Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is associated with high prevalence, disability, and mortality rates. As one of the most populous countries facing a significant burden of COPD, the extent of this burden in China remains inadequately defined. This study utilizes data from the Global Burden of Disease Study 2021 (GBD 2021) to analyze the current status and trends of COPD burden in China, aiming to provide epidemiological data to support prevention, early intervention, and policy formulation related to COPD.
Methods:
This study employs the GBD 2021 database and utilizes various statistical methods, including estimated annual percentage change, Joinpoint regression analysis, decomposition analysis, predictive analysis, and risk factor attribution, to conduct a stratified analysis of the burden of COPD in China by sex, age, and time.
Results:
Between 1990 and 2021, the age-standardized rate (ASR) of COPD in China showed a significant decline, with projections indicating that this trend will continue. However, the rate of decline has slowed in recent years, and the absolute number of COPD patients continues to rise. In 2021, the age-standardized incidence rate (ASIR) was 215.62 per 100,000, the age-standardized prevalence rate (ASPR) was 2,499.35 per 100,000, the age-standardized mortality rate (ASMR) was 73.23 per 100,000, and the age-standardized disability-adjusted life years (ASDR) was 1,227.66 per 100,000. The decline was more pronounced in females than in males, with females experiencing a lower overall burden. For both sexes, the ASR of COPD increased with age; prior to age 60, rates were similar, but after age 60, males exhibited higher ASMR and ASDR than females. Population aging is identified as the primary driver of the increasing burden of COPD, while epidemiological changes contribute to its reduction. Smoking remains the leading risk factor for mortality, with eight related risk factors identified.
Conclusion:
While the ASR of COPD in China has significantly improved, the absolute burden continues to escalate, with notable differences by age and sex. Future efforts should focus on enhancing preventive measures for major risk factors and implementing early screening for high-risk populations to promote early diagnosis and treatment strategies, thereby alleviating the disease burden.
1 Background
Chronic obstructive pulmonary disease (COPD) is a common chronic respiratory condition characterized by persistent airflow limitation and chronic airway inflammation. Due to its high prevalence, significant disability burden, elevated mortality rates, and prolonged disease course, COPD has become one of the most pressing public health issues globally (1–5). The insidious onset and atypical early clinical manifestations of COPD contribute to a low diagnostic rate. It is estimated that approximately 70% of COPD patients worldwide remain undiagnosed, leading to delays in seeking medical attention and disease progression (6). Research indicates that undiagnosed COPD patients face a mortality risk approximately 23% higher than those without airflow limitation (7). Insufficient diagnosis hinders timely intervention, making patients more susceptible to acute exacerbations. About 46% of COPD patients experience at least one acute exacerbation annually, with 19% requiring hospitalization (8). Acute exacerbations not only accelerate the decline in lung function but also severely impair quality of life, significantly increasing the risks of hospitalization, disability, and mortality, thereby exacerbating the burden on both families and healthcare systems.
In the context of a growing global burden, the latest data from the Global Burden of Disease Study 2021 (GBD 2021) reveals that China ranks first in the world for the incidence, prevalence, and mortality of COPD, indicating an extremely heavy disease burden (9). This burden is further exacerbated by a lack of awareness and management deficiencies. Research shows that approximately two-thirds of patients with moderate to severe COPD in China exhibit no obvious clinical symptoms, with awareness rates below 1%. Only 5.9% of patients have undergone pulmonary function testing (such as spirometry), and merely 11.7% have received any form of treatment (10). Concurrently, demographic aging, ongoing population growth, and environmental pollution are expected to further drive the rising trend of COPD burden in China over the coming decades (11, 12).
To optimize the prevention and control strategies for COPD in China, it is essential to gain a deeper understanding of the evolving trends in its disease burden. This study utilizes the GBD 2021 database and employs various statistical methods, including trend analysis, decomposition analysis, predictive modeling, and attribution of risk factors, to systematically assess the changes in the burden of COPD in China from 1990 to 2021 and to forecast its future trajectory. The aim is to provide important evidence-based support for the formulation of precise and sustainable public health interventions.
2 Materials and methods
2.1 Data sources and disease definition
This study is based on all available data related to COPD in China from the GBD 2021 database, including multi-source data from the China Disease Surveillance System, Cause of Death Registry, national chronic disease epidemiological surveys (such as the China Chronic Disease and Nutrition Surveillance, the China Pulmonary Health Study), and published respiratory disease research. The Global Burden of Disease (GBD) project integrates and estimates these data using a set of standardized modeling methods, including DisMod-MR, spatiotemporal Gaussian process regression, and Bayesian meta-regression. Since the GBD database is an integrated data source, the original literature list is not provided. For a comprehensive methodology and data sources, please refer to the core GBD 2021 paper (13). This study extracted and used all age-specific and sex-specific indicators related to COPD in China from the GBD 2021 database, including incidence, prevalence, mortality, and Disability-Adjusted Life Years (DALYs). These can be found at: https://vizhub.healthdata.org/gbd-results?params=gbd-api-2021-permalink/ec7be55cfb5472a2f931c4f9a18f3e76.
The data selection criteria were as follows: the region was limited to “China,” the disease category was specified as “chronic obstructive pulmonary disease,” risk factors were selected as “most detailed risks,” the gender included “male, female, and overall,” and the time frame was “1990–2021.” To ensure comprehensive age coverage for burden estimation, we selected all standard 5-year age intervals (i.e., <5 years, 5–9 years, …, 95 years and older) from the GBD database for age groups, in order to fully capture the distribution of COPD across the entire lifespan. The diagnosis of COPD was based on the International Classification of Diseases, 10th Revision (ICD-10) codes, including J41, J42, J43, J44, and J47. The extracted indicators included incidence, prevalence, mortality, and disability-adjusted life years (DALYs), with all indicators reported alongside a 95% uncertainty interval (UI). Additionally, all age-standardized rate (ASR) indicators in this study, including Age-Standardized Incidence Rate (ASIR), Age-Standardized Prevalence Rate (ASPR), Age-Standardized Mortality Rate (ASMR), and Age-Standardized DALYs Rate (ASDR), were directly extracted from the final estimates of the GBD 2021 database. In generating these estimates, GBD used its standardized GBD World Standard Population Structure for calculation, aimed at eliminating the influence of regional and temporal population age composition differences, ensuring high comparability of disease burden trends across different countries and globally. China’s population data can be found directly at: https://vizhub.healthdata.org/gbd-results?params=gbd-api-2021-permalink/67a8e77c3f7b6b0e9152f344ef217f96. All data cleaning, statistical analyses, and visualizations were conducted using R software (version 4.4.2), utilizing packages such as dplyr, tidyverse, BAPC, and ggplot2. Statistical significance was set at P < 0.05.
2.2 Statistical analysis
To assess the temporal trends in the burden of COPD in China from 1990 to 2021, this study employed a combined analysis of the estimated annual percentage change (EAPC) and Joinpoint regression model (14, 15). The formula for calculating EAPC is: EAPC = 100 × [exp(β) − 1], where β represents the linear regression coefficient between the natural logarithm of ASR [ln(ASR)] and year (X): ln(ASR) = α + βX + ε. Joinpoint regression segments the time series by identifying “turning points” in trend changes, calculating the annual percentage change (APC) for each segment and the average annual percent change (AAPC) for the overall trend. EAPC, AAPC, and APC are reported with 95% confidence intervals (CI); if the effect value >0 and the lower limit >0, it indicates an upward trend; conversely, if the effect value <0 and the upper limit <0, it indicates a downward trend.
This study also employed the DasGupta decomposition method to quantify the net changes in the burden of COPD from 1990 to 2021, assessing the independent contributions of population growth, aging, and epidemiological changes to reveal the relative impact of different driving factors on the evolution of COPD burden (16, 17).
Future trend predictions were conducted using the Bayesian Age-Period-Cohort (BAPC) model to evaluate the changes in the burden of COPD in China from 2022 to 2050. The BAPC model utilized a second-order random walk (RW2) prior to smooth the effects of age, period, and birth cohort, combined with nested Laplace approximation to avoid convergence and mixing issues commonly faced in traditional Bayesian analyses using Markov Chain Monte Carlo methods, thereby enhancing predictive accuracy (18).
Additionally, the population attributable fraction (PAF) was calculated to assess the relative contribution of various risk factors to the burden of COPD. PAF represents the proportion of disease burden that could be avoided by completely eliminating a specific exposure, calculated using the formula: PAF = [P × (RR − 1)]/[P × (RR − 1) + 1], where P is the prevalence of the exposure in the population, and RR is the relative risk (or odds ratio, OR) of the exposed group compared to the non-exposed group. P and RR are typically estimated based on population survey data and epidemiological literature.
3 Results
3.1 Disease burden
Between 1990 and 2021, the ASR for COPD in China showed significant improvement, although the absolute disease burden continued to rise. The ASIR decreased from 271.22 per 100,000 (95% UI: 251.66–288.62) to 215.62 per 100,000 (95% UI: 198.00–234.90), with an EAPC of −0.84% (95% CI: −0.88%, −0.81%). The decline in women (EAPC: −0.96%, 95% CI: −1.05%, −0.86%) was significantly faster than in men (EAPC: −0.71%, 95% CI: −0.80%, −0.62%). The ASPR decreased from 2761.81 per 100,000 (95% UI: 2498.94–3033.60) to 2499.35 per 100,000 (95% UI: 2236.21–2793.29), with an EAPC of −0.33% (95% CI: −0.37%, −0.29%), showing a similar downward trend in both sexes. The ASMR decreased significantly from 231.78 per 100,000 (95% UI: 198.98–257.42) to 73.23 per 100,000 (95% UI: 59.73–86.85), with an EAPC of −4.25% (95% CI: −4.48%, −4.02%). Women experienced a faster decline (EAPC: −5.00%, 95% CI: −5.28%, −4.72%) compared to men (EAPC: −3.57%, 95% CI: −3.79%, −3.35%). The ASDR dropped from 3852.57 per 100,000 (95% UI: 3349.97–4279.01) to 1227.66 per 100,000 (95% UI: 1048.45–1442.54), with an EAPC of −4.19% (95% CI: −4.38%, −3.99%), and again, the decline in women (EAPC: −4.67%, 95% CI: −4.91%, −4.43%) was faster than in men (EAPC: −3.74%, 95% CI: −3.92%, −3.56%). Despite the continued decline in ASR, the absolute disease burden of COPD has significantly increased: incident cases rose from 2.16 million to 4.43 million, the total number of cases increased from 23.14 million to 50.58 million, and the number of deaths rose from 1.24 million to 1.29 million. Although the total DALYs decreased from 26.09 million to 23.64 million, the overall burden remains high (Figure 1).
FIGURE 1

Burden of COPD [(A) ASIR; (B) ASPR; (C) ASMR; (D) ASDR; (E) Incidence; (F) Prevalence; (G) Mortality; (H) DALYs].
Joinpoint regression analysis indicates that between 1990 and 2021, all types of ASR for COPD showed a declining trend. However, the rate of decline in ASIR slowed after 2008, in ASPR after 2018, and in both ASMR and ASDR after 2015 (Figure 2).
FIGURE 2
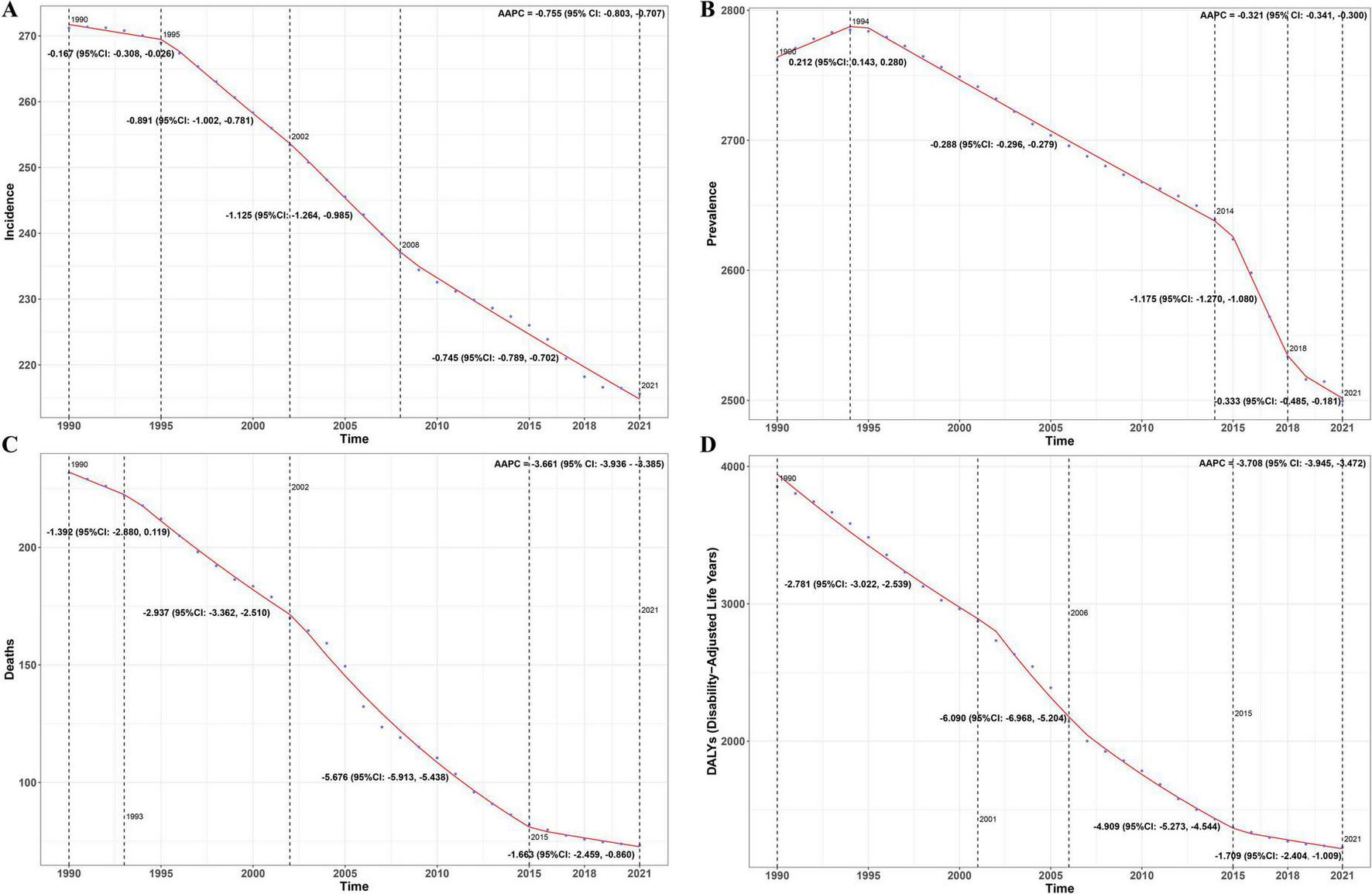
AAPC results [(A) ASIR; (B) ASPR; (C) ASMR; (D) ASDR].
3.2 Age-sex-temporal trends
Analysis by age and sex revealed that the ASR for COPD increased with age in both sexes. The male ASPR peaked in the 85–89 age group, while ASMR and ASDR were highest in the 90–94 age group, followed by a slight decline. In women, the ASR continued to increase with age. Specifically, the differences between males and females were minimal before age 60, but after 60, males exhibited higher ASMR and ASDR than females. The absolute number of patients was mainly concentrated in the 60–89 age group (Figure 3). Age and time analysis showed a decline in ASIR, ASMR, and ASDR across all age groups, while ASPR remained relatively stable (Supplementary Figure 1). Time and sex analysis showed a decline in ASR for both sexes, with males consistently showing higher ASIR, ASMR, and ASDR than females. However, since 2015, the gap in ASPR between males and females has gradually narrowed (Supplementary Figure 2).
FIGURE 3
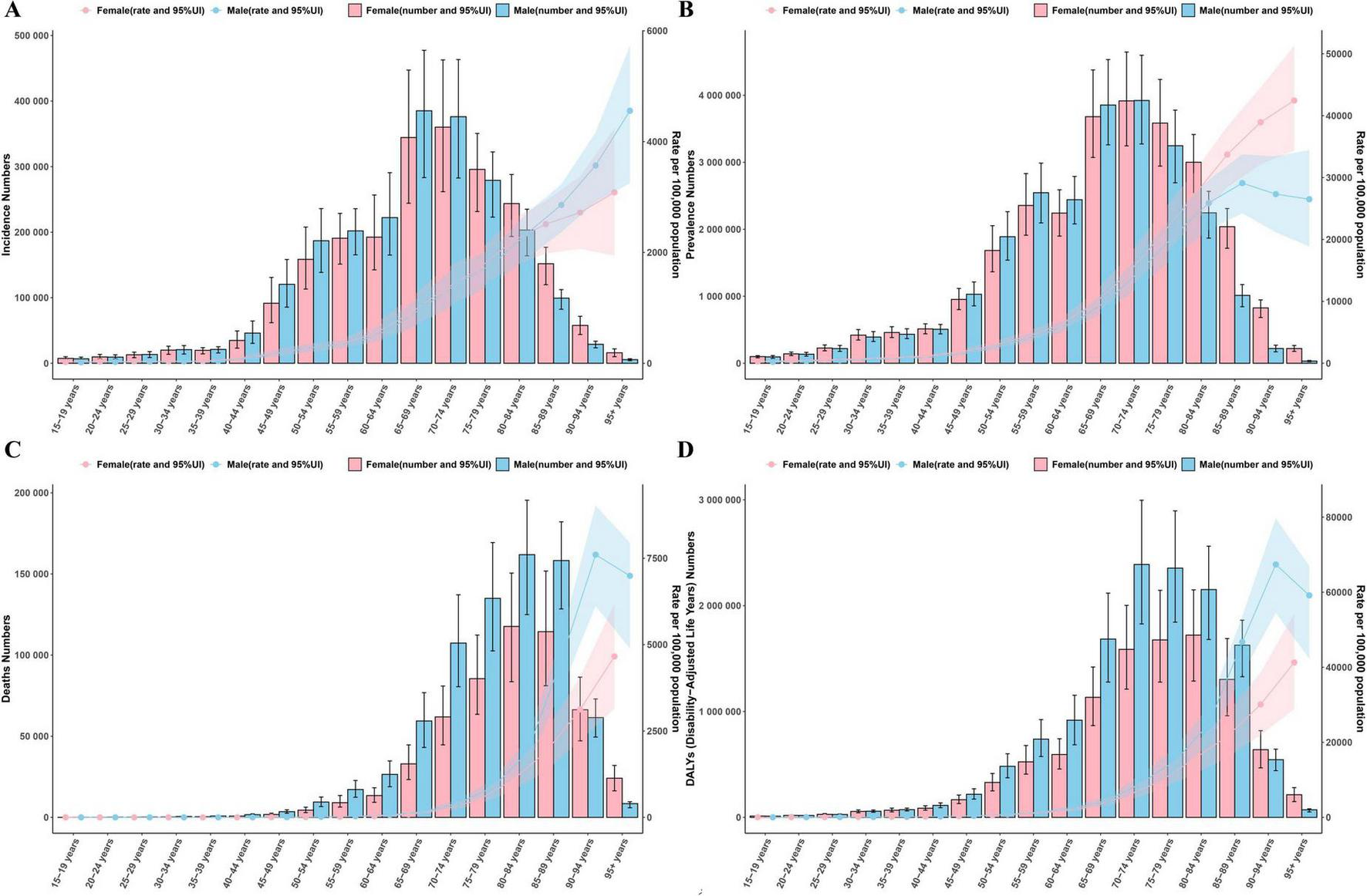
Age-sex analysis results [(A) ASIR; (B) ASPR; (C) ASMR; (D) ASDR].
3.3 Decomposition analysis
The decomposition analysis showed that population aging was the primary driver of the rising absolute burden of COPD. Its contribution to the increase in incidence was 90.75% (an increase of 2.06 million cases), and to the increase in prevalence, it was 77.63% (an increase of 21.30 million cases). Epidemiological factors offset part of this increase, contributing −34.20% (a reduction of 778,000 cases) to the incidence rate. The net increase in deaths was 47,500, mainly driven by aging (contribution of 3010.63%, an increase of 1.43 million) and population growth (contribution of 979.86%, an increase of 465,000), but this increase was largely offset by improvements in epidemiology (contribution of −3890.49%, a reduction of 1.85 million). In terms of health loss, aging resulted in an increase of 23.05 million DALYs (a + 937.92% increase), while epidemiological improvements led to a reduction of 34.48 million DALYs (a −1402.98% decrease), making it the decisive factor in reducing the health burden (Figure 4).
FIGURE 4
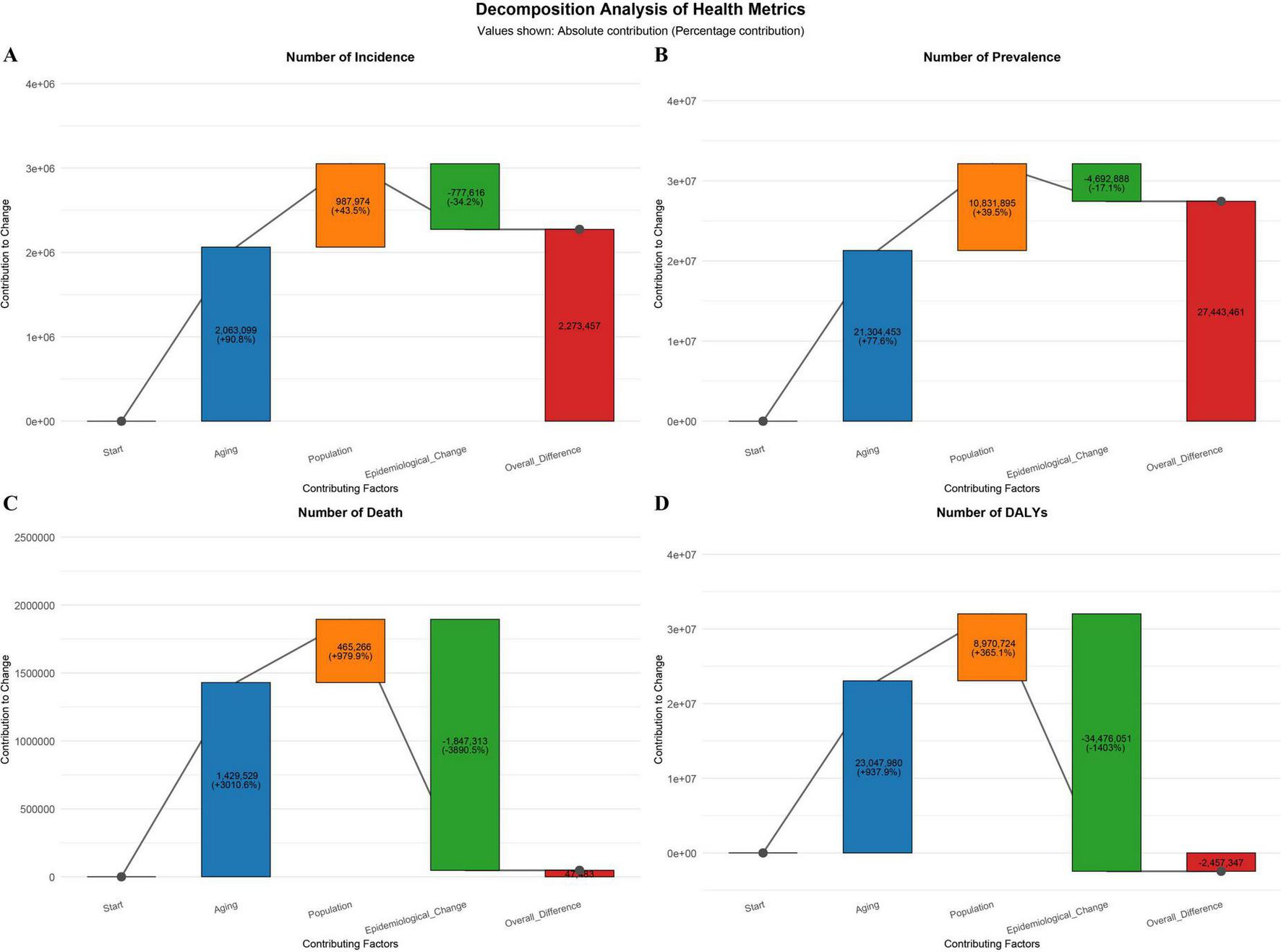
Decomposition analysis results [(A) ASIR; (B) ASPR; (C) ASMR; (D) ASDR].
3.4 Predictive analysis
The predictive model suggests that between 2022 and 2050, both the ASR and the absolute number of COPD cases in China will continue to decline, with the disease burden in males remaining higher than in females. By 2050, the expected values are: ASIR: 233.96 (211.21–256.71) per 100,000, ASPR: 2793.42 (2609.80–2977.05) per 100,000, ASMR: 22.30 (14.20–30.40) per 100,000, and ASDR: 533.64 (383.73–683.55) per 100,000 per year (Figure 5 and Supplementary Table 1).
FIGURE 5
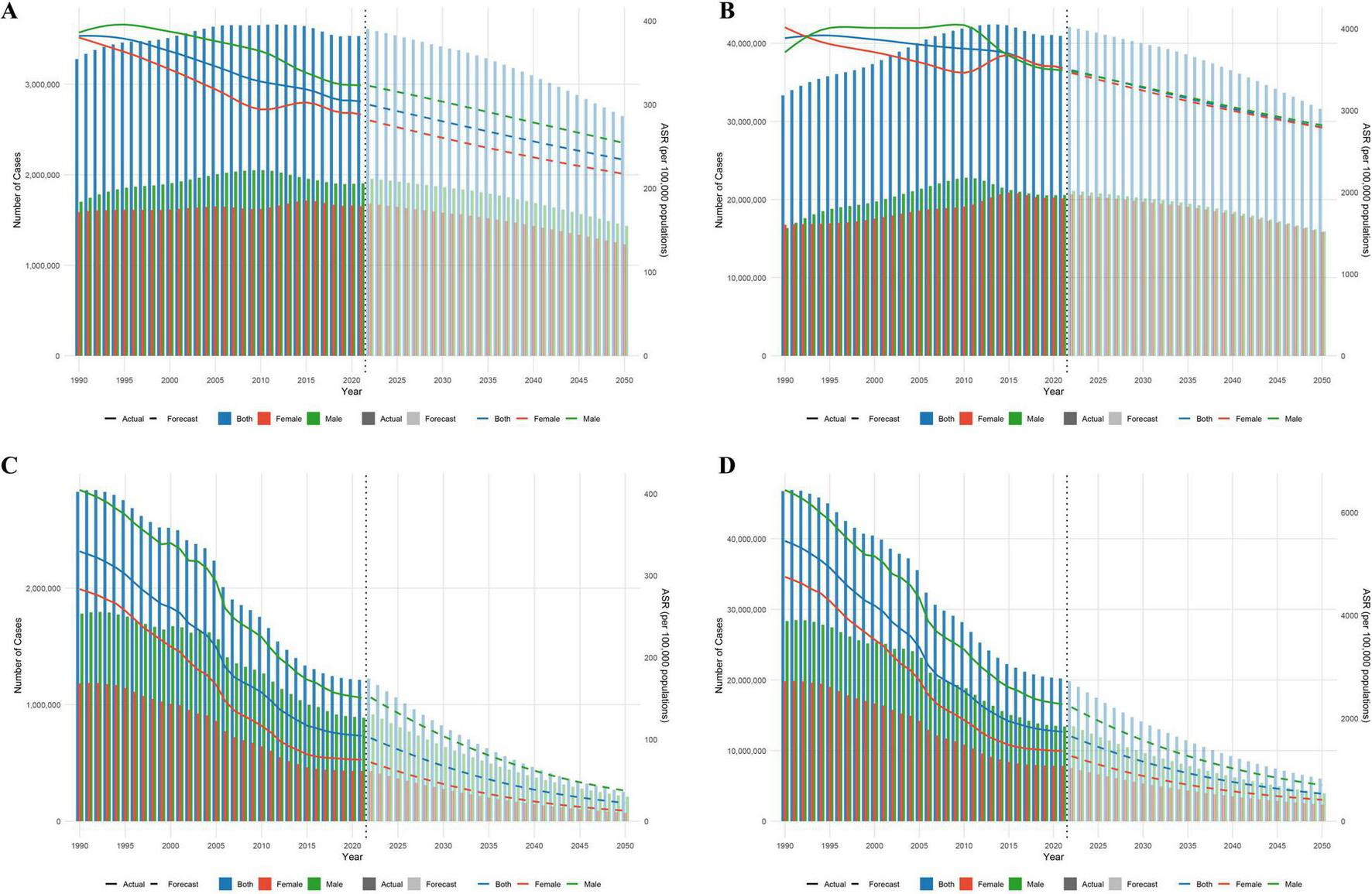
Predictive analysis results [(A) Incidence; (B) Prevalence; (C) Mortality; (D) DALYs].
3.5 Attribution of risk factors for ASMR
Attribution analysis revealed that the primary risk factor for COPD is smoking, with the PAF increasing from 41.63% in 1990 to 42.58% in 2021. The PAF for environmental particulate pollution continued to rise, peaking at 35.86% in 2015 (95% CI: 35.27–36.46) before decreasing to 30.20% in 2021. The PAF for indoor solid fuel pollution decreased significantly, from 55.96% in 1990 to 8.32% in 2021, a reduction of 85.10%. The PAF for occupational exposure to particulate matter/gases/smoke remained stable, ranging from 18.07 to 18.35%. The PAF for cold exposure ranged from 11.19 to 12.79%, with 2021 at 11.54%, significantly higher than that for heat exposure (0.24%–0.79%, 2021: 0.55%). The PAF for environmental ozone pollution showed a U-shaped trend, peaking at 16.45% in 2008 and gradually decreasing to 9.80% in 2021. Additionally, the PAF for second-hand smoke steadily decreased from 10.19% to 9.22% (Figure 6).
FIGURE 6
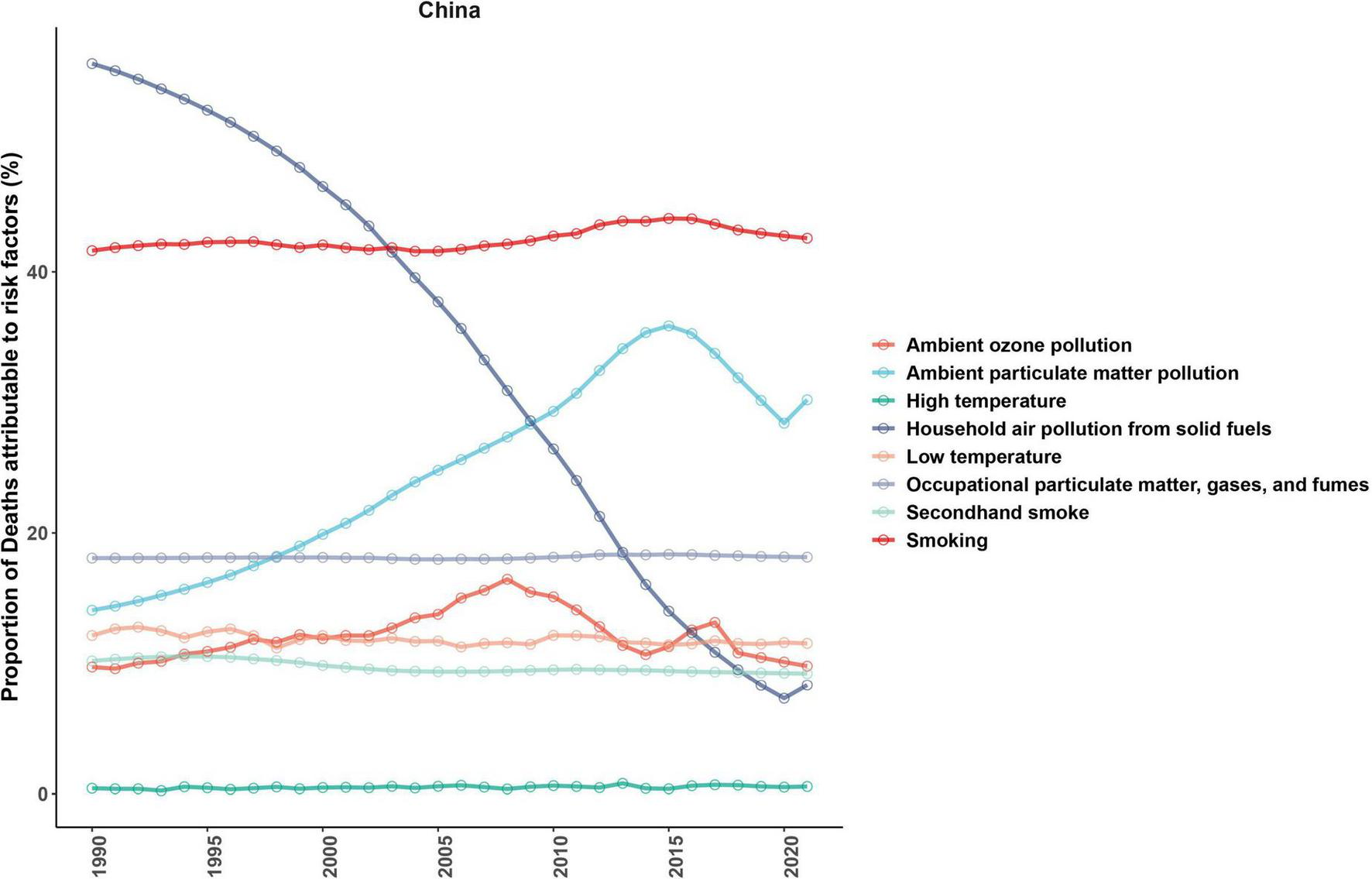
Attributable risk factors for ASMR in COPD.
4 Discussion
This study systematically assessed the trends in the burden of COPD in China from 1990 to 2021. The results show that although the ASR have significantly decreased, the absolute burden continues to increase, indicating that China has made progress in addressing COPD, but still faces significant challenges. Predictive analyses further suggest that the ASR will continue to decline in the future, reflecting the positive impact of China’s rapid socioeconomic development on reducing chronic disease risks, including improvements in nutrition, living conditions, educational levels, and healthcare systems (19, 20). In recent years, the government’s increasing attention to COPD and the strengthening of policy support have contributed to this trend. For example, in 2014, COPD monitoring was incorporated into the national chronic disease and nutrition monitoring system, and the “China National Plan for the Prevention and Treatment of Chronic Diseases (2017–2025)” released in 2017 proposed achieving a 25% lung function testing rate by 2025 and controlling the mortality of chronic respiratory diseases (21). The expansion of insurance coverage, advances in diagnostic and treatment technologies, and improvements in basic public health services have also provided a safeguard for reducing mortality (22, 23). Despite the significant decline in COPD ASR, the actual number of patients continues to increase, and APC analysis shows that the rate of decline in ASR has slowed in recent years. This further underscores the significant ongoing challenge that COPD poses to China. Among people aged 40 and above, the awareness rate of COPD is only 0.9%, with awareness of related knowledge and lung function testing at just 5.7 and 3.4%, respectively (24). Therefore, enhancing public knowledge on the prevention and treatment of COPD, along with the widespread implementation of a three-tier prevention strategy, remains a key measure to reduce the COPD burden.
A core finding of this study is the divergence between the decline in China’s COPD ASIR and ASPR from 1990 to 2021, alongside the increasing trend in absolute case numbers. This seemingly contradictory result is actually a classic epidemiological characteristic, primarily driven by significant changes in China’s demographic structure, particularly the rapid aging of its population (25). Age-standardized rates, calculated using a standard population structure, aim to eliminate the confounding effects of differences in the age composition of the population across time periods. Therefore, the decline in both ASIR and ASPR indicates that, after adjusting for the effects of population aging, the true risk of COPD across all age groups in China has decreased, corroborating the positive impact of public health interventions, improved healthcare access, and environmental policies over the past three decades. In contrast, the increase in absolute case numbers is mainly attributed to demographic factors. The risk of developing COPD significantly increases with age (26). Consequently, despite the decline in risk rates across age groups, the sharp expansion of the elderly population (which is already the highest-risk group) has ultimately led to a net increase in the total number of cases. Our decomposition analysis provides precise quantitative evidence for this mechanism: the contribution of population aging to the growth of both incidence and prevalence of COPD is 90.75 and 77.63%, respectively, far exceeding the impacts of population growth and epidemiological changes. This finding underscores the dual challenge faced by China’s healthcare system: while continuing to implement effective risk-reduction strategies, it must also actively address the long-term trend of rising COPD burden driven by population aging.
Further gender-based analysis shows that both male and female ASR values decrease year by year, with the rate of decline faster in women, and the ASR lower in women compared to men. This may be related to the significantly higher smoking rate in men in China (27, 28), as well as their increased exposure to occupational dust (e.g., mineral dust, inorganic dust, metal dust, and grain dust) and chemical irritants (29, 30). Additionally, estrogen may reduce women’s susceptibility through anti-inflammatory and alveolar protective effects, whereas men are more likely to experience environmental damage during critical periods of lung development (31, 32). Compared to men, women generally have better health awareness and healthier lifestyle habits (e.g., appropriate intake of fruits and vegetables, low-salt diet), and exhibit higher treatment compliance, which may contribute to the observed gender differences in COPD (33). Therefore, measures such as smoking cessation, occupational protection, and enhancing health awareness should be adopted to improve men’s health behaviors.
Age-related analysis revealed a significant increase in COPD ASR with age, reflecting the central role of aging in disease progression. Aging, in essence, refers to the decline in the body’s ability to respond to environmental stress, leading to immune aging, reduced airway defense, and loss of lung parenchymal elasticity, all of which increase susceptibility to disease (34, 35). Furthermore, aging interacts with risk factors such as smoking and pollution, accelerating disease progression. This study found that the burden of COPD peaks among the elderly, attributable both to the extension of the exposure window as life expectancy increases in China and the cumulative effect of long-term exposure to tobacco smoke, indoor fuel pollution, and environmental particulate matter (36). Notably, after age 60, male ASMR and ASDR were higher than in females. This primarily reflects the higher prevalence of lung parenchymal damage in men, resulting from lifelong heavy smoking, which accelerates mortality risk, while women tend to have an airway inflammation type of COPD with relatively slower disease progression (37). The absolute number of patients is concentrated in the 60–89 age group, which not only reflects the aging population but also suggests that it typically takes a long latency period for exposure to risk factors to manifest as significant airflow limitation, highlighting the cumulative effect of COPD. It is noteworthy that this study found a significant number of COPD patients in the younger age group of <40 years. This phenomenon may be explained by multiple factors. First, early life is a critical window for lung development, during which exposure to adverse factors (such as maternal smoking, severe lower respiratory tract infections in childhood, malnutrition, and indoor/outdoor air pollution) may hinder the lungs from reaching their full potential. This could lead to individuals exhibiting lower baseline lung function in early adulthood, thus developing airflow limitation earlier in life (38). Second, genetic susceptibility (such as α-1 antitrypsin deficiency or other common genetic variations) may make some individuals more sensitive to environmental exposures, such as tobacco smoke, accelerating the decline in lung function (39). Furthermore, as clinical awareness of COPD increases and diagnostic capabilities improve, more mild or early-stage patients are being identified and diagnosed at younger ages. Although the age-specific prevalence in this group is much lower than in the elderly population, the absolute number of patients remains a significant disease burden, given China’s large population. This finding underscores the critical importance of advancing the prevention window for COPD, suggesting that public health interventions should target childhood and adolescence, aiming to optimize lung development and reduce early adverse exposures, thus delaying or preventing the onset of COPD from the early stages of the life course. Decomposition analysis further quantified the role of aging in COPD, showing that population aging accounted for 90.75% of the increase in incidence and 77.63% of the increase in prevalence, becoming the primary driver of the rising absolute burden. This phenomenon aligns with China’s accelerating aging process. It is worth noting that the net increase in deaths is largely driven by aging (contributing 3010.60%, an increase of 1.43 million) and population growth (contributing 979.90%, an increase of 465,000), far outpacing the expansion of population size, highlighting the impact of cumulative exposure damage, multimorbidity, and immune aging on elderly COPD patients (35). However, significant improvements in epidemiological factors (with contributions ranging from −34.20 to −3890.50%) have been the main factors mitigating the growth of the COPD burden, directly reflecting the effectiveness of China’s anti-smoking campaigns, clean energy policies, and chronic respiratory disease management. Nonetheless, APC analysis indicates that the rate of decline in ASR has slowed in recent years, particularly with ASPR remaining relatively stable, indicating that existing measures have not yet been able to reverse the trend of case accumulation driven by population aging.
Regarding attributable risk factors, smoking remains the primary modifiable risk factor for COPD-related mortality, with its PAF rising from 41.63% in 1990 to 42.58% in 2021. This indicates that despite ongoing tobacco control policies, the large smoking base and cumulative exposure effects continue to cause significant health losses. Tobacco smoke promotes lung tissue damage through mechanisms involving airway inflammation, oxidative stress, and protease–antiprotease imbalance, with men being more prone to the emphysema type of COPD, which carries a higher risk of mortality (37, 40). The PAF for environmental particulate exposure follows an inverse U-shape, peaking in 2008 at 35.86% (95% CI: 35.27–36.46), before decreasing to 30.20% in 2021. Although the concentrations of pollutants like PM2.5 have significantly decreased, urban heat island effects and extreme temperature variations still pose a significant threat to elderly populations (41, 42). The PAF for cold exposure has remained at around 11.50%, significantly higher than that for heat exposure (0.55% in 2021). This difference is attributed to mechanisms such as bronchospasm, impaired mucociliary function, and increased infection risk, particularly in the elderly (43, 44). The PAF for solid fuel use decreased by more than 85%, highlighting the effectiveness of China’s clean energy policies, though rural areas in the western regions remain concentrated sites of residual risk, requiring solutions such as increased clean energy adoption and improved indoor ventilation (45, 46). Occupational exposure has remained stable at around 18%, suggesting that occupational health management still needs improvement, with continued exposure in high-risk industries like mining and construction maintaining high COPD burdens in men (47).
Although this study provides a comprehensive analysis of the COPD disease burden, it has limitations. Firstly, the research is primarily based on national-level data and does not address provincial heterogeneity, which may obscure regional differences. Secondly, the GBD model does not include some potential risk factors (e.g., e-cigarettes, genetic factors) and their interactions, and there is an issue of multiexposure collinearity that may affect the accuracy of the attribution results.
5 Conclusion
In conclusion, the ASR for COPD in China significantly declined from 1990 to 2021, with expectations that this trend will continue. However, the rate of decline has slowed in recent years, and the absolute number of patients continues to rise, indicating that COPD remains a significant public health issue. The ASR for both males and females increases with age, with similar rates prior to age 60. After 60, the male ASMR and ASDR are higher than those in females. Population aging is the primary driver of the increased disease burden, while epidemiological changes have reduced the burden. Smoking remains the leading risk factor for COPD-related mortality, and eight other related risk factors have been identified. Future efforts should focus on strengthening smoking cessation, environmental governance, and lung function screening for high-risk populations to enable early diagnosis and treatment, along with the development of targeted health management and medical strategies to reduce the COPD burden. Additionally, it should be considered that GBD estimates may be affected by insufficient reporting of underlying data, misclassification of diagnoses, or inconsistencies in coding, which could reduce the reliability of the results.
Statements
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XW: Investigation, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft. JiL: Investigation, Methodology, Project administration, Validation, Writing – original draft. JL: Formal analysis, Resources, Software, Supervision, Writing – original draft. LZ: Data curation, Formal analysis, Investigation, Validation, Writing – original draft. XZ: Funding acquisition, Resources, Software, Supervision, Validation, Writing – original draft. RC: Funding acquisition, Investigation, Methodology, Project administration, Software, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. We acknowledge the Natural Science Foundation of Gansu Province Project (project number: 23JRRF0002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1674952/full#supplementary-material
References
1.
Adeloye D Song P Zhu Y Campbell H Sheikh A Rudan I et al Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. (2022) 10:447–58. 10.1016/S2213-260000511-7
2.
Amegadzie J Mehareen J Khakban A Joshi P Carlsten C Sadatsafavi M . 20-year trends in excess costs of COPD.Eur Respir J. (2025) 65:2400516. 10.1183/13993003.00516-2024
3.
Boers E Barrett M Su J Benjafield A Sinha S Kaye L et al Global burden of chronic obstructive pulmonary disease through 2050. JAMA Netw Open. (2023) 6:e2346598. 10.1001/jamanetworkopen.2023.46598
4.
Christenson S Smith B Bafadhel M Putcha N . Chronic obstructive pulmonary disease.Lancet. (2022) 399:2227–42. 10.1016/S0140-673600470-6
5.
Fabbri L Celli B Agustí A Criner G Dransfield M Divo M et al COPD and multimorbidity: recognising and addressing a syndemic occurrence. Lancet Respir Med. (2023) 11:1020–34. 10.1016/S2213-260000261-8
6.
Diab N Gershon A Sin D Tan W Bourbeau J Boulet L et al Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2018) 198:1130–9. 10.1164/rccm.201804-0621CI
7.
Martinez C Mannino D Jaimes F Curtis J Han M Hansel N et al Undiagnosed obstructive lung disease in the united states. Associated factors and long-term mortality. Ann Am Thorac Soc. (2015) 12:1788–95. 10.1513/AnnalsATS.201506-388OC
8.
Lim S Lam D Muttalif A Yunus F Wongtim S Lan le TT et al Impact of chronic obstructive pulmonary disease (COPD) in the Asia-Pacific region: the EPIC Asia population-based survey. Asia Pac Fam Med. (2015) 14:4. 10.1186/s12930-015-0020-9
9.
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2100–32. 10.1016/S0140-673600367-2
10.
Fang L Gao P Bao H Tang X Wang B Feng Y et al Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. (2018) 6:421–30. 10.1016/S2213-260030103-6
11.
Amegadzie J Lee T Sadatsafavi M Lynd L Sin D Johnson K . Trends in hospital admissions for chronic obstructive pulmonary disease over 16 years in Canada.CMAJ. (2023) 195:E1172–9. 10.1503/cmaj.221051
12.
Wang C Xu J Yang L Xu Y Zhang X Bai C et al Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health [CPH] study): a national cross-sectional study. Lancet. (2018) 391:1706–17. 10.1016/S0140-673630841-9
13.
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2133–61. 10.1016/S0140-673600757-8
14.
Liu Z Jiang Y Yuan H Fang Q Cai N Suo C et al The trends in incidence of primary liver cancer caused by specific etiologies: results from the global burden of disease study 2016 and implications for liver cancer prevention. J Hepatol. (2019) 70:674–83. 10.1016/j.jhep.2018.12.001
15.
Cao F Liu Y Ni Q Chen Y Wan C Liu S et al Temporal trends in the prevalence of autoimmune diseases from 1990 to 2019. Autoimmun Rev. (2023) 22:103359. 10.1016/j.autrev.2023.103359
16.
Fitzmaurice C Allen C Barber RM Barregard L Bhutta ZA . Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study.JAMA Oncol. (2017) 3:524–48. 10.1001/jamaoncol.2016.5688
17.
Luo L . Assessing validity and application scope of the intrinsic estimator approach to the age-period-cohort problem.Demography. (2013) 50:1945–67. 10.1007/s13524-013-0243-z
18.
Hu W Fang L Zhang H Ni R Pan G . Global disease burden of COPD from 1990 to 2019 and prediction of future disease burden trend in China.Public Health. (2022) 208:89–97. 10.1016/j.puhe.2022.04.015
19.
Cai L Wang X Fan L Shen J Liu Y Golden A . Socioeconomic variations in chronic obstructive pulmonary disease prevalence, diagnosis, and treatment in rural Southwest China.BMC Public Health. (2020) 20:536. 10.1186/s12889-020-08687-5
20.
Yip W Fu H Jian W Liu J Pan J Xu D et al Universal health coverage in China part 1: progress and gaps. Lancet Public Health. (2023) 8:e1025–34. 10.1016/S2468-266700254-2
21.
Liang Y Sun Y . COPD in China: current status and challenges.Arch Bronconeumol. (2022) 58:790–1. 10.1016/j.arbres.2022.04.001
22.
Zhu B Wang Y Ming J Chen W Zhang L . Disease burden of COPD in China: a systematic review.Int J Chron Obstruct Pulmon Dis. (2018) 13:1353–64. 10.2147/COPD.S161555
23.
Bai J Zhao Y Yang D Ma Y Yu C . Secular trends in chronic respiratory diseases mortality in Brazil, Russia, China, and South Africa: a comparative study across main BRICS countries from 1990 to 2019.BMC Public Health. (2022) 22:91. 10.1186/s12889-021-12484-z
24.
Cong S Yao J Fan J Wang N Wang B Bao H et al [Analysis on awareness of chronic obstructive pulmonary disease (COPD) status and related knowledge in patients with COPD in China, 2014-2015]. Zhonghua Liu Xing Bing Xue Za Zhi. (2020) 41:1034–40. 10.3760/cma.j.cn112338-20200206-00074
25.
Man W Wang S Yang H . Exploring the spatial-temporal distribution and evolution of population aging and social-economic indicators in China.BMC Public Health. (2021) 21:966. 10.1186/s12889-021-11032-z
26.
Al Wachami N Guennouni M Iderdar Y Boumendil K Arraji M Mourajid Y et al Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. (2024) 24:297. 10.1186/s12889-024-17686-9
27.
Wang N Feng Y Bao H Cong S Fan J Wang B et al [Survey of smoking prevalence in adults aged 40 years and older in China, 2014]. Zhonghua Liu Xing Bing Xue Za Zhi. (2018) 39:551–6. 10.3760/cma.j.issn.0254-6450.2018.05.003
28.
Zhao Z Zhang M Wu J Xu X Yin P Huang Z et al E-cigarette use among adults in China: findings from repeated cross-sectional surveys in 2015-16 and 2018-19. Lancet Public Health. (2020) 5:e639–49. 10.1016/S2468-266730145-6
29.
Kokturk N Kilic H Baha A Lee S Jones P . Sex difference in chronic obstructive lung disease. does it matter? A concise review.COPD. (2016) 13:799–806. 10.1080/15412555.2016.1199666
30.
Peng L Xiao S Gao W Zhou Y Zhou J Yang D et al Short-term associations between size-fractionated particulate air pollution and COPD mortality in Shanghai, China. Environ Pollut. (2020) 257:113483. 10.1016/j.envpol.2019.113483
31.
Liang C Chung H Dobson A Sandin S Weiderpass E Mishra G . Female reproductive histories and the risk of chronic obstructive pulmonary disease.Thorax. (2024) 79:508–14. 10.1136/thorax-2023-220388
32.
Reddy K Oliver B . Sexual dimorphism in chronic respiratory diseases.Cell Biosci. (2023) 13:47. 10.1186/s13578-023-00998-5
33.
Siegfried J . Sex and gender differences in lung cancer and chronic obstructive lung disease.Endocrinology. (2022) 163:bqab254. 10.1210/endocr/bqab254
34.
Schmeer C Kretz A Wengerodt D Stojiljkovic M Witte O . Dissecting aging and senescence-current concepts and open lessons.Cells. (2019) 8:1446. 10.3390/cells8111446
35.
Easter M Bollenbecker S Barnes J Krick S . Targeting aging pathways in chronic obstructive pulmonary disease.Int J Mol Sci. (2020) 21:6924. 10.3390/ijms21186924
36.
Peng X . China’s demographic history and future challenges.Science. (2011) 333:581–7. 10.1126/science.1209396
37.
Aryal S Diaz-Guzman E Mannino DM . COPD and gender differences: an update.Transl Res. (2013) 162:208–18. 10.1016/j.trsl.2013.04.003
38.
Hopkinson N Bush A Allinson J Faner R Zar H Agustí A . Early life exposures and the development of chronic obstructive pulmonary disease across the life course.Am J Respir Crit Care Med. (2024) 210:572–80. 10.1164/rccm.202402-0432PP
39.
Faner R Cho M Koppelman G Melén E Verleden S Dharmage S et al Towards early detection and disease interception of COPD across the lifespan. Eur Respir Rev. (2025) 34:240243. 10.1183/16000617.0243-2024
40.
Hopkinson NS . COPD, smoking, and social justice.Lancet Respir Med. (2022) 10:428–30. 10.1016/S2213-260000130-8
41.
Yang X Zhang T Zhang Y Chen H Sang S . Global burden of COPD attributable to ambient PM2.5 in 204 countries and territories, 1990 to 2019: a systematic analysis for the global burden of disease study 2019.Sci Total Environ. (2021) 796:148819. 10.1016/j.scitotenv.2021.148819
42.
Yin P Brauer M Cohen A Wang H Li J Burnett R et al The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990-2017: an analysis for the global burden of disease study 2017. Lancet Planet Health. (2020) 4:e386–98. 10.1016/S2542-519630161-3
43.
Eccles R . An explanation for the seasonality of acute upper respiratory tract viral infections.Acta Otolaryngol. (2002) 122:183–91. 10.1080/00016480252814207
44.
Zhao Q Guo Y Ye T Gasparrini A Tong S Overcenco A et al Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. (2021) 5:e415–25. 10.1016/S2542-519600081-4
45.
Qiu S Chen X Chen X Luo G Guo Y Bian Z et al Solid fuel use, socioeconomic indicators and risk of cardiovascular diseases and all-cause mortality: a prospective cohort study in a rural area of Sichuan. China. Int J Epidemiol. (2022) 51:501–13. 10.1093/ije/dyab191
46.
Salvi S Barnes P . Chronic obstructive pulmonary disease in non-smokers.Lancet. (2009) 374:733–43. 10.1016/S0140-673661303-9
47.
Murgia N Gambelunghe A . Occupational COPD-The most under-recognized occupational lung disease?Respirology. (2022) 27:399–410. 10.1111/resp.14272
Summary
Keywords
chronic obstructive pulmonary disease, China, incidence, prevalence, mortality, DALYs
Citation
Wang X, Liu J, Li J, Zhang L, Zeng X and Cai R (2025) Burden of chronic obstructive pulmonary disease in China from 1990 to 2021: a population-based study. Front. Med. 12:1674952. doi: 10.3389/fmed.2025.1674952
Received
28 July 2025
Accepted
06 October 2025
Published
15 October 2025
Volume
12 - 2025
Edited by
Davor Plavec, Children’s Hospital Srebrnjak, Croatia
Reviewed by
Wei Wang, Capital Medical University, China
Marija Gomerčić Palčić, Sestre Milosrdnice University Hospital Center, Croatia
Updates
Copyright
© 2025 Wang, Liu, Li, Zhang, Zeng and Cai.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruijun Cai, ruijun0311@126.com
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.