Abstract
Background:
Kidney stones frequently coexist with chronic kidney disease (CKD), sharing common risk factors and leading to adverse outcomes. While percutaneous nephrolithotomy (PCNL) and ureteroscopy (URS) are both effective treatment options, the safety of PCNL has been well-established in CKD patients, whereas the safety profile of URS remains less clear.
Methods:
A retrospective cohort study using the TriNetX database was conducted to compare outcomes in CKD patients undergoing URS or PCNL. Patients aged ≥18 years with a diagnosis of renal stones and CKD were included, excluding those on dialysis. Propensity score matching (PSM) was performed to balance baseline characteristics. The primary outcome was the 5-year rate of major adverse kidney events (MAKE), a composite of mortality, dialysis initiation, and worsened renal function. Secondary outcomes included all-cause mortality and dialysis dependence. Subgroup and sensitivity analyses were performed to ensure robustness.
Results:
Of 5,470 eligible patients, 837 underwent URS and 4,633 underwent PCNL, with 723 patients matched in each group post-PSM. There was no significant difference in MAKE between URS and PCNL (HR 0.93; 95% CI 0.68–1.28; p = 0.6952). All-cause mortality (HR 0.98; 95% CI 0.70–1.36; p = 0.9125) and dialysis dependence (HR 0.57; 95% CI 0.23–1.38; p = 0.2128) were also similar. The limitation of this study is the lack of data on stone size and location.
Conclusion:
In CKD patients with renal stones, URS demonstrated comparable safety and efficacy compared to PCNL, with no significant differences in MAKE, all-cause mortality, or dialysis dependence over 5 years. However, the lack of information regarding stone size, anatomical location, and procedure-specific details (e.g., device use or surgical technique) is a major limitation of our study.
Introduction
Kidney stones are one of the most common kidney diseases, with a rising prevalence worldwide (21.11%) (1). The management of renal stones primarily involves percutaneous nephrolithotomy (PCNL) and ureteroscopy (URS). PCNL is the first-line procedure for renal calculi larger than 20 mm, as it provides the advantage of a higher stone-free rate and is not constrained by stone burden or composition (2, 3). Unfortunately, an international multicenter study involving 5,803 patients undergoing PCNL reported an overall complication rate of 21.5%, including bleeding, sepsis, renal insufficiency, mortality, and so forth (4, 5). URS, a relatively newer technique for managing urolithiasis, is often preferred due to its higher stone-free rate compared to shockwave lithotripsy and its lower complication rate compared to PCNL (6). The complications associated with URS include bleeding, perforation, and renal injury, among others. The overall complication rate for URS ranges from 9 to 21%, with the majority being minor and not requiring intervention (7, 8).
Kidney stones and CKD share several common risk factors, including inadequate fluid intake, bacterial infections, and urinary tract anomalies, which may contribute to their frequent coexistence (9). Moreover, urolithiasis has been associated with a higher risk of developing CKD compared to individuals without urolithiasis (10). Patients with concomitant CKD and renal stones exhibit worse prognoses and elevated surgical risks, highlighting the need for greater attention to this population (11, 12). Both URS and PCNL are effective methods for renal stone removal; however, they may cause renal parenchymal damage and further deteriorate renal function (13–15). A systematic review has demonstrated that PCNL is safe and effective for patients with CKD (11). Additionally, an observational study involving 60 patients supports the conclusion that PCNL is safe and effective for CKD patients (12). On the other hand, URS is considered a less invasive procedure, potentially offering a viable alternative for those patients with higher surgical risks. Although multiple observational studies suggest that URS could be a potential treatment option for renal stones in CKD patients, their conclusions are limited by small sample sizes and a lack of long-term follow-up data (16, 17).
It remains unclear whether URS is as safe as PCNL in patients with CKD and renal stones. To address this knowledge gap, our study utilizes the TriNetX database to compare outcomes between patients undergoing URS and PCNL, focusing on critical endpoints such as mortality and the need for dialysis in 5 years.
Methods
Data source
This retrospective cohort study utilized the TriNetX database, which compiles de-identified patient-level data derived from electronic health records. The database gathers information from healthcare organizations (HCOs), primarily academic medical centers, encompassing their main hospitals, affiliated satellite hospitals, and outpatient clinics. The data include patient demographics, diagnoses [using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)], procedures [coded via the ICD-10 Procedure Coding System or Current Procedural Terminology (CPT)], medications (categorized by the Veterans Affairs Drug Classification System and RxNorm codes), laboratory tests [identified through Logical Observation Identifiers Names and Codes (LOINC)], and healthcare utilization metrics. For this study, we accessed data from TriNetX’s Global Collaborative Network, which spans over 124 million patients across 131 HCOs in 15 countries (18).
The results were validated using industry-standard methodologies and presented in summarized form. Further details about the database are available online (19) and in prior publications. The results were validated using independent, industry-standard methods, and provided to investigators in a summarized format. Further details about the database are available online (19) and have been previously described in the literature (18).
Since the study utilized only aggregated statistical summaries of de-identified data, the need for informed consent was waived. The study adhered to the ethical principles of the Declaration of Helsinki (20) and complied with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (21). Notably, information regarding stone size, composition, and anatomical location was not available in the TriNetX database. This limitation should be considered when interpreting the study findings.
Ethics approval and consent to participate
The Western Institutional Review Board granted a waiver for informed consent, citing TriNetX’s capability to generate only aggregated and statistical summaries from de-identified data obtained from multiple healthcare providers. This approach ensures the protection of patient privacy and confidentiality. As the study relied solely on aggregated statistical summaries of de-identified data, informed consent was deemed unnecessary and subsequently waived. As per institutional and regulatory guidelines, studies using such data are exempt from Institutional Review Board approval.
Cohort
The study included patients aged 18 years or older with a diagnosis of renal stones and CKD. Patients who have already undergoing dialysis were excluded. Participants who underwent procedures for renal stones were categorized into two groups: those treated with URS and those treated with PCNL. For this study, the database was last accessed on November 16, 2024. The index event was the date of the URS or PCNL treatment. Both groups were followed for up to 5 years. Supplementary Table 1 provides detailed information on the codes used to identify demographics, diagnoses, and laboratory parameters.
Covariables
A 1:1 propensity score matching (PSM) was performed using 25 variables, including demographics, diagnoses, and laboratory data. Covariate selection was informed by clinical relevance, prioritizing major comorbidities and risk factors known to influence renal failure and mortality (22). The selected variables were used to address baseline imbalances between the URS and PCNL groups. These variables encompassed (1) age, sex, race, and ethnicity; (2) comorbidities included essential hypertension, disorder of lipoprotein metabolism, diabetes mellitus, overweight and obesity, ischemic heart disease, heart failure, cerebrovascular disease, calculus in bladder, hyperparathyroidism and disorder of parathyroid gland, hyperparathyroidism, systemic lupus erythematosus, and uric acid nephrolithiasis; and (3) laboratory data such as estimated glomerular filtration rate, calcium, phosphate, magnesium, parathyrin intact, and urate level. Additional information on the categorization and codes used to define the covariates can be found in Supplementary Table 1.
Primary and secondary outcomes
The primary outcome was the cumulative incidence of major adverse kidney event (MAKE), which was defined as mortality, initiation of dialysis, or worsened renal function. Secondary outcomes included dialysis dependence and all-cause mortality. Patients were followed from the day after the index date for up to 5 years.
Subgroup and sensitivity analysis
We conducted prespecified subgroup analyses based on age (≥65 or <65 years), gender (male or female), patients with advanced chronic kidney disease (estimated glomerular filtration rate <45 mL/min/1.73m2) and the presence or absence of diabetes mellitus, overweight and obesity, heart failure, and coronary artery disease to determine whether the outcomes were consistent across different populations.
To evaluate the robustness of our findings, we conducted a sensitivity analysis by changing the follow-up period to one and 2 years and removing PSM analysis.
Statistical analysis
The baseline characteristics of the two groups were summarized as means with standard deviations (SDs) for continuous variables and as counts with percentages for categorical variables. Comparisons of categorical variables were performed using the χ2 test, while continuous variables were analyzed with an independent two-sample t-test. One-to-one PSM was carried out using the greedy nearest neighbor algorithm with a caliper width of 0.1 pooled SDs to ensure balance in baseline characteristics between the groups. Matching was considered adequate if the standardized difference between the groups was less than 0.1 (Table 1) (23).
Table 1
| Characteristics | Before matching, no. (%) | After matching, no. (%) | ||||
|---|---|---|---|---|---|---|
| URS (n = 837) | PCNL (n = 4,633) | Standardized difference | URS (n = 723) | PCNL (n = 723) | Standardized difference | |
| Age, mean(SD), years | 60.6 ± 15.9 | 61.1 ± 14.8 | 0.0329 | 60.5 ± 15.9 | 60.0 ± 15.7 | 0.0332 |
| Sex | ||||||
| Female | 368 (46.8%) | 2,186 (48.7%) | 0.0368 | 339 (46.8%) | 339 (46.8%) | <0.0001 |
| Male | 396 (50.4%) | 2,215 (49.3%) | 0.0216 | 364 (50.3%) | 369 (51.0%) | 0.0138 |
| Race | ||||||
| White | 566 (72.1%) | 3,487 (77.7%) | 0.1297 | 565 (78.1%) | 544 (75.2%) | 0.0687 |
| Black or African American | 46 (5.8%) | 359 (8.0%) | 0.0844 | 46 (6.3%) | 47 (6.5%) | 0.0056 |
| Unknown race | 146 (18.5%) | 345 (7.6%) | 0.3272 | 85 (11.7%) | 107 (14.7%) | 0.0898 |
| Asian | 12 (1.5%) | 137 (3.0%) | 0.1020 | 12 (1.6%) | 10 (1.3%) | 0.0226 |
| Comorbidities | ||||||
| Essential hypertension | 409 (52.1%) | 2,456 (54.7%) | 0.0528 | 385 (53.2%) | 389 (53.8%) | 0.0111 |
| Disorder of lipoprotein metabolism | 209 (26.6%) | 1,804 (40.2%) | 0.2909 | 209 (28.9%) | 196 (27.1%) | 0.0401 |
| Diabetes mellitus | 238 (30.3%) | 1,479 (32.9%) | 0.0569 | 219 (30.2%) | 207 (28.6%) | 0.0364 |
| Overweight and obesity | 186 (23.6%) | 1,173 (26.1%) | 0.0566 | 174 (24.0%) | 162 (22.4%) | 0.0393 |
| Ischemic heart disease | 130 (16.5%) | 839 (18.6%) | 0.0561 | 123 (17.0%) | 113 (15.6%) | 0.0374 |
| Heart failure | 68 (8.6%) | 461 (10.2%) | 0.0551 | 64 (8.8%) | 59 (8.1%) | 0.0248 |
| Cerebrovascular disease | 52 (6.6%) | 383 (8.5%) | 0.0723 | 50 (6.9%) | 53 (7.3%) | 0.0161 |
| Calculus in bladder | 50 (6.3%) | 341 (7.6%) | 0.0483 | 48 (6.6%) | 42 (5.8%) | 0.0344 |
| Hyperparathyroidism and disorder of parathyroid gland | 20 (2.5%) | 150 (3.3%) | 0.0470 | 20 (2.7%) | 14 (1.9%) | 0.0548 |
| Hyperparathyroidism, unspecified | 13 (1.6%) | 116 (2.5%) | 0.0645 | 13 (1.7%) | 10 (1.3%) | 0.0332 |
| Systemic lupus erythematosus | 10 (1.2%) | 38 (0.8%) | 0.0417 | 10 (1.3%) | 10 (1.3%) | <0.0001 |
| Uric acid nephrolithiasis | 10 (1.2%) | 59 (1.3%) | 0.0036 | 10 (1.3%) | 10 (1.3%) | <0.0001 |
| Characteristics | Before matching, mean ± SD | After matching, mean ± SD | ||||
|---|---|---|---|---|---|---|
| URS (n = 837) | PCNL (n = 4,633) | Standardized difference | URS (n = 723) | PCNL (n = 723) | Standardized difference | |
| Laboratory data | ||||||
| Estimated glomerular filtration rate, mL/min/1.73 m2 | 57.9 ± 30.7 | 58.2 ± 27.4 | 0.0107 | 57.9 ± 30.7 | 59.2 ± 32.9 | 0.0411 |
| Calcium, mg/dL | 9.0 ± 0.7 | 9.2 ± 0.6 | 0.3123 | 9.0 ± 0.7 | 9.3 ± 0.7 | 0.3519 |
| Phosphate, mg/dL | 3.3 ± 0.7 | 3.3 ± 0.8 | 0.0150 | 3.3 ± 0.7 | 3.2 ± 0.7 | 0.1539 |
| Magnesium, mg/dL | 1.8 ± 0.2 | 1.8 ± 0.2 | 0.0400 | 1.8 ± 0.2 | 1.8 ± 0.2 | 0.0414 |
| Parathyrin intact, pg/mL | 69 ± 48.1 | 76.8 ± 81.8 | 0.1162 | 68.6 ± 48.2 | 70.5 ± 53.6 | 0.0370 |
| Urate, mg/dL | 6.35 ± 1.8 | 6.45 ± 2.2 | 0.0503 | 6.35 ± 1.8 | 6.56 ± 2.9 | 0.0848 |
Baseline characteristics of the URS and PCNL groups before and after propensity score matching.
URS, ureteroscopy; PCNL, percutaneous nephrolithotomy; SD, standardized differences.
Survival probabilities after PSM were estimated using the Kaplan–Meier method and log-rank tests. Hazard ratios (HRs) with 95% confidence intervals (CIs) and p-values were determined using Cox proportional hazards regression models for all outcomes. The E-value method was applied to assess the potential influence of unmeasured confounding, estimating the minimum strength of association an unmeasured confounder would require to account for the observed differences between the two groups. An E-value of x indicates that the observed association could only be attributed to an unmeasured confounder if it were associated with both the treatment and the outcome by a risk ratio of at least x, beyond the effects of the measured confounders (Table 2) (24).
Table 2
| Outcome | Number of patients with outcomes | HR (95%CI) | p-value | E-value | |
|---|---|---|---|---|---|
| URS (n = 723) | PCNL (n = 723) | ||||
| Primary outcome | |||||
| Major adverse kidney events | 79 | 77 | 0.93 (0.68–1.28) | 0.6952 | 1.36 |
| Secondary outcome | |||||
| Dialysis dependence | 10 | 13 | 0.57 (0.23–1.38) | 0.2128 | 2.90 |
| All-cause mortality | 75 | 70 | 0.98 (0.70–1.36) | 0.9125 | 1.16 |
Comparison of URS vs. PCNL for primary and secondary outcomes.
URS, ureteroscopy; PCNL, percutaneous nephrolithotomy; HR, hazard ratio.
All statistical tests were two-sided, with a significance threshold set at p < 0.05. Statistical analyses were conducted using the analytic tools available on the TriNetX platform.
Results
A total of 2,232,383 patients aged over 18 were diagnosed with renal stones. Among them, 232,426 had a prior diagnosis of chronic kidney disease. After excluding patients undergoing hemodialysis, 5,470 individuals underwent URS or PCNL within 2 weeks of their renal stone diagnosis. Of these, 837 patients received URS, while 4,633 received PCNL. Based on demographics, comorbidities, and laboratory data, PSM resulted in 723 patients in each group (Figure 1).
Figure 1

Flow diagram of cohort construction. CKD, chronic kidney disease; URS, ureteroscopy; PCNL, percutaneous nephrolithotomy.
Before PSM, there were no significant differences in age (60.6 ± 15.9 vs. 61.1 ± 14.8, p = 0.3827) or the proportion of males (50.4% vs. 49.3%, p = 0.5762) between the URS and PCNL groups. However, the URS group had a lower percentage of White (72.1% vs. 77.7%, p = 0.0006), African American (5.8% vs. 8.0%, p = 0.0377), and Asian patients (1.5% vs. 3.0%, p = 0.0174) compared to the PCNL group. Patients who underwent URS also had a lower prevalence of dyslipidemia (26.6% vs. 40.2%, p < 0.0001) compared to those in the PCNL group. Other comorbidities were similar between the two groups. Regarding laboratory data, the URS group had a lower serum calcium level (9.06 ± 0.7 vs. 9.28 ± 0.6, p < 0.0001) compared to the PCNL group, while other laboratory parameters were comparable between the groups. After matching, the baseline characteristics were balanced and showed no significant differences between the groups (p > 0.05) (Table 1).
The propensity score density curves before and after matching are presented in Supplementary Figure 1.
Primary outcome
Over the 5-year follow-up period, 79 (10.9%) patients experienced MAKE in the URS group, and 77 (10.7%) individuals in PCNL group. There is no significant difference between URS and PCNL group [HR 0.93; 95% CI 0.68–1.28; p = 0.6952 (Table 2 and Figure 2)].
Figure 2
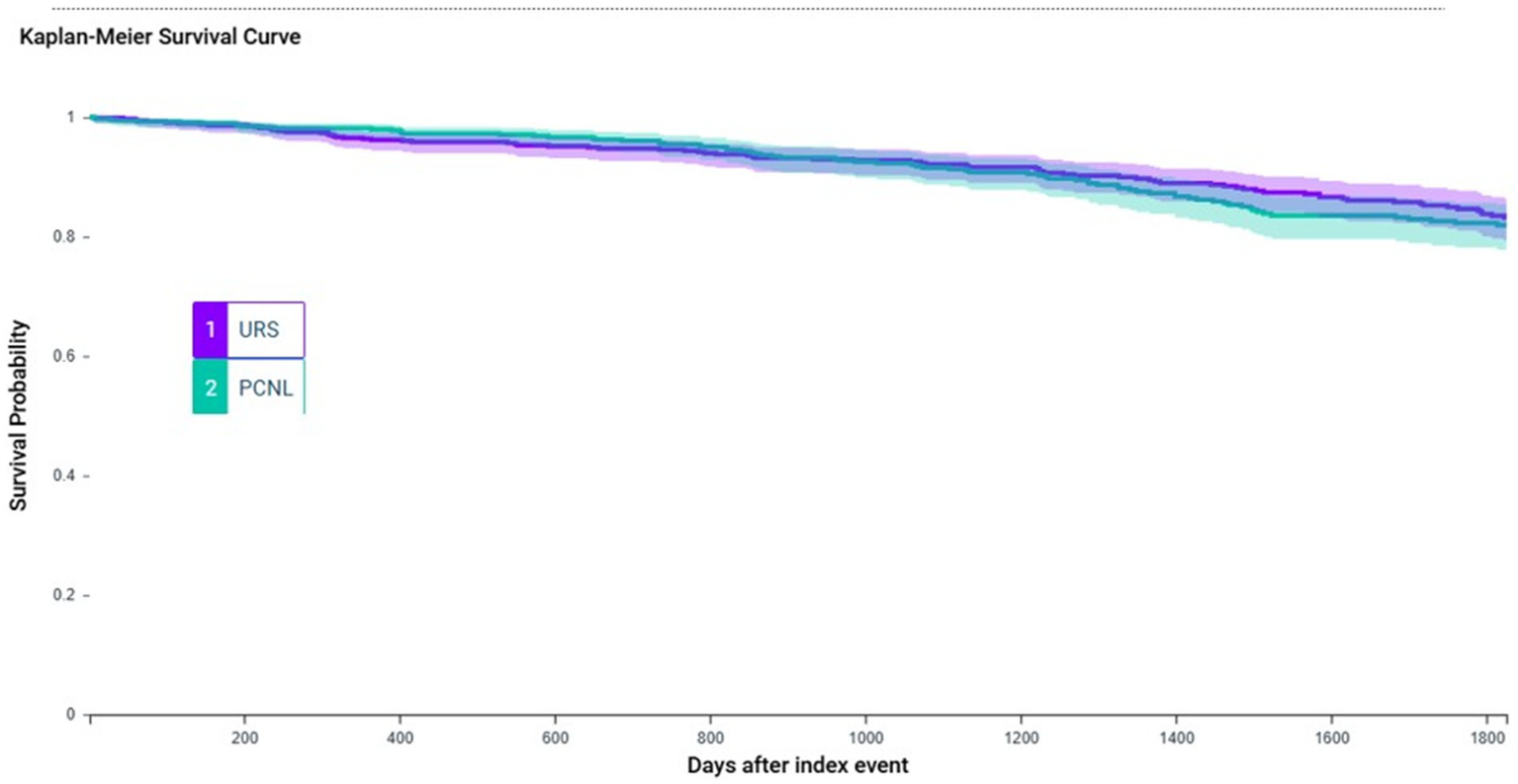
This Kaplan–Meier survival curve compares patients who received URS versus PCNL. There is no significant difference in 5 year MAKE rate between two groups. URS, ureteroscopy; PCNL, percutaneous nephrolithotomy; MAKE, major adverse kidney events.
Secondary outcome
The risk of dialysis dependence (HR 0.57; 95% CI 0.23–1.38; p = 0.2128) and all-cause mortality (HR 0.98; 95% CI 0.70–1.36; p = 0.9125) showed no statistical difference between patients who received URS and PCNL (Table 2). Based on the E-value analysis, it is improbable that unmeasured confounders had a substantial impact on our results. The E-values for the point estimates were 1.36 for MAKE, 2.90 for dialysis dependence, and 1.16 for all-cause mortality, respectively (Table 2).
Subgroup and sensitivity analysis
The results of this study were consistent across subgroups, including age (≥65 or <65 years), sex (male or female), patients with advanced CKD (estimated glomerular filtration rate <45 mL/min/1.73 m2) and the presence or absence of diabetes mellitus, obesity, heart failure, and coronary artery disease (Supplementary Table 2).
In sensitivity analyses, the outcomes remained non-significant at both the 1-year and 3-year follow-ups and were consistent in analyses without PSM (Supplementary Table 2).
Discussion
Our research revealed no significant difference in the 5-year MAKE cumulative incidence rate between URS and PCNL in patients with CKD. Similarly, the secondary outcomes showed no significant differences in 5-year all-cause mortality or dialysis dependence between the two groups. These findings were consistent across subgroups stratified by age, sex, advanced CKD, and the presence or absence of diabetes mellitus, obesity, heart failure, or coronary artery disease. Sensitivity analyses confirmed these results at 1-and 3-year follow-ups, as well as in analyses without PSM.
Clinical diagnosis of CKD has been found to be more prevalent in kidney stone formers compared to control subjects, highlighting the potential impact of kidney stones on renal function (25). This association may be due to repeated episodes of obstructive uropathy, infections, or inflammation caused by stones, which can lead to progressive kidney damage and scarring (9). The coexistence of CKD and renal stones is associated with a significantly worse prognosis compared to patients without CKD (11). CKD patients are also more vulnerable to surgical complications and slower recovery (26) Moreover, the presence of both conditions may accelerate the progression of renal function decline, increasing the risk of end-stage kidney disease, and mortality (11, 12, 27). These findings underscore the importance of early detection and management of kidney stones to mitigate the risk of CKD progression.
Previous studies have demonstrated the safety and effectiveness of PCNL in CKD patients, highlighting its ability to achieve high stone-free rates while maintaining acceptable complication rates (11, 12). These findings suggest that PCNL is a reliable option for managing renal stones in patients with impaired kidney function, particularly for those with large or complex stones. In contrast, the safety of the newer technique, URS, in CKD patients is less well-documented but shows promising potential. While URS is widely recognized for its minimally invasive nature and shorter recovery times, there is limited evidence specifically evaluating its long-term outcomes and safety profile in patients with compromised renal function (16, 17). In CKD patients, URS offers potential advantages due to its minimally invasive nature, shorter hospitalization, and lower risk of bleeding and renal parenchymal injury compared to PCNL (6, 28). Previous smaller studies have suggested that URS may preserve renal function in selected CKD patients, supporting its safety profile (16). However, the lower stone-free rate of URS relative to PCNL raises concerns about residual stones, which may predispose patients to recurrent obstruction and infection, ultimately compromising renal outcomes (17, 29, 30). Our study adds to the limited evidence by demonstrating that URS is comparable to PCNL in terms of long-term MAKE and survival in CKD patients. These findings suggest that URS may be considered a reasonable alternative, particularly in patients with high surgical risk, though further prospective studies are needed to confirm these benefits and address the impact of residual stone burden. This study leveraged a large multicenter database and PSM to enhance statistical power and minimize the impact of measured confounders. Our findings suggest that URS could be considered a less invasive alternative to PCNL for patients with CKD, particularly in cases where minimizing surgical risk is a priority. Future studies, particularly randomized controlled trials, are needed to validate these findings and explore long-term outcomes in CKD patients undergoing URS or PCNL.
Limitation
This study has several limitations. First, its retrospective design may introduce inherent selection bias, residual confounding, and misclassification of exposures or outcomes, despite the application of PSM to balance measured covariates. Second, detailed clinical information such as stone size, composition, and location was not available in the database, which represents a major limitation given their strong influence on treatment outcomes. In addition, key procedural outcomes, including stone-free rate, retreatment rate, hospital stay, and procedure-specific complications, were not captured. Finally, technical variations, such as the use of suction or access sheaths during URS and ultrasound guidance or specialized devices during PCNL, were also unavailable, which may have further affected outcomes. Third, the database does not provide information on the size or location of the renal stones, which are important factors influencing treatment outcomes. Fourth, the event rate for dialysis was low, which may have reduced the statistical power to detect significant differences in this outcome. Third, as an observational study, it cannot establish causal relationships between the treatments and outcomes. Fifth, the TriNetX database does not provide sufficient detail to distinguish between rigid ureteroscopy and flexible retrograde intrarenal surgery. The inability to precisely differentiate procedure types remains a limitation.
Sixth, the database does not include information on the causes of death, limiting our ability to analyze mortality. Finally, being a retrospective study also makes the findings inherently weaker; therefore, we recommend that similar investigations be conducted prospectively to provide more definitive evidence.
Conclusion
This study demonstrates that both URS and PCNL are viable options for managing renal stones in patients with CKD, with no significant differences observed in 5-year MAKE rates, all-cause mortality, or dialysis dependence between the two procedures. Given its minimally invasive nature and comparable long-term safety profile, URS can be considered a safe alternative to PCNL in CKD patients, particularly in those where reducing surgical risk is a priority. Further research is necessary to confirm these results and provide a deeper understanding of the long-term outcomes of URS and PCNL in CKD patients.
Statements
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://trinetx.com/.
Ethics statement
The studies involving humans were approved by since the study utilized only aggregated statistical summaries of de-identified data, the need for informed consent was waived. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because since the study utilized only aggregated statistical summaries of de-identified data, the need for informed consent was waived.
Author contributions
J-KC: Data curation, Methodology, Writing – review & editing, Writing – original draft. J-YW: Writing – review & editing, Writing – original draft, Formal analysis, Project administration. Y-ML: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1644526/full#supplementary-material
References
1.
Moftakhar L Jafari F Ghoddusi Johari M Rezaeianzadeh R Hosseini SV Rezaianzadeh A . Prevalence and risk factors of kidney stone disease in population aged 40-70 years old in Kharameh cohort study: a cross-sectional population-based study in southern Iran. BMC Urol. (2022) 22:205. doi: 10.1186/s12894-022-01161-x
2.
Setthawong V Srisubat A Potisat S Lojanapiwat B Pattanittum P . Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. (2023) 8:Cd007044. doi: 10.1002/14651858.CD007044.pub4
3.
Jones P Elmussareh M Aboumarzouk OM Mucksavage P Somani BK . Role of minimally invasive (Micro and ultra-mini) PCNL for adult urinary stone disease in the modern era: evidence from a systematic review. Curr Urol Rep. (2018) 19:27. doi: 10.1007/s11934-018-0764-5
4.
de la Rosette J Assimos D Desai M Gutierrez J Lingeman J Scarpa R et al . The clinical research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, complications, and outcomes in 5803 patients. J Endourol. (2011) 25:11–7. doi: 10.1089/end.2010.0424
5.
Taylor E Miller J Chi T Stoller ML . Complications associated with percutaneous nephrolithotomy. Transl Androl Urol. (2012) 1:223–8. doi: 10.3978/j.issn.2223-4683.2012.12.01
6.
Tugcu V Resorlu B Sahin S Atar A Kocakaya R Eksi M et al . Flexible Ureteroscopy versus retroperitoneal laparoscopic Ureterolithotomy for the treatment of proximal ureteral stones >15 mm: a single surgeon experience. Urol Int. (2016) 96:77–82. doi: 10.1159/000430452
7.
Türk C Petřík A Sarica K Seitz C Skolarikos A Straub M et al . EAU guidelines on interventional treatment for urolithiasis. Eur Urol. (2016) 69:475–82. doi: 10.1016/j.eururo.2015.07.041
8.
Somani BK Giusti G Sun Y Osther PJ Frank M De Sio M et al . Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the clinical research Office of Endourological Society URS global study. World J Urol. (2017) 35:675–81. doi: 10.1007/s00345-016-1909-0
9.
Chuang TF Hung HC Li SF Lee MW Pai JY Hung CT . Risk of chronic kidney disease in patients with kidney stones-a nationwide cohort study. BMC Nephrol. (2020) 21:292. doi: 10.1186/s12882-020-01950-2
10.
Kim JY Lee JK Park JT Chang TI . Risk of incident chronic kidney disease among patients with urolithiasis: a nationwide longitudinal cohort study. Clin Kidney J. (2024) 17:sfae030. doi: 10.1093/ckj/sfae030
11.
Mehra K Satpathy P Joshi A Manikandan R . Percutaneous Nephrolithotomy in patients with chronic kidney disease: a systematic review. Urol Int. (2022) 106:461–8. doi: 10.1159/000520266
12.
Adiga P Pudakalkatti SR Shivakumar V Jain M Sreenidhi RN Manohar CS et al . Is percutaneous nephrolithotomy safe in chronic kidney disease patients!!!Urol Ann. (2022) 14:317–21. doi: 10.4103/ua.ua_100_21
13.
Basnet RB Shrestha A Shrestha PM Joshi BR . Risk factors for postoperative complications after percutaneous Nephrolithotomy. J Nepal Health Res Counc. (2018) 16:79–83. doi: 10.3126/jnhrc.v16i1.19371
14.
Ganpule AP Vijayakumar M Malpani A Desai MR . Percutaneous nephrolithotomy (PCNL) a critical review. Int J Surg. (2016) 36:660–4. doi: 10.1016/j.ijsu.2016.11.028
15.
Kallidonis P Ntasiotis P Somani B Adamou C Emiliani E Knoll T et al . Systematic review and meta-analysis comparing percutaneous Nephrolithotomy, retrograde intrarenal surgery and shock wave lithotripsy for lower pole renal stones less than 2 cm in maximum diameter. J Urol. (2020) 204:427–33. doi: 10.1097/JU.0000000000001013
16.
Aghamir SMK . Successful retrograde intrarenal surgery (RIRS) for a 2-centimeter stone in a chronic renal failure (CRF) patient. Int J Surg Case Rep. (2021) 87:106375. doi: 10.1016/j.ijscr.2021.106375
17.
Reeves T Pietropaolo A Somani BK . Ureteroscopy and laser stone fragmentation is safe and tends to improve renal function in patients with chronic kidney disease: prospective outcomes with a minimum follow-up of 6 months. J Endourol. (2020) 34:423–8. doi: 10.1089/end.2019.0784
18.
Palchuk MB London JW Perez-Rey D Drebert ZJ Winer-Jones JP Thompson CN et al . A global federated real-world data and analytics platform for research. JAMIA Open. (2023) 6:ooad035. doi: 10.1093/jamiaopen/ooad035
19.
TriNetX . Available online at: https://trinetx.com.
20.
World medical association . World Medical Association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
21.
Cuschieri S . The STROBE guidelines. Saudi J Anaesth. (2019) 13:S31–4. doi: 10.4103/sja.SJA_543_18
22.
Zhang X Fang Y Zou Z Hong P Zhuo Y Xu Y et al . Risk factors for progression of CKD with and without diabetes. J Diabetes Res. (2022) 2022:1–12. doi: 10.1155/2022/9613062
23.
Zhang Z Kim HJ Lonjon G Zhu Y . Balance diagnostics after propensity score matching. Ann Transl Med. (2019) 7:16. doi: 10.21037/atm.2018.12.10
24.
Vander Weele TJ Ding P . Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. (2017) 167:268–74. doi: 10.7326/M16-2607
25.
Rule AD Bergstralh EJ Melton LJ 3rd Li X Weaver AL Lieske JC . Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol. (2009) 4:804–11. doi: 10.2215/CJN.05811108
26.
You Y Zhang Y Qiang L Sun Y Zhang J Bou E et al . Prevalence and risk factors for perioperative complications of CKD patients undergoing elective hip surgery. J Orthop Surg Res. (2019) 14:82. doi: 10.1186/s13018-019-1118-9
27.
Reeves T Pietropaolo A Gadzhiev N Seitz C Somani BK . Role of Endourological procedures (PCNL and URS) on renal function: a systematic review. Curr Urol Rep. (2020) 21:21. doi: 10.1007/s11934-020-00973-4
28.
Wu T Duan X Chen S Yang X Tang T Cui S . Ureteroscopic lithotripsy versus laparoscopic Ureterolithotomy or percutaneous Nephrolithotomy in the Management of Large Proximal Ureteral Stones: a systematic review and Meta-analysis. Urol Int. (2017) 99:308–19. doi: 10.1159/000471773
29.
Chen P Wei TT Huang EY Lin TP Huang TH Lin CC et al . Comparison of stone-free rate between percutaneous nephrolithotomy and retrograde intrarenal surgery. J Chin Med Assoc. (2023) 86:485–8. doi: 10.1097/JCMA.0000000000000913
30.
Rule AD Krambeck AE Lieske JC . Chronic kidney disease in kidney stone formers. Clin J Am Soc Nephrol. (2011) 6:2069–75. doi: 10.2215/CJN.10651110
Summary
Keywords
CKD, MAKE, PCNL, renal stone, URS
Citation
Chiou J-K, Wu J-Y and Lin Y-M (2025) Comparative outcomes of ureteroscopy and percutaneous nephrolithotomy in CKD patients with renal calculi: a propensity-matched cohort study. Front. Med. 12:1644526. doi: 10.3389/fmed.2025.1644526
Received
10 June 2025
Accepted
22 September 2025
Published
03 October 2025
Volume
12 - 2025
Edited by
Limin Liu, Northwest University, China
Reviewed by
Juan Francisco Monzón Falconi, Hospital Quirón Teknon, Spain
Ahmed Reda, Assiut University Hospital, Egypt
Updates
Copyright
© 2025 Chiou, Wu and Lin.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Min Lin, xxpil305a@gmail.com; Jheng-Yan Wu, andy10271@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.