Abstract
We present a case of a 28-year-old female patient who has suffered from hemoptysis for a period of 10 years. Examinations revealed an anomalous celiac aorta supply to normal basal segment of the lung. The patient was improved after embolisation with a vascular plug. This case demonstrates the deadly risk posed by anomalous systemic arterial supply to normal basal segments of the lung. As a minimally invasive procedure, transarterial embolization (TAE) is a safe and effective therapeutic choice.
Introduction
An anomalous celiac aorta supply to normal basal segment of the lung is an uncommon congenital anomaly. This condition is characterized by the presence of an anomalous artery originating from the celiac aorta, which supplies to normal basal lung segment. Patients frequently present with symptoms such as hemoptysis, chest discomfort, recurrent infections, or congestive heart failure secondary to pulmonary hyperperfusion or hypertension. The primary interventions employed in the management of this condition include surgical procedures and transarterial embolization (TAE). The present case report documents a successful management strategy for this vascular anomaly, employing the Amplatzer vascular plug (AVP) II embolization technique.
Case description
A 28-year-old female patient with a ten-year history of recurrent haemoptysis was transferred to our hospital. She had previously been diagnosed with bronchiectasis on multiple occasions at other medical facilities, despite undergoing treatment for both infection and haemostasis. She’s married with no children and no history of smoking. A physical examination revealed no abnormalities in her breathing or heart sounds. A comprehensive blood examination was conducted, encompassing various parameters including blood routine, liver and kidney function, and coagulation function. The results showed that the patient’s blood profile was normal. Computed tomography (CT) scan of the chest revealed thickening of the left lower pulmonary vein(Figure 1A). Subsequent computed tomography angiography (CTA) revealed an anomalous arterial branch arising from the celiac aorta,which originated at the T12-L1 level (Figures 1B–D). Angiographic examinations confirmed the presence of an anomalous artery originating from the celiac aorta. The diagnosis of anomalous celiac aorta supply to normal basal segments of the lung was thereby confirmed. Further diagnostic procedures were performed, including echocardiography. The results indicated a mean pulmonary artery pressure of 21 mmHg (normal range: 9–18 mmHg). There was no evidence of dilatation in the right atrium or right ventricle, nor of any observable enlargement of the pulmonary artery.
Figure 1

(A) CT of the chest showed thickening of the left lower pulmonary vein. (B–D) CTA showed bronchi in the blood supply area originating from the normal left lower pulmonary bronchi, and the pulmonary vein of the left lower hilar is thickened. The thick branch of the celiac aorta supplied part of the basal segments of the lung through the diaphragm (yellow arrow).
Following the presentation of treatment options, which included surgery, observation, or TAE, the patient opted for the latter due to its minimally invasive nature (Figure 2). Pre-procedural management encompassed a 3-day course of intravenous dexamethasone (5 mg daily) and antibiotics to prevent pulmonary infarction or infected necrosis. Subsequent to embolisation, the patient exhibited resolution of hemoptysis and chest discomfort, with discharge occurring on post-procedural day5.
Figure 2
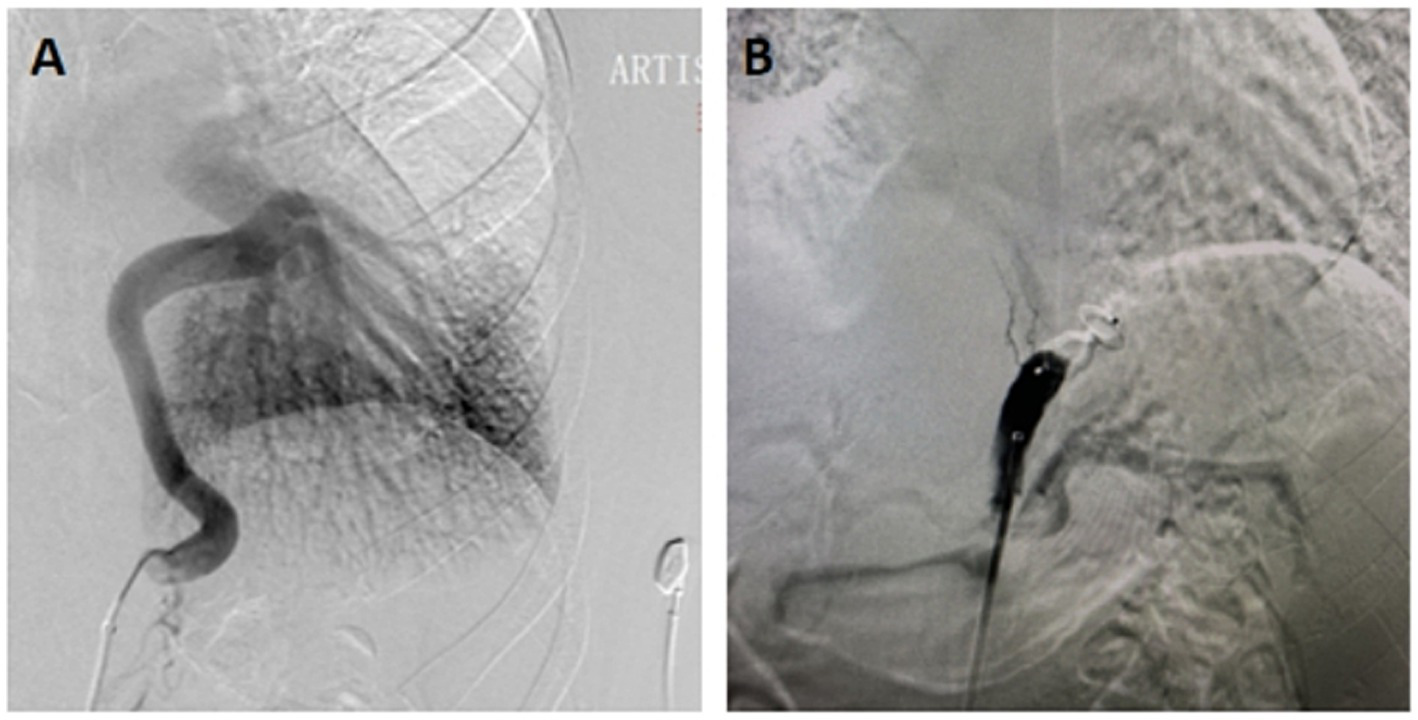
(A) Angiography showed a large supply arising from the celiac aorta to normal basal segments of the lung. (B) After proximal arterial embolization with AVP, a aortogram showed occlusion of the celiac aorta.
Discussion
Anomalous celiac aorta supply to normal basal segments of the lung was previously classified as type 1 pulmonary sequestration according to Pryce’s terminology since 1946 (1). This is a extremly rare congenital vascular malformation and most scholars consider this anomaly to differ from classic sequestration because of the normal bronchial connection (2). The subject is characterized by an anomalous systemic artery, drainage to the normal pulmonary vein, absence of the normal pulmonary artery, and no anomaly of the bronchus. The aetiology of this anomaly remains unclear, although it may be related to persistence of an embryonic connection between the aorta and pulmonary parenchyma (3).
Advances in imaging technology have enabled the definitive diagnosis of this anomaly through visualization of the pulmonary vasculature, bronchi, and parenchyma. Angiography further provides a haemodynamic assessment and evaluation of the shunt. This congenital malformation predominantly affects the left basal lung segment, typically manifesting as a solitary aberrant vessel originating from the left descending thoracic aorta. It is an uncommon occurrence for the congenital abnormality to be located in the right basal segment of the lung (4). In such cases, there is often an association with two or more anomalous arteries arising from either the proximal celiac aorta or the celiac trunk. Among the cases reported to date, only two were of this origin (5, 6). Our patient represents the third rare case. The most common clinical symptoms include hemoptysis, as was the case in the present instance. Furthermore, there have been reports of extensive hemoptysis resulting in death while the patient was under observation (7). In addition, there are literature reports on the clinical manifestations of dyspnoea, chest pain, recurrent infection and congestive heart failure (8). In our case, the patient presented with repeated episodes of hemoptysis and was misdiagnosed with bronchiectasis for a period of ten years. If not treated in a timely manner, this anomalous systemic artery-to-pulmonary vein drainage creates a left-to-left shunt, which can lead to progressive pulmonary hypertension, massive hemoptysis, and eventual heart failure. It is particularly pertinent to note that the likelihood of exacerbation of hemoptysis is increased during pregnancy (9).
The treatment of this abnormality is recommended for symptomatic or asymptomatic patients due to the risk of congestive heart failure in children and hemoptysis in adults (10). The main treatment has been surgical excision, such as lung lobectomy, ligation, or division of the anomalous artery. TAE is a procedure that shares similarities with surgical ligation as a treatment for this anomaly, yet it is a less invasive procedure. In recent years, an increasing number of cases have been selected for embolisation treatment (11–13). The necessity of endovascular treatment was determined as a means of averting the progression of pulmonary hypertension and the potential for sudden death from extensive hemoptysis. The utilisation of mechanical embolisation agents, encompassing coils, detachable balloons, Amplatzer occlusion devices and Amplatzer vascular plugs (AVPs), constitutes a viable approach for this purpose (14). However,the utilisation of liquid embolisation materials is not advised due to the elevated risk of extensive embolisation, which can potentially result in pulmonary embolisation and pulmonary infarction. Previous studies have demonstrated the efficacy of coils and AVPs in the embolisation of the ascending aorta. Jiang et al. conducted a comprehensive evaluation of various embolisation methodologies, juxtaposing the progression of embolisation techniques and embolisation agents through the course of time (14). The study concluded that the detachable AVP surpasses the utilisation of multiple coils in terms of efficacy for the embolisation of the ascending aorta. Consequently, this methodology was adopted, yielding positive outcomes; however, further observation is warranted to ensure long-term stability.
In summary, TAE represents a minimally invasive, safe, and effective approach for managing anomalous systemic arterial supply to pulmonary basal segments, with no major complications observed. It may thus serve as a primary alternative to surgical intervention. Periodic contrast-enhanced CT follow-up remains essential to monitor potential recanalization or hemoptysis recurrence from compensatory systemic collaterals.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZL: Data curation, Investigation, Project administration, Writing – original draft, Writing – review & editing. RW: Investigation, Software, Validation, Writing – original draft. YN: Formal Analysis, Funding acquisition, Visualization, Writing – review & editing. DX: Investigation, Methodology, Supervision, Writing – original draft. JN: Conceptualization, Methodology, Project administration, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Wuhan Science and Technology Bureau (NO. 2023020201020543).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Pryce DM . Lower accessory pulmonary artery with intralobar sequestration of lung: a report of seven cases. J Pathol Bacteriol. (1946) 58:457–67.
2.
Mori S Odaka M Asano H Marushima H Yamashita M Kamiya N et al . Anomalous systemic arterial supply to the basal segments of the lung: feasible thoracoscopic surgery. Ann Thorac Surg. (2013) 96:990–4. doi: 10.1016/j.athoracsur.2013.04.099
3.
Giancaspro G Hahn L Hsiao A Kligerman SJ . Anomalous systemic arterial supply to normal basal segments of the lung. Radiol Cardiothorac Imaging. (2022) 4:e220029. doi: 10.1148/ryct.220029
4.
Akiba T Marushima H Kamiya N Odaka M Kinoshita S Takeyama H et al . Anomalous systemic arterial supply to the basal segments of the lung with three aberrant arteries. Gen Thorac Cardiovasc Surg. (2012) 60:118–21. doi: 10.1007/s11748-011-0778-0
5.
Jiang S Shi JY Zhu XH Chen C Sun XW Yu D et al . Endovascular embolization of the complete type of anomalous systemic arterial supply to normal basal lung segments: a report of four cases and literature review. Chest. (2011) 139:1506–13. doi: 10.1378/chest.10-1022
6.
Iijima Y Ishikawa M Iwai S Motono N Usuda K Morinaga M et al . Role of indocyanine green in anomalous arterial supply to the normal dorsobasal segment of the lung. J Cardiothorac Surg. (2022) 17:52. doi: 10.1186/s13019-022-01791-0
7.
Rubin EM Garcia H Horowitz MD Guerra JJ Jr . Fetal massive hemoptysis secondary to intralobar sequestration. Chest. (1994) 106:954–5.
8.
Ebihara M Fujimori S Suzuki S Yotsumoto T Kikunaga S Ohtsuka R et al . Anomalous systemic arterial supply to the left basal lung with a calcified abnormal vessel: a case report. Surg Case Rep. (2022) 8. Published 2022 Jun 22:121. doi: 10.1186/s40792-022-01469-8
9.
Hawke K Joshi K Lau H Halder A Duncan P Wolski P . Anomalous systemic arterial supply to the basal segment of the lung presenting with haemoptysis in the third trimester of pregnancy. Obstet Med. (2024) 17:53–7. doi: 10.1177/1753495X221125975
10.
Ema T Neyatani H Yamamoto S Iizuka S Yasuda K Funai K et al . Anomalous systemic arterial supply to the basal lung segments with high serum carbohydrate antigen 19-9 levels-a case report. AME Case Rep. (2021) 5:3. Published 2021 Jan 25. doi: 10.21037/acr-20-35
11.
Kuroda Y Morita K Toyoshima Y Kamei N Hatakeyama T . Anomalous systemic arterial supply to the basal segment of the left lung: the role of balloon occlusion pulmonary angiography. Pediatr Int. (2023) 65:e15451. doi: 10.1111/ped.15451
12.
Kim JH Kim SS Ha KS Bae J Park Y . Anomalous arterial supply to normal basal segment of the right lower lobe: endovascular treatment with the Amplatzer vascular plug. Tuberc Respir Dis. (2014) 76:295–8. doi: 10.4046/trd.2014.76.6.295
13.
Hatakeyama T Homma T Otsubo K Sakai H Kimura H Miyazawa T et al . Anomalous systemic arterial supply to the basal segment of the lung (ABLL) in the right lower lobe: preoperative embolization and Thoracoscopic surgery. Cureus. (2025) 17:e82152. doi: 10.7759/cureus.82152
14.
Jiang S Yu D Jie B . Transarterial embolization of anomalous systemic arterial supply to Normal basal segments of the lung. Cardiovasc Intervent Radiol. (2016) 39:1256–65. doi: 10.1007/s00270-016-1361-y
Summary
Keywords
anomalous celiac aorta supply to normal basal segment of the lung, hemoptysis, transarterial embolization, Amplatzer vascular plug, case report
Citation
Li Z, Wang R, Niu Y, Xia D and Ni J (2025) Anomalous celiac aorta supply to normal basal segments of the lung: a case report. Front. Med. 12:1655687. doi: 10.3389/fmed.2025.1655687
Received
28 June 2025
Accepted
22 September 2025
Published
03 October 2025
Volume
12 - 2025
Edited by
Mehmet Ali Bedirhan, Yedikule Teaching Hospital, Türkiye
Reviewed by
Yunus Seyrek, Yedikule Teaching Hospital, Türkiye
Antonio Borzelli, Hospital Antonio Cardarelli, Italy
Updates
Copyright
© 2025 Li, Wang, Niu, Xia and Ni.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jixiang Ni, jxnee77@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.