- 1Mental Health Center, West China Hospital, Sichuan University, Chengdu, China
- 2Clinical Medicine College of Southwest Medical University, Luzhou, China
Chronic cough in adults is commonly caused by respiratory disorders (e.g., cough variant asthma, CVA), ear, nose and throat (ENT) disorders (e.g., postnasal drip), digestive disorders (e.g., gastroesophageal reflux disease, GERD), as well as anaphylaxis and allergy. Tic cough is infrequent in adults but warrants consideration in individuals who have excluded these somatic disorders and exhibit inadequate response to diagnostic treatments, especially those with a history of tic disorder or ongoing tic symptoms. In these cases, a multi-disciplinary treatment (MDT) for chronic cough that includes psychiatrists is recommended as the optimal management approach.
Background
Chronic cough is known as a respiratory symptom that lasts more than 8 weeks (1), is often a burdensome condition which is commonly caused by respiratory disorders such as cough variant asthma (CVA), ear, nose and throat (ENT) disorders, digestive disorders, anaphylaxis and allergy (2–11), and features complex causes and leads to insomnia, anxiety, and other symptoms (12–17). About 40% of adults with chronic cough referred for specialist evaluation have persistent cough despite optimal treatment of conditions associated with chronic cough, known as refractory chronic cough (RCC) (18). RCC is a disorder of the brain and the respiratory system (19), in 2020, recent data from tertiary cough specialist clinics have reported prevalence rates up to 60% (20). Currently gabapentin is the first choice in pharmacologic treatment (21). Even after various tests and treatments, it is still difficult to consider the possibility of tic cough (22). Tic cough is a type of vocal tic in tic disorders (23, 24). Tic cough can be characterized by coughing, throat clearing and so on due to the momentary activation of local muscles in the laryngeal part of the pharynx (12). A case of an adult with a tic cough was found in a chronic cough MDT which is reported below.
Case description
A 32-year-old male presented with a cough 11 years ago after catching a cold in winter, which manifested as a sudden, explosive, persistent dry cough with occasional thin white sputum. He consulted ENT, respiratory medicine, traditional Chinese medicine (TCM), cough specialist outpatient, and other departments, he had been diagnosed with “rhinitis, asthma, upper airway cough syndrome, intractable cough, chronic cough, chronic nonatrophic gastritis (CNAG), and reflux esophagitis,” and he had been treated with loratadine, budesonide for 2 months, antibiotics (He had no recollection of the names or uses of the antibiotics he had taken. He claimed to have undergone chest CT scans at different hospitals prior to taking the medication and said the results were normal.), gabapentin, omeprazole, mosapride and Chinese medicine, which did not relieve the cough. He has never smoked, works in a healthy environment, and has no history of exposure to dust or heavy metals. He had COVID-19 pneumonia in 2022, and he continued to cough after the pneumonia resolved. In addition, he reported that the cough was more pronounced when he focused on it. Gastroscopy was performed 4 years prior, which suggested superficial gastritis and a duodenal bulbar ulcer (stage A2). After regular treatment with proton pump inhibitors, another gastroscopy in the following year suggested CNAG. Eighteen months ago, the individual consulted different departments in the hospital. Chest high-resolution CT revealed a few small inflammatory nodules in both lungs; the pulmonary function test revealed an FEV1/FVC% of 76.93%, with moderate airflow limitation in the small airways and slightly impaired lung function; the results of the bronchial provocation test (BPT), fractional exhaled nitric oxide (FENO: 14 ppb) and allergen tests were negative; and lymphocyte and total IgE levels were normal according to routine blood tests. Sixteen months ago, he received MDT for chronic cough, which involves pneumology, gastroenterology, ENT, allergology, integrated traditional and western medicine, and psychiatry physicians.
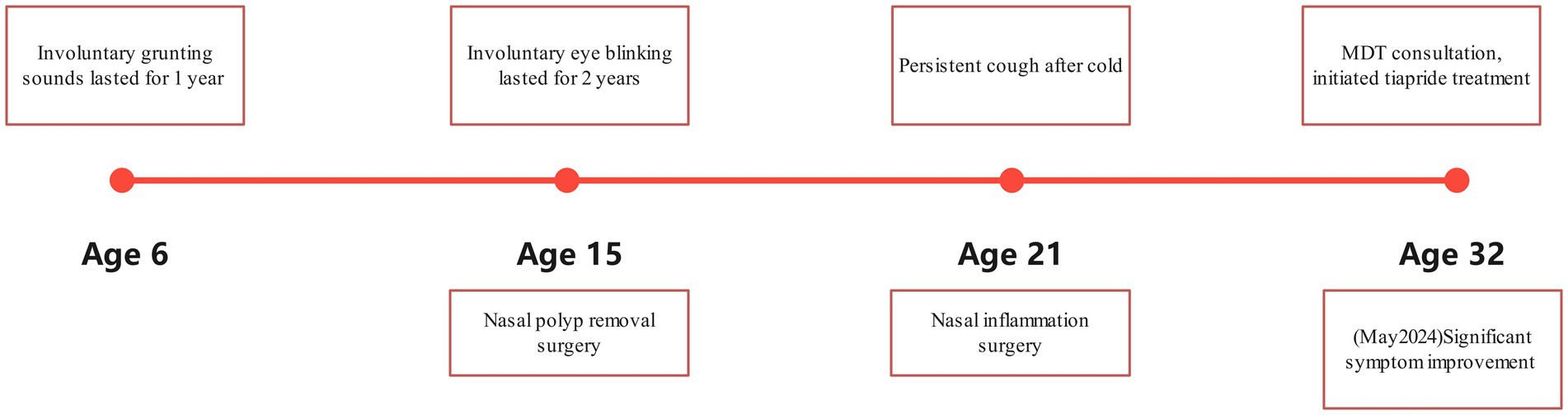
The MDT ruled out organic disorders and found that he used to have frequent blinking, involuntary head turning, and coughing approximately once a minute for 1–2 s each time, which was similar to “throat clearing.” Psychiatric assessment revealed no depression, anxiety, or insomnia. Past history included involuntary grunting at age 6 (duration: 1 year) and involuntary blinking exacerbated by electronic screens at age 15 (duration: 2 years), previously diagnosed as Tourette syndrome (TS) at a local hospital and resolving post-medication. Notably, the patient’s father had a history of involuntary blinking and unexplained coughing between ages 30–45 years, resolving spontaneously without intervention (Figure 1). During the MDT consultation, the patient was identified and diagnosed with tic disorder by a psychiatrist and recommended the use of medication, and the diagnosis and treatment plan was affirmed and supported by other MDT specialists (respiratory medicine, otolaryngology, gastroenterology). The MDT facilitator then informed the patient of the diagnosis and treatment plan, and the patient expressed agreement and accepted the psychiatrist’s diagnosis and treatment plan.
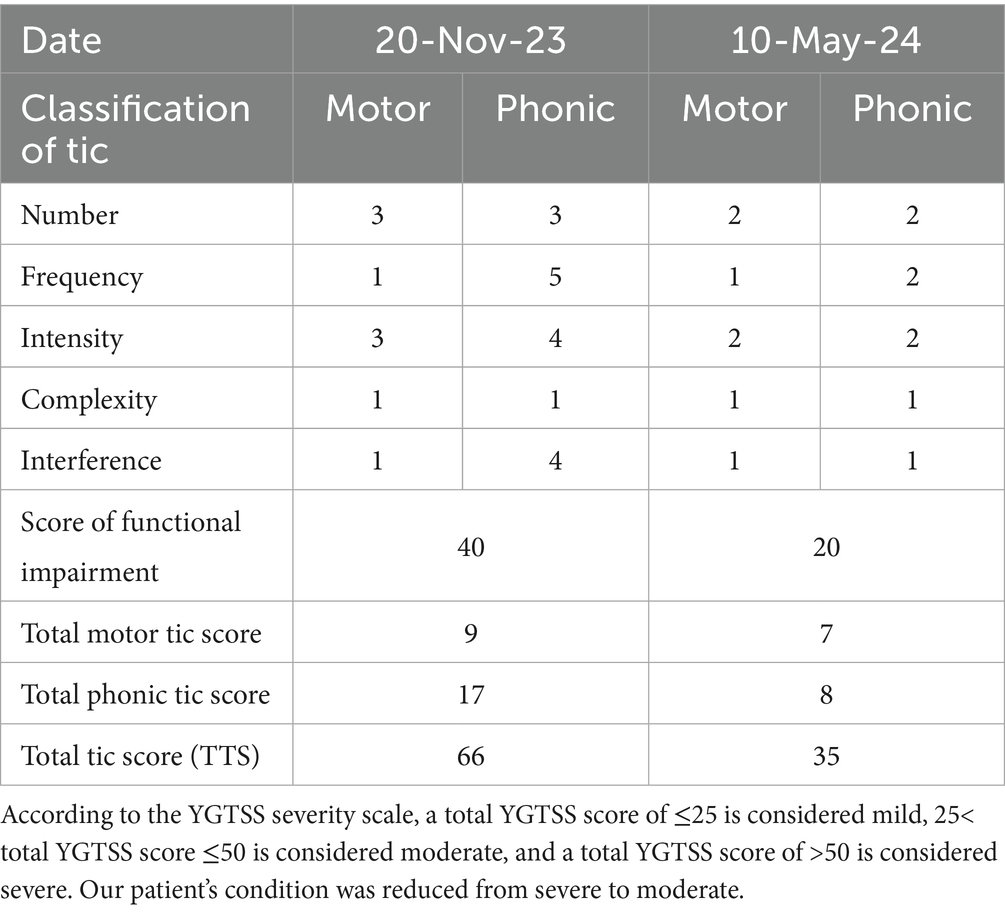
Tic cough was considered by the MDT, he scored 66 on the Yale Global Tic Severity Scale (YGTSS), the MDT strictly followed the first-line drug guidelines for the treatment of tic disorder, using the most commonly used clinical dopamine receptor antagonists (anti-psychotics), tiapride hydrochloride which was given 0.1 g orally three times daily (tid). Mild symptom improvement at 1 month prompted dose escalation to 0.2 g tid, yielding significant cough reduction. However, bothersome daytime somnolence affecting work led to self-reduction back to 0.1 g tid. At 5 months, the YGTSS score improved to 35 (Table 1), but persistent daytime fatigue prompted self-discontinuation after 7 months, resulting in cough recurrence matching pretreatment severity. Re-initiation of tiapride hydrochloride subsequently improved symptoms again. Leicester cough questionnaire (LCQ) score is used to evaluate the effect of cough on quality of life, the patient’s LCQ score from 65 to 108, the lower the score, the more serious the impact of chronic cough on quality of life is.
Discussion
Tic is caused by a pathological enhancement of the motor program driven by abnormally elevated dopaminergic neurotransmission (25, 26). Tic disorders are often diagnosed at ages 4–8 years and are most commonly diagnosed at ages 8–12 years. The condition is predominantly observed in males and typically improves progressively during adolescence and early adulthood (27, 28). Motor tics usually precede vocal tics. Simple motor tics in the earliest stages involve the face, head, or neck (27), such as facial twitching, eye blinking, frowning, head shaking, neck twisting and shoulder shrug. Vocal tics are characterized by sudden, involuntary vocalizations, such as imitating coughing, sneezing, or throat clearing, as well as grunts and wheezes (24, 29). Cough-like symptoms caused by vocal tics are clinically referred to as tic coughs (22). Maria et al. reported that individuals with tic cough accounted for approximately 6% of all children referred for prolonged or recurrent cough (30), and classical antipsychotics are effective against this symptom (31). In China, children with tic-associated coughs, characterized primarily by throat-clearing sounds, are commonly misdiagnosed with respiratory conditions such as postnasal drip syndrome (PNDS) and CVA (32–37). The neuropathological mechanism of tic cough is currently unknown, some of the literature suggests that Tourette’s syndrome is associated with chronic cough, manifested by tic and abnormal corpus callosum (38, 39), further research is required in the future.
Tic disorder symptoms are characterized by recurrence and variability. Consistent with prior research, tic symptoms are highly variable and fluctuate over time (27), with symptom frequency typically decreasing by late adolescence or young adulthood (40–42). However, tics may still recur in adulthood. Sara M. et al. reported 16 individuals with a childhood diagnosis of TS who reemerged with tics in adulthood, with an average latency of 16 years (40). Klawans et al. reported four individuals who presented with a variety of motor and vocal tics before the age of 9 years, with tics resolving completely by the age of 20 years but recurring after the age of 60 years (28). The onset of tic disorders, which are often first observed in children and adolescents, has also been reported in adulthood. However, first episodes in adulthood are much less common than relapses (43–45). Chouinard S et al. conducted a study on 411 individuals with tic disorders and reported that 22 of them first presented with tic disorders after the age of 21 years. A careful review of their medical history further confirmed that 9 had a history of transient tic disorder in childhood, whereas the other 13 had a new onset of tic disorders in adulthood (41). However, few reports on tic cough in adults exist. Esther et al. reported a 27-year-old male with chronic cough that was not treated for 1 year and was successfully treated with low-dose haloperidol after psychiatric consultation (46).
The 2015 CHEST Expert Guidelines recommend replacing the diagnostic terms “habit cough” and “somatic cough” with “tic cough” and “psychogenic cough,” respectively. The term “somatic cough” should be replaced by “psychogenic cough” (22). Tic cough rarely occurs in adulthood. When standard investigations reveal no abnormality and targeted therapies prove ineffective in adults with chronic cough, tic disorders should be considered, particularly in those with a history of tics or concurrent tic symptoms. A chronic cough MDT team with psychiatrists is the optimal model to achieve this goal (47). The MDT is oriented to patients and supported by multidisciplinary experts, which not only provides patients with the best diagnosis and treatment plan (48–50) but also effectively reduces the waste of medical resources (51).
Conclusion
The possibility of tic cough should be considered in adults with chronic cough, and MDT involving psychiatrists can make a surprising effective.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval were not required for the study of human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients or patients' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the patient for the publication of this case report.
Author contributions
WY: Validation, Writing – original draft. ZQ: Writing – review & editing, Supervision, Data curation, Investigation. DL: Formal analysis, Visualization, Writing – review & editing. YM: Software, Methodology, Project administration, Resources, Writing – original draft. CQ: Funding acquisition, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was partly funded by the 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (grant no. 2022HXFH029) (CQ), and the Ministry of Science and Technology Department of the People’s Republic of China, STI2030-Major Projects (grant no. 2021ZD0200600) (CQ).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Morice, A, Dicpinigaitis, P, Mcgarvey, L, et al. Chronic cough: new insights and future prospects. Eur Respir Rev. (2021) 30:210127. doi: 10.1183/16000617.0127-2021
2. Lai, K, Tang, J, Zhan, W, Li, H, Yi, F, Long, L, et al. The spectrum, clinical features and diagnosis of chronic cough due to rare causes. J Thorac Dis. (2021) 13:2575–82. doi: 10.21037/jtd-20-2671
3. Irwin, RS, Glomb, WB, and Chang, AB. Habit cough, tic cough, and psychogenic cough in adult and pediatric populations: accp evidence-based clinical practice guidelines. Chest. (2006) 129:174s–9s. doi: 10.1378/chest.129.1_suppl.174S
4. Grinevica, A, Udre, A, Balodis, A, and Strumfa, I. Tic cough in an adolescent with organic brain pathology-a case report and literature review. Brain Sci. (2024) 14:79. doi: 10.3390/brainsci14010079
5. Spero, K, Bayasi, G, Beaudry, L, Barber, K, and Khorfan, F. Overdiagnosis of Copd in hospitalized patients. Int J Chron Obstruct Pulmon Dis. (2017) 12:2417–23. doi: 10.2147/COPD.S139919
6. Diab, N, Patel, M, O'byrne, P, et al. Narrative review of the mechanisms and treatment of cough in asthma, cough variant asthma, and non-asthmatic eosinophilic bronchitis. Lung. (2022) 200:707–16. doi: 10.1007/s00408-022-00575-6
7. Palombini, BC, Villanova, CA, Araújo, E, Gastal, OL, Alt, DC, Stolz, DP, et al. A pathogenic triad in chronic cough: asthma, postnasal drip syndrome, and gastroesophageal reflux disease. Chest. (1999) 116:279–84. doi: 10.1378/chest.116.2.279
8. Chang, AB, Lasserson, TJ, Gaffney, J, Connor, FL, and Garske, LA. Gastro-oesophageal reflux treatment for prolonged non-specific cough in children and adults. Cochrane Database Syst Rev. (2011) 2011:Cd004823. doi: 10.1002/14651858.CD004823.pub4
9. Everett, CF, Kastelik, JA, Thompson, RH, and Morice, AH. Chronic persistent cough in the community: a questionnaire survey. Cough. (2007) 3:5. doi: 10.1186/1745-9974-3-5
10. Yousaf, N, Montinero, W, Birring, SS, and Pavord, ID. The long term outcome of patients with unexplained chronic cough. Respir Med. (2013) 107:408–12. doi: 10.1016/j.rmed.2012.11.018
11. Koskela, HO, Lätti, AM, and Purokivi, MK. Long-term prognosis of chronic cough: a prospective, observational cohort study. BMC Pulm Med. (2017) 17:146. doi: 10.1186/s12890-017-0496-1
12. Gill, CE, and Kompoliti, K. Clinical features of Tourette syndrome. J Child Neurol. (2020) 35:166–74. doi: 10.1177/0883073819877335
13. Freeman, RD. Tic disorders and ADHD: answers from a world-wide clinical dataset on Tourette syndrome. Eur Child Adolesc Psychiatry. (2007) 16:15–23. doi: 10.1007/s00787-007-1003-7
14. Kurlan, R, Como, PG, Miller, B, Palumbo, D, Deeley, C, Andresen, EM, et al. The behavioral spectrum of tic disorders: a community-based study. Neurology. (2002) 59:414–20. doi: 10.1212/wnl.59.3.414
15. Lewin, AB, Chang, S, Mccracken, J, et al. Comparison of clinical features among youth with tic disorders, obsessive-compulsive disorder (Ocd), and both conditions. Psychiatry Res. (2010) 178:317–22. doi: 10.1016/j.psychres.2009.11.013
16. Robertson, MM, Trimble, MR, and Lees, AJ. The psychopathology of the Gilles de la Tourette syndrome. A phenomenological analysis. Br J Psychiatry. (1988) 152:383–90. doi: 10.1192/bjp.152.3.383
17. Virtanen, S, Sidorchuk, A, Fernández De La Cruz, L, et al. Association of Tourette Syndrome and Chronic tic Disorder with Subsequent Risk of alcohol- or drug-related disorders, criminal convictions, and death: a population-based family study. Biol Psychiatry. (2021) 89:407–14. doi: 10.1016/j.biopsych.2020.09.014
18. Gibson, P, Wang, G, Mcgarvey, L, et al. Treatment of unexplained chronic cough: chest guideline and expert panel report. Chest. (2016) 149:27–44. doi: 10.1378/chest.15-1496
19. Cho, PSP, and Turner, RD. Chronic refractory cough: a disorder of the brain and the respiratory system. Chest. (2022) 162:736–7. doi: 10.1016/j.chest.2022.06.005
20. Song, WJ, and Chung, KF. Pharmacotherapeutic options for chronic refractory cough. Expert Opin Pharmacother. (2020) 21:1345–58. doi: 10.1080/14656566.2020.1751816
21. Visca, D, Beghè, B, Fabbri, LM, Papi, A, and Spanevello, A. Management of chronic refractory cough in adults. Eur J Intern Med. (2020) 81:15–21. doi: 10.1016/j.ejim.2020.09.008
22. Vertigan, AE, Murad, MH, Pringsheim, T, Feinstein, A, Chang, AB, Newcombe, PA, et al. Somatic cough syndrome (previously referred to as psychogenic cough) and tic cough (previously referred to as habit cough) in adults and children: chest guideline and expert panel report. Chest. (2015) 148:24–31. doi: 10.1378/chest.15-0423
23. Leckman, JF. Phenomenology of tics and natural history of tic disorders. Brain Dev. (2003) 25:S24–8. doi: 10.1016/S0387-7604(03)90004-0
24. Saritha, D, and Elangovan, S. A case of vocal tics presented as chronic cough treated with risperidone. Indian J Psychiatry. (2023) 65:605–7. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_117_23
25. Maia, TV, and Conceição, VA. The roles of phasic and tonic dopamine in tic learning and expression. Biol Psychiatry. (2017) 82:401–12. doi: 10.1016/j.biopsych.2017.05.025
26. Leckman, JF, and Riddle, MA. Tourette's syndrome: when habit-forming systems form habits of their own? Neuron. (2000) 28:349–54. doi: 10.1016/S0896-6273(00)00114-8
27. Singer, HS. Tics and Tourette syndrome. Continuum (Minneap Minn). (2019) 25:936–58. doi: 10.1212/CON.0000000000000752
28. Klawans, HL, and Barr, A. Recurrence of childhood multiple tic in late adult life. Arch Neurol. (1985) 42:1079–80. doi: 10.1001/archneur.1985.04060100061023
29. Karakaya, I, and Şişmanlar, ŞG. Tic disorders in the differential diagnosis of chronic cough in children in relation to four cases. Turk Pediatri Ars. (2015) 50:176–9. doi: 10.5152/TurkPediatriArs.2015.1215
30. Mallet, MC, Elmiger, A, Glick, S, Krasnova, T, de Jong, CCM, Kern, B, et al. Diagnosis in children with prolonged or recurrent cough: findings from the Swiss Paediatric airway cohort. Pediatr Pulmonol. (2025) 60:e27499. doi: 10.1002/ppul.27499
31. Párraga, HC, Harris, KM, Párraga, KL, Balen, GM, and Cruz, C. An overview of the treatment of Tourette's disorder and tics. J Child Adolesc Psychopharmacol. (2010) 20:249–62. doi: 10.1089/cap.2010.0027
32. Zhang, X, and Zhou, H. Analysis of 28 cases of chronic cough misdiagnosis caused by tic disorder in children. Med. J. Commun. (2014) 28:1006–2440.
33. Tian, X, and Tian, X. Analysis of 48 cases of chronic cough caused by Tourette's syndrome. Chin J Misdiagn. (2010) 10:1009–6647.
34. Wang, M. Analysis of the misdiagnosis of 21 cases of chronic cough caused by Tourette's syndrome in children. Chin J Misdiagn. (2010) 10:1009–6647.
35. Yan, Y, Tang, J, and Ji, W. Clinical analysis of 24 cases of chronic cough caused by multiple tics. Chin J Pract Pediatr. (2009) 24:1005–2224.
36. Zhang, X. Clinical analysis of 33 cases of chronic cough caused by multiple tic disorders. Aerospace Med J. (2013) 24:443–4. doi: 10.3969/j.issn.2095-1434.2013.04.036
37. Liu, S, Gao, L, and Ma, C. Performance of chronic persistent cough in 31 children with Tourette. Pract J Pediatr Clin Med. (2012) 27:387–8. doi: 10.3969/j.issn.1003-515X.2012.05.028
38. Tan, H, Büyükavci, M, and Arik, A. Tourette's syndrome manifests as chronic persistent cough. Yonsei Med J. (2004) 45:145–9. doi: 10.3349/ymj.2004.45.1.145
39. Duncan, KL, and Faust, RA. Tourette syndrome manifest as chronic cough. Int J Pediatr Otorhinolaryngol. (2002) 65:65–8. doi: 10.1016/S0165-5876(02)00122-2
40. Schaefer, SM, Chow, CA, Louis, ED, and Robakis, D. Tic exacerbation in adults with Tourette syndrome: a case series. Tremor Other Hyperkinet Mov (NY). (2017) 7:450. doi: 10.5334/tohm.339
41. Eapen, V, Lees, AJ, Lakke, JP, et al. Adult-onset tic disorders. Mov Disord. (2002) 17:735–40. doi: 10.1002/mds.10180
42. Riegel, B, Warmoth, JE, Middaugh, SJ, Kee, WG, Nicholson, LC, Melton, DM, et al. Psychogenic cough treated with biofeedback and psychotherapy. A review and case report. Am J Phys Med Rehabil. (1995) 74:155–8.
43. Erenberg, G, Cruse, RP, and Rothner, AD. The natural history of Tourette syndrome: a follow-up study. Ann Neurol. (1987) 22:383–5. doi: 10.1002/ana.410220317
44. Shprecher, DR, Gannon, K, Agarwal, N, Shi, X, and Anderson, JS. Elucidating the nature and mechanism of tic improvement in Tourette syndrome: a pilot study. Tremor Other Hyperkinet Mov (NY). (2014) 4:217. doi: 10.5334/tohm.190
45. Groth, C, Mol Debes, N, Rask, CU, Lange, T, and Skov, L. Course of Tourette syndrome and comorbidities in a large prospective clinical study. J Am Acad Child Adolesc Psychiatry. (2017) 56:304–12. doi: 10.1016/j.jaac.2017.01.010
46. Kim, S, Greene, DJ, Bihun, EC, Koller, JM, Hampton, JM, Acevedo, H, et al. Provisional tic disorder is not so transient. Sci Rep. (2019) 9:3951. doi: 10.1038/s41598-019-40133-4
47. Şentürk Pilan, B, Özbaran, B, Çelik, D, Özcan, T, Özen, S, Gökşen, D, et al. Psychiatric view for disorders of sex development: a 12-year experience of a multidisciplinary team in a university hospital. J Pediatr Endocrinol Metab. (2020) 33:605–11. doi: 10.1515/jpem-2019-0513
48. Min, X, and Sun, P. Discussion on the multidisciplinary comprehensive treatment mode of malignant tumors in general hospitals. Proceeding of Clinical Medicine. (2021) 30:1671–8631.
49. Lu, Y, Yang, J, Chen, Y, and Jiang, L. Investigation and analysis on the development of multidisciplinary collaborative diagnosis and treatment mode in tertiary hospitals in China. Chin Hosp. (2021) 25:21–3. doi: 10.19660/j.issn.1671-0592.2021.2.07
50. Qin, L, He, Q, He, X, Liu, L, Huang, H, Dai, J, et al. Application and practice of multidisciplinary team service model in West China Hospital of Sichuan University. Chin J West China Med J. (2024) 39:88–92. doi: 10.7507/1002-0179.202304120
Keywords: chronic cough, tic disorder, tic cough, multidisciplinary treatment, psychiatric evaluation
Citation: Yang W, Qiu Z, Liu D, Meng Y and Qiu C (2025) Chronic tic cough in adults: a case report. Front. Med. 12:1657223. doi: 10.3389/fmed.2025.1657223
Edited by:
Antonio M. Esquinas, Hospital General Universitario Morales Meseguer, SpainReviewed by:
Made Agustya Darma Putra Wesnawa, Udayana University, IndonesiaYap Sing Yee, Putra Malaysia University, Malaysia
Copyright © 2025 Yang, Qiu, Liu, Meng and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changjian Qiu, cWl1Y2hhbmdqaWFuQHdjaHNjdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Wanjing Yang1†
Wanjing Yang1† Yajing Meng
Yajing Meng Changjian Qiu
Changjian Qiu