Abstract
Background:
Antimicrobial resistance (AMR) represents a significant global health threat, which is worsened by the inappropriate distribution of antibiotics without a prescription. Cultural conventions and the easy accessibility of pharmacies in Saudi Arabia further aggravate this situation. Community pharmacists play a crucial role in antimicrobial stewardship, yet they continue to face substantial challenges.
Objective:
The objective of this study was to examine the barriers and determinants that influence community pharmacists’ capability to reduce over-the-counter (OTC) antibiotic sales in the Aseer region of Saudi Arabia.
Methods:
A cross-sectional survey was conducted with 269 community pharmacists, utilizing a validated, self-administered questionnaire. Data were analyzed using descriptive statistics, Chi-square tests, Kruskal-Wallis tests, and ordinal logistic regression to assess associations between demographic characteristics and pharmacists’ views of obstacles and stewardship practices.
Results:
The type of pharmacy was significantly associated with perceived barriers (p = 0.027), with chain pharmacists reporting more challenges than independent pharmacists. Logistic regression also showed that working in a chain pharmacy (OR = 2.01) and holding a PharmD degree (OR = 1.56) were predictors of higher perceived barriers. These findings suggest that both organizational factors and educational background shape how pharmacists perceive obstacles to reducing inappropriate antibiotic dispensing. Other demographic variables lacked statistical significance.
Conclusion:
The study highlights that systemic and educational factors strongly influence pharmacists’ roles in antimicrobial stewardship. This indicates that targeted interventions such as continuous professional education, digital prescription monitoring, and stronger regulatory enforcement are necessary to support pharmacists and reduce the dispensing of inappropriate antibiotics. These measures also align with Saudi Arabia’s Vision 2030 healthcare priorities. To our knowledge, this is the first study to investigate these barriers within the Aseer region, offering novel evidence on how organizational and educational contexts shape stewardship practices. The findings provide insights that extend beyond Saudi Arabia, informing global antimicrobial resistance containment strategies.
Introduction
Antimicrobial resistance (AMR) represents a substantial worldwide health risk, compromising the effectiveness of antibiotics and elevating morbidity, mortality, and healthcare expenditures. The World Health Organization (WHO) projects that AMR may result in 10 million fatalities each year by 2050 if not addressed (25). The misuse of antibiotics, especially via over-the-counter (OTC) sales and self-medication, is a significant contributor to AMR, observed in both developed and developing countries (1). Cultural behaviors, easy access to pharmacies, and patient expectations in Saudi Arabia intensify this problem, with research indicating that 60–80% of patients request medications for viral infections (2). Community pharmacists, as primary healthcare practitioners, are crucial in managing antibiotic distribution and educating the public, but encounter substantial obstacles in reducing OTC antibiotic sales. This study examines these obstacles and determinants in the Aseer region, emphasizing the role of pharmacists in advancing Saudi Arabia’s Vision 2030–aligned healthcare reforms and national AMR containment strategies (3).
The improper distribution of antibiotics without prescriptions, commonly described as over-the-counter (OTC) antibiotic sales, is a prevalent problem in Saudi Arabia. Nafisah et al. (4) reported that 78% of pharmacists in Makkah dispensed antibiotics without prescriptions, driven by patient demand and financial incentives. Saha et al. (5) found that 65% of pharmacists experienced patient pressure to provide antibiotics, especially in chain pharmacies characterized by high customer volumes and sales targets. Another study noted that urban chain pharmacies are frequent sites for dispensing medications without prescriptions, with 45% of pharmacists attributing this practice to financial incentives (6). These behaviors contribute to the overuse of antibiotics, particularly broad-spectrum drugs, and promote the emergence of multidrug-resistant organisms (7). In 2018, the Saudi Ministry of Health (MoH) introduced a prescription-only law to curb OTC antibiotic sales, resulting in a 23.2% decrease in total antimicrobial sales and a 70% reduction in amoxicillin sales from 2017 to 2019 (7). However, sales of “Watch” medicines, including amoxicillin/clavulanic acid, increased by 6.5%, reflecting incomplete adherence and a shift toward broader-spectrum antibiotics, potentially worsening AMR (7). AlRukban et al. (8) highlighted that antibiotics are frequently dispensed in response to inappropriate requests, as only 36.7% of pharmacists consistently required valid prescriptions.
Systemic and cultural barriers hinder effective antibiotic stewardship. The lack of integrated patient tracking systems and incomplete prescription information, reported by 60% of pharmacists (5), complicates adherence to regulations. Other studies have also shown that inadequate infrastructure and weak physician–pharmacist communication undermine stewardship efforts globally (9). Culturally, self-medication is widespread in Saudi Arabia, with Al-Rasheed et al. (2) reporting that 65% of patients self-medicate due to easy accessibility and trust in pharmacists. Essack et al. (1) emphasized that community pharmacists are well-positioned to lead stewardship through patient education and enforcement of prescription policies, but they require training and systemic support. AlRukban et al. (8) found that only 19.5% of pharmacists actively counsel patients to prevent misuse; however, lack of time and limited privacy often restrict these initiatives.
The perspectives and preparedness of pharmacists regarding stewardship are essential. Saleh et al. (9) discovered that advanced training enhances adherence to antibiotic dispensing standards, especially among PharmD graduates. Haddadin et al. (6) observed a 25% decrease in non-prescribed dispensing following the 2018 regulation; however, adherence remains inconsistent due to enforcement deficiencies. Saha et al. (5) emphasized the need for compulsory AMR training to strengthen pharmacists’ contributions to public education and compliance with legislation. The 2018 rule corresponds with Vision 2030’s objective to enhance healthcare systems; nonetheless, its efficacy relies on overcoming obstacles such as patient awareness and pharmacy infrastructure (7).
Despite these regulatory advancements, existing studies in Saudi Arabia have primarily focused on antibiotic sales trends or general pharmacist practices, with limited attention to regional variations such as those in the Aseer region. Few studies have examined how systemic and cultural obstacles to antimicrobial stewardship interact with regional health reforms such as Saudi Arabia’s Vision 2030, despite the fact that international research has highlighted these obstacles. This gap restricts understanding of how community pharmacists perceive and respond to barriers under evolving regulatory and healthcare contexts. The novelty of the present study lies in its regional focus and in examining organizational and educational factors such as pharmacy type and pharmacist training that shape stewardship practices. Therefore, this study aims to investigate the specific barriers faced by community pharmacists in the Aseer region, with the hypothesis that demographic, organizational, and educational characteristics significantly influence their perceptions of obstacles to reducing inappropriate antibiotic dispensing, thereby providing evidence to support national and global AMR stewardship efforts.
Materials and methods
Study design
This research utilized a cross-sectional design, employing a questionnaire as the principal instrument for data collection. The study was conducted among community pharmacists in the Aseer region of Saudi Arabia. Participants independently completed the questionnaire, ensuring anonymity and confidentiality of responses. Participation was voluntary, and informed consent was obtained before survey initiation.
Study population
The questionnaire was distributed to 300 community pharmacists in the Aseer region using a convenience sampling approach, rather than a true randomization method, as participation depended on the pharmacists’ availability and willingness to respond. Each selected pharmacy typically employed 2–3 pharmacists working in two shifts. According to recent statistics, approximately 747 registered community pharmacists in Aseer were eligible to participate (10). The minimum sample size of 252 was estimated using a standard sample size formula based on a 95% confidence interval, a 5% margin of error, and a 50% response distribution (11). The study ultimately included 269 community pharmacists, ensuring adequate representation. The overall response rate was 89.7%, as some pharmacists declined or did not complete the survey, which may have introduced non-response bias. To minimize this risk, follow-up reminders were sent electronically during the data collection period. The inclusion criteria were licensed community pharmacists working in the Aseer region, while interns, unlicensed staff, and incomplete responses were excluded from the analysis.
Study tool and data collection
The questionnaire was developed to align with the study’s objective of exploring barriers and determinants of de-escalating over-the-counter (OTC) antibiotic sales, drawing on previous studies (1, 2, 4–9). It comprised four domains: Domain I (6 items) captured demographic characteristics, including age, gender, educational background, years of experience, pharmacy type (chain vs. independent), and location (urban vs. rural); Domain II (8 items) assessed perceptions of barriers to reducing OTC antibiotic sales, such as patient self-medication and systemic gaps; Domain III (6 items) evaluated determinants like continuous education and antimicrobial stewardship; Domain IV (6 items) explored pharmacists’ roles in AMR containment and alignment with Vision 2030. Across these domains, items were structured as a mix of Likert-scale questions (five-point), dichotomous (yes/no), and multiple-choice formats.
A pilot study was carried out involving 20 community pharmacists in Abha, Aseer, to ensure both reliability and validity. The pilot evaluated clarity, relevance, and internal consistency, yielding a Cronbach’s alpha of 0.81, indicating robust reliability. Content and face validity were confirmed by three senior pharmacy practice professionals, who reviewed the items for appropriateness and coverage. Their structured feedback was incorporated into the final version of the questionnaire. The pilot data were excluded from the final analysis.
The questionnaire was created using Google Forms and electronically disseminated to pharmacists in Abha, Khamis Mushait, and other prominent cities in Aseer from July to October 2024, which constituted the full duration of data collection for this study. Participation was optional, and pharmacists were not obligated to provide their identity or the location of their pharmacy. Inquiries regarding the survey were promptly addressed and resolved. Data confidentiality was protected via restricted access to a limited study team. Because the survey was distributed exclusively online, pharmacists without reliable internet access or adequate digital literacy may have been underrepresented. However, online dissemination was chosen for its feasibility, wide reach, and ability to maintain confidentiality. The full questionnaire is provided as a Supplementary Appendix for reference.
Statistical analysis
The completed surveys were examined for precision and completeness. Incomplete or missing responses were excluded listwise from the analysis to maintain data integrity, and sensitivity checks confirmed that excluded cases did not significantly alter overall results (12). The data were encoded and input into SPSS version 24 (IBM Corp., Armonk, NY, United States).
Descriptive statistics, encompassing frequencies and percentages, encapsulated demographic factors such as age, gender, education, pharmacy type, geography, and experience. Responses to Likert-scale items regarding barriers, determinants, and pharmacists’ roles were classified as ordinal data, with medians and interquartile ranges (IQRs) utilized to convey core tendencies and variability. Normality of continuous variables was tested using the Shapiro–Wilk test (13), and the results supported the use of non-parametric statistics for skewed data.
The Chi-Square Test (χ2) of Independence analyzed the relationships between demographic characteristics (e.g., gender, pharmacy type, location) and outcomes, such as high versus low perceived barriers or support for stewardship, with a p-value < 0.05 indicating statistical significance. The Kruskal-Wallis H Test was employed to compare views among demographic categories (e.g., age, education, experience), appropriate for non-normally distributed ordinal data. When significant differences were observed, post hoc pairwise comparisons were performed using Dunn’s test with Bonferroni correction to control for multiple testing (14).
Ordinal logistic regression determined predictors of elevated perceived barriers and diminished stewardship support, utilizing gender, age, education, pharmacy type, location, and experience as independent variables. All assumptions for ordinal regression, including proportional odds and absence of multicollinearity, were verified before analysis (15). The threshold for statistical significance was established at α < 0.05.
Ethical approval and informed consent statements
The study received approval from the Research Ethics Committee of King Khalid University (ECM# 2021-3606). Informed consent was obtained from all participants before data collection.
Results
Demographic characteristics
This research included 269 community pharmacists from the Aseer region. The predominant demographic of participants was male (64%). The majority were recently graduated, with 56% falling within the age range of 20–29 years. Pharmacists aged 30–39 represented 29.7%, and those aged 40 and older were 14.3% of the sample. Most respondents held a PharmD degree (71%), followed by bachelor’s degrees (22.3%) and postgraduate certificates (6.7%). A significant majority (89%) were employed in chain pharmacies, whereas 11% were engaged in independent community pharmacies. Seventy-nine percent of participants practiced in urban regions. Regarding professional experience, 46% had less than 5 years, 33.5% had between 6 and 10 years, and 20.5% had more than 11 years. In addition to categorical frequencies, the median age of respondents was 28 years (IQR = 25–34), and the median years of experience was 5 years (IQR = 2–9). Table 1 summarizes the demographic characteristics of participants.
Table 1
| Characteristic | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 172 | 64.0% |
| Female | 97 | 36.0% | |
| Age group (years) | 20–29 years | 151 | 56.0% |
| 30–39 years | 80 | 29.7% | |
| 40+ years | 38 | 14.3% | |
| Education level | Bachelor’s degree | 60 | 22.3% |
| PharmD | 191 | 71.0% | |
| Postgraduate degree | 18 | 6.7% | |
| Pharmacy type | Chain pharmacy | 239 | 89.0% |
| Independent pharmacy | 30 | 11.0% | |
| Location | Urban | 212 | 79.0% |
| Rural | 57 | 21.0% | |
| Years of experience | 0–5 years | 124 | 46.0% |
| 6–10 years | 90 | 33.5% | |
| 11+ years | 55 | 20.5% |
Demographic characteristics of participants (N = 269).
Summary statistics (Median, IQR): Age = 28 (25–34); Years of experience = 5 (2–9).
Perceived barriers to antibiotic stewardship
Pharmacists identified multiple barriers that hinder efforts to restrict OTC antibiotic sales. Patient demand was a major issue, with 64.3% reporting that patients often preferred antibiotics without prescriptions. Similarly, 66.5% cited the lack of rigorous prescription regulations as a challenge, and 50.6% noted social expectations for rapid access to antibiotics. Financial incentives also played a role, with 72.5% acknowledging that profit motives conflicted with stewardship practices. These findings highlight how patient expectations, weak enforcement, and financial pressures interact to perpetuate inappropriate antibiotic dispensing. Supplementary Table and Figure 1 illustrate that patient self-medication and ease of access to pharmacies were perceived as the most influential drivers of misuse.
Figure 1
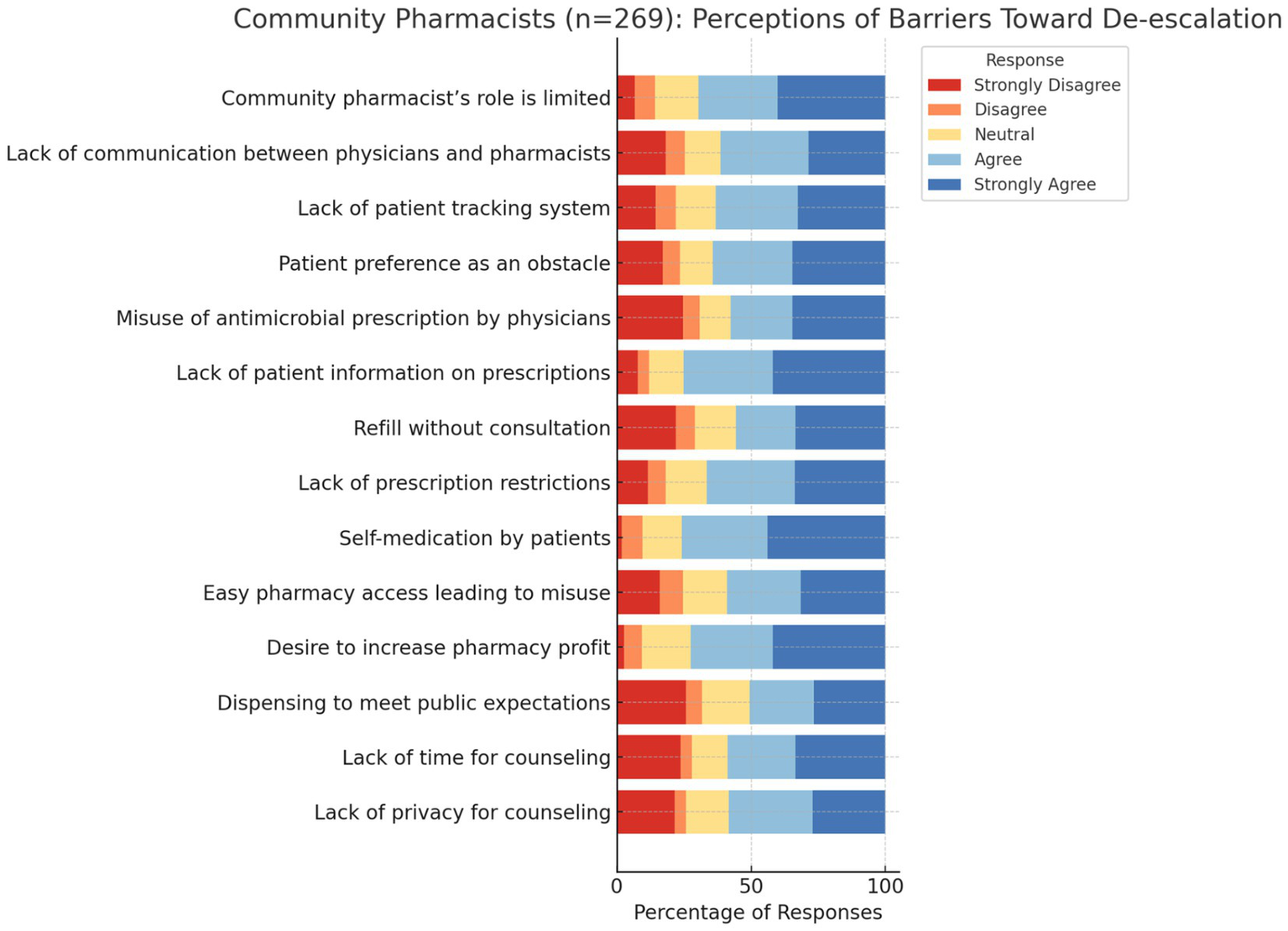
Perceived barriers to antibiotic stewardship.
Pharmacists’ perspectives on stewardship, regulations, and public awareness
Community pharmacists expressed strong support for stewardship and regulations aimed at curbing inappropriate antibiotic use. The highest consensus was observed for pharmacist involvement in stewardship programs (median = 5, IQR = 4–5). Support for Ministry of Health regulations also ranked highly (median = 4, IQR = 2–5). Continuous professional education was emphasized (median = 4, IQR = 3.0). Public awareness efforts were rated as insufficient (median = 4, IQR = 3–5), while insured patients were frequently perceived as receiving unnecessary antibiotics (median = 4, IQR = 3–5). Perspectives on primary healthcare centers were mixed (median = 3, IQR = 2–4). All IQR values were reported in Table 2.
Table 2
| Item | Median | IQR (Q1–Q3) |
|---|---|---|
| Community pharmacists need continuous education | 4 | 3–5 |
| MoH regulations beneficial | 4 | 3–5 |
| Physicians easily prescribe to insured patients | 4 | 2–5 |
| Awareness programs for the public are insufficient | 4 | 2–5 |
| Role of PHC centers needs improvement | 3 | 2–4 |
| Pharmacists should engage more in stewardship programs | 5 | 4–5 |
Pharmacists’ perspectives on stewardship, regulations, and public awareness (Median and IQR: Q1-Q3).
IQR, interquartile range (25th–75th percentile). Responses measured on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree).
Inferential analysis of demographic factors and stewardship perceptions
The Chi-square test examined associations between demographic factors and perceived barriers (Table 3). “High barriers” were defined as scores ≥ the median, while “low barriers” were scores < the median. Pharmacy type showed a statistically significant correlation with perceived barriers (χ2 = 4.89, p = 0.027), with chain pharmacists reporting greater difficulties. No significant associations were found for gender (p = 0.143) or location (p = 0.081).
Table 3
| Demographic variable | High barriers (n, %) | Low barriers (n, %) | χ2 | p-value |
|---|---|---|---|---|
| Gender | 96 (55.8%) | 76 (44.2%) | 2.14 | 0.143 |
| Pharmacy type | 152 (63.6%) | 87 (36.4%) | 4.89 | 0.027* |
| Location | 162 (76.4%) | 50 (23.6%) | 3.05 | 0.081 |
Association between demographic characteristics and perceived barriers.
* p < 0.05, statistically significant.
The Kruskal–Wallis H test compared perceptions across age, education, and experience (Table 4). Significant differences were observed among age groups (H = 6.48, p = 0.039) and educational levels (H = 4.12, p = 0.043), with younger pharmacists and PharmD graduates reporting greater awareness of barriers. Variations based on years of experience were not statistically significant (p = 0.088). Dunn’s post hoc tests with Bonferroni correction identified the specific group differences.
Table 4
| Variable | Mean rank (high barriers) | Mean rank (low barriers) | H statistic | p-value |
|---|---|---|---|---|
| Age group | 145.2 | 127.6 | 6.48 | 0.039* |
| Education level | 141.8 | 123.3 | 4.12 | 0.043* |
| Years of experience | 138.4 | 129.5 | 2.91 | 0.088 |
Comparison of perceived barriers across age, education, and experience.
* p < 0.05, statistically significant.
Regression analysis
Ordinal logistic regression identified key predictors of perceived barriers (Table 5). Pharmacists in chain pharmacies were more likely to report higher barriers (OR = 2.01, p = 0.019), and PharmD degree holders also reported greater restrictions (OR = 1.56, p = 0.041). Other demographic variables were not significant. Model diagnostics indicated acceptable fit (Hosmer–Lemeshow p > 0.05), adequate explained variance (Nagelkerke R2 = 0.21), and no evidence of multicollinearity.
Table 5
| Predictor variable | Odds ratio (OR) | 95% Confidence interval (CI) | p-value |
|---|---|---|---|
| Male gender (vs. female) | 1.24 | 0.82–1.89 | 0.308 |
| Chain pharmacy (vs. independent) | 2.01 | 1.12–3.58 | 0.019* |
| Urban location (vs. rural) | 1.43 | 0.91–2.25 | 0.120 |
| Age 30–39 (vs. 20–29) | 0.81 | 0.50–1.30 | 0.379 |
| Age 40 + (vs. 20–29) | 0.69 | 0.39–1.24 | 0.210 |
| PharmD (vs. bachelor’s) | 1.56 | 1.02–2.39 | 0.041* |
| Postgraduate (vs. bachelor’s) | 1.24 | 0.58–2.65 | 0.577 |
| Experience 6–10 years (vs. < 5 years) | 1.12 | 0.69–1.82 | 0.641 |
| Experience 11+ years (vs. < 5 years) | 0.92 | 0.51–1.68 | 0.783 |
Ordinal logistic regression predicting high perceived barriers and low stewardship support.
* p < 0.05, statistically significant.
Discussion
Antimicrobial resistance (AMR) continues to pose a global health problem, severely compromising the efficacy of current therapeutic measures. Misuse of antimicrobials, particularly the over-the-counter distribution of antibiotics, has been a principal catalyst of this problem (7, 16). Saudi Arabia has reported elevated levels of antimicrobial usage, prompting the need for regulatory measures to mitigate misuse and enhance stewardship. The implementation of the national antimicrobial prescription-only policy in 2018 marked a significant advancement in Saudi Arabia’s initiatives to address AMR. Subsequent to this policy, multiple studies demonstrated significant decreases in antibiotic sales. Alajmi et al. (7) reported a 23.2% decrease in retail antimicrobial sales from 2017 to 2019, highlighting the prompt effects of regulatory enforcement. Alzahrani et al. (16) observed a 9–10% reduction in antimicrobial usage rates in community pharmacies (7, 16).
Community pharmacists, as essential stakeholders identified by our study findings, predominantly viewed the law favorably. Alakhali et al. (17) reported that almost 90% of pharmacists agreed that implementing the prescription-only policy would help decrease inappropriate antimicrobial usage. A study by Alrasheedy et al. (18) corroborated this finding, demonstrating that the percentage of pharmacies distributing antibiotics without prescriptions dramatically decreased after the implementation of law enforcement measures (17, 18). Our own regression results support this, showing that pharmacists in chain pharmacies were twice as likely to report higher barriers (OR = 2.01, 95% CI: 1.12–3.62), while PharmD graduates were 1.56 times more likely (95% CI: 1.02–2.39) to recognize stewardship challenges compared to bachelor’s degree holders.
Despite these positive advancements, numerous difficulties persist. Full adherence to the policy has not yet been attained. Alhomoud et al. (19) discovered that antibiotics are still dispensed without prescriptions in certain community pharmacies, frequently influenced by patient requests, economic incentives, or misunderstandings about the need for medical consultations for infections. Another study identified systemic hurdles such as financial incentives, patient expectations, and inadequate regulatory enforcement as significant obstacles to complete compliance (7). Our findings confirm these challenges, with financial motives and patient pressure ranked among the highest barriers reported by pharmacists.
The policy has inadvertently altered antibiotic prescribing practices. Sales of narrow-spectrum antibiotics, such as amoxicillin, have declined, whereas broader-spectrum medicines, like amoxicillin/clavulanic acid, have had an uptick in sales (7). This tendency, albeit indicative of enhanced regulatory compliance, introduces new concerns for AMR by potentially fostering the selection of resistant species.
The intricacy of AMR mitigation is exacerbated by cultural and infrastructural elements. Raju et al. (20) indicated that hardly one-third of pharmacists consistently solicit genuine prescriptions, highlighting persistent deficiencies in practice. Cultural attitudes that endorse self-medication and reliance on pharmacists as primary providers persist in Saudi society (8, 14). Moreover, infrastructural constraints, such as the lack of integrated computerized prescribing and patient tracking systems, impede the complete achievement of stewardship objectives (5).
In response to these issues, Saudi Arabia has established an extensive National Action Plan for AMR (2022–2025), in accordance with the World Health Organization’s Global Action Plan. This approach focuses on fortifying regulatory frameworks, advancing public and professional education, improving monitoring systems, and optimizing antibiotic utilization in both human and animal health sectors (21).
Our study contributes to this context by demonstrating that organizational (pharmacy type) and educational (PharmD vs. bachelor’s) characteristics significantly influence pharmacists’ perceptions of barriers. Specifically, chain pharmacists reported higher barriers due to organizational pressures such as profit-driven business models and sales targets, while PharmD graduates—trained more extensively in stewardship—demonstrated heightened awareness of inappropriate dispensing practices. These interpretations are consistent with evidence from Saudi Arabia and the Gulf, where commercial consolidation has been linked to increased patient load and sales-driven dispensing pressures (18, 19). These findings emphasize that, beyond regulation, workplace dynamics and professional training strongly influence stewardship outcomes.
Pharmacists are particularly equipped to play a pivotal role in the efficacy of antimicrobial resistance containment efforts. Their accessibility and function as primary health advisors allow them to implement prescription rules, inform patients about the dangers of improper antibiotic usage, and advocate for safe practices (20). For pharmacists to excel in this role, continuous professional development, supportive regulatory frameworks, and incentive models that discourage profit-driven dispensing in chain settings are essential. This aligns with global evidence from systematic reviews, which demonstrate that clinical pharmacists play a central role in ASPs through prospective audit, feedback, and educational interventions, directly improving antimicrobial use and stewardship outcomes (22).
Comparisons with international studies suggest that these challenges are not unique to Saudi Arabia. For example, evidence from Egypt indicates that inappropriate antibiotic dispensing is prevalent in community pharmacies, often due to patient demand and inadequate regulation (23). In Jordan, Haddadin et al. (6) documented that nearly 40% of community pharmacies dispensed antibiotics without prescriptions, highlighting organizational and regulatory gaps. Qualitative work by Saleh et al. (23) further emphasized structural barriers, such as commercial pressures and a lack of stewardship training, as key challenges for pharmacists. A recent systematic review of pharmacist-led antimicrobial stewardship interventions in low-and middle-income countries further supports these findings, showing that organizational pressures and limited resources commonly hinder optimal stewardship, yet targeted pharmacist-driven interventions significantly improve prescribing practices (24). These parallels situate the Aseer findings within the broader LMIC and GCC context, strengthening their relevance to global AMR stewardship efforts.
Future initiatives must emphasize ongoing pharmacist education regarding antimicrobial stewardship principles, stricter enforcement of prescription regulations, the establishment of national digital prescribing systems, and public awareness campaigns designed to alter societal perceptions of antibiotics. Furthermore, comprehensive monitoring and evaluation frameworks are crucial to guarantee that regulatory interventions result in enduring behavioral modifications among both providers and patients. Community and chain pharmacies’ incentive models need to be adjusted to remove the connection between financial gain and antibiotic sales volume to specifically address structural barriers. Compulsory AMR-focused training and continuing education programs should be adapted to various qualification levels (PharmD vs. bachelor’s) in order to address educational barriers and guarantee that all pharmacists gain the skills required for stewardship. These recommendations align directly with Saudi Arabia’s Vision 2030 reforms, which place a high priority on improving primary care, digital health infrastructure, and the use of rational medicine.
This study possesses multiple shortcomings that warrant acknowledgment. A significant portion of the data concerning antimicrobial sales and pharmacist conduct was obtained via self-reported surveys, which may be influenced by social desirability bias and underreporting. Secondly, whereas national databases like IQVIA and SFDA sales statistics offer significant insights, they may not comprehensively account for informal or uncontrolled sales transpiring outside registered pharmacies. The research primarily concentrated on urban environments, which may restrict applicability to rural regions where the implementation of antimicrobial rules could vary. Moreover, the influence of external factors, including public health initiatives or seasonal fluctuations in infection rates, was not uniformly considered in the available data. Although alterations in prescribing patterns were seen, establishing causal links between policy enforcement and antimicrobial resistance trends necessitates additional longitudinal and microbiological surveillance to provide more robust evidence. These constraints underscore the necessity for more thorough and methodical research in subsequent assessments. Ultimately, the higher proportion of chain pharmacy participants reflects the actual distribution in urban areas of Aseer, where chains dominate due to commercial consolidation. Stratified sampling was not applied due to resource constraints, though future studies should ensure proportional representation of independent pharmacies to enhance generalizability. Therefore, sampling bias due to overrepresentation of chain pharmacies may limit generalizability, especially for rural or independent pharmacy perspectives.
Conclusion
Antimicrobial resistance (AMR) represents an evolving risk to public health worldwide and in Saudi Arabia. This study is the first to explore barriers to the de-escalation of over-the-counter antibiotic sales in the Aseer region, providing novel regional insights into organizational and educational determinants of stewardship. Although many advancements have occurred since the implementation of the 2018 prescription-only policy, significant obstacles persist. Community pharmacists are essential in implementing antimicrobial stewardship; nevertheless, they face systemic obstacles such as patient expectations, commercial pressures, and insufficient regulatory support. Our findings demonstrate that PharmD graduates, due to their stronger stewardship training, reported greater awareness of barriers, while chain pharmacists perceived more challenges, likely reflecting higher patient volumes and profit-driven sales models.
The results underscore that, in addition to legal enforcement, a comprehensive strategy is essential. Practical next steps include mandatory AMR-focused continuing education for pharmacists, stricter enforcement of prescription-only dispensing laws, integration of national digital prescription monitoring systems, and restructuring of financial incentives in pharmacies to prioritize stewardship over sales. Enhanced coordination between pharmacists and physicians and targeted public awareness campaigns are also necessary to reduce self-medication behaviors.
These policy-level recommendations directly align with Saudi Arabia’s National Action Plan for AMR (2022–2025) and Vision 2030 healthcare reforms, particularly in strengthening primary care, expanding digital health infrastructure, and promoting rational medicine use. Future initiatives must also prioritize the enhancement of rural healthcare infrastructure to ensure equitable implementation across diverse settings. Policymakers can convert regulatory frameworks into long-lasting behavioral change by addressing both structural and educational barriers. Policymakers, healthcare professionals, and the general public can work together to make sustainable, measurable progress in reducing the misuse of antibiotics and preserving their efficacy for future generations.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Research Ethical Committee at King Khalid University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SA: Conceptualization, Funding acquisition, Investigation, Resources, Writing – original draft, Writing – review & editing. SS: Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors extend their appreciation to the Deanship of Research and Graduate Studies at King Khalid University for funding this work through the Large Research Project under grant number RGP2/82/46.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. Article language polishing and proofreading.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Essack SY Desta AT Abotsi RE Agoba EE . Antimicrobial resistance in the WHO African region: current status and roadmap for action. J Public Health. (2017) 39:8–13. doi: 10.1093/pubmed/fdw015
2.
Al Rasheed A Yagoub U Alkhashan H Abdelhay O Alawwad A Al Aboud A et al . Prevalence and predictors of self-medication with antibiotics in Al Wazarat health Center, Riyadh City, KSA. Biomed Res Int. (2016) 2016:1–8. doi: 10.1155/2016/3916874
3.
Alsowaida YS Thabit AK Almangour TA Saleh KB Mahrous A Almutairi MS et al . Infectious diseases pharmacy practice, education, and research in Saudi Arabia: a review and future perspectives by the infectious diseases pharmacy specialty network at the Saudi Society of Clinical Pharmacy. Saudi Pharm J. (2022) 30:1836–43. doi: 10.1016/j.jsps.2022.10.014
4.
Nafisah SB Nafesa SB Alamery AH Alhumaid MA AlMuhaidib HM Al-Eidan FA . Over-the-counter antibiotics in Saudi Arabia, an urgent call for policy makers. J Infect Public Health. (2017) 10:522–6. doi: 10.1016/j.jiph.2016.09.016
5.
Saha SK Barton C Promite S Mazza D . Knowledge, perceptions and practices of community pharmacists towards antimicrobial stewardship: a systematic scoping review. Antibiotics. (2019) 8:263. doi: 10.3390/antibiotics8040263
6.
Haddadin RN Alsous M Wazaify M Tahaineh L . Evaluation of antibiotic dispensing practice in community pharmacies in Jordan: a cross sectional study. PLoS One. (2019) 14:e0216115. doi: 10.1371/journal.pone.0216115
7.
Alajmi AM Alamoudi AA Halwani AA Almangour TA Almozain NH Al-Jedai A et al . Antimicrobial resistance awareness, antibiotics prescription errors and dispensing patterns by community pharmacists in Saudi Arabia. J Infect Public Health. (2023) 16:34–41. doi: 10.1016/j.jiph.2022.11.026
8.
AlRukban M AlRuthia Y Almasaoud M Al-Owairdhi M Alsouan A Alrabiah A et al . Community pharmacists’ views of the enforced antibiotics dispensing law and its impact on oral antibiotics sales in Saudi Arabia. Risk Manag Healthc Policy. (2020) 13:2899–907. doi: 10.2147/RMHP.S278404
9.
Saleh D Abu Farha R Alefishat E . Impact of educational intervention to promote Jordanian community pharmacists’ knowledge and perception towards antimicrobial stewardship: pre-post interventional study. Infect Drug Resist. (2021) 14:3019–27. doi: 10.2147/IDR.S324865
10.
Alshahrani SM Orayj K Alqahtani AM Algahtany MA . Community pharmacists’ perceptions towards the misuse and abuse of pregabalin: a cross-sectional study from aseer region, Saudi Arabia. Healthcare. (2021) 9:1281. doi: 10.3390/healthcare9101281
11.
Kadam P Bhalerao S . Sample size calculation. Int J Ayurveda Res. (2010) 1:55–7. doi: 10.4103/0974-7788.59946
12.
Acock AC . Working with missing values. J Marriage Fam. (2005) 67:1012–28. doi: 10.1111/j.1741-3737.2005.00191.x
13.
Shapiro SS Wilk MB . An analysis of variance test for normality (complete samples). Biometrika. (1965) 52:591–611. doi: 10.1093/biomet/52.3-4.591
14.
Dunn OJ . Multiple comparisons using rank sums. Technometrics. (1964) 6:241–52. doi: 10.1080/00401706.1964.10490181
15.
Steyerberg EW Harrell FE . Regression modeling strategies: With applications, to linear models, logistic and ordinal regression, and survival analysis. Heidelberg: Springer (2016).
16.
Alzahrani KO Alshahrani SM Alajel SM . Evaluating the effectiveness of the Ministry of Health restriction policy on seasonal antibiotic consumption trends in Saudi Arabia, 2016–2020. Front Pharmacol. (2023) 14:1242087. doi: 10.3389/fphar.2023.1242087
17.
Alakhali KM . Attitudes and perceptions of community pharmacists to antibiotic dispensing and microbial resistance. A study in Aseer region, Kingdom of Saudi Arabia. King Khalid Univ J Health Sci. (2016) 1:6–11. doi: 10.4103/1658-743X.291745
18.
Alrasheedy AA Alsalloum MA Almuqbil FA Almuzaini MA Aba Alkhayl BS Albishri AS et al . The impact of law enforcement on dispensing antibiotics without prescription: a multi-methods study from Saudi Arabia. Expert Rev Anti-Infect Ther. (2020) 18:87–97. doi: 10.1080/14787210.2020.1705156
19.
Alhomoud F Aljamea Z Almahasnah R Alkhalifah K Basalelah L Alhomoud FK . Self-medication and self-prescription with antibiotics in the Middle East—do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. (2017) 57:3–12. doi: 10.1016/j.ijid.2017.01.014
20.
Raju R Srinivas SC Siddalingegowda SM Vaidya R Gharat M Kumar TP . Community pharmacists as antimicrobial resistance stewards: a narrative review on their contributions and challenges in low-and middle-income countries. J Pharm Pharm Sci. (2024) 27:12721. doi: 10.3389/jpps.2024.12721
21.
World Health Organization, World Organization for Animal Health, UN Environment . Antimicrobial Resistance Multi-Partner Trust Fund annual report 2021: Annual report 2023. Geneva, Switzerland: World Health Organization (2022).
22.
Dighriri IM Alnomci BA Aljahdali MM Althagafi HS Almatrafi RM Altwairqi WG et al . The role of clinical pharmacists in antimicrobial stewardship programs (ASPs): a systematic review. Cureus. (2023) 15:151. doi: 10.7759/cureus.50151
23.
Sabry NA Farid SF Dawoud DM . Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Soc Adm Pharm. (2014) 10:168–84. doi: 10.1016/j.sapharm.2013.03.004
24.
Marins TA de Jesus GR Holubar M Salinas JL Guglielmi GP Lin V et al . Evaluation of interventions led by pharmacists in antimicrobial stewardship programs in low-and middle-income countries: a systematic literature review. Antimicrob Steward Healthc Epidemiol. (2024) 4:e198. doi: 10.1017/ash.2024.342
25.
WHO . UN Interagency Coordination Group on Antimicrobial Resistance presents its report to the UN SG. Who.int. (2019). Available at: https://www.who.int/news/item/28-04-2019-un-interagency-coordination-group-on-antimicrobialresistance-presents-its-report-to-the-un-sg (Accessed September 15, 2025).
Summary
Keywords
antimicrobial stewardship, antimicrobial resistance (AMR), over-the-counter antibiotics, community pharmacists, pharmacy practice, de-escalation, barriers
Citation
Alshahrani SM and Shaik Alavudeen S (2025) Barriers and determinants of over-the-counter antibiotic sales de-escalation: perspectives of community pharmacists in Aseer, Saudi Arabia. Front. Med. 12:1677246. doi: 10.3389/fmed.2025.1677246
Received
31 July 2025
Accepted
12 September 2025
Published
22 September 2025
Volume
12 - 2025
Edited by
Muhammad Hashim Ghouri, University Institute of Physical Therapy (UIPT) at The University of Lahore, Pakistan
Reviewed by
Akhtar Rasul, Government College University, Faisalabad, Pakistan
Hafiza Sana Ashraf, The University of Lahore, Pakistan
Javid Iqbal Mir, Moderna Inc, United States
Updates
Copyright
© 2025 Alshahrani and Shaik Alavudeen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sultan M. Alshahrani, shahrani@kku.edu.sa
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.