- Department of Obstetrics and Gynecology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Uterine mesothelial cysts (UMCs) are rare, benign lesions that arise from the mesothelial lining of the uterus and are only sporadically documented in the literature. Because of their extremely low incidence, the clinical presentation and imaging features of UMCs are often nonspecific, which makes preoperative diagnosis particularly challenging. We report the case of a 46-year-old nulliparous woman who presented with an intramural cystic mass of the uterus. Preoperative imaging suggested a benign lesion, but the differential diagnosis included cystic degeneration of leiomyoma, adenomyotic cyst, and endometriosis. The patient underwent a laparoscopic cystectomy, during which the cyst was completely excised without intraoperative complications. She recovered uneventfully and was discharged on postoperative day three. Histopathological examination confirmed the diagnosis of a uterine mesothelial cyst. At 1 month of follow-up, no recurrence was observed. This case highlights the importance of surgical excision for both definitive diagnosis and treatment, emphasizes the challenges in preoperative assessment, and contributes valuable clinical evidence to the limited body of knowledge on UMCs.
Introduction
Mesothelial cysts are rare mesenchymal lesions, most of which are benign (1), with fewer than 5,000 documented cases worldwide since their first description by Mennemeyer and Smith in 1979 (2, 3). However, only six cases of mesothelial cysts in the uterine corpus have been documented. Although the exact pathogenesis of UMC remains unclear, it is generally suspected to involve a developmental disorder of mesothelial cells (4). Chronic inflammation of the peritoneum is widely considered the primary reason behind the development of mesothelial cysts, as it may promote cellular proliferation and the migration of mesothelial cells within peritoneal tissues (3). The presence of mesothelial cysts can be associated with conditions such as pelvic inflammatory disease, previous abdominal surgeries, and endometriosis (3, 5, 6). Karpathiou et al. (7) suggested that mesothelial cystic lesions are predominantly benign, although malignant transformation could potentially be related to chronic inflammation resulting from repeated interventions. Due to the unpredictable biological behavior and atypical clinical symptoms of UMC, early identification and aggressive treatments are essential.
Case presentation
The patient was a 46-year-old married nulliparous Chinese woman who worked in an office environment. She denied smoking, alcohol consumption, or use of recreational drugs. She reported mild psychological distress due to a prolonged history of infertility but had no psychiatric disorders. Her family history was unremarkable for gynecological malignancies, endometriosis, or other cystic lesions. She sought medical attention at Wuhan Union Hospital on December 16, 2024, due to a persistent uterine mass. She had previously undergone curettage following a pregnancy and had no other notable medical conditions or prior surgeries. Although she occasionally experienced abdominal distension, she did not report abdominal pain, abnormal uterine bleeding, or dysmenorrhea.
Physical examination
Upon bimanual pelvic examination, it was observed that the uterus was enlarged with thickened adnexa. The abdomen was found to be soft and non-sensitive, with the presence of an approximately 8 × 8 cm palpable mass.
Laboratory and imaging results
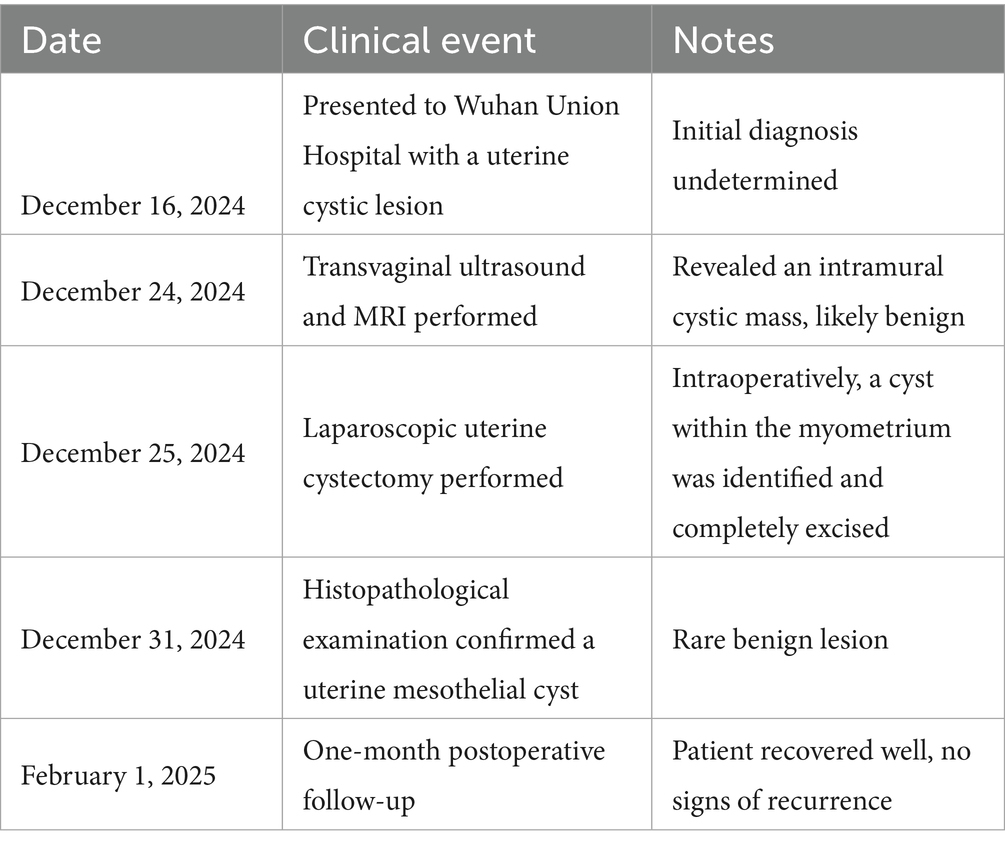
Serum tumor markers, including CA125, CA19-9, CEA, and AFP, showed no specific abnormalities. Transvaginal color Doppler ultrasound identified a hypoechoic mass measuring approximately 90 × 75 mm in the anterior uterine corpus, characterized by well-defined margins and internal septations, with Doppler imaging showing blood flow within the mass (Figure 1A). Pelvic MRI confirmed the presence of a cystic structure in the anterior part of the uterine corpus, showing hyperintensity on T2 imaging and mild enhancement along its periphery (Figure 1B).
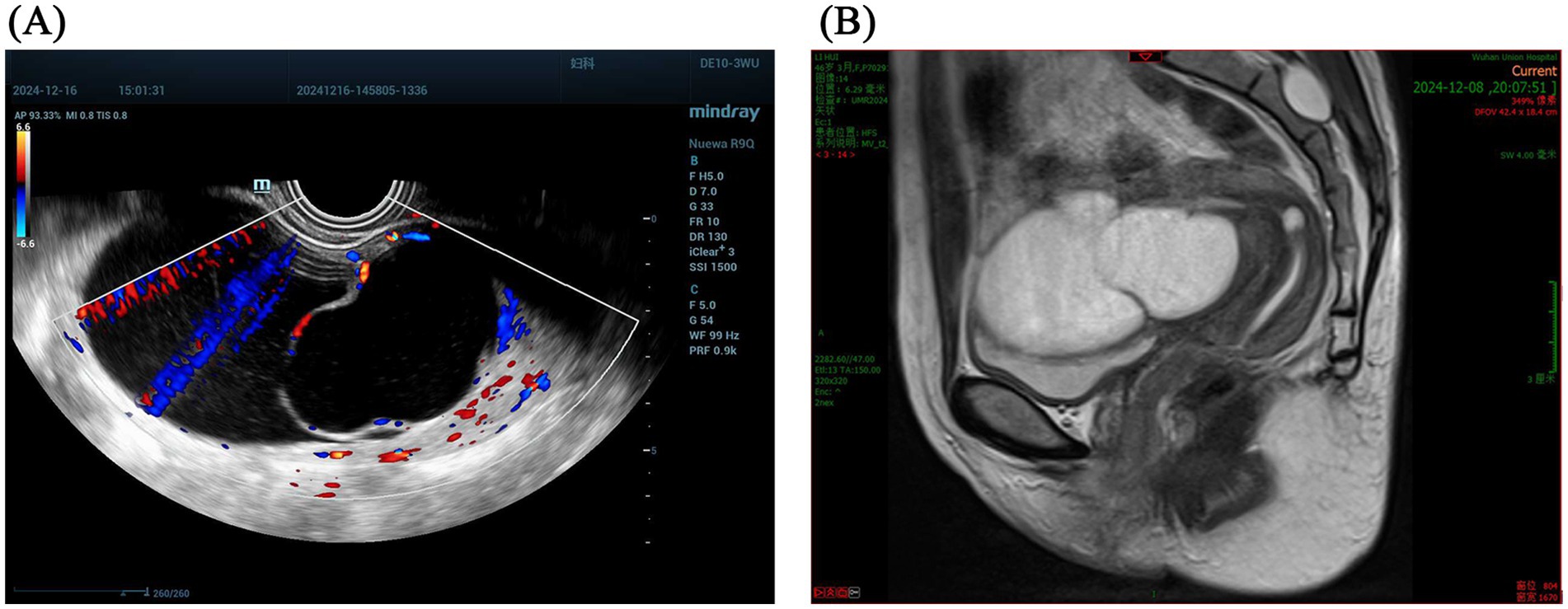
Figure 1. (A) Transvagina1 color Doppler ultrasound identified a hypoechoic mass characterized by well-defined margins and internal septations, with Doppler imaging showing blood flow. (B) Pelvic MRI confirmed the presence of a cystic structure in the anterior part of the uterine corpus.
Preoperative differential diagnosis
Based on the patient’s clinical presentation and preoperative imaging, we considered several entities that can manifest as an intramural cystic lesion of the uterus. The working differential included cystic degeneration of a leiomyoma, adenomyotic cyst, intramyometrial endometriosis, adenomatoid tumor, and other rare cystic lesions (e.g., Müllerian remnant or lymphangioma).
Surgical treatment
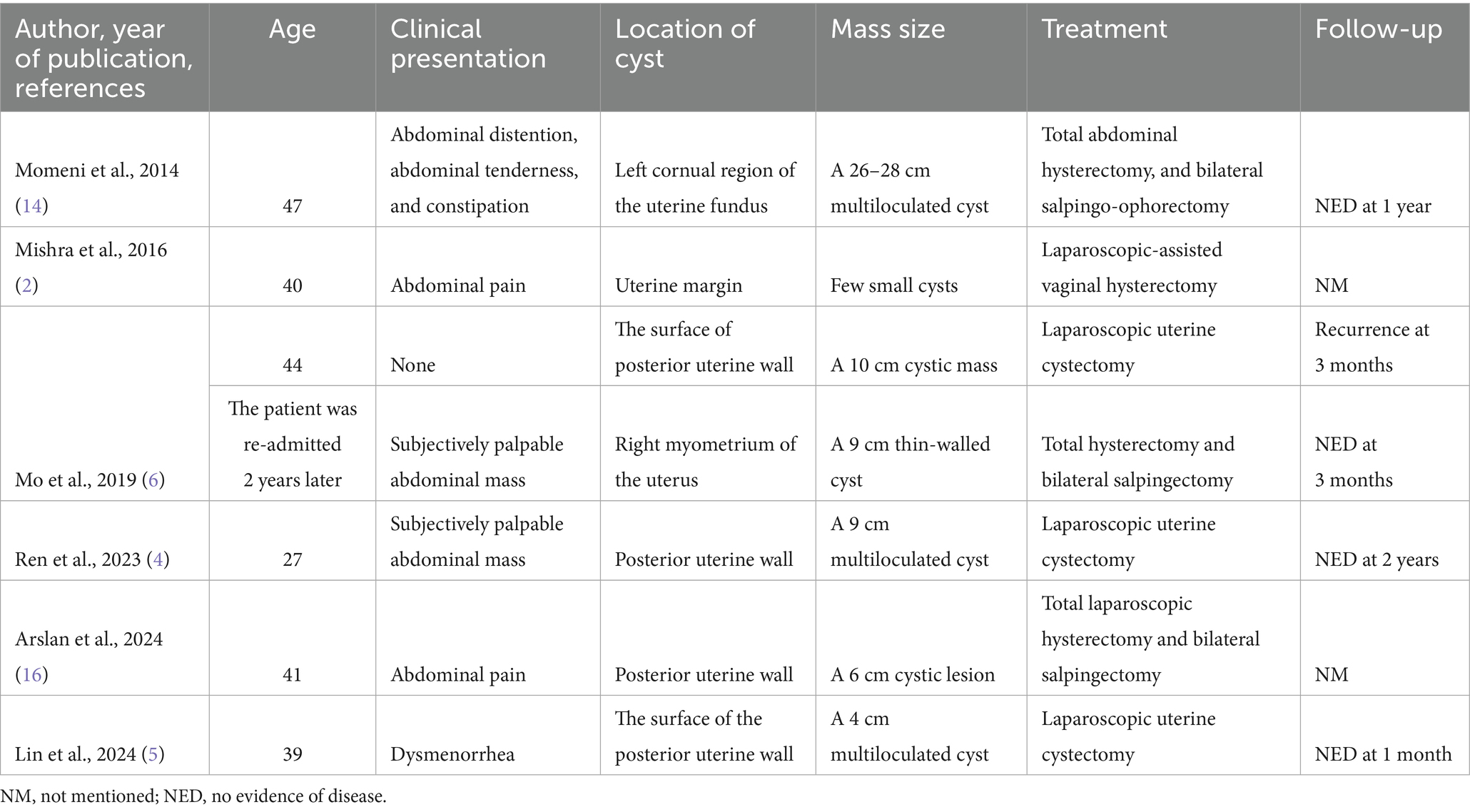
During the surgery, a multilocular cyst filled with clear yellow fluid was discovered in the anterior wall of the uterus, with no other abnormalities detected (Figure 2A). The cyst was found near the endometrium and myometrium, exhibiting a smooth wall without nodules. Extensive adhesions to neighboring tissues made it challenging to separate the cyst from the uterus, requiring precise dissection along an unclear myometrial boundary (Figure 2B). The cyst was excised laparoscopically with no complications, and the patient was discharged within 3 days. Conclusive histological examinations ruled out cancer and confirmed the benign nature of the uterine cyst. Under the microscope, the cyst exhibited a single-layer lining of flattened epithelial cells, transitioning from cuboidal to columnar shapes, lacking cilia (Figures 2C,D). Additionally, no signs of cellular atypia, mitotic activity, or tissue necrosis were observed. The definitive pathology identified the lesion as a uterine mesothelial cyst.
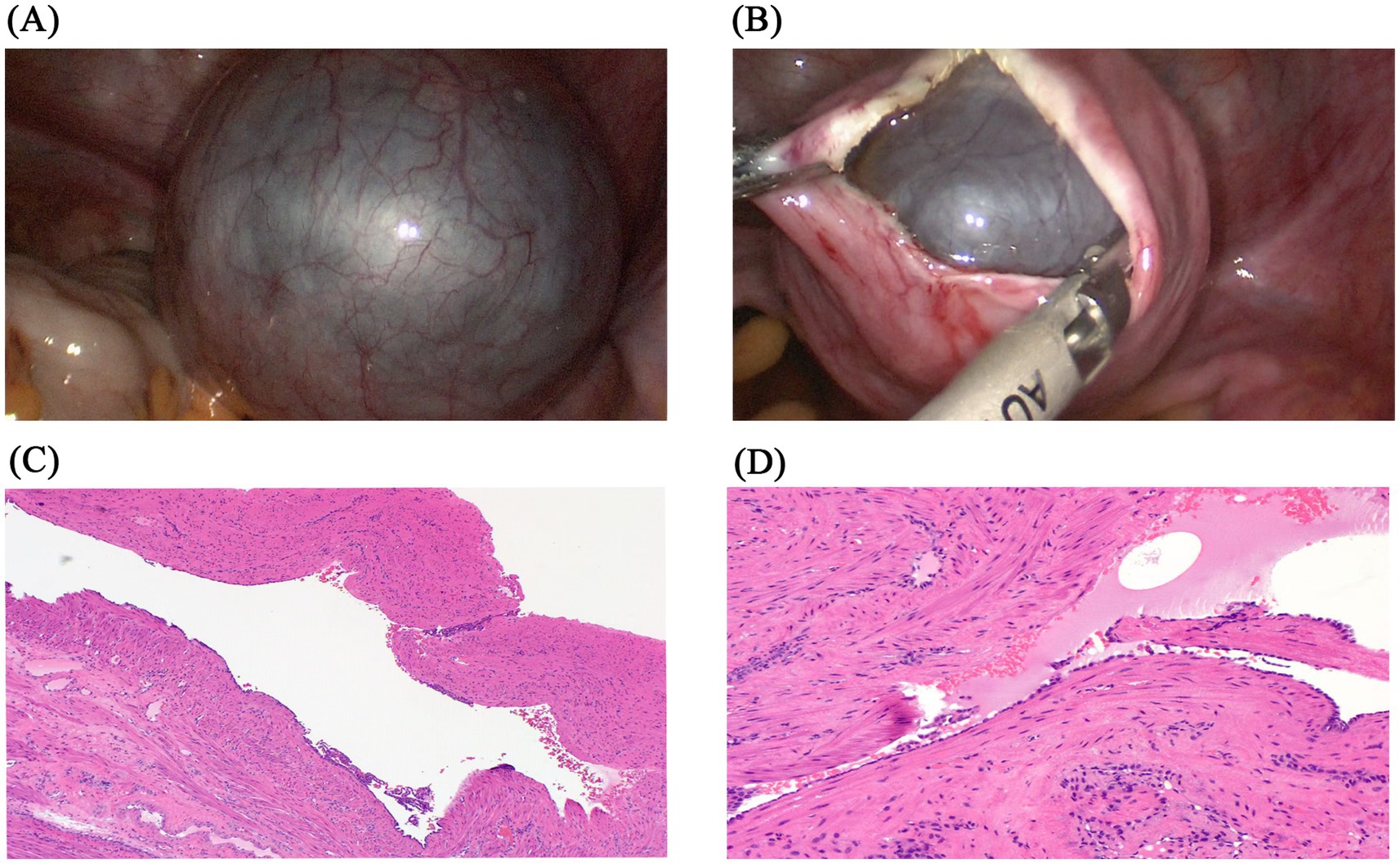
Figure 2. Examples of uterine mesothelial cysts pathology sections. (A) Uterine mesothelial cyst in the anterior uterine corpus. (B) Following incision of the myometrium, the intrauterine cyst is exposed. (C) Representative image of hematoxylin and eosin staining (40×) shows a single-layer lining of flattened epithelial cells. (D) Representative image of hematoxylin and eosin staining (100×) shows a transition from cuboidal to columnar morphology, with an absence of cilia.
Rationale for surgical intervention
Although conservative strategies such as monitoring or cyst aspiration could have been considered, surgical excision was deemed more appropriate for several reasons. First, the imaging characteristics were non-specific, and histopathological confirmation was required to establish a definitive diagnosis. Second, aspiration or observation alone would carry a risk of recurrence and would not reliably exclude malignancy. Finally, laparoscopic excision provided both diagnostic and therapeutic benefits with low morbidity, making it the most reasonable management strategy.
Follow-up and outcome
The patient successfully recovered from the surgery, and a follow-up examination after 1 month showed no signs of recurrence. The treatment timeline of the patient is presented in Table 1.
Discussion
The clinical manifestations and imaging findings of uterine mesothelial cysts (UMCs) are often non-specific, leading to a relatively high rate of missed diagnoses. Uterine mesothelial cysts can develop on any peritoneal surface, including the round ligament, adnexa, mesentery, or peritoneum (2). In the uterus, the majority of reported cases involve the round ligament, often presenting a resemblance to an inguinal hernia. Instances of mesothelial cysts within the uterine corpus are exceptionally rare, and most mesothelial cysts appear benign (1). We found six cases of uterine mesothelial cysts after a Pubmed search of English-language studies published (Table 2). Six patients’ clinical presentations, locations and characteristics of the cysts, interventions, and outcomes were reviewed. Most cysts were detected during further evaluation for abdominal pain, and more than half were located in the posterior uterine wall. All patients were older than 39 years, except for one 27-year-old nulliparous woman reported by Ren et al. (4). With the exception of this patient, who underwent cyst excision alone to preserve fertility, nearly all others underwent total hysterectomy and achieved satisfactory outcomes, with no recurrence observed during follow-up. However, Mo et al. (6) also described a patient who experienced recurrence 3 months after cystectomy, which contrasts with the report by Ren.
Many patients diagnosed with UMC have a prior history of pelvic inflammatory disease, endometriosis, or abdominal surgeries (3, 5, 6). Several studies suggest that uterine mesothelial cysts may have a congenital origin, originating from invagination and metaplasia of mesothelial cells or residual endodermal tissues within the uterus (8–11). Factors such as dust, chronic irritation or inflammation (2, 12, 13), endometriosis (14), and previous abdominal surgeries (14) are known to induce hyperplastic and neoplastic changes in mesothelial cells, potentially enhancing their proliferation and migration in underlying peritoneal tissues (14, 15).
Uterine mesothelial cysts generally present without specific clinical manifestations. Patients may be asymptomatic or exhibit symptoms such as abdominal masses (4), pelvic pain, abdominal distention, menorrhagia (6) or constipation (5, 16). The rarity of these cysts and the nonspecific nature of their symptoms pose challenges in preoperative identification.
Imaging plays a central role in the diagnostic process of uterine mesenchymal neoplasms (UMC). Various imaging techniques are indispensable for a precise diagnosis of UMC. In asymptomatic cases, serial ultrasound imaging is crucial for observing fluctuations in cyst dimensions and monitoring benign cystic mesothelioma (6). Computed tomography (CT) and magnetic resonance imaging (MRI) are highly effective in identifying and delineating uterine lesions (17). However, pathological analysis stands out as the gold standard for definitive confirmation of UMC (5, 16).
Microscopic evaluation typically reveals cysts surrounded by smooth muscle bundles, lined with a cuboidal-to-flat epithelial layer lacking cilia (16). Immunohistochemistry lacks a universally accepted standard; therefore, combining multiple markers enhances accuracy (4), calretinin is widely utilized due to its specificity and sensitivity to mesothelial cells (18). Additionally, HBME-1 (4), WT1, and cytokeratin 5/6 (6) are valuable for identifying mesothelial differentiation (19, 20). WT1 is shown to be less sensitive compared to calretinin (18). In various studies, the lining cells exhibited focal positive for WT1 (2, 16), while PAX8 expression remains inconsistent, yielding no definitive conclusions (2, 5). Test for estrogen receptor (ER), progesterone receptor (PR), and GATA3 typically yield negative results (4, 5, 16).
Given the extremely low incidence and limited number of published cases, no standardized treatment approach for uterine mesothelial cysts has been established. Treatment options encompass hormonal therapies, percutaneous aspiration or sclerotherapy guided by ultrasound, laser ablation, and chemotherapy, and various surgical interventions (21). However, despite these strategies, the recurrence rates are notably high (14, 21, 22). Ultrasound-guided aspiration typically offers only transient relief as a rapid reaccumulation occurs (23). En bloc surgical excision, though ideal, presents technical challenges due to the thin cyst walls and multicystic structures, increasing the risk of recurrence and potential damage to healthy uterine muscle (4, 5). Long-term monitoring is advisable due to the likelihood of recurrence and the potential for misdiagnosis (4, 5). For older patients or those not desiring pregnancy, hysterectomy—either total or partial—is recommended as the definitive treatment (4, 5).
In view of the patient’s long-standing history of infertility in this case, the potential impact of uterine mesothelial cysts on reproductive outcomes is of clinical interest. Although the exact relationship between UMCs and infertility remains unclear, an intramural cystic lesion may distort the uterine cavity, compromise endometrial receptivity, or interfere with implantation. Surgical excision in this case was performed not only for diagnostic and therapeutic purposes but also to restore normal uterine anatomy and preserve reproductive potential. In this case, the duration of follow-up was limited to 1 month, longer follow-up is needed to assess fertility outcomes, and further reports are required to clarify the association between UMCs and infertility. In conclusion, this study emphasizes the clinical manifestations, diagnosis, and therapeutic options for UMC, providing crucial insights for prompt detection and efficient management of this uncommon condition.
Patient perspective
“I felt anxious when I realized that a cyst was found in my uterus, as I was worried about its impact on my fertility and health. Although I was initially hesitant about undergoing surgery, I decided to follow the doctor’s advice. My recovery was smooth, I am relieved with the outcome and hope my experience can encourage other women facing similar conditions.”
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Clinical Medical Research Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YS: Data curation, Methodology, Writing – original draft. YL: Project administration, Writing – review & editing. CY: Data curation, Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors express their gratitude to the patient and her family for consenting to the release of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. González-Moreno, S, Yan, H, Alcorn, KW, and Sugarbaker, PH. Malignant transformation of “benign” cystic mesothelioma of the peritoneum. J Surg Oncol. (2002) 79:243–51. doi: 10.1002/jso.10081
2. Mishra, A, Malik, S, Agarwal, K, Yadav, A, and Gautam, A. Benign cystic mesothelioma of uterus: an unusual cause of pelvic pain. J Obstet Gynaecol India. (2016) 66:720–2. doi: 10.1007/s13224-016-0917-8
3. Mennemeyer, R, and Smith, M. Multicystic, peritoneal mesothelioma: a report with electron microscopy of a case mimicking intra-abdominal cystic hygroma (lymphangioma). Cancer. (1979) 44:692–8. doi: 10.1002/1097-0142(197908)44:2<692::AID-CNCR2820440242>3.0.CO;2-6
4. Ren, XC, Liu, W, Hu, LR, and Mao, M. Mesothelial cyst of uterus in a nullipara patient: a case report. Medicine. (2023) 102:e33159. doi: 10.1097/MD.0000000000033159
5. Lin, YT, Tsai, JH, Ko, ME, Hsu, C, Sheen, JY, Sheu, BC, et al. Uterine mesothelial cysts mimicking ovarian cysts in a primipara patient with a history of cesarean section: a case report and review of the literature. Taiwan J Obstet Gynecol. (2024) 63:414–7. doi: 10.1016/j.tjog.2023.09.025
6. Mo, SP, Wang, MY, and Li, JK. Mesothelial cyst of uterine corpus misdiagnosed as leiomyoma. Chin Med J. (2019) 132:1502–3. doi: 10.1097/CM9.0000000000000291
7. Karpathiou, G, Casteillo, F, Dridi, M, and Peoc’h, M. Mesothelial cysts. Am J Clin Pathol. (2021) 155:853–62. doi: 10.1093/ajcp/aqaa189
8. Ingle, SB, Hinge Ingle, CR, and Patrike, S. Epithelial cysts of the spleen: a minireview. World J Gastroenterol. (2014) 20:13899–903. doi: 10.3748/wjg.v20.i38.13899
9. Morgenstern, L. Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg. (2002) 194:306–14. doi: 10.1016/S1072-7515(01)01178-4
10. Esparza Estaún, J, González Alfageme, A, and Sáenz, BJ. Radiological appearance of diaphragmatic mesothelial cysts. Pediatr Radiol. (2003) 33:855–8. doi: 10.1007/s00247-003-1014-6
11. Carboni, F, Valle, M, Camperchioli, I, Levi Sandri, GB, Sentinelli, S, and Garofalo, A. Mesothelial cyst of the round ligament of the liver. J Minim Access Surg. (2016) 12:83–5. doi: 10.4103/0972-9941.158954
12. Noiret, B, Renaud, F, Piessen, G, and Eveno, C. Multicystic peritoneal mesothelioma: a systematic review of the literature. Pleura Peritoneum. (2019) 4:20190024. doi: 10.1515/pp-2019-0024
13. van Ruth, S, Bronkhorst, MW, van Coevorden, F, and Zoetmulder, FA. Peritoneal benign cystic mesothelioma: a case report and review of the literature. Eur J Surg Oncol. (2002) 28:192–5. doi: 10.1053/ejso.2000.1215
14. Momeni, M, Pereira, E, Grigoryan, G, and Zakashansky, K. Multicystic benign cystic mesothelioma presenting as a pelvic mass. Case Rep Obstet Gynecol. (2014) 2014:852583. doi: 10.1155/2014/852583
15. Elbouhaddouti, H, Bouassria, A, Mouaqit, O, Benjelloun el, B, Ousadden, A, Mazaz, K, et al. Benign cystic mesothelioma of the peritoneum: a case report and literature review. World J Emerg Surg. (2013) 8:43. doi: 10.1186/1749-7922-8-43
16. Arslan, G, and Acar Sabir, Y. Mesothelial cyst in the uterine myometrium: a rare localization. Cureus. (2024) 16:e75158. doi: 10.7759/cureus.75158
17. Azeem, Z, Sharma, J, Johnson, R, Price, N, Yabar, MZ, and Ghosh, D. Excision of benign multicystic peritoneal mesothelioma and deep infiltrating endometriosis with bowel involvement—a case report. Case Rep Womens Health. (2024) 44:e00658. doi: 10.1016/j.crwh.2024.e00658
18. Carneiro, FP, Muniz-Junqueira, MI, Pittella-Silva, F, Carneiro, MV, Takano, GHS, Vianna, LMS, et al. A panel of markers for identification of malignant and non-malignant cells in culture from effusions. Oncol Rep. (2017) 38:3538–44. doi: 10.3892/or.2017.6022
19. Ordóñez, NG. Immunohistochemical diagnosis of epithelioid mesotheliomas: a critical review of old markers, new markers. Hum Pathol. (2002) 33:953–67. doi: 10.1053/hupa.2002.128248
20. Hurlimann, J. Desmin and neural marker expression in mesothelial cells and mesotheliomas. Hum Pathol. (1994) 25:753–7. doi: 10.1016/0046-8177(94)90243-7
21. Vallerie, AM, Lerner, JP, Wright, JD, and Baxi, LV. Peritoneal inclusion cysts: a review. Obstet Gynecol Surv. (2009) 64:321–34. doi: 10.1097/OGX.0b013e31819f93d4
22. Rapisarda, AMC, Cianci, A, Caruso, S, Vitale, SG, Valenti, G, Piombino, E, et al. Benign multicystic mesothelioma and peritoneal inclusion cysts: are they the same clinical and histopathological entities? A systematic review to find an evidence-based management. Arch Gynecol Obstet. (2018) 297:1353–75. doi: 10.1007/s00404-018-4728-2
Keywords: uterine mesothelial cyst, preoperative diagnosis, etiology, clinical treatment, histopathology
Citation: Shao Y, Liu Y and Yang C (2025) Case Report: Uterine mesothelial cyst in a nulliparous woman—diagnostic and clinical challenges of a rare benign lesion. Front. Med. 12:1672439. doi: 10.3389/fmed.2025.1672439
Edited by:
Xin Zhang, Jiangmen Central Hospital, ChinaReviewed by:
Stylianos Sergios Chatziioannou, European University Cyprus, CyprusAshok Kumar Jyothi, Government Degree College for Women Khammam, India
Copyright © 2025 Shao, Liu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun Yang, MzAzNTc0Nzk1QHFxLmNvbQ==
 Ying Shao
Ying Shao Yi Liu
Yi Liu Chun Yang
Chun Yang