Abstract
Objective:
This randomized pilot study assessed the feasibility and acceptability of a remote yoga intervention and examined potential effects on pain, sleep and the psychological variables anxiety and depression.
Method:
The intervention for the experimental group consisted of Hatha Yoga sessions, guided by video, lasting 60 min, divided into three moments: stillness and awareness of breathing, practice of postures (asanas), and meditation. Participants randomized to the intervention group participated in guided group video practice sessions for 2 weeks in the community church hall. Participants randomized to the control group were instructed to maintain their normal daily routine. The feasibility measures evaluated were: acceptance rates, ability to complete the intervention, external interference from other physical activities, and adverse effects. Outcome measures (self-reported pain, anxiety, depression, and sleep quality) were assessed at baseline and post-intervention. The Wilcoxon test was used to analyze the differences between groups, and the Mann–Whitney U test to compare the control group and the different moments of the intervention group. The effect size was assessed using Cohen’s d.
Results:
In the comparisons between the groups, there were no significant differences in any of the outcomes. The group that performed the intervention presented a significant reduction in anxiety. In addition, improvements were observed in the intervention group in pain, depression, and sleep quality according to the mean values, with a small to moderate effect size. Regarding the feasibility measures, the study had excellent acceptance rates; all participants completed the intervention. There was no external interference from other physical activities of the groups, and no serious adverse effects were reported.
Conclusion:
The asynchronous Hatha Yoga intervention was feasible, well accepted, and safe to be applied remotely in a group of women with chronic pain, living in a rural community. Despite the short duration of the Hatha Yoga intervention, the data presented suggest that improvements in anxiety, pain, depression, and sleep quality were observed in women with chronic pain. Large-scale randomized controlled trials are suggested to evaluate the effects of this modality on pain-related and psychological outcomes.
1 Introduction
Chronic pain is defined as pain persisting for more than 3 months and is often associated with functional disability and emotional distress (1). This condition is highly prevalent among older adults (2, 3), negatively affecting the quality of life, mental health, and functional capacity of this population (4, 5). Evidence suggests that women are more likely than men to experience chronic pain, reporting greater intensities, frequencies, and durations of pain and depression (6).
Diotaiuti et al. (7) highlighted that attentional focus and cognitive orientation can significantly modulate the perception of pain, providing theoretical support for mind–body practices, such as yoga, in managing chronic pain.
In this sense, mind–body interventions, have been included as part of the therapeutic approach to chronic pain (8), combining physical postures (asana), breathing techniques (pranayama), and meditation (dyana) to promote physical and mental wellbeing (9). Focusing on deep controlled breathing, attention to physical comfort, redirecting attention, mindful practice, relaxation, and slow, gentle movements can produce better awareness of afferent (sensory) feedback, allowing for a more effective response to efferent (motor) commands, reducing muscle tension and spasms associated with pain (10).
Systematic reviews (11–13), have shown the effects of yoga in reducing pain and disability in people with chronic musculoskeletal pain. However, these studies did not explore the impact of this intervention modality on psychological outcomes and/or sleep disorders in this population. Studies carried out with healthy older people point out that yoga interventions improve outcomes such as depression, mental health, vitality, sleep quality, and quality of life (14). Yoga seems to promote healthy psychological responses, indicating its potential as a strategy for emotion regulation.
In most clinical studies, yoga sessions are led in person by an instructor (15). However, access to this intervention format can be a major barrier for residents of rural areas, due to the unavailability of yoga instructors and the difficulties of transportation and travel to large centers, making participation difficult, with large associated costs and time demands (15, 16). Although other remote forms of applying yoga interventions (videos, apps, video conferencing) have been developed and used (17, 18), few studies have investigated how remote Hatha Yoga interventions can be applied in practical real-world situations. Thus, the purpose of this pilot study was to evaluate the feasibility and acceptance of a remote Hatha Yoga intervention (asynchronous videos) and to examine the potential effects on chronic musculoskeletal pain, sleep, and psychological variables (anxiety and depression) of women with chronic pain.
2 Method
2.1 Design
This is a 2-week feasibility, and controlled pilot study comparing Hatha Yoga with a control group. The study included a sample of women, living in a rural area in southern Brazil, with complaints of chronic musculoskeletal pain. The study was carried out within the ethical standards of the Declaration of Helsinki and following Resolution 196/96 of the Ministry of Health.
2.2 Participants
The participants were recruited from a rural region in the city of Itajaí between November and December 2022. The eligibility criteria were: women, over 18 years of age, who had been complaining of musculoskeletal pain for more than 3 months. Women who had practiced yoga in the previous year, or with cognitive or functional limitations that prevented the practice of group physical activity (to minimize the risks of performing an unsupervised exercise intervention) were excluded. Women who had limitations to stand up or lie on the floor (transition required between Hatha Yoga postures) were also excluded.
The recruitment method for the composition of the intervention group and control group included dissemination in the neighborhood community group and messaging groups through mobile applications. Participants who showed interest in participating were invited to an interview in the neighborhood church hall, and those eligible for the study were asked to sign the consent form. Group allocation was determined by a simple random draw.
2.3 Intervention and control
The intervention group participated in video-guided Hatha Yoga sessions (60 min), applied 2 times a week for 2 weeks, in a location provided by the community church. The sessions were accompanied by a physical education professional who started the video and offered instructions, when necessary. The video intervention was specifically adapted to meet the needs of the target population by a certified yoga instructor and included three moments: (1) Stillness and Awareness of Breathing (Pranas and Dayana’s), (2) Practices of the Asana Postures (postures) in the sitting, supine, and standing positions, and (3) and meditation (main postures are illustrated in Figure 1). The sessions were developed to occur fluidly from the beginning, with small transition intervals between postures, facilitating the development of Pratyahara (abstraction of the senses) and command and synchronization of movements with breathing (Table 1 Hatha Yoga Intervention Protocol via video). In addition, rest postures were added, which as well as physical rest, allow moments of recollection and observation of the body and breathing. The video contains instructions on posture variations and the use of a yoga mat, blocks, blankets, and a chair, when necessary, according to the physical limitations of the participants.
Figure 1

Postures (asanas) used in the Hatha Yoga protocol.
Table 1
| Division and time in minutes of realization | Practice description |
|---|---|
| Philosophy from Hatha Yoga (5 min) | Explanations of the importance of the practice and reflections on the philosophy of Hatha Yoga. |
| Quieting and awareness of the breath (10 min) | Performing breathing exercises (pranas); and Dhyana meditation (meditation) in the positions: Sukusana and lying supine with the knees semi-flexed. |
| Postures psychophysical (25 min) | Performing ten psychophysical postures (asanas) in the sitting, supine, and standing positions as a way of cultivating the body and mind. The postures worked were: Baddha Konasana, Dandasana, Marjaryasana, Balasana, Tadasana, Chakoravakasana, Uttanasana, Utkatasana and Navasana (Figure 1). Participants were encouraged to stretch as much as possible without exceeding the limits of their comfort. Repetition was consistent week after week and linked pose to pose. Each posture was held for approximately 20 to 30 s, with rest periods lasting 30 s to 1 min between postures. Mats were used to perform the positions. Chairs for. The instruction was to concentrate on breathing and try to relax. |
| Meditation | Execution of the meditative practice in the positions: Savasana and Sukusana. |
Hatha Yoga exercise program intervention protocol (video).
The control group participants did not receive any type of intervention and were instructed not to start Hatha Yoga classes or exercise programs during the 2 weeks.
2.4 Procedures
The stages of data collection are described in Figure 2. The outcomes evaluated before and after the intervention were: Pain Intensity, Depression, Anxiety, and Sleep Quality. Feasibility measures were also evaluated: adverse effects/safety, acceptability, ability to complete the intervention, and external interference from other physical activities.
Figure 2
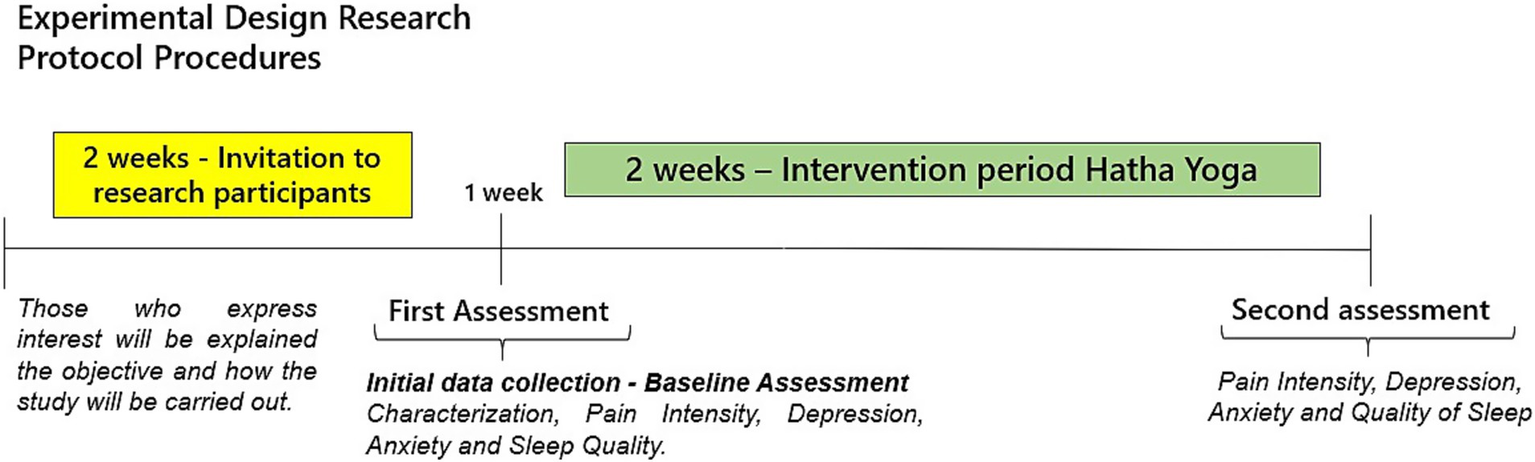
Data collection procedures and steps.
2.4.1 Viability
Safety was assessed through records of adverse events during and outside of yoga classes. Unexpected injuries (falls, fractures, sprains, muscle tension, and/or joint pain) were considered adverse effects. These events were monitored and recorded by the physical education professional who accompanied the sessions.
Acceptability was assessed using a form with questions related to participant satisfaction, that was applied at the end of the intervention. The form consisted of two questions: (1) How do you evaluate the yoga classes? (bad, fair, good, very good, great), and (2) Would you consider continuing to practice yoga? (yes or no).
The ability to complete the intervention was characterized by the ability to perform the postures and movements during the Hatha Yoga intervention and by the need to adapt or modify postures. These aspects were monitored and recorded by the professional present at the sessions.
Contamination was assessed through participants’ reports related to beginning of other exercises during the intervention.
2.4.2 Outcomes
Pain intensity—assessed using the Numerical Pain Scale (NPS), a simple scale often utilized to assess variations in subjective pain intensity (19). The scale ranges from 0 to 10, where 0 represents “no pain” and 10 represents “extreme pain.” Participants were asked to state their pain level on the scale at the time of each assessment (before and after the intervention).
Sleep quality—assessed using the Pittsburgh Sleep Quality Index (PSQI), a self-report instrument developed by Buysse et al. (20), which assesses sleep quality in the previous month. Our study used a short version of the PSQI that was adapted and validated for Brazil (21). This version assesses sleep quality over the previous 7 days; it consists of 9 questions that assess duration, subjective quality, efficiency, disorders, medication, daytime dysfunctions, latency, and total sleep quality. The PSQI score ranges from 0 to 21; the higher the score, the worse the sleep quality. A score > 5 indicates difficulty in at least two domains.
Depression and anxiety—the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were used to assess depression and anxiety levels. Higher scores indicate higher levels of depression and anxiety. Each questionnaire consists of 21 questions, with each question scored from 0 to 3. The BDI scale was validated in Portuguese for Brazil by Gorenstein (22), with a score < 10 being classified as minimal or no depression, 10–18 as mild to moderate depression, 19–29 as moderate to severe depression, and 30–63 as severe depression. A BAI score of 0–21 indicates very low anxiety, 22–35 moderate anxiety, and 36 or more high anxiety.
2.5 Statistical analysis
For descriptive analysis, mean, standard deviation, and percentage were calculated. For inferential statistics, normality analysis was first performed with the Shapiro–Wilk test. To analyze the differences between groups, the Wilcoxon test was used, and the Mann–Whitney U test was used to compare the control group and the different moments of the intervention group. The α established as the significance level was p < 0.05 (95%). The data were statistically treated with the Statistical Package for Social Science 20.0® (IBM, USA). The Cohen’s d effect size was also calculated; a value of d = 0.2 was indicative of a small effect, d = 0.5 a medium effect, and d = 0.8 a large effect (23).
3 Results
3.1 Characteristics of the participants
Thirteen women participated in the study, distributed into an intervention group (n = 8) and a control group (n = 5). The sociodemographic and clinical characteristics at baseline are described in Table 2. The age of the participants ranged from 47 to 77 years (62.9 ± 9.3). The participants were predominantly retired (69.2%), with low education (only 2 participants completed high school), and with a family income of less than or equal to 5 minimum wages. The most commonly reported primary sites of pain by the participants were the lower limbs and spine. Mean pain intensity ranged from 1 to 9, with a mean score of 5.2 (± 2.8). Participants in the Hatha Yoga group tended to have lower mean pain scores than those in the control group. Approximately 50% of the intervention group participants were physical activity practitioners, while none of the women in the control group performed physical activity.
Table 2
| Variable | Control (n = 5) | Intervention (n = 8) |
|---|---|---|
| Age | 63.4 ± 8.9 | 62.6 ± 10.7 |
| Marital status | ||
| Single | 0 (0.0%) | 1 (12.5%) |
| Married woman | 4 (80.0%) | 5 (62.5%) |
| Widow | 1 (20.0%) | 2 (25.0%) |
| Professional status | ||
| Active | 1 (20.0%) | 3 (37.5%) |
| Retired | 4 (80.0%) | 5 (62.5%) |
| Schooling | ||
| Incomplete elementary education | 2 (40.0%) | 6 (75.0%) |
| Complete elementary education | 2 (40.0%) | 1 (12.5%) |
| Middle school | 1 (20.0%) | 1 (12.5%) |
| Family income (MW) | ||
| 1–2 | 3 (60.0%) | 4 (50.0%) |
| 3–5 | 2 (40.0%) | 4 (50.0%) |
| Pain intensity | 4.0 ± 03.0 | 5.9 ± 02.6 |
| Pain site | ||
| Column | 4 (80.0%) | 4 (50.0%) |
| Lower limbs | 1 (20.0%) | 3 (37.5%) |
| Upper limbs | 0 (0.0%) | 1 (12.5%) |
| BMI | ||
| Normal | 2 (40.0%) | 3 (37.5%) |
| Overweight | 2 (40.0%) | 4 (50.0%) |
| Obesity | 1 (20.0%) | 1 (12.5%) |
| Practice of activity physics | ||
| No | 5 (100%) | 4 (50.0%) |
| Yes | 0 (0.0%) | 4 (50.0%) |
Sociodemographic and clinical characteristics of 13 women with pain complaints who participated as intervention group during 2 weeks of the remote Yoga intervention and 2 weeks in the control group.
Family income was categorized between those who received 1–2 minimum wages (MW) and those who received 3–5 MW; BMI, Body Mass Index.
3.2 Feasibility
3.2.1 Recruitment
A total of 26 women were selected for eligibility, and 13 were deemed eligible for participation. The reasons for ineligibility were: no complaints of pain at the time of the study (03), presented functional limitations (01), and were not available to participate in the study (02). The 16 women considered eligible for participation were divided into two groups: 11 in the intervention group and five in the control group. After the 2 weeks of intervention, there were eight participants in the IG and five in the control group. The reasons for discontinuation in the study were: family commitments (02) and health problems, influenza (01) (Figure 3).
Figure 3
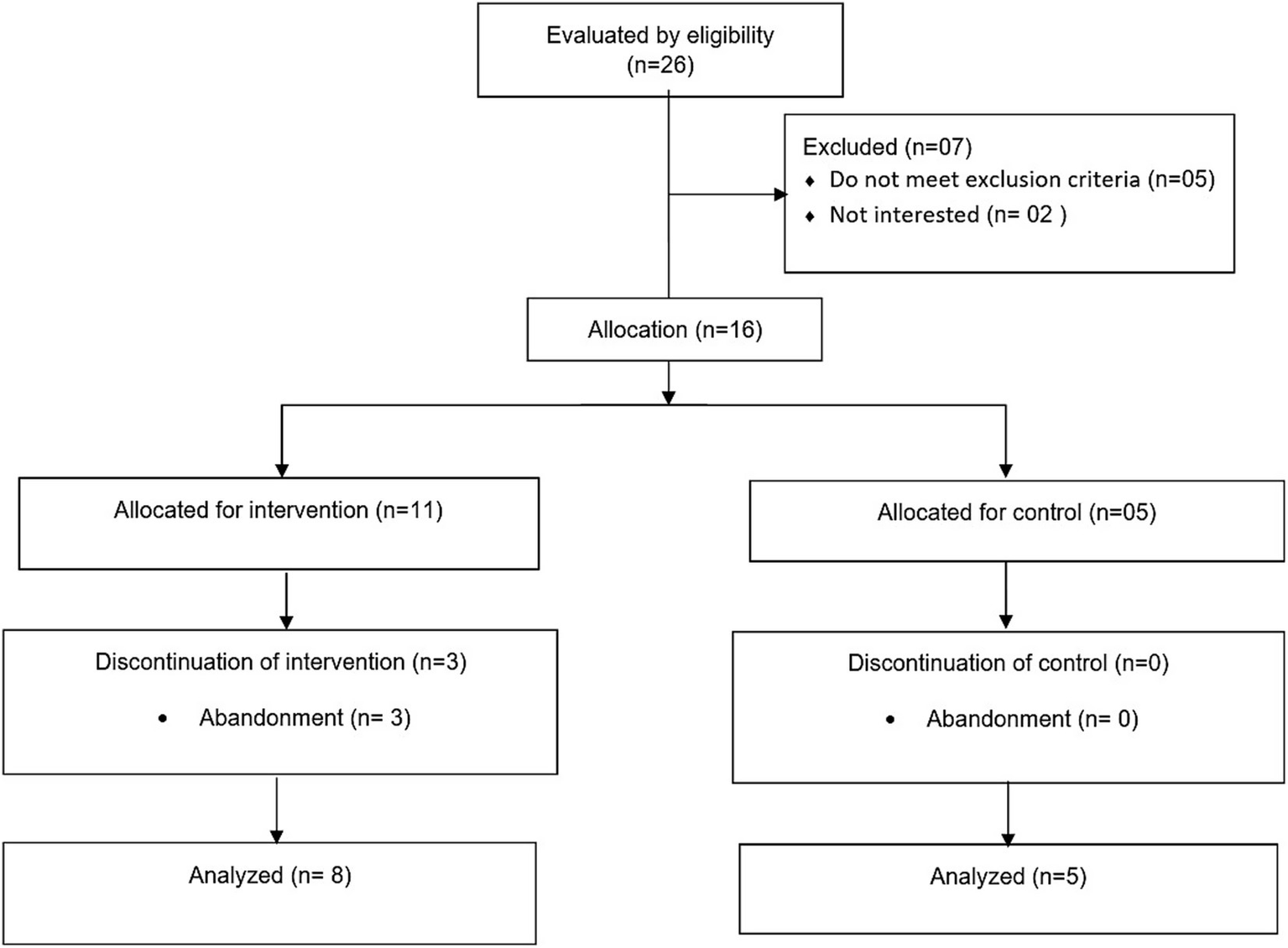
Inclusion–exclusion flowchart of the 26 study participants for eligibility.
3.2.2 Adverse effects
During the intervention period, only non-serious adverse events (muscle or joint pain) were reported. One participant reported pain in performing the “Adho Mukha Syanasana” posture (Dow Dog Pose) and another reported pain in maintaining the “Dandayamana Bharmasana” (Balance Table Pose) posture, as she had reduced flexibility due to retractions resulting from burn scars.
3.2.3 Acceptability
All participants were satisfied with the intervention (25% very good/75% excellent) and would recommend the program to other women (100%).
3.2.4 Ability to complete the intervention
All participants were able to complete the postures and movements presented in the video. The video used for the session suggested alternative postures or adaptations to the postures presented. Two participants asked for verbal guidance to perform the “Dandayamana Bharmasana” (Balance Table Pose). No changes to the intervention protocols were necessary after the study began, the participants were able to perform as initially proposed.
3.2.5 Contamination
No participants in either group performed any other physical activity or exercise program during the study period (2 weeks).
3.3 Outcomes
In the intragroup comparison, there was a significant improvement in the anxiety status of the intervention group, when comparing pre and post-test, with a p-value of less than 0.01 (and an intervention effect size of moderate to large). Although pain intensity did not present significant differences, there was a 1.5 reduction in mean values (moderate effect size). There were no significant differences in the sleep quality of the two groups after 2 weeks of Yoga (post-test) (Table 3). On the other hand, based on the results of the mean values and the effect size presented, there was an improvement in the overall sleep quality on the PSQI and the intervention group depression.
Table 3
| Variables | Intervention (n = 08) | Cohen’s d | Control (n = 05) | ||||
|---|---|---|---|---|---|---|---|
| Pre X ± (dp) |
Post X ± (dp) |
p-value | Pre X ± (dp) |
Post X ± (dp) |
p-value | ||
| Pain intensity (END) | 5.87 ± 2.58 | 4.37 ± 2.77 | 0.10 | 0.50** | 4.00 ± 3.00 | 5.80 ± 1.78 | 0.102 |
| Anxiety | 8.12 ± 6.26 | 4.12 ± 4.58 | 0.01* | 0.67** | 7.60 ± 9.91 | 5.60 ± 9.78 | 0.04* |
| Depression | 3.25 ± 2.49 | 4.12 ± 4.15 | 0.43 | 0.26 *** | 4.80 ± 7.46 | 4.80 ± 6.61 | 1.00 |
| Sleep—PSQI | |||||||
| Subjective quality | 1.12 ± 0.64 | 1.00 ± 0.92 | 0.65 | 0,15 | 1.20 ± 1.09 | 1.00 ± 1.24 | 0.31 |
| Latence | 0.87 ± 0.64 | 1.37 ± 0.91 | 0.19 | 0.42 *** | 1.20 ± 1.30 | 1.20 ± 1.30 | 1.00 |
| Duration | 0.87 ± 1.24 | 0.50 ± 1.06 | 0.18 | 0.43 *** | 0.60 ± 1.34 | 0.60 ± 1.34 | 1.00 |
| Efficiency | 1.25 ± 1.28 | 0.75 ± 1.16 | 0.19 | 0.42 *** | 0.60 ± 1.34 | 0.60 ± 1.34 | 1.00 |
| Disturbance | 0.87 ± 0.64 | 1.12 ± 0.35 | 0.31 | 0.33 *** | 1.40 ± 0.89 | 1.40 ± 0.89 | 1.00 |
| Medication | 0.75 ± 1.38 | 0.37 ± 1.06 | 0.31 | 0.33 *** | 0.60 ± 1.34 | 0.00 ± 0.00 | 0.31 |
| Dysfunction | 0.50 ± 0.75 | 0.37 ± 0.74 | 0.31 | 0.33 *** | 0.40 ± 0.89 | 0.40 ± 0.89 | 1.00 |
| PSQI total score | 6.25 ± 4.92 | 5.12 ± 4.70 | 0.68 | 0.14 | 5.80 ± 7.98 | 5.20 ± 6.64 | 0.31 |
Effects of two-week yoga intervention on pain, anxiety, depression, and sleep.
*Significant difference p < 0.05; Wilcoxon test was used; X, average; (SD), standard deviation; **Effect size ≥ 0.50 is considered a good effect size. ***Effect size ≥ 0.20 is considered a small effect size. The significant differences and observed effect sizes are highlighted in bold.
In the intergroup comparison (intervention group and control group) at the post-test moment, there were no significant differences in the variables investigated (Table 4).
Table 4
| Variable | Pre-intervention | Pre control | p | Post intervention | Post control | p |
|---|---|---|---|---|---|---|
| Pain intensity (END) | 5.87 ± 2.58 | 4.00 ± 3.00 | 0.23 | 4.37 ± 2.77 | 5.80 ± 1.78 | 0.54 |
| Anxiety | 8.12 ± 6.26 | 7.60 ± 9.91 | 0.55 | 4.12 ± 4.58 | 5.60 ± 9.78 | 0.71 |
| Depression | 3.25 ± 2.49 | 4.80 ± 7.46 | 0.65 | 4.12 ± 4.15 | 4.80 ± 6.61 | 0.82 |
| Sleep—PSQI | ||||||
| Subjective quality | 1.12 ± 0.64 | 1.20 ± 1.09 | 0.86 | 1.00 ± 0.92 | 1.00 ± 1.24 | 0.80 |
| Latence | 0.87 ± 0.64 | 1.20 ± 1.30 | 0.75 | 1.37 ± 0.91 | 1.20 ± 1.30 | 0.70 |
| Duration | 0.87 ± 1.24 | 0.60 ± 1.34 | 0.65 | 0.50 ± 1.06 | 0.60 ± 1.34 | 0.92 |
| Efficiency | 1.25 ± 1.28 | 0.60 ± 1.34 | 0.26 | 0.75 ± 1.16 | 0.60 ± 1.34 | 0.65 |
| Disturbance | 0.87 ± 0.64 | 1.40 ± 0.89 | 0.28 | 1.12 ± 0.35 | 1.40 ± 0.89 | 0.64 |
| Medication | 0.75 ± 1.38 | 0.60 ± 1.34 | 0.84 | 0.37 ± 1.06 | 0.00 ± 0.00 | 0.43 |
| Dysfunction | 0.50 ± 0.75 | 0.40 ± 0.89 | 0.65 | 0.37 ± 0.74 | 0.40 ± 0.89 | 0.92 |
| PSQI total score | 6.25 ± 4.92 | 5.80 ± 7.98 | 0.40 | 5.12 ± 4.70 | 5.20 ± 6.64 | 0.40 |
Comparisons between the intervention and control groups.
*Significant difference p < 0.05; The Mann–Whitney U test was used.
Figure 4 presents the main results found and expectations for studies and recommendations.
Figure 4
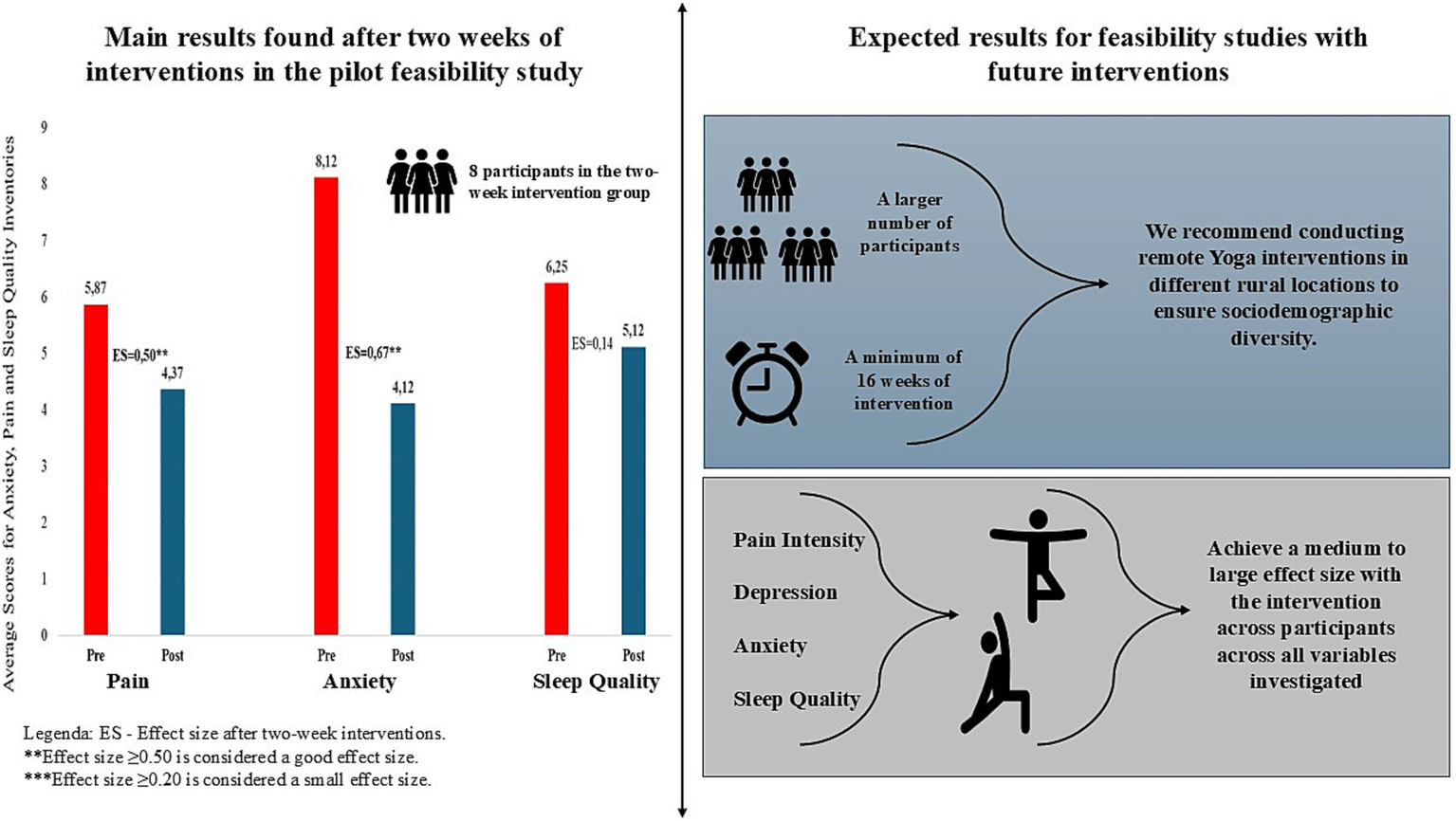
Main results found and expectations for future studies.
4 Discussion
Chronic pain affects the health and quality of life of older women, limiting their work activities and interfering with social relationships. Several non-pharmacological interventions can contribute to the control of pain and other related symptoms, however, they can be difficult to access for residents of rural areas, as these programs are usually offered in large centers or reference health services. A nationwide systematic review showed that the southern region of Brazil is the most affected by chronic pain in the country (24). Considering the impacts on public health arising from the needs of patients affected by a multitude of diseases, patients being taken to integrated health centers and hospitals due to chronic pain can further inflate the demands on care systems. Thus, studies such as the present feasibility study are needed in more remote locations, such as rural and hard-to-reach areas, as a way to study and mitigate the impacts of pain in various populations that need care.
Over 3 weeks, 16 women were recruited to the study. The research was disseminated by representatives of the community groups, which may have facilitated recruitment, as most of the women already knew each other or had familial ties. The proposal for a Hatha Yoga activity was well received and at the end of the intervention, all participants were satisfied and stated that they would recommend it to other women in the community with chronic musculoskeletal pain. This result indicates the feasibility of carrying out a clinical study using the proposed protocol with a larger number of participants.
No serious adverse events were recorded. As expected, some participants reported pain during some postures and/or the need for adaptations. However, none of the participants failed to carry out the proposed activities. The instructions in the video and the supervision of a trained physical education professional (not specialized in yoga) likely enhanced participants’ confidence and their safety perception. During the 2 weeks of intervention, there was no external interference from other physical activities (none of the participants started another type of exercise), making it possible to evaluate the acute effects of the modality without interference.
4.1 Outcomes
In the present study, women with musculoskeletal pain complaints showed a significant improvement in anxiety. This reduction in the BAI score was also seen in the control group, however, the women in the group that practiced Hatha Yoga for 2 weeks presented a greater reduction, with a moderate to large effect size.
There was no significant reduction in pain intensity in either group. The intervention group showed a reduction in the END score after the intervention (moderate effect size), however, of less than two points (or a reduction of approximately 30%), thus not representing a clinically important difference. There were also no significant reductions in the other outcomes, although slight improvements with a small effect size were found in the variables’ depression, latency, duration, efficiency, disorders, medications, and sleep dysfunction. A systematic review with meta-analysis revealed positive effects of yoga in women with sleep problems, using PSQI scores in 16 randomized controlled trials, compared to the control group for the improvement in sleep quality among women (25), which strengthens our results. The lack of improvement in these outcomes, in both sleep and pain, may be due to the small sample size, or point to the need for longer exposure to the intervention to produce a pain reduction and improve sleep quality. Furthermore, psychological constructs like fear of pain have been shown to play a key role in chronic pain experiences (26), supporting the relevance of evaluating cognitive-emotional factors together with physical symptoms.
Considering the current study and the literature investigating the problem, we present recommendations to treat chronic pain through evidence-based yoga interventions (Table 5).
Table 5
| Yoga interventions (27, 28) |
|
| Adaptations of interventions (28) |
|
| Artificial Intelligence in the Application of Yoga (29, 30) |
|
| Adherence to practice (28, 31) |
|
| Physical and mental benefits (4, 27, 28, 32, 33) |
|
| Public Policies (28, 31, 34) |
|
Evidence-based recommendations for yoga interventions to treat chronic pain.
4.2 Limitations and future studies
The current study did not have sufficient statistical power to detect differences between the groups and 2 weeks may have been insufficient to observe significant effects, however, the reduction in anxiety with a moderate to large effect size and the trend to improvement in the other outcomes provide support for larger-scale controlled studies and comparisons between programs of different durations. In our study, the participants had similar characteristics (low education, limited income, older age), which may limit the application of the results to other communities. Therefore, we suggest that future studies be conducted in different rural locations to ensure sociodemographic diversity; and for random group assignment, that sequence generation, allocation concealment, and group implementation be described in greater detail. The Numerical Pain Scale was used as an instrument for the pain outcome due to its ease of application in the context of the study. However, as this is a one-dimensional instrument that only measures pain intensity, it is possible that multidimensional pain instruments or those that assess the impact of pain on functionality could provide more information about the effect of the intervention on this outcome.
4.3 Strengths and applications
This study addresses a significant public health problem, chronic pain, with a focus on women in rural communities, a group often overlooked in clinical trials. Our results demonstrate that a remote intervention is possible and well-accepted in a population with limited access to resources. The use of asynchronous videos for yoga practices with supervision by health professionals (without yoga training) makes the intervention replicable in other remote regions with limited resources. The high satisfaction rate of the participants and the absence of serious adverse events are positive results. We reinforce the need for future studies with larger samples, considering different durations of intervention and with active control groups (such as relaxation or stretching interventions, to reduce the impact of the placebo effect) and participants from different rural locations, in order to assess the generalizability of the results.
5 Conclusion
An asynchronous Hatha Yoga intervention designed for people with musculoskeletal pain, even in a short period, was feasible and safe to apply to a group of women with chronic pain, residents of a rural community, who had moderate pain. Despite the short duration of the Hatha Yoga intervention, the data presented suggest that improvements in anxiety, pain, depression, and sleep quality were observed in women with chronic pain. Adverse events were mild, and the intervention was well accepted by the participants, with a high satisfaction rate.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by the Human Research Ethics Committee (CAAE 24584213.0.0000.0118) of the State University of Santa Catarina. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AA: Writing – review & editing, Supervision, Writing – original draft, Methodology, Project administration, Conceptualization. AD’O: Formal analysis, Writing – original draft, Supervision, Data curation, Writing – review & editing, Investigation, Project administration, Visualization. CS: Formal analysis, Writing – original draft, Investigation. SM: Writing – review & editing, Writing – original draft. PD: Writing – original draft, Visualization, Writing – review & editing. ML: Investigation, Conceptualization, Writing – review & editing, Supervision, Writing – original draft, Project administration, Validation, Data curation, Visualization, Methodology, Formal analysis.
Funding
The author(s) declared that financial support was received for this work and/or its publication. This work has been supported by the following Brazilian research agencies: Foundation for research and innovation support of the State of Santa Catarina—FAPESC, Research Program for the SUS: Shared Management in Health—PPSUS 16/2020; e PAP 027/2020 by the Coordination for the Improvement of Higher Education Personnel—Brazil (CAPES)—Funding Code 001, and by the National Council for Scientific and Technological Development (CNPq). Coordination for the Improvement of Higher Education Personnel—CAPES Functional Scholarship at Doctoral level—NOTICE PPGCMHN004/2024; There was also a financing contribution from of the Italian Ministry of University and Research pursuant to D.D. No. 1159 of July 23, 2023 - PROBEN Call.
Acknowledgments
The authors would like to thank CAPES (Coordination for the Improvement of Higher Education Personnel—Brazil) for supporting the doctoral scholarship during the research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Correction note
A correction has been made to this article. Details can be found at: 10.3389/fmed.2025.1760969.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Treede RD Rief W Barke A Aziz Q Bennett MI Benoliel R et al . Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. (2019) 160:19–27. doi: 10.1097/J.PAIN.0000000000001384
2.
Fayaz A Croft P Langford RM Donaldson LJ Jones GT . Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. (2016) 6:e010364. doi: 10.1136/BMJOPEN-2015-010364,
3.
Patel KV Guralnik JM Dansie EJ Turk DC . Prevalence and impact of pain among older adults in the United States: findings from the 2011 national health and aging trends study. Pain. (2013) 154:2649–57. doi: 10.1016/J.PAIN.2013.07.029,
4.
Andrade A Vilarino GT Bevilacqua GG . What is the effect of strength training on pain and sleep in patients with fibromyalgia?Am J Phys Med Rehabil. (2017) 96:889–93. doi: 10.1097/PHM.0000000000000782,
5.
Domenichiello AF Ramsden CE . The silent epidemic of chronic pain in older adults. Prog Neuro-Psychopharmacol Biol Psychiatry. (2019) 93:284–90. doi: 10.1016/J.PNPBP.2019.04.006,
6.
Zis P Daskalaki A Bountouni I Sykioti P Varrassi G Paladini A . Depression and chronic pain in the elderly: links and management challenges. Clin Interv Aging. (2017) 12:709–20. doi: 10.2147/CIA.S113576,
7.
Diotaiuti P Corrado S Mancone S Falese L Rodio A Siqueira TC et al . Influence of cognitive orientation and attentional focus on pain perception. Int J Environ Res Public Health. (2021) 18:7176. doi: 10.3390/IJERPH18137176,
8.
George SZ Fritz JM Silfies SP Schneider MJ Beneciuk JM Lentz TA et al . Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. (2021) 51:CPG1–CPG60. doi: 10.2519/JOSPT.2021.0304/ASSET/IMAGES/LARGE/JOSPT-CPG1-FIG007.JPEG
9.
Nayak NN Shankar K . Yoga: a therapeutic approach. Phys Med Rehabil Clin N Am. (2004) 15:783–98. doi: 10.1016/j.pmr.2004.04.004,
10.
Schmid AA Fruhauf CA Sharp JL Van Puymbroeck M Bair MJ Portz JD . Yoga for people with chronic pain in a community-based setting: a feasibility and pilot RCT. J Evi Bas Integra Medic. (2019) 24:2515690X19863763. doi: 10.1177/2515690X19863763,
11.
Büssing A Ostermann T Lüdtke R Michalsen A . Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. (2012) 13:1–9. doi: 10.1016/J.JPAIN.2011.10.001,
12.
Wen YR Shi J Wang YF Lin YY Hu ZY Lin YT et al . Are mind-body exercise beneficial for treating pain, function, and quality of life in middle-aged and old people with chronic pain? A systematic review and Meta-analysis. Front Aging Neurosci. (2022) 14:921069. doi: 10.3389/FNAGI.2022.921069,
13.
Wieland LS Skoetz N Pilkington K Vempati R D’Adamo CR Berman BM . Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. (2017) 2017:CD010671. doi: 10.1002/14651858.CD010671.PUB2
14.
Menezes CB Dalpiaz NR Kiesow LG Sperb W Hertzberg J Oliveira AA . Yoga and emotion regulation: a review of primary psychological outcomes and their physiological correlates. Psychol Neurosci. (2015) 8:82–101. doi: 10.1037/H0100353
15.
Brosnan P Nauphal M Tompson MC . Acceptability and feasibility of the online delivery of hatha yoga: a systematic review of the literature. Complement Ther Med. (2021) 60:102742. doi: 10.1016/J.CTIM.2021.102742,
16.
James-Palmer A Anderson EZ Daneault JF . Remote delivery of yoga interventions through technology: scoping review. J Med Internet Res. (2022) 24:e29092. doi: 10.2196/29092,
17.
da Cruz WM D’ Oliveira A Dominski FH Diotaiuti P Andrade A . Mental health of older people in social isolation: the role of physical activity at home during the COVID-19 pandemic. Sport Sci Health. (2022) 18:597–602. doi: 10.1007/S11332-021-00825-9
18.
D’Oliveira A De Souza LC Langiano E Falese L Diotaiuti P Vilarino GT et al . Home physical exercise protocol for older adults, applied remotely during the COVID-19 pandemic: protocol for randomized and controlled trial. Front Psychol. (2022) 13:182. doi: 10.3389/FPSYG.2022.828495,
19.
Hartrick CT Kovan JP Shapiro S . The numeric rating scale for clinical pain measurement: a ratio measure?Pain Pract. (2003) 3:310–6. doi: 10.1111/J.1530-7085.2003.03034.X,
20.
Buysse DJ Reynolds CF Monk TH Berman SR Kupfer DJ . The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
21.
de Araujo PAB Sties SW Wittkopf PG Netto AS Gonzáles AI Lima DP et al . Índice da qualidade do sono de pittsburgh para uso na reabilitação cardiopulmonar e metabólica. Rev Bras Med Esporte. (2015) 21:472–5. doi: 10.1590/1517-869220152106147561
22.
Gorenstein C Andrade LHS . Validation of a Portuguese version of the Beck depression inventory and state-trait anxiety inventory in Brazilian subjects. PsycNET. (1996) 29:453–7.
23.
Cohen J . Statistical power analysis for the behavioral sciences. 2nd ed. New York: Laurence Erlbaum Associates (1988).
24.
Aguiar DP Souza CP d Q Barbosa WJM Santos-Júnior FFU de Oliveira AS . Prevalence of chronic pain in Brazil: systematic review. Braz J Pain. (2021) 4:257–67. doi: 10.5935/2595-0118.20210041
25.
Wang WL Chen KH Pan YC Yang SN Chan YY . The effect of yoga on sleep quality and insomnia in women with sleep problems: a systematic review and meta-analysis. BMC Psychiatry. (2020) 20:195. doi: 10.1186/S12888-020-02566-4,
26.
Diotaiuti P Corrado S Mancone S Cavicchiolo E Chirico A Siqueira TC et al . A psychometric evaluation of the Italian short version of the fear of pain questionnaire-III: psychometric properties, measurement invariance across gender, convergent, and discriminant validity. Front Psychol. (2023) 13:1087055. doi: 10.3389/FPSYG.2022.1087055,
27.
Arya S Yadav RK Venkataraman S Deepak KK Bhatia R . Objective evidence for chronic back pain relief by medical yoga therapy. Front Pain Res. (2022) 3:1060685. doi: 10.3389/FPAIN.2022.1060685,
28.
Tankha H Gaskins D Shallcross A Rothberg M Hu B Guo N et al . Effectiveness of virtual yoga for chronic low back pain: a randomized clinical trial. JAMA Netw Open. (2024) 7:e2442339. doi: 10.1001/JAMANETWORKOPEN.2024.42339,
29.
Chamola V Gummana EP Madan A Rout BK Rodrigues JJPC . Advancements in yoga pose estimation using artificial intelligence: a survey. Curr Bioinforma. (2024) 19:264–80. doi: 10.2174/1574893618666230508105440
30.
Kavuri R Bangari M Yarram H Talari H . Application of artificial intelligence on camera-based human pose prediction for yoga: a methodological study. Lecture. (2024) 843:87–98. doi: 10.1007/978-981-99-8476-3_8
31.
Nair PMK Kriplani S Kodali PB Maheshwari A Bhalavat KD Singh D et al . Characteristics of patients who use yoga for pain management in Indian yoga and naturopathy settings: a retrospective review of electronic medical records. Front Pain Res. (2023) 4:1185280. doi: 10.3389/FPAIN.2023.1185280,
32.
Anheyer D Haller H Lauche R Dobos G Cramer H . Yoga for treating low back pain: a systematic review and meta-analysis. Pain. (2022) 163:E504–17. doi: 10.1097/J.PAIN.0000000000002416,
33.
Vilarino GT Andreato LV de Souza LC Branco JHL Andrade A . Effects of resistance training on the mental health of patients with fibromyalgia: a systematic review. Clin Rheumatol. (2021) 40:4417–25. doi: 10.1007/s10067-021-05738-z,
34.
Nair PMK Keswani J Vadiraja HS . Editorial: Yoga for pain relief. Front Pain Res. (2024) 5:1422483. doi: 10.3389/FPAIN.2024.1422483,
Summary
Keywords
anxiety, depression, mental health, pain, sleep quality, yoga
Citation
Andrade A, D’Oliveira A, da Silveira Moreira CJ, Mancone S, Diotaiuti P and da Luz Koerich MHA (2025) Immediate effects of yoga on anxiety, depression, and sleep in women with chronic pain in a rural community setting: a pilot feasibility study. Front. Med. 12:1671950. doi: 10.3389/fmed.2025.1671950
Received
23 July 2025
Accepted
20 October 2025
Published
03 November 2025
Corrected
16 December 2025
Volume
12 - 2025
Edited by
Pradeep M. K. Nair, Mirakle Integrated Health Centre, India
Reviewed by
Jyoti R. Keswani, Sant Hirdaram Medical College of Naturopathy and Yogic Sciences, India
Moodala Girishankara K. S., Swami Vivekananda Yoga Anusandhana Samsthana, India
Updates
Copyright
© 2025 Andrade, D’Oliveira, da Silveira Moreira, Mancone, Diotaiuti and da Luz Koerich.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandro Andrade, alexandro.andrade.phd@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.