial and were randomly allocated into three equal groups. Group 1 received the SoC treatment (anxiolytics) at the discretion of the anesthesiologist (n = 100). Group 2 received reflexology treatment on top of SoC (n = 101), and Group 3 received sham reflexology treatment in addition to SoC (n = 99; see Figure 1). The study was single-blinded because while patients in the study arms that involved reflexology did not know whether they were being treated with real reflexology or sham reflexology, and the treatment was described to them as medicinal foot massage rather than reflexology, the therapists, however, did know whether they were giving real or sham reflexology treatment.
Figure 1
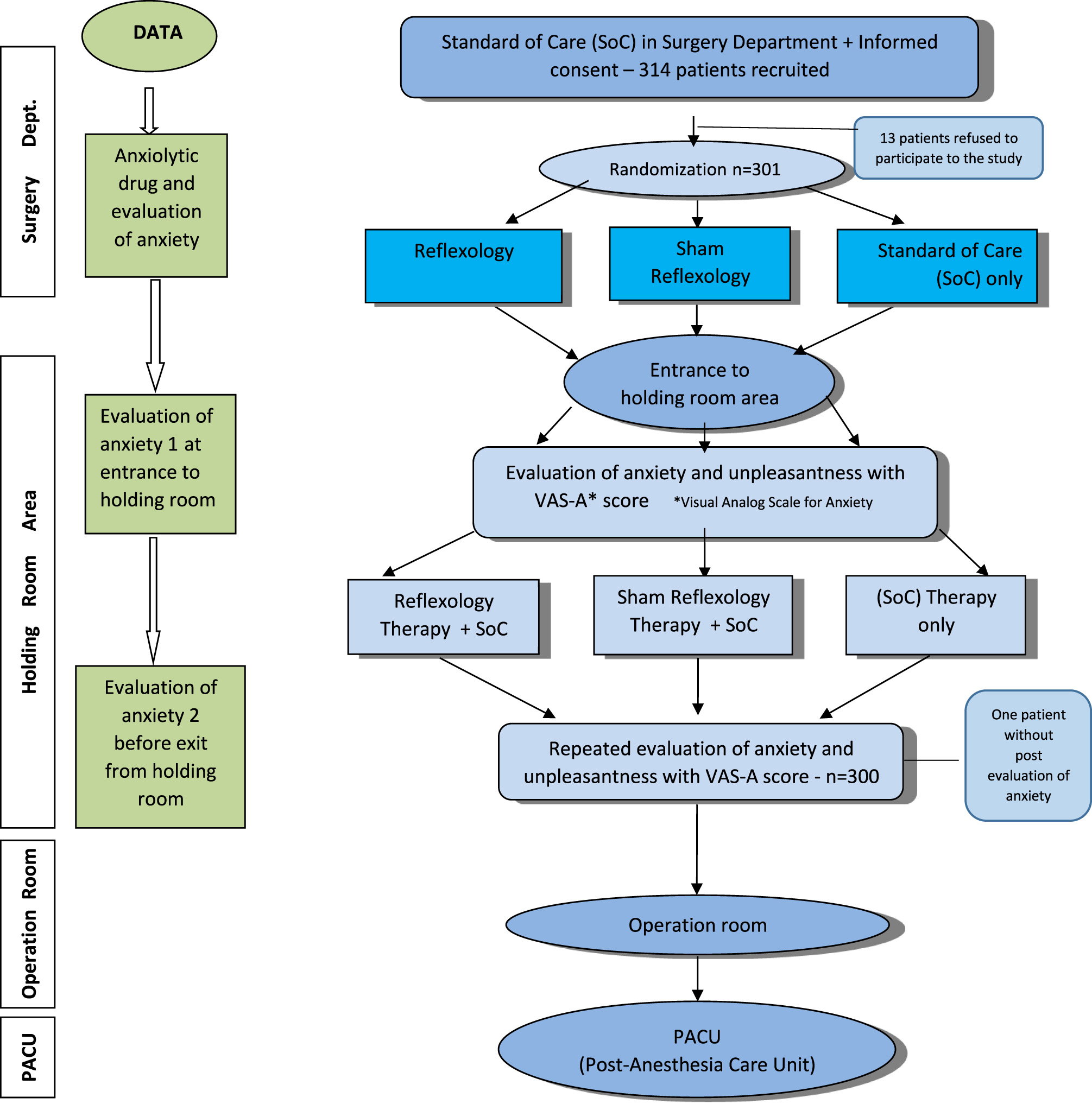
Study procedure.
Inclusion criteria: (1) patients aged 18 years undergoing LC who consented to the study. Exclusion criteria: (1) patients with a history of obstructive sleep apnea; (2) contraindication for benzodiazepines; (3) hemodynamic instability; (4) patients with feet ulcers; (5) patients undergoing a LC together with another surgical procedure.
2.2 Study objective
The primary study objective was to examine the effectiveness of a combined treatment of reflexology on top of SoC in comparison to a combined treatment of sham reflexology on top of SoC and in comparison to SoC treatment alone in reducing preoperative anxiety in elective LC.
2.3 Sampling method and study procedure
The study was conducted at the Bnai Zion Medical Center in Haifa. Participants were recruited between July 2016 and October 2019.
Patients that agreed to be included in the study were randomly assigned to one of the three study groups using a designated software (randomization.com; see Figure 1). Patients were asked to rate their level of anxiety and their level of comfort using the visual analog scale (VAS) and visual analog scale for anxiety (VAS-A) questionnaire at the surgery department and in the HRA. Subsequently, patients were told whether they had been assigned to the intervention group involving foot massage—without specifying whether it would be real or sham reflexology—or to the control arm.
2.4 Therapeutic approach protocol
The study included three treatment groups:
A. SoC (group 1) included premedication about 2 h before the operation with the anxiolytics oxazepam and diazepam, according to the anesthesiology department protocol and at the discretion of the anesthesiologist, regardless of the study arm. It should be clarified that in some cases the anesthesiologist decided not to administer anxiolytics, or the patient chose not to receive them. In cases where premedication was administered, the instructions were to administer 10 mg of diazepam to patients under the age of 65, and 10 mg of oxazepam to patients over 65. This protocol is supported by the study conducted by Pomara et al. (23) which found that older patients taking diazepam tend to suffer from side effects of memory and psychomotor performance impairments.
B. Reflexology (group 2) intervention involved a 15-min treatment in the induction room, provided by three reflexologists from the hospital staff. The reflexology protocol was developed through a Delphi method (31). The Delphi expert panel comprised 20 reflexologists with at least 2 years of clinical experience. Using a three-round Delphi process, the first-round open question was developed by four therapists from our Medical Center based on their experience treating preoperative anxiety. Consensus was defined as ≥80% agreement. Topics without consensus were reconsidered in subsequent rounds. Participants were contacted by email, with addresses kept confidential to ensure anonymity and prevent individual dominance (31).
C. Sham reflexology (group 3) intervention was provided by two complementary medicine practitioners with knowledge in touch therapy (shiatsu) and included 15 min of gentle, non-specific foot massage. Similarly to the true reflexology protocol, the protocol for this treatment was also determined in a consensus-reaching process among a group of four experienced reflexologists.
2.5 Assessment tools
The level of anxiety was evaluated both before and after the treatments, using the VAS-A questionnaire for anxiety and the VAS scale for the level of comfort (rated from 0—not comfortable at all, to 10—very comfortable). VAS Comfort questionnaires were used in order to support the assessment of anxiety by VAS-A. The control group was assessed at the same time points. The questionnaire was given to the patient at the surgery department by a study coordinator. At the HRA questionnaires were given by the nursing staff before and after the intervention, shortly before the patient was transferred to the operating room. Baseline assessment was carried out at the entrance to the HRA through a VAS-A valid anxiety questionnaire for current anxiety level from 0—no anxiety, up to 10—maximum anxiety (14). Similar to pain scale, it is common to divide the anxiety symptoms into categories; low anxiety (VAS-A ≤ 4), moderate to severe anxiety (VAS-A ≥ 4), severe anxiety (VAS-A ≥ 7).
2.6 Sample size calculation and statistical analysis
The calculation of the sample size was carried out using GPower software, which examines the sample size with reference to ANOVA variance analysis. The comparison between the three different groups, given a confidence level of 95%, power of 85% and an effect size that is considered medium according to Cohen's 0.25, alongside the definition of one unit of VAS as the low value for clinical significance (32), required a sample size of at least 45 subjects per group for our primary endpoint (mean difference between the three groups in VAS-A). For the secondary endpoint (mean difference between the three groups for patients with VAS above four), and for stratification of age, sex, as well as according to the administration of anxiolytics, ~100 subjects were recruited to each group. Since the result distribution was not normal, a variance test was conducted using Kruskal–Wallis' non-parametric test to compare the average change in preoperative anxiety in the induction room. Due to multiple comparisons (between three groups), the p-value in these tests was 0.014 in order to overcome the false discovery rate (FDR), and p < 0.05 for the purpose of bilateral comparison (33). Of note, both per-protocol and intention-to-treat analyses were planned, but since there was no patient cross-over, there was no need to differentiate between the analyses.
2.7 IRB approval
The study was approved by the local IRB (Helsinki Committee), approval no. BNZ-0041-09 and is also registered at clinicaltrials.gov (NCT01733771).
3 Results
We approached 314 eligible candidates. A total of 300 patients were included in the study. The rate of consent to participate in the study was very high−95.5% (300/314). Thirteen patients (4.1%) refused to participate in the study, and one patient (0.3%) could not undergo an evaluation of his anxiety level after the treatment because he was taken to the operating room before being asked again.
3.1 Patients' characteristics
The characteristics of the patients in the entire study population are presented in Table 1. No statistically significant differences were found between the different groups. All patients were able to receive the anxiolytics oxazepam and diazepam.
Table 1
| Parameter | Total no. of patients | R | SR | SoC | p-Value |
|---|---|---|---|---|---|
| N = 300 | n = 101 | n = 99 | n = 100 | ||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age, years (average ± SD) | 49.8 ± 15.6 | 51.2 ± 14.5 | 49.9 ± 16.9 | 48.5 ± 15.3 | p = 0.46 |
| BMI | 28.4 ± 5.4 | 28.3 ± 5.9 | 28.6 ± 5.3 | 28.3 ± 5.1 | p = 0.93 |
| Sex (female) | 188 (63%) | 60 (59%) | 62 (63%) | 66 (66%) | p = 0.63 |
| Surgery in the past | 187 (64%) | 69 (70%) | 54 (55%) | 64 (67%) | p = 0.07 |
| An inflammatory process that required hospitalization before surgery | 127 (46%) | 49 (50%) | 43 (47%) | 35 (41%) | p = 0.4 |
| Patients who received anxiolytics (diazepam or oxazepam) | 72 (25%) | 23 (23%) | 24 (25%) | 25 (26%) | p = 0.86 |
| Comorbidity | |||||
| Cardiovasculary | 103 (35%) | 37 (37%) | 32 (33%) | 34 (34%) | p = 0.86 |
| Gastroenterology/hepatobiliary | 38 (13%) | 17 (17%) | 10 (10%) | 11 (11%) | p = 0.32 |
| Renal/urology | 23 (8%) | 6 (6%) | 10 (10%) | 7 (7%) | p = 0.65 |
| Metabolic/endocrinology | 152 (51%) | 53 (53%) | 48 (49%) | 51 (51%) | p = 0.92 |
| Hemato-oncology | 8 (18.2%) | 5 (11.4%) | 2 (4.5%) | 2 (4.9%) | p = 0.37 |
| Neurology | 3 (1%) | 3 (3%) | – | – | – |
| Others | 53 (18%) | 15 (15%) | 20 (20%) | 18 (18%) | p = 0.63 |
| Baseline VAS-A in surgery department mean (SD) | 4.2 ± 2.6 | 4.2 ± 2.6 | 4.4 ± 2.6 | 3.9 ± 2.6 | p = 0.33 |
Study population characteristics.
p = 0.014 (between three groups). R, reflexology; RS, sham reflexology; SoC, standard of care.
3.2 Baseline anxiety and comfort levels in the ward and HRA
The VAS-A anxiety evaluation performed in the ward revealed an average anxiety level of 4.2 in the entire sample. Upon entering the HRA ~2–6 h later, an average anxiety level of 5.3 was measured, an increase of 1.1 points in the VAS-A scale. The average VAS comfort level, the complementary index to the VAS-A, was 5.1 upon entering the HRA. As part of the data processing, we focused on the group of patients whose anxiety level was rated as moderate-high when they arrived at the HRA, prior to the intervention (a VAS-A score higher than 4). This group included a total of 221 patients (74%). Among these patients, the average level of anxiety upon entering the HRA and before the intervention was 6.5 (Table 2).
Table 2
| VAS comfort and VAS-anxiety baseline in holding room area | N | Mean (SD) | p-Value between 3 groups |
|---|---|---|---|
| VAS comfort (0–10) | 300 | 5.1 (2.2) | p = 0.71 |
| R | 101 | 5.2 (2.3) | |
| SR | 99 | 5.1 (2.2) | |
| SoC | 100 | 5.1 (2.2) | |
| VAS-A (0–10) | 300 | 5.3 (2.7) | p = 0.47 |
| R | 101 | 5.1 (3.2) | |
| SR | 99 | 5.5 (2.4) | |
| SoC | 100 | 5.1 (2.7) | |
| VAS-A ≥4 moderate to severe anxiety | 212 | 6.47 (1.9) | p = 0.19 |
| R | 61 | 6.8 (1.9) | |
| SR | 83 | 6.2 (1.8) | |
| SoC | 68 | 6.5 (1.9) | |
| VAS-A ≥7 severe anxiety | 73 | 8.93 (1.0) | p = 0.61 |
| R | 25 | 9.08 (0.9) | |
| SR | 23 | 8.85 (1.0) | |
| SoC | 25 | 8.84 (1.0) | |
| VAS-A < 4 low anxiety | 78 | 1.71 (0.97) | p = 0.57 |
| R | 33 | 1.57 (0.94) | |
| SR | 16 | 1.88 (1.08) | |
| SoC | 29 | 1.76 (0.95) |
Baseline outcomes evaluation in holding room area per groups and per categories of VAS-A and VAS comfort.
R, reflexology; SR, sham reflexology; SoC, standard of care. p = 0.014 (between three groups).
With regard to the correlation between the VAS-A anxiety score and the VAS comfort score measured in the “Before” evaluation at the HRA in the entire study population, the Pearson coefficient shows a strong negative correlation between anxiety and comfort: the higher the levels of anxiety, the lower the levels of comfort. The strength of the correlation is r = −0.714, p < 0.0001.
3.3 Pre-and post-intervention anxiety assessment
Table 3 shows the change in the average level of anxiety “Before” and “After” the intervention in the HRA, for each type of treatment. With the complementary medicine treatments, the average differences in anxiety level are negative, meaning that a [statistically significant] decrease was observed in the level of anxiety between the evaluation “Before” and the evaluation “After” the intervention. With the SoC alone, the difference is positive, indicating that a certain increase in anxiety was observed in the second evaluation.
Table 3
| Mean difference VAS-A | N | Mean difference (SD) | Median | p-Value between three group | p-Value between two group | 95% CI |
|---|---|---|---|---|---|---|
| VAS-A all anxiety levels | ||||||
| R | 101 | −2.83 (2.12) | 2.25 | p < 0.0001 | SoC vs. SR p < 0.0001 | [(−3.25)–(−2.41)] |
| SR | 99 | −1.99 (1.85) | 2.00 | SoC vs. R p < 0.0001 | [(−2.36)–(−1.62)] | |
| SoC | 100 | 0.24 (1.06) | 0.00 | SR vs. R p = 0.021 | (0.03–0.46) | |
| VAS-A ≥4 moderate to severe anxiety | ||||||
| R | 66 | −3.58 (2.14) | 3.00 | p < 0.0001 | SoC vs. SR p < 0.0001 | [(−4.11)–(−3.06)] |
| SR | 81 | −2.16 (1.93) | 2.00 | SoC vs. R p < 0.0001 | [(−2.58)–(−1.73)] | |
| SoC | 70 | 0.20 (1.3) | 0.00 | SR vs. R p = 0.022 | [(−0.07)–(0.47)] | |
| VAS-A ≥7 severe anxiety | ||||||
| R | 25 | −4.84 (2.49) | 5.00 | p < 0.0001 | SoC vs. SR p < 0.0001 | [(−5.87)–(−3.81)] |
| SR | 22 | −3.27 (2.02) | 3.50 | SoC vs. R p < 0.0001 | [(−2.38)–(−4.17)] | |
| SoC | 25 | 0.20 (0.70) | 0.00 | SR vs. R p = 0.35 | [(−0.09)–(0.49)] | |
| VAS-A<4 low anxiety | ||||||
| R | 32 | −1.28 (0.86) | 1 | p < 0.0001 | SoC vs. SR p < 0.0001 | [(−1.59)–(−0.97)] |
| SR | 16 | −1.12 (1.14) | 1 | SoC vs. R p < 0.0001 | [(−1.73)–(−0.51)] | |
| SoC | 29 | 0.34 (0.89) | 0.00 | SR vs. R p = 1.00 | (0.004–0.68) | |
Mean difference anxiety in holding room area by groups and by level of initial anxiety level.
R, reflexology; SR, sham reflexology; SoC, standard of care. p = 0.014 (between three groups). p < 0.05 (between two group).
Bilateral comparisons show a statistically significant difference in the reduction of anxiety levels after intervention between the reflexology and sham reflexology treatments (0.8) p = 0.022, a finding that is significant but has no clinical significance. A statistically significant difference was also observed in the comparisons between the SoC group and the sham reflexology group (2.2) and between SoC and reflexology groups, p < 0.0001, with clinical significance. Figure 2 describes each of the treatments using a box-plot and the Kruskal–Wallis test.
Figure 2
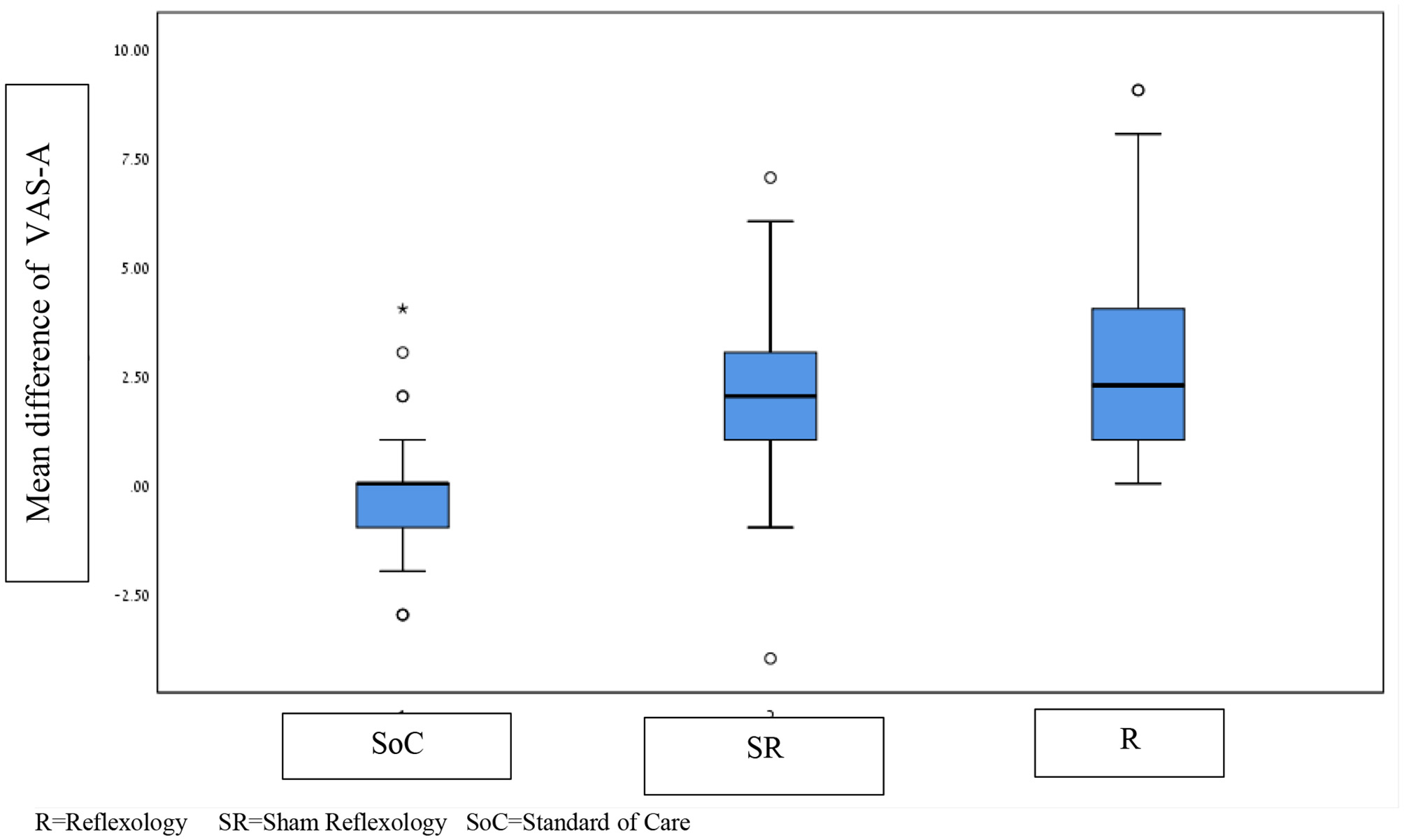
Differences in the average anxiety scores in the holding room area in the three groups. R, reflexology; SR, sham reflexology; SoC, standard of care. *Meaning that several patients had changes in VAS-A far outside the main distribution.
3.4 The change in average anxiety level in the HRA among patients with initial moderate-to-high anxiety level VAS-A ≥4
Once again, we conducted a Kruskal–Wallis test between the study groups for participants with VAS-A ≥4, while looking at the difference in anxiety levels between “Before” and “After” the intervention as an outcome. A statistically significant difference emerged between reflexology and sham reflexology (1.3) p = 0.022, with a clinical significance defined as minimal to small. Moreover, a significant difference was found between the SoC group and the sham reflexology group, and between SoC and reflexology groups, p < 0.001 (see Table 3 and Figure 3).
Figure 3
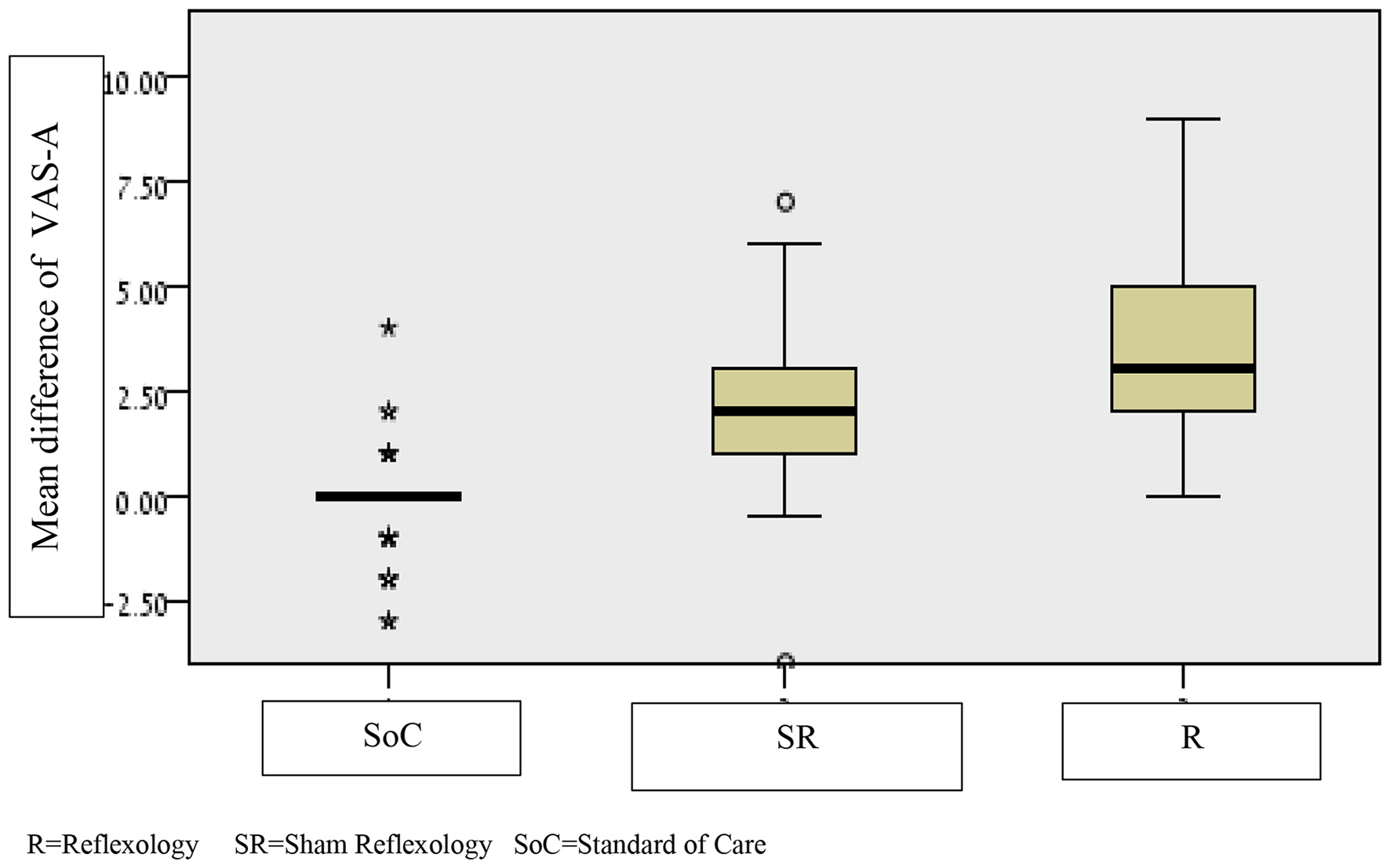
Differences in average anxiety scores before and after the holding room area intervention in the three groups, restricted to patients with moderate-high anxiety VAS-A ≥4. R, reflexology; SR, sham reflexology; SoC, standard of care. *Meaning that several patients had changes in VAS-A far outside the main distribution.
3.5 Data analysis of the study population stratified by use of anxiolytics
Twenty-five percent of the study population received anxiolytics about 2 h before the operation. No significant differences were found between the different study arms with regard to the administration of anxiolytics (see Table 1). Analysis of the effect of anxiolytics will be published in a separate article.
3.6 Safety issues
No abnormal reactions to the reflexology or sham reflexology were reported during or immediately after the treatments. In four cases, mild involuntary reactions of foot twitches were observed during the reflexology treatment.
4 Discussion
The aim of this study was to examine the effect of reflexology as well as sham reflexology in parallel with SoC treatment on pre-operative anxiety in patients undergoing elective laparoscopic cholecystectomy. The study findings indicate that reflexology treatments have a clinically modest advantage over sham reflexology in reducing preoperative anxiety in patients with a moderate-to-high baseline level of anxiety (VAS-A ≥4), and that both interventions have a considerable advantage over the standard of care, regardless of anxiolytics administration.
To the best of our knowledge, this study is the first to evaluate anxiety levels among cholecystectomy patients pre- and post-reflexology intervention immediately before entering the operating room thus, it reliably indicates anxiety levels directly before the operation, following administration of SoC.
4.1 The findings in light of previous studies
In the present study, the initial average anxiety levels measured in the HRA using the VAS-A scale before entering the operating room and before the intervention were clinically significant (5.3), were validated by the complementary VAS-Comfort scale and were similar to the average measured in studies conducted by Perks (34) and Mackenzie (35). The average level of anxiety measured in the present study is also similar to the results of a study conducted using a similar outline, which evaluated the level of anxiety in the HRA—showing an average VAS-A score of 5.5 in 360 patients undergoing different types of operations (17). The breakdown of anxiety severity was also similar to previous studies, with 70% of the study population exhibiting initial moderate-to-high anxiety levels (VAS-A score of 4–10), which require special attention from the medical staff due to the risk of peri-operative complications.
The clinical benefit observed with reflexology, as compared to sham reflexology and SoC, is a finding unique to our study. An extensive literature review has shown that most of the studies that examined the efficacy of non-pharmacological treatments for preoperative anxiety did not include a sham intervention arm (17, 35, 36). Out of three studies that did include a sham reflexology arm, all with relatively small sample sizes (15–73), only one (29) reported that real reflexology had a relative advantage over sham reflexology (28, 37).
4.2 Timing the treatment of preoperative anxiety
Our findings show an average increase of one VAS-A unit from the moment the elective-surgery patients are admitted to the surgery department until they are taken to the HRA, where the level of anxiety reaches its peak. Therefore, it appears appropriate to treat preoperative anxiety from the moment patients are informed of the surgical intervention at the preoperative clinic. At this stage, surgeons play a crucial role in the way they explain the procedure, including its benefits and potential risks (38). Approximately 2 weeks before surgery, patients typically attend a preoperative clinic, where it is appropriate to consider pharmacological, psychological, and/or complementary interventions, particularly for those with high anxiety. Finally, during hospitalization prior to surgery, proactive interventions are recommended both in the department and in the HRA. Future studies should evaluate the optimal timing and modalities for such interventions.
4.3 Reflexology and sham reflexology
The study demonstrated a clear therapeutic advantage of both true and sham reflexology over the standard of care in reducing preoperative anxiety. Reflexology also showed a relatively small but significant advantage over sham reflexology in patients with moderate-to-high baseline anxiety. These findings highlight the potential benefits associated with touch-based treatments. They also indicate that the Delphi process, used to standardize this intervention, was appropriate. This further justifies its use in the absence of formal practice guidelines. It is important to note that, although statistically significant, the advantage of true reflexology over sham reflexology is clinically modest on the VAS scale. Nevertheless, the large sample size supports the robustness of this finding. Future studies should aim to identify patient subgroups that may derive greater benefit from true reflexology. In addition, foot massage is defined as a non-specific massage of the feet; however, reflex points used in reflexology may sometimes be stimulated unintentionally. In contrast, the sham reflexology protocol in our study was carefully designed to avoid applying pressure to reflex points associated with relaxation. We reviewed the literature to evaluate the impact of foot massage, which may resemble our sham protocol, and found no studies assessing its efficacy for preoperative anxiety. The few studies that examined the effect of foot massage on preoperative anxiety involved complex interventions, such as patient education, preventing isolation of the effect of foot massage (39).
4.4 Study limitations and strengths
This study has some limitations that need to be considered. First, it was performed in one medical center. However, the department in which the study was carried out performs a considerable number of LC in the northern part of Israel. In addition, the therapists participating in our study knew that they were giving a sham treatment. Although not assessed in this study, this could have had an unconscious effect on the therapist and on his/her confidence in the treatment, and the patients might have sensed it. Furthermore, although anxiety is a multifaceted experience, we only used the VAS-A tool for its assessment in our study, since it is applicable and practical in the setting we explored. Future studies should incorporate questionnaires, which assess complex elements of the anxiety experience. Objective data related to physiological expressions of anxiety, such as heart rate variability, blood cortisol levels, and other indicators, would have supported our findings. However, we included in the questionnaire an aspect of the patient's comfort in order to assess the reliability of the reported level of anxiety and the correlation between the two variable was high.
Having said that, the study has some significant strengths that should be mentioned. It had a controlled, randomized design, which reduces the potential for selection and information biases and for confounding. Importantly, we have included a study arm focusing on sham reflexology, which neutralized the non-specific placebo effect of the real treatment that has been investigated. In addition, the department in which the study was carried out has a patient population characterized by socio-demographic diversity, which increases the generalizability of our findings. Furthermore, the high response rate (over 95%) significantly reduces the potential for a volunteer bias.
5 Conclusion
Our randomized controlled study indicates that reflexology in combination with standard of care reduces preoperative anxiety in patients undergoing elective LC. The modest relative advantage of reflexology over sham reflexology was particularly evident in patients experiencing moderate-to-high baseline levels of anxiety (VAS-A≥4). Future studies should evaluate point specificity, best timing and manipulation, as well as mechanism of action in order to identify the specific effects of reflexology.
In addition, we have found out that both reflexology (+SoC) and sham reflexology (+SoC) were superior to SoC alone in reducing pre-operative anxiety, suggesting that guidelines regarding the current SoC protocols may need rethinking.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by IRB (Helsinki Committee), approval no. BNZ-0041-09. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AS: Validation, Formal analysis, Conceptualization, Project administration, Methodology, Writing – review & editing, Data curation, Supervision, Investigation, Writing – original draft, Software, Visualization. K-BL: Writing – review & editing, Formal analysis, Methodology, Software, Investigation, Supervision, Conceptualization, Writing – original draft, Validation. SM: Writing – review & editing, Supervision, Validation, Writing – original draft, Methodology, Software, Visualization. SA: Writing – review & editing, Methodology, Software. GY: Writing – review & editing, Methodology, Project administration, Validation. B-AE: Supervision, Validation, Writing – review & editing, Formal analysis, Visualization. MI: Writing – review & editing, Supervision, Visualization, Validation. SG: Conceptualization, Supervision, Methodology, Validation, Writing – review & editing. GS: Investigation, Visualization, Validation, Supervision, Writing – review & editing. SD: Methodology, Visualization, Writing – review & editing, Validation. SE: Validation, Resources, Conceptualization, Formal analysis, Writing – original draft, Visualization, Investigation, Supervision, Data curation, Writing – review & editing, Methodology, Software.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to Ronit Leiba for the statistical processing and to Ilana Merhav and Tanya Kligerman, librarians at the Bnai-Zion Medical Center, for their assistance in the literature search. We also would like to thank Avi Aviel and Myriam Rosenblum for volunteering for the research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Sanders G Kingsnorth AN . Gallstones. BMJ. (2007) 335:295–9. 10.1136/bmj.39267.452257.AD
2.
Greenberger NJ Paumgartner G . Chapter 311. Diseases of the Gallbladder and Bile Ducts.New York, NY: McGraw-Hill Education (2012).
3.
ERAS Society . ERAS Guidelines for Perioperative Care in Elective Surgery (2023). Available online at: https://erassociety.org/guidelines
4.
Maranets I Kain ZK . Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg. (1999) 89:1346–51. 10.1097/00000539-199912000-00003
5.
Zeev ZN Sevarinoa F Alexandera GM Pincusa S Mayes LC . Preoperative anxiety and postoperative pain in women undergoing hysterectomy: a repeated-measures design. J Psychosom Res. (2000) 49:417–22. 10.1016/S0022-3999(00)00189-6
6.
Ali A Altun D Oguz BH Ilhan M Demircan F Koltka K . The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparascopic cholecystectomy. J Anesth. (2014) 28:222–7. 10.1007/s00540-013-1712-7
7.
Broadbent E Kahokehr A Booth RJ Thomas J . A brief relaxation intervention reduces stress and improves surgical wound healing response: a randomised trial. Brain Behav Immun. (2011) 26:212–7. 10.1016/j.bbi.2011.06.014
8.
Van den Bosch JE Moons KG Bonsel GJ Kalkman CJ . Does measurement of preoperative anxiety have added value for predicting postoperative nausea and vomiting?Anesth Analg. (2005) 100:1525–32. 10.1213/01.ANE.0000149325.20542.D4
9.
Kitagawa R Yasui-Furukori N Tsushima T Kaneko S Fukuda I . Depression increases the length of hospitalization for patients undergoing thoracic surgery: a preliminary study. Psychosomatics. (2011) 52:428–32. 10.1016/j.psym.2011.03.010
10.
Derbyshire D Smith G . Sympathoadrenal responses to anaesthesia and surgery. Br J Anaesth. (1984) 56:725–39. 10.1093/bja/56.7.725
11.
Pritchard M . Measuring anxiety in surgical patients using a visual analogue scale. Nurs Stand. (2010) 25:40–4. 10.7748/ns.25.11.40.s53
12.
Kindler CH Harms C Amsler F Scholl T . The visual analog scale allows effective measurement of preoperative anxiety and detection of patients' anesthetic concerns. Anesth Analg. (2000) 90:706–12. 10.1097/00000539-200003000-00036
13.
Elkins G Staniunas R Rajab MH Marcus J . Use of a numeric visual analog anxiety scale among patients undergoing colorectal surgery. Clin Nurs Res. (2004) 13:237–44. 10.1177/1054773803262222
14.
Hornblow AR Kidson MA . The visual analog scale for anxiety: a validation study. Aust N Z J Psychiatry. (1976) 10:339–41. 10.3109/00048677609159523
15.
Agarwal A Ranjan R Dhiraaj S Lakra A Kumar M Singh U . Acupressure for prevention of pre-operative anxiety: a prospective, randomised, placebo controlled study. Anaesthesia. (2005) 60:978–81. 10.1111/j.1365-2044.2005.04332.x
16.
Flory N Salazar GM Lang EV . Hypnosis for acute distress management during medical procedures. Intl Clin Exp Hypnosis. (2007) 55:303–17. 10.1080/00207140701338670
17.
Attias S Keinan Boker L Arnon Z Ben-Arye E Bar'am A Sroka G et al . Effectiveness of integrating individualized and generic complementary medicine treatments with standard care versus standard care alone for reducing preoperative anxiety. J Clin Anesth. (2016) 29:54–64. 10.1016/j.jclinane.2015.10.017
18.
Kimberger O Illievich U Lenhardt R . The effect of skin surface warming on pre-operative anxiety in neurosurgery patients. Anaesthesia. (2007) 62:140–5. 10.1111/j.1365-2044.2007.04934.x
19.
Kong VKF Irwin MG . Gabapentin: a multimodal perioperative drug?Br J Anaesth. (2007) 99:775–86. 10.1093/bja/aem316
20.
Pekcan M Celebioglu B Demir B Saricaoglu F . The effect of premedication on preoperative anxiety. Middle East J Anesthesiol. (2005) 18:421−33.
21.
Kröll W Wisiak UV List WF . Preoperative subjective anxiety. Double blind study using oxazepam. Anaesthesist. (1988) 37:752−7.
22.
Bucx Martin JL Krijtenburg Pi Kox M . Preoperative use of anxiolytic-sedative agents; are we on the right track?J Clin Anesth. (2016) 33:135–40. 10.1016/j.jclinane.2016.03.025
23.
Pomara N Stanley B Block R Berchou RC Stanley M Greenblatt DJ et al . Increased sensitivity of the elderly to the central depressant effects of diazepam. J Clinical Psychiatry. (1985) 46:185−7.
24.
Saadat H Drummond-Lewis J Maranets I Kaplan D . Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg. (2006) 102:1394–6. 10.1213/01.ane.0000204355.36015.54
25.
Ben-Arye E Segev Y Galil G Marom I Gressel O Stein N et al . Acupuncture during gynecological oncology surgery: a randomized controlled trial assessing the impact of integrative therapies on perioperative pain and anxiety. Int J Gynecol Cancer. (2023) 33:1–10. 10.1002/cncr.34542
26.
Hudson BF Davidson J Whiteley MS . The impact of hand reflexology on pain, anxiety and satisfaction during minimally invasive surgery under local anaesthetic: a randomised controlled trial. Int J Nurs Stud. (2015) 52:1789–97. 10.1016/j.ijnurstu.2015.07.009
27.
Levy I Attias S Stern Lavee T Avneri O Cohen G Balachsan S et al . The effectiveness of foot reflexology on anxiety and duration of labor in primiparas: an open-label randomized controlled trial. Complement Ther Clin Pract. (2019) 35:1–9. 10.1016/j.ctcp.2019.101085
28.
Hughes CM Smyth S Lowe-Strong AS . Reflexology for the treatment of pain in people with multiple sclerosis: a double-blind randomised sham-controlled clinical trial. Multiple Sclerosis. (2009) 15:1329–38. 10.1177/1352458509345916
29.
Quinn F Hughes CM Baxter GD . Reflexology in the management of low back pain: a pilot randomised controlled trial. Complement Ther Med. (2008) 16:3–8. 10.1016/j.ctim.2007.05.001
30.
Schulz KF Altman DG Moher D . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. (2010) 63:e1–37. 10.1016/j.jclinepi.2010.03.004
31.
Attias S Schiff E Arnon Z Nae B Somri M Avneri O et al . Using a Delphi consensus process to develop a structured reflexology treatment protocol to reduce preoperative anxiety. Complement Ther Clin Pract. (2019) 35:353–60. 10.1016/j.ctcp.2019.03.016
32.
Jensen MP Chen C Brugger AM . Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. (2003) 4:407–14. 10.1016/S1526-5900(03)00716-8
33.
Benjamini Y Hochberg Y . Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statis Soc B. (1995) 57:289–300. 10.1111/j.2517-6161.1995.tb02031.x
34.
Perks A Chakravarti S Manninen P . Preoperative anxiety in neurosurgical patients. J Neurosurg Anesthesiol. (2009) 21:127–30. 10.1097/ANA.0b013e31819a6ca3
35.
Mackenzie JW . Daycase anaesthesia and anxiety. A study of anxiety profiles amongst patients attending a day bed unit. Anaesthesia. (1989) 44:437–40. 10.1111/j.1365-2044.1989.tb11349.x
36.
Wang SM Kulkarni L Dolev J Kain ZN . Music and preoperative anxiety: a randomized, controlled study. Anesth Analg. (2002) 94:1489–94. 10.1213/00000539-200206000-00021
37.
Holt J Lord J Acharya U White A O'Neill N Shaw S et al . The effectiveness of foot reflexology in inducing ovulation: a sham-controlled randomized trial. Fertil Steril. (2009) 91:2514–9. 10.1016/j.fertnstert.2008.04.016
38.
Rooney T Sharpe L Todd J Richmond B Colagiuri B . The relationship between expectancy, anxiety, and the nocebo effect: a systematic review and meta-analysis with recommendations for future research. Health Psychol Rev. (2022) 17:550–77. 10.1080/17437199.2022.2125894
39.
Chandrababu R Nayak BS Pai VB N R George LS Devi ES et al . Effects of foot massage and patient education in patients undergoing coronary artery bypass graft surgery: a randomized controlled trial. Complement Ther Clin Pract. (2020) 40:101215. 10.1016/j.ctcp.2020.101215
Summary
Keywords
preoperative anxiety, surgery, cholecystectomy, integrative medicine, reflexology
Citation
Samuel A, Lital K-B, Mostafa S, Ariel S, Yael G, Eran B-A, Ibrahim M, Gideon S, Sagi G, Dan S and Elad S (2025) Effectiveness of standard of care, vs. its combination with reflexology and sham reflexology on preoperative anxiety in patients undergoing elective laparoscopic cholecystectomy: a single-blinded randomized controlled trial. Front. Med. 12:1634575. doi: 10.3389/fmed.2025.1634575
Received
24 May 2025
Accepted
21 August 2025
Published
12 September 2025
Volume
12 - 2025
Edited by
Christian S. Kessler, Immanuel Hospital Berlin, Germany
Reviewed by
Andreas Michalsen, Charité University Medicine Berlin, Germany
Randy Horwitz, University of Arizona, United States
Klaus Kramer, University Hospital Ulm, Germany
Updates
Copyright
© 2025 Samuel, Lital, Mostafa, Ariel, Yael, Eran, Ibrahim, Gideon, Sagi, Dan and Elad.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Attias Samuel samuel.attias@b-zion.gov.il
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.