- 1Department of Urology, Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences, Shanghai, China
- 2Department of Gynaecology and Obstetrics, Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences, Shanghai, China
- 3Department of Nursing, Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences, Shanghai, China
Background: While the importance of cultural and spiritual care proficiencies is well-validated in cancer supportive care and critical care settings, their relevance in urology remains to be substantiated. Gauging the spiritual care requisites of nurses within urology divisions may foster enhanced sentiments of hope, serenity, and fortitude among patients.
Objectives: This study aimed to examine cultural and spiritual care proficiencies among nurses tending to urology patients and to ascertain the correlation between the personal and professional attributes of these nurses and their perspectives on cultural and spiritual care competencies.
Methods: Thirty-five nurses affiliated with the urology department of Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences, China, were provided with a questionnaire encompassing the spiritual care competency scale and the cultural competence scale. All participating nurse practitioners were female, of Han Chinese ethnicity, adhered to Chinese culture, and were devoid of religious affiliations. Both instruments used a 6-point Likert scale (1: vehemently disagree, 2: disagree, 3: slightly disagree, 4: slightly agree, 5: agree, and 6: vehemently agree).
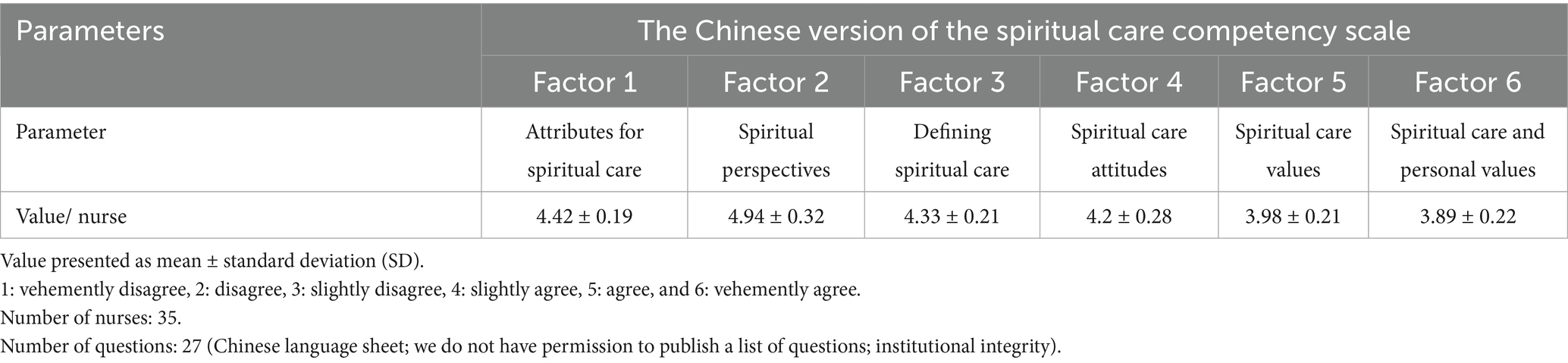
Results: Participating nurses possessed education at or above the junior college level. Nurses aged 35 and older accounted for 26%, while 63% had a decade or fewer of experience in urological nursing in China. The preeminent value within the spiritual care competency scale pertained to spiritual perspectives (factor 2; 4.94 ± 0.32/nurse), succeeded by attributes for spiritual care (factor 1; 4.42 ± 0.19/nurse), defining spiritual care (factor 3; 4.33 ± 0.21/nurse), spiritual care attitudes (factor 4; 4.2 ± 0.28/nurse), spiritual care values (factor 5; 3.98 ± 0.21/nurse), and spiritual care personal values (factor 6; 3.89 ± 0.22/nurse). The clinical nursing cultural competence scale registered at 4.24 ± 0.79/nurse. No associations were evident between personal/professional traits and perceptions of cultural and spiritual care competencies (p > 0.05 for all comparisons).
Conclusion: Nurses functioning within the urology department exhibited an affirmative outlook toward cultural and spiritual care proficiencies. The personal and professional attributes of nurses in urology are generally uncorrelated with their perceptions of cultural and spiritual care competencies. Nurses in the urology department have a heavy workload and insufficient knowledge of spiritual care practices.
Introduction
Spiritual care, predicated on astute attention to patients’ values and beliefs, demands considerable expertise and is enacted within a relationship of trust and confidence between healthcare professionals and patients (1). Spirituality constitutes an indispensable element of wellbeing, particularly for patients (2). Spiritual care identifies and addresses the exigencies of individuals confronting ill health, trauma, and life crises (3), correlating to enhanced quality of life and salutary health outcomes (4). The term ‘spiritus’, derived from the Latin for ‘to breathe’, denotes the vital essence of life, the wellspring of spirituality (5). China’s Health Planning Commission has affirmed the efficacy of cultural and spiritual care in improving the health outcomes of individuals experiencing ill health, trauma, and life crises (6), while underscoring the imperative for heightened cultural competence awareness among Chinese clinical nurses (7). Disparities persist in the competence and perceptions of spiritual care among these nurses (8). The significance of cultural and spiritual care competencies is well-documented in cancer supportive care (5, 9) and critical care units (7). Comparative analyses of these competencies across diverse diseases and settings are detailed in Table 1. However, their role remains nascent in urology (10), despite their manifest importance for nurses attending to urological patients (11). Ascertaining the spiritual needs of nurses within urology departments may foster hope, tranquility, and resilience in patients, encourage positive health behaviors, and facilitate the selection of appropriate coping mechanisms (10). Existing research on spirituality has predominantly focused on populations within England and the United States, largely encompassing Christian cultures (2), thereby accentuating the need for further investigation into spirituality in nursing across diverse ethnicities within the Asian populace (12).
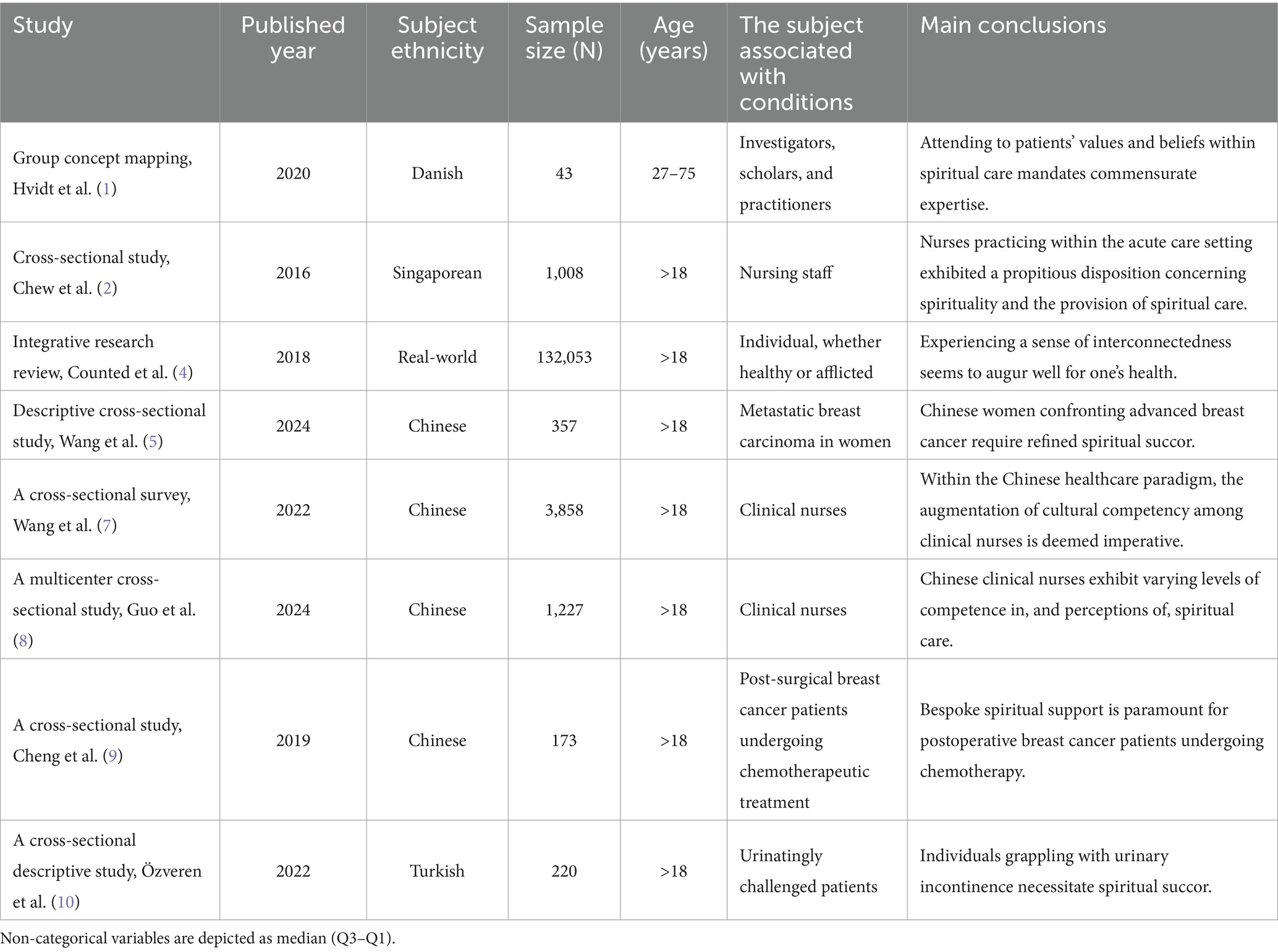
Table 1. Details of comparative studies on cultural and spiritual care competencies for different diseases in different settings.
Objectives
This cross-sectional pilot study aimed to investigate the cultural and spiritual care competencies possessed by nurses tending to urology patients. Furthermore, it aimed to assess the correlation between nurses’ personal and professional attributes and their perceived cultural and spiritual care competencies within the urological context.
Materials and methods
Ethics approval and consent to participate
The authors meticulously crafted the cross-sectional study’s protocols, subsequently ratified by the Human Ethics Committee of Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences (Approval No. SJdcH14178, dated December 5, 2022). This investigation adheres strictly to Chinese law and the v2008 Declaration of Helsinki (latest Chinese iteration). Prior to commencement, informed consent for participation and publication (across diverse formats and publications) was secured from all participating nurses. Ethical endorsement encompassed the authorized utilization of instruments—the Spiritual Care Competency Scale (Chinese version) and the Clinical Nursing Cultural Competence Scale (Chinese version)—through approvals granted by both the institutional Human Ethics Committee and the Department of Health and Education of China.
Design and setting
A quantitative, subjective, pilot cross-sectional study was conducted among nurses providing care to urology patients at Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences, China (a secondary-level hospital without affiliation to a tertiary institution).
Inclusion criteria
The study encompassed all nursing staff affiliated with urological patients, specifically those serving within the urology division from 31 December 2022 to 31 December 2024.
Exclusion criteria
Nurses declining participation by withholding data were excluded from the study; non-respondents were neither tracked nor comparatively analyzed.
Sample size calculations
Using a descriptive methodology with Kendall’s and Spearman’s correlation analyses (13), predicated on the questionnaire volume, and stipulating α = 0.05, β = 0.8, a 95% confidence interval (CI), and 2.3 participants per variable, the calculated sample size for this study comprised 35 nurses.
Outcome measures
The spiritual care competency scale (Chinese version)
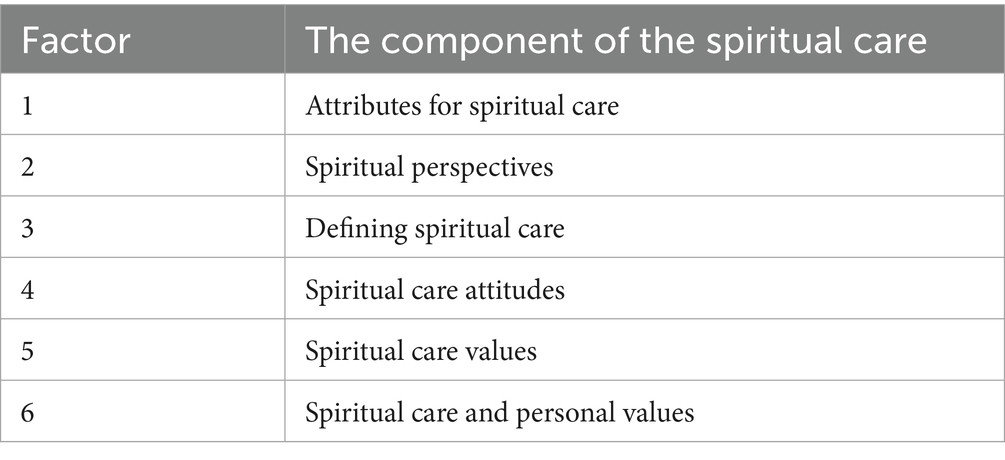
Comprising 27 questions in total, responses are gauged via a 6-point Likert scale (encompassing vehemently disagree, slightly disagree, disagree, vehemently agree, slightly agree, and agree). The spiritual care competency scale exhibits a six-factor structure, elaborated upon in Table 2. Cronbach’s α values range from 0.71 to 0.82 (14).
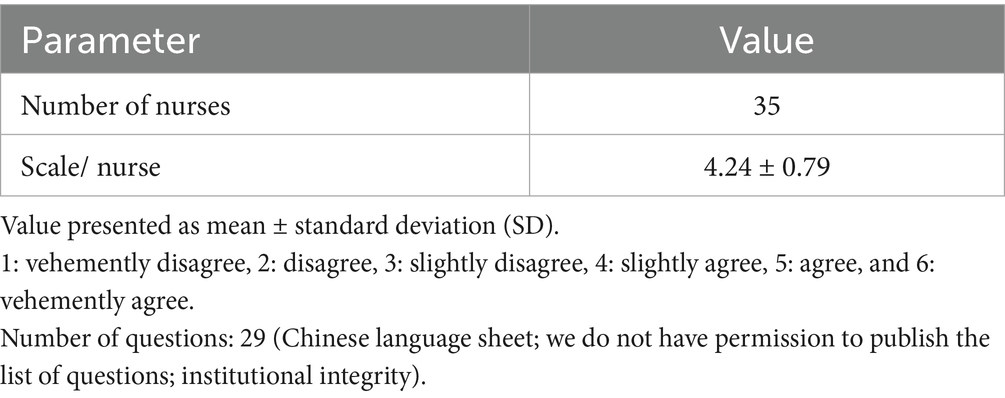
The clinical nursing cultural competence scale (Chinese version)
Cultural competence was delineated into four facets, gauged via a 29-item instrument. These items encompass cultural proficiencies (11 items), cultural erudition (8 items), cultural acumen (7 items), and cultural sensitivity (3 items). Responses are predicated on a 6-point Likert scale (ranging from vehement disagreement to tempered agreement). The derived Cronbach’s α was 0.88 (15).
Scale measurements and data collections
Each nurse was furnished with a QR-coded questionnaire to be duly completed within 1 week. After completion, the researchers shall collate the data in the background.
A 6-point Likert scale, as delineated in Table 3, was used for both instruments: the spiritual care competency scale and the clinical nursing cultural competence scale. Both instruments have been validated for use in Chinese populations. The authors personally administered both questionnaires and conducted the scoring process.
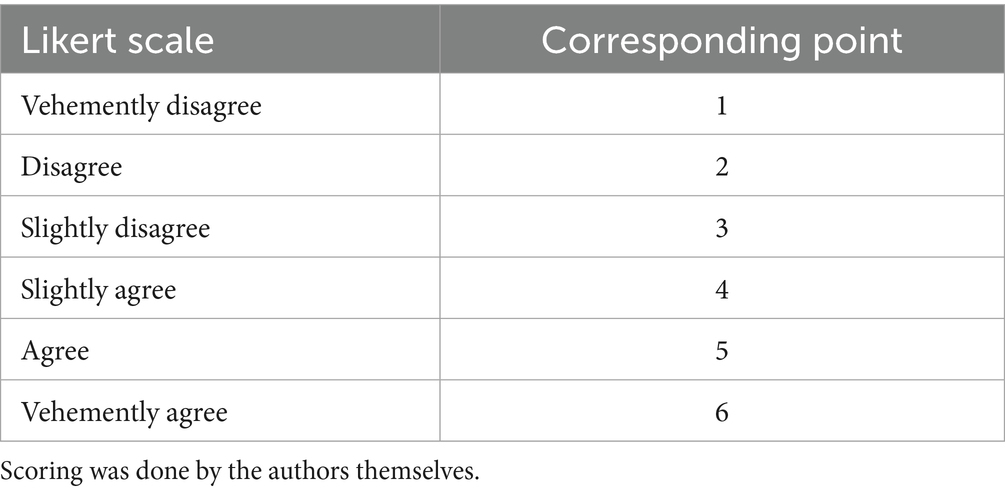
Table 3. Six-point Likert scale for the Chinese version of the spiritual care competency scale and the Chinese version of the clinical nursing cultural competence scale.
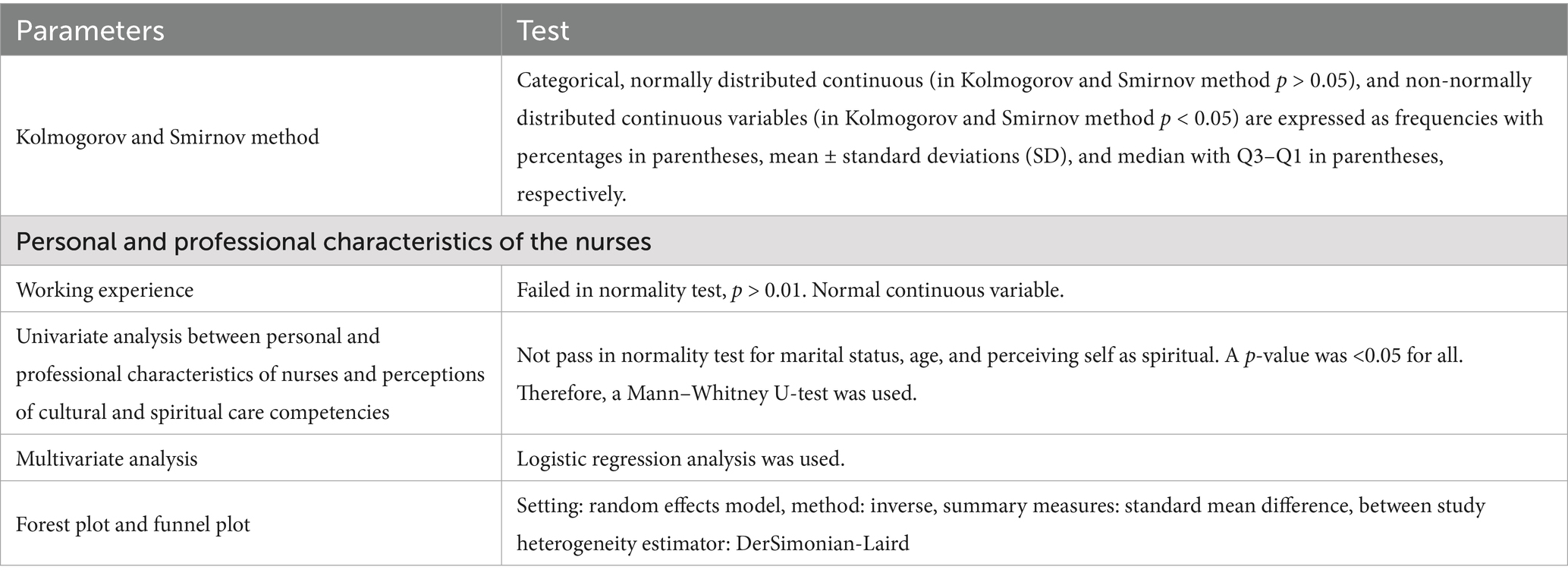
Data analysis
Statistical analyses were conducted utilizing InStat 3.01 (GraphPad Software, San Diego, CA, USA). Categorical variables are presented as frequencies (percentages). Continuous, normally distributed variables are summarized as mean ± standard deviation (SD). Non-normally distributed continuous variables are expressed as median [interquartile range (Q3–Q1)]. Means and SD were used for normal distributions; otherwise, median and quartiles (Q1, Q3) were reported when n was > 8; if n was ≤ 8, the Min-Max range was utilized. The Soup calculator® LLB (USA) was used for median, Q3, and Q1 calculations. The chi-square (ꭓ2) or Fisher’s exact test was applied to categorical variables. The Kolmogorov–Smirnov test assessed continuous variable normality, while the Bartlett test evaluated variance homogeneity in normally distributed continuous variables. The Mann–Whitney U-tests were used for univariate analyses. Both univariate and subsequent multivariate (logistic regression) analyses assessed associations between personal/professional characteristics of urology nurses and perceptions of cultural/spiritual care competencies (2). Significance was defined as a p-value of < 0.05 at 95% CI (two-tailed). Forest and funnel plots were generated via metaanalysisonline.com (2024–2025, ELIXIR Hungary). I2 > 50% indicated moderate heterogeneity. VisualGPT’s map maker1 was used to generate flowcharts.2 AI generator created the Graphical Abstract. Premium English Translator3 and Grammarly enhanced the English language. The Sentence Shortener4 AI condensed the text.
Results
Cohort demographics
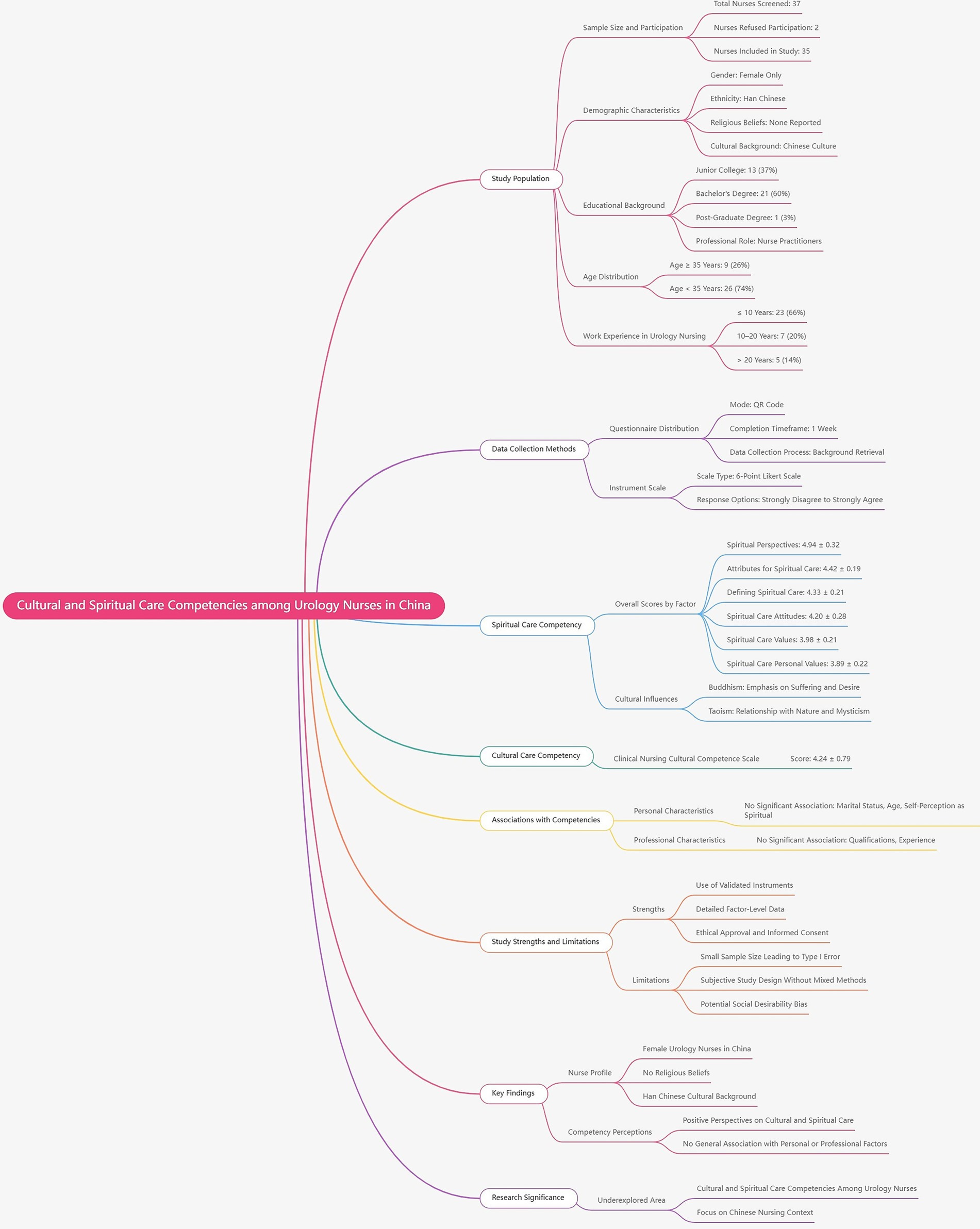
From 31 December 2022 to 31 December 2024, a cohort of 37 nurses underwent screening for study eligibility. Of these, two declined to furnish comprehensive data, resulting in their exclusion (n = 2). Data originating from 35 nurses used within the urology department of Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China, were included in the study. A flow diagram illustrating the cross-sectional pilot study design is provided in Figure 1.
Outcome measures
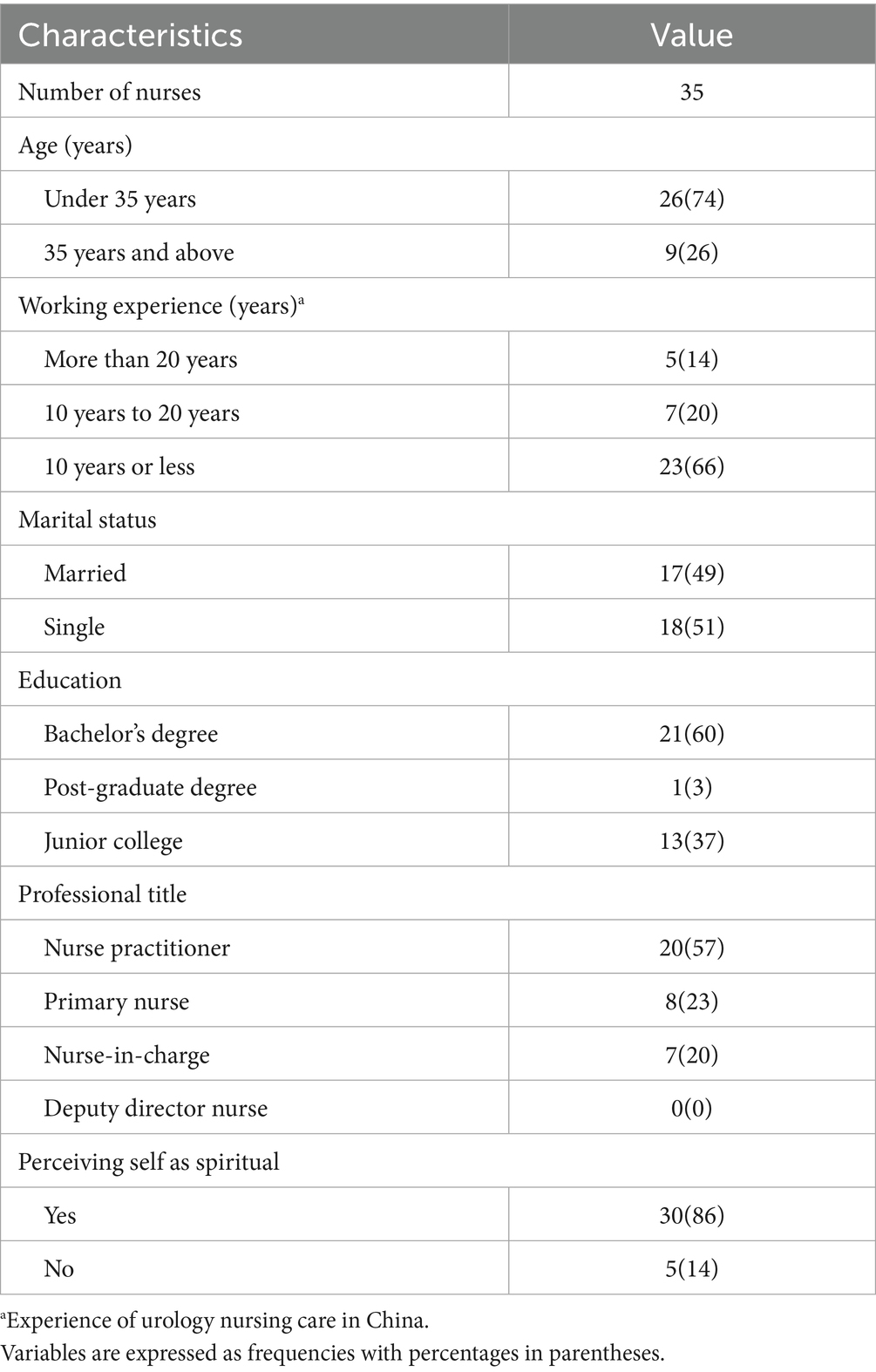
Nurse demographics
The cohort solely comprised individuals identifying as female, with no professed religious affiliations. All participants self-identified as being of Han Chinese ethnicity, possessed no less than a junior college-level education, and were registered nurse practitioners, demonstrably aligned with prevailing Chinese cultural norms. Nurses aged 35 years and older accounted for 26%, while 66% had a decade or fewer of experience in urological nursing within China. Comprehensive demographic and professional data pertaining to nurses engaged in urological patient care are delineated in Table 4.
Spiritual care competency scale (Chinese version)
Factor 2 exhibited the highest values, followed sequentially by factors 1, 3, 4, 5, and 6. Granular data about the Spiritual Care Competency Scale are presented in Table 5.
Clinical nursing cultural competence scale (Chinese version)
The Clinical Nursing Cultural Competence Scale yielded a mean score of 4.24 ± 0.79 per nurse (Table 6).
Correlation analysis
A univariate analysis identified marital status (p = 0.045, Mann–Whitney U-test), age ≥ 35 years (p = 0.039, Mann–Whitney U-test), and self-perceived spirituality (p = 0.041, Mann–Whitney U-test) as factors correlated with perceptions of cultural and spiritual care competencies (univariate analysis data not included). Multivariate logistic regression analyses revealed no statistically significant associations between personal/professional characteristics and perceived cultural/spiritual care competencies. The specifics are detailed in Table 7.
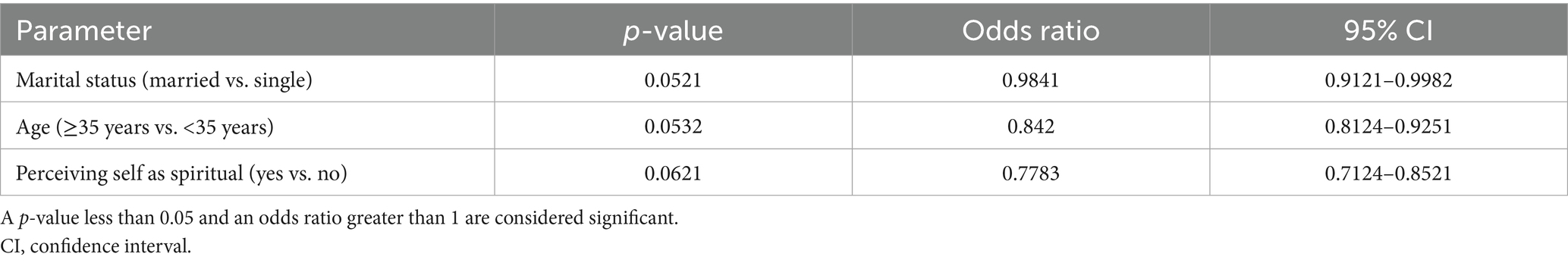
Table 7. Multivariate logistic regression analyses for the association between personal and professional characteristics of nurses and perceptions of cultural and spiritual care competencies.
Subsequent analysis incorporating three personal/professional characteristics (Figure 2), utilizing a random-effects model with inverse variance weighting to compute the hazard ratio (HR), revealed a statistically notable difference. The pooled HR was 0.87 (95% CI: 0.78–0.97; exact p-value for random effect was 0.013 and t-value was −2.49). The test for overall effect exhibited statistical significance (p < 0.05, random effects model with inverse variance). Significant heterogeneity was detected (p < 0.01, random effects model with inverse variance), implying variability in the magnitude and/or direction of individual personal/professional characteristics. The I2 statistic indicated that 88.7% of observed variance was attributed to heterogeneity rather than random error.
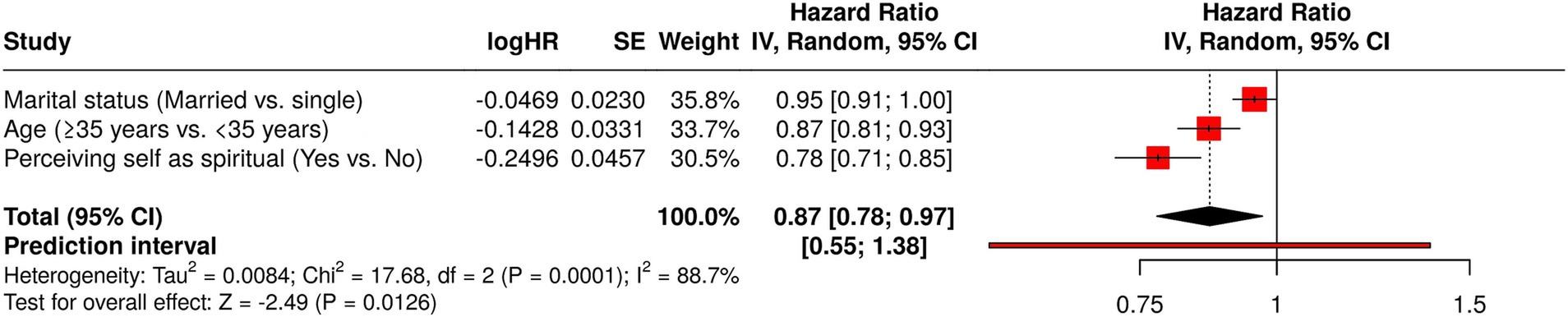
Figure 2. Forest plot illustrates the correlation between individual and occupational attributes and perspectives on cultural and spiritual care proficiencies.
Bias assessment
The funnel plot analysis (Figure 3) did not indicate substantial bias in nurse personal/professional characteristic assessment, though Egger’s test suggested funnel plot asymmetry (intercept: −9.03, 95% CI: −9.58 to −8.48, t: −32.22, p-value: 0.052, Egger’s test).
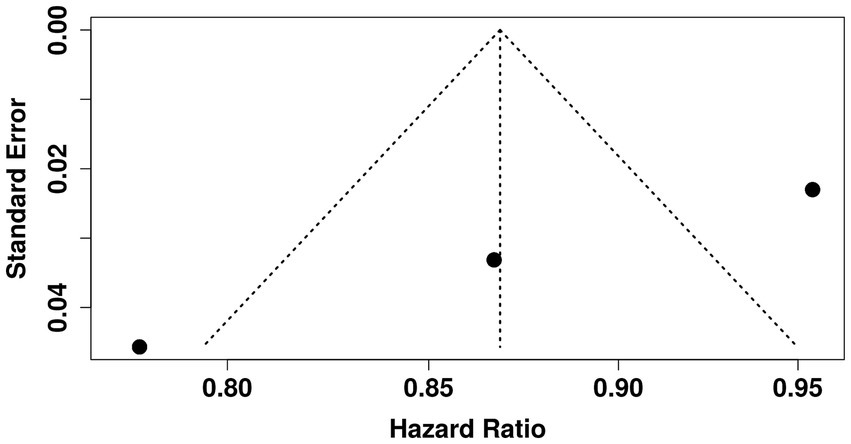
Figure 3. Funnel plot shows the association between personal and professional characteristics and perceptions of cultural and spiritual care competencies.
Assumption testing
Details regarding the assumption tests conducted in this study, inclusive of justifications for the choice of the conclusive tests, are shown in Table 8.
Discussion
All nurses are ethnically Han Chinese, female, and profess no religious affiliation. The gender demographics in this study align with the China Health Statistical Yearbook data from 2002 to 2020 (16), reflecting the higher proportion of women in Chinese healthcare. While China’s predominant ethnicity is Han Chinese (17), the ruling party maintains a secular stance (18). Consequently, nurses caring for urology patients in China are typically female, of Han Chinese ethnicity, and non-religious.
The spiritual care competency scale across all factors registered a mean score of 4 or higher per nurse (indicating mild agreement), while the cultural competence scale yielded a mean score of 4.24 ± 0.79 per nurse (surpassing mild agreement). These findings regarding spiritual care competency align with previous research, including a cross-sectional study (4.92 for acute care nurses’ spiritual care competency) (2), an integrative research review (moderate level for clinical nurses’ spiritual care competency) (4), a multicenter cross-sectional study (> 4 for clinical nurses’ spiritual care competency) (8), and a cross-sectional survey (moderate level for clinical nurses’ spiritual care competency) (7). In essence, nurses in Chinese urology departments exhibit a favorable disposition toward cultural and spiritual care competencies, which should be leveraged to cultivate stronger nurse–patient rapport.
Advanced age (≥ 35 years) and a self-perceived spiritual inclination, while not directly correlated with perceived cultural and spiritual care competence, emerge as salient variables in univariate analyses. These findings regarding the association between perceived cultural and spiritual care competence align with those of a prior cross-sectional study (7). Spiritual care transcends specific religious (e.g., Buddhist) or regional practices (1), demanding experiential knowledge and specialized expertise (1, 19). Spiritual care prioritizes an individual’s core beliefs and meaning-making, whereas cultural care honors their traditions, values, and customs (20). The personal and professional attributes of nurses in urology are generally independent of perceived cultural and spiritual care competencies, as such care constitutes a fundamental dimension of human existence (1).
The research, while termed a cross-sectional survey, incorporates a mere 35 nurses from a solitary medical facility. This markedly diminutive, homogenous, and unrepresentative cohort—comprising solely Han Chinese women, devoid of religious affiliations—substantially curtails the capacity for broad extrapolation. Given the extensive diversity among urology nurses nationwide, exemplified by our affiliation with Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China, a sample of 35 cannot be deemed reflective of the Chinese nursing population at large. Acknowledging this limitation, the interpretation confines itself to the cohort under scrutiny, refraining from generalizations applicable to all nurses in China. Furthermore, an excessively large sample size may introduce unwarranted complexity and financial burdens, thereby rendering the study impracticable. Such circumstances constitute ethically untenable scenarios and warrant avoidance (21).
The mean scores for spiritual care and personal values registered below 4 (mild agreement), attributable to nurses’ misinterpretations of spiritual care or its conflation with religious perspectives (2). Conversely, spiritual perspective values exhibited higher mean scores across all factors, a finding resonant with the prevalence of Buddhism (with its pronounced emphasis on suffering rooted in desire) and Taoism (which emphasize the individual’s harmonious integration with nature through mystical insight, intuition, and acceptance of natural processes) in China (22). Moreover, spiritual care values also averaged below 4 (mild agreement), owing to nurses’ workload and insufficient knowledge of spiritual care practices (2). Consequently, authorities should prioritize addressing nurses’ perceptions of cultural and spiritual care competencies and implementing specialized training programs for urology nurses in these critical domains.
Following multivariate (logistic regression) analyses, univariate analyses were performed to ascertain the relationship between the individual and occupational characteristics of nurses caring for urology patients and their adjudged cultural and spiritual care aptitudes. For this study, forest and funnel plots using a random-effects model with the inverse variance method were preferred. Employing the univariate analysis as a predictive ‘filter’ within a multivariable model is erroneous (23). The employment of both univariate and multivariable regression requires justification, given their potential to yield contradictory outcomes (23). Furthermore, concurrent model usage cannot be considered a validation ‘instrument’; a singular approach is thus advisable. Therefore, this study exclusively utilized forest and funnel plots, leveraging a random-effects model with the inverse variance method, to examine the association between nurses’ personal and professional attributes and their perceived cultural and spiritual care expertise in urology patient management.
Limitations
Despite the study’s commendable focus on an under-researched demographic (urology nurses in China), utilization of validated instruments for spiritual and cultural care competency assessment, provision of granular factor-level data conducive to targeted training initiatives, and adherence to rigorous ethical approval and informed consent protocols, several limitations warrant consideration. The modest sample size elevates the risk of Type I error, and the study’s reliance on subjective methodologies, without an objective mixed-methods design (1), introduces potential bias from social desirability responses (2). Beyond age and educational attainment, other examined variables demonstrated negligible influence on the perceptions of cultural and spiritual care competencies. The sample’s homogeneity restricts the generalizability of findings beyond the immediate study context, and the conclusions drawn should be regarded as preliminary.
Conclusion
Urology nurses demonstrated a salutary outlook on cultural and spiritual care proficiencies. Personal and professional attributes of urology nurses are generally dissociated from perceptions of cultural and spiritual care competence. Authorities should prioritize nurses’ perceptions regarding cultural and spiritual care aptitude and the provision of specialized training in these domains. This study addresses a hitherto underexplored subject: cultural and spiritual care competence among urology nurses in China.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The designed protocols of the cross-sectional study were prepared by the authors themselves. These protocols were approved by the human ethics committee of the Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences. The approval number of the human ethics committee is 2024-024, approved dated December 5, 2024. The study follows the law of China and the v2008 Declaration of Helsinki (the latest Chinese version). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
WZ: Resources, Validation, Writing – original draft, Methodology, Supervision, Writing – review & editing, Conceptualization. YW: Writing – original draft, Investigation, Visualization, Resources, Conceptualization, Writing – review & editing, Methodology. MG: Writing – original draft, Conceptualization, Visualization, Resources, Methodology, Writing – review & editing. LZ: Software, Writing – review & editing, Resources, Writing – original draft, Supervision, Methodology. QY: Formal analysis, Methodology, Writing – review & editing, Writing – original draft, Conceptualization, Resources, Visualization. DR: Writing – original draft, Software, Data curation, Methodology, Resources, Conceptualization, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Jiading District Key Medical Discipline (NO. XK202404).
Acknowledgments
The authors are thankful to the medical and non-medical staff of the Jiading District Central Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SD, standard deviations; Q3, third quartile value; Q1, first quartile value; ꭓ2 test, chi-square test; CI, confidence interval.
Footnotes
References
1. Hvidt, NC, Nielsen, KT, Kørup, AK, Prinds, C, Hansen, DG, Viftrup, DT, et al. What is spiritual care? Professional perspectives on the concept of spiritual care identified through group concept mapping. BMJ Open. (2020) 10:e042142–10. doi: 10.1136/bmjopen-2020-042142
2. Chew, BW, Tiew, LH, and Creedy, DK. Acute care nurses' perceptions of spirituality and spiritual care: an exploratory study in Singapore. J Clin Nurs. (2016) 25:2520–7. doi: 10.1111/jocn.13290
3. Nissen, RD, Viftrup, DT, and Hvidt, NC. The process of spiritual care. Front Psychol. (2021) 12:1–11. doi: 10.3389/fpsyg.2021.674453
4. Counted, V, Possamai, A, and Meade, T. Relational spirituality and quality of life 2007 to 2017: an integrative research review. Health Qual Life Outcomes. (2018) 16:1–18. doi: 10.1186/s12955-018-0895-x
5. Wang, Z, Tang, X, Li, L, Zhou, H, Zhu, Y, Chen, L, et al. Spiritual care needs and their attributes among Chinese inpatients with advanced breast cancer based on the Kano model: a descriptive cross-sectional study. BMC Palliat Care. (2024) 23:50–12. doi: 10.1186/s12904-024-01377-8
6. Ferrell, BR, Twaddle, ML, Melnick, A, and Meier, DE. National consensus project clinical practice guidelines for quality palliative care guidelines, 4th edition. J Palliat Med. (2018) 21:1684–9. doi: 10.1089/jpm.2018.0431
7. Wang, R, Wu, YY, Duan, GX, Liang, C, Tan, L, Pu, Y, et al. Critical cultural competence of clinical nurses in China: a cross-sectional survey. J Nurs Manag. (2022) 30:1042–52. doi: 10.1111/jonm.13590
8. Guo, W, Liu, X, Zhang, Y, Chen, R, Qi, W, Deng, J, et al. Competence and perceptions of spiritual care among clinical nurses: a multicentre cross-sectional study. J Clin Nurs. (2024) 33:1432–43. doi: 10.1111/jocn.16932
9. Cheng, SL, Yusuf, A, He, YY, Tang, WZ, and Sulaiman, NABS. Spiritual needs and influencing factors of postoperative breast cancer women undergoing chemotherapy: a cross-sectional study. Risk Manag Healthc Policy. (2024) 17:843–53. doi: 10.2147/RMHP.S453184
10. Özveren, H, Karabey, T, and Gülnar, E. Spiritual care needs of patients with urinary incontinence and affecting factors: a cross-sectional descriptive study in Turkey. J Relig Health. (2022) 61:4433–49. doi: 10.1007/s10943-022-01613-6
11. Campain, N, Mabedi, C, Savopoulos, V, Payne, SR, and MacDonagh, R. Understanding cultural and logistical contexts for urologists in low-income countries. BJU Int. (2022) 129:273–9. doi: 10.1111/bju.15690
12. Murgia, C, Notarnicola, I, Caruso, R, De Maria, M, Rocco, G, and Stievano, A. Spirituality and religious diversity in nursing: a scoping review. Healthcare. (2022) 10:1–22. doi: 10.3390/healthcare10091661
13. May, JO, and Looney, SW. Sample size charts for spearman and Kendall coefficients. J Biom Biostat. (2020) 11:1–7. doi: 10.37421/jbmbs.2020.11.440
14. Hu, Y, Tiew, LH, and Li, F. Psychometric properties of the Chinese version of the spiritual care-giving scale (C-SCGS) in nursing practice. BMC Med Res Methodol. (2019) 19:21–13. doi: 10.1186/s12874-019-0662-7
15. Lin, MH, Chang, TH, Lee, YH, Wang, PY, Lin, LH, and Hsu, HC. Developing and validating the nursing cultural competence scale in Taiwan. PLoS One. (2019) 14. doi: 10.1371/journal.pone.0220944
16. Li, M, Raven, J, and Liu, X. Feminization of the health workforce in China: exploring gendered composition from 2002 to 2020. Hum Resour Health. (2024) 22:15–1. doi: 10.1186/s12960-024-00898-w
17. Kong, W, Xiao, Y, Wang, B, Zhu, Z, Hu, L, Tang, H, et al. Comorbidities of scars in China: a national study based on hospitalized cases. Burns Trauma. (2021) 9:1–8. doi: 10.1093/burnst/tkab012
18. Murgia, C, Notarnicola, I, Rocco, G, and Stievano, A. Spirituality in nursing: a concept analysis. Nurs Ethics. (2020) 27:1327–43. doi: 10.1177/0969733020909534
19. Paal, P. Cultural safety and spiritual care In: MC Best, editor. Spiritual Care in Palliative Care. Cham: Springer (2024):415–422.
20. Martínez-Mesa, J, González-Chica, DA, Bastos, JL, Bonamigo, RR, and Duquia, RP. Sample size: how many participants do I need in my research? An Bras Dermatol. (2014) 89:609–15. doi: 10.1590/abd1806-4841.20143705
21. Ryff, CD. Spirituality and well-being: theory, science, and the nature connection. Religion. (2021) 12:1–19. doi: 10.3390/rel12110914
22. Wang, H, Peng, J, Wang, B, Lu, X, Zheng, JZ, Wang, K, et al. Inconsistency between univariate and multiple logistic regressions. Shanghai Arch Psychiatry. (2017) 29:124–8. doi: 10.11919/j.issn.1002-0829.217031
Keywords: cultural care competencies, nurses, professional characteristics, spiritual care competencies, urology
Citation: Zhu W, Wang Y, Gu M, Zheng L, Yan Q and Ren D (2025) Cultural and spiritual acumen in Chinese urology nursing: a quantitative and qualitative pilot investigation. Front. Med. 12:1666924. doi: 10.3389/fmed.2025.1666924
Edited by:
Maha Atout, Philadelphia University, JordanReviewed by:
Annemiek Schep-Akkerman, Dutch College of General Practitioners, NetherlandsFatemeh Estebsari, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2025 Zhu, Wang, Gu, Zheng, Yan and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongmei Ren, MTg1MTYwMTA2MTFAMTYzLmNvbQ==; cmVuZG9uZ21laTI2QGdtYWlsLmNvbQ==
†ORCID: Wenting Zhu, orcid.org/0009-0003-9523-5389
Yilin Wang, orcid.org/0009-0009-6830-0302
Minjia Gu, orcid.org/0009-0002-6024-2418
Liqing Zheng, orcid.org/0009-0009-6340-4794
Qin Yan, orcid.org/0009-0007-1118-3657
Dongmei Ren, orcid.org/0009-0005-2405-7807
 Wenting Zhu1†
Wenting Zhu1† Dongmei Ren
Dongmei Ren