Abstract
There is a wide variety of causes of pancreatitis, such as cholelithiasis and ethanol, of which only a small percentage are induced by foreign bodies, while cases of pancreatitis due to accidental ingestion of fish bone are seldom reported. Most accidentally ingested fish bones are eliminated through the digestive tract. It is very rare for them to penetrate the gastrointestinal tract and enter the pancreas, causing related complications. Here, we present a case of pancreatitis secondary to accidental ingestion of a fish bone. The case was initially poorly managed with medical treatment and further imaging suggestive of perforation and infection, which was successfully removed after exploratory laparotomy and intraoperative gastroscopy. A history of accidental fish bone ingestion is important and that contrast-enhanced computed tomography is indispensable for an early diagnosis. Endoscopic removal has the advantages of being less invasive, less painful, and easier to perform and is therefore preferred in most patients in recent years.
1 Introduction
Acute pancreatitis (AP), affecting approximately 34 per 100,000 individuals annually, is predominantly caused by gallstones, alcohol, or hyperlipidemia (1, 2). Foreign body-induced AP, however, accounts for <1% of cases, with fish bone penetration into the pancreas being exceptionally rare (3). Accidental ingestion of fish bones is common in life, most of which are passed from the gastrointestinal tract on their own, while a small number of them will penetrate the intestinal wall and enter neighboring organs, causing inflammation or abscess formation (4). Most ingested fish bones pass uneventfully through the gastrointestinal tract; perforation occurs in <1%, and pancreatic involvement is scarcely documented (5, 6). Here, we present a case of fish bone-induced pancreatitis in a patient with Billroth II anatomy, emphasizing diagnostic pitfalls and management strategies.
2 Case presentation
An 85-year-old man presented with 3 days of severe epigastric pain, nausea, and fever (38.3 °C). The abdominal pain was of a severe degree, not self-relieving. The patient has hypertension and Meniere’s disease, as well as a history of cerebral infarction. He denied alcohol consumption or gallstone history but had undergone a Billroth II gastrojejunostomy for a gastric ulcer more than 40 years ago. Physical examination revealed fever up to 38.3 °C, with pressure and rebound tenderness on palpation of the upper abdomen. Laboratory findings revealed elevated leukocytosis (13.8 × 109/L) and CRP (119.4 mg/L), but normal serum amylase (58 U/L) (Table 1). Abdominal contrast-enhanced computed tomography (CECT) demonstrated pancreatic head edema and peripancreatic exudation (Figure 1A). No biliary obstruction was observed. Consequently, the diagnosis of acute pancreatitis was made. After admission to the hospital, the patient was fasted, given gastrointestinal decompression, acid suppression with proton pump inhibitors, inhibition of pancreatic secretion with growth inhibitors, anti-infection with antibiotics, and started on intravenous fluids.
Table 1
| Test | Result | Reference range |
|---|---|---|
| White blood cell count, 109/L | 13.8 | 3.5–9.5 |
| Neutrophil, 109/L | 12.6 | 1.8–6.3 |
| Hemoglobin, g/L | 104.0 | 130.0–175.0 |
| Platelet count, 109/L | 173.0 | 125.0–350.0 |
| High-sensitivity C-reactive protein, mg/L | 119.4 | < 10.0 |
| Amylase, U/L | 58.0 | 20.0–125.0 |
| Procalcitonin, ng/mL | 0.46 | < 0.065 |
Blood test results on admission.
Figure 1

(A) Contrast-enhanced computed tomography showed fullness of the head of the pancreas, peripheral oozing, and blurring of the surrounding fat space (black arrow). (B) Contrast-enhanced computed tomography showed a localized hyperdense shadow (red triangle) in the head-duodenal region of the pancreas with a long diameter of approximately 21 mm and a fixed morphology.
However, after several days of treatment, initial conservative therapy (fasting, antibiotics, octreotide) failed to alleviate the symptoms. Although the abdominal pain persisted, the blood and urine amylase levels were still not high. Repeat CECT revealed a linear hyperdensity shadow in the pancreatic head-duodenal region (Figure 1B). The patient then underwent an emergency laparotomy and was classified as ASA IIIE according to the American Society of Anesthesiologists (ASA) Physical Status Classification System. Emergency surgery revealed infection around the pancreatic head and duodenum. Despite abscess drainage, no foreign body was initially detected. Intraoperative endoscopy was subsequently performed, and a 2.1 cm long fish bone was identified in the gastric pouch, which was successfully removed with foreign body forceps. The patient experienced intraoperative tachycardia and hemodynamic instability, requiring postoperative intensive care with endotracheal intubation for further life support. Two weeks later, with stable vital signs and no surgical complications, he made a full recovery and was successfully discharged from the hospital. Figure 2 shows the timeline of clinical presentation and treatment during hospitalization.
Figure 2
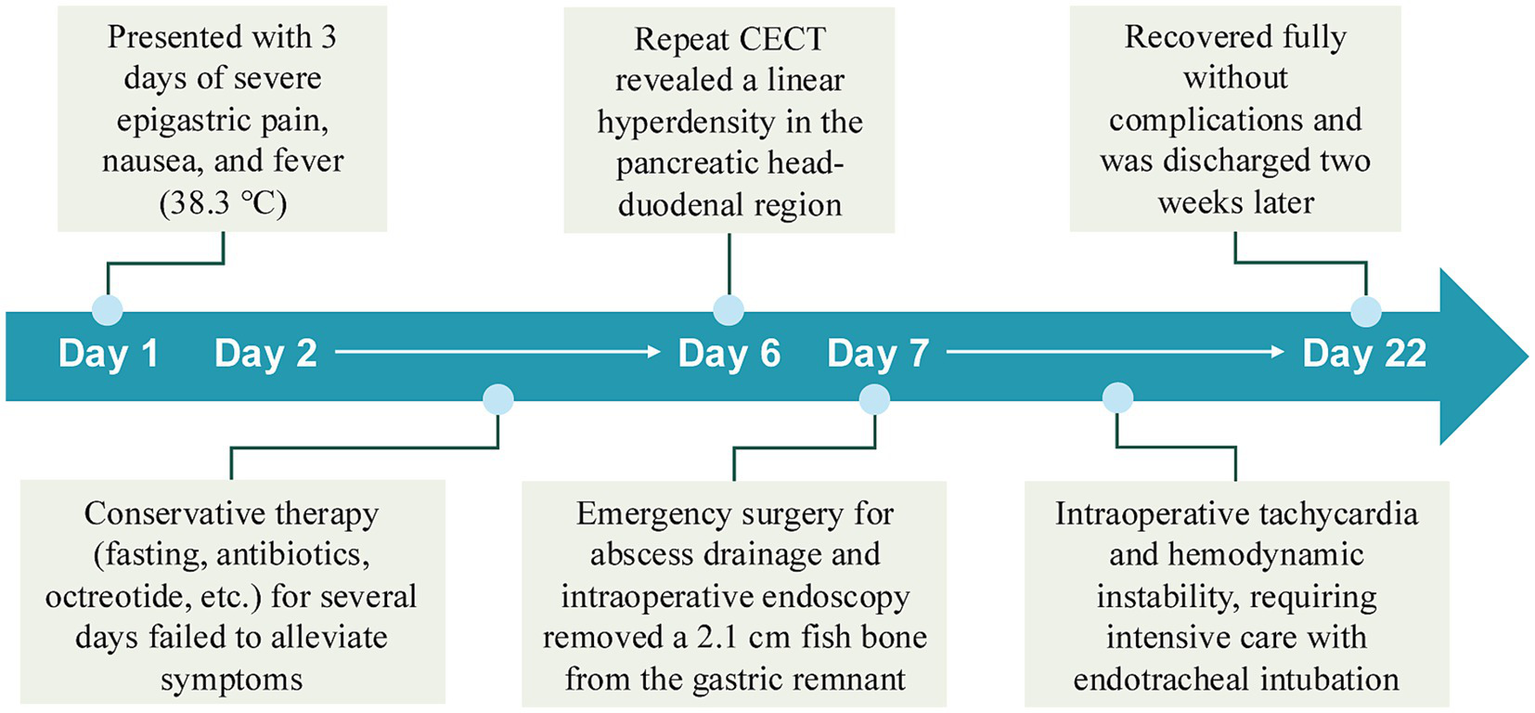
Timeline of clinical presentation and management.
3 Discussion
Acute pancreatitis is a common clinical disorder of the digestive system, usually caused by abnormal activation of pancreatic enzymes and self-digestion of pancreatic tissue. It has a wide range of causes. Globally, the most common causes in patients with acute pancreatitis are cholelithiasis, alcohol and hyperlipidemia (2). An uncommon cause of pancreatitis is foreign body-induced pancreatitis.
The diagnosis of acute pancreatitis needs to be established on two of the following three items: characteristic abdominal pain, elevated blood amylase or lipase, and typical imaging changes. If a patient has a presentation of abdominal pain suggestive of acute pancreatitis, but serum amylase and/or lipase activity is less than three times the upper limit of normal, imaging studies are required to confirm the diagnosis (7, 8). Severe pancreatic necrosis or microcirculatory impairment may limit enzyme production and release, explaining the discordance between clinical and biochemical findings (9, 10). The delay in patient visits also connected with the decline in amylase levels to some extent (serum amylase levels often rise within hours of the onset of symptoms and revert to normal within three to five days) (11, 12). Diagnostic imaging is crucial in individuals with little or no enzyme elevation (13). CECT is the most effective imaging technique to assess the severity of AP, distinguish other serious abdominal conditions, and find complications. In addition, CECT can determine the presence of pancreatic necrosis and provide clues to the etiology of AP, which is an important clinical guideline for subsequent treatment (7).
Foreign body-induced AP is clinically uncommon. Fish bones are one of the most common foreign bodies causing perforation, mostly seen in cultures where unfilleted fish is a culinary delicacy (14). For instance, people in some Asian countries tend to prefer freshwater fish with numerous small bones. However, cases of fish bones penetrating the gastrointestinal tract and causing pancreatitis are very rare, with only less than 20 cases reported to date (4). A systematic analysis of 16 cases (Table 2) revealed: median age 65 years (range: 32–85), 56% male; 100% cases relied on CT, while only 19% exhibited elevated amylase; The prognosis for those who underwent surgery in time was mostly favorable; Endoscopic/laparoscopic approaches increased post-2018, reflecting a shift toward minimally invasive techniques.
Table 2
| Author | Patient details | Chief complaint | Pancreatic enzyme levels | Diagnosis | Fish bone size (cm) | Site of perforation | Treatment |
|---|---|---|---|---|---|---|---|
| Goh et al. (20) | 60 Y/O, F | Epigastric discomfort for 2 weeks | N/A | CT | 3.0 | Stomach | Laparotomy |
| Goh et al. (21) | 32 Y/O, M | Fever with chills and rigors for 5 days | − | CT | 3.0 | Duodenum | Laparotomy |
| Wang et al. (22) | 68 Y/O, M | Dull pain over the epigastric area for 4 weeks | − | CT | 2.3 | Stomach | Laparotomy |
| Chiu et al. (3) | 66 Y/O, F | Fever and chills, epigastric pain, and body weight loss of about 3 kilograms for 2 weeks | + | CT | N/A | Stomach | Laparotomy |
| Yasuda et al. (23) | 73 Y/O, F | Persistent upper abdominal dull pain for 3 days | − | CT | 4.0 | Duodenum | Laparotomy |
| Symeonidis et al. (24) | 57 Y/O, F | Midepigastric pain, nausea, and vomiting for 1 day | + | Contrast-enhanced CT | N/A | Duodenum | Laparotomy |
| Huang et al. (6) | 53 Y/O, F | Intermittent, dull epigastric pain for 3 months, worsening abdominal pain and fever for 2 days | N/A | CT | 3.2 | Stomach | Laparotomy |
| Wang et al. (25) | 65 Y/O, M | Recurrent upper abdominal pain and gradual weight loss for 2 months | − | CT | 3.0 | Stomach | Laparotomy |
| Mima et al. (26) | 80 Y/O, M | Epigastric pain for 1 day | − | CT | 2.5 | Stomach | Laparoscopic surgery |
| Xie et al. (27) | 32 Y/O, M | Abdominal pain over 5 days | − | Endoscopic ultrasonography and CT | 3.5 | Stomach | Laparoscopic surgery |
| Attila et al. (28) | 76 Y/O, M | Epigastric pain for 2 days | N/A | CT | 3.5 | Duodenum | Endoscopic removal |
| Mulita et al. (29) | 59 Y/O, F | Fever and epigastric pain for 2 days | − | CT | 3.0 | Stomach | Laparoscopic surgery |
| Wang et al. (30) | 67 Y/O, M | Abdominal pain over 3 months | − | Bone condition CT | 3.2 | Stomach | Laparoscopic surgery |
| Sharma et al. (14) | 64 Y/O, M | Epigastric pain for two days | + | CT | 3.3 | Stomach | Endoscopic removal |
| Wu et al. (4) | 49 Y/O, F | Worsening dull epigastric pain for over 2 months, general soreness, and fever for 2 days | − | Contrast-enhanced CT | 4 | Stomach | Laparoscopic surgery |
| Our case | 85 Y/O, M | Epigastric pain for 3 days | − | Contrast-enhanced CT | 2.1 | Stomach | Endoscopic removal |
Reported cases of pancreatic injury induced by accidental ingestion of fish bone.
M, male; F, female; +, outside normal limits; −, within normal limits.
In our case, altered anatomy (Billroth II anatomy) may predispose to fish bone retention and migration. Post-surgical adhesions likely facilitated transmural penetration into the pancreas. In addition, fish bone migration as a physical trauma leads to parenchymal cell damage in the pancreas, where intracellular contents, including damage-associated molecular patterns, are released into the extracellular area and trigger a local inflammatory cascade (e.g., TLR4/NF-κB activation) by binding to Toll-like receptors and other pattern recognition receptors, further leading to pancreatic parenchymal injury and abscess formation (15–17). Moreover, depending on the trajectory of the foreign body, the fish bone can be located in different organs, including the small intestine, retroperitoneum, and liver. For instance, a case of an ingested fish bone at the caudate lobe has also been described (18).
Medical treatment of acute pancreatitis includes fluid resuscitation, reduction of pancreatic fluid secretion, and control of inflammation. If conservative treatment is not effective, the cause of the disease should be found and removed as early as possible by endoscopy or surgery. Once a foreign body is diagnosed, such as a fish bone, the choice of laparotomy or laparoscopic surgery or endoscopic treatment depends on the length, location, and complications of the fish bone. Endoscopic removal has the advantages of being less invasive, less painful, and easier to perform and is therefore preferred in most patients. A small percentage of patients may develop complications such as abdominal abscesses and require surgery. Laparoscopy also offers a magnified view and better visualization of the lesser sac, which could lead to less invasive approaches, especially for high-risk patients such as an 85-year-old patient. Probably, this should be the first approach, but the patient had previous upper gastrointestinal surgery, and potentially there were adhesions in the area. If there is evidence that part of the hyperdense foreign body is in the lumen of the stomach, then obviously an endoscopic removal should be the optimal approach. In certain circumstances, effective drainage and infection control can also facilitate patient recovery when a fish bone is not easily accessible, as it may become encapsulated by human tissue and remain dormant. Katsuhiko Horii et al. documented a case of a hepatic abscess resulting from fish bone penetration. Percutaneous abscess drainage was performed under ultrasonographic guidance. Following drainage, the patient became afebrile, and imaging findings demonstrated that the abscess cavity had decreased in size (19). It is worth noting that if minimally invasive drainage proves insufficient, surgery serves as the definitive treatment.
4 Conclusion
When we see a patient with normal amylase AP, we should consider not only whether it is severe pancreatitis, but also whether it is caused by alcoholic, hypertriglyceridemic or a foreign body, such as the fish bone mentioned in this case. A history of accidental ingestion of fish bone is important, and CECT is indispensable for early diagnosis. Endoscopic removal, when feasible, offers a safer alternative to laparotomy.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Huzhou Central Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YW: Conceptualization, Writing – original draft. YQ: Data curation, Writing – original draft. WH: Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Zhejiang Chinese Medical University Education and Teaching Reform Project (No. YB24012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Lee PJ Papachristou GI . New insights into acute pancreatitis. Nat Rev Gastroenterol Hepatol. (2019) 16:479–96. doi: 10.1038/s41575-019-0158-2
2.
Szatmary P Grammatikopoulos T Cai W Huang W Mukherjee R Halloran C et al . Acute pancreatitis: diagnosis and treatment. Drugs. (2022) 82:1251–76. doi: 10.1007/s40265-022-01766-4
3.
Chiu Y-H How C-K Chen J-D . Fish bone-induced pancreatitis. Clin Gastroenterol Hepatol. (2010) 8:e27. doi: 10.1016/j.cgh.2009.09.037
4.
Wu Y-J Chen Y-Y Hsieh Y-C . Unusual pancreatic abscess secondary to embedded fish bone: a challenging clinical scenario. Diagnostics. (2022) 12:2999. doi: 10.3390/diagnostics12122999
5.
Yen H-H Hsu Y-C . Education and imaging: gastrointestinal: pyogenic liver abscess associated with a penetrating fish bone. J Gastroenterol Hepatol. (2010) 25:1900. doi: 10.1111/j.1440-1746.2010.06551.x
6.
Huang Y-H Siao F-Y Yen H-H . Pre-operative diagnosis of pancreatic abscess from a penetrating fish bone. QJM. (2013) 106:955–6. doi: 10.1093/qjmed/hcs166
7.
Banks PA Freeman ML . Practice guidelines in acute pancreatitis. Am J Gastroenterol. (2006) 101:2379–400. doi: 10.1111/j.1572-0241.2006.00856.x
8.
Working Party of the British Society of gastroenterology, Association of Surgeons of Great Britain and Ireland, pancreatic Society of Great Britain and Ireland, Association of Upper GI surgeons of Great Britain and Ireland, UK guidelines for the management of acute pancreatitis. Gut. (2005) 54:iii1–9. doi: 10.1136/gut.2004.057026
9.
Banks PA Bollen TL Dervenis C Gooszen HG Johnson CD Sarr MG et al . Acute pancreatitis classification working group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. (2013) 62:102–11. doi: 10.1136/gutjnl-2012-302779
10.
Yadav D Pitchumoni CS . Issues in hyperlipidemic pancreatitis. J Clin Gastroenterol. (2003) 36:54–62. doi: 10.1097/00004836-200301000-00016
11.
Ismail OZ Bhayana V . Lipase or amylase for the diagnosis of acute pancreatitis?Clin Biochem. (2017) 50:1275–80. doi: 10.1016/j.clinbiochem.2017.07.003
12.
Frossard J-L Steer ML Pastor CM . Acute pancreatitis. Lancet. (2008) 371:143–52. doi: 10.1016/S0140-6736(08)60107-5
13.
Wang Y-Y Qian Z-Y Jin W-W Chen K Xu X-D Mou Y-P et al . Acute pancreatitis with abdominal bloating and distension, normal lipase and amylase: a case report. Medicine (Baltimore). (2019) 98:e15138. doi: 10.1097/MD.0000000000015138
14.
Sharma N Zivari K Kaur A Kureshi A Mayer I . Fish bone-induced pancreatitis. Cureus. (2022) 14:e26191. doi: 10.7759/cureus.26191
15.
Hoque R Malik AF Gorelick F Mehal WZ . Sterile inflammatory response in acute pancreatitis. Pancreas. (2012) 41:353–7. doi: 10.1097/MPA.0b013e3182321500
16.
Vaz J Akbarshahi H Andersson R . Controversial role of toll-like receptors in acute pancreatitis. World J Gastroenterol. (2013) 19:616–30. doi: 10.3748/wjg.v19.i5.616
17.
Chen X Ji B Han B Ernst SA Simeone D Logsdon CD . NF-kappaB activation in pancreas induces pancreatic and systemic inflammatory response. Gastroenterology. (2002) 122:448–57. doi: 10.1053/gast.2002.31060
18.
Kehagias D Mulita F Maroulis I Benetatos N . Caudate lobe: the last barrier - an unusual place for a foreign body. ANZ J Surg. (2022) 92:1218–1220. doi: 10.1111/ans.17226
19.
Horii K Yamazaki O Matsuyama M Higaki I Kawai S Sakaue Y . Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today. (1999) 29:922–6. doi: 10.1007/BF02482788
20.
Goh BKP Jeyaraj P-R Chan H-S Ong H-S Agasthian T Chang KTE et al . A case of fish bone perforation of the stomach mimicking a locally advanced pancreatic carcinoma. Dig Dis Sci. (2004) 49:1935–7. doi: 10.1007/s10620-004-9595-y
21.
Goh BKP Yong W-S Yeo AWY . Pancreatic and hepatic abscess secondary to fish bone perforation of the duodenum. Dig Dis Sci. (2005) 50:1103–6. doi: 10.1007/s10620-005-2712-8
22.
Wang W-L Liu K-L Wang H-P . Clinical challenges and images in GI. Pancreatic abscess resulting from a fish bone penetration of the stomach. Gastroenterology. (2008) 135:1865, 2160. doi: 10.1053/j.gastro.2008.10.067
23.
Yasuda T Kawamura S Shimada E Okumura S . Fish bone penetration of the duodenum extending into the pancreas: report of a case. Surg Today. (2010) 40:676–8. doi: 10.1007/s00595-009-4110-x
24.
Symeonidis D Koukoulis G Baloyiannis I Rizos A Mamaloudis I Tepetes K . Ingested fish bone: an unusual mechanism of duodenal perforation and pancreatic trauma. Case Rep Gastrointest Med. (2012) 2012:308510. doi: 10.1155/2012/308510
25.
Wang W-G Zhang Y Wang L Chen Y Tian B-L . Chronic pancreatic inflammatory granuloma caused by foreign body presenting as a pancreatic pseudotumor: a case report and literature review. Pancreatology. (2015) 15:573–5. doi: 10.1016/j.pan.2015.05.474
26.
Mima K Sugihara H Kato R Matsumoto C Nomoto D Shigaki H et al . Laparoscopic removal of an ingested fish bone that penetrated the stomach and was embedded in the pancreas: a case report. Surg Case Rep. (2018) 4:149. doi: 10.1186/s40792-018-0559-4
27.
Xie R Tuo B-G Wu H-C . Unexplained abdominal pain due to a fish bone penetrating the gastric antrum and migrating into the neck of the pancreas: a case report. World J Clin Cases. (2019) 7:805–8. doi: 10.12998/wjcc.v7.i6.805
28.
Attila T Mungan Z . Fish bone penetrating into the head of pancreas in a patient with Billroth II Gastrojejunostomy. GE Port J Gastroenterol. (2019) 26:221–2. doi: 10.1159/000489720
29.
Mulita F Papadopoulos G Tsochatzis S Kehagias I . Laparoscopic removal of an ingested fish bone from the head of the pancreas: case report and review of literature. Pan Afr Med J. (2020) 36:123. doi: 10.11604/pamj.2020.36.123.23948
30.
Wang Y Luo X Zhang J . Successful laparoscopic treatment for sustained abdominal pain due to fish bone migrating into the neck of the pancreas: a case report and thinking about surgical approach through the literature review. Surg Case Rep. (2021) 7:91. doi: 10.1186/s40792-021-01174-y
Summary
Keywords
fish bone, pancreatitis, foreign body, perforation, endoscopic removal
Citation
Wei Y, Qian Y and He W (2025) Case Report: A rare cause of pancreatitis - fish bone. Front. Med. 12:1645292. doi: 10.3389/fmed.2025.1645292
Received
11 June 2025
Revised
12 October 2025
Accepted
04 November 2025
Published
14 November 2025
Volume
12 - 2025
Edited by
Akira Andoh, Shiga University of Medical Science, Japan
Reviewed by
Ming Yuan Tan, Khoo Teck Puat Hospital, Singapore
Dimitrios Kehagias, University of Patras, Greece
Updates
Copyright
© 2025 Wei, Qian and He.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weimei He, heweimei1030@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.