- 1Rehabilitation Medicine College, Shandong Second Medical University, Weifang, China
- 2Department of Cardio-Pulmonary Circulation, Innovation and Incubation Center (IIC), Shanghai Pulmonary Hospital, School of Medicine, Tongji University, Shanghai, China
- 3Bioenvironmental Science Program, Morgan State University, Baltimore, MD, United States
- 4Department of Radiology, Shanghai Pulmonary Hospital, School of Medicine, Tongji University, Shanghai, China
Pulmonary hypertension (PH) is a significant global health challenge that profoundly impacts exercise tolerance and quality of life for affected individuals. While advancements in pharmacological therapies have improved symptom management, exercise capacity, and overall well-being, there is a growing recognition of rehabilitation therapy as a promising non-pharmacological approach. Rehabilitation therapy aims to restore or enhance physical, psychological, and social functioning in individuals compromised by disease, injury, or congenital conditions through an integrated approach encompassing medical, social, and educational interventions. In the context of PH, rehabilitation therapy encompasses diverse modalities, including exercise training, inspiratory muscle training, neuromuscular electrical stimulation, and psychological support. These interventions target key symptoms such as exercise intolerance and dyspnea, with the goal of improving patient outcomes and fostering a return to independent and meaningful living. Emerging evidence demonstrates that rehabilitation therapy is both safe and effective in enhancing cardiopulmonary function, muscle strength, and exercise capacity. Furthermore, it has been shown to alleviate anxiety and depression, improve quality of life, and facilitate reintegration into familial and social roles. This review provides a comprehensive overview of the clinical features, prevalence, and current treatment landscape of PH, with a particular focus on the role and advancements in rehabilitation therapy. We discuss the therapeutic potential of rehabilitation therapy in addressing the multifaceted challenges of PH and explore future directions and innovative approaches in this evolving field. By highlighting the clinical utility and research progress of rehabilitation therapy, this review aims to offer new insights and perspectives for optimizing the management of PH and improving patient outcomes.
1 Introduction
PH is a complex and progressively worsening cardiopulmonary disease affecting approximately 1% of the global population, posing a significant health burden on patients (1). Despite substantial advancements in pharmacologic therapies, the majority of patients continue to suffer from varying degrees of right heart dysfunction (2). As a result, they often experience reduced exercise capacity and a markedly diminished quality of life (3, 4). Currently, despite the availability of numerous targeted therapies, PH remains an incurable condition (5). Contrary to earlier beliefs, impaired exercise tolerance in PH is not solely attributable to central cardiopulmonary dysfunction. Recent studies have demonstrated that peripheral factors—particularly skeletal muscle and cerebrovascular impairments—also contribute significantly to exercise limitation (6–9). The pathophysiological mechanisms underlying skeletal muscle dysfunction in PH patients can be broadly categorized into three key domains: mitochondrial abnormalities, microcirculatory disturbances, and changes in muscle morphology (10).
In PH patients, mitochondrial structure and density within skeletal muscle are significantly reduced, accompanied by downregulation of critical proteins in the electron transport chain. This results in impaired mitochondrial metabolism and reduced cellular energy production. A hallmark of skeletal muscle dysfunction in PH is diminished systemic oxygen uptake. Lower oxygen saturation levels and decreased capillary density further compromise oxygen delivery and utilization. Additionally, reduced expression of microRNA-126 (miR-126), which plays a role in microvascular development and maintenance, exacerbates capillary rarefaction and impairs muscle oxygenation. Furthermore, the maximum contractile force and active stiffness of type II muscle fibers are markedly diminished. Myosin expression is reduced, while muscle atrophy and increased signaling for protein degradation are observed. There is also a notable shift in fiber type from type I to type II muscle fibers, which further decreases muscle endurance and strength. The combined effects of mitochondrial, microvascular, and myofibrillar abnormalities lead to severe peripheral muscle dysfunction and are a major contributor to the exercise intolerance characteristic of PH.
Therefore, despite advances in drug therapy, the long-term management of PH remains challenging. Exploring novel therapeutic strategies—particularly those targeting peripheral muscle dysfunction—is crucial for improving patient outcomes. Importantly, rehabilitation therapy can improve the characteristics of peripheral muscles (11). This review aims to provide a comprehensive overview of PH, including its clinical manifestations, epidemiology, and current treatment strategies. Particular emphasis is placed on the role of rehabilitation therapy, highlighting recent advances and evidence supporting its ability to enhance mobility, muscle function, and overall quality of life in patients with PH. Furthermore, the potential of emerging rehabilitation approaches in the management of PH will be discussed. By synthesizing these aspects, this review seeks to offer deeper insights into the evolving landscape of PH treatment, with a focus on rehabilitation therapy as a promising adjunctive strategy. Ultimately, improving our understanding of these therapeutic options may not only enhance clinical outcomes and prognosis for patients with PH but also inspire new directions in the research and management of related cardiopulmonary disorders.
2 Fundamental concepts in pulmonary hypertension
2.1 Definition of pulmonary hypertension
PH is a group of life-threatening pulmonary vascular disorders characterized by vasoconstriction and remodeling, leading to elevated pulmonary vascular pressure and resistance, ultimately resulting in death from right heart failure (12). Definitive diagnosis requires invasive hemodynamic evaluation via right heart catheterization, with PH defined by a mean pulmonary artery pressure (mPAP) ≥ 20 mmHg and a pulmonary capillary wedge pressure (PCWP) ≤ 15 mmHg (12). According to the World Health Organization (WHO), PH is classified into five major groups based on etiology: (1) pulmonary arterial hypertension (PAH), (2) PH associated with left heart disease, (3) PH associated with lung diseases and/or hypoxia, (4) PH associated with pulmonary artery obstructions, and (5) PH with unclear and/or multifactorial mechanisms. The prevalence varies significantly across these groups, with PH due to left heart disease being the most common subtype. Notably, the overall prevalence of PH has been increasing in recent years (13). Despite ongoing research, the underlying pathophysiological mechanisms of PH remain incompletely understood. However, irrespective of the causative classification, all subtypes of PH share a common pathological consequence: right ventricular remodeling, which can ultimately progress to right heart failure and death (14, 15).
2.2 Clinical manifestations and management of pulmonary hypertension
In the early clinical stages, the symptoms of PH are often nonspecific and easily misattributed to other conditions. Therefore, the early detection of PH may be difficult solely relying on clinical manifestations. Systematic diagnostic methods are needed, including both functional assessment and the use of advanced imaging techniques. The initial assessment typically begins with a comprehensive analysis of clinical manifestations, such as exertional dyspnea, fatigue, and syncope. Electrocardiogram (ECG) examinations may reveal the load pattern of the right ventricle, while chest X-rays can show structural changes in the heart and lungs. Through pulmonary function tests combined with arterial blood gas analysis, key information regarding ventilation efficiency and abnormal gas exchange can be provided. For a clear assessment, echocardiography serves as the main screening tool for estimating pulmonary artery pressure and evaluating right heart function. Ventilation/perfusion imaging remains indispensable for detecting the cause of thromboembolic events. The final diagnosis is based on right heart catheterization. As the disease progresses, symptoms are increasingly provoked by minimal physical activity and manifest at rest. Patients may develop chest pain, exertional syncope, lower extremity edema, and hepatic congestion—classic signs of right heart failure—indicating disease progression (12, 16). Overall, the clinical manifestations of PH range from mild to severe and evolve gradually, closely associated with the development of right heart failure. Beyond hemodynamic disturbances—such as elevated pulmonary vascular resistance, reduced stroke volume, and diminished cardiac index—PH also induces a range of systemic pathophysiologic changes. These include reduced skeletal muscle strength and endurance, as well as weakened respiratory muscles, particularly the diaphragm. Such impairments significantly reduce peak oxygen uptake, contributing to worsening fatigue, dyspnea, and overall functional decline. These cascading effects ultimately lead to profound exercise intolerance and markedly diminished quality of life (17).
These mechanisms highlight that PH is not merely a cardiopulmonary disorder but a systemic disease characterized by widespread metabolic and functional impairments, affecting patients’ physiological resilience and exercise tolerance through multiple pathways. Epidemiological data suggest that the incidence of PH ranges from 2.0 to 7.6 cases per million adults annually, with a prevalence between 11 and 26 cases per million. PH can affect individuals of all ages, though it is four times more common in women than in men. Interestingly, while more women are affected, men with PH tend to have poorer survival outcomes (18, 19). Current treatment strategies for PH are broadly divided into general measures, supportive therapies, and targeted pharmacologic interventions. Research has confirmed that the 14 core signaling pathways exhibit highly consistent and synergistic activation characteristics in patients with various types of PH (20). After the approval of PH-specific drugs, the 5-year survival rate of PH patients increased from 34 to 60% (21), with notable advances in symptom control, exercise capacity, hemodynamic parameters, and overall outcomes (22). However, while multi-targeted therapy shows great potential, it also faces practical challenges such as complex drug interactions, high treatment costs, and significant individual response variations.
Because PH is often diagnosed at an advanced stage, many patients already present with significant physical limitations at the time of diagnosis. Therefore, identifying additional therapeutic approaches is critical for improving prognosis and long-term functional outcomes. In this context, rehabilitation therapy has attracted increasing attention due to its low cost, ease of implementation, and noninvasive nature. Emerging evidence supports the safety and clinical efficacy of rehabilitation therapy in PH, positioning it as a promising adjunctive treatment. This approach offers new hope for enhancing the quality of life in patients living with this debilitating condition.
3 Strategies for implementing rehabilitation therapy
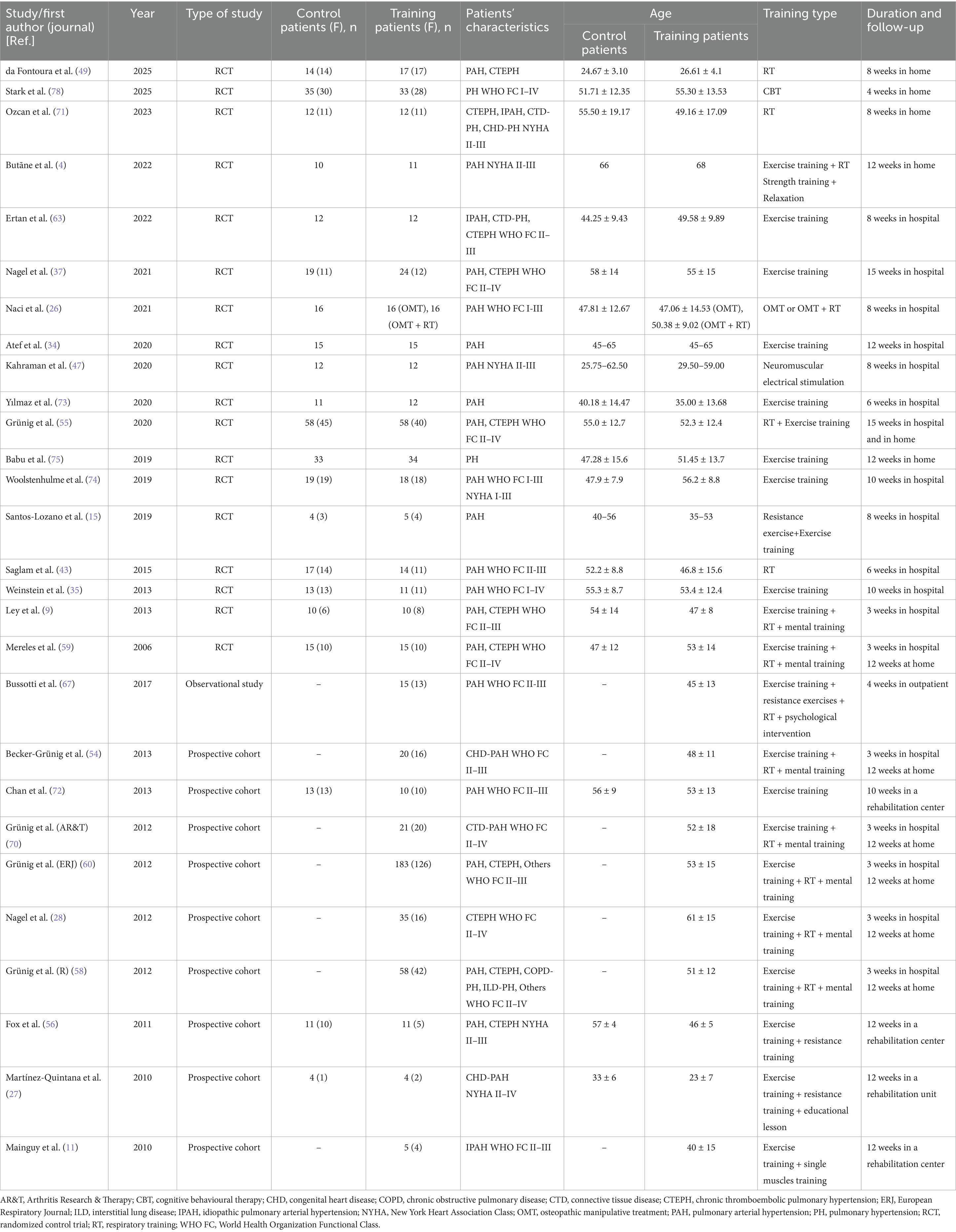
Rehabilitation therapy is increasingly recognized as a powerful, non-pharmacological strategy that not only restores or enhances physical, psychological, and social functioning in individuals affected by disease, injury, or congenital conditions, but also empowers them to reintegrate fully into family life and society. By integrating medical, social, and educational interventions, it delivers comprehensive, person-centered care that fosters optimal recovery, meaningful participation in daily activities, and a confident return to valued social roles. Rehabilitation therapy not only significantly enhances the quality of life for patients with PH, but also alleviates the associated familial and societal burdens. Moreover, it can effectively slow disease progression, address psychological challenges, and facilitate a smoother reintegration into family life and society. Therefore, the widespread promotion and application of rehabilitation concepts and techniques hold substantial value in improving the overall recovery outcomes for PH patients. We searched PubMed, EMBASE, and the Cochrane Collaboration database using the keywords “exercise training” or “rehabilitation” and “pulmonary hypertension.” In clinical practice, the application of rehabilitation therapy in PH can be broadly classified into four key areas: exercise training, inspiratory muscle training, neuromuscular electrical stimulation, and psychological intervention (Table 1). Carrying out rehabilitation therapy for patients with PH, the short-term rehabilitation goals are to rapidly alleviate symptoms such as shortness of breath and fatigue, increase the 6-minute walking distance, maintain blood oxygen saturation, and learn abdominal breathing. The long-term rehabilitation goals are to continuously improve cardiopulmonary endurance, right heart function and quality of life, reduce the frequency of acute exacerbations and hospitalizations, enable the patients to return to family, society, and work, and delay the progression of the disease to the end stage. The rehabilitation therapy team consists of occupational therapists (OT), physical therapists (PT), and speech therapists (ST). Its size is continuously expanding among medical professionals and is playing an irreplaceable core role in the medical service system. Among them, cardiopulmonary physical therapists (CPT), as sub-specialists of PT, bear the main responsibility in the rehabilitation treatment of patients with PH. Through evidence-based exercise training, breathing strategies, and lifestyle interventions, they systematically improve the patients’ cardiopulmonary endurance and quality of life.
3.1 Exercise training
Restricted exercise capacity is a hallmark symptom of PH, profoundly impacting patients’ quality of life. During physical activity, the body relies on the integrated functions of the respiratory and cardiovascular systems to meet the increased metabolic demands of skeletal muscle contraction. In individuals with PH, impairments in both systems significantly limit their exercise tolerance. Beyond central cardiopulmonary dysfunction, emerging evidence has highlighted the contribution of peripheral abnormalities to exercise intolerance in PH. These include a reduced number and density of capillaries in skeletal muscle, diminished oxidative enzyme activity, and muscle fiber atrophy—all of which negatively influence muscle oxygen utilization and endurance capacity (23). Additionally, morphological and functional alterations in peripheral muscle are frequently observed, such as decreased muscle strength, a lower proportion of type I muscle fibers, and a metabolic shift favoring anaerobic pathways over aerobic metabolism (24). These changes collectively exacerbate exercise limitation and reduce quality of life.
Exercise training, as an economical and easily scalable health intervention, has received substantial support from evidence-based medical research for its multiple health benefits. Physiologically, exercise training significantly enhances cardiopulmonary function, optimizes body composition, improves insulin sensitivity, and regulates lipid metabolism. Psychosocially, its effects are equally remarkable, including alleviating depressive and anxious symptoms, enhancing cognitive function, and delaying the aging process. This multi-dimensional health promotion effect is particularly important for patients with chronic diseases, providing a practical and non-pharmacological intervention option for their disease management and health improvement. It has the potential not only to enhance functional capacity but also to mitigate disease progression by reversing some of the underlying pathophysiological mechanisms. This dual effect—both therapeutic and prognostic—renders exercise training a compelling adjunct in disease management (25–28). Once, there were concerns that increased shear stress on the pulmonary vasculature during exercise might accelerate vascular remodeling and worsen PH. Consequently, exercise training was not routinely recommended. However, recent studies have demonstrated that, when properly supervised, exercise training is safe and beneficial for individuals with cardiopulmonary diseases, including PH (29). Improvements have been noted in cardiorespiratory function, physical performance, and overall quality of life.
Patients with PH constitute a particularly vulnerable population, exhibiting degrees of functional impairment and poor long-term prognosis comparable to, or even exceeding, those observed in heart failure (30–32). These outcomes are primarily driven by progressive increases in pulmonary vascular resistance, declining right ventricular function, and systemic involvement affecting multiple organ systems. The 2022 European Society of Cardiology (ESC) Guidelines for the diagnosis and treatment of PH now advocate for structured rehabilitation therapy in stable PH patients. Specifically, exercise training should be undertaken under professional supervision and in combination with optimized pharmacotherapy. This reflects a paradigm shift, positioning exercise as a safe and effective adjunctive intervention in well-compensated PH patients. In clinical settings, exercise training typically begins under hospital supervision, with the initial intensity set at 60–80% of peak oxygen uptake (peak VO₂) or 40–60% of maximal heart rate (29). It is critical to initiate exercise training at low intensity, progressively increasing workload based on individual tolerance. Continuous monitoring of heart rate (<120 beats/min) and oxygen saturation (>85%) is essential to ensure safety during exercise training sessions (29). Given constraints such as cost and hospitalization duration, continuous inpatient rehabilitation therapy may not be feasible for all patients. Therefore, structured outpatient or home-based exercise training programs are encouraged during the maintenance phase. Approved pharmacological therapies reduce right ventricular afterload and enhance cardiac output, while exercise training addresses peripheral dysfunction—together synergistically improving oxygen delivery and utilization.
Evidence supports the efficacy of supervised home-based rehabilitation therapy in PH, demonstrating improvements in exercise capacity, lower limb muscle strength, activities of daily living (ADL), and health-related quality of life (33). Aerobic training, particularly low-to-moderate intensity, is the modality of choice, whereas high-intensity isometric exercises are generally discouraged due to the risk of syncope. Notably, aerobic exercise may also improve sleep quality and reduce fatigue degree, further contributing to overall patient well-being (34, 35). Additionally, exercise training significantly improved vascular stiffness and right ventricle function, and there is growing interest in the anti-inflammatory effects of exercise on markers including C-Reactive Protein (CRP) and Tumor Necrosis Factor-alpha (TNF-α) as a potential therapeutic mechanism in PH (36, 37). Inflammatory factors play a significant role in the development of PH by driving persistent inflammation and promoting pulmonary vascular remodeling. Reducing inflammatory responses can alleviate the progression of PH. Acute bouts of exercise elevate stress hormone levels, reflecting an immediate stress response. In contrast, long-term exercise training appears to attenuate this response, potentially improving the body’s ability to manage chronic stress and systemic inflammation (38). In summary, exercise training represents a valuable and evidence-based strategy for improving functional status, quality of life, and possibly disease trajectory in patients with PH. When implemented appropriately and in conjunction with targeted medical therapy, it can significantly contribute to comprehensive disease management. However, it must be strictly noted that patients with PH who have contraindications must not undergo exercise training (12). Different types of PH require tailored rehabilitation therapy to improve cardiopulmonary function and enhance muscle strength. Additionally, for patients with PH secondary to left heart disease or lung disease, rehabilitation therapy should primarily focus on controlling the underlying primary disease.
3.2 Inspiratory muscle training
Although exercise intolerance in patients with PH has long been mainly attributed to cardiopulmonary hemodynamic disorders caused by increased pulmonary vascular resistance and increased right ventricular afterload, such as limited right ventricular output, insufficient cardiac output compensation caused by increased PH, ventilation-perfusion imbalance and hypoxemia. Peripheral muscle dysfunction is usually a direct consequence of hemodynamic problems in the PH center and studies have shown that the degree of impairment of respiratory muscle function in PH is greater than that of the surrounding skeletal muscle strength (39, 40). The impaired systemic oxygen uptake rate, as a direct physiological link between central circulation defects and peripheral metabolic dysfunction, forms a harmful feedback loop. Central problems deteriorate peripheral function, and the deterioration of peripheral function further limits overall motor ability and quality of life. This complex interaction indicates that to achieve effective treatment of PH, a multi-pronged strategy must be adopted to address both central hemodynamic abnormalities and peripheral muscle pathological issues simultaneously.
In recent years, accumulating evidence now highlights the significant role of peripheral factors—particularly skeletal and respiratory muscle impairments. These peripheral changes often precede measurable hemodynamic deterioration, further limiting exercise capacity even in early stages of disease. Respiratory muscle dysfunction, especially involving the diaphragm, has emerged as a critical contributor to ventilatory inefficiency and exercise limitation in PH. During exercise training, compromised respiratory muscle function impairs oxygen delivery, predisposing patients to hypoxemia. Diaphragmatic muscle biopsies from patients with PH reveal pathological changes such as muscle fiber atrophy, reduced contractile force, and decreased capillary density (41, 42). These structural alterations culminate in weakened diaphragmatic performance, which contributes to increased dyspnea, reduced ventilatory efficiency, and maladaptive respiratory patterns. Intervention measures should not only be limited to enhancing cardiopulmonary capacity, but also focus on the training of peripheral muscles, especially respiratory muscles. Currently, the main rehabilitation therapy for patients with PH involves training of the inspiratory muscles.
Inspiratory muscle training (IMT) has gained attention as a non-pharmacological intervention to enhance respiratory mechanics and overall functional capacity in PH. IMT strategies encompass abdominal breathing, pursed lip breathing, inspiratory resistance training using threshold devices, and dynamic exercise protocols combined with respiratory control techniques. Abdominal breathing is a breathing technique characterized by the primary use of the diaphragm muscle to draw air deeply into the lungs, resulting in visible expansion of the abdomen rather than the chest. Pursed lip breathing is a controlled breathing technique where you inhale slowly through the nose and exhale gently through pursed lips, as if blowing out a candle or whistling softly. The primary goal is to prolong exhalation and create back-pressure in the airways. A study conducted the first prospective clinical trial of IMT in patients with PH (43). The results show that IMT can serve as an important treatment option to help PH patients improve their exercise capacity and quality of life, and reduce fatigue and breathing difficulties. External diaphragmatic pacemakers (EDP) can enhance the elasticity of the diaphragm and alleviate diaphragmatic atrophy, thereby improving the respiratory function of patients. EDP, as a non-invasive rehabilitation method, can be combined with IMT and applied to patients with PAH. These interventions aim to strengthen respiratory musculature, reduce the sensation of breathlessness, and improve exercise tolerance and quality of life in patients with PH (44). In summary, a comprehensive understanding of the hemodynamic burden and respiratory muscle dysfunction in patients with PH underscores the importance of implementing integrated, multidisciplinary rehabilitation therapy. The combination of various rehabilitation approaches may offer a feasible and clinically valuable adjunctive therapy to improve functional status and quality of life in this complex patient population.
3.3 Neuromuscular electrical stimulation
With the advancement of research, it has become evident that exercise training can exert beneficial effects in patients with PH. However, due to the progressive nature of the disease and its associated symptoms, not all patients are suitable candidates for participation in structured exercise training. Individuals with overt signs or symptoms of advanced right-heart failure, including chest pain, dyspnea, cyanosis of the lips or skin, profound fatigue, near-syncope, abdominal distension, peripheral edema, or hypotension, must engage in exercise training only with the utmost caution and under CPT supervision (45). Neuromuscular Electrical Stimulation (NMES) is a therapeutic technique that employs low-frequency pulsed electrical currents to stimulate nerves and elicit muscle contractions, thereby enhancing muscle function. As a non-invasive and adjustable modality, NMES is widely utilized to improve muscle strength, increase joint range of motion, reduce edema and muscle atrophy, promote tissue healing, and alleviate pain (46, 47). Compared with traditional exercise training, NMES demonstrates significant advantages in situations where movement is not possible or during the early stages of rehabilitation therapy. In patients with chronic obstructive pulmonary disease (COPD), studies have found that NMES can significantly enhance the quality of the quadriceps femoris and effectively improve its function. This is of great significance for the improvement of the overall physical function of patients, especially for those in the stage of severe COPD (48). This result provides support and basis for applying NMES as an innovative treatment approach to patient groups who are unable to undergo conventional pulmonary rehabilitation program for various reasons. There are also similar studies on PH, but the current evidence is limited. Could we consider using NMES as an auxiliary means for routine exercise training and as an alternative method for patients who cannot tolerate physical activity due to the advanced severity of the disease? Notably, NMES imposes a lower metabolic load on the cardiopulmonary system, making it a more tolerable and potentially safer intervention for patients with significant exercise limitations. By improving peripheral muscle strength and functional mobility, NMES represents a valuable therapeutic option in the comprehensive management of PH.
3.4 Psychological interventions
Previous studies on PH mainly focused on reducing the mortality and morbidity rates of patients. However, in recent years, the research perspective has gradually shifted to the profound impact of this disease on patients’ activity ability and life participation. Affected by symptoms such as breathing difficulties and fatigue, PH patients often have difficulty completing some household chores, and in severe cases, they even cannot have long conversations or walk. The limitation of activities leads many patients to have to give up the activities they were once passionate about, and their social scope significantly shrinks. Some patients further actively reduce interaction with relatives and friends due to the concern that “others do not understand.” This widespread functional limitation and participation restriction is inevitably accompanied by significant psychological and social burdens. When with the help of CPT, IMT can be implemented more safely and effectively, leading to greater improvements in respiratory muscle strength, exercise capacity, and dyspnea in symptomatic PH patients (49). PT and OT design and implement individualized functional training programs, aiming to directly improve patients’ activity ability and the efficiency of daily task execution. This improvement in functional status not only helps to alleviate the frustration caused by physiological limitations but also effectively relieves the resulting psychological stress, enhancing the patients’ coping ability and self-efficacy. Ultimately, comprehensive rehabilitation therapy is expected to significantly improve the overall quality of life of this vulnerable group.
4 The role of rehabilitation in pulmonary hypertension and its potential adverse effects
In the assessment of rehabilitation outcomes for patients with PH, various indicators such as 6-minute walk test, Borg Dyspnea Scale, arterial blood gas variables, New York Heart Association(NYHA) function class, pulmonary function tests, echocardiogram, as well as Quality-of-Life Scores (QoL scores) and the number of annual acute exacerbations are typically combined to comprehensively reflect exercise endurance, symptom improvement, optimization of cardiopulmonary function, and long-term prognosis. This review mainly presents 6-minute walk test, maximal oxygen uptake and peak VO₂, and quality of life.
4.1 Exercise capacity
4.1.1 Six-minute walk test
In recent years, invasive cardiopulmonary exercise testing, performed alongside right heart catheterization, has garnered significant attention as a valuable tool for accurately identifying the underlying cardiopulmonary mechanisms driving exercise intolerance in complex clinical conditions (50). However, invasive procedures carry various risks, are costly, have high technical requirements, and may also have the problem of poor patient tolerance. In parallel, the 6-Minute Walk Test (6MWT) remains a simple, cost-effective, safe, and widely accepted method for assessing functional exercise capacity. Developed initially to evaluate endurance in adults with chronic heart failure (51), the 6MWT measures the maximum distance a patient can walk at a self-paced speed on a flat, hard surface during 6 min, allowing for rest as needed, reflecting submaximal exercise capacity. This test provides a practical indicator of physical function and quality of life, as it reflects the ability to perform everyday activities (52). However, performance on the 6MWT is influenced by multiple factors, including gender, age, height, weight, comorbidities, and oxygen requirements.
Evidence-based research supports the utility of the 6MWT in evaluating exercise capacity, monitoring the efficacy of medical interventions, and providing prognostic insights for patients with cardiovascular or respiratory diseases. Its applications have broadened in recent years, particularly as rehabilitation therapy have gained traction. The 6MWT has proven to be an effective tool in assessing treatment impact on exercise capacity and has frequently served as a primary endpoint in trials involving patients with PH (53–56). Notably, predictive equations have been developed to estimate peak VO₂ from 6-minute walk distance (6MWD), offering an alternative to cardiopulmonary exercise testing for patients unable to undergo more rigorous assessments (57).
Clinical trials underscore the benefits of exercise training in patients with PH. In prospective studies, significant improvements in prognostic parameters—including 6MWD, peak VO₂, exercise capacity, and quality of life—have been observed, along with upgrades in WHO functional class (WHO FC). These benefits were most pronounced in patients initially classified as WHO FC IV compared to WHO FC II/III (58). In the randomized controlled trial (RCT) involving patients with severe chronic PH, a 15-week exercise training led to significant gains in 6MWD as compared to the control group (59). Similarly, in patients with PH and chronic thromboembolic pulmonary hypertension (CTEPH), a rehabilitation therapy combining inpatient and home-based interventions—featuring low-intensity aerobic training and respiratory therapy—yielded clinically meaningful improvements in exercise tolerance and 6MWD (60, 61).
Further supporting these findings, a 6-month regimen of combined aerobic and strength training demonstrated substantial improvements in 6MWD without exercise-related adverse events, with benefits persisting for at least 3 months post-intervention (62). Long-term exercise training have proven to be safe and effective in enhancing functional capacity, psychological well-being, and quality of life in patients with PH. Targeted strengthening of lower extremity muscles, particularly the quadriceps, has shown to significantly improve walking ability in patients with muscle atrophy or weakness, as increased muscle strength directly correlates with greater 6MWD (7, 63). Additionally, psychological factors play a critical role in 6MWT performance. Interventions such as psychological support, motivational enhancement, and behavioral therapies have been shown to boost patient confidence and adherence to rehabilitation programs, indirectly improving outcomes on the 6MWT.
A study of a home-based rehabilitation therapy for PH patients further highlights the efficacy of exercise training in improving both functional parameters and quality of life. Remarkably, patients maintained significant gains in respiratory muscle strength and 6MWD even 6 months after completing the rehabilitation therapy (64). These findings collectively underscore the significant and sustained benefits that exercise training, as an integral component of a comprehensive pulmonary rehabilitation program, can deliver for the physical and psychological well-being of patients with PH. This reinforces the critical importance of incorporating such evidence-based rehabilitation therapy into the standard comprehensive care pathway.
4.1.2 Maximal oxygen uptake and peak oxygen uptake
Maximal oxygen uptake (VO₂ max) refers to the highest amount of oxygen an individual can intake and utilize per unit time, serving as a key indicator of cardiorespiratory endurance. An increase in VO₂ max reflects improved cardiorespiratory fitness, and previous studies have demonstrated that VO₂ max in patients with PH significantly improves following exercise training (65). Similarly, peak VO₂ is an essential measure of aerobic capacity and cardiorespiratory function, representing the maximum ability of the body to uptake, deliver, and utilize oxygen during exercise. Evidence suggests that mean peak VO₂ also increases significantly after exercise training (60, 66).
4.2 Quality of life
For patients with PH, the physiological functional impairments caused by the disease progression will significantly reduce their quality of life. This progressive functional limitation not only affects the patients’ ability to take care of themselves in daily life, but also leads to a significant decrease in their working ability and social participation. Therefore, in the clinical management of PH, in addition to the treatment targeting the disease itself, special attention needs to be paid to the assessment and improvement of the patients’ quality of life. Rehabilitation therapy is part of the recommended management plan of PH and is important to better quality of life and exercise tolerance. Exercise training, as an adjunct to disease-targeted pharmacotherapy, can significantly enhance the quality of life in patients with PH (59, 66–69). The study have found that the patients with connective tissue disease-associated pulmonary hypertension (CTD-PH) were given exercise training on the basis of drug treatment, and their quality of life scores were significantly improved after exercise training (70). Compared to control groups, IMT has been shown to improve brachial blood pressure and central blood pressure, alleviate dyspnea, increase respiratory muscle strength, enhance pulmonary carbon monoxide diffusion capacity at total lung capacity, and strengthen knee extensor muscles. Additionally, IMT improves exercise capacity, physical activity, and ADL, while reducing fatigue and anxiety, ultimately enhancing overall quality of life (71). The 36-Item Short Form Health Survey (SF-36), which comprises two composite scales, demonstrates high validity, reliability, and stability in PH. The two summary scores assess physical health and mental health. Higher scores on each subscale indicate better health status.
Studies have shown that long-term exercise training leads to significant improvements in quality of life in PH patients, as measured by the SF-36 (62), as well as through rehabilitation therapy such as plate exercise training (54, 72). Following the rehabilitation therapy, participants in the exercise group demonstrated significant improvements in QoL scores, particularly in mental health, along with positive trends in physical functioning and socialization compared to the control group (60, 73). Collectively, these findings suggest that scientifically structured rehabilitation therapy plays a crucial role in improving both the physical and mental health, as well as the overall quality of life, of patients with PH.
4.3 Adverse events during the intervention
A number of high-quality studies have confirmed that during the individualized rehabilitation therapy for patients with PH under the guidance of CPT, the incidence of adverse events is extremely low. Patients with PH generally do not experience significant adverse effects during rehabilitation interventions. Vigorous aerobic exercise training was not associated with substantial declines in left ventricular systolic or diastolic function in women with PH. Aerobic exercise training may be beneficial for reducing afterload and may preserve left ventricular diastolic function (74). However, some reports indicate that despite the notable improvements in exercise tolerance and quality of life achieved through rehabilitation therapy, there remains a risk of adverse events due to the unique cardiopulmonary limitations and reduced exercise tolerance characteristic of PH patients. The most frequently reported adverse events are cardiac arrhythmias, dyspnea, and respiratory infections (55, 60, 75). For example, in one study involving 183 PH patients who underwent 3 weeks of hospital-based exercise training followed by a home-based program, adverse events such as respiratory infections and syncope were observed in 13% of participants. These findings suggest that while exercise training is an effective adjunct therapy for PH patients, it is not entirely without risk and warrants careful monitoring throughout the intervention period (58).
5 Future directions and opportunities for rehabilitation in pulmonary hypertension
In recent years, the integration of Virtual Reality (VR) technology into rehabilitation therapy has garnered increasing attention, particularly in the management of chronic diseases, where it has demonstrated unique potential. VR seamlessly merges real and virtual environments, enabling the replication of various scenarios to create immersive experiences for users (76). Patients with PH often experience chest discomfort, and invasive procedures such as right heart catheterization or injections may further contribute to pain and distress. Studies have shown that VR technology can effectively distract patients from procedural pain by providing highly immersive virtual environments, thereby significantly reducing their perception of treatment-related discomfort. As an emerging adjunctive therapy, VR offers the advantage of alleviating pain through non-pharmacological means, thus avoiding the potential side effects associated with analgesic medications.
Moreover, PH patients frequently bear significant psychological burdens, including anxiety, depression, and other emotional disturbances, particularly as the disease progresses, all of which directly affects their quality of life. To effectively improve the quality of life of these patients, comprehensive rehabilitation therapy is necessary. On the one hand, VR can provide relaxing experiences—such as virtual exposure to natural environments and guided meditation—that help reduce emotional stress and psychological distress. On the other hand, VR includes low-intensity exercise training to improve cardiorespiratory fitness, thereby continuously improving the quality of life of patients. VR technology facilitates patient engagement in such exercises within a virtual environment, including simulated walking, cycling, and other activities. Real-time monitoring of physiological parameters, such as heart rate and oxygen saturation, through sensors ensures that exercise intensity remains within safe limits. The gamification and interactive features of VR further enhance the appeal of rehabilitation therapy, mitigating monotony and boosting patient participation and motivation.
In addition to its therapeutic applications, VR holds significant promise in medical education. Three-dimensional visualization allows VR to vividly illustrate the pathophysiology and treatment processes of PH, aiding patients in comprehending disease progression and drug mechanisms. Simulations of medication use and standardized rehabilitation instructions can strengthen patients’ adherence to treatment and foster a sense of empowerment and confidence. Despite its considerable promise, the widespread adoption of VR technology remains limited by the high costs associated with equipment and software. Furthermore, individual variability means that not all patients tolerate VR well. Some patients may experience dizziness, nausea, imbalance, or coordination difficulties, leading to poor adaptability (77). Significantly, although the potential of VR in PH management is substantial, current research in this area is limited. Further RCT are urgently needed to validate its efficacy and safety, thereby establishing a stronger clinical evidence base for the application of VR technology in the treatment of PH.
6 Conclusion
In the management of PH, pharmacological therapy remains the cornerstone, as medications can improve patients’ hemodynamics. However, rehabilitation is emerging as an effective adjunct therapy that is garnering increasing attention. Systematic rehabilitation has been shown to significantly enhance exercise tolerance and quality of life in PH patients. It is important to emphasize that rehabilitation is not a replacement for medication, but rather serves as a vital complementary approach. Patients should receive optimized pharmacological treatment for at least 3 months before initiating a structured rehabilitation therapy to ensure clinical stability. By integrating systematic rehabilitation with optimized medication, a synergistic effect can be achieved, resulting in improved quality of life and functional status for PH patients. This comprehensive management strategy embodies the principle of patient-centered care, focusing not only on effective disease control but also on overall health, long-term prognosis, and quality of life, striving for an optimal balance between survival and well-being.
A variety of rehabilitation therapy approaches, including exercise training, IMT, NMES, and psychological interventions, have demonstrated benefits in enhancing exercise capacity and cardiorespiratory function in PH patients. Gradual increases in exercise intensity can improve the body’s oxygen utilization efficiency without placing undue strain on the heart. Exercise training during rehabilitation therapy also promotes the release of endorphins, improves mood, and enhances cognitive performance. As a result, patients’ functional abilities and ADL are enhanced to varying degrees. Importantly, the safety and feasibility of rehabilitation in PH have been increasingly validated, with studies indicating that rehabilitation is safe when conducted under professional supervision. In addition, patient and family education is a critical component of rehabilitation, fostering a better understanding of the disease and the importance of ongoing rehabilitation, thereby enhancing self-management capabilities (Figure 1).
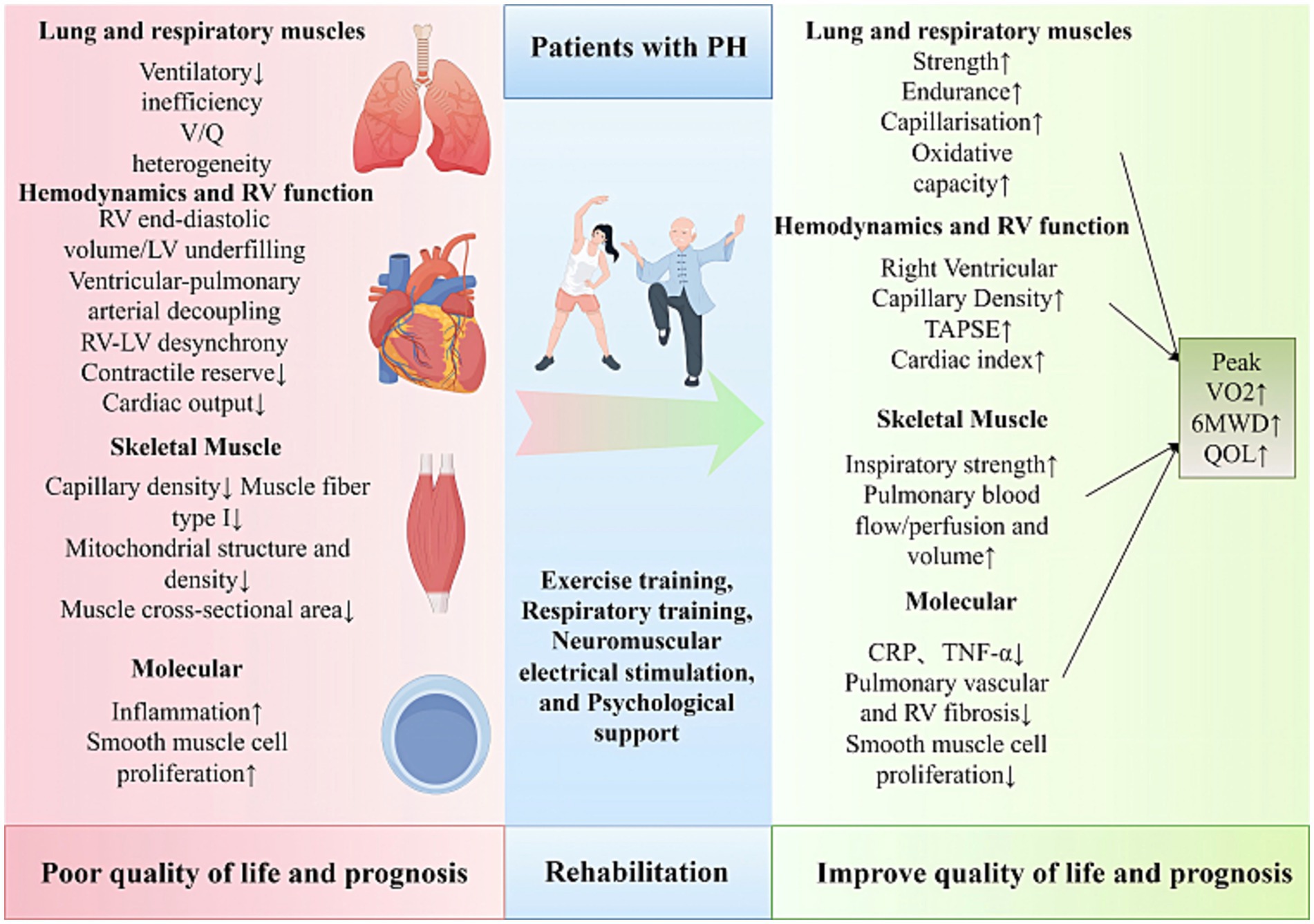
Figure 1. Clinical benefits of exercise training for pulmonary hypertension. 6MWD, 6-Minute Walk Distance; CRP, C-Reactive Protein; LV, Left Ventricle; QOL, Quality of Life; RV, Right Ventricle; TNF-α, Tumor Necrosis Factor-alpha; TAPSE, Tricuspid Annular Plane Systolic Excursion; V/ Q, Ventilation/ Perfusion.
Looking forward, more high-quality RCTs are needed to clarify the specific indications and applicability of rehabilitation therapy across different PH patient subtypes. Further investigation is warranted to establish evidence-based exercise prescriptions for PH, including optimal modalities, intensity parameters, intervention duration, supervision requirements, and implementation settings. Long-term follow-up studies are essential to evaluate the sustainability of rehabilitation benefits and to assess their impact on key outcomes such as time to clinical deterioration and survival. Furthermore, comprehensive clinical data regarding adverse events during rehabilitation therapy are necessary to inform the continual refinement of rehabilitation programs for PH patients.
Author contributions
YL: Writing – original draft, Writing – review & editing. XG: Writing – original draft, Writing – review & editing. PL: Writing – original draft, Writing – review & editing. SJ: Writing – original draft, Writing – review & editing. FW: Writing – original draft, Writing – review & editing. FL: Writing – original draft, Writing – review & editing. PY: Writing – original draft, Writing – review & editing. XW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by y the Program of Key Research and Development projects in Hainan Province (ZDYF2024SHFZ057), Joint Research Development Project between Shenkang and United Imaging on Clinical Research and Translation (SKLY2022CRT202), Program of National Natural Science Foundation of China (82370057), the Program of Natural Science Foundation of Shanghai (22ZR1452400).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer YS declared a shared affiliation with the authors SJ, FW, FL, and PY to the handling editor at the time of review.
The handling editor J-ML declared a shared affiliation with the authors SJ, FW, FL, and PY at the time of review.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hoeper, MM, Humbert, M, Souza, R, Idrees, M, Kawut, SM, Sliwa-Hahnle, K, et al. A global view of pulmonary hypertension. Lancet Respir Med. (2016) 4:306–22. doi: 10.1016/S2213-2600(15)00543-3
2. Gomberg-Maitland, M, Bull, TM, Saggar, R, Barst, RJ, Elgazayerly, A, Fleming, TR, et al. New trial designs and potential therapies for pulmonary artery hypertension. J Am Coll Cardiol. (2013) 62:D82–91. doi: 10.1016/j.jacc.2013.10.026
3. Ganderton, L, Jenkins, S, Gain, K, Fowler, R, Winship, P, Lunt, D, et al. Short term effects of exercise training on exercise capacity and quality of life in patients with pulmonary arterial hypertension: protocol for a randomised controlled trial. BMC Pulm Med. (2011) 11:25. doi: 10.1186/1471-2466-11-25
4. Butāne, L, Spilva-Ekerte, L, Skride, A, and Šmite, D. Individually tailored remote physiotherapy program improves participation and autonomy in activities of everyday life along with exercise capacity, self-efficacy, and low-moderate physical activity in patients with pulmonary arterial hypertension: a randomized controlled study. Medicina (Kaunas). (2022) 58:662. doi: 10.3390/medicina58050662
5. Galiè, N, Channick, RN, Frantz, RP, Grünig, E, Jing, ZC, Moiseeva, O, et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur Respir J. (2019) 53:1801889. doi: 10.1183/13993003.01889-2018
6. Lai, YC, Provencher, S, and Goncharova, EA. TAKling GDF-15 and skeletal muscle atrophy in pulmonary hypertension: are we there yet? Thorax. (2019) 74:103–5. doi: 10.1136/thoraxjnl-2018-212680
7. Grünig, E, Eichstaedt, C, Barberà, JA, Benjamin, N, Blanco, I, Bossone, E, et al. ERS statement on exercise training and rehabilitation in patients with severe chronic pulmonary hypertension. Eur Respir J. (2019) 53:1800332. doi: 10.1183/13993003.00332-2018
8. Nickel, NP, Yuan, K, Dorfmuller, P, Provencher, S, Lai, YC, Bonnet, S, et al. Beyond the lungs: systemic manifestations of pulmonary arterial hypertension. Am J Respir Crit Care Med. (2020) 201:148–57. doi: 10.1164/rccm.201903-0656CI
9. Ley, S, Fink, C, Risse, F, Ehlken, N, Fischer, C, Ley-Zaporozhan, J, et al. Magnetic resonance imaging to assess the effect of exercise training on pulmonary perfusion and blood flow in patients with pulmonary hypertension. Eur Radiol. (2013) 23:324–31. doi: 10.1007/s00330-012-2606-z
10. Malenfant, S, Lebret, M, Breton-Gagnon, É, Potus, F, Paulin, R, Bonnet, S, et al. Exercise intolerance in pulmonary arterial hypertension: insight into central and peripheral pathophysiological mechanisms. Eur Respir Rev. (2021) 30:200284. doi: 10.1183/16000617.0284-2020
11. Mainguy, V, Maltais, F, Saey, D, Gagnon, P, Martel, S, Simon, M, et al. Effects of a rehabilitation program on skeletal muscle function in idiopathic pulmonary arterial hypertension. J Cardiopulm Rehabil Prev. (2010) 30:319–23. doi: 10.1097/HCR.0b013e3181d6f962
12. Humbert, M, Kovacs, G, Hoeper, MM, Badagliacca, R, Berger, RMF, Brida, M, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. (2022) 43:3618–731. doi: 10.1093/eurheartj/ehac237
13. Wijeratne, DT, Lajkosz, K, Brogly, SB, Lougheed, MD, Jiang, L, Housin, A, et al. Increasing incidence and prevalence of World Health Organization groups 1 to 4 pulmonary hypertension: a population-based cohort study in Ontario, Canada. Circ Cardiovasc Qual Outcomes. (2018) 11:e003973. doi: 10.1161/CIRCOUTCOMES.117.003973
14. Leggio, M, Fusco, A, Limongelli, G, and Sgorbini, L. Exercise training in patients with pulmonary and systemic hypertension: a unique therapy for two different diseases. Eur J Intern Med. (2018) 47:17–24. doi: 10.1016/j.ejim.2017.09.010
15. Santos-Lozano, A, Fiuza-Luces, C, Fernández-Moreno, D, Llavero, F, Arenas, J, López, JA, et al. Exercise benefits in pulmonary hypertension. J Am Coll Cardiol. (2019) 73:2906–7. doi: 10.1016/j.jacc.2019.03.489
16. He, M, Jiang, R, Fei-Sun, JS, Cao, JX, Wang, L, and Shi, JY. Cardiac magnetic resonance imaging-derived septum swing index detects pulmonary hypertension: A diagnostic study. J Transl Int Med. (2023) 11:459–467. doi: 10.2478/jtim-2023-0114
17. Eichstaedt, CA, Benjamin, N, Xanthouli, P, Marra, AM, and Grünig, E. The role of rehabilitation in patients with pulmonary arterial hypertension. Curr Opin Pulm Med. (2019) 25:398–404. doi: 10.1097/MCP.0000000000000609
18. Jacobs, W, van de Veerdonk, MC, Trip, P, de Man, F, Heymans, MW, Marcus, JT, et al. The right ventricle explains sex differences in survival in idiopathic pulmonary arterial hypertension. Chest. (2014) 145:1230–6. doi: 10.1378/chest.13-1291
19. Hatton, N, and Ryan, JJ. Sex differences in response to pulmonary arterial hypertension therapy: is what's good for the goose, good for the gander? Chest. (2014) 145:1184–6. doi: 10.1378/chest.13-3061
20. Adu-Amankwaah, J, Shi, Y, Song, H, Ma, Y, Liu, J, Wang, H, et al. Signaling pathways and targeted therapy for pulmonary hypertension. Signal Transduct Target Ther. (2025) 10:207. doi: 10.1038/s41392-025-02287-8
21. Yang, Y, Zeng, Z, Yang, Q, Wang, H, Zhang, H, Yan, W, et al. The challenge in burden of pulmonary arterial hypertension: a perspective from the global burden of disease study. MedComm. (2020) 202:e70175. doi: 10.1002/mco2.70175
22. Galiè, N, Corris, PA, Frost, A, Girgis, RE, Granton, J, Jing, ZC, et al. Updated treatment algorithm of pulmonary arterial hypertension. J Am Coll Cardiol. (2013) 62:D60–72. doi: 10.1016/j.jacc.2013.10.031
23. Galie, N, Manes, A, and Palazzini, M. Exercise training in pulmonary hypertension: improving performance but waiting for outcome. Eur Heart J. (2016) 37:45–8. doi: 10.1093/eurheartj/ehv440
24. Batt, J, Ahmed, SS, Correa, J, Bain, A, and Granton, J. Skeletal muscle dysfunction in idiopathic pulmonary arterial hypertension. Am J Respir Cell Mol Biol. (2014) 50:74–86. doi: 10.1165/rcmb.2012-0506OC
25. Leggio, M, Fusco, A, Armeni, M, D'Emidio, S, Severi, P, Calvaruso, S, et al. Pulmonary hypertension and exercise training: a synopsis on the more recent evidences. Ann Med. (2018) 50:226–33. doi: 10.1080/07853890.2018.1432887
26. Naci, B, Demir, R, Onder, OO, Sinan, UY, and Kucukoglu, MS. Effects of adding respiratory training to osteopathic manipulative treatment on exhaled nitric oxide level and cardiopulmonary function in patients with pulmonary arterial hypertension. Am J Cardiol. (2022) 162:184–90. doi: 10.1016/j.amjcard.2021.09.023
27. Martínez-Quintana, E, Miranda-Calderín, G, Ugarte-Lopetegui, A, and Rodríguez-González, F. Rehabilitation program in adult congenital heart disease patients with pulmonary hypertension. Congenit Heart Dis. (2010) 5:44–50. doi: 10.1111/j.1747-0803.2009.00370.x
28. Nagel, C, Prange, F, Guth, S, Herb, J, Ehlken, N, Fischer, C, et al. Exercise training improves exercise capacity and quality of life in patients with inoperable or residual chronic thromboembolic pulmonary hypertension. PLoS One. (2012) 7:e41603. doi: 10.1371/journal.pone.0041603
29. Bigot, M, Guy, JM, Monpere, C, Cohen-Solal, A, Pavy, B, Iliou, MC, et al. Cardiac rehabilitation recommendations of the group exercise rehabilitation sports - prevention (GERS-P) of the French Society of Cardiology: 2023 update. Arch Cardiovasc Dis. (2024) 117:521–41. doi: 10.1016/j.acvd.2024.05.119
30. Paolillo, S, Farina, S, Bussotti, M, Iorio, A, PerroneFilardi, P, Piepolil, MF, et al. Exercise testing in the clinical management of patients affected by pulmonary arterial hypertension. Eur J Prev Cardiol. (2012) 19:960–71. doi: 10.1177/1741826711426635
31. Benza, RL, Miller, DP, Barst, RJ, Badesch, DB, Frost, AE, and McGoon, MD. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL registry. Chest. (2012) 142:448–56. doi: 10.1378/chest.11-1460
32. O'Callaghan, DS, and Humbert, M. A critical analysis of survival in pulmonary arterial hypertension. Eur Respir Rev. (2012) 21:218–22. doi: 10.1183/09059180.00003512
33. Inagaki, T, Terada, J, Tanabe, N, Kawata, N, Kasai, H, Sugiura, T, et al. Home-based pulmonary rehabilitation in patients with inoperable or residual chronic thromboembolic pulmonary hypertension: a preliminary study. Respir Investig. (2014) 52:357–64. doi: 10.1016/j.resinv.2014.07.002
34. Atef, H, and Abdeen, H. Effect of exercise on sleep and cardiopulmonary parameters in patients with pulmonary artery hypertension. Sleep Breath. (2021) 25:1953–60. doi: 10.1007/s11325-020-02286-9
35. Weinstein, AA, Chin, LM, Keyser, RE, Kennedy, M, Nathan, SD, Woolstenhulme, JG, et al. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med. (2013) 107:778–84. doi: 10.1016/j.rmed.2013.02.006
36. Richter, MJ, Grimminger, J, Krüger, B, Ghofrani, HA, Mooren, FC, Gall, H, et al. Effects of exercise training on pulmonary hemodynamics, functional capacity and inflammation in pulmonary hypertension. Pulm Circ. (2017) 7:20–37. doi: 10.1086/690553
37. Nagel, C, Benjamin, N, Egenlauf, B, Eichstaedt, CA, Fischer, C, Palevičiūtė, E, et al. Effect of supervised training therapy on pulmonary arterial compliance and stroke volume in severe pulmonary arterial hypertension and inoperable or persistent chronic thromboembolic pulmonary hypertension. Respiration. (2021) 100:369–78. doi: 10.1159/000512316
38. Hackney, AC, and Lane, AR. Exercise and the regulation of endocrine hormones. Prog Mol Biol Transl Sci. (2015) 135:293–311. doi: 10.1016/bs.pmbts.2015.07.001
39. Kabitz, HJ, Schwoerer, A, Bremer, HC, Sonntag, F, Walterspacher, S, Walker, D, et al. Impairment of respiratory muscle function in pulmonary hypertension. Clin Sci (Lond). (2008) 114:165–71. doi: 10.1042/CS20070238
40. Manders, E, de Man, FS, Handoko, ML, Westerhof, N, van Hees, HW, Stienen, GJ, et al. Diaphragm weakness in pulmonary arterial hypertension: role of sarcomeric dysfunction. Am J Physiol Lung Cell Mol Physiol. (2012) 303:L1070–8. doi: 10.1152/ajplung.00135.2012
41. Potus, F, Malenfant, S, Graydon, C, Mainguy, V, Tremblay, È, Breuils-Bonnet, S, et al. Impaired angiogenesis and peripheral muscle microcirculation loss contribute to exercise intolerance in pulmonary arterial hypertension. Am J Respir Crit Care Med. (2014) 190:318–28. doi: 10.1164/rccm.201402-0383OC
42. de Man, FS, van Hees, HW, Handoko, ML, Niessen, HW, Schalij, I, Humbert, M, et al. Diaphragm muscle fiber weakness in pulmonary hypertension. Am J Respir Crit Care Med. (2011) 183:1411–8. doi: 10.1164/rccm.201003-0354OC
43. Saglam, M, Arikan, H, Vardar-Yagli, N, Calik-Kutukcu, E, Inal-Ince, D, Savci, S, et al. Inspiratory muscle training in pulmonary arterial hypertension. J Cardiopulm Rehabil Prev. (2015) 35:198–206. doi: 10.1097/HCR.0000000000000117
44. Tran, D, Munoz, P, Lau, EMT, Alison, JA, Brown, M, Zheng, Y, et al. Inspiratory muscle training improves inspiratory muscle strength and functional exercise capacity in pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: a pilot randomised controlled study. Heart Lung Circ. (2021) 30:388–95. doi: 10.1016/j.hlc.2020.06.006
45. Chiu, YW, and Huang, WC. Cardiopulmonary exercise test and rehabilitation for pulmonary hypertension patients. Acta Cardiol Sin. (2022) 38:663–6. doi: 10.6515/ACS.202211_38(6).20220603A
46. Doucet, BM, Lam, A, and Griffin, L. Neuromuscular electrical stimulation for skeletal muscle function. Yale J Biol Med. (2012) 85:201–15.
47. Kahraman, BO, Savci, S, Ozsoy, I, Baran, A, Acar, S, Ozpelit, E, et al. Effects of neuromuscular electrical stimulation in patients with pulmonary arterial hypertension: a randomized controlled pilot study. J Cardiol. (2020) 75:702–8. doi: 10.1016/j.jjcc.2019.12.013
48. Maddocks, M, Nolan, CM, Man, WD, Polkey, MI, Hart, N, Gao, W, et al. Neuromuscular electrical stimulation to improve exercise capacity in patients with severe COPD: a randomised double-blind, placebo-controlled trial. Lancet Respir Med. (2016) 4:27–36. doi: 10.1016/S2213-2600(15)00503-2
49. da Fontoura, FF, Roncato, G, Meyer, GMB, da Luz Goulart, C, Spilimbergo, FB, Cipriano Junior, G, et al. Inspiratory muscle training on exercise capacity, dyspnoea and health status in pulmonary hypertension: a randomised controlled trial. Respirology. (2025) 30:760–9. doi: 10.1111/resp.70054
50. Oldham, WM, Oliveira, RKF, Wang, RS, Opotowsky, AR, Rubins, DM, Hainer, J, et al. Network analysis to risk stratify patients with exercise intolerance. Circ Res. (2018) 122:864–76. doi: 10.1161/CIRCRESAHA.117.312482
51. Guyatt, GH, Sullivan, MJ, Thompson, PJ, Fallen, EL, Pugsley, SO, Taylor, DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. (1985) 132:919–23. doi: 10.2478/jtim-2023-0114
52. Enright, PL, and Sherrill, DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. (1998) 158:1384–7. doi: 10.1164/ajrccm.158.5.9710086
53. Galiè, N, Manes, A, Negro, L, Palazzini, M, Bacchi-Reggiani, ML, and Branzi, A. A meta-analysis of randomized controlled trials in pulmonary arterial hypertension. Eur Heart J. (2009) 30:394–403. doi: 10.1093/eurheartj/ehp022
54. Becker-Grünig, T, Klose, H, Ehlken, N, Lichtblau, M, Nagel, C, Fischer, C, et al. Efficacy of exercise training in pulmonary arterial hypertension associated with congenital heart disease. Int J Cardiol. (2013) 168:375–81. doi: 10.1016/j.ijcard.2012.09.036
55. Grünig, E, Ehlken, N, Ghofrani, A, Staehler, G, Meyer, FJ, Juenger, J, et al. Effect of exercise and respiratory training on clinical progression and survival in patients with severe chronic pulmonary hypertension. Respiration. (2011) 81:394–401. doi: 10.1159/000322475
56. Fox, BD, Kassirer, M, Weiss, I, Raviv, Y, Peled, N, Shitrit, D, et al. Ambulatory rehabilitation improves exercise capacity in patients with pulmonary hypertension. J Card Fail. (2011) 17:196–200. doi: 10.1016/j.cardfail.2010.10.004
57. Ross, RM, Murthy, JN, Wollak, ID, and Jackson, AS. The six minute walk test accurately estimates mean peak oxygen uptake. BMC Pulm Med. (2010) 10:31. doi: 10.1186/1471-2466-10-31
58. Grünig, E, Lichtblau, M, Ehlken, N, Ghofrani, HA, Reichenberger, F, Staehler, G, et al. Safety and efficacy of exercise training in various forms of pulmonary hypertension. Eur Respir J. (2012) 40:84–92. doi: 10.1183/09031936.00123711
59. Mereles, D, Ehlken, N, Kreuscher, S, Ghofrani, S, Hoeper, MM, Halank, M, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. (2006) 114:1482–9. doi: 10.1161/CIRCULATIONAHA.106.61
60. Grünig, E, MacKenzie, A, Peacock, AJ, Eichstaedt, CA, Benjamin, N, Nechwatal, R, et al. Standardized exercise training is feasible, safe, and effective in pulmonary arterial and chronic thromboembolic pulmonary hypertension: results from a large European multicentre randomized controlled trial. Eur Heart J. (2021) 42:2284–95. doi: 10.1093/eurheartj/ehaa696
61. Fukui, S, Ogo, T, Takaki, H, Ueda, J, Tsuji, A, Morita, Y, et al. Efficacy of cardiac rehabilitation after balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Heart. (2016) 102:1403–9. doi: 10.1136/heartjnl-2015-309230
62. Kagioglou, O, Mouratoglou, SA, Giannakoulas, G, Kapoukranidou, D, Anifanti, M, Deligiannis, A, et al. Long-term effect of an exercise training program on physical functioning and quality of life in pulmonary hypertension: a randomized controlled trial. Biomed Res Int. (2021) 2021:8870615. doi: 10.1155/2021/8870615
63. Ertan, O, Aslan, GK, Akinci, B, Bilge, AK, Inanc, M, and Okumus, G. Effect of ground-based walk training in pulmonary hypertension. Am J Cardiol. (2022) 174:172–8. doi: 10.1016/j.amjcard.2022.03.040
64. Wojciuk, M, Ciolkiewicz, M, Kuryliszyn-Moskal, A, Chwiesko-Minarowska, S, Sawicka, E, Ptaszynska-Kopczynska, K, et al. Effectiveness and safety of a simple home-based rehabilitation program in pulmonary arterial hypertension: an interventional pilot study. BMC Sports Sci Med Rehabil. (2021) 13:79. doi: 10.1186/s13102-021-00315-y
65. González-Saiz, L, Fiuza-Luces, C, Sanchis-Gomar, F, Santos-Lozano, A, Quezada-Loaiza, CA, Flox-Camacho, A, et al. Benefits of skeletal-muscle exercise training in pulmonary arterial hypertension: the WHOLEi+12 trial. Int J Cardiol. (2017) 231:277–83. doi: 10.1016/j.ijcard.2016.12.026
66. Ehlken, N, Lichtblau, M, Klose, H, Weidenhammer, J, Fischer, C, Nechwatal, R, et al. Exercise training improves peak oxygen consumption and haemodynamics in patients with severe pulmonary arterial hypertension and inoperable chronic thrombo-embolic pulmonary hypertension: a prospective, randomized, controlled trial. Eur Heart J. (2016) 37:35–44. doi: 10.1093/eurheartj/ehv337
67. Bussotti, M, Gremigni, P, Pedretti, RFE, Kransinska, P, Di Marco, S, Corbo, P, et al. Effects of an outpatient service rehabilitation Programme in patients affected by pulmonary arterial hypertension: an observational study. Cardiovasc Hematol Disord Drug Targets. (2017) 17:3–10. doi: 10.2174/1871529X16666161130123937
68. Aslan, GK, Akıncı, B, Yeldan, I, and Okumus, G. A randomized controlled trial on inspiratory muscle training in pulmonary hypertension: effects on respiratory functions, functional exercise capacity, physical activity, and quality of life. Heart Lung. (2020) 49:381–7. doi: 10.1016/j.hrtlng.2020.01.014
69. Talwar, A, Sahni, S, Verma, S, Khan, SZ, Dhar, S, and Kohn, N. Exercise tolerance improves after pulmonary rehabilitation in pulmonary hypertension patients. J Exerc Rehabil. (2017) 13:214–7. doi: 10.12965/jer.1732872.436
70. Grünig, E, Maier, F, Ehlken, N, Fischer, C, Lichtblau, M, Blank, N, et al. Exercise training in pulmonary arterial hypertension associated with connective tissue diseases. Arthritis Res Ther. (2012) 14:R148. doi: 10.1186/ar3883
71. Ozcan Kahraman, B, Tanriverdi, A, Savci, S, Odaman, H, Akdeniz, B, Sevinc, C, et al. Effects of inspiratory muscle training in patients with pulmonary hypertension. Am J Cardiol. (2023) 203:406–13. doi: 10.1016/j.amjcard.2023.06.097
72. Chan, L, Chin, LMK, Kennedy, M, Woolstenhulme, JG, Nathan, SD, Weinstein, AA, et al. Benefits of intensive treadmill exercise training on cardiorespiratory function and quality of life in patients with pulmonary hypertension. Chest. (2013) 143:333–43. doi: 10.1378/chest.12-0993
73. Yılmaz, BC, Güçlü, MB, Keleş, MN, Taçoy, GA, and Çengel, A. Effects of upper extremity aerobic exercise training on oxygen consumption, exercise capacity, dyspnea and quality of life in patients with pulmonary arterial hypertension. Heart Lung. (2020) 49:564–71. doi: 10.1016/j.hrtlng.2020.04.006
74. Woolstenhulme, JG, Guccione, AA, Herrick, JE, Collins, JP, Nathan, SD, Chan, L, et al. Left ventricular function before and after aerobic exercise training in women with pulmonary arterial hypertension. J Cardiopulm Rehabil Prev. (2019) 39:118–26. doi: 10.1097/HCR.0000000000000397
75. Babu, AS, Padmakumar, R, Nayak, K, Shetty, R, Mohapatra, AK, and Maiya, AG. Effects of home-based exercise training on functional outcomes and quality of life in patients with pulmonary hypertension: a randomized clinical trial. Indian Heart J. (2019) 71:161–5. doi: 10.1016/j.ihj.2019.03.002
76. Zhao, J, Zhang, X, Lu, Y, Wu, X, Zhou, F, Yang, S, et al. Virtual reality technology enhances the cognitive and social communication of children with autism spectrum disorder. Front Public Health. (2022) 10:1029392. doi: 10.3389/fpubh.2022.1029392
77. Lambert, V, Boylan, P, Boran, L, Hicks, P, Kirubakaran, R, Devane, D, et al. Virtual reality distraction for acute pain in children. Cochrane Database Syst Rev. (2020) 10:Cd010686. doi: 10.1002/14651858.CD010686.pub2
Keywords: pulmonary hypertension, rehabilitation, exercise limitation, exercise, quality of life
Citation: Liu Y, Guo X, Liu P, Jia S, Wang F, Li F, Yuan P and Wang X (2025) Rehabilitation applications and progress in managing pulmonary hypertension. Front. Med. 12:1659818. doi: 10.3389/fmed.2025.1659818
Edited by:
Jin-Ming Liu, Tongji University, ChinaReviewed by:
Yuanyuan Sun, Tongji University, ChinaChun Feng, Shanghai First Rehabilitation Hospital, China
Copyright © 2025 Liu, Guo, Liu, Jia, Wang, Li, Yuan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fei Li, ZmVsaXhfYmV5b25kQGhvdG1haWwuY29t; Ping Yuan, cGFuZHl5dWFuQHRvbmdqaS5lZHUuY24=; Xuejing Wang, a2Z3eGpAd2ZtYy5lZHUuY24=
†These authors have contributed equally to this work
 Yuyan Liu
Yuyan Liu Xiao Guo1,2†
Xiao Guo1,2† Fei Li
Fei Li Ping Yuan
Ping Yuan