- 1Department of Neurosurgery, University Medical Center of the Johannes Gutenberg-University of Mainz, Mainz, Germany
- 2Department of Neuroradiology, University Medical Center of the Johannes Gutenberg-University of Mainz, Mainz, Germany
- 3Institute of Medical Biostatistics, Epidemiology and Informatics, University Medical Center of the Johannes Gutenberg-University of Mainz, Mainz, Germany
A Correction on
Evaluation of the SOFA score as a tool to predict DCI-associated infarctions after spontaneous subarachnoid hemorrhage
by Kurz, E., Fassl, V., Brockmann, C., Schulze, A., Kalasauskas, D., Ringel, F., and Neulen, A. (2025). Front. Med. 12:1580643. doi: 10.3389/fmed.2025.1580643
There was a mistake in Figure 1 as published. There are incorrect values in section C of the figure. The corrected Figure 1 appears below.
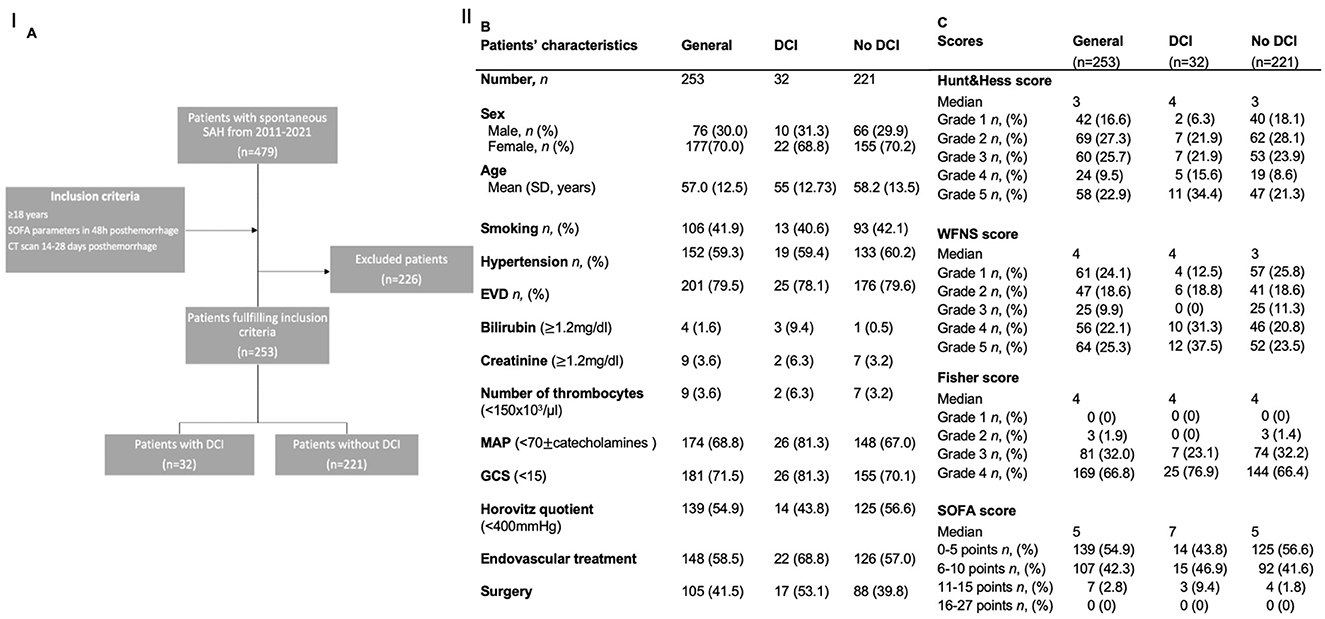
Figure 1. (A) Flowchart illustrating the selection process for the inclusion of patients. (B, C) Demographics and scores of the study population and for the subgroups of patients with and without DCI. AUC: area under the curve; DCI: delayed cerebral infarctions; EVD: external ventricular drainage; MCA: middle cerebral artery; ICA: internal cerebral artery; SD: standard deviation; SOFA: Sequential Organ Failure Assessment score; WFNS: World Federation of Neurosurgical Societies score.
The original version of this article has been updated.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: subarachnoid hemorrhage, SAH, delayed cerebral ischemia, DCI, Sequential Organ Failure Assessment score, SOFA score, clinical
Citation: Kurz E, Fassl V, Brockmann C, Schulze A, Kalasauskas D, Ringel F and Neulen A (2025) Correction: Evaluation of the SOFA score as a tool to predict DCI-associated infarctions after spontaneous subarachnoid hemorrhage. Front. Med. 12:1661506. doi: 10.3389/fmed.2025.1661506
Received: 07 July 2025; Accepted: 19 August 2025;
Published: 19 September 2025.
Edited and reviewed by: Ata Murat Kaynar, University of Pittsburgh, United States
Copyright © 2025 Kurz, Fassl, Brockmann, Schulze, Kalasauskas, Ringel and Neulen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elena Kurz, ZWxlbmFrdXJ6QHQtb25saW5lLmRl; Axel Neulen, YXhlbC5uZXVsZW5AdW5pbWVkaXppbi1tYWluei5kZQ==
 Elena Kurz
Elena Kurz Verena Fassl1
Verena Fassl1 Darius Kalasauskas
Darius Kalasauskas Florian Ringel
Florian Ringel Axel Neulen
Axel Neulen