Abstract
Objective:
This study aimed to explore the clinical characteristics, treatment determinants, and outcomes of elderly patients with sharp esophageal foreign bodies (EFBs) in Wuhan, China.
Method:
We conducted a retrospective analysis of 58 elderly patients (≥65 years) with sharp EFBs treated at Wuhan Central Hospital from January 2017 to June 2023. Patients were allocated to either an endoscopic (n = 43) or surgical (n = 15) treatment group based on clinical severity. We analyzed demographics, EFB type, injury severity, pre-hospital delay, laboratory findings, length of hospital stay, and functional outcomes using the Barthel Index. Statistical comparisons, including effect sizes and 95% confidence intervals, were performed, and a multivariable logistic regression analysis was conducted to identify independent predictors for surgical intervention.
Results:
No significant differences were observed in baseline demographics (p > 0.05). Fish bones (60.3%) were the most common EFB. Factors significantly associated with requiring surgical treatment included longer pre-hospital delay (median 3.0 vs. 0.5 days, p < 0.001), presence of fever (60.0% vs. 4.7%, p < 0.001), leukocytosis (46.7% vs. 16.3%, p = 0.031), dysphagia (20.0% vs. 2.3%, p = 0.041), and pre-existing esophageal diseases (53.3% vs. 14.0%, p = 0.004). All patients in the surgical group had esophageal perforation or a peri-esophageal abscess, compared to only 25.6% in the endoscopic group (p < 0.001). Multivariable analysis identified pre-hospital delay (OR 2.55, 95% CI [1.29–5.04]) and presence of fever at admission (OR 15.8, 95% CI [3.01–82.9]) as independent predictors for surgery. Endoscopic treatment was associated with a significantly shorter hospital stay (mean 4.3 vs. 13.7 days, p < 0.001) and superior functional recovery at discharge (p = 0.008) and 1 month post-procedure (p < 0.001).
Conclusion:
Delayed medical consultation, severe complications like perforation and abscess, and underlying esophageal comorbidities are key factors necessitating surgical intervention for sharp EFBs in the elderly. Fever at admission and pre-hospital delay are strong independent predictors of the need for surgery. Prompt diagnosis and endoscopic management, when feasible, are associated with shorter hospitalizations and better functional outcomes.
Introduction
Esophageal foreign body (EFB) is a common emergency in otolaryngology and thoracic surgery. Delayed diagnosis or improper treatment can cause serious complications, including death (1, 2). The causes of EFB ingestion are multifactorial and closely related to the patient’s age, eating habits, mental status, and underlying diseases (3, 4). Additionally, pre-existing esophageal lesions, such as stenosis, cancer, or motility disorders, increase the risk of impaction. EFBs are particularly prevalent in the elderly and children (5, 6). Elderly individuals often experience cognitive decline, tooth loss, weakened swallowing functions, and decreased mucosal sensation, making them susceptible to accidental ingestion of foreign objects like dislodged dentures or poorly chewed food (7). While children typically ingest blunt objects, sharp EFBs in adults are more likely to damage the esophagus, causing perforation and other severe complications, thus requiring more urgent treatment (8).
The complications of EFBs arise from direct injury to the esophagus and adjacent structures in the neck, chest, and mediastinum (9). The spectrum of complications is wide, with the most feared being an aortoesophageal fistula, which can cause fatal hemorrhage (10). Therefore, a thorough understanding of the clinical characteristics of EFBs and prompt, accurate diagnosis are crucial for effective treatment and improved prognosis. This article presents a retrospective study of the clinical features, treatment modalities, and outcomes of sharp EFBs in elderly patients in the Wuhan area, aiming to provide a theoretical basis for optimizing diagnosis and treatment selection in this vulnerable population.
Materials and methods
Patient population
We retrospectively reviewed the clinical data of patients admitted with sharp EFBs to Wuhan Central Hospital between January 2017 and June 2023. A patient flowchart is provided in Figure 1. Inclusion criteria were: (1) Patients aged ≥65 years old. (2) Diagnosis of a sharp EFB (defined as a hard object with sharp edges) confirmed by digestive endoscopy or computed tomography (CT) scan after admission. (3) The foreign body remained impacted in the esophagus during treatment. (4) The patient or their family provided consent for treatment. Exclusion criteria were: (1) No EFB identified on imaging or endoscopy. (2) Patient withdrew from or refused treatment. All patients or their families in this study signed informed consent forms. This study was reviewed and approved by the Ethics Committee of Wuhan Central Hospital (No. WHZXKYL2023-185).
Figure 1

Flowchart of patient selection for the study.
Study groups and data collection
After screening, a total of 58 patients were included in the final analysis. Patients were divided into an endoscopic treatment group (n = 43) and a surgical treatment group (n = 15) based on their presenting clinical severity and the presence of complications.
Diagnostics
Upon presentation, a detailed history of foreign body ingestion was recorded. All patients underwent diagnostic imaging to confirm the diagnosis. In our cohort, 5 patients (8.6%) underwent a barium meal examination, all 58 patients (100%) had a CT scan, and 53 patients (91.4%) underwent digestive endoscopy for diagnosis or treatment. Body temperature and white blood cell count were monitored to assess for infection. Based on imaging, endoscopy, and surgical findings, the degree of esophageal injury was classified as mucosal injury, ulcer, perforation, or peri-esophageal abscess.
Treatments
The decision to proceed with endoscopic or surgical treatment was made by a multidisciplinary team including the attending thoracic surgeon and endoscopist based on a comprehensive clinical evaluation. Generally, endoscopic removal was the first-line approach for all patients. Surgical intervention was indicated for patients who met one or more of the following criteria, indicating severe clinical conditions: (1) Radiological evidence of esophageal perforation with extraluminal contamination (e.g., mediastinitis, para-esophageal abscess, or significant pneumomediastinum); (2) Clinical signs of sepsis or hemodynamic instability; (3) Failure of endoscopic removal, defined as the inability to safely dislodge and extract the foreign body without causing further esophageal injury; or (4) High suspicion of major vascular injury based on preoperative CT imaging. All endoscopic procedures were performed by senior endoscopists with at least 10 years of experience, using standard flexible gastroscopes (Olympus GIF-Q260J). The choice of endoscopic removal tool (e.g., foreign-body forceps, snare, or basket) was at the discretion of the endoscopist based on the EFB’s shape, size, and location. To ensure safe extraction and protect the esophageal mucosa and pharynx from injury during retrieval, a protective overtube was used at the discretion of the endoscopist, particularly for larger or irregularly shaped sharp objects. Endoscopic failure, which necessitated conversion to surgery, was documented in cases where the foreign body could not be visualized, grasped, or safely removed without significant risk of mucosal tearing or perforation, as judged by the attending endoscopist. For patients undergoing successful endoscopic treatment, post-procedural management depended on the extent of esophageal injury. Patients with minor mucosal damage were managed with a liquid diet, while those with suspected or contained perforation without significant infection received nasogastric tube feeding. Surgical treatment involved foreign body removal, esophageal repair, debridement of abscesses, and placement of drainage tubes, with additional interventions as needed for complications.
Analysis indicators
The analysis indicators included: (1) Basic patient information: age, gender, comorbidities. (2) Admission-related indicators: EFB type, degree of esophageal injury, fever (axillary temperature >37.3 °C), white blood cell count (normal range: 3.5–9.5 × 109/L), time from onset to admission, hospital stay, and pain score (Visual Analogue Scale). Pre-existing esophageal-related diseases included conditions such as esophageal stenosis, a history of esophageal cancer (post-treatment, no active disease), or severe reflux esophagitis. Abnormal swallowing function was primarily identified by the clinical symptom of dysphagia, as reported in the patient’s history. (3) Quality of life comparison: We compared the functional status (Barthel Index total score) between the two groups at admission, at discharge, and 1 month post-procedure. The Barthel Index was used to assess the impact of the event and treatment on patients’ functional independence in activities of daily living (ADL), a critical outcome in geriatric populations. While not a direct measure of disease-specific quality of life, it provides valuable insight into the broader functional recovery (11).
Statistical analysis
Data analysis was conducted using SPSS 23.0 software. Normally distributed data are expressed as mean ± standard deviation (Mean ± SD) and compared using an independent sample t-test. Non-normally distributed data are represented by the median (interquartile range, IQR) and compared using the Mann–Whitney U test. Count data are expressed as n (%) and compared using the chi-square test or Fisher’s exact test. Effect sizes were calculated: odds ratios (OR) with 95% confidence intervals (CI) for categorical data, Cohen’s d for t-tests, and Rosenthal’s r for non-parametric comparisons. To identify independent predictors of requiring surgical treatment, a binary logistic regression analysis was performed. Variables that were statistically significant in the univariate analysis (p < 0.05) were included in the multivariable model. A p-value <0.05 was considered statistically significant.
Results
Types of foreign bodies
The types of sharp objects included jujube pits, fish bones, bullfrog bones, poultry bones, and pig bones. Fish bones (n = 35, 60.3%) and jujube pits (n = 15, 25.9%) were the most common. The incidence rates of bullfrog bones, poultry bones, and pig bones were 2 (3.4%), 4 (6.9%), and 2 (3.4%), respectively (examples are shown in Figure 2).
Figure 2
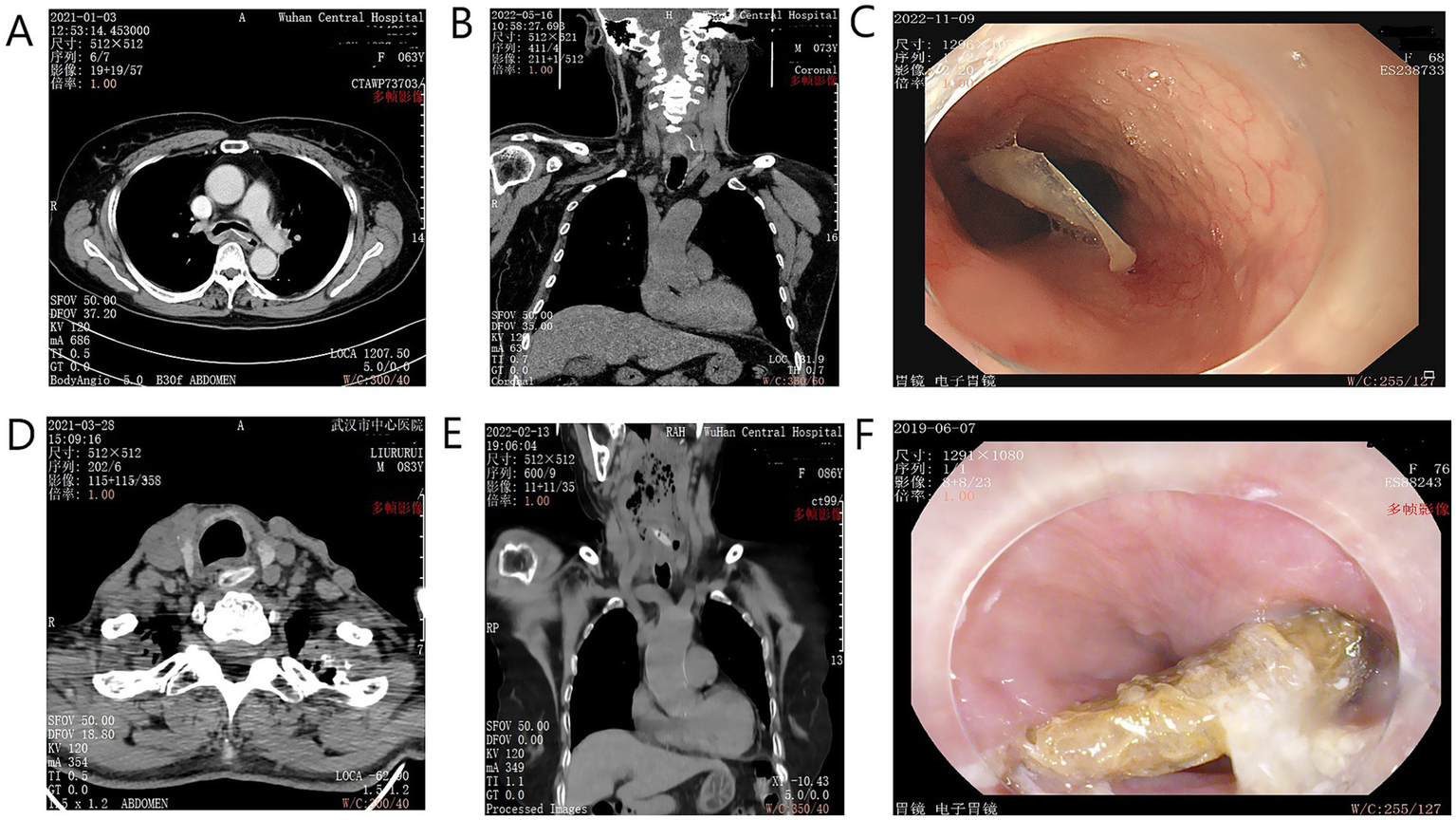
Examples of sharp foreign bodies identified by CT and endoscopy. (A) Axial CT scan showing a fish bone penetrating the esophageal wall. (B) Coronal CT view of a similar injury. (C) Endoscopic view of an impacted fish bone. (D) Axial CT showing a jujube pit in the cervical esophagus. (E) Coronal CT view of an impacted jujube pit causing peri-esophageal inflammation. (F) Endoscopic view of a large, impacted jujube pit.
Baseline characteristics and clinical presentation
The baseline characteristics of the 58 patients are compared in Table 1. There were no significant demographic differences between groups (p > 0.05). However, patients in the surgical group had a significantly longer median pre-hospital delay compared to the endoscopic group [3.00 (IQR 1.00, 4.00) days vs. 0.50 (IQR 0.19, 1.00) days; p < 0.001]. A significantly higher proportion of patients in the surgical group presented with fever (60.0% vs. 4.7%; p < 0.001) and an abnormal white blood cell count (46.7% vs. 16.3%; p = 0.031) at admission.
Table 1
| Index | Endoscopic treatment group (n = 43) | Surgical treatment group (n = 15) | Statistic (Z/χ2) | p-value | Effect size (OR/r) [95% CI] |
|---|---|---|---|---|---|
| Gender (Female, %) | 25 (58.1) | 11 (73.3) | 0.981 | 0.431 | 1.94 [0.48, 7.78] |
| Age (years, median [IQR]) | 70.0 [67.0, 80.0] | 68.0 [66.0, 71.0] | −0.512 | 0.609 | – |
| Time from onset to admission (days, median [IQR]) | 0.50 [0.19, 1.00] | 3.00 [1.00, 4.00] | −3.651 | <0.001 | −0.48 |
| Fever upon admission (Yes, %) | 2 (4.7) | 9 (60.0) | 18.411 | <0.001 | 29.25 [5.41, 158.1] |
| WBC count upon admission (abnormal, %) | 7 (16.3) | 7 (46.7) | 4.640 | 0.031 | 4.36 [1.20, 15.82] |
| Residence (city, %) | 14 (32.6) | 7 (46.7) | 0.864 | 0.353 | 1.81 [0.55, 5.96] |
| Education level (junior high or less, %) | 28 (65.1) | 14 (93.3) | 4.321 | 0.109 | – |
Comparison of baseline demographic and clinical characteristics between the endoscopic and surgical treatment groups.
Data are presented as n (%), median (IQR), or mean ± SD. Statistical comparisons were made using the Mann–Whitney U test, chi-square test, or Fisher’s exact test. OR, Odds Ratio; CI, Confidence Interval; r, Rosenthal’s r effect size for Mann–Whitney U test. p-values in bold are statistically significant.
Differences in EFB location, injury severity, and treatment
Sharp object impaction occurred most frequently in the upper esophagus in both groups, with no significant difference in location (p > 0.05) (Table 2). The median pain score was significantly higher in the surgical group [3.00 (IQR 3.00, 3.00)] compared to the endoscopic group [2.00 (IQR 1.00, 3.00); p = 0.003]. The effect size (Rosenthal’s r = −0.39) indicates a medium-sized effect, where the negative correlation signifies that the surgical group (coded as the higher value group) was associated with higher pain scores. There was a significant difference in esophageal injury severity: all 15 patients (100%) in the surgical group had esophageal perforation or a peri-esophageal abscess, compared to only 11 of 43 patients (25.6%) in the endoscopic group (p < 0.001) (Table 2). Among the 15 surgical cases, 5 underwent right thoracotomy, 7 required a cervical incision after failed endoscopic attempts, and 3 had other surgical approaches.
Table 2
| Index | Endoscopic treatment group (n = 43) | Surgical treatment group (n = 15) | Statistic (Z/χ2) | p-value | Effect size (r) |
|---|---|---|---|---|---|
| EFB position | 0.311 | 0.856 | – | ||
| Upper esophagus | 28 (65.1%) | 10 (66.7%) | |||
| Middle esophagus | 14 (32.6%) | 5 (33.3%) | |||
| Lower esophagus | 1 (2.3%) | 0 (0%) | |||
| Pain score (VAS, median [IQR]) | 2.00 [1.00, 3.00] | 3.00 [3.00, 3.00] | −2.940 | 0.003 | −0.39 |
| Damage degree (Perforation/Abscess, %) | 11 (25.6%) | 15 (100%) | 20.342 | <0.001 | - |
Differences in EFB location and injury severity between the two patient groups.
Data are presented as n (%) or median (IQR). p-values in bold are statistically significant.
Correlation of dental status and comorbidities with treatment selection
There were no significant differences in dental status between the groups (p > 0.05) (Table 3). However, comorbidities were strongly associated with treatment selection. Patients requiring surgery were significantly more likely to have pre-existing esophageal-related diseases (53.3% vs. 14.0%; p = 0.004) or present with dysphagia (20.0% vs. 2.3%; p = 0.041) compared to those managed endoscopically (Table 4).
Table 3
| Index | Endoscopic treatment group (n = 43) | Surgical treatment group (n = 15) | Statistic (Z/χ2) | p-value |
|---|---|---|---|---|
| Number of teeth (median [IQR]) | 22.0 [12.0, 26.0] | 24.0 [18.0, 28.0] | −0.731 | 0.465 |
| Tooth loss (Yes, %) | 37 (86.0%) | 11 (73.3%) | 1.237 | 0.268 |
| Fixed partial denture (Yes, %) | 17 (39.5%) | 6 (40.0%) | 0.003 | 0.955 |
| Removable dentures (Yes, %) | 13 (30.2%) | 2 (13.3%) | 1.758 | 0.317 |
Comparison of dental status between the two patient groups.
Data are presented as n (%) or median (IQR).
Table 4
| Index | Endoscopic treatment group (n = 43) | Surgical treatment group (n = 15) | Statistic (χ2) | p-value | OR [95% CI] |
|---|---|---|---|---|---|
| Esophageal-related comorbidities (Yes, %) | 6 (14.0%) | 8 (53.3%) | 8.211 | 0.004 | 6.67 [1.81, 24.51] |
| Dysphagia (Yes, %) | 1 (2.3%) | 3 (20.0%) | 4.175 | 0.041 | 10.64 [1.02, 110.6] |
Comparison of comorbidities and dysphagia between the two patient groups.
Data are presented as n (%). p-values in bold are statistically significant.
Multivariable analysis of predictors for surgical treatment
To identify independent predictors for requiring surgical intervention, a binary logistic regression analysis was performed. The variables included were pre-hospital delay, fever at admission, abnormal WBC count, dysphagia, and pre-existing esophageal disease. The analysis, summarized in Table 5, revealed that a longer pre-hospital delay (OR 2.55, 95% CI [1.29–5.04]; p = 0.007) and the presence of fever at admission (OR 15.8, 95% CI [3.01–82.9]; p = 0.001) were significant independent predictors for the necessity of surgical treatment. Other factors did not retain statistical significance in the multivariable model.
Table 5
| Variable | Odds ratio (OR) | 95% confidence interval (CI) | p-value |
|---|---|---|---|
| Pre-hospital delay (per day increase) | 2.55 | 1.29–5.04 | 0.007 |
| Fever at admission (Yes vs. No) | 15.8 | 3.01–82.9 | 0.001 |
| Abnormal WBC count (Yes vs. No) | 2.10 | 0.52–8.45 | 0.298 |
| Pre-existing esophageal disease (Yes vs. No) | 3.45 | 0.88–13.5 | 0.075 |
| Dysphagia (Yes vs. No) | 4.02 | 0.35–46.1 | 0.261 |
Multivariable logistic regression analysis of predictors for surgical treatment.
WBC, White Blood Cell. p-values in bold are statistically significant.
Post-treatment outcomes and follow-up
All patients were discharged without major complications. As shown in Table 6, endoscopic treatment was associated with a significantly shorter hospital stay (mean 4.30 vs. 13.73 days; mean difference −9.43, 95% CI for difference [−12.50, −6.36]; p < 0.001, Cohen’s d = −2.18). While functional status at admission was similar between groups (p = 0.429), the endoscopic group had significantly higher Barthel Index scores at discharge (mean 89.53 vs. 76.00; mean difference 13.53, 95% CI [3.78, 23.28]; p = 0.008) and at 1 month post-procedure (mean 100.00 vs. 97.00; mean difference 3.00, 95% CI [1.88, 4.12]; p < 0.001). At the 6-month follow-up, four patients in the surgical group reported minor residual symptoms (e.g., occasional dysphagia or retrosternal discomfort), compared to two in the endoscopic group. All symptomatic patients underwent a follow-up gastroscopy, which revealed mild esophageal mucosal inflammation without evidence of stenosis or residual foreign bodies; they were managed conservatively with proton pump inhibitors.
Table 6
| Index | Endoscopic treatment group (n = 43) | Surgical treatment group (n = 15) | Statistic (t) | p-value | Effect size (Cohen’s d) [95% CI for difference] |
|---|---|---|---|---|---|
| Duration of hospitalization (days, mean ± SD) | 4.30 ± 2.05 | 13.73 ± 6.20 | −8.912 | <0.001 | −2.18 [−12.5, −6.3] |
| Barthel Index Score (mean ± SD) | |||||
| At admission | 70.12 ± 24.51 | 75.00 ± 19.63 | −0.796 | 0.429 | – |
| At discharge | 89.53 ± 14.89* | 76.00 ± 20.02 | 2.845 | 0.008 | 0.79 [3.8, 23.3] |
| 1 month after discharge | 100.00 ± 0.00* | 97.00 ± 4.55* | 4.701 | <0.001 | 1.31 [1.9, 4.1] |
Comparison of post-treatment outcomes between the two patient groups.
Data are presented as mean ± SD. *p < 0.05 compared with the score at admission within the same group. p-values in bold are statistically significant.
Discussion
Management of sharp EFBs in the elderly presents a significant clinical challenge due to age-related comorbidities and the high risk of severe complications. This study provides valuable insights by identifying key predictors for surgical intervention in this vulnerable population. Our principal finding is that pre-hospital delay and the presence of fever on admission are strong, independent predictors of the need for surgery, a conclusion strengthened by our multivariable analysis. These findings underscore the critical importance of early presentation and diagnosis in improving outcomes.
This study has several limitations that must be acknowledged. As a single-center, retrospective analysis, it is susceptible to selection bias. The small sample size, especially in the surgical group (n = 15), limits the statistical power for detecting smaller effect sizes and compromises the robustness of the multivariable analysis, underscoring the need for validation in larger, multicenter cohorts. The use of the Barthel Index, while useful for assessing general functional recovery, is not a specific measure of post-esophageal intervention quality of life. Despite these limitations, our study provides valuable clinical insights into managing a high-risk condition in a vulnerable population.
EFBs are common in the elderly for several reasons, including dulled mucosal sensation, poor dentition leading to inadequate chewing, and underlying esophageal or neurological conditions that impair swallowing (11–13). Timely removal is the cornerstone of EFB management. Endoscopic removal is the preferred first-line treatment due to its minimally invasive nature and high success rate, reported to be between 92.5 and 98.9% (1, 14, 15). However, for patients with severe complications like large perforation, mediastinitis, or systemic sepsis, surgery becomes necessary. Choosing the appropriate treatment is especially critical in elderly patients to minimize morbidity.
Our data strongly suggest that the primary drivers for surgical intervention are the development of severe complications like perforation and infection. This was confirmed by our finding that all patients in the surgical group had perforation or abscess and is further supported by our multivariable analysis, which identified pre-hospital delay and fever as strong, independent predictors of needing surgery. Delayed presentation is a critical factor; prolonged impaction (>24 h) is a known risk factor for esophageal perforation, with complication rates increasing significantly over time (16, 17). Our findings align with this, showing that delayed medical attention leads to a higher likelihood of complications necessitating surgery.
Pre-existing esophageal diseases and dysphagia were also associated with surgical treatment in our univariate analysis. Elderly patients with underlying swallowing difficulties may not recognize the symptoms of an EFB, leading to delayed diagnosis until severe symptoms like odynophagia develop, by which time a perforation may have already occurred. In contrast, dental status had little impact on treatment selection in our cohort, likely because the main EFBs were small items like fish bones and jujube pits rather than large dentures (18, 19).
Endoscopic treatment is the preferred modality for uncomplicated EFBs due to its safety and efficacy (20, 21). Recent guidelines continue to emphasize early endoscopic intervention to prevent the progression to more severe complications that would mandate surgical intervention (22). Surgery is reserved for complex cases with complications like abscesses or major vessel injury (23). While life-saving, surgical treatment is associated with longer hospitalization, higher costs, and more significant postoperative pain, as demonstrated in our study.
The predominance of fish bones and jujube pits in our study is likely linked to local dietary habits in Wuhan and may not be generalizable to other regions. Provided there are no contraindications, early endoscopy should be performed to remove such objects. Even in cases of small perforations without abscesses, endoscopic management followed by conservative care can be sufficient.
Conclusion
Delayed medical consultation, severe complications such as perforation and abscess formation, and pre-existing esophageal conditions are key determinants that necessitate surgical intervention for sharp EFBs in the elderly population. Fever at admission and longer pre-hospital delay are strong independent predictors of the need for surgery. Prompt diagnosis and endoscopic management, when clinically appropriate, are associated with significantly shorter hospital stays, reduced morbidity, and better functional outcomes. Therefore, we recommend prompt CT evaluation and endoscopic intervention for elderly patients with suspected sharp EFBs to prevent complications. Future large-scale, prospective studies are warranted to confirm these predictors and explore the utility of specific quality-of-life instruments in this population.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Wuhan Central Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JX: Data curation, Formal analysis, Investigation, Writing – original draft. BC: Data curation, Formal analysis, Investigation, Writing – original draft. YL: Conceptualization, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
EFBs, Esophageal Foreign Bodies; CT, Computed Tomography; ADL, Activities of Daily Living; Mean ± SD, Mean ± Standard Deviation; IQR, Interquartile Range; OR, Odds Ratio; CI, Confidence Interval.
References
1.
Huang Y Lu T Liu Y Zhan C Ge D Tan L et al . Surgical management and prognostic factors in esophageal perforation caused by foreign body. Esophagus. (2019) 16:188–93. doi: 10.1007/s10388-018-0652-6
2.
Zong Y Zhao H Sun C Ji M Wu Y Zhang S et al . Differences between intentional and accidental ingestion of foreign body in China. BMC Gastroenterol. (2020) 20:90. doi: 10.1186/s12876-020-01224-z
3.
Fang Y Qin Z . Comparison of endoscopy alone with surgery converted from endoscopy for the removal of esophageal foreign bodies in adults: a retrospective study from a single center. Med Sci Monit. (2021) 27:e929142. doi: 10.12659/MSM.929142
4.
Takeno S Ishii H Nanashima A Nakamura K . Aortoesophageal fistula: review of trends in the last decade. Surg Today. (2020) 50:1551–9. doi: 10.1007/s00595-019-01937-z
5.
Alsayegh R Hudson T Gurberg J . Pediatric patient with persistent postoperative fevers after esophageal foreign body removal. JAMA Otolaryngol Head Neck Surg. (2024) 150:75–6. doi: 10.1001/jamaoto.2023.3366
6.
Fung BM Sweetser S . Wong Kee song LM, Tabibian JH: foreign object ingestion and esophageal food impaction: an update and review on endoscopic management. World J Gastrointest Endosc. (2019) 11:174–92. doi: 10.4253/wjge.v11.i3.174
7.
Mi X Li Z . Esophageal disease. In: MuZFangJ, editors. Practical otorhinolaryngology – head and neck surgery: Diagnosis and treatment. Singapore: Springer Singapore (2021). 285–92.
8.
Suzuki T Shimada H . [Esophageal foreign body]. Kyobu geka. Jpn J Thorac Surg. (2022) 75:895–900.
9.
Sagvand BT Najafali D Yardi I Sahadzic I Afridi L Kohler A et al . Emergent endoscopy for esophageal foreign body removal: the impact of location. Cureus. (2022) 14:e21929. doi: 10.7759/cureus.21929
10.
Hu K Chen G Hu D . Removal of an esophageal foreign body under real-time miniprobe endoscopic ultrasound guidance. Dig Endosc. (2022) 34:e145–6. doi: 10.1111/den.14399
11.
Soni A Roy R Gupta Y . Esophageal foreign bodies in pediatric age group with different durations of time from ingestion to effective treatment. Indian J Otolaryngol Head Neck Surg. (2023) 75:1421–8. doi: 10.1007/s12070-023-03578-8
12.
Schaefer TJ Trocinski D . Esophageal foreign body. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC. (2025)
13.
Alturkmani OG Al-Badawi MM Alturkmani SG Al-Midani MH Attar SA . A case report of non-intentional foreign body ingestion in an elderly patient. Cureus. (2023) 15:e37684. doi: 10.7759/cureus.37684
14.
Wu DQ Chen SY Chen KG Wang T Li GY Huang XS . Factors influencing the fasting time in adult patients after the endoscopic Management of Sharp Esophageal Foreign Bodies. Ther Clin Risk Manag. (2024) 20:39–45. doi: 10.2147/TCRM.S451517
15.
Liao F Zhu Z Pan X Li B Zhu Y Chen Y et al . Safety and efficacy of nonoperative treatment in esophageal perforation caused by foreign bodies. Clin Transl Gastroenterol. (2022) 13:e00451. doi: 10.14309/ctg.0000000000000451
16.
Zhang S Wen J Du M Liu Y Zhang L Chu X et al . Diabetes is an independent risk factor for delayed perforation after foreign bodies impacted in esophagus in adults. United European Gastroenterol J. (2018) 6:1136–43. doi: 10.1177/2050640618784344
17.
Chirica M Kelly MD Siboni S Aiolfi A Riva CG Asti E et al . Esophageal emergencies: WSES guidelines. World J Emerg Surg. (2019) 14:26. doi: 10.1186/s13017-019-0245-2
18.
Harale M Oommen A Faruqi AA Mundada M Pancholi T Yammanuru B et al . Cross-sectional study comparing activities of daily living using Barthel index within a geriatric population having non-communicable diseases. Cureus. (2024) 16:e65046. doi: 10.7759/cureus.65046
19.
Zhang X Jiang Y Fu T Zhang X Li N Tu C . Esophageal foreign bodies in adults with different durations of time from ingestion to effective treatment. J Int Med Res. (2017) 45:1386–93. doi: 10.1177/0300060517706827
20.
Rammohan R Joy M Natt D Saggar T Magam SG Gomez S et al . Navigating the esophagus: effective strategies for foreign body removal. Cureus. (2023) 15:e38593. doi: 10.7759/cureus.38593
21.
Demiroren K . Management of gastrointestinal foreign bodies with brief review of the guidelines. Pediatr Gastroenterol Hepatol Nutr. (2023) 26:1–14. doi: 10.5223/pghn.2023.26.1.1
22.
Wei DH Liu W . Clinical research Progress of foreign bodies in digestive tract. Clin Res Clin Trials. (2022) 6:01–6. doi: 10.31579/2693-4779/093
23.
Syamal MN . Adult Esophageal Foreign Bodies. Otolaryngol Clin N Am. (2024) 57:609–21. doi: 10.1016/j.otc.2024.01.003
Summary
Keywords
esophagus, foreign body, elderly, endoscopy, surgery, outcomes
Citation
Xu J, Chen B and Liu Y (2025) Clinical outcomes of sharp esophageal foreign bodies in elderly patients: a retrospective study from Wuhan, China. Front. Med. 12:1653609. doi: 10.3389/fmed.2025.1653609
Received
25 June 2025
Accepted
26 September 2025
Published
28 October 2025
Volume
12 - 2025
Edited by
Marios Kyriazis, National Gerontology Centre, Cyprus
Reviewed by
Suat Evirgen, Amasya University, Türkiye
Rajkiran Srinivas Raju, Department of Pediatric Surgery, India
Updates
Copyright
© 2025 Xu, Chen and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Liu, liuyong1@zxhospital.com
†ORCID: Yong Liu, orcid.org/0000-0002-4048-5837
Baojun Chen, orcid.org/0000-0002-3497-698X
Jiahang Xu, orcid.org/0000-0001-9282-2084
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.