Abstract
Background:
School-based vision screening plays a vital role in identifying visual problems at an early stage. There is limited evidence on the frequency of visual impairment and its associated risk factors among school-aged children.
Objective:
This research aimed to assess the prevalence of visual impairment and its associated risk factors among school children enrolled in Government Schools of Rawalpindi.
Methodology:
An analytical cross-sectional study was conducted among 320 schoolchildren in the Rawalpindi district of Punjab province from July to December 2024. Presenting visual acuity was assessed using the validated Peek Acuity app on smartphone with the tumbling E optotypes. Visual impairment was defined as presenting visual acuity worse than 6/12, based on failure to correctly identify at least four out of five optotypes at the 6/12 level at a testing distance of 3 m. A validated questionnaire was utilized to assess risk factors associated with visual impairment. The prevalence of visual impairment was presented as frequencies and percentages. Binary logistic regression was performed with visual impairment as the dependent variable, considering age, gender, father's educational status, mother's educational status, household income, maternal illness during pregnancy, parent with visual impairment, sibling with visual impairment, birth weight, gestational age, complications at birth, serious infection during childhood, history of head trauma or injury, duration of television exposure, and duration of mobile/computer exposure as independent variables. Variables with a p < 0.05 and a 95% confidence interval in the multivariate model were considered statistically significant.
Results:
A total of 320 study participants were included in this study. Visual impairment was identified in 82 children (25.6%), consisting of 35 males (42.68%) and 47 females (57.3%). It was categorized as mild in 30 (36.58%) and moderate in 52 (63.41%) children. In multivariate analysis, parent with visual impairment [4.201 (2.221–7.948)], low birth weight [0.376 (0.189–0.749)], small gestational age [0.231 (0.113–0.475)] and exposure to mobile and computer devices [2.368 (1.040–5.393)] were factors significantly associated with visual impairment.
Conclusion:
This study identified a high burden of visual impairment among schoolchildren, with a greater proportion observed in females and predominantly presenting with moderate severity.
1 Introduction
According to universal estimates, there are around 19 million children with visual impairment globally, the majority of whom live in low- and middle-income countries (LMICs) (1). Pakistan ranks third among 20 countries most affected by blindness and moderate to severe visual impairment, following India and Bangladesh (2). It is estimated that over two million children in Pakistan are living with blindness or visual impairment (3). However, the burden of vision loss in Pakistan in the last one decade remained unclear (2).
Visual impairment in children is caused by a variety of factors, with uncorrected refractive errors being the leading cause, both in children and adults (4). Additionally, recent systematic review (2000–2020) reported that uncorrected refractive errors are the most prevalent cause of vision impairment among children (1).
Evidence indicates that uncorrected refractive errors in infancy and early childhood may lead to developmental delays (5) and are associated with clinically recognized deficits in cognitive and visual-motor skills (6). Visual impairment during childhood poses significant barriers to learning (7), development, and academic achievement, which can ultimately affect future employment prospects and socioeconomic standing (8, 9).
The World Health Organization (WHO) has prioritized the correction of refractive errors as one of the target areas to eliminate avoidable causes of visual impairment (10, 11) while majority of causes of visual impairment can be prevented or treated using highly cost effective measures (12). Conventional ophthalmic tools are expensive, non-portable, and require specialized training, limiting their accessibility (13). Thus, there is a need for accessible, self-manageable, and automated tools for visual acuity tests to increase early detection and timely assistance for those with visual impairment (14). With rising global smartphone use, mobile health (mHealth) approaches are increasingly recognized as cost-effective, user-friendly tools for early detection and management of visual impairment (15). Some studies have introduced innovative mobile-based visual acuity testing methods, including a validated mobile app shown to produce results comparable to standard Snellen charts (16, 17).
This study investigates the use of smartphone-based vision screening to address the high burden of undiagnosed visual impairment among schoolchildren in underserved communities of Rawalpindi, Pakistan. In addition, this study aimed to identify the underlying factors associated with visual impairment among children, addressing a critical gap in the existing evidence.
2 Materials and methods
An analytical cross-sectional study was conducted in Federal Government schools in Rawalpindi district of Punjab province from July to December 2024 using two stage probability sampling technique. Based upon the list of all FG schools obtained from FGEI, four schools among 22 were selected randomly using computer generated numbers. The total sample size was distributed proportionally based on their population size to the selected schools. Next the stratified random sampling was employed. A list of students was obtained from each school. Children were stratified on the basis of age and gender and selected proportionally (Figure 1). Study participants were 5–15 years of age as per WHO recommendations for vision screening (18), male and female (in equal proportion).
Figure 1
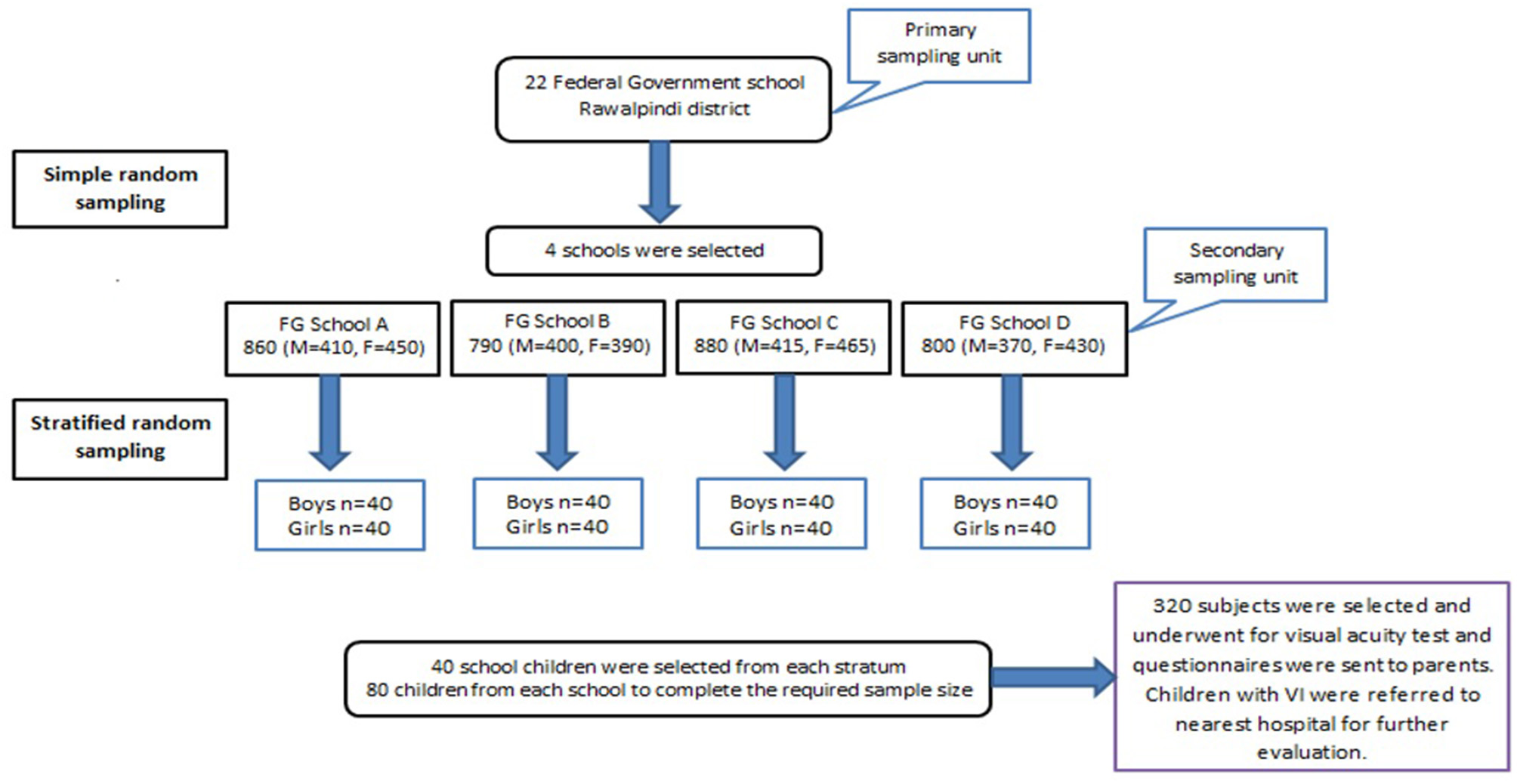
Schematic representation of sampling techniques in Federal Government Schools, Rawalpindi.
Using the Cochrane formula (https://dissertationdataanalysishelp.com/cochrans-sample-size-calculator/), a sample size of 272 was calculated with a 95% confidence interval, 5% margin of error, and 21.8% population proportion (19). After adjusting for a 20% non-response rate, the final sample size was 320. Pupils aged 5–15 years, with parents' written informed consent submitted timely to the teachers were eligible for the participation. Children with known refractive error or using spectacles or with an apparent eye disease (such as conjunctivitis, red eye, ocular trauma, trachoma, etc.) were excluded.
A meeting was held with the principal of each FG school to explain the research objectives. A brief awareness session was conducted during the school assembly to inform students and parents about the importance of vision screening, followed by an interactive Q&A session. Key study details were communicated to caregivers and participants through school staff. All data was kept confidential and private, using coding and aggregate reporting to ensure anonymity by removing identifiable information. The data was used solely for research purposes and was not shared with any third party maintaining strict confidentiality.
External eye diseases were identified by external eye examination with the help of a medical torch. Children who met the inclusion criteria underwent the visual acuity test using the validated Peek Acuity app (https://peekvision.org/solutions/peek-acuity/). This app, which includes a comprehensive software platform with data collection capabilities, was used on a smartphone. The Peek Acuity app has demonstrated a sensitivity of 84.6%, specificity of 97.7%, positive predictive value of 68.8%, and negative predictive value of 99.1% (17, 20). It employs a smartphone-based tumbling-E optotype displayed in four orientations, the participant indicates the direction, and the tester inputs the response via swipe. The test uses a single isolated optotype without crowding bars, presented one at a time in random orientations, thereby minimizing the tester bias. All testing was performed using a Samsung Galaxy (Tab A 10.1-inch) tablet, with manual calibration performed prior to testing to ensure optotypes were displayed at the correct physical size. In accordance with Peek Acuity's calibration guidance for this screen size, the test distance was fixed at 3 m under natural daylight room illumination. Results are output in both LogMAR and Snellen (metric/imperial), with a visual blur simulation to aid participant understanding.
The right eye was tested first, followed by the left eye. Visual impairment was defined as presenting visual acuity worse than 6/12 in the better eye, determined by correctly identifying four out of five optotypes at the 6/12 level, when tested at a distance of 3 m under natural daylight room illumination (Figure 2). According to International Classification of Diseases 11th revision, 2018, following cut-off values for the severity of visual impairment were used (21). Mild –presenting visual acuity worse than 6/12 but better than 6/18 in the best-corrected eye. Moderate- presenting visual acuity worse than 6/18 but better than 6/60. Severe- presenting visual acuity worse than 6/60 but better than 3/60. Blindness as VA worse than 3/60 in the better eye with the best possible correction.
Figure 2
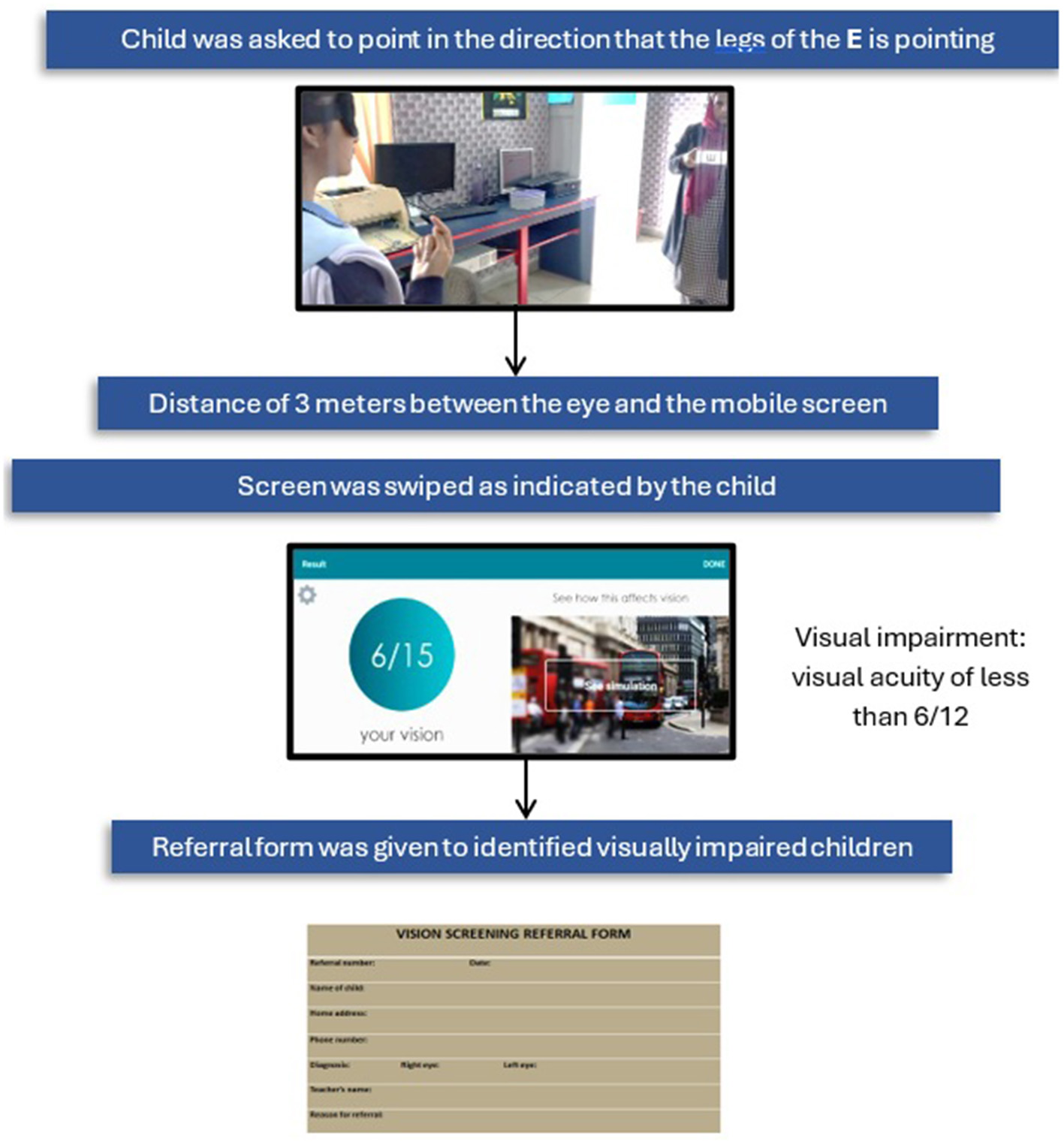
Vision screening procedure.
Participants with VA worse than 6/12 in “either eye” were re-examined and those who continued to meet the criteria for visual impairment were given a referral slip to the nearest hospital for further evaluation. An Urdu version of the validated and structured closed-ended questionnaire (22) were used to assess risk factors associated with visual impairment, which were prepared following research and consultation with experienced experts in the subject area (see Supplementary material). The questionnaire was pre-tested in pilot study before data collection.
Data were entered and analyzed using SPSS version 27 software and checked for normality by applying Kolmogorov-Smirnov (KS) test. Sociodemographic characteristics of participants were presented in tables using simple frequency distribution and percentages for categorical data.
Percentage used to present the frequency of visual impairment among study participants. Potential risk factors associated with visual impairment were first analyzed by comparing children with and without visual impairment in bivariate models. If significant differences will be shown in the univariate model, these risk factors will be included together in multiple logistic regression models with visual impairment as dependent variable. Variables with p < 0.05 and 95% confidence interval in the multivariate model were considered statistically significant. To overcome the non-response rate, adjusted sample size with 20% non-response rate used.
3 Results
A total of 320 children participated in this study, all of whom were aged between five and fifteen years and were evaluated for visual impairment. The baseline characteristics and frequency of risk factors among participants were assessed (Tables 1, 2). Visual impairment was identified in 82 children (25.6%), consisting of 35 males (42.68%) and 47 females (57.3%). Among these, 38 children (46.3%) were aged 5–10 years, while 44 children (56.7%) were aged 11–15 years (Table 3). The severity of visual impairment was categorized as mild in 30 (36.58%) children and moderate in 52 (63.41%) children (Figure 3).
Table 1
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age (years) | ||
| 5–10 | 160 | 50 |
| 11–15 | 160 | 50 |
| Gender | ||
| Male | 160 | 50 |
| Female | 160 | 50 |
| Father educational status | ||
| None | 25 | 7.8 |
| Primary | 109 | 34 |
| Secondary | 186 | 58 |
| Mother educational status | ||
| None | 33 | 10.3 |
| Primary | 116 | 36.2 |
| Secondary | 171 | 53.4 |
| Household income | ||
| Low-less than PKR 42,000 | 141 | 44 |
| Lower middle-PKR 42,000–99,999 | 150 | 46.8 |
| Middle-PKR 1,00,000–1,49,000 | 29 | 9 |
Sociodemographic characteristics of participants.
Table 2
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Maternal illness during pregnancy | ||
| Yes | 67 | 21 |
| No | 253 | 79 |
| Parent with visual impairment | ||
| Yes | 108 | 33.7 |
| No | 253 | 66.2 |
| Sibling with visual impairment | ||
| Yes | 59 | 18.4 |
| No | 261 | 81.5 |
| Birth weight (BW) (g) | ||
| Low BW < 2,500 g | 54 | 16.8 |
| BW 2,500 g or >2,500 g | 266 | 83.1 |
| Gestational period (weeks) | ||
| GA < 37weeks | 89 | 27.8 |
| GA 37 weeks or >37 weeks | 231 | 72.2 |
| Complications at birth | ||
| Yes | 30 | 9.3 |
| No | 281 | 87.8 |
| Serious infections during childhood | ||
| Yes | 53 | 16.5 |
| No | 267 | 83.4 |
| Head trauma or eye injury | ||
| Yes | 15 | 4.7 |
| No | 305 | 95.3 |
| Duration of TV exposure | ||
| < 2 h | 71 | 22.1 |
| 2–4 h | 146 | 45.6 |
| >4 h | 103 | 32.1 |
| Duration of mobile/computer exposure | ||
| < 2 h | 85 | 26.6 |
| 2–4 h | 123 | 38.4 |
| >4 h | 112 | 35 |
Frequency of risk factors among participants.
Table 3
| Age (years) | Visual impairment | Total | |||
|---|---|---|---|---|---|
| Male | Female | ||||
| Frequency | Percentage % | Frequency | Percentage % | ||
| 5–10 years | 12 | 14.63 | 26 | 31.7 | 38 (46.3%) |
| 11–15 years | 23 | 28.04 | 21 | 25.6 | 44 (56.7%) |
| Total | 35 (42.68%) | 47 (57.31%) | 82 (25.6%) | ||
Frequency of visual impairment by age and gender.
Figure 3
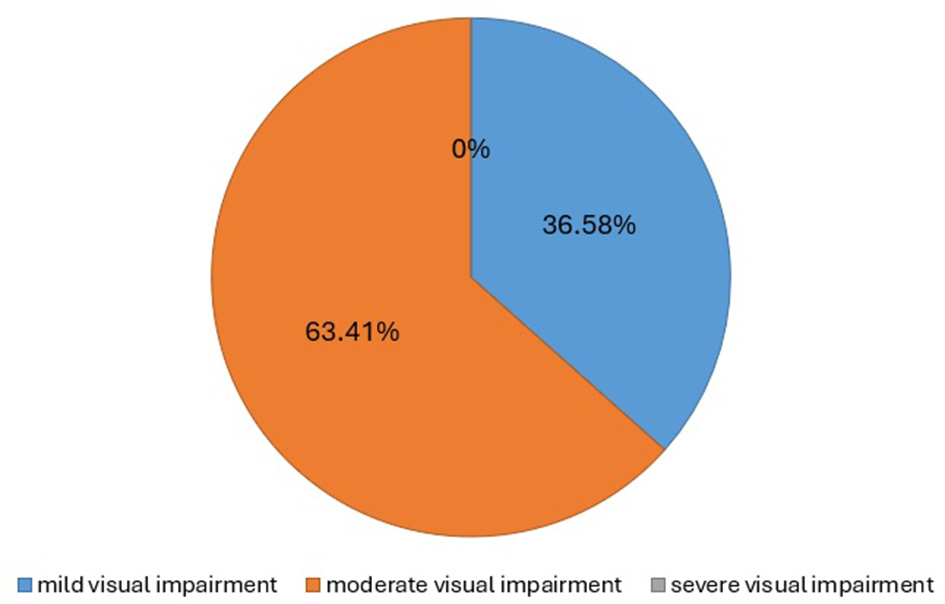
Severity of visual impairment.
A logistic regression model was employed to identify risk factors influencing visual impairment in children. The univariate analysis revealed a significant odds ratio (OR) with a 95% confidence interval (CI) and a p-value of < 0.05. The univariate (crude) logistic regression results for all independent variables are presented in Table 4. It was found that children with a positive family history of VI among parents exhibited a significantly higher prevalence of vision impairment [COR 4.849 (2.845–8.266)]. Additionally, low birth weight [COR 0.083 (0.42–0.161)], small gestational age [COR 0.147 (0.085–0.256)] and complications at birth among children [COR 2.360 (1.277–4.363)] was linked to a notably increased prevalence. Similarly, a significant association was found among those exposed to mobile devices or computers for more than 4 h [COR 2.216 (1.25–3.926)].
Table 4
| Variable | Visual impairment | Univariate analysis COR (95% CI) | Multivariate analysis AOR (95% CI) | |
|---|---|---|---|---|
| Yes ( n = 82) | No ( n = 238) | |||
| Age (years) | ||||
| 5–10 | 38 | 122 | 1.218 (0.736–2.014) | |
| 11–15 | 44 | 116 | ||
| Gender | ||||
| Male | 35 | 125 | 1.485 (0.895–2.464) | |
| Female | 47 | 113 | ||
| Father educational status | ||||
| None | 09 | 16 | 1 | |
| Primary | 34 | 75 | 0.472 (0.194–1.148) | |
| Secondary | 39 | 147 | 0.585 (0.342–1.002) | |
| Mother educational status | ||||
| None | 10 | 23 | 1 | |
| Primary | 35 | 81 | 0.635 (0.278–1.452) | |
| Secondary | 37 | 134 | 0.639 (0.373–1.095) | |
| Household income | ||||
| Low-less than PKR 42,000 | 47 | 94 | 1 | |
| Lower middle-PKR 42,000–99,999 | 30 | 120 | 0.417 (0.149–1.161) | |
| Middle-PKR100,000–149,000 | 5 | 24 | 0.833 (0.294–2.365) | |
| Maternal illness during pregnancy | ||||
| Yes | 19 | 48 | 1.194 (0.653–2.181) | |
| No | 63 | 190 | ||
| Parent with visual impairment | ||||
| Yes | 50 | 58 | 4.849 (2.845–8.266) | 4.201(2.221–7.948)*** |
| No | 32 | 180 | ||
| Sibling with visual impairment | ||||
| Yes | 19 | 40 | 1.493 (0.807–2.762) | |
| No | 63 | 198 | ||
| Birth weight (BW) (g) | ||||
| Low BW < 2,500g | 22 | 32 | 0.155 (0.089–0.268) | 0.376 (0.189–0.749)** |
| BW 2,500 g or >2,500 g | 60 | 206 | ||
| Gestational period (weeks) | ||||
| GA < 37weeks | 48 | 41 | 0.147 (0.085–0.256) | 0.231 (0.113–0.475)*** |
| GA 37 weeks or >37 weeks | 34 | 197 | ||
| Complications at birth | ||||
| Yes | 30 | 9 | 2.360 (1.277–4.363) | 1.293 (0.563–2.970) |
| No | 36 | 245 | ||
| Serious infections during childhood (trachoma, measles) | ||||
| Yes | 16 | 37 | ||
| No | 66 | 201 | 1.317 (0.688–2.520) | |
| Head trauma or eye injury | ||||
| Yes | 6 | 9 | 2.009 (0.692–5.828) | |
| No | 76 | 229 | ||
| Duration of TV exposure | ||||
| < 2 h | 10 | 61 | 1 | |
| 2–4 h | 45 | 101 | 1.402 (0.627–3.13) | |
| >4 h | 27 | 76 | 2.167 (0.974–4.823) | |
| Duration of mobile/computer exposure | ||||
| < 2 h | 12 | 73 | 1 | |
| 2–4 h | 27 | 96 | 3.791 (1.848–7.785) | 2.368 (1.040–5.393)* |
| >4 h | 43 | 69 | 2.216 (1.25–3.926) | |
Univariate (crude) and multivariate logistic regression of factors associated with visual impairment among schoolchildren.
* p < 0.05; **p ≤ 0.01; ***p ≤ 0.001.
COR, crude odds ratio; AOR, adjusted odds ratio.
(All independent variables tested in the univariate analysis are presented, regardless of statistical significance).
Variables significant at the univariate level were subsequently included in the multivariate logistic regression model. In the adjusted analysis, four variables remained independently associated with visual impairment: parental visual impairment [AOR 4.201 (2.221–7.948)], low birth weight [AOR 0.376 (0.189–0.749)], small gestational age [AOR 0.231 (0.113–0.475)] and prolong exposure to mobile and computer devices [AOR 2.368 (1.040–5.393)]. The pooled results are presented in Figure 4, which shows the forest plot summarizing the overall effect estimates.
Figure 4
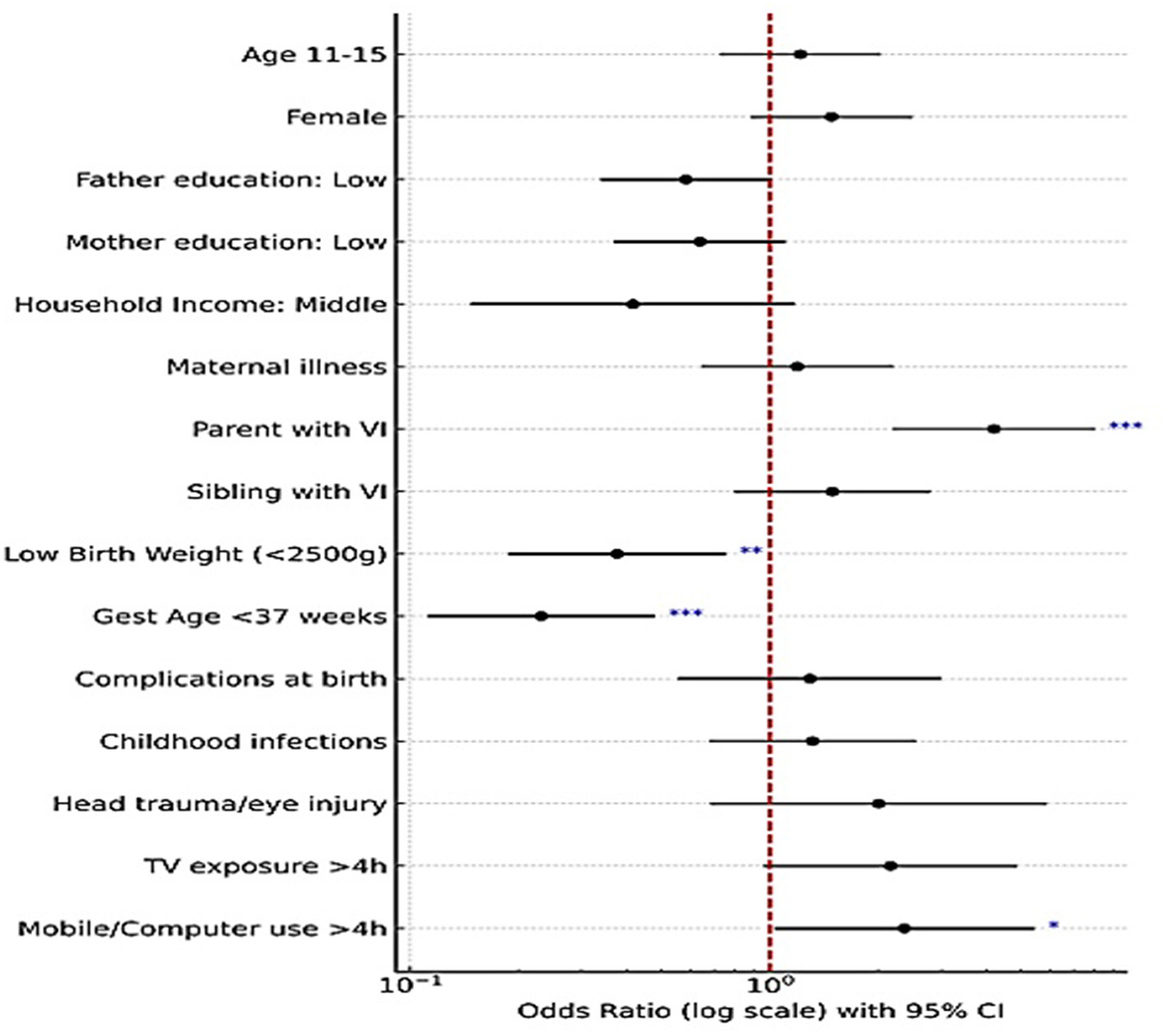
Forest plot of factors associated with visual impairment (results of bivariate and multivariate logistic regression; with 95% CI; significance indicated as *p < 0.05; **p ≤ 0.01; ***p ≤ 0.001).
Furthermore, to check for potential multicollinearity among independent variables, variance inflation factors (VIFs) and tolerance values were examined. All variables included in the final model demonstrated acceptable VIF values (< 3) and tolerance >0.3 (23), indicating no significant collinearity and ensuring the stability of the regression estimates.
4 Discussion
This study contributes important data on childhood vision health in low-to-middle-income communities (LMICs) by reporting the frequency of visual impairment among school children, in contrast to previous regional studies. mHealth-based screening tools represent an emerging innovation with substantial potential to enhance health outcomes. Our study demonstrated significant improvements in early detection, particularly in resource-limited settings, where such tools prove especially effective. The result shows a notable prevalence of visual impairment among school children compared to previous regional studies. A study conducted in 2018 reported a prevalence of 17.5% (24), while another study in 2016 found a prevalence of 12.4% (25). The 2017 national survey in Pakistan reported a prevalence of 15.38%, which projected a rise in the coming years (4). International studies, including those from South Africa (26) and Egypt (27), have reported varying prevalence rates ranging from 16% to 29.4% further highlighting the variability of VI rates across different regions and populations.
The disparity could be attributed to a variety of factors, including differences in study design, the target population, and the specific inclusion criteria used. Economic disparities, ethnic differences, and access to healthcare services likely play a significant role in influencing the prevalence of visual impairments (28). Additionally, varied operational definitions taken into consideration by investigators are the reason for variations in prevalence data from research conducted in other Pakistani cities and even in other countries (29).
Family history emerged as a strong risk factor for visual impairment in our study. This association is a common finding across multiple studies (23, 26, 30). A family history of myopia, in particular, has been linked to a higher risk of visual impairment as mentioned in a review that focused on the prevalence and etiology of VI (31). Genetic contributions to visual impairment have been demonstrated through familial and genome-wide association studies, indicating that its etiology is complex (32).
We found that among the birth-related factors, low birth weight (< 2,500 g) was a significant risk factor for visual impairment. Children with low birth weight were more likely to experience VI, with an OR of 2.45 (95% CI, 1.14–5.26) (33). Low birthweight was also identified in other comparable studies that have demonstrated the association between low birth weight and an increased risk of refractive errors and other visual disorders (34, 35). Studies have shown that low birth weight disrupts the process by which the eye becomes more focused as a child grows, leading to a higher incidence of refractive errors (36).
Another important finding in our study was the increased risk of visual impairment among preterm children, who are more likely to experience ocular disorders such as refractive errors. This finding corroborates study from Ethiopia in 2024 which reported refractive errors were the leading type of ocular morbidity seen in 115/222 (51.8%) preterm children (36). Similarly, a report from Sweden (37) and Africa (38), found that nearly half of the children who were screened for preterm had refractive error. The association between prematurity and visual impairment may be linked to the underdevelopment of the visual system, which is more vulnerable in preterm children (39).
Lastly, our study also highlights the high prevalence of visual impairment among students involved in near work activities, including screen time (video games, computers, and mobile devices). This aligns with findings from studies conducted in other regions in which the children who spent more than 4 h per day engaged in near work activities were found to have a significantly higher prevalence of visual impairment (28). Prolonged near work activities have been shown to increase the risk of developing refractive errors, particularly myopia, as the eye undergoes excessive accommodation during close-up tasks (40).
This study addresses an important area with limited reviews in the existing literature and has several strengths including use of a two-stage sampling design, use of validated tool, appropriate sample size and finally analysis through robust analytical approach to assess the prevalence and associated risk factors. However, there are several limitations. The study utilized basic screening tests for visual impairment instead of comprehensive clinical eye examinations. While these screening tests can detect obvious visual impairments, they may overlook more subtle cases of refractive errors or other ocular conditions. In addition, visual impairment classification depends on uncorrected visual acuity (UCVA) instead of best-corrected visual acuity (BCVA). The study also employed a single optotype acuity task rather than full line-based acuity testing, which may overestimate visual performance and limit comparability with studies using standard line acuity measures. As this work was limited to school-based screening, the subsequent referral process and outcomes were not captured. Consequently, information on the proportion of referred children who received further evaluation and the specific types of refractive errors identified could not be determined. Longitudinal studies would be better suited for tracking the progression of visual impairment over time and for examining the causal relationships between risk factors and visual impairment. Our research concentrated on children from low-income communities, which may restrict the generalizability of our findings to other regions or socio-economic groups. Moreover, environmental factors such as air pollution and nutritional deficiencies, which could significantly impact the development of visual impairment, were not considered in this study.
5 Conclusion
This study identified a high burden of visual impairment among schoolchildren, with a greater proportion observed in females and predominantly presenting with moderate severity. Multivariate analysis revealed that parental history of visual impairment, exposure to mobile and computer devices, low birth weight, and small gestational age were significantly associated factors. Future research should evaluate referral uptake and the spectrum of refractive errors detected to strengthen the evidence for integrated screening-to-care pathways. Additional studies in other regions of Pakistan are required to obtain a more comprehensive understanding of the national burden of visual impairment among children.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical Review Committee, Armed Forces Postgraduate Medical Institute (AFPGMI), Rawalpindi, Pakistan. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
AJ: Conceptualization, Data curation, Methodology, Writing – original draft. SM: Conceptualization, Methodology, Supervision, Writing – review & editing. RH: Data curation, analysis, Writing – review & editing. UM: Formal analysis, Methodology, Writing – review & editing. AA: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are deeply indebted to the National University of Medical Sciences, which gave ethical clearance to conduct this research. We would also like to acknowledge the FGEI and school administration for their cooperation to conduct the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1661710/full#supplementary-material
References
1.
Alrasheed S . Systematic review and meta-analysis of childhood visual impairment in the Eastern Mediterranean Region. East Mediterr Health J. (2023) 29:482–90. 10.26719/emhj.23.020
2.
Hassan B Ahmed R Li B Noor A Hassan ZU . A comprehensive study capturing vision loss burden in Pakistan (1990–2025): findings from the Global Burden of Disease (GBD) 2017 study. PLoS ONE. (2019) 14:e0216492. 10.1371/journal.pone.0216492
3.
Hoeben M Langelaan M Klevering J Keunen JE van Rens GH . Low vision rehabilitation for better quality of life in visually impaired adults. Cochrane Database Syst Rev. (2020) 1:CD006543. 10.1002/14651858.CD006543.pub2
4.
Cao H Cao X Cao Z Zhang L Han Y Guo C . The prevalence and causes of pediatric uncorrected refractive error: pooled data from population studies for global burden of disease (GBD) sub-regions. PLoS ONE. (2022) 17:e0268800. 10.1371/journal.pone.0268800
5.
Atlaw D Shiferaw Z Sahiledengele B Degno S Mamo A Zenbaba D et al . Prevalence of visual impairment due to refractive error among children and adolescents in Ethiopia: a systematic review and meta-analysis. PLoS ONE. (2022) 17:e0271313. 10.1371/journal.pone.0271313
6.
Al Ghailani NA Noushad B Khurshid F Ismail GM . Parents'awareness and perception of children's refractive error. A qualitative study. Malays J Public Health Med. (2020) 20:85–91. 10.37268/mjphm/vol.20/no.3/art.656
7.
Kulp MT Ciner E Maguire M Moore B Pentimonti J Pistilli M et al . Uncorrected hyperopia and preschool early literacy: results of the vision in preschoolers–hyperopia in preschoolers (VIP-HIP) study. Ophthalmology. (2016) 123:681–9. 10.1016/j.ophtha.2015.11.023
8.
Maduka-Okafor FC Okoye O Ezegwui I Oguego NC Okoye OI Udeh N et al . Refractive error and visual impairment among school children: result of a South-Eastern Nigerian regional survey. Clini Ophthalmol. (2021) 15:2345–53. 10.2147/OPTH.S298929
9.
Loh L Prem-Senthil M Constable PA . A systematic review of the impact of childhood vision impairment on reading and literacy in education. J Optom. (2024) 17:100495. 10.1016/j.optom.2023.100495
10.
World Health Organization . Blindness and Visual Impairment [Fact sheet] (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (Accessed April 14, 2024).
11.
Pi LH Chen L Liu Q Ke N Fang J Zhang S et al . Prevalence of eye diseases and causes of visual impairment in school aged children in Western China. J Epidemiol. (2012) 22:37–44. 10.2188/jea.JE20110063
12.
Bourne R Steinmetz JD Flaxman S Briant PS Taylor HR Resnikoff S et al . Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. (2021) 9:e130–43. 10.1016/S2214-109X(20)30425-3
13.
Suo L Ke X Zhang D Qin X Chen X Hong Y et al . Use of mobile apps for visual acuity assessment: systematic review and meta-analysis. JMIR Mhealth Uhealth. (2022) 10:e26275. 10.2196/26275
14.
O'Neill S McAndrew D . The validity of visual acuity assessment using mobile technology devices in the primary care setting. Aust Fam Physician. (2016) 45:212–5.
15.
Brady CJ Eghrari AO Labrique AB . Smartphone-based visual acuity measurement for screening and clinical assessment. JAMA. (2015) 314:2682. 10.1001/jama.2015.15855
16.
Perera C Chakrabarti R Islam FMA Crowston J . The eye phone study: reliability and accuracy of assessing Snellen visual acuity using smartphone technology. Eye. (2015) 29:888–94. 10.1038/eye.2015.60
17.
Bastawrous A Rono HK Livingstone IA Weiss HA Jordan S Kuper H et al . Development and validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol. (2015) 133:930–7. 10.1001/jamaophthalmol.2015.1468
18.
World health organization . Vision and Eye Screening Implementation Handbook. (2024). Available online at: https://www.who.int/publications/i/item/9789240082458 (Accessed November 24, 2024).
19.
Jadoon MZ Dineen B Bourne RR Shah SP Khan MA Johnson GJ et al . Prevalence of blindness and visual impairment in Pakistan: the Pakistan National Blindness and Visual Impairment Survey. Invest Ophthalmol Vis Sci. (2006) 47:4749–55. 10.1167/iovs.06-0374
20.
Han X Scheetz J Keel S Liao C Liu C Jiang Y et al . Development and validation of a smartphone-based visual acuity test (vision at home). Transl Vis Sci Technol. (2019) 8:27. 10.1167/tvst.8.4.27
21.
World health organization . ICD-11 for Mortality and Morbidity Statistics (Version: 04/2019) Vision Impairment Including Blindness. (2019). Available online at: https://icd.who.int/browse11/lm/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1103667651 (Accessed July 8, 2024).
22.
Chia A Lin X Dirani M Gazzard G Ramamurthy D Quah BL et al . Risk factors for strabismus and amblyopia in young Singapore Chinese children. Ophthalmic Epidemiol. (2013) 20:138–47. 10.3109/09286586.2013.767354
23.
Kim JH . Multicollinearity and misleading statistical results. Korean J Anesthesiol. (2019) 72:558–69. 10.4097/kja.19087
24.
Inam S Asghar F Naeem T Unum A Ahsan U Latif A . Prevalence and comparison of undetected refractive errors among children of age b/w 5–10 years in public & private sector schools. Pak J Med Health Sci. (2018) 12:157–60.
25.
Ertekin YH Tekin M Uludag A Arikan S Sahin EM . Vision screening in children: is 7–9 years of age a threshold for visual impairment?Pak J Med Sci. (2016) 32:1194–98. 10.12669/pjms.325.10367
26.
Andersen T Jeremiah M Thamane K Littman-Quinn R Dikai Z Kovarik C et al . Implementing a school vision screening program in Botswana using smartphone technology. Telemed J E-Health. (2020) 26:255–8. 10.1089/tmj.2018.0213
27.
Yamamah GA Talaat Abdel Alim AA Mostafa YS Ahmed RA Mahmoud AM . Prevalence of visual impairment and refractive errors in children of South Sinai, Egypt. Ophthalmic Epidemiol. (2015) 22:246–52. 10.3109/09286586.2015.1056811
28.
Merrie YA Tegegne MM Munaw MB Alemu HW . Prevalence and associated factors of visual impairment among school-age children in Bahir Dar City, Northwest Ethiopia. Clin Optom. (2019) 11:135–43. 10.2147/OPTO.S213047
29.
Sambuddha Ghosh SG Udayaditya Mukhopadhyay UM Dipankar Maji DM Gautam Bhaduri GB . Visual impairment in urban school children of low-income families in Kolkata, India. Indian J Public Health. (2012) 56:163–7. 10.4103/0019-557X.99919
30.
Liu D Zhang L Shou M Yu H Yang Y Cheng H . The prevalence and risk factors of abnormal vision among preschool children. Pediatric Health Med Ther. (2024) 15:339–49. 10.2147/PHMT.S487164
31.
Atowa UC Hansraj R Wajuihian SO . Visual problems: a review of prevalence studies on visual impairment in school-age children. Int J Ophthalmol. (2019) 12:1037–43. 10.18240/ijo.2019.06.25
32.
Martínez-Albert N Bueno-Gimeno I Gené-Sampedro A . Risk factors for myopia: a review. J Clin Med. (2023) 12:6062. 10.3390/jcm12186062
33.
O'Connor AR Stephenson TJ Johnson A Tobin MJ Ratib S Moseley M et al . Visual function in low birthweight children. Br J Ophthalmol. (2004) 88:1149–53. 10.1136/bjo.2003.035154
34.
Pai AS Wang JJ Samarawickrama C Burlutsky G Rose KA Varma R et al . Prevalence and risk factors for visual impairment in preschool children: the Sydney paediatric eye disease study. Ophthalmol. (2011) 118:1495–500. 10.1016/j.ophtha.2011.01.027
35.
Powls A Botting N Cooke RW Stephenson G Marlow N . Visual impairment in very low birthweight children. Arch Dis Child Fetal Neonat Ed. (1997) 76:F82–7. 10.1136/fn.76.2.F82
36.
Robitaille JM . Long-term visual outcomes in prematurely born children. J Binocul Vis Ocul Motil. (2024) 74:1–8. 10.1080/2576117X.2023.2287633
37.
Hellgren KM Tornqvist K Jakobsson PG Lundgren P Carlsson B Källén K. et al . Ophthalmologic outcome of extremely preterm infants at 6.5 years of age: extremely preterm infants in Sweden study (EXPRESS). JAMA Ophthalmol. (2016) 134:555–62. 10.1001/jamaophthalmol.2016.0391
38.
Sathar A Abbas S Nujum ZT Benson JL Sreedevi GP Saraswathyamma SK . Visual outcome of preterm infants screened in a tertiary care hospital. Middle East Afr J Ophthalmol. (2019) 26:158–62. 10.4103/meajo.MEAJO_64_17
39.
Tsumi E Hazan I Regev T Leeman S Barrett C Fried Regev N et al . The association between gestational age and risk for long term ophthalmic morbidities among offspring delivered in different preterm subgroups. J Clin Med. (2022) 11:2562. 10.3390/jcm11092562
40.
Wang J Li M Zhu D Cao Y . Smartphone overuse and visual impairment in children and young adults: systematic review and meta-analysis. J Med Int Res. (2020) 22:e.21923. 10.2196/21923
Summary
Keywords
visual impairment, preventable blindness, school age children, mHealth-based vision screening, Pakistan, risk factors
Citation
Javed A, Mohsin S, Habib R, Malik UA and Ahmad AMR (2025) Prevalence and associated risk factors of visual impairment in school children: mHealth-based vision screening in government schools of Rawalpindi, Pakistan. Front. Med. 12:1661710. doi: 10.3389/fmed.2025.1661710
Received
11 July 2025
Accepted
30 September 2025
Published
21 October 2025
Volume
12 - 2025
Edited by
José Aparecido Da Silva, University of Brasilia, Brazil
Reviewed by
Nicole Ross, New England College of Optometry, United States
Rania Zaki, Ain Shams University, Egypt
Updates
Copyright
© 2025 Javed, Mohsin, Habib, Malik and Ahmad.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ayesha Javed drayeshajaved3@gmail.comShamaila Mohsin sm104177@hotmail.comAbdul Momin Rizwan Ahmad abdul.momin@york.ac.uk
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.