- 1The Center of Excellence in Low vision and Vision Rehabilitation, Eye Hospital of Wenzhou Medical University, Wenzhou, China
- 2National Clinical Research Center for Ocular Diseases, Wenzhou, Zhejiang, China
- 3The Optometry Center, The Quzhou Affiliated Hospital of Wenzhou Medical University, Quzhou People's Hospital, Quzhou, Zhejiang, China
Objective: To demonstrate public awareness of low vision rehabilitation (LVR) in China and identify related influencing factors.
Methods: This cross-sectional study assessed low vision rehabilitation awareness using a Delphi method validated questionnaire. The questionnaires were distributed through Vision China conferences (2022–2023) and representative hospitals in all provinces across China, targeting public and vision professionals.
Results: 1,482 questionnaires (360 were from visually impaired individuals) were collected, including 952 from the public and 530 from vision professionals. The mean total scores accounted for 37.0% and 55.6% of the maximum scores, respectively. For the public, individuals with higher education, good visual acuity, working in medical system, and having eye check yearly or more frequent were associated with better awareness of LVR. For vision professionals, participants aged over 40 years old, with better visual acuity, and knowing the low vision referral process demonstrated a better awareness of LVR. The main sources of LVR information for the public were doctors' advice (about 29%) and news media/online information (about 28%).
Discussion: The awareness of LVR in China is insufficient in both the public and vision professionals. Regular eye checks, doctors' advice, and scientific education are essential to improve the awareness of the public. It is crucial to develop low-vision education in the medical curriculum and expand low-vision continuing education and forums to improve awareness among vision professionals.
Introduction
The World Health Organization (WHO) adopts visual acuity in daily life as the criterion for assessing visual impairment, categorizing it into mild, moderate, severe visual impairment, and blindness. Low vision is categorized into moderate and severe visual impairment (1). According to the 2020 WHO vision report, 2.2 billion people in the world were visually impaired (2), among which 295 million were moderate to severe visual impairment (3). People with low vision usually have a decreased independence and quality of life (2, 4, 5). Low vision rehabilitation (LVR) could minimize the impact and improve the quality of life (6–8). Application of low vision aids, functional visual acuity training, skills training and psychological supports are all efficient methods for LVR (2, 4).
Besides the global initiative for the elimination of avoidable blindness, China Disabled Persons' Federation (CDPF) and National Health Commission of China have done lots of work to promote LVR services in China (9). The 13th 5-Year Plan of National Eye Health, released by National Health Commission of China, has stipulated that tertiary hospitals must set up low vision clinic and provide LVR services (10). With the efforts of the National Health Commission of China and CDPF, LVR services have been gradually improved during the past decades (11).
However, considering the large number of low vision population and relatively few vision professionals in China, only a very low proportion of people with low vision are actually receiving LVR services (12). One of the reasons is that the amount of ophthalmologists and optometrists is far less than enough. Another reason is suspected that the accessibility and availability of LVR services is not fully opened to the public. Many of the low-vision patients regretted not going to LVR clinics earlier, and many others refused to accept rehabilitation because of misunderstandings. Previous researches have revealed that the acceptance rate of low vision aids among elderly patients with visual impairment in Wenzhou, China was below 50%. Around 60% of the individuals with visual impairment still prefer to conventional refractive correction to improve their vision (13, 14).
The insufficient access and low acceptance of LVR in China demonstrated that cognitive blind spots or misunderstandings LVR exist in the public. With this in mind, this study was designed and conducted to demonstrate the current state and related factors of LVR awareness of the public in China. Then scientific education as well as low-vision training for the vision professionals would be targeted designed to improve the present situation.
Methods
Questionnaire design
A “Survey of public Awareness on Low Vision Rehabilitation in China” questionnaire was designed and used to demonstrate the current state of LVR awareness. There were two subscales of awareness items in the questionnaire, which was the public subscale and vision professional subscale, respectively. If the interviewee was a vision professional, including ophthalmologists, optometrists, eye nurses, vision therapists, and vision company practitioners, then they answered items for vision professionals, otherwise they answered items facing to the public. An additional part of the questionnaire was items designed for people with visual impairments. This part aimed to reveal their situation on visual rehabilitation services.
The Delphi method (15–18) was used to select items and test the effectiveness and reliability of the questionnaire. An item bank (57 items) was collected through literature review and professional experiences. Two rounds of expert consultations were conducted based on the item bank. The expert consultations involved 20 experts, including seven low vision specialists, one rehabilitation training professional, eight ophthalmologists, three statistics experts, and one special education expert. One ophthalmologist's advice was not reliable and was excluded. After two rounds of expert consultations and a pilot study, a finalized questionnaire was produced, which included eight demographic items for all participants, 10 for the public, 16 for the vision professionals, and four for the visually impaired (Appendix 1). The Cronbach's α is 0.7 in vision and non-vision professional items.
Survey and data collection
An online mobile application named Wenjuanxing, which has functions equivalent to Amazon Mechanical Turk, was used to distribute the questionnaire. Individuals scan a QR code to access and answer the questionnaire.
This survey was conducted with two distinct participant groups: the general public and vision professionals. The questionnaire was distributed through representative hospitals in all provinces across China. Additionally, the survey was distributed to vision professionals attending the Vision China Conference in 2022 and 2023. Vision China Conference is one of the large-scale visual conferences in China. Attendees include ophthalmologists, optometrists, nurses, researchers, and visual enterprise employees, representing a highly representative cohort in vision professionals.
The sum score of all items of each participant was used to determine the person's LVR awareness. The mean score of an item of all the participants was used to assess the awareness of a particular item. If all the items were answered correctly, a maximizing score would be obtained.
Statistical method
Data was analyzed using a Chinese version of SPSS 25.0. Mean ± SD and median (quantile) were used to describe quantitative data. Frequency and composition ratios were used to describe categorical data. The sum score of each subscale was calculated. Principal component analysis (PCA) was used for questionnaire structure analysis. One-way analysis of variance (ANOVA) and logistic regressions were performed to show the relations of scores with demographics. p < 0.05 were considered as statistically significant.
Results
Demographic information
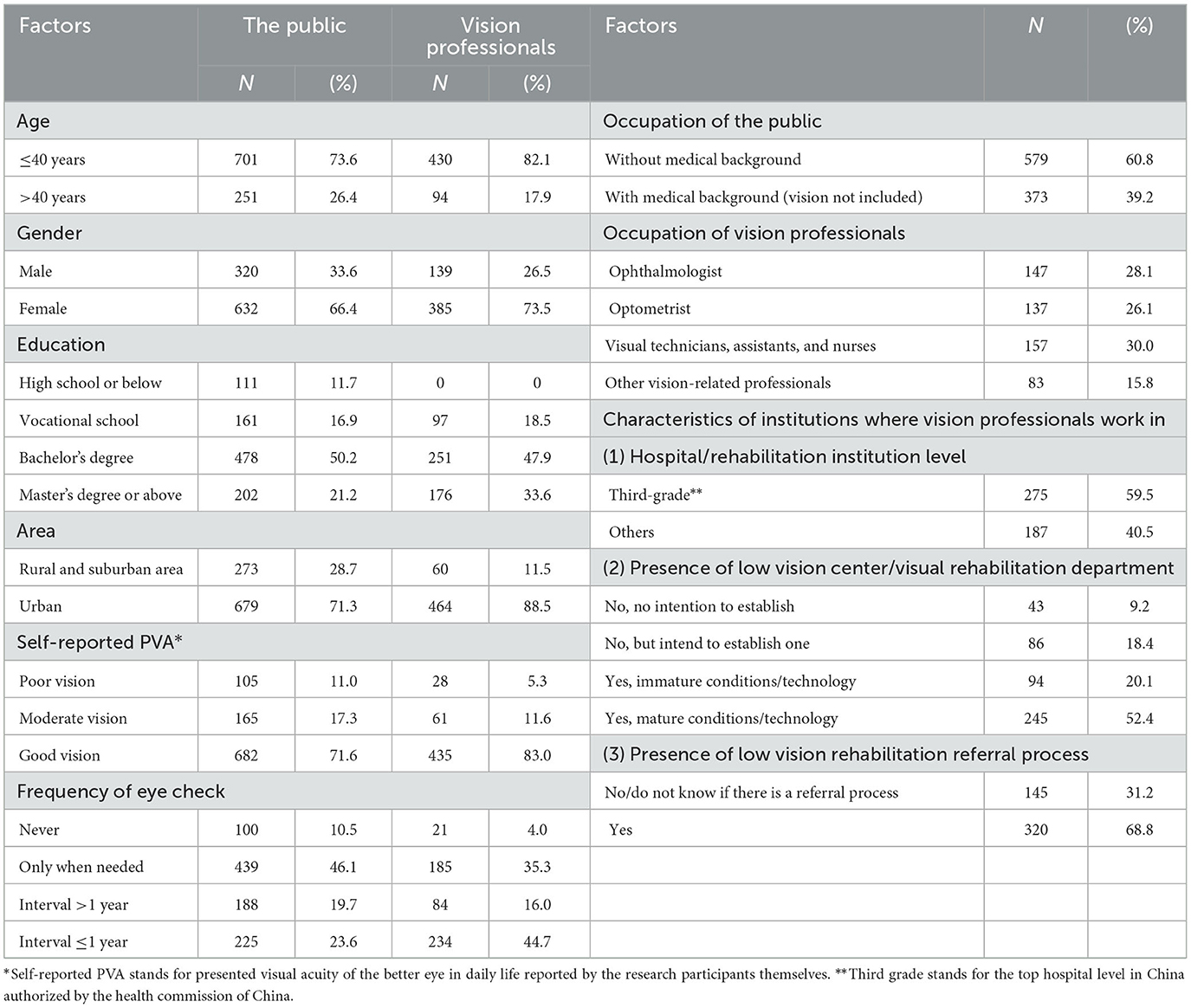
A total of 1,482 questionnaires were collected, among which 952 was from the public and 530 was from the vision professionals. Six vision professional participants were excluded because they were < 18 years old, so 524 valid vision professional questionnaires were analyzed (Table 1).
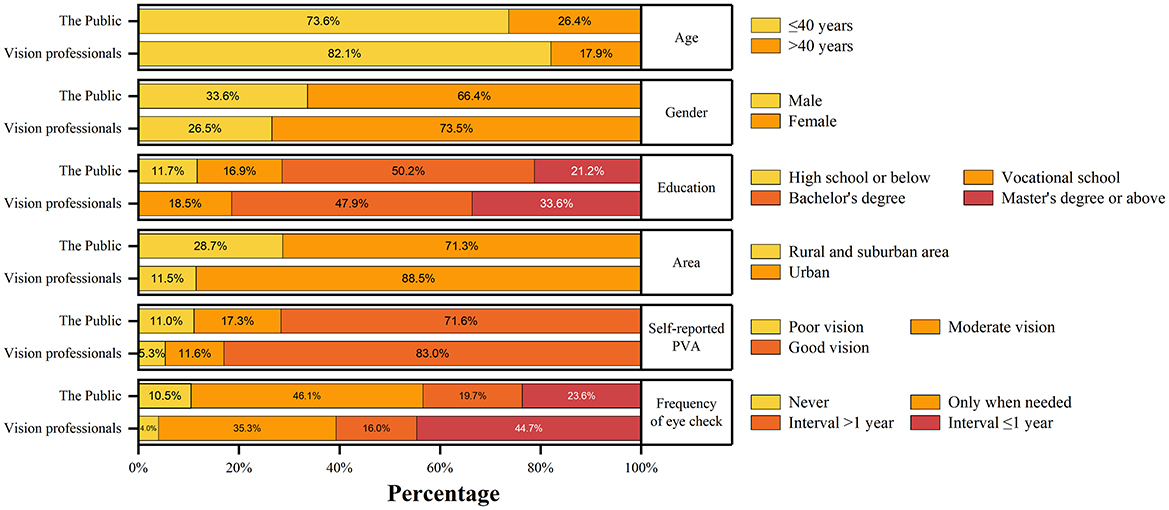
Regardless of the public and the vision professionals, the majority of the participants was from Eastern China (57.9% in the public; 48.2% in the vision professionals, Figure 1). The age, gender, education level proportion and visual acuity was all similar in both groups. About 70% of the public and 90% of the vision professionals lived in urban areas, respectively. Details were listed in Table 1 and Figure 2.
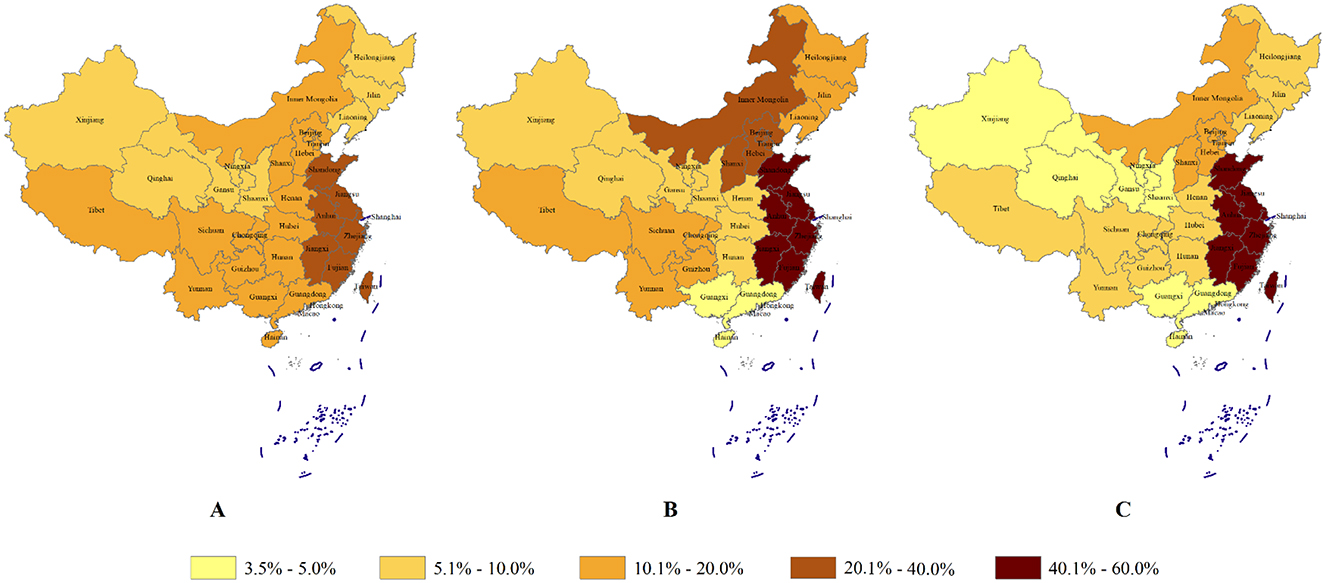
Figure 1. The proportion of population in each region of China and the proportion of the the questionnaire subjects in each region of China. Three maps of China labeled A, B, and C show varying population percentages. Color gradients: light yellow represents 3.5% to 5%, increasing to dark brown for 40.1% to 60%. Map A is the real proportion of populations in each region of China. Map B is the proportion of subjects who answered the public items in each region. Map C is the proportion of subjects who answered the vision professionals items in each region of China.
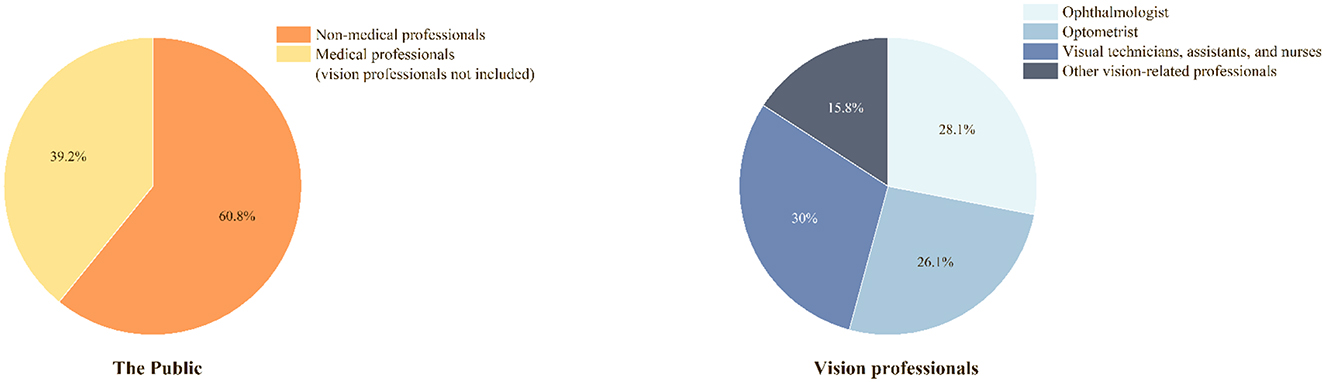
The majority of the public participants were without medical education background (60.8%). For vision professional participants, 59.5% worked in a tertiary hospital/institute, and 68.8% knew how to refer low-vision patients to LVR departments (Table 1, Figure 3).
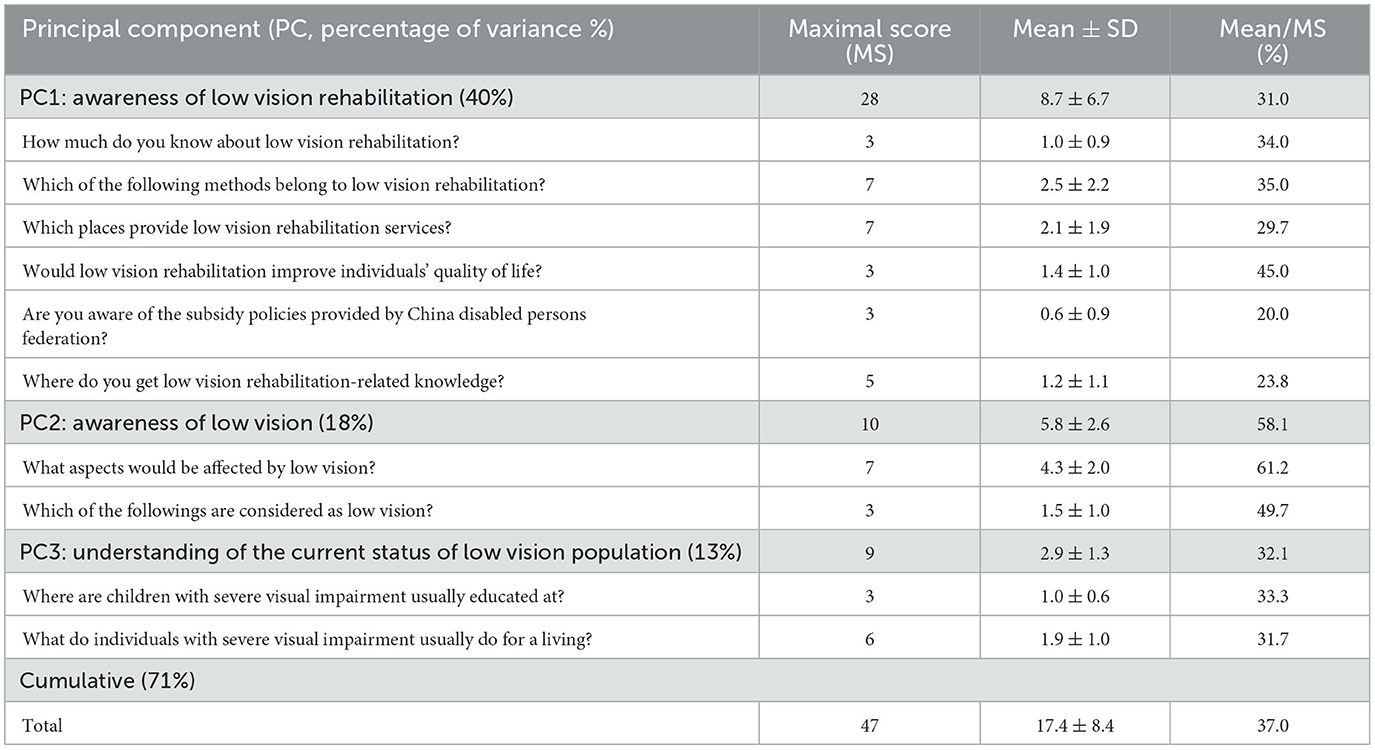
Sum score of LVR and principal component analysis
The mean sum score of all items in the public group accounted for 37.0% of the maximizing score (17.4/47.0). All the items could be categorized into 3 principal components, which accounted for 71% of the total variations, using principal component analysis (PCA). The three components were interpreted as awareness of LVR (PC1), awareness of low vision (PC2), understanding of the current living status of low vision population (PC3). The percentage of the mean score of the three principal components accounted for 31.0, 58.1 and 32.1% of the maximizing score, respectively (Table 2).
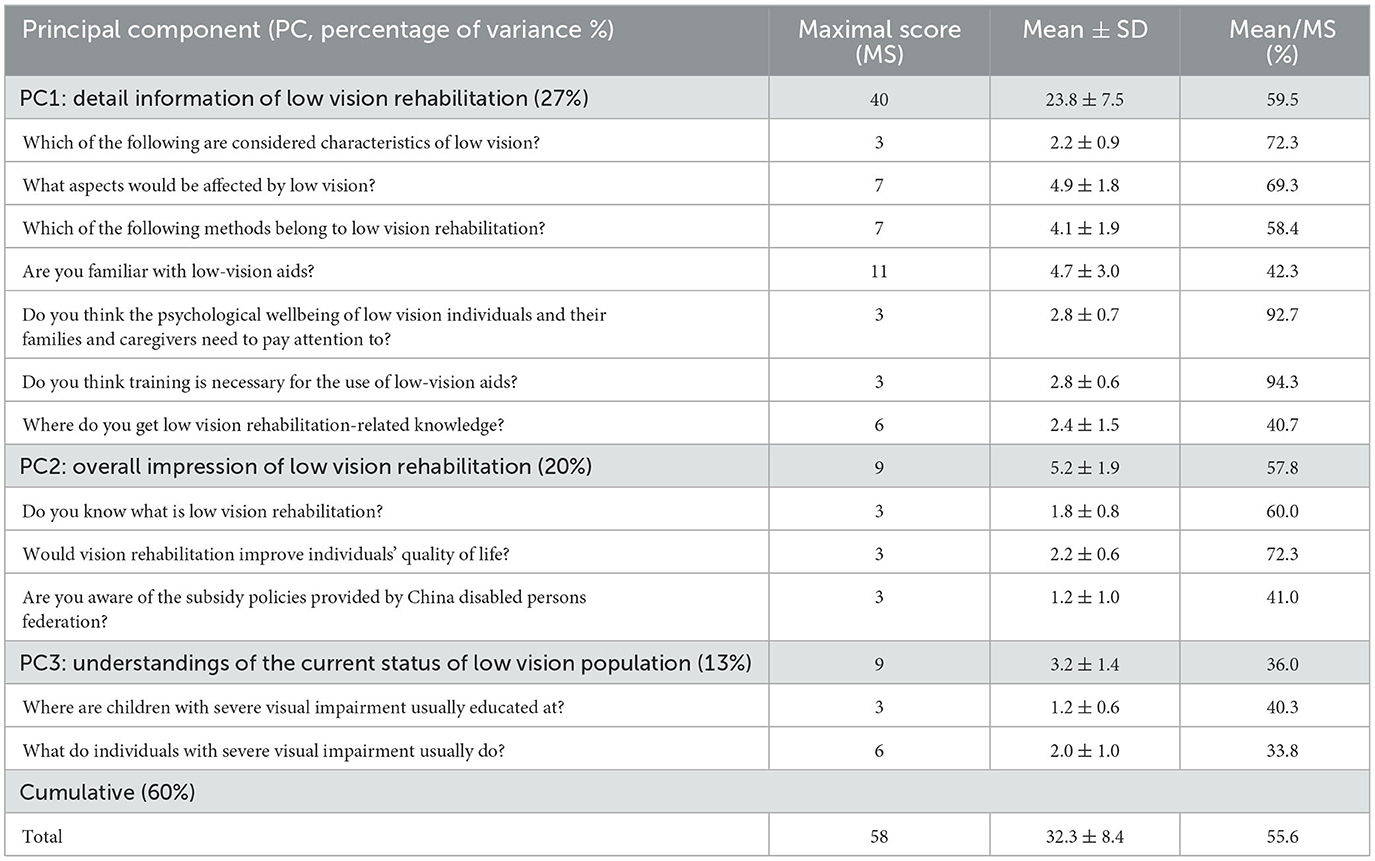
The mean sum score of all items of the vision professionals accounted for 55.6% of the maximizing score (32.3/58.0). All the items were also categorized into three principal components, which accounted for 60% of the total variations, using PCA. The 3 components were interpreted as Detailed information of LVR (PC1), Overall impression of LVR (PC2), understanding of the current living status of low vision population (PC3). The percentage of the mean score of the three principal components accounts for 59.5, 57.8 and 36.0% of the maximizing score, respectively (Table 3).
Factors that affected LVR awareness
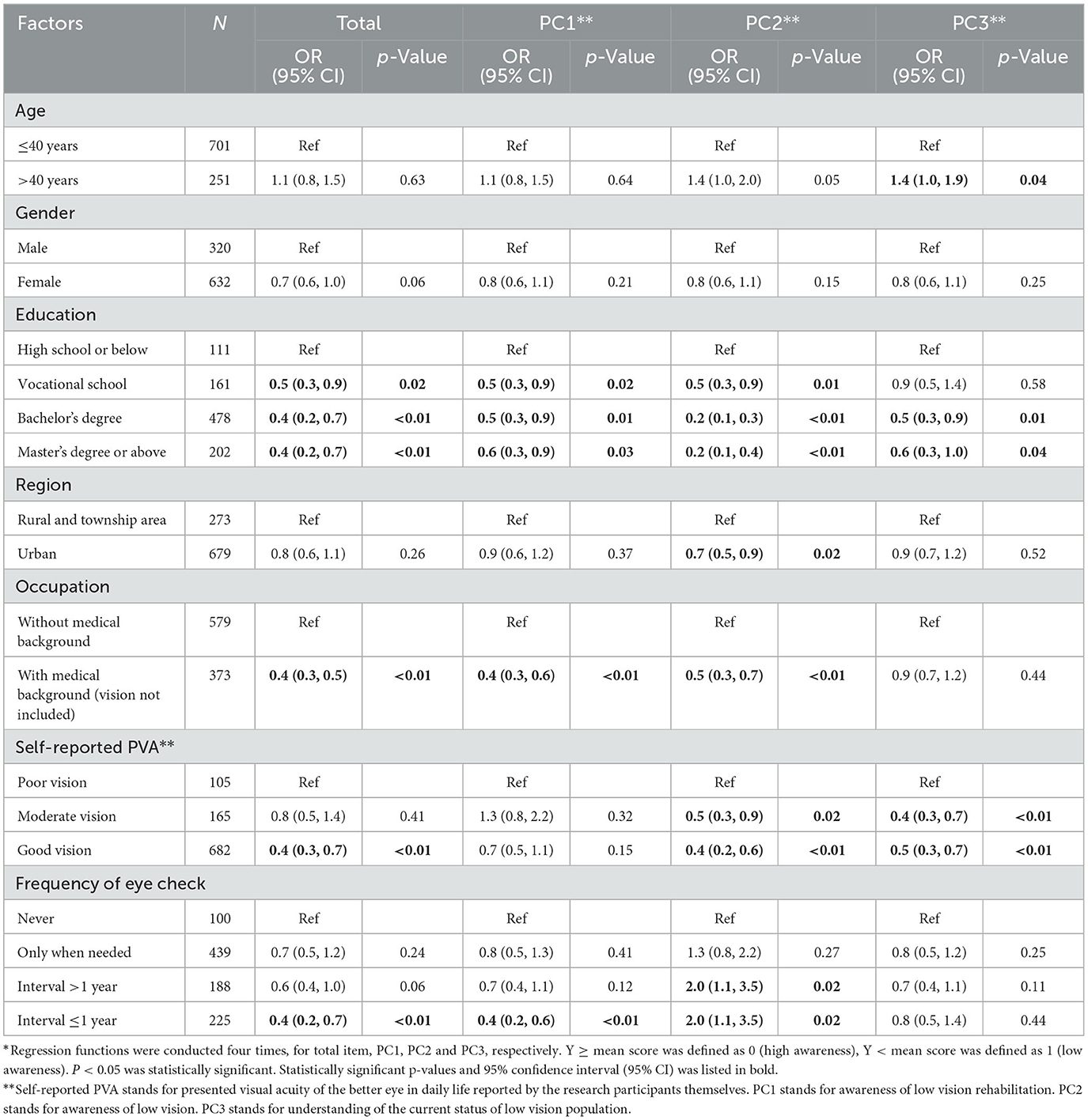
Multiple logistic regressions of sum scores of total items in the public group indicated that participants with higher education levels [OR (95% CI): vocational school, 0.5 (0.3, 0.9); bachelor's degree, 0.4 (0.2, 0.7), master's degree or above, 0.4 (0.2, 0.7)], with medical background [OR (95% CI): 0.4 (0.3, 0.5)], with good visual acuity [OR (95% CI): 0.4 (0.3, 0.7)], having eye checked every year or less [OR (95% CI): 0.4 (0.2, 0.7)] (Table 4).
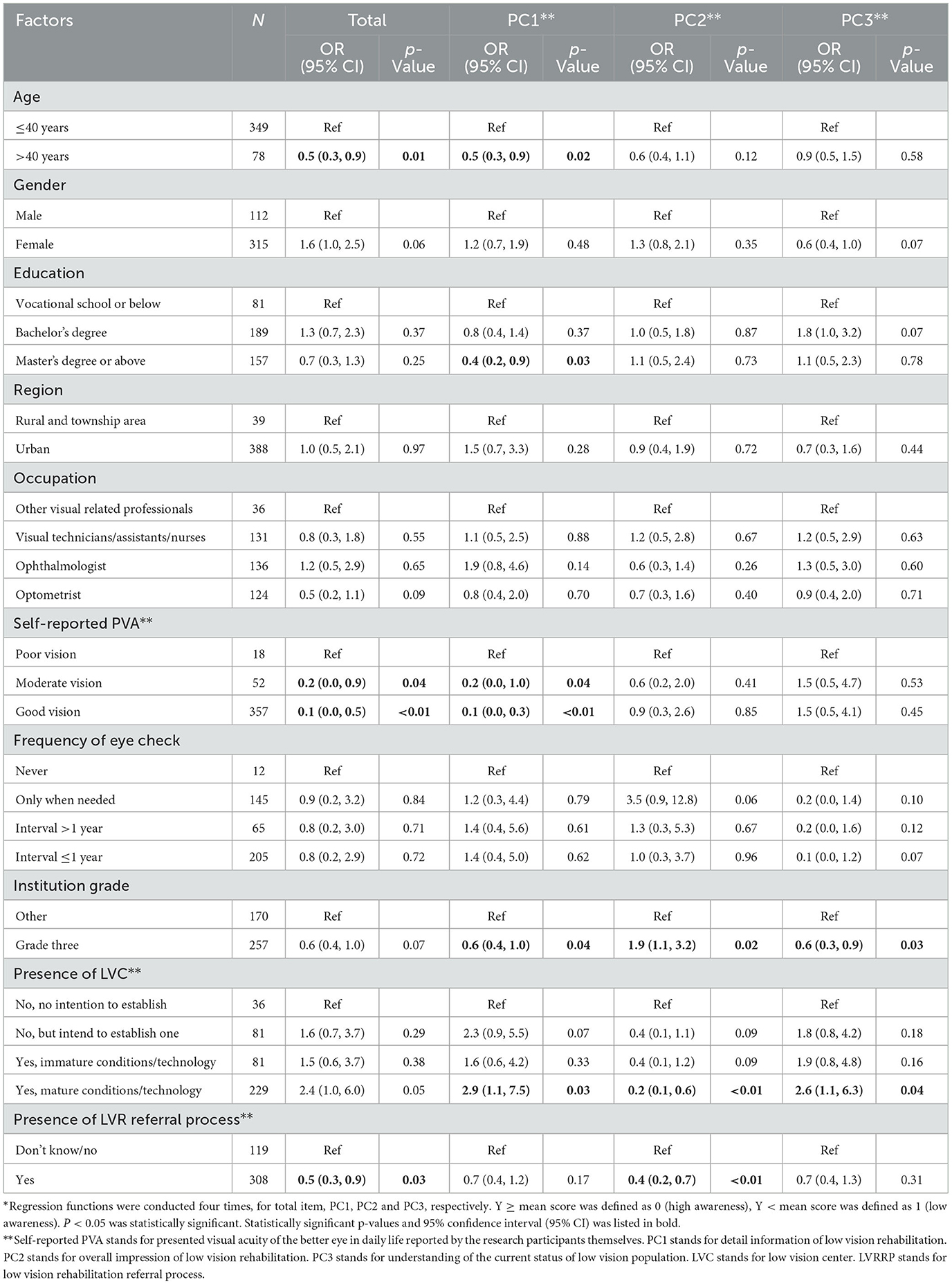
For the vision professionals, participants who aged elder than 40 years old [OR (95% CI): 0.5 (0.3, 0.9)], with a better visual acuity [OR (95% CI): moderate, 0.2 (0.0, 0.9), good, 0.1 (0.0, 0.5)] demonstrated a better awareness of low vision. Besides, vision professionals who knew the low vision referral process of the institute which he/she worked in [OR (95% CI): 0.5 (0.3, 0.9)] showed a better awareness than those who did not know (Table 5).
Sources of knowledge on low vision rehabilitation
The sum score of total items above the average was defined as high awareness and below the average was defined as low awareness. For the public, the main sources of obtaining LVR information were through doctors' advice (about 29%) and news media or internet (about 28%). A higher percentage of participants obtain parts of the knowledge from public awareness activities in the high awareness group, compared to the low awareness group (22.7 vs. 14.6%, p < 0.05). For the vision professionals, the main sources of obtaining LVR information in the low awareness group was through medical school education (30.0%) while in the higher awareness group, knowledge pathways were pluralistic, including medical school education, continual education, conference, and peer exchanges. A higher percentage of participants obtain parts of the knowledge from self-learning in the high awareness group compared to the low awareness group (17.0 vs. 12.6%, p < 0.05, Figure 4).
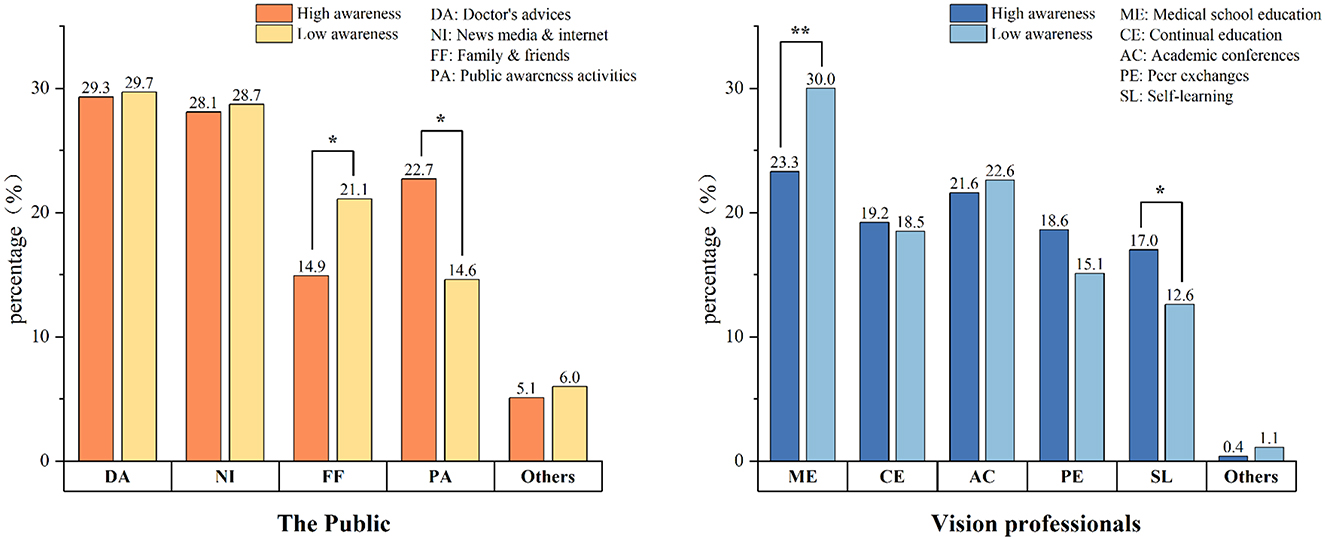
Figure 4. Sources of knowledge on low vision rehabilitation. High awareness stands for an individual's total score higher than mean score. Low awareness stands for an individual's score lower than mean score. p < 0.05 was statistically significant. *p < 0.05. **p < 0.01.
Discussion
We demonstrate that both the public and vision professionals lack overall awareness of LVR in China through this study. Misconceptions and the lack of awareness about rehabilitation services among people pose a significant barrier to the development of LVR (19–23). It is essential to enhance the importance of low vision publicity, then people can understand and pay more attention to it.
Low awareness of LVR in both the public and vision professionals
The mean score of total items was only one third of the maximal score in the public. The low awareness of LVR was not only demonstrated in low cognition of what is LVR, but also manifested in less attention to the living status of people with low vision. The public with higher levels of education and having medical background demonstrated better awareness. It is no doubts that people working in medical system have a better cognition of health compared to the public. Participants with better education have a higher possibility to represent a better level of cognition (24–27), or have better learning abilities, which leads to effective pathways to obtain LVR-related knowledge (28).
The average score of total items in the vision professionals is about one half of the maximal score, which is far from enough for a qualified vision professional. Most vision professionals know what low vision is and believe that visual rehabilitation training is necessary, while lack the awareness on how to deliver LVR. Vision professionals also show low attention to the survival status of individuals with low vision. Similar results have been presented in previous studies (29, 30). Research by Jose indicated that 64.0% of vision professionals lack awareness of LVR, and 62.1% of the vision professionals lack relevant training, which is a major obstacle to providing LVR services (31).
It is surprised to found that a better awareness of LVR of a vision professional was not related to whether an institution had a visual rehabilitation center or not, but associated with a settled process of low vision referral. We speculated that referral process indicated that this institution has a high possibility of implementing LVR services. Even if a doctor did not deliver LVR themselves, a timely referral informed a low vision person where to get LVR services, was equally helpful (32). The presence of a referral process allows resources and information sharing among staff, therefore, they would have a better understanding of LVR. This speculation is supported by literature researches. Data showed that the level of a hospital is not determined by department settings, but relies on high quality services (33, 34).
To improve awareness of the public
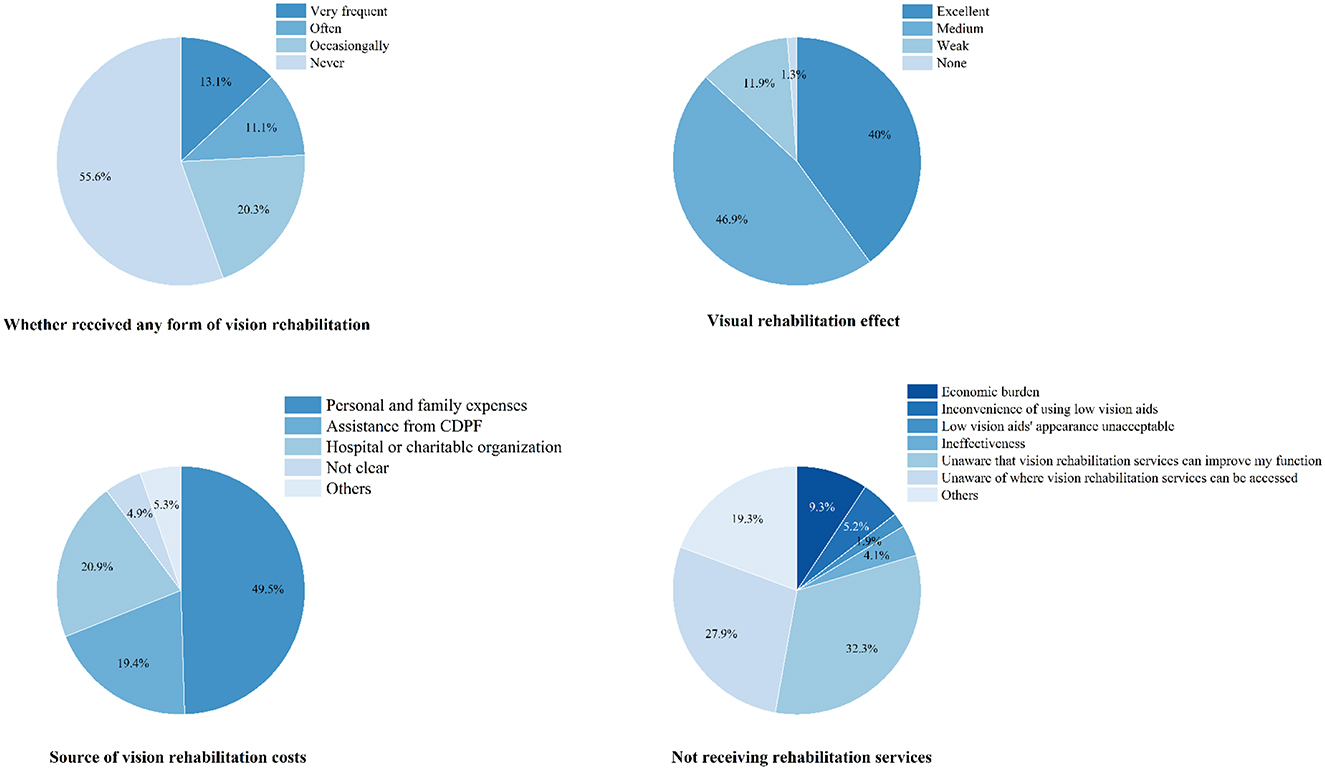
Although the public awareness on detailed LVR is limited at this moment, participants with visual impairments who have received rehabilitation services show a positive attitude toward visual rehabilitation (Figure 5), which is consistent with previous findings (4, 35–37).
The study also showed that the public mainly obtain low vision rehabilitation information through doctors' advice and public media. This emphasizes that the first visit doctor delivers low vision rehabilitation advice to the patient is important (38). The truth that participants who undergone eye check more frequently shew better awareness could also demonstrate the statement. The second method revealed form the results was that vision professionals should increase positive guidance and scientific education of LVR though public media. A survey conducted in Australia concerning LVR services revealed that 85% of Australian participants stated that receiving information about LVR was a facilitating factor in utilizing low vision services (32). However, negative behaviors and attitudes from ophthalmologists in introducing and recommending LVR services to patients have been found to be barriers to patients' acceptance of LVR services (32, 39).
In summary, public awareness can be gradually influenced (40). Doctors' advice in the clinic and scientific education though public media would help to improve the situation.
To improve awareness of vision professionals
The primary approach of obtaining information was through studying during medical school education, for vision professionals with low awareness of LVR. For vision professionals with higher awareness, they get their knowledge from diverse ways, such as medical school education, continual education, academic conferences, and peer exchanges.
The results revealed that to improve basic low vision knowledge and awareness, college or university education would be helpful. Besides, university and college time is crucial for personal growth and the reshaping of values (41, 42). Low vision education during this period would help to create a systematic impression and be much more efficient than later casual learning (43).
Comprehensive and cutting-edge knowledge of low vision would mainly come from literatures and academic discussions. And standard LVR procedures would be provided in continual education courses (44). The cultivation of a better awareness and abilities in the later stage, attending more low vision conferences, symposiums and continual education would be a second chance.
Limitations
The participants of the present study covered various provinces and cities nationwide in China, but with a primary concentration in eastern China and the hospitals involved were relatively in a high level in China. As the eastern side is much more developed than the northwest and southwest of China, if the awareness of the eastern area was not sufficient, then other areas would be even lower. The study might overestimate the current awareness of the public and the vision professional in China, but would not impact the solutions it revealed. Another limitation of the study comes from a cross-sectional study with self-reported answers, which can't tell why the study subjects lack awareness as well as the quantitative effectiveness the solutions, which needs later longitudinal studies to confirm.
Conclusions
The awareness of LVR in China is insufficient in both the public and vision professionals. Emphasizing the importance of doctor's advices in the clinic and scientific education through public media to improve the awareness of the public. And it is crucial to develop low vision education in medical curriculum and expand low vision conferences and continuing education to improving awareness of the vision professionals.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Eye Hospital of Wenzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XL: Conceptualization, Data curation, Investigation, Supervision, Writing – original draft, Writing – review & editing. RZ: Investigation, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Validation, Visualization. YL: Data curation, Formal analysis, Investigation, Writing – original draft. JZ: Data curation, Visualization, Writing – review & editing. XH: Investigation, Writing – review & editing. QC: Investigation, Writing – review & editing. NL: Investigation, Writing – review & editing. JC: Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by Zhejiang Province Medical and Health Science and Technology Project [No. 2025ky1016], National Key Research and Development Program of China [No. 2023YFC3604001] and Science and Technology Project of Wenzhou Science and Technology Bureau [No. Y2020358]. The authors declare that they have no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1659439/full#supplementary-material
References
1. Lupón M, Cardona G, Armayones M. Public knowledge of low vision and blindness, and readability of on-topic online information. J Optom. (2021) 14:240–6. doi: 10.1016/j.optom.2020.06.005
2. World Health Organization. World Report on Vision (2020). Available online at: https://www.who.int/Publications/i/Item/9789241516570 (Accessed October 8, 2019)
3. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the global burden of disease study. Lancet Glob Health. (2021) 9:e130–43. doi: 10.1016/S2214-109X(20)30425-3
4. van Nispen RM, Virgili G, Hoeben M, Langelaan M, Klevering J, Keunen JE, et al. Low vision rehabilitation for better quality of life in visually impaired adults. Cochrane Database Syst Rev. (2020) 1:Cd006543. doi: 10.1002/14651858.CD006543.pub2
5. Parravano M, Petri D, Maurutto E, Lucenteforte E, Menchini F, Lanzetta P, et al. Association between visual impairment and depression in patients attending eye clinics: a meta-analysis. JAMA Ophthalmol. (2021) 139:753–61. doi: 10.1001/jamaophthalmol.2021.1557
6. Gothwal VK, Sumalini R, Bharani S. Assessing the effectiveness of low vision rehabilitation in children: an observational study. Invest Ophthalmol Vis Sci. (2015) 56:3355–60. doi: 10.1167/iovs.14-15760
7. Gothwal VK, Bharani S. Outcomes of multidisciplinary low vision rehabilitation in adults. Invest Ophthalmol Vis Sci. (2015) 56:7451–61. doi: 10.1167/iovs.15-16892
8. Lamoureux EL, Pallant JF, Pesudovs K, Rees G, Hassell JB, Keeffe JE. The effectiveness of low-vision rehabilitation on participation in daily living and quality of life. Invest Ophthalmol Vis Sci. (2007) 48:1476–82. doi: 10.1167/iovs.06-0610
9. Catalog of Basic Rehabilitation Services for Persons with Disabilities (2019 Edition). Available online at: https://www.cdpf.org.cn/zwgk/ggtz1/67dc0197c7bb4ef3be5c93dbe7e68e63.htm (Accessed July 24, 2019).
10. National Eye Health Plan for the 13th Five-Year Plan (2016–2020). Available online at: https://www.ndrc.gov.cn/fggz/fzzlgh/gjjzxgh/201707/t20170720_1196852.html (Accessed July 20, 2017).
11. Zhan L, An L, Feng J, Xu X. Analysis of human resource allocation and service delivery for low vision in tertiary medical institutions in mainland China. Chin J Optom Ophthalmol Vis Sci. (2019) 21:297–301. doi: 10.3760/cma.j.issn.1674-845X.2019.04.010
12. Ni L, Li K, Jiang L, Chen J, Chen Y, Li X, et al. A nurse's perspective on visual rehabilitation of outpatients with low vision in China. Rehabil Nurs. (2020) 45:45–53. doi: 10.1097/rnj.0000000000000178
13. Li X, Chen G, Deng R, Lin N, Ni L, Jiang L, et al. The needs for visual improvement of patients presented at low-vision center in Wenzhou, China. J Ophthalmol. (2019) 2019:3586370. doi: 10.1155/2019/3586370
14. Li X, Chen J, Xu G, Zhong Y, Jang L, Lin L, et al. Development of an elderly low vision quality of life questionnaire for less-developed areas of China. Qual Life Res. (2015) 24:2403–13. doi: 10.1007/s11136-015-0970-2
15. Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE. (2011) 6:e20476. doi: 10.1371/journal.pone.0020476
16. Lee PP, Sultan MB, Grunden JW, Cioffi GA. Assessing the importance of IOP variables in glaucoma using a modified Delphi process. J Glaucoma. (2010) 19:281–7. doi: 10.1097/IJG.0b013e3181b4ca8d
17. Behrens A, Doyle JJ, Stern L, Chuck RS, McDonnell PJ, Azar DT, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. (2006) 25:900–7. doi: 10.1097/01.ico.0000214802.40313.fa
18. Douglas RS, Tsirbas A, Gordon M, Lee D, Khadavi N, Garneau HC, et al. Development of criteria for evaluating clinical response in thyroid eye disease using a modified Delphi technique. Arch Ophthalmol. (2009) 127:1155–60. doi: 10.1001/archophthalmol.2009.232
19. Sarabandi A, Vatankhah S, Kamali M, Aryankhesal A. Essential components of rehabilitation services provided to visually impaired people. Clin Exp Optom. (2021) 104:215–21. doi: 10.1111/cxo.13121
20. Lam N, Leat SJ. Barriers to accessing low-vision care: the patient's perspective. Can J Ophthalmol. 2013;48:458–62. doi: 10.1016/j.jcjo.2013.02.014
21. Mwilambwe A, Wittich W, Freeman EE. Disparities in awareness and use of low-vision rehabilitation. Can J Ophthalmol. (2009) 44:686–91. doi: 10.3129/i09-179
22. MacLachlan J, Rudman DL, Klinger L. Low vision: a preliminary exploration of its impact on the daily lives of older women and perceived constraints to service use. Phys Occup Ther Geriatrics. (2007) 26:43–62. doi: 10.1300/J148v26n02_03
23. Chiang PP, O'Connor PM, Le Mesurier RT, Keeffe JE. A global survey of low vision service provision. Ophthalmic Epidemiol. (2011) 18:109–21. doi: 10.3109/09286586.2011.560745
24. Rimkus CM, Avolio IMB, Miotto EC, Pereira SA, Mendes MF, Callegaro D, et al. The protective effects of high-education levels on cognition in different stages of multiple sclerosis. Mult Scler Relat Disord. (2018) 22:41–8. doi: 10.1016/j.msard.2018.03.001
25. Park S, Choi B, Choi C, Kang JM, Lee JY. Relationship between education, leisure activities, and cognitive functions in older adults. Aging Ment Health. (2019) 23:1651–60. doi: 10.1080/13607863.2018.1512083
26. Chen Y, Lv C, Li X, Zhang J, Chen K, Liu Z, et al. The positive impacts of early-life education on cognition, leisure activity, and brain structure in healthy aging. Aging. (2019) 11:4923–42. doi: 10.18632/aging.102088
27. Takashi S, Kumiko I. Barriers to the utilization of low-vision rehabilitation services among over-50-year-old people in east and southeast asian regions: a scoping review. Int J Environ Res Public Health. (2023) 20:7141. doi: 10.3390/ijerph20237141
28. Du C, Miyazaki Y, Dong X, Li M. Education, social engagement, and cognitive function: a cross-lagged panel analysis. J Gerontol B Psychol Sci Soc Sci. (2023) 78:1756–64. doi: 10.1093/geronb/gbad088
29. Khan SA, Shamanna B, Nuthethi R. Perceived barriers to the provision of low vision services among ophthalmologists in India. Indian J Ophthalmol. (2005) 53:69–75. doi: 10.4103/0301-4738.15293
30. Okoye OI, Aghaji A, Umeh R, Nwagbo D, Chuku A. Barriers to the provision of clinical low-vision services among ophthalmologists in Nigeria. Vis Impair Res. (2007) 9:11–7. doi: 10.1080/13882350701198702
31. Jose J, Thomas J, Bhakat P, Krithica S. Awareness, knowledge, and barriers to low vision services among eye care practitioners. Oman J Ophthalmol. (2016) 9:37–43. doi: 10.4103/0974-620X.176099
32. O'Connor PM, Mu LC, Keeffe JE. Access and utilization of a new low-vision rehabilitation service. Clin Exp Ophthalmol. (2008) 36:547–52. doi: 10.1111/j.1442-9071.2008.01830.x
33. Comprehensive Hospital Grading Management Standards (Trial Draft). Available online at: http://www.100md.com/html/WestMed/manage/006/02/0060202.html (Accessed November 23, 2019).
34. Level 3 Hospital Evaluation Criteria (2025 Edition). Available online at: https://www.nhc.gov.cn/yzygj/c100068/202506/25229edc80d34694b7debf54ddef9f9f.shtml (Accessed June 10, 2025).
35. Özen Tunay Z, Idil A, Seza Petriçli I, Özdemir Ö. Low vision rehabilitation in older adults. Turk J Ophthalmol. (2016) 46:118–22. doi: 10.4274/tjo.68878
36. Özen Tunay Z, Çalişkan D, Idil A, Öztuna D. Clinical characteristics and low vision rehabilitation methods for partially sighted school-age children. Turk J Ophthalmol. (2016) 46:68–72. doi: 10.4274/tjo.82653
37. Gopalakrishnan S, Sudharshan S, Raman R, Saranya V, Majumder PD, Biswas J. Visual rehabilitation of patients with low vision in uveitis. Indian J Ophthalmol. (2019) 67:101–4. doi: 10.4103/ijo.IJO_875_18
38. Lam N, Leat SJ. Reprint of: barriers to accessing low-vision care: the patient's perspective. Can J Ophthalmol. (2015) 50 Suppl 1:S34–9. doi: 10.1016/j.jcjo.2015.04.007
39. Spafford MM, Laliberte Rudman D, Leipert BD, Klinger L, Huot S. When self-presentation trumps access: why older adults with low vision go without low-vision services. J Appl Gerontol. (2010) 29:579–602. doi: 10.1177/0733464809345494
40. Matti AI, Pesudovs K, Daly A, Brown M, Chen CS. Access to low-vision rehabilitation services: barriers and enablers. Clin Exp Optom. (2011) 94:181–6. doi: 10.1111/j.1444-0938.2010.00556.x
41. Pascarella ET, Terenzini PT. How College Affects Students: A Third Decade of Research. Vol. 2. San Francisco, CA: Jossey-Bass; ERIC (2005).
42. Mayhew MJ, Rockenbach AN, Bowman NA, Seifert TA, Wolniak GC. How College Affects Students: 21st Century Evidence that Higher Education Works. San Francisco, CA: John Wiley & Sons; Jossey-Bass (2016).
43. Sibandze BT, Scafide KN. Among nurses, how does education level impact professional values? A systematic review. Int Nurs Rev. (2018) 65:65–77. doi: 10.1111/inr.12390
Keywords: low vision rehabilitation, awareness, questionnaire, vision professionals, public
Citation: Li X, Zhu R, Liu Y, Zhang J, Hu X, Chi Q, Lin N and Chen J (2025) Public awareness of low vision rehabilitation in China. Front. Med. 12:1659439. doi: 10.3389/fmed.2025.1659439
Received: 04 July 2025; Accepted: 31 July 2025;
Published: 22 August 2025.
Edited by:
Jinhai Huang, Fudan University, ChinaReviewed by:
Nida Amin, Green International University Lahore, PakistanMemoona Arshad, The University of Faisalabad, Pakistan
Copyright © 2025 Li, Zhu, Liu, Zhang, Hu, Chi, Lin and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Chen, Y2pAZXllLmFjLmNu
†ORCID: Xiaoman Li orcid.org/0000-0003-1747-8695
Jie Chen orcid.org/0000-0002-8156-9332
 Xiaoman Li1,2†
Xiaoman Li1,2† Na Lin
Na Lin Jie Chen
Jie Chen