- 1Department of Anesthesiology and Perioperative Medicine, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Asthma Center, Children's Hospital Affiliated to Shandong University, Jinan, China
- 3Department of Anesthesia and Surgery, Zibo Central Hospital, Zibo, China
The landscape of surgical care is undergoing a profound transformation, driven by rapid advancements in technology and a persistent focus on enhancing patient outcomes. At the forefront of this evolution are innovative nursing practices within the intraoperative setting, which are proving instrumental in elevating patient safety, optimizing operational efficiency, and significantly reducing complications across a spectrum of surgical specialties. This report provides a comprehensive analysis of these cutting-edge nursing interventions from the foundational principles of perioperative care to the integration of advanced technologies such as Artificial Intelligence (AI), robotics, virtual reality, and personalized medicine. Perioperative nurses, traditionally recognized for their critical roles in maintaining sterile environments and advocating for patient wellbeing, are now embracing expanded responsibilities as technological integrators, data interpreters, and champions of evidence-based protocols such as Enhanced Recovery After Surgery (ERAS). The adoption of these innovative practices has led to demonstrable improvements, including shorter hospital stays, reduced opioid consumption, and decreased complication rates. However, the path to widespread adoption is not without its challenges, encompassing human factors such as resistance to change, organizational barriers such as insufficient resources, and technical complexities related to data accuracy and regulation. To fully harness the potential of innovative intraoperative nursing, healthcare organizations must strategically invest in continuous, accessible training programs that balance technological proficiency with core nursing judgment. Cultivating a culture that empowers nurse-led innovation, prioritizes human-centered technology design, and strengthens multidisciplinary collaboration is paramount. Furthermore, a commitment to evidence-based implementation and addressing health equity in technology access will ensure that advancements benefit all patients and that the nursing profession continues to thrive as a vital force in shaping the future of surgical care.
1 Introduction
Surgical care, a cornerstone of modern medicine, relies fundamentally on the meticulous and dynamic contributions of the intraoperative nursing team. As medical science and technology advance at an unprecedented pace, the role of these highly skilled professionals is continuously evolving, moving beyond traditional responsibilities to embrace innovative practices that directly influence patient outcomes (1, 2). This report delves into the transformative impact of these innovations, highlighting how perioperative nurses are not merely adapting to change but are actively driving improvements in patient safety, operational efficiency, and complication reduction across a diverse array of surgical specialties. Innovative nursing practices in intraoperative care are characterized by the proactive pursuit and development of novel methods, technologies, and tools aimed at promoting health, preventing diseases, and enhancing the overall quality of patient care (3). This extends beyond mere adoption of new tools; it involves critical thinking by nurses on the front lines, who are uniquely positioned to identify more efficient processes or repurpose existing items for alternate uses, thereby improving clinical practice (4). To ground this analysis, we acknowledge the foundational definition of the intraoperative nurse provided by organizations such as the Association of periOperative Registered Nurses (AORN) (5, 6). However, the role has expanded far beyond traditional duties. It is now defined by an internationally recognized competency profile that demands adept teamwork, sophisticated technology integration, and advanced critical decision-making to manage the complex, high-stakes surgical environment (7–10). These evolving competencies, which will be detailed further in this report, establish the intraoperative nurse not just as a caregiver but as a clinical leader and safety integrator. This perspective suggests that innovation is not a sporadic event or an optional add-on but rather a fundamental, ongoing requirement for contemporary nursing practice. For perioperative nursing to remain at the cutting edge and continuously improve patient care, fostering an environment where nurses are encouraged to actively seek and implement novel solutions is essential. This requires a shift in mindset, moving away from viewing innovation as an isolated project and toward embedding it as a core competency within nursing education and professional development programs from the outset. The observation that there is a lagging innovation ability among clinical nurses' points to a systemic gap that necessitates addressing through structured education and dedicated time for collaborative problem-solving and brainstorming (4, 11).
Perioperative nurses function as integral members of the surgical team, engaging in close collaboration with surgeons, anesthesiologists, and surgical technologists to deliver seamless and coordinated care (8, 9). During the intraoperative phase, their expertise is crucial in ensuring that all safety protocols are rigorously followed, that communication among team members is fluid and effective, and that patient rights and preferences are respected, particularly when the patient is under anesthesia and unable to self-advocate (3, 12). In this high-stakes environment, even with advanced technology, the unique human roles of vigilance, advocacy, and ethical oversight performed by nurses become even more critical. Nurses serve as a vital “human firewall” against potential errors, ensuring that technological advancements enhance care quality without diminishing the essential human element of patient safety and individualized attention. This highlights a crucial need for training programs that not only impart technological proficiency but also reinforce core nursing principles, ensuring a balanced approach to advanced surgical care.
This manuscript is a comprehensive narrative review designed to synthesize and analyze the existing literature on innovative nursing practices in intraoperative care. A structured literature search was conducted to identify relevant articles, guidelines, and reports.
2 Methodology
2.1 Search strategy and data sources
We searched several major electronic databases, including PubMed/MEDLINE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Scopus, and Google Scholar. The search was conducted to identify literature published between January 2010 and July 2025 to ensure a focus on contemporary and innovative practices. The search strategy employed a combination of keywords and Medical Subject Headings (MeSH) terms using Boolean operators (AND, OR). Key search terms included (“intraoperative nursing” OR “perioperative nursing” OR “theater nurse”) AND (“innovation” OR “technology” OR “advanced practice” OR “evidence-based practice”) AND (“surgical outcomes” OR “patient safety” OR “surgical efficiency”). Additional targeted searches were performed for specific topics, such as “Artificial Intelligence in surgery,” “robotics in nursing,” “Enhanced Recovery After Surgery (ERAS),” and “virtual reality in nursing education.”
2.2 Inclusion and exclusion criteria
Articles were selected for inclusion based on the following criteria:
• Inclusion criteria: the inclusion criteria were as follows: (1) peer-reviewed original research, systematic reviews, narrative reviews, and professional guidelines; (2) direct relevance to nursing roles and practices within the intraoperative phase of surgical care; (3) focus on the implementation or impact of new technologies, protocols (e.g., ERAS), or innovative nursing roles; and (4) published in the English language.
• Exclusion criteria: the exclusion criteria were as follows: (1) articles published before 2010; (2) studies focusing exclusively on preoperative or postoperative care without a clear link to intraoperative practices; (3) non-peer-reviewed content, dissertations, or conference abstracts without a subsequent full publication; and (4) articles not available in English.
2.3 Data synthesis
The selected literature was analyzed using a narrative synthesis approach. The information extracted from the articles was organized thematically according to the core topics of this review: foundational nursing principles, technological innovations [AI, robotics, virtual reality (VR)/augmented reality (AR), etc.], ERAS protocols, specialty-specific practices, and challenges to implementation. The findings were critically evaluated and integrated to construct a cohesive narrative that identifies key trends, quantifies impacts where data were available, and outlines future directions for intraoperative nursing. This approach allowed for a broad and comprehensive exploration of the topic from multiple perspectives.
3 The core competency profile of the contemporary intraoperative nurse
Contemporary intraoperative nursing is defined by a multifaceted competency profile that moves beyond foundational safety duties to integrate advanced clinical and systemic responsibilities. This profile, which serves as the standard for practice in today's technologically driven surgical environments, is understood through key domains encompassing complex teamwork, systems coordination, and technology management. The competencies detailed below demonstrate the evolution of the nurse's role from a task-oriented focus to that of a clinical leader and safety integrator (3, 6, 13, 14).
3.1 Foundational safety competencies
The bedrock of safe surgical practice is formed by several non-negotiable responsibilities: the meticulous setup and maintenance of the sterile field to prevent surgical site infections; the precise positioning of the client to prevent injury; and serving as the unwavering patient advocate to ensure safety and consent are verified when the patient is most vulnerable (15–18).
3.2 Teamwork and systems coordination
Intraoperative nursing excellence requires seamless integration within the multidisciplinary team. Nurses are central to facilitating clear and structured communication, a competency exemplified by the nurse-led implementation of standardized handoff protocols such as SHRIMPS to ensure continuity of care during personnel changes (1, 19). This extends to system-level coordination, where nurses play a pivotal role in implementing complex, evidence-based pathways such as ERAS. In this capacity, they coordinate actions across the entire surgical team to ensure adherence to protocols that accelerate recovery and reduce complications (20, 21).
3.3 Critical decision-making and evidence-based practice
The dynamic operating room environment demands constant critical thinking, which is structured through a clear and synergistic relationship between the nursing process, evidence-based practice (EBP), and documentation. The nursing process (assessment, diagnosis, planning, implementation, and evaluation) serves as the foundational framework for critical thinking, providing a systematic method for delivering individualized care (22, 23). This framework is then elevated by EBP, which informs every step of the process with the best available research, clinical expertise, and patient values (24). For example, when positioning a patient, the nurse uses the nursing process to assess risk, but it is EBP that guides them to select a specific, research-backed technique to prevent nerve damage (25, 26). Finally, meticulous intraoperative documentation serves as the indispensable record that captures the EBP-driven decisions made within the nursing process. This documentation provides legal proof of care, ensures continuity during handoffs, and supplies crucial data for quality improvement, making the entire cycle of thinking and action visible and verifiable (27, 28) (Figure 1).
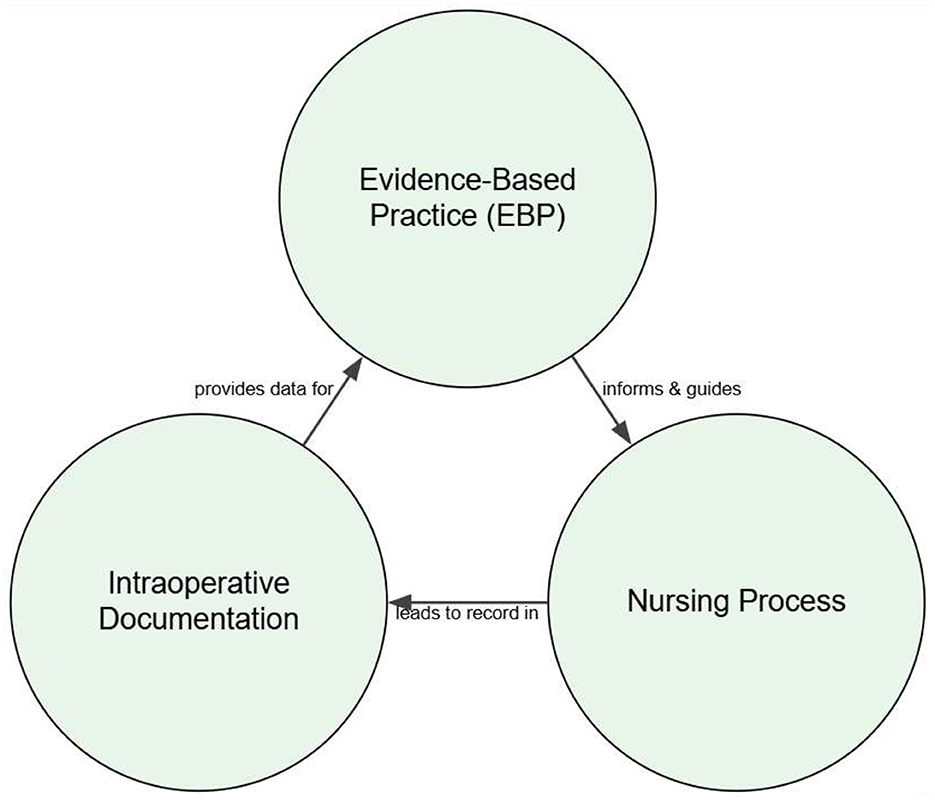
Figure 1. Dynamic framework for evidence-based intraoperative nursing. This model illustrates the cyclical and interdependent relationship between core nursing functions aimed at achieving optimal patient outcomes. The nursing process provides the structured methodology for patient care. This process is continuously informed by EBP, which integrates the best research to guide clinical decisions. All actions and observations are captured through intraoperative documentation, which not only ensures legal and safety standards but also provides critical data for quality improvement, feeding back into and refining future EBP. This cyclical flow highlights that intraoperative nursing is a continuous process of action, validation, and improvement.
3.4 Technology integration
A defining competency of the contemporary intraoperative nurse is the ability to manage and integrate advanced technologies. This role has shifted from manual assistance to that of a technology manager, responsible for preparing robotic systems, handling patient-specific 3D-printed guides, and interpreting data from an array of digital sources (29–31). As the subsequent sections will detail, this technological proficiency is not a separate skill but is woven into all other competencies to enhance surgical precision, improve efficiency, and elevate patient safety.
4 Technological innovations driving intraoperative care transformation
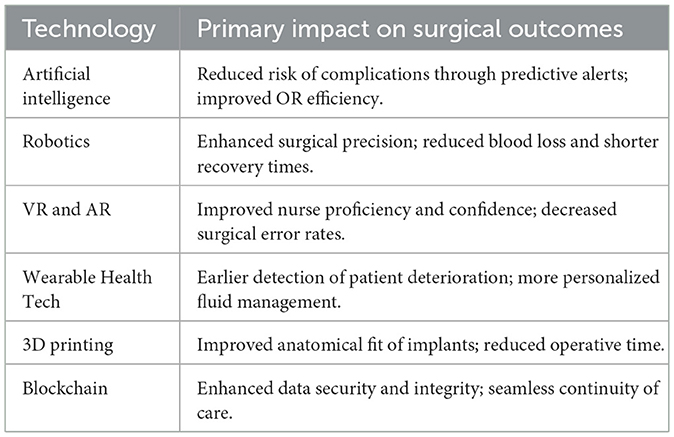
The integration of advanced technologies is fundamentally reshaping intraoperative nursing, moving beyond traditional methods to create more precise, efficient, and safer surgical environments. These innovations are not merely tools but are becoming integral partners in the delivery of patient care, demanding new skillsets and a collaborative approach from perioperative nurses (32) (Table 1).
4.1 AI and robotics
AI and robotics are revolutionizing perioperative nursing by enhancing efficiency and clinical decision-making (33, 34). A key application of AI is predictive analytics, which uses machine learning algorithms to analyze vast datasets and forecast potential adverse events. This empowers nurses to move from a reactive to a proactive model of care by identifying high-risk patients before complications arise (35). In practice, AI offers real-time decision support during surgery and helps optimize OR logistics such as scheduling and staff assignments, freeing nurses to focus on direct patient care (36–38).
Robotic systems, often guided by AI, enhance surgical precision, minimize invasiveness, and reduce the administrative burden on nursing staff (39). For nurses, the integration of these technologies marks a shift from manual assistance to the role of a technology manager. Key responsibilities now include preparing robotic equipment, interpreting data from predictive models, and applying critical thinking to ensure that all technological recommendations align with the patient's holistic needs (36, 39).
4.2 Virtual reality (VR) and augmented reality (AR)
VR and AR are transforming nursing education and patient experience. These immersive technologies provide realistic, risk-free training simulations, allowing nurses to practice complex procedures and enhance their clinical reasoning (40, 41). For patients, VR can be used to reduce preoperative anxiety and manage postoperative pain (42, 43). AR provides real-time information overlays during procedures, aiding in anatomical visualization and procedural guidance (44). The primary impact is improved nursing proficiency and enhanced patient safety through better training and a reduction in surgical errors (45).
4.3 Wearable health technologies
Wearable health technologies are creating a new continuum of patient data that directly impacts intraoperative nursing practice. While traditionally used for pre- and postoperative monitoring, these data provide a crucial baseline for the intraoperative period. The nurse can access a patient's pre-operative data from their personal wearable devices—such as activity levels, sleep patterns, or baseline heart rate variability—to create a more holistic and personalized intraoperative care plan (46). Furthermore, the emergence of intraoperative wearable sensors is creating a new stream of real-time data for which the nurse is responsible. These sensors can offer continuous monitoring of core body temperature, muscle oxygenation, or subtle hemodynamic shifts that may not be captured by standard monitors. The intraoperative nurse's role is to integrate this new data with traditional monitoring, interpret its clinical significance, and use it to anticipate needs and facilitate timely interventions (47–49). This transforms the nurse's function from periodic data collection to the continuous, proactive surveillance of a data-rich patient, directly connecting wearable technology to intraoperative safety and outcomes (31, 50–52).
4.4 3D printing
3D printing enables the creation of patient-specific surgical guides and implants, shifting a portion of the surgical planning to the pre-operative phase (53–55). However, this innovation places a critical and high-stakes responsibility on the intraoperative nurse, who functions as the final point of safety verification within the sterile field. The nurse's specific contribution involves more than just instrument management; it is a crucial safety intervention. They are responsible for meticulously cross-referencing the unique identifiers on the sterile 3D-printed device against the patient's records and the surgical plan immediately before use. By confirming this match and communicating it to the team, the nurse provides a definitive safeguard against a potential wrong-site, wrong-procedure, or wrong-implant error. This direct nursing action is indispensable for the safe and effective application of personalized surgical technology, directly linking their vigilance to improved surgical precision and patient outcomes (56–58).
4.5 Blockchain technology
Blockchain technology enhances the security, integrity, and privacy of patient data by providing a decentralized and immutable ledger for health information (59, 60). For perioperative nurses, this means becoming familiar with advanced charting and documentation systems that leverage blockchain principles, ensuring that data are accurately recorded and securely accessible for continuity of care (61) (Table 1).
5 Enhanced recovery after surgery (ERAS) protocols: a nursing imperative
ERAS protocols represent a paradigm shift in perioperative management, moving from traditional, fragmented care to a holistic, evidence-based, and patient-centered approach. These multimodal pathways are designed to reduce the physiological and psychological stress of surgery, thereby accelerating recovery and improving outcomes (62). Far from being a simple checklist, ERAS is a dynamic process where nurses play a central, coordinating role across the entire surgical journey (20).
5.1 The nurse's role across the ERAS continuum
The success of ERAS is critically dependent on nursing leadership and meticulous execution of specific interventions at each phase (20, 21, 63):
1. Preoperative phase: the nurse's role begins well before surgery with crucial interventions such as patient education and counseling, nutritional optimization through protocols like carbohydrate loading, and promoting pre-habilitation (64, 65).
2. Intraoperative phase: inside the operating room, the intraoperative nurse is key to maintaining the physiological balance that is central to ERAS. Their specific contributions include the following (66–68):
○ Goal-directed fluid therapy: collaborating closely with the anesthesia team to maintain euvolemia (optimal fluid balance), preventing both dehydration and fluid overload, which are known to cause complications.
○ Normothermia maintenance: actively managing patient temperature using warming blankets and other technologies to prevent inadvertent hypothermia, which can impair wound healing and increase infection risk.
○ Opioid-sparing multimodal analgesia: working with the team to utilize a combination of non-opioid analgesics and regional anesthesia techniques, a cornerstone of ERAS is designed to reduce opioid-related side effects such as nausea and ileus.
3. Postoperative phase: the nurse's role is perhaps most visible in the postoperative phase, where they drive the recovery process through (63, 69):
○ Early mobilization: actively encouraging and assisting patients to get out of bed and walk within hours of their surgery to prevent blood clots, improve lung function, and hasten the return of bowel function.
○ Early oral nutrition: promptly discontinuing IV fluids and reintroducing the oral diet to stimulate gut function and provide necessary nutrients for healing.
○ Proactive nausea and vomiting management: administering antiemetics prophylactically to prevent these common side effects, which are major barriers to early feeding and mobilization.
5.2 Impact and nursing leadership
The implementation of these nurse-driven ERAS interventions has yielded significant, quantifiable improvements in patient outcomes. Studies consistently show reduced length of hospital stay (LOS), decreased complication rates, and a dramatic reduction in opioid consumption (70, 71).
ERAS empowers nurses by positioning them as leaders and coordinators of the multidisciplinary team. It demands a high degree of autonomous clinical judgment and challenges traditional hierarchies, requiring strong institutional support to overcome resistance to changes such as early feeding or catheter removal (72). Ultimately, ERAS is a powerful example of how structured, evidence-based nursing practice can fundamentally elevate the standard of surgical care.
6 Innovative organizational models: staffing based on nursing care complexity
Beyond individual practices, significant innovation occurs at the organizational level through new models of perioperative nursing care. Traditional staffing approaches, often based on rigid, one-size-fits-all ratios, are being replaced by more dynamic, evidence-based frameworks (73, 74). Driven by pressures such as staff shortages and the need for greater efficiency, these models prioritize flexibility and the strategic alignment of nursing competencies with specific patient and procedural demands (75).
The central principle of these innovative models is the shift from staffing based on surgical procedure type to a more nuanced allocation based on nursing care complexity. This involves a data-driven assessment of the anticipated nursing workload, recognizing that a technically simple surgery may still require intensive nursing care and vice versa (76). Key features of these models often include the strategic use of flexible roles, such as a circulating nurse who can support multiple operating rooms, and the empowerment of nurses through their involvement in workload assessment and scheduling decisions (76, 77). This aligns with frameworks such as the WHO's Workload Indicators of Staffing Need (WISN), which advocate for staffing based on empirical data rather than tradition (78).
A practical application of these principles is demonstrated by Cenacchi et al. (77), who implemented a tiered staffing model at a major university hospital. By differentiating between surgical and nursing complexity, they were able to create a flexible system: high-intensity nursing procedures were assigned three dedicated nurses, while medium-intensity cases were managed effectively with fewer staff by incorporating a shared circulating nurse. This data-driven approach allowed the organization to optimize resource allocation, ensuring that expertise was concentrated where it was most needed (77).
Ultimately, these innovative organizational models enhance operational efficiency and patient safety while fostering greater professional autonomy and leadership within the intraoperative nursing team.
7 Innovative nursing practices across diverse surgical specialties
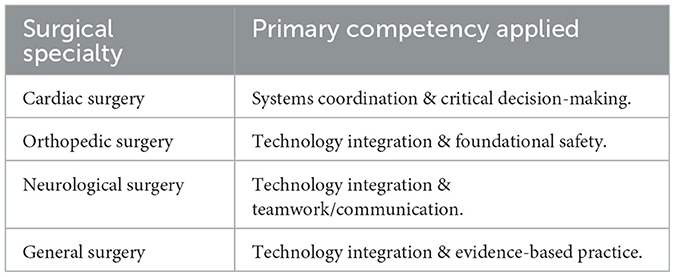
Innovations in intraoperative nursing are manifesting at both the broad organizational level and in the specialized, hands-on practices within different surgical domains. A holistic view reveals a shift toward more dynamic, evidence-based systems that empower nurses to enhance patient safety and efficiency.
7.1 Specialty-specific adaptations of intraoperative nursing practice
Within these innovative organizational structures, the core competencies of intraoperative nursing are adapted with specialized clinical reasoning to meet the unique demands of each surgical field. The nurse's role is not static; it requires dynamic application of skills and knowledge tailored to the specific technologies, procedures, and patient risks of the specialty.
7.1.1 Cardiac surgery
The nurse's role in this high-acuity environment centers on the precise management of sterile components for life support. A primary responsibility is handling the aortic and venous cannulas for cardiopulmonary bypass (CPB), ensuring correct sutures are available for securing them, and managing the cardioplegia delivery system used to arrest the heart. The nurse collaborates directly with the perfusionist by handling the sterile tubing and probes passed to and from the CPB machine. They must also manage multiple chest tubes and epicardial pacing wires, anticipating the surgeon's needs with specialized long instrumentation for deep thoracic work, all while contributing to the meticulous management of the patient's coagulopathy and hemodynamic stability (79–85).
7.1.2 Orthopedic surgery
Nursing practice here is defined by the management of high-torque equipment and complex implant sequences. In joint arthroplasty, the nurse's role involves the sequential organization of numerous reamers, broaches, and trials, ensuring the correct size is available at each step. For robotic-assisted procedures, specific nursing tasks include sterile draping of the robotic arm, assisting with the anatomical registration process, and managing the robotic end effectors. Furthermore, the nurse is responsible for the precise mixing and handling of polymethylmethacrylate (PMMA) bone cement, a critical step that involves being vigilant for the signs of Bone Cement Implantation Syndrome (BCIS) and managing the cement's exothermic reaction (86–91).
7.1.3 Neurological surgery
The nurse in neurosurgery acts as a direct guardian of neurological tissue through meticulous technique. Key responsibilities include sterile draping and intraoperative manipulation of the surgical microscope, which requires delicate coordination with the surgeon. In procedures utilizing Intraoperative Neuromonitoring (IONM), the nurse's specific contribution involves managing the sterile field to prevent interference with monitoring signals; this includes carefully placing subdermal needle electrodes as directed and controlling saline irrigation to avoid creating electrical bridges that could corrupt the data. Constant management of irrigation fluids is also critical for maintaining the temperature and moisture of delicate neural structures, directly helping to prevent iatrogenic injury (22, 23, 92–94).
7.1.4 General surgery (laparoscopic)
In minimally invasive surgery, the nurse functions as a technology and system specialist. Their role extends beyond handling instruments to managing the entire laparoscopic setup from the sterile field. This includes troubleshooting the camera (e.g., cleaning, white-balancing, and defogging the lens) and managing the pneumoperitoneum by communicating with the anesthesia provider about insufflation pressures. A critical safety function is managing multiple advanced energy devices (e.g., ultrasonic scalpels and vessel sealers). The nurse must ensure each device is connected to the generator with the correct power settings requested by the surgeon, a crucial step in preventing unintended thermal injury to the patient (1, 19, 95, 96) (Table 2).
7.2 Synthesis: key themes in nursing innovation
While the literature extensively details technological innovations within various surgical specialties, there is a noticeable gap in explicitly detailing the nuanced nursing roles developed specifically for the intraoperative phase (93). The precise contributions of nurses in integrating technologies such as robotics and 3D printing often remain implicit rather than explicitly documented (1, 97). This underscores the critical importance of dedicated nursing research to articulate and validate these unique and often “unsung” contributions, ensuring that the full scope of nursing innovation is recognized.
Despite the increasing technological sophistication across different surgical fields, a consistent and profound theme remains: the unwavering commitment to holistic patient care, encompassing both physical and psychological wellbeing (98, 99). The humanistic aspects of nursing—providing comfort, managing anxiety, and addressing patient fears—remain a constant and innovative imperative. This highlights that technological progress must always be balanced with compassionate, comprehensive care to achieve the best possible patient outcomes (97, 100–102).
8 Challenges and strategies for innovation adoption in perioperative nursing
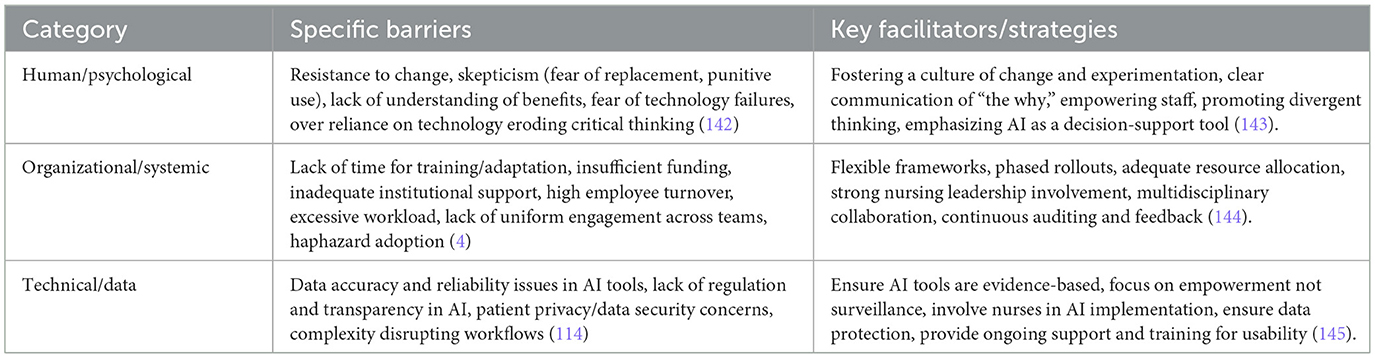
The integration of innovative practices and advanced technologies into perioperative nursing, while promising, is often met with a complex array of challenges. These obstacles span human, organizational, and technical domains, necessitating comprehensive and strategic approaches for successful and sustainable adoption (1, 103).
8.1 Barriers
• Human factors: resistance to change is a significant barrier, often stemming from skepticism among nurses who fear job displacement or punitive use of data generated by new technologies (104, 105). Nurses, who rely heavily on intuition and clinical judgment, may be concerned that AI or other automated systems could diminish their professional autonomy and expertise (106). A lack of understanding of the benefits of new innovations and a fear of technology failures further contribute to this resistance (100, 107).
• Organizational/systemic factors: healthcare organizations frequently face systemic barriers to innovation. These include a lack of sufficient time for training and adaptation to new systems, inadequate funding for technology acquisition and implementation, and insufficient institutional support for innovative initiatives (4). High employee turnover and excessive workload also hinder the capacity for nurses to engage with and adopt new practices (108). A notable challenge is the lack of uniform engagement with new protocols, such as ERAS, across multidisciplinary teams, leading to inconsistencies in care (72). Furthermore, the haphazard adoption of new surgical technologies without proper evaluation carries the potential for significant patient harm, as evidenced by past experiences (109).
• Technical/data factors: technologies themselves can present barriers. Concerns about the accuracy and reliability of data used to train AI tools, a lack of clear regulation and transparency in AI algorithms, and critical issues related to patient privacy and data security are prevalent (101, 110). The inherent complexity of integrating new technologies can also disrupt existing workflows, causing delays and resistance (107, 111).
The implementation of innovative nursing practices and technologies in the operating room is fundamentally a change management challenge. Technical solutions alone are insufficient; success hinges on addressing the psychological, cultural, and systemic factors that influence human behavior and organizational readiness. This means that strategic planning for innovation must prioritize human-centered design, robust training, and empowering frontline nurses as co-creators and champions of change (Table 3).
8.2 Critical appraisal of ethical dilemmas in technology integration
The integration of advanced technologies into intraoperative care presents profound ethical challenges that extend beyond technical implementation to the core of nursing practice. While frameworks such as the ANA's “5 Rights of AI” offer guidance (112), a deeper critical appraisal is necessary to navigate the complex dilemmas nurses face. This requires operationalizing core bioethical principles—beneficence (acting for the patient's good), non-maleficence (do no harm), and justice (ensuring equitable care)—within the high-stakes surgical environment.
Concrete ethical dilemmas frequently emerge in practice. For example:
• Algorithmic bias and justice: consider an AI-driven decision support tool that uses historical data to predict a patient's risk of surgical site infection. If the algorithm was trained on data that underrepresents certain demographic groups, it may inaccurately assign a lower risk score to a patient from that group, leading to less stringent intraoperative precautions. This creates a direct conflict with the principle of justice. The nurse is faced with the dilemma of either following the flawed data-driven recommendation or advocating for a higher level of care based on their own assessment, potentially challenging the protocol (113).
• Accountability and clinical judgment: a critical conflict arises when an AI-generated alert or recommendation contradicts an experienced nurse's clinical judgment (106). If a wearable device shows stable vitals but the nurse observes subtle, unquantifiable signs of patient deterioration, a decision must be made. If the nurse trusts their intuition and initiates a rapid response, they may be questioned for acting against the data. If they trust the technology and a negative outcome occurs, who bears the responsibility? This ambiguity in accountability—whether it lies with the nurse, the institution, or the technology developer—is a significant unresolved challenge.
• Data privacy and autonomy: the continuous stream of data from integrated technologies creates vulnerabilities. A data privacy breach could expose highly sensitive patient information, violating the principle of non-maleficence by causing potential harm (114). Furthermore, ensuring true informed consent (patient autonomy) becomes more complex when patients may not fully understand how their data are being used, stored, or potentially commercialized.
Operationalizing an ethical response requires nurses to act as vigilant patient advocates. This involves treating AI tools as adjuncts, not arbiters, of care; questioning and reporting potential biases in technology; and championing robust data security measures. The nurse's role is to serve as the essential “human firewall,” ensuring that technological advancements are always applied through a lens of ethical reasoning, clinical expertise, and unwavering commitment to patient safety and equity (115, 116).
8.3 Strategies for successful implementation
Overcoming these barriers requires a multi-faceted and integrated approach:
• Fostering a culture of change and innovation: healthcare organizations must actively cultivate an environment that embraces change and innovation. This involves encouraging experimentation, reframing failures as valuable learning opportunities, and empowering staff to actively contribute to continuous improvement initiatives (117, 118). Promoting divergent thinking, encouraging calculated risk-taking, fostering tolerance for failure, and building agility and autonomy within nursing teams are crucial steps in this cultural transformation (119, 120).
• Flexible frameworks and phased rollouts: a “one-size-fits-all” approach to innovation is often ineffective. Instead, strategies should be customized based on the unique needs of each unit, patient population, and acuity level (119). Implementing a test-and-launch model, starting with small-scale pilots and gradually expanding, can effectively reduce risk and increase proper usage and acceptance (121).
• Targeted education and simulation-based training: comprehensive education is essential for successful innovation adoption, and simulation-based training stands out as a key strategic facilitator. This approach allows nurses to develop and refine skills in a safe, controlled environment without any risk to patients. These programs should focus not only on the technical operation of new technologies such as robotics or VR but also on critical thinking, teamwork, and crisis management skills required to use them effectively (122, 123). High-fidelity simulations, whether using advanced mannequins or immersive Virtual Reality (VR) environments, bridge the gap between theory and practice (102, 124). They enable nurses to build muscle memory for complex procedures, practice communication and decision-making during rare or high-stakes events, and gain confidence with new technologies, which helps overcome resistance to change and fear of failure (40, 41). By integrating robust simulation into training, healthcare organizations can ensure that intraoperative nurses achieve both technical proficiency and the situational awareness needed to translate innovation into safer patient care (125).
• Strong nursing leadership and multidisciplinary collaboration: early involvement of nursing leaders in the decision-making process for technology selection and implementation is paramount (126). Nurse leaders are uniquely positioned to encourage, motivate, and empower their colleagues and other healthcare professionals to embrace new practices (72, 127). Building cohesive multidisciplinary teams that are aligned and “pushing in the same direction” is critical for a successful implementation of complex protocols such as ERAS (128, 129). Adherence to professional guidelines from organizations such as AORN, ANA, and WHO provides a foundational framework for safe and effective innovation (7, 112, 130, 131).
• Communicate “the why”: clearly articulating the purpose and tangible benefits of new tools to clinicians is crucial for gaining acceptance and buy-in. Utilizing multiple communication channels to reinforce these messages ensures broader understanding and engagement (132, 133).
8.4 The imperative of evidence-based implementation for sustainable innovation
While innovation is crucial for advancing healthcare, its adoption must be rigorously guided by evidence and an unwavering commitment to patient safety. The literature highlights that “haphazard adoption of new surgical technologies without proper evaluation has the potential to cause significant harm” (109). Therefore, nurses are advised to consider innovation “in the context of evidence-based practice” (134, 135). A significant challenge lies not only in developing innovations but also in systematically evaluating their efficacy and integrating them into practice through robust evidence-based implementation strategies. This is particularly relevant for protocols such as ERAS, where, despite an “extensive evidence-base,” nurses may still hesitate to fully implement elements without explicit clinician “permission” due to ingrained traditional mindsets (72, 136). This situation underscores the need for strong leadership to champion evidence-based approaches, overcome resistance to change based solely on tradition, and ensure that new practices are not just adopted but are sustained through continuous auditing and feedback loops. This ensures that innovation truly translates into improved patient outcomes and becomes a permanent feature of perioperative care.
9 Conclusion, future directions, and recommendations
The comprehensive analysis presented in this report unequivocally demonstrates that innovative nursing practices are profoundly elevating surgical outcomes across diverse specialties. The integration of advanced technologies, coupled with a steadfast adherence to evidence-based protocols like ERAS, has consistently led to enhanced patient safety, improved operational efficiency, and significant reductions in complications. Perioperative nurses, once primarily focused on technical assistance, have evolved into indispensable leaders within the surgical team. Their roles now encompass sophisticated technological integration, astute data interpretation, and the championing of holistic, patient-centered care. This evolution underscores the critical importance of the perioperative nurse as a technologically adept, critically thinking, and ethically grounded advocate, whose contributions are essential for optimizing patient experiences and achieving superior surgical results.
9.1 Strategic imperatives for the future operating room
The integration of AI and advanced technologies is redefining the perioperative nurse's role from a technical assistant to a clinical data curator and technology manager (137, 138). This shift requires a proactive response from healthcare organizations. To ensure nurses can meet these future demands, institutions must invest in comprehensive, continuous training programs. These programs must extend beyond technical operation to include data literacy, critical evaluation of AI outputs, and the ethical implications of new technologies (139). Simultaneously, organizations must foster a culture of nurse-led innovation by providing the time, resources, and institutional support for nurses to lead the change (117, 118). True integration also demands strengthening multidisciplinary collaboration through standardized communication protocols and shared technological platforms that ensure seamless teamwork across the entire surgical journey.
9.2 The ethical mandate for equitable and human-centered care
As surgical care becomes highly personalized through genomics and data-intensive technologies, profound ethical challenges emerge regarding equitable access, data privacy, and the potential for algorithmic bias to worsen health disparities (140, 141). Nursing profession's core commitment to patient advocacy mandates an ethically grounded approach to technology adoption (115, 116). Therefore, organizations must develop and implement clear ethical frameworks for all advanced technologies, ensuring that patient privacy, data security, and human accountability remain paramount. As patient advocates, nurses should be central to the development and review of these frameworks. Furthermore, there is an imperative to address health equity by creating strategies that ensure advancements in surgical care and training are accessible to all patients and clinicians, including those in rural or under-resourced settings. Ultimately, technology adoption must be prioritized through a human-centered lens, involving nurses in the design and selection of tools to guarantee they augment, rather than impede, the essential clinical judgment and compassionate care that define the nursing profession.
Author contributions
LG: Data curation, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. HZ: Data curation, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. YS: Data curation, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. CQ: Data curation, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Gen AI was used in the creation of this manuscript. During the preparation and revision of this manuscript, the authors utilized the generative artificial intelligence tool Gemini and ChatGPT. AI was employed for the Language Enhancement and Editing to improve grammar, syntax, and clarity, and to ensure a consistent academic tone throughout the document. The authors meticulously reviewed, critically evaluated, and edited all text generated by the AI. The authors take full and final responsibility for all content in this manuscript, including the factual accuracy of all statements, the appropriateness of citations, and the originality of the work. The entire manuscript was checked for plagiarism by the authors.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hussain AK, Kakakhel MM, Ashraf MF, Shahab M, Ahmad F, Luqman F, et al. Innovative approaches to safe surgery: a narrative synthesis of best practices. Cureus. (2023) 15:e49723. doi: 10.7759/cureus.49723
2. Tabatabaei Mohammadi A, Keihani Far Y, Hossein Zadeh R, Bagherian Kenari SBP, Erfan Ghanbarzadeh MK, Seyed Mohammad Ali Fazayel, PY, et al. Contemporary Surgical Innovations: A Comprehensive Guide to Emerging Technologies and Practices. Iran: Independently (2024). p. 283.
3. Chellam Singh B, Arulappan J. Operating room nurses' understanding of their roles and responsibilities for patient care and safety measures in intraoperative practice. SAGE Open Nurs. (2023) 9:23779608231186247. doi: 10.1177/23779608231186247
4. Gao L, Lu Q, Hou X, Ou J, Wang M. Effectiveness of a nursing innovation workshop at enhancing nurses' innovation abilities: a quasi-experimental study. Nurs Open. (2022) 9:418–27. doi: 10.1002/nop2.1080
5. Girard N. Nursing care delivery models. The perioperative environment. Aorn J. (1993) 57:481–8. doi: 10.1016/S0001-2092(07)64104-0
6. Clipper B. The Innovation Handbook: A Nurse Leader's Guide to Transforming Nursing. Indianapolis, IN: Sigma Theta Tau (2023).
8. Alqarny HAM, Algarni ANM, Alshehri ASM, Alshehri MAY, Alshehri MMM, Alshehri AA, et al. Interdisciplinary collaboration in healthcare: the synergy of nurses, laboratory services, anesthesiologists, emergency, and operative teams. J Int Crisis Risk Commun Res. (2024) 7:1295.
9. Hanawi MK, Hilal FM, Aljohani AM, Bader HA, Almalky MA, Shiekh KE, et al. Exploring the role of operating room technician in maintaining safety and accuracy in anesthetic drug delivery. J Int Crisis Risk Commun Res. (2024) 7:3119.
10. Larsen PD. Artificial intelligence and nursing practice. Rehabil Nurs. (2024) 49:73–4. doi: 10.1097/RNJ.0000000000000454
11. Stella M, Zaytseva A. Forma mentis networks map how nursing and engineering students enhance their mindsets about innovation and health during professional growth. PeerJ Comput Sci. (2020) 6:e255. doi: 10.7717/peerj-cs.255
12. Baradaran K, Gracia C, Alimohammadi E. Exploring strategies to enhance patient safety in spine surgery: a review. Patient Saf Surg. (2025) 19:3. doi: 10.1186/s13037-025-00426-2
13. Adamina M, Gié O, Demartines N, Ris F. Contemporary perioperative care strategies. J Br Surg. (2013) 100:38–54. doi: 10.1002/bjs.8990
14. Dean HF, Carter F, Francis NK. Modern perioperative medicine - past, present, and future. Innov Surg Sci. (2019) 4:123–31. doi: 10.1515/iss-2019-0014
15. Almansour MS, Althobiti NMA, Alharthi FFA, Alharthi MAG, Alharthi ASD, Al Mansour MHA, et al. Preparing the operating room for various surgical procedures. J Int Crisis Risk Commun Res. (2024) 7:3258.
16. Hussein AM. Enhancing patient safety in the operating room: a comprehensive guide from a nurse's perspective. Open J Nurs. (2024) 14:252–66. doi: 10.4236/ojn.2024.146018
17. Salazar Maya ÁM, Osorio Galeano SP. Nursing care related with surgical position. Investigación y educación en enfermería. Invest Educ Enferm. (2023) 41:03. doi: 10.17533/udea.iee.v41n1e03
18. Anderton J. The prone position for the surgical patient: a historical review of the principles and hazards. Br J Anaesth. (1991) 67:452–63. doi: 10.1093/bja/67.4.452
19. Abraham J, Rosen M, Greilich PE. Improving perioperative handoffs: moving beyond standardized checklists and protocols. Joint Comm J Qual Patient Saf. (2023) 49:341–4. doi: 10.1016/j.jcjq.2023.05.002
20. Achrekar MS. Enhanced recovery after surgery (ERAS) nursing programme. Asia-Pac J Oncol Nurs. (2022) 9:3. doi: 10.1016/j.apjon.2022.02.003
21. Mithany RH, Daniel N, Shahid MH, Aslam S, Abdelmaseeh M, Gerges F, et al. Revolutionizing surgical care: the power of enhanced recovery after surgery (ERAS). Cureus. (2023) 15:e48795. doi: 10.7759/cureus.48795
22. Guzzi G, Ricciuti RA, Della Torre A, Lo Turco E, Lavano A, Longhini F, et al. Intraoperative neurophysiological monitoring in neurosurgery. J Clin Med. (2024) 13:2966. doi: 10.3390/jcm13102966
23. Oliva AM, Montejano J, Simmons CG, Vogel SA, Isaza CF, Clavijo CF. New frontiers in intraoperative neurophysiologic monitoring: a narrative review. Ann Transl Med. (2023) 11:388. doi: 10.21037/atm-22-4586
24. Yu H, Wu L. Analysis of the effects of evidence-based nursing interventions on promoting functional recovery in neurology and general surgery intensive care patients. Altern Ther Health Med. (2024) 30.
25. Nilsson U, Gruen R, Myles P. Postoperative recovery: the importance of the team. Anaesthesia. (2020) 75:e158–64. doi: 10.1111/anae.14869
27. Titler MG. The evidence for evidence-based practice implementation. In:Hughes RG, , editor. Patient safety and Quality: An Evidence-based handBook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (2008).
28. Ernstmeyer K, Christman E. Chapter 4: Nursing process. In:Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, , editors. Nursing Fundamentals. Eau Claire, WI: Chippewa Valley Technical College (2021).
29. Akbari L, Aarabi A, Bahrami M. Challenges of intraoperative documentation and its role in patient safety: an integrative review. Iran J Nurs Midwifery Res. (2025) 30:141–9. doi: 10.4103/ijnmr.ijnmr_413_23
30. Alhaseri MOM, Ashour AS, Albishri BH, Al-Mutairi AH, Al-Hazmi MA, Alhujaily YM, et al. The Role of Operating Room and Anesthesia Technicians in Ensuring Surgical Success and Patient Safety. (2019).
31. Loftus TJ, Tighe PJ, Filiberto AC, Efron PA, Brakenridge SC, Mohr AM, et al. Artificial intelligence and surgical decision-making. JAMA Surg. (2020) 155:148–58. doi: 10.1001/jamasurg.2019.4917
32. Panahi O. Innovations in surgical healthcare: the future of medicine. Int J Res Med Health Sci. (2025) 1:1−8.
33. Singam A. Revolutionizing patient care: a comprehensive review of artificial intelligence applications in anesthesia. Cureus. (2023) 15:e49887. doi: 10.7759/cureus.49887
34. Nijkamp N, Wakefield E. The Future of Artificial Intelligence in Perioperative Nursing. Lyndoch, SA: ACORN (2024). p. e1–4.
35. Dixon D, Sattar H, Moros N, Kesireddy SR, Ahsan H, Lakkimsetti M, et al. Unveiling the influence of AI predictive analytics on patient outcomes: a comprehensive narrative review. Cureus. (2024) 16:e59954. doi: 10.7759/cureus.59954
36. Wei Q, Pan S, Liu X, Hong M, Nong C, Zhang W. The integration of AI in nursing: addressing current applications, challenges, and future directions. Front Med. (2025) 12:1545420. doi: 10.3389/fmed.2025.1545420
37. Rony MKK, Alrazeeni DM, Akter F, Nesa L, Chandra Das D, Uddin MJ, et al. The role of artificial intelligence in enhancing nurses' work-life balance. J Med Surg Public Health. (2024) 3:100135. doi: 10.1016/j.glmedi.2024.100135
38. Rony MKK, Parvin MR, Ferdousi S. Advancing nursing practice with artificial intelligence: enhancing preparedness for the future. Nurs Open. (2024) 11:2070. doi: 10.1002/nop2.2070
39. Maleki Varnosfaderani S, Forouzanfar M. The Role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering. (2024) 11:337. doi: 10.3390/bioengineering11040337
40. Iqbal AI, Aamir A, Hammad A, Hafsa H, Basit A, Oduoye MO, et al. Immersive technologies in healthcare: an in-depth exploration of virtual reality and augmented reality in enhancing patient care, medical education, and training paradigms. J Prim Care Community Health. (2024) 15:21501319241293311. doi: 10.1177/21501319241293311
41. Havola S, Haavisto E, Mäkinen H, Engblom J, Koivisto J-M. The effects of computer-based simulation game and virtual reality simulation in nursing students' self-evaluated clinical reasoning skills. CIN: Comput Inf Nurs. (2021) 39:725–35. doi: 10.1097/CIN.0000000000000748
42. Keny C. The Potential of Immersive Virtual Reality as a Non-Pharmacological Method for Postoperative Pain Relief Among Older Adults. San Francisco, CA: University of California, San Francisco (2024).
43. Niyonkuru E, Iqbal MA, Zhang X, Ma P. Complementary approaches to postoperative pain management: a review of non-pharmacological interventions. Pain Ther. (2025) 14:121–44. doi: 10.1007/s40122-024-00688-1
44. Charlet M. Chapter 7 - Surgery of the future: harnessing the power of virtual reality and augmented reality. In:Hemanth DJ, Jeyanthi PM, , editors. Leveraging Metaverse and Analytics of Things (AoT) in Medical Systems. Cambridge, MA: Academic Press (2025). p. 125–45. doi: 10.1016/B978-0-443-24049-2.00003-0
45. Ruscher A. Optimizing Postoperative Care: The Significance of Simulation Training in Reducing Adverse Events and Promoting Patient Safety. Boston, MA: Northeastern University (2024).
46. Adeghe EP, Okolo CA, Ojeyinka OT. A review of wearable technology in healthcare: monitoring patient health and enhancing outcomes. OARJ Multidiscip Stud. (2024) 7:142–8. doi: 10.53022/oarjms.2024.7.1.0019
47. Appelboom G, Yang AH, Christophe BR, Bruce EM, Slomian J, Bruyère O, et al. The promise of wearable activity sensors to define patient recovery. J Clin Neurosci. (2014) 21:1089–93. doi: 10.1016/j.jocn.2013.12.003
48. Kalid N, Zaidan A, Zaidan B, Salman OH, Hashim M, Muzammil H. Based real time remote health monitoring systems: a review on patients prioritization and related“ big data” using body sensors information and communication technology. J Med Syst. (2018) 42:1–30. doi: 10.1007/s10916-018-0916-7
49. Eddahchouri Y, Peelen RV, Koeneman M, Touw HR, van Goor H, Bredie SJ. Effect of continuous wireless vital sign monitoring on unplanned ICU admissions and rapid response team calls: a before-and-after study. Br J Anaesth. (2022) 128:857–63. doi: 10.1016/j.bja.2022.01.036
50. Kang HS, Exworthy M. Wearing the future—wearables to empower users to take greater responsibility for their health and care: scoping review. JMIR mHealth uHealth. (2022) 10:e35684. doi: 10.2196/35684
51. Tariq MU. Advanced wearable medical devices and their role in transformative remote health monitoring. In: Transformative Approaches to Patient Literacy and Healthcare Innovation. London: IGI Global (2024). p. 308–26. doi: 10.4018/979-8-3693-3661-8.ch015
52. Fatima S. Transforming healthcare with AI and machine learning: revolutionizing patient care through advanced analytics. Int J Educ Sci Res Rev. (2024) 11.
53. Przadka M, Pajak W, Kleinrok J, Pec J, Michno K, Karpiński R, et al. Advances in 3D printing applications for personalized orthopedic surgery: from anatomical modeling to patient-specific implants. J Clin Med. (2025) 14:3989. doi: 10.3390/jcm14113989
54. Malukhin K, Ehmann K. Mathematical modeling and virtual reality simulation of surgical tool interactions with soft tissue: a review and prospective. J Eng Sci Med Diagn Ther. (2018) 1:020802. doi: 10.1115/1.4039417
55. Fadero PE, Shah M. Three dimensional (3D) modelling and surgical planning in trauma and orthopaedics. Surgeon. (2014) 12:328–33. doi: 10.1016/j.surge.2014.03.008
56. Fong AJ, Smith M, Langerman A. Efficiency improvement in the operating room. J Surg Res. (2016) 204:371–83. doi: 10.1016/j.jss.2016.04.054
57. Bakshi I, Rawat HS, Singh S. Exploring the impact of 3D printing on advancing reconstructive surgery: a comprehensive review. Int Multidiscip Res J. (2024) 6:1–16. doi: 10.36948/ijfmr.2024.v06i02.14675
58. Paxton NC, Tetsworth K, Woodruff MA. Personalization for surgical implants. In:Paul G, Doweidar MH, , editors. Digital Human Modeling and Medicine. London: Elsevier (2023). p. 849–74. doi: 10.1016/B978-0-12-823913-1.00019-1
59. Chang SE, Chen Y. Blockchain in health care innovation: literature review and case study from a business ecosystem perspective. J Med Internet Res. (2020) 22:e19480. doi: 10.2196/19480
60. Liu H, Crespo RG, Martínez OS. Enhancing privacy and data security across healthcare applications using blockchain and distributed ledger concepts. Healthcare. (2020) 8:243. doi: 10.3390/healthcare8030243
61. Ali Beshi ZI, Altuwayr GM, Alaryani SA, Beshi FI, Alghamdi SSA, Alobayli MYS. Leveraging the Implementation of Technology in Enhancing Nursing Practice and Patient Outcomes.
62. Zhang D, Ding H, Shen C, Liu Y, Jia N. Evaluating the role of nursing interventions in enhanced recovery after surgery for minimally invasive spine surgery: a retrospective analysis. Fron Surg. (2025) 12:1519135. doi: 10.3389/fsurg.2025.1519135
63. Li Y, Yan C, Li J, Wang Q, Zhang J, Qiang W, et al. A nurse-driven enhanced recovery after surgery (ERAS) nursing program for geriatric patients following lung surgery. Thorac Cancer. (2020) 11:1105–13. doi: 10.1111/1759-7714.13372
64. Jain SN, Lamture Y, Krishna M. Enhanced recovery after surgery: exploring the advances and strategies. Cureus. (2023) 15:e47237. doi: 10.7759/cureus.47237
65. Ismail MF, Sharma R. Redefining Perioperative Care: The Pivotal Role of Anesthesiologists in Enhanced Recovery After Surgery (ERAS) Protocols.
66. Tippireddy S, Ghatol D. Anesthetic Management for Enhanced Recovery After Major Surgery (ERAS). Treasure Island, FL: StatPearls Publishing (2023).
67. Altman AD, Helpman L, McGee J, Samouëlian V, Auclair MH, Brar H, et al. Enhanced recovery after surgery: implementing a new standard of surgical care. CMAJ. (2019) 191:E469–75. doi: 10.1503/cmaj.180635
68. Miller TE, Roche AM, Mythen M. Fluid management and goal-directed therapy as an adjunct to Enhanced Recovery After Surgery (ERAS). Can J Anaesth. (2015) 62:158–68. doi: 10.1007/s12630-014-0266-y
69. Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. (2022) 11:121–9. doi: 10.2217/cer-2021-0258
70. Chou D, Mundis G, Wang M, Fu K-M, Shaffrey C, Okonkwo D, et al. Minimally invasive surgery for mild-to-moderate adult spinal deformities: impact on intensive care unit and hospital stay. World Neurosurg. (2019) 127:e649–55. doi: 10.1016/j.wneu.2019.03.237
71. Echeverria-Villalobos M, Stoicea N, Todeschini AB, Fiorda-Diaz J, Uribe AA, Weaver T, et al. Enhanced recovery after surgery (ERAS): a perspective review of postoperative pain management under ERAS pathways and its role on opioid crisis in the United States. Clin J Pain. (2020) 36:219–26. doi: 10.1097/AJP.0000000000000792
72. Balfour A, Amery J, Burch J, Smid–Nanninga H. Enhanced recovery after surgery (ERAS®): barriers and solutions for nurses. Asia-Pac J Oncol Nurs. (2022) 9:100040. doi: 10.1016/j.apjon.2022.02.002
73. Tan VS, editor Maximizing Workforce. HRD for Developing States and Companies: Proceedings of the 2005 Brunei Darussalam AEMC Convention. Singapore: Institute of Southeast Asian Studies (2005).
74. Zhang Q, Yu B, Ou Y, Zhou X, Zou S, Peng H, et al. Progress of research on methods of human resource allocation in operating room nursing. Front Public Health. (2025) 13:1539108. doi: 10.3389/fpubh.2025.1539108
75. Khaw KW, Alnoor A, Al-Abrrow H, Tiberius V, Ganesan Y, Atshan NA. Reactions towards organizational change: a systematic literature review. Curr Psychol. (2022) 1–24. doi: 10.1007/s12144-022-03070-6
76. Griffiths P, Saville C, Ball J, Jones J, Pattison N, Monks T. Nursing workload, nurse staffing methodologies and tools: a systematic scoping review and discussion. Int J Nurs Stud. (2020) 103:103487. doi: 10.1016/j.ijnurstu.2019.103487
77. Cenacchi C, Giusti M, Peghetti A, Quirini S, Tinelli F, Giorgi S, et al. Optimization of nursing staff standards in the perioperative settings of the IRCCS University Hospital of Bologna. An improvement project. Front Public Health. (2025) 13:1601290. doi: 10.3389/fpubh.2025.1601290
78. Namaganda GN, Whitright A, Maniple EB. Lessons learned from implementation of the Workload Indicator of Staffing Need (WISN) methodology: an international Delphi study of expert users. Hum Resour Health. (2022) 19:138. doi: 10.1186/s12960-021-00675-z
79. Wang S-R, Zhou K, Zhang W. Application progress of nursing intervention in cardiac surgery. World J Clin Cases. (2023) 11:7943. doi: 10.12998/wjcc.v11.i33.7943
80. Elmetwaly RM, El Sayed RA. Chest tube removal: efficacy of cold application and breathing exercises on pain and anxiety level. Evid-Based Nurs Res. (2020) 2:12. doi: 10.47104/ebnrojs3.v2i4.159
81. Yang K, Shao X, Lv X, Yang F, Shen Q, Fang J, et al. Perioperative psychological issues and nursing care among patients undergoing minimally invasive surgeries. Laparosc Endosc Robot Surg. (2022) 5:92–9. doi: 10.1016/j.lers.2022.06.001
82. Lobdell KW, Appoo JJ, Rose GA, Ferguson B, Chatterjee S. Technological advances to enhance recovery after cardiac surgery. J Hosp Manag Health Policy. (2021) 5. doi: 10.21037/jhmhp-20-114
83. Raheem AA, Song HJ, Chang KD, Choi YD, Rha KH. Robotic nurse duties in the urology operative room: 11 years of experience. Asian J Urol. (2017) 4:116–23. doi: 10.1016/j.ajur.2016.09.012
84. Hardin SR, Kaplow R. Cardiac Surgery Essentials for Critical Care Nursing. Burlington, MA: Jones & Bartlett Learning (2025).
85. Qiu X. Nurse-led intervention in the management of patients with cardiovascular diseases: a brief literature review. BMC Nurs. (2024) 23:6. doi: 10.1186/s12912-023-01422-6
86. Sun J. Impacts of operating room refined nursing on orthopedic surgery patients. Bone Arthrosurg Sci. (2023) 1:14–20. doi: 10.26689/bas.v1i3.5726
87. Wong KC. 3D-printed patient-specific applications in orthopedics. Orthop Res Rev. (2016) 8:57–66. doi: 10.2147/ORR.S99614
88. Almutairi AND, Alshahrani WAF, Almansour HAA, Alotaibi KM, Alqasmi LH, Sheikh MM, et al. The role of advanced prosthetic technologies in enhancing patient mobility and independence: implications for nursing practice in orthopedic surgery. J Ecohumanism. (2024) 3:13048–55. doi: 10.62754/joe.v3i8.6169
89. Suarez-Ahedo C, Lopez-Reyes A, Martinez-Armenta C, Martinez-Gomez LE, Martinez-Nava GA, Pineda C, et al. Revolutionizing orthopedics: a comprehensive review of robot-assisted surgery, clinical outcomes, and the future of patient care. J Robot Surg. (2023) 17:2575–81. doi: 10.1007/s11701-023-01697-6
90. Struemph JM, Chong AC, Wooley PH. Evaluation of different experience levels of orthopaedic residents effect on polymethylmethacrylate (PMMA) bone cement mechanical properties. Iowa Orthop J. (2015) 35:193–8.
91. Arora M, Chan EK, Gupta S, Diwan AD. Polymethylmethacrylate bone cements and additives: a review of the literature. World J Orthop. (2013) 4:67–74. doi: 10.5312/wjo.v4.i2.67
92. Shady RHA, El-Shaboury RHR, Elsaid RAA, Ahmed SAE-M, Badawy GG, Hamed WE, et al. Enhancing nursing practice through patient outcome measures: a framework for optimizing care in intracranial surgery. BMC Nurs. (2025) 24:402. doi: 10.1186/s12912-025-02960-x
93. Zagzoog N. Feasibility of Skull Base Neuronavigation Using Optical Topographic Imaging Toward Guidance of Human and Robotic Drill Operators. Toronto, ON: University of Toronto (2023).
94. Gertsch JH, Moreira JJ, Lee GR, Hastings JD, Ritzl E, Eccher MA, et al. Practice guidelines for the supervising professional: intraoperative neurophysiological monitoring. J Clin Monit Comput. (2019) 33:175–83. doi: 10.1007/s10877-018-0201-9
95. Nagpal K, Vats A, Lamb B, Ashrafian H, Sevdalis N, Vincent C, et al. Information transfer and communication in surgery: a systematic review. Ann Surg. (2010) 252:225–39. doi: 10.1097/SLA.0b013e3181e495c2
96. Alshammri A, Almalki A, Alasmary M, Alshihre M, Al-Qarni H, Alqahtani T, et al. The impact of patient-centered care at work: make a difference to the patient experience. Int J Sci Res. (2022) 1:171–87. doi: 10.59992/IJSR.2022.v1n2p8
97. Darko EM, Kleib M, Lemermeyer G, Tavakoli M. Robotics in nursing: protocol for a scoping review. JMIR Res Protoc. (2023) 12:e50626. doi: 10.2196/50626
99. Anurogo D, Hidayat NA. The Art Of Televasculobiomedicine 5.0. Makassar: Nas Media Pustaka (2023).
100. Mani Z, Chouk I. Consumer resistance to innovation in services: challenges and barriers in the internet of things era. J Prod Innov Manag. (2018) 35:780–807. doi: 10.1111/jpim.12463
101. Chaudhary G. Unveiling the black box: bringing algorithmic transparency to AI. Masaryk Univ J Law Technol. (2024) 18:93–122. doi: 10.5817/MUJLT2024-1-4
102. Malone M, Way DP, Leung CG, Danforth D, Maicher K, Vakil J, et al. Evaluation of high-fidelity and virtual reality simulation platforms for assessing fourth-year medical students' encounters with patients in need of urgent or emergent care. Ann Med. (2024) 56:2382947. doi: 10.1080/07853890.2024.2382947
103. Javed H, Olanrewaju OA, Owusu FA, Saleem A, Pavani P, Tariq H, et al. Challenges and solutions in postoperative complications: a narrative review in general surgery. Cureus. (2023) 15:e50942. doi: 10.7759/cureus.50942
104. Ngafeeson M. Understanding User Resistance to Information Technology in Healthcare: The Nature and Role Of Perceived Threats. (2015).
105. Amin SM, El-Gazar HE, Zoromba MA, El-Sayed MM, Atta MHR. Sentiment of nurses towards artificial intelligence and resistance to change in healthcare organisations: a mixed-method study. J Adv Nurs. (2025) 81:2087–98. doi: 10.1111/jan.16435
106. Traynor M, Boland M, Buus N. Autonomy, evidence and intuition: nurses and decision-making. J Adv Nurs. (2010) 66:1584–91. doi: 10.1111/j.1365-2648.2010.05317.x
107. Lee AT, Ramasamy RK, Subbarao A. Barriers to and facilitators of technology adoption in emergency departments: a comprehensive review. Int J Environ Res Public Health. (2025) 22:479. doi: 10.3390/ijerph22040479
108. Hayward D, Bungay V, Wolff AC, MacDonald V. A qualitative study of experienced nurses' voluntary turnover: learning from their perspectives. J Clin Nurs. (2016) 25:1336–45. doi: 10.1111/jocn.13210
109. Konda NN, Lewis TL, Furness HN, Miller GW, Metcalfe AJ, Ellard DR. Surgeon views regarding the adoption of a novel surgical innovation into clinical practice: systematic review. BJS Open. (2024) 8:zrad141. doi: 10.1093/bjsopen/zrad141
110. Martin P, Jamal O, Bozorg S, Khullar T, Workman R. Overcoming the Barriers to AI Adoption in Transport. (2025).
111. Adepoju AH, Austin-Gabriel B, Eweje A, Collins A. Framework for automating multi-team workflows to maximize operational efficiency and minimize redundant data handling. IRE J. (2022) 5:663–4.
112. AMERICAN NURSES Association. The Ethical Use of Artificial Intelligence in Nursing practice. Position Statement by ANA Center for Ethics and Human Rights. Silver Spring, MD: American Nurses Association (2022).
113. Balahur A, Jenet A, Hupont IT, Charisi V, Ganesh A, Griesinger CB, et al. Data Quality Requirements for Inclusive, Non-Biased and Trustworthy AI. (2022).
114. Williamson SM, Prybutok V. Balancing privacy and progress: a review of privacy challenges, systemic oversight, and patient perceptions in AI-driven healthcare. Appl Sci. (2024) 14:675. doi: 10.3390/app14020675
115. Wynn M. The digital dilemma in nursing: a critique of care in the digital age. Br J Nurs. (2024) 33:496–9. doi: 10.12968/bjon.2024.0023
116. Johnson EA, Galatzan BJ. A critical juncture: reimagining nursing professional identity and regulation in the ethical integration of innovation and technology in healthcare. J Nurs Regul. (2025) 16:10–6. doi: 10.1016/j.jnr.2025.03.005
117. Ahsan MJ. Cultivating a culture of learning: the role of leadership in fostering lifelong development. Learn Organ. (2025) 32:282–306. doi: 10.1108/TLO-03-2024-0099
119. Bynens M. Empowering Excellence: Strategies for Cultivating a Culture of Bold Decision-Making in Teams.
120. Madanchian M. Leadership dynamics in innovative teams. In: Mastering Innovation in Business. London: IGI Global (2025). p. 103–30. doi: 10.4018/979-8-3693-3759-2.ch005
121. Montes JO, Olleros FX. Microfactories and the new economies of scale and scope. J Manuf Technol Manag. (2020) 31:72–90. doi: 10.1108/JMTM-07-2018-0213
122. Koukourikos K, Tsaloglidou A, Kourkouta L, Papathanasiou IV, Iliadis C, Fratzana A, et al. Simulation in clinical nursing education. Acta Inform Med. (2021) 29:15–20. doi: 10.5455/aim.2021.29.15-20
123. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, et al. The impact of simulation-based training in medical education: a review. Medicine. (2024) 103:e38813. doi: 10.1097/MD.0000000000038813
124. Chen FQ, Leng YF, Ge JF, Wang DW, Li C, Chen B, et al. Effectiveness of virtual reality in nursing education: meta-analysis. J Med Internet Res. (2020) 22:e18290. doi: 10.2196/18290
125. Phillips-Wren G, AI. tools in decision making support systems: a review. Int J Artif Intell Tools. (2012) 21:1240005. doi: 10.1142/S0218213012400052
126. Shoman H. Identification Ranking and Prioritization of Decision-Making Criteria for the Early Adoption of Innovative Surgical Technologies into the Canadian Healthcare System: A Multi-Criteria Decision Analysis. Montreal, QC: McGill University (2023). doi: 10.1001/jamanetworkopen.2023.43703
127. Broome ME. Transformational Leadership in Nursing: From Expert Clinician to Influential Leader. Cham: springer publishing company. (2024). doi: 10.1891/9780826192554
129. Ahmed A, McGough D, Austin S, editors. Integration of BIM in higher education: case study of the adoption of bim into coventry university's department of civil engineering, architecture and building. In: Sustainable Building and Construction Conference. Coventry: Coventry University (2013).
130. Clayton JL, Miller KJ. Professional and regulatory infection control guidelines: collaboration to promote patient safety. AORN J. (2017) 106:201–10. doi: 10.1016/j.aorn.2017.07.005
131. Williams K. Guidelines in practice: patient information management. AORN J. (2023) 117:52–60. doi: 10.1002/aorn.13844
132. Applequist J, Miller-Day M, Cronholm PF, Gabbay RA, Bowen DS. “In principle we have agreement, but in practice it is a bit more difficult”: obtaining organizational buy-in to patient-centered medical home transformation. Qual Health Res. (2017) 27:909–22. doi: 10.1177/1049732316680601
133. Johnston KA, Taylor M. Engagement as communication: pathways, possibilities, and future directions. In: Johnston KA, Taylor M, , editors. The Handbook of Communication Engagement. Hoboken, NJ: John Wiley & Sons (2018). p. 1–15. doi: 10.1002/9781119167600.ch1
134. Camargo FC, Iwamoto HH, Galvão CM, Monteiro DAT, Goulart MB, Garcia LAA. Models for the implementation of evidence-based practice in hospital based nursing: a narrative review1. Texto Contexto-Enfermagem. (2018) 26. doi: 10.1590/0104-07072017002070017
135. Schimböck F, Eichhorn J. Creating A Virtual Nursing Journal Club: AN Innovative Teaching Method to Achieve Evidence-Based Practice in Healthcare. (2018).
136. Greenhalgh T. How to Implement Evidence-based Healthcare. Hoboken, NJ: John John Wiley & Sons (2017).
137. Panda N, Perez N, Tsangaris E, Edelen M, Pusic A, Zheng F, et al. Enhancing patient-centered surgical care with mobile health technology. J Surg Res. (2022) 274:178–84. doi: 10.1016/j.jss.2022.01.005
138. Bekbolatova M, Mayer J, Ong CW, Toma M, editors. Transformative potential of AI in healthcare: definitions, applications, and navigating the ethical landscape and public perspectives. Healthcare. (2024) 12:125. doi: 10.3390/healthcare12020125
139. Bangun AV, Pragholapati A. Enhancing critical thinking skills in nursing higher education in preparation for the industrial revolution 4.0. KnE Life Sci. (2021) 793−804. doi: 10.18502/kls.v6i1.8756
140. King CR, Shambe A, Abraham J. Potential uses of AI for perioperative nursing handoffs: a qualitative study. JAMIA Open. (2023) 6:ooad015. doi: 10.1093/jamiaopen/ooad015
141. Sánchez AMR, Bhatia I, Pinto SF. Navigating Artificial Intelligence from a Human Rights Lens: Impacts, Tradeoffs and Regulations for Groups in Vulnerable Situations. (2023).
142. George AS, Baskar T, Srikaanth PB. The erosion of cognitive skills in the technological age: how reliance on technology impacts critical thinking, problem-solving, and creativity. Partners Univers Innov Res Publ. (2024) 2:147–63.
143. Leoni L, Gueli G, Ardolino M, Panizzon M, Gupta S. AI-empowered KM processes for decision-making: empirical evidence from worldwide organisations. J Knowl Manag. (2024) 28:320–47. doi: 10.1108/JKM-03-2024-0262
Keywords: intraoperative nursing, surgical innovation, perioperative care, healthcare technology, patient outcomes
Citation: Guo L, Zuo H, Sun Y and Qian C (2025) Elevating surgical outcomes: a comprehensive analysis of innovative nursing practices in intraoperative care across diverse specialties. Front. Med. 12:1665160. doi: 10.3389/fmed.2025.1665160
Received: 17 July 2025; Accepted: 05 September 2025;
Published: 03 October 2025.
Edited by:
Martina Giusti, University of Florence, ItalyReviewed by:
Yari Longobucco, University of Florence, ItalySilvio Quirini, IRCCS University Hospital of Bologna, Italy
Copyright © 2025 Guo, Zuo, Sun and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengcheng Qian, UTE4NzY0MDA4MTY5QG91dGxvb2suY29t
 Ling Guo1
Ling Guo1 Chengcheng Qian
Chengcheng Qian