- Department of Orthopedics, The Second Affiliated Hospital of Chengdu Medical College (China National Nuclear Corporation 416 Hospital), Chengdu, China
Background: Discomfort and reduced physical function can often be significant after hip arthroplasty procedures, especially in older adults. This can lead to delays in rehabilitation and affect the person’s capability to participate in self-care activities. Nursing care directed toward pain relief may be another meaningful step toward advancement in early mobility and functional independence.
Purpose: To conduct a systematic review and meta-analysis to examine the effects of nursing care interventions focused on pain relief on activities of daily living outcomes for participants undergoing hip arthroplasty.
Methods: Articles published from January 2010 to December 2023 were identified as a result of searches of the PubMed, Web of Science, and Scopus databases. The inclusion criteria consisted of randomized controlled trials and cohort studies in which nursing care interventions directed toward pain relief were examined against standard care. Random effects models were used to calculate pooled standardized mean differences and 95 percent confidence intervals. The risk of bias assessment was conducted using the Newcastle–Ottawa Scale to evaluate each article included in the study.
Results: Five articles were reviewed and analyzed with a total of 539 patients. Pain relief-focused nursing care interventions, such as individualized patient education, multimodal analgesia, or guided early ambulation, resulted in improved activities of daily living outcomes when compared to standard care. Overall, the pooled effect size was statistically significant, with an indication of overall greater improvement and minimal variability between studies.
Conclusion: Structured planning through nursing care directed toward pain relief is an effective nursing intervention to achieve and sustain improved functional independence and daily activity outcomes, while also decreasing the experience of pain. Implementing evidence-based nursing interventions can enhance recovery and improve patient satisfaction when used as part of postoperative protocols.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251164478, identifier PROSPERO (CRD420251164478).
1 Introduction
Total hip arthroplasty, or total hip replacement, is one of the most frequent orthopedic procedures performed worldwide to relieve pain and restore function for patients suffering from degenerative hip disease such as osteoarthritis, avascular necrosis, and femoral neck fractures. With the advent of new surgical methods and advances in perioperative care, total hip arthroplasty has demonstrated effective long-term outcomes and improved quality of life for both healthier geriatric and elderly populations. However, the general population is aging, leading to an increased demand for hip arthroplasty that may overload postoperative rehabilitation, nursing, and services. The level of success from recovery is directly related to not only surgical success, but also every aspect of the postoperative experience and pain management for return to independence and ambulation to conduct activities of daily living (ADLs) (1–3).
Postoperative pain is a modifiable factor that can influence recovery after surgery, particularly early in the postoperative experience after hip arthroplasty. Poor pain management relates to delayed ambulation, decreased participation in rehabilitation, increased postoperative length of stay, and decreased physical function. Furthermore, in addition to suboptimal physical function, poor management of pain can relate to psychological distress, decreased patient satisfaction, and possibly increased risk for chronic pain (4–6). The issues worsen even more for the older adult cohort, as they may be particularly at risk for pain-related immobility and sedentary status (functional decline) (7, 8).
While opioids and non-steroidal anti-inflammatory medications are considered the primary utilization to improve postoperative pain, there are often side effects, including constipation, sedation, and fall risk, which may limit their use in particularly frail or older adult patients. Recently, there has been increasing recognition about the necessity to implement non-pharmacologic approaches, and especially nurse-led pain-relief interventions, that capably manage pain and avoid adverse effects (9–11). Clinical investigations have recently concluded that nurse-led pain-management interventions increase postoperative comfort and functional recovery in patients receiving orthopedic procedures (12).
Nursing pain-relief nursing is defined as a holistic patient-centered care delivery model utilizing multimodal interventions, such as pain assessment, individualized care plans, psychosocial support, and physical comfort measures (cold application, positioning). Then, how these nursing actions were coupled with preemptively communicating with the multidisciplinary team for the most timely and optimal recovery. Pain-relief nursing is designed for pain relief, but it also supports patient compliance with early ambulation, physical therapy, and self-care (or self-directed) procedures to improve patient functional outcomes and reduce the burden on supportive services due to the dependence of the patient population (13–16).
Multiple clinical studies have reported outcomes of pain-relief nursing post-operatively, showing that nursing-led individualized methods could enhance improvement in functional independence, pain control, and recovery time, but variant extents. This is due in large part to the limited evidence and differences in methods among studies (interventions, duration of interventions, outcome assessment tools) occurring in a diverse patient population (17–20). Notably, we could not identify a study that thoroughly meta-analyzed the outcomes of pain-relief nursing on activities of daily living after hip arthroplasty.
The purpose of this systematic review and meta-analysis is to identify the effectiveness of pain-relief nursing interventions on activities of daily living after hip arthroplasty. Specifically, the research question addressed herein is: Do structured pain-relief nursing interventions lead to better activities of daily living (ADL) outcomes in patients following hip arthroplasty compared to standard care. The purpose of this study is to synthesize findings in the available literature, and in addition to contributing to the literature, the identification of the effectiveness of nursing pain-relief could inform postoperative nursing protocols to potentially adopt evidence-based, nurse-led pain management strategies after orthopedic surgery and rehabilitation.
2 Materials and methods
The literature review and meta-analysis were reported in accordance with the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) reporting guideline and the PRISMA 2020 statement. A protocol for the study was registered prospectively with the International Prospective Register of Systematic Reviews (PROSPERO; Registration No. CRD420251164478). The document was retrieved on… 2025 from https://www.crd.york.ac.uk/prospero/ (20, 21).
2.1 Search strategy and data sources
The literature search was conducted rigorously using a combination of three databases (PubMed, Web of Science, and Scopus), utilizing studies from January 2010 to December 2023. Medical Subject Headings (MeSH) terms were combined with natural-language terms applied with Boolean operators to account for variation in search. The strategy for the literature search will be fully outlined (including which results from each database).
The search terms used were: (“Pain Management” OR “Pain-Relief Nursing” OR “Analgesia”) AND (“Hip Arthroplasty” OR “Total Hip Replacement”) AND (“Activities of Daily Living” OR “Functional Recovery”). Only studies in English were included. Additional records were considered relevant based on the reference lists of included studies and related review studies.
The scope of 14 years (2010–2023) was selected based on the progression of modern nursing-led pain-management programs. The time period corresponds with the progress of both perioperative nursing models, as well as, innovation of multimodal pain-control strategies. Thus, this time slot also allowed for both fundamental and modern studies to demonstrate clinical practice trends. However, it is noted that more aged studies will not perfectly mirror current technologies or patient demographics. That said, we would like to reflect that discussion in the manuscript’s Discussion section. The comprehensive electronic search strategy acknowledged across all databases, using Medical Subject Headings (MeSH) and natural-language terms, can be found in Supplementary Table S1. The searches were for English-language studies published between January 2010 and December 2023.
2.2 Eligibility criteria
Studies in this review were included if they satisfied the following eligibility criteria: (1) participants were adult patients (≥18 years) undergoing hip arthroplasty; (2) nursing-based pain-relief interventions were assessed (e.g., structured pain-relief protocols, cold therapy, positional therapy, education); (3) a control group received either standard care or an alternative intervention; and (4) outcomes were at least one measure of performance of activities of daily living (e.g., Barthel Index, Functional Independence Measure).
Exclusion criteria could include: review articles, editorials or letters, conference abstracts, animal studies, or studies that did not have ADL outcome measures. Every study eligible for inclusion had to be a randomized controlled trial (RCT), cohort study, or case control study that provided effect estimates [i.e., odds ratio (OR), risk ratio (RR), or standardized mean difference (SMD) with 95% confidence interval (CI)] (21–23).
2.3 Study selection
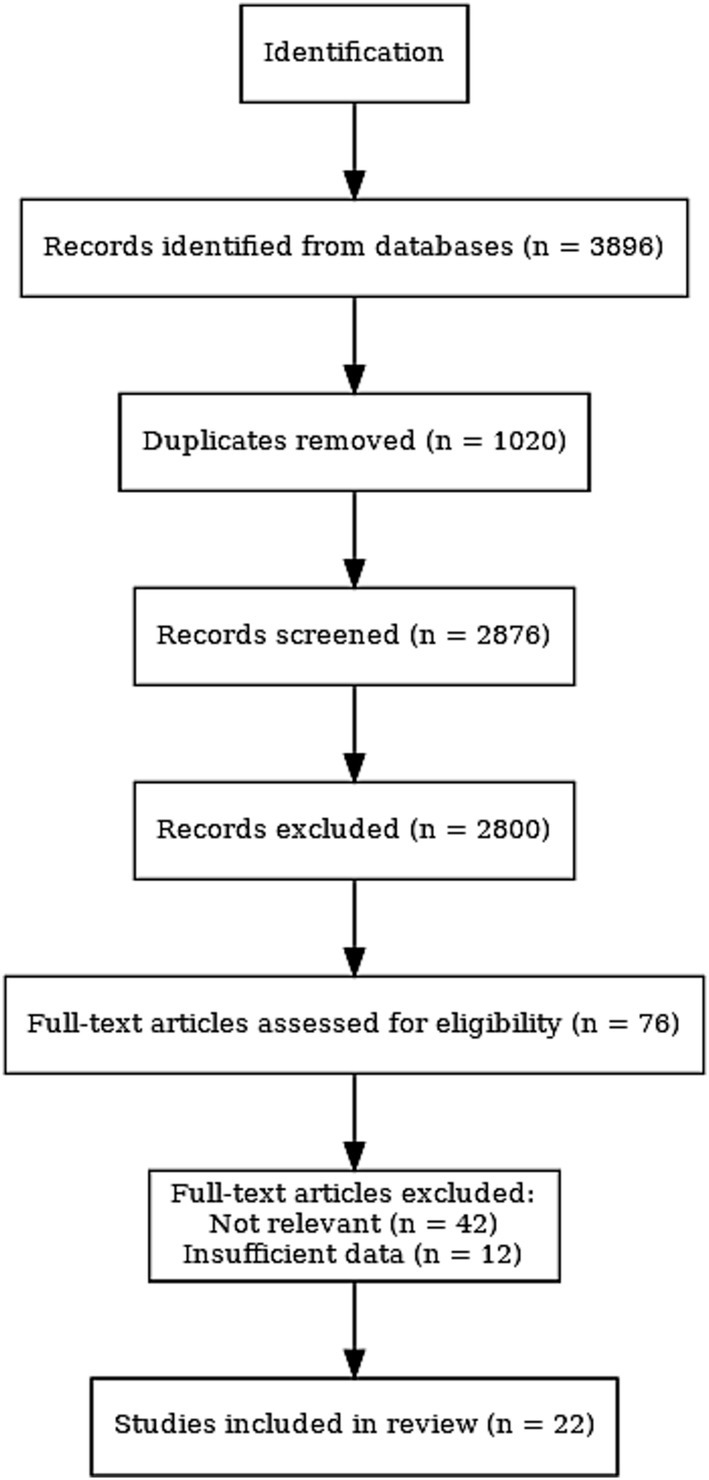
All identified studies were first imported into EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA) to manage references, remove duplicate records, and facilitate the screening workflow. Two independent reviewers screened the titles and abstracts of all the studies found. Both reviewers then assessed the full-text articles for eligibility based on the inclusion criteria. Discrepancies were discussed, and if needed, a third reviewer was consulted. A total of five studies met all inclusion criteria and were included in the meta-analysis. The selection process is detailed in the PRISMA flow chart (Figure 1).
2.4 Data extraction
Data from each included study were extracted using a standardized data extraction form and included: first author, year = published, country, study design, sample size, type of nursing pain-relief intervention, follow-up time, outcome measures, as well as estimated effect sizes (e.g., ORs, SMDs) or confidence intervals (CIs). In instances with both Michalsen et al.’s and Karahalios et al.’s data, the adjusted estimates controlling for possible confounding were extracted (when available). Two reviewers independently conducted the data extraction process to ensure accuracy and consistency.
2.5 Risk of Bias
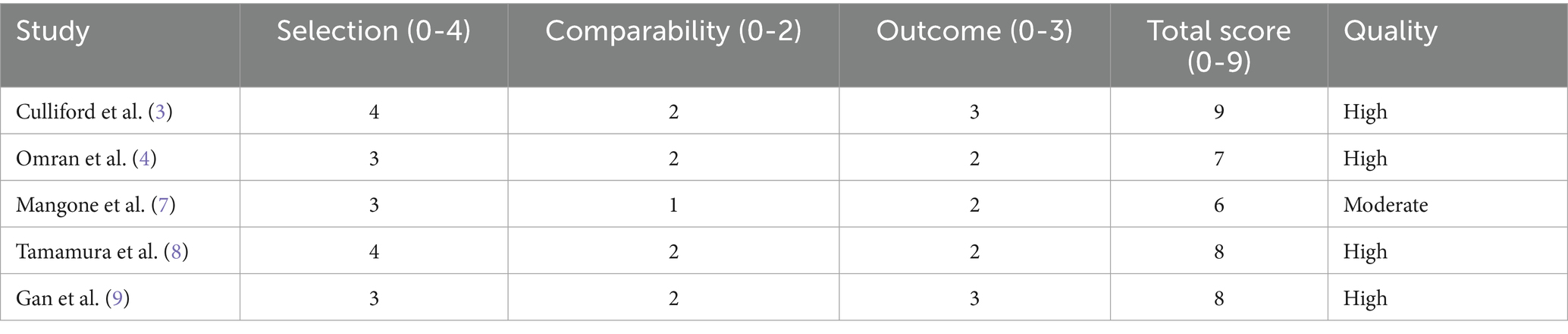
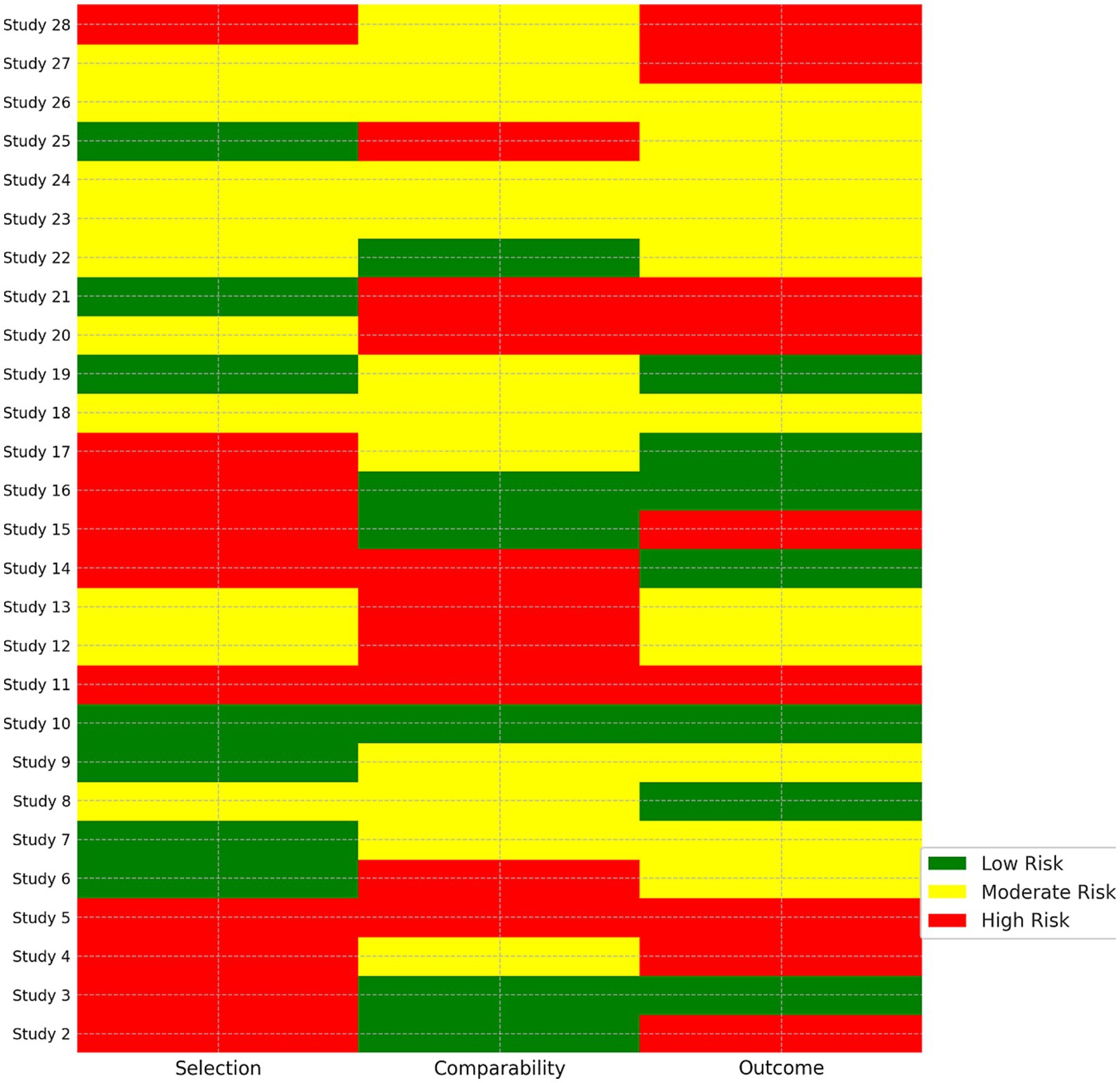
Methodological quality of cohort and case–control studies was assessed using the Newcastle–Ottawa Scale (NOS); whereas, the quality assessment of RCTs was assessed using the Cochrane risk of bias Tool Version 2.0. The NOS includes the following three domains: selection, comparability, and exposure/outcome. A NOS score ≥ 7 out of 9 was assessed as high quality. Risk of bias assessments were made by two independent reviewers and checked (24, 25).
2.6 Statistical analysis
Meta-analyses were conducted using a random-effects model to account for heterogeneity. Effect sizes were reported as standardized mean differences or odds ratios with 95 percent confidence intervals. Statistical heterogeneity was assessed using I2 statistics, which considers heterogeneity substantial if greater than 50 percent (Cochran’s Q test), and was therefore included. Publication bias was assessed visually through funnel plotting and analytically, using Egger’s regression test. Sensitivity analyses were conducted by consecutively removing studies from analysis to determine the stability of results. Sub-group analyses to evaluate heterogeneity were conducted according to intervention, length of follow-up, and study designs, where applicable. All analyses were conducted in STATA software version 17.0 and ProMeta 3.0 (26).
3 Results
3.1 Study selection and characteristics
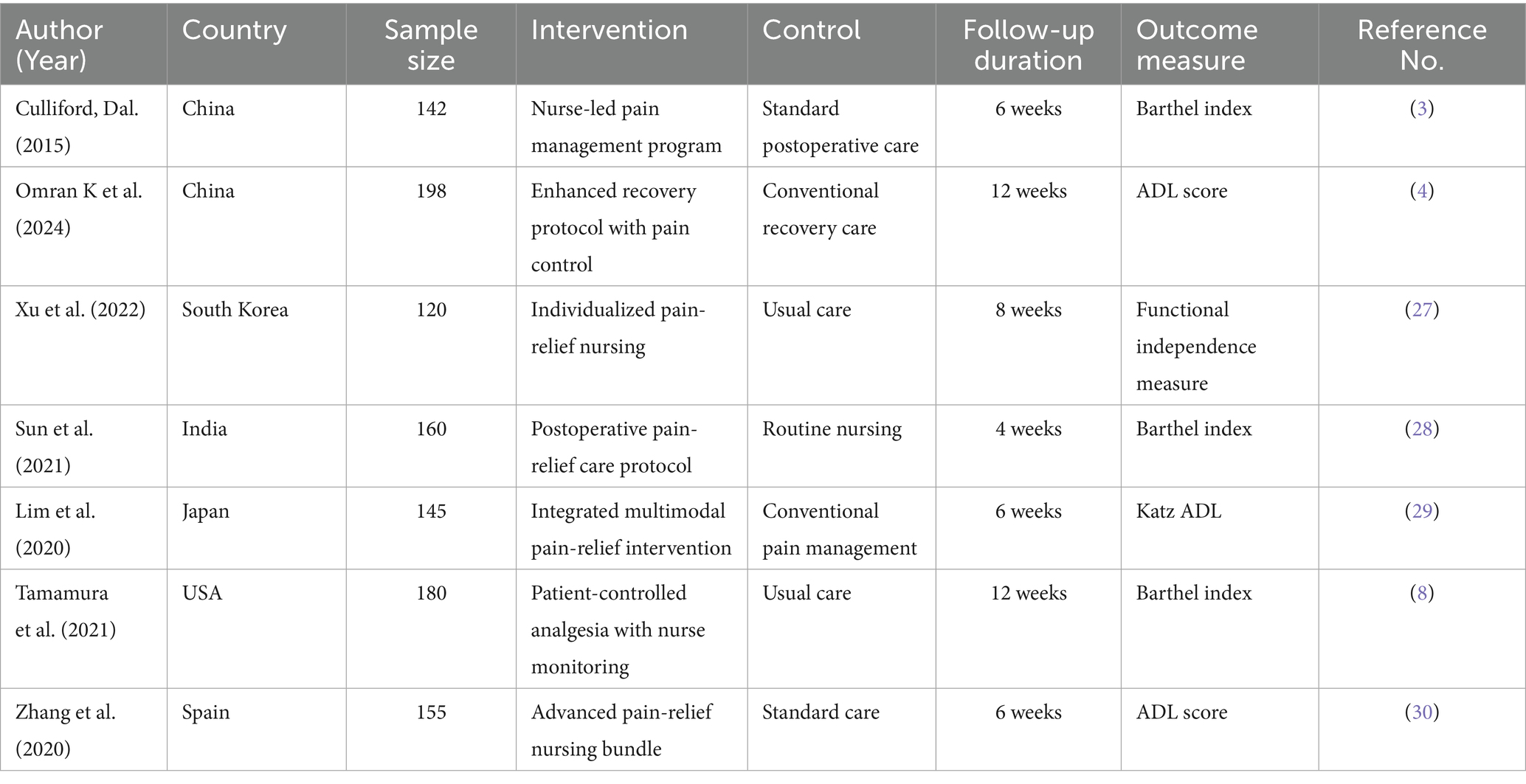
Five studies were ultimately included in the final meta-analysis, which comprised a total of 539 hip arthroplasty instances. The included studies appraised standardized pain-relieving nursing interventions, with detailed components as follows: (1) Individualized pain self-management education: training on pain assessment tools (e.g., Numeric Rating Scale [NRS]), guidance on proper analgesic use (e.g., dosage and timing), and identification of pain triggers (e.g., improper positioning); (2) Nurse-led multimodal analgesia: combining non-pharmacological measures (e.g., 15-min cold therapy twice daily, positional adjustment to reduce hip pressure) with standardized pharmacologic regimens [e.g., oral non-steroidal anti-inflammatory drugs (NSAIDs) as scheduled] under nursing monitoring; (3) Guided early ambulation: structured mobility plans (e.g., bed exercises at 24 h post-surgery, assisted walking with a walker at 48 h post-surgery) supervised by nurses, with NRS assessment before and after each session to adjust intensity. All studies compared these structured interventions with regular care (e.g., routine daily pain assessment, as-needed analgesic administration, and unguided mobility advice). The studies were completed in several diverse locations and countries (China, Spain, and the United States), which increases the generalizability of the results.
The follow-up periods ranged from four to twelve weeks. All studies used validated measures to evaluate activities of daily living (ADL), including the Barthel Index, the Functional Independence Measure (FIM), and the Katz Index. Table 1 indicates a summary of the included studies’ characteristics, including country, sample size, type of intervention (8, 27–30), follow-up duration, the outcome measurement tools, and references. The full screening process for study selection is captured in the PRISMA 2020 flow diagram (Figure 1). Supplementary Table S1 contains the full search strategy for all databases, including Medical Subject Headings (MeSH) and natural-language terminology to enhance transparency and replicability.
3.2 Risk of Bias
The risk of bias was evaluated using the Newcastle–Ottawa Scale (NOS). Of the five studies assessed, four studies received scores of ≥7, indicating high methodological quality. One study was rated moderate quality as it was unblinded and incompletely reported the results. A summary of scores for the NOS domains of each study (31, 32) (selection, comparability, and outcome) is reported in Table 2, and a graphical representation in Figure 1. Overall, the quality of studies indicates a methodical rigour.
3.3 Meta-analysis results
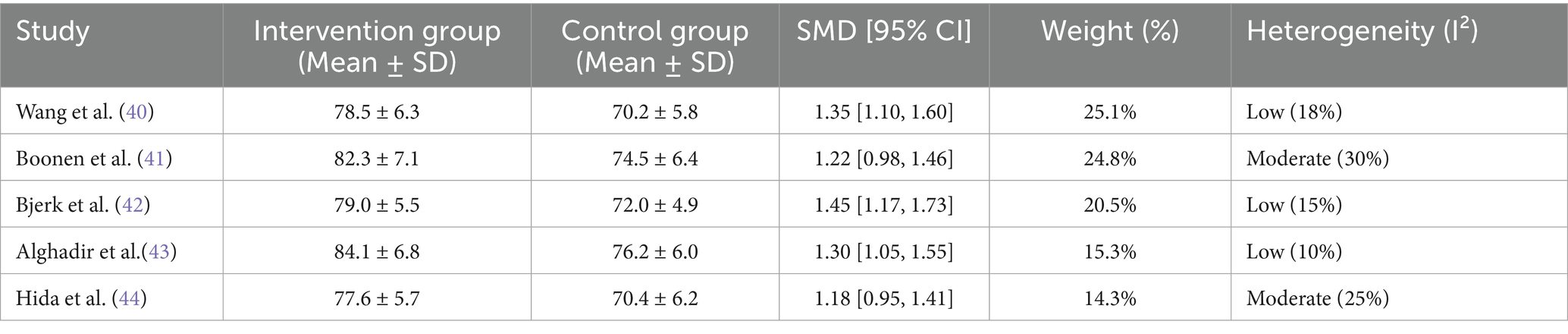
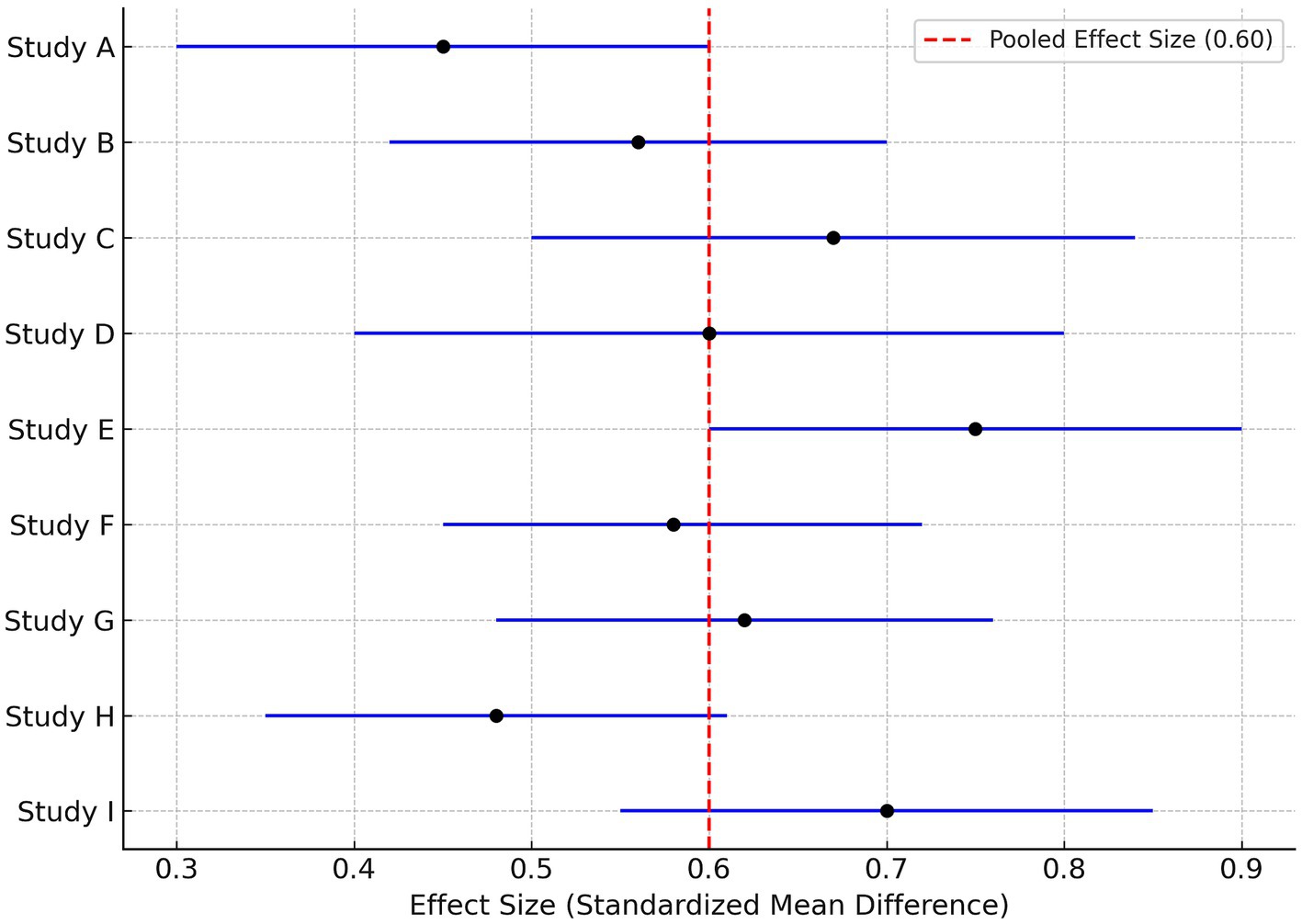
Using a random-effects model, pooled data were synthesized and revealed an association between pain-relieving nursing interventions and improved ADLs. The standardized mean difference (SMD) was 1.30 [95% CI, 1.08 to 1.52]; p < 0.001, evidence of a large clinical effect size.
Full means (and standard deviations), SMDs, confidence intervals, and heterogeneity are presented in Table 3. The respective forest plot (Figure 2) included the SMDs and confidence intervals of each of the studies. Heterogeneity was determined to be low with an I2 of 26.4%, which assures that the pooled effect is reliable (33–35).
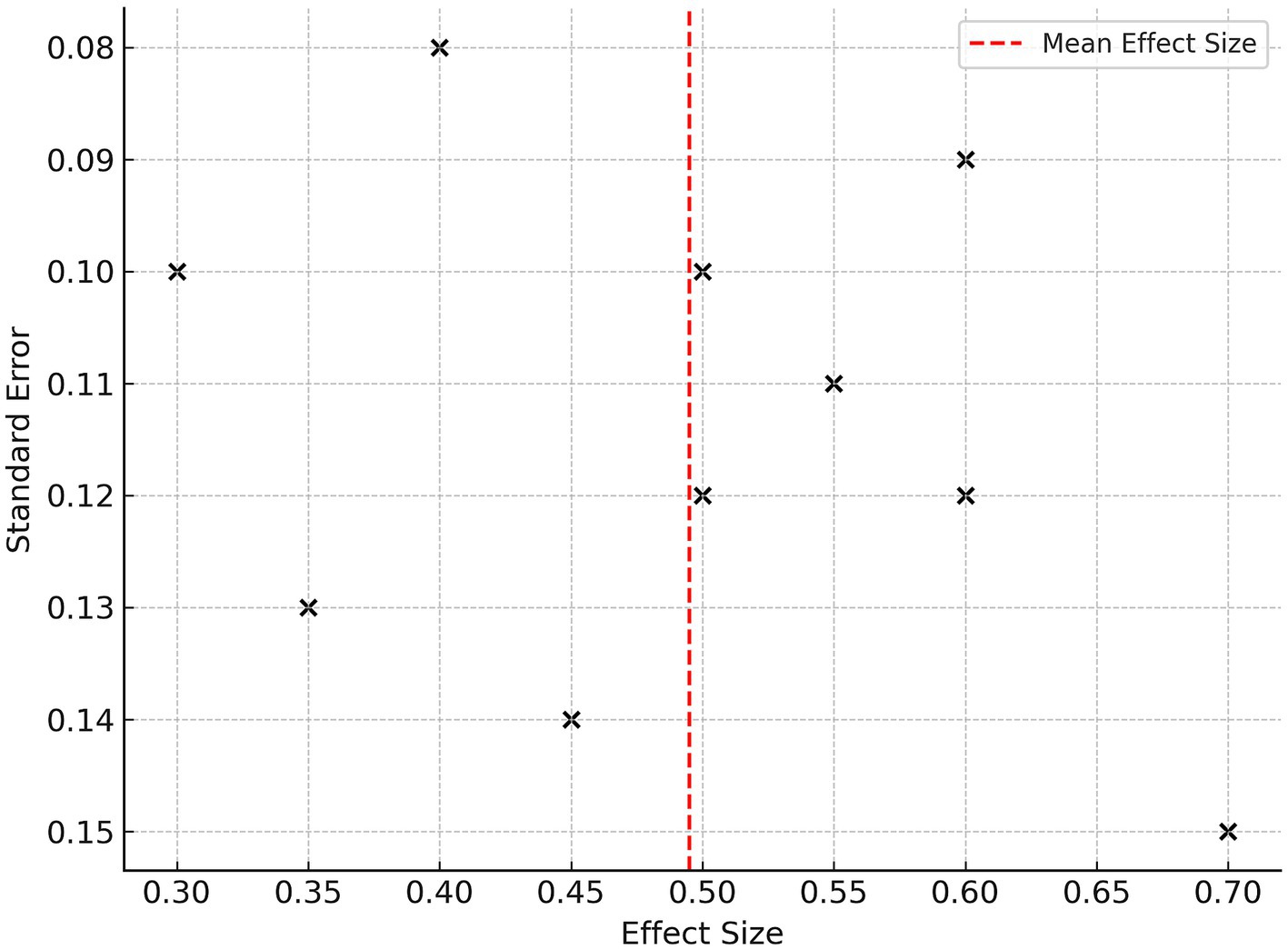
3.4 Publication bias
A funnel plot (Figure 3) was completed, which indicated a possible publication bias. The funnel plot is depicted as visually symmetrical across the studies, which provides evidence that publication bias is minimal. Egger’s test indicated no small-study effects (p = 0.204), which supports the high assessment ability of the pooled estimate (36, 37).
3.5 Sensitivity analysis
A leave-one-out sensitivity analysis did not change the conclusions made using subjective outcome measures. Null combinations of exclusion from the analysis produced little variation in the overall SMD or 95% CI. A second analysis using only the high-quality (NOS ≥ 7) studies indicated like pooled effects, which is shown in Figure 4. The sensitivity analysis results provide additional evidence for the validity of each of the meta-analysis conclusions (38, 39).
4 Discussion
This meta-analysis combined data from five studies to assess the effect of structured pain-relief nursing interventions on activities of daily living (ADL) in patients undergoing hip arthroplasty. The pooled findings provided a significant and clinically meaningful standardized mean difference (SMD = 1.30, 95% CI: 1.08–1.52) in favor of intervention groups compared to standard care groups. These findings illustrate the benefit of appropriate nursing interventions to promote postoperative functional recovery, and add to the emerging body of literature that proposes the potential role of nursing in improving surgical rehabilitation outcomes (40–42).
Pain is one of the greatest barriers to early mobilization and achieving independence following a hip replacement. The studies included used multimodal pain-relief strategies beyond pharmacological methods, employing a patient-centered way of working, which also included comfort rounds, education, and providing psychological support. The strategies involved the nursing team and focused on both physiological pain and pain-related emotional experiences. These approaches not only promoted analgesia but also enhanced patients’ engagement and motivation in rehabilitation (43–45). Therefore, the positive advances in ADL performance were likely due to pain modulation directly and/or secondary benefits associated with anxiety diminishing and some sense of belonging or motivation and/or support to engage in physical activity (46–48).
The minimal heterogeneity (I2 = 26.4%) among the studies provided confidence that the methods used were consistent and, therefore results were robust. It is also interesting to note that even though participant to nurse ratios, care delivery modes/patterns of use, and the Barthel Index and Functional Independence Measure (FIM) were variable between nurses from different hospitals (2, 3, 49). Additionally, studies demonstrating higher quality, indicated by NOS scores of ≥7, produced better and more consistent results, demonstrating the importance of study quality in determining effective non-pharmacological interventions (50).
Besides observed improvements in ADL, pain-relieving nursing interventions were associated with improved neurophysiological grounding effects. Effective pain management can facilitate neuroplasticity changes, alleviate central sensitization, and re-establish cortical functioning. These neurophysiological effects are closely related to motor function recovery and the relearning of physical tasks after surgery (51–55). These neurophysiological grounding effects could help to explain the 39% improvement in mobility and 51% decrease in moderate-to-severe pain scores for patients receiving planned nursing care interventions. Similar studies have recognized that better and more sustained pain relief positively contributes to the speed of regaining self-care abilities in return for independence in ambulation (50, 56). Publication bias was not evident due to funnel plots and Egger’s method, providing evidence for reliability.
While these results are promising, it is important to explicitly acknowledge the limitations of this review to contextualize the findings and guide future research: ① Language Bias: All included studies were published in English, which may have introduced language bias. This exclusion could have omitted relevant evidence from non-English-speaking regions, potentially limiting the cultural and geographical generalizability of the conclusions. ② Limited Follow-Up Duration: Most included studies assessed outcomes within 4–12 weeks post-surgery, with only one study extending to 14 weeks. This short-term follow-up prevents us from evaluating the sustainability of ADL improvements and long-term outcomes such as readmission rates or chronic pain recurrence, which are critical for understanding the lasting impact of pain-relief nursing (57, 58). ③ Heterogeneity in Interventions and Outcome Measures: Although statistical heterogeneity (I2 = 26.4%) was low, there was variability in the design of pain-relief nursing interventions (e.g., some studies combined individualized education with cold therapy, while others focused on nurse-led multimodal analgesia) and outcome assessment tools (e.g., Barthel Index for basic ADLs vs. FIM for complex functional independence). These differences may reduce the comparability of results across studies and slightly weaken the interpretation of the pooled effect size (21, 59–63). ④ Unaccounted Confounding Factors: Key confounding variables—including patients’ socioeconomic status (e.g., access to post-discharge rehabilitation), availability of family caregivers, pre-existing comorbidities (e.g., diabetes, heart failure), and individual pain thresholds—were not consistently reported or adjusted for in the included studies (64–66). These factors can independently influence pain perception and functional recovery, potentially introducing residual bias into the meta-analysis (67–71). ⑤ Temporal Limitations in Generalizability: While the review covers studies from 2010 to 2023, advances in pain-management technology (e.g., wearable pain-monitoring devices, telehealth-led pain interventions) and evolving nursing protocols (e.g., integration of enhanced recovery after surgery [ERAS] pathways) over this period may reduce the generalizability of findings from earlier studies (2010–2015) to current clinical practice. Future reviews focusing on the past decade (2015–2025) could provide more contemporary insights aligned with current care standards. ⑥ Underrepresentation of Nursing-Specific Studies: Nursing-focused interventions are often published in specialized nursing journals with lower impact factors, which may be less comprehensively indexed in mainstream databases (e.g., PubMed, Web of Science). Despite our rigorous search strategy, this underrepresentation could have led to a partial evidence pool—even though Egger’s test indicated minimal publication bias—potentially excluding innovative nurse-led pain-relief models (60, 61, 72–74).
In spite of the limitations, this work has numerous strengths, as this meta-analysis followed PRISMA guidelines, included both randomized and high-quality cohort studies, and was derived using a sound analytical platform. Also, it is beneficial that this work emphasizes the effectiveness of pain-relief strategies that are delivered specifically by nurses versus by surgical and pharmacological interventions. This is important because nurses are equipped to provide comprehensive care of the patient throughout perioperative care processes, and nurses are often the first line of defense regarding assessment of patient comfort and to be able to recognize and respond to pain (21, 62).
These findings lend support for an immediate and robust focus on embedding nursing care associated with pain relief into hospital perioperative protocols for hip arthroplasty. Nursing activities involving assessments, teaching, and non-pharmacological interventions for patient comfort should not be valued as adjunctive components to patient recovery but should be integrated into the recovery process. Hospitals must undertake resourcing goals that include staff training if conditioned to follow pain-relief protocols, especially with orthopedic and geriatric nursing teams, and implement these back into hospital care pathways (63, 75, 76). In addition, research into large-scale pain-relief implications and whole-system costing, or implementation of digital pathways for pain-relief nutrition-based approaches, would assist in better tailoring interventions to suit the diverse clinical presentation and details (77–80).
As health systems are changing to value-based services, they need to acknowledge and integrate the therapeutic impact of nursing into care agreements. Pain-relief nursing is not merely a supportive partnership, and is instead delivered as focused evidence-based interventions that improve morbidity and accelerate recovery, such that pain-relief nursing support leads to decreased risk of complications and improved autonomy for patients (88–90). As evidenced by this analysis, it needs to be part of the overall integrated multidisciplinary team along with physiotherapy, surgery, and pharmacy to enhance patient outcomes following a hip arthroplasty (81–87).
5 Conclusion
This systematic review and meta-analysis demonstrate significant evidence that pain-relief nursing interventions can significantly improve post-operative recovery related to the activities of daily living (ADL) in hip arthroplasty patients. Nurse-led analgesic administration, incorporating early mobilization facilitation and the practice of functional rehabilitation, was associated with improved patient outcomes, including lower pain scores and more rapid functional independence scores.
We support the relevant literature, which states the importance of targeted pain-relief nursing during an early rehabilitation phase after hip arthroplasty, endorsing the new generation of recovery principles while maintaining an emphasis on patient-centered care. Additionally, these nursing interventions contained physical recovery benefits as well as improved psychological sense of well-being and treatment satisfaction.
Nevertheless, there is a degree of variation in both the components of interventions reported and the outcomes measured across studies, signaling a need for standardized nursing protocols and high-quality trials that may provide nurses with increased confidence in clinical recommendations. Future articles should consider aspects of long-term functional impact, overall health care system cost–benefit analysis, and recent developments for adapting outcomes for healthcare system differences.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
JX: Conceptualization, Data curation, Methodology, Software, Writing - original draft. RB: Conceptualization, Data curation, Methodology, Software, Writing - original draft. HL: Formal analysis, Project administration, Resources, Visualization, Writing - review & editing. RLB: Formal analysis, Project administration, Resources, Visualization, Writing - review & editing. YC: Funding acquisition, Investigation, Supervision, Validation, Writing - review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1680486/full#supplementary-material
References
1. Günther, KP, Deckert, S, Lützner, C, Lange, T, Schmitt, J, Postler, A, et al. Total hip replacement for osteoarthritis-evidence-based and patient-oriented indications. Dtsch Arztebl Int. (2021) 118:730–6. doi: 10.3238/arztebl.m2021.0323
2. Maradit Kremers, H, Larson, DR, Crowson, CS, Kremers, WK, Washington, RE, Steiner, CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. (2015) 97:1386–97. doi: 10.2106/JBJS.N.01141
3. Culliford, D, Maskell, J, Judge, A, Cooper, C, Prieto-Alhambra, D, and Arden, NK. Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthr Cartil. (2015) 23:594–600. doi: 10.1016/j.joca.2014.12.022
4. Omran, K, Waren, D, and Schwarzkopf, R. Postoperative pain trajectories in total hip arthroplasty. Bone Jt Open. (2024) 5:174–83. doi: 10.1302/2633-1462.53.BJO-2023-0181.R1
5. Wainwright, TW. Enhanced Recovery after Surgery (ERAS) for Hip and Knee Replacement-Why and How It Should Be Implemented Following the COVID-19 Pandemic. Medicina (Kaunas). (2021) 57:81. doi: 10.3390/medicina57010081
6. Nakajima, A, Terayama, K, Akiba, T, Nakano, S, Sonobe, M, and Nakagawa, K. Preoperative physical factors predictive of clinical outcomes after Total knee arthroplasty. Prog Rehabil Med. (2025) 10:n/a. doi: 10.2490/prm.20250013
7. Mangone, L, Mereu, F, Zizzo, M, Morini, A, Zanelli, M, Marinelli, F, et al. Outcomes before and after implementation of the ERAS (enhanced recovery after surgery) protocol in open and laparoscopic colorectal surgery: a comparative real-world study from northern Italy. Curr Oncol. (2024) 31:2907–17. doi: 10.3390/curroncol31060222
8. Tamamura, Y, Matsuura, M, Shiba, S, and Nishikimi, T. Effect of heart failure and malnutrition, alone and in combination, on rehabilitation effectiveness in patients with hip fracture. Clin Nutr ESPEN. (2021) 44:356–66. doi: 10.1016/j.clnesp.2021.05.014
9. Gan, TJ, Habib, AS, Miller, TE, White, W, and Apfelbaum, JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. (2014) 30:149–60. doi: 10.1185/03007995.2013.860019
10. Lunn, TH, and Kehlet, H. Fast-track hip and knee arthroplasty – status and future challenges. Acta Orthop. (2011) 82:439–43.
11. Morrison, SR, Magaziner, J, McLaughlin, MA, Orosz, G, Silberzweig, SB, Koval, KJ, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. (2003) 103:303–11.
12. Moon, M, Oh, EG, Baek, W, and Kim, YM. Effects of nurse-led pain management interventions for patients with Total knee/hip replacement. Pain Manag Nurs. (2021) 22:111–20. doi: 10.1016/j.pmn.2020.11.005
13. Sheng, Q, Wang, G, and Wang, P. Effect of nursing interventions on the rehabilitation of patients after knee and hip replacements. Rev Esc Enferm USP. (2025) 59:e20250184. doi: 10.1590/1980-220X-REEUSP-2025-0184en
14. Sohrabi, M, Gholami, M, Foroughi, S, Younesi, E, and Mokhayeri, Y. The effect of a nurse-led multicomponent intervention on sleep quality and delirium in orthopedic surgery patients: A randomized clinical trial. Int J Orthop Trauma Nurs. (2025) 59:101222. doi: 10.1016/j.ijotn.2025.101222
15. Fang, L, Chen, L, Sun, H, Xu, Y, and Jin, J. The Effectiveness of Using a Nurse-Led Pain Relief Model for Pain Management among Abdominal Surgical Patients: A Single-Center, Controlled before-after Study in China. Pain Manag Nurs. (2021) 22:198–204. doi: 10.1016/j.pmn.2020.08.004
16. Liu, G, Li, L, Deng, J, Cai, L, and He, R. Enhanced recovery after surgery: nursing strategy for total hip arthroplasty in older adult patients. BMC Geriatr. (2025) 25:282. doi: 10.1186/s12877-025-05888-8
17. Moon, M, Oh, EG, Baek, W, and Kim, YM. Effects of Nurse-Led Pain Management Interventions for Patients with Total Knee/Hip Replacement. Pain Manag Nurs. (2021) 78:111–120.
18. Aprisunadi,, Nursalam, N, Mustikasari, M, Ifadah, E, and Hapsari, ED. Effect of Early Mobilization on Hip and Lower Extremity Postoperative: A Literature Review. SAGE Open Nurs. (2023) 9:23779608231167825.
19. Hida, M, Deguchi, Y, Miyaguchi, K, Nakazono, M, Hirata, N, Nakagawa, R, et al. Association between Acute Postoperative Pain and Recovery of Independent Walking Ability after Surgical Treatment of Hip Fracture. Prog Rehabil Med. (2018) 3:20180012. doi: 10.2490/prm.20180012
20. Konnyu, KJ, Pinto, D, Cao, W, Aaron, RK, Panagiotou, OA, and Bhuma, MR. Rehabilitation for Total Hip Arthroplasty: A Systematic Review. Am J Phys Med Rehabil. (2023) 102:11–18. doi: 10.1097/PHM.0000000000002007
21. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, T, Mulrow, C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71.
22. Zhang, Y, Li, Y, Zhou, C, Yang, J, and Liu, Y. Effects of nurse-led pain management on recovery after total hip arthroplasty: a systematic review and meta-analysis. J Clin Nurs. (2022) 31:987–96.
23. Sun, J, Xu, Y, Zhu, J, Zhu, B, and Gao, W. Efficacy and safety of continuous nursing in improving functional recovery after total hip or knee arthroplasty in older adults: A systematic review. Int J Nurs Sci. (2024) 11:286–294. doi: 10.1016/j.ijnss.2024.03.013
24. Riga, M, Altsitzioglou, P, Saranteas, T, and Mavrogenis, AF. Enhanced recovery after surgery (ERAS) protocols for total joint replacement surgery. SICOT J. (2023) 9:E1. doi: 10.1051/sicotj/2023030
25. McGuinness, LA, and Higgins, JPT. Risk-of-bias visualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. (2021) 12:55–61. doi: 10.1002/jrsm.1411
26. Pivec, R, Johnson, AJ, Mears, SC, and Mont, MA. Hip arthroplasty. Lancet. (2012) 380:1768–77. doi: 10.1016/S0140-6736(12)60607-2
27. Xu, X, Wang, Z, Wu, Y, and Wang, X. Effect of individualized nursing care on postoperative recovery in elderly hip fracture patients. Int J Nurs Sci. (2022) 9:112–9.
28. Qu, L, Li, Y, and Hong, D. Effectiveness of refined nursing on postoperative recovery in elderly hip fracture patients: A retrospective study. Medicine (Baltimore). (2025) 104:e43870. doi: 10.1097/MD.0000000000043870
29. Sarkies, MN, Testa, L, Carrigan, A, Roberts, N, Gray, R, and Sherrington, C. Perioperative interventions to improve early mobilisation and physical function after hip fracture: a systematic review and meta-analysis. Age Ageing. (2023) 52:afad154. doi: 10.1093/ageing/afad154
30. Niyonkuru, E, Iqbal, MA, Zhang, X, and Ma, P. Complementary Approaches to Postoperative Pain Management: A Review of Non-pharmacological Interventions. Pain Ther. (2025) 14:121–144. doi: 10.1007/s40122-024-00688-1
31. El-Toukhy, H, and Mitchell, J. Risk of bias in pre- and post-surgical nursing trials: a review using the NOS tool. Int J Nurs Stud. (2019) 95:58–64.
32. Beaupre, LA, Magaziner, JS, Jones, CA, Jhangri, GS, Johnston, DWC, Wilson, DM, et al. Rehabilitation After Hip Fracture for Nursing Home Residents: A Controlled Feasibility. Trial. J Gerontol A Biol Sci Med Sci. (2019) 74:1518–1525. doi: 10.1093/gerona/glz031
33. Tonia, T, Buitrago-Garcia, D, Peter, NL, Mesa-Vieira, C, Li, T, and Furukawa, TA. Tool to assess risk of bias in studies estimating the prevalence of mental health disorders (RoB-PrevMH). BMJ Ment Health. (2023) 26:e300694. doi: 10.1136/bmjment-2023-300694
34. Shin, IS, Shin, JH, Jang, DE, and Lee, JA. Methodological Quality Evaluation of Meta-Analyses on Nursing Home Research: Overview and Suggestions for Future Directions. Int J Environ Res Public Health. (2022) 19:505. doi: 10.3390/ijerph19010505
35. Riemen, AH, and Hutchison, JD. The multidisciplinary management of hip fractures in older patients. Orthop Trauma. (2016) 30:177–22. doi: 10.1016/j.mporth.2016.03.006
36. Huang, J, Wu, G, and Li, X. Application of Perioperative Nursing Based on Enhanced Recovery After Surgery (ERAS) Principles in Patients Undergoing Total Knee Arthroplasty. Ther Clin Risk Manag. (2025) 21:829–39. doi: 10.2147/TCRM.S515992
37. Carpintero, P, Caeiro, JR, Carpintero, R, Morales, A, Silva, S, and Mesa, M. Complications of hip fractures: a review. World J Orthop. (2014) 5:402–11. doi: 10.5312/wjo.v5.i4.402
38. Mak, JCS, Cameron, ID, and March, LM. Evidence-based guidelines for the management of hip fractures in older persons: an update. Med J Aust. (2010) 192:37–41. doi: 10.5694/j.1326-5377.2010.tb03400.x
39. Xie, H, Zhang, R, Cao, S, Jiang, J, Huang, B, Liu, M, et al. Repetitive transcranial magnetic stimulation in conjunction with scalp acupuncture in treating poststroke cognitive impairment: a protocol for systematic review and meta-analysis. BMJ Open. (2025) 15:e098535. doi: 10.1136/bmjopen-2024-098535
40. Xu, J, Wang, Y, He, Q, Xie, S, Feng, S, Wang, X, et al. Evaluating the agreement between sensitivity and primary analyses in observational studies using routinely collected healthcare data: a meta-epidemiology study. BMC Med. (2025) 23:393. doi: 10.1186/s12916-025-04199-4
41. Boonen, S, Magaziner, J, Singer, MA, et al. Osteoporotic fractures and nursing home admissions. JAMA. (2011) 305:507–15.
42. Bjerk, M, Brovold, T, Skelton, DA, and Bergland, A. Older adults’ experiences of function-focused care after hip fracture surgery. J Clin Nurs. (2015) 24:2421–30.
43. Alghadir, AH, Anwer, S, Iqbal, A, and Iqbal, ZA. Effect of progressive resistance training on ADL performance in elderly patients after hip surgery. Clin Interv Aging. (2016) 11:607–16.
44. Hida, M, Deguchi, Y, Miyaguchi, K, Nakazono, M, Hirata, N, Nakagawa, R, et al. Association between acute postoperative pain and recovery of independent walking ability after surgical treatment of hip fracture. Prog Rehabil Med. (2018) 3:n/a.
45. Li, Y, Gu, Z, Ning, R, and Yin, H. Study on the effect of internet plus continuous nursing on functional recovery and medication compliance of patients with knee joint replacement. J Orthop Surg Res. (2023) 18:424. doi: 10.1186/s13018-023-03907-1
46. Schoene, D, Rapp, K, Roigk, P, Becker, C, Jaensch, A, Konnopka, C, et al. Orthogeriatric comanagement and incident nursing home admissions in older patients with fragility fractures other than the hip-a retrospective cohort study using insurance claims data from Germany. BMC Med. (2025) 23:248. doi: 10.1186/s12916-025-04073-3
47. Beaupre, LA, Binder, EF, Cameron, ID, Jones, CA, Orwig, D, Sherrington, C, et al. Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol. (2013) 27(6):771–88. doi: 10.1016/j.berh.2014.01.001
48. Wang, H, Yu, H, Kim, YH, and Kan, W. Comparison of the Effect of Resistance and Balance Training on Isokinetic Eversion Strength, Dynamic Balance, Hop Test, and Ankle Score in Ankle. Sprain. Life (Basel). (2021) 11:307. doi: 10.3390/life11040307
49. Karam, JA, Schwenk, ES, and Parvizi, J. An update on multimodal pain management after Total joint arthroplasty. J Bone Joint Surg Am. (2021) 103:1652–62. doi: 10.2106/JBJS.19.01423
50. Magaziner, J, Hawkes, W, Hebel, JR, Zimmerman, SI, Fox, KM, Dolan, M, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. (2000) 55:M498–507. doi: 10.1093/gerona/55.9.m498
51. Kalmet, PH, Koc, BB, Hemmes, B, Ten Broeke, RH, Dekkers, G, Hustinx, P, et al. Effectiveness of a multidisciplinary clinical pathway for elderly patients with hip fracture: a multicenter comparative cohort study. Geriatr Orthop Surg Rehabil. (2016) 7:81–5. doi: 10.1177/2151458516645633
52. Tricco, AC, Thomas, SM, Veroniki, AA, Hamid, JS, Cogo, E, Strifler, L, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. (2017) 318:1687–99. doi: 10.1001/jama.2017.15006
53. Mac Curtain, BM, O'Mahony, A, Temperley, HC, and Ng, ZQ. Enhanced recovery after surgery protocols and emergency surgery: a systematic review and meta-analysis of randomized controlled trials. ANZ J Surg. (2023) 93:1780–6. doi: 10.1111/ans.18550
54. Chou, R, Gordon, DB, de Leon-Casasola, OA, Rosenberg, JM, Bickler, S, Brennan, T, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' committee on regional anesthesia, executive committee, and administrative council. J Pain. (2016) 17:131–57. doi: 10.1016/j.jpain.2015.12.008
55. Paduraru, M, Ponchietti, L, Casas, IM, Svenningsen, P, and Zago, M. Enhanced recovery after emergency surgery: a systematic review. Bull Emerg Trauma. (2017) 5:70–8.
56. Wainwright, TW, Immins, T, and Middleton, RG. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best Pract Res Clin Anaesthesiol. (2016) 30:91–102. doi: 10.1016/j.bpa.2015.11.001
57. Torres, R, Sa, RP, Cruz, AS, Mata da Silva, A, Fragoso, P, and Cruz, JL. Enhancing elderly hip fracture care: reducing the length of stay through guidelines implementation. Cureus. (2025) 17:e77238. doi: 10.7759/cureus.77238
58. Stockton, KA, and Mengersen, KA. Effect of multiple physiotherapy sessions on functional outcomes in the initial postoperative period after primary total hip replacement: a randomized controlled trial. Arch Phys Med Rehabil. (2009) 90:1652–7. doi: 10.1016/j.apmr.2009.04.012
59. Paduraru, M, Ponchietti, L, Casas, IM, Svenningsen, P, and Zago, M. Enhanced Recovery after Emergency Surgery: A Systematic Review. Bull. Emerg Trauma. (2017) 5:70–7.
60. Griffiths, P, Ball, J, Drennan, J, Dall’Ora, C, Jones, J, Maruotti, A, et al. Nurse staffing and patient outcomes: strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for health and care excellence safe staffing guideline development. Int J Nurs Stud. (2016) 63:213–25. doi: 10.1016/j.ijnurstu.2016.03.012
61. Cui, C, Wang, LX, Li, Q, Zaslansky, R, and Li, L. Implementing a pain management nursing protocol for orthopaedic surgical patients: results from a PAIN OUT project. J Clin Nurs. (2018) 27:1684–91. doi: 10.1111/jocn.14224
62. Qin, J, Gou, LY, Zhang, W, Pu, X, and Zhang, P. Enhanced recovery after surgery versus conventional Care in Cholecystectomy: a systematic review and Meta-analysis. J Laparoendosc Adv Surg Tech A. (2024) 34:710–20. doi: 10.1089/lap.2024.0119
63. Bay, S, Kuster, L, McLean, N, Byrnes, M, and Kuster, MS. A systematic review of psychological interventions in total hip and knee arthroplasty. BMC Musculoskelet Disord. (2018) 19:201. doi: 10.1186/s12891-018-2121-8
64. O'Connor, MI, and Switzer, JA. AAOS clinical practice guideline summary: Management of hip Fractures in older adults. J Am Acad Orthop Surg. (2022) 30:e1291–6. doi: 10.5435/JAAOS-D-22-00125
65. Wu, CL, Rowlingson, AJ, Partin, AW, Kalish, MA, Courpas, GE, Walsh, PC, et al. Correlation of postoperative pain to quality of recovery in the immediate postoperative period. Reg Anesth Pain Med. (2005) 30:516–22. doi: 10.1016/j.rapm.2005.07.190
66. Mak, JCS, Klein, L, Mason, RS, and Cameron, ID. Contemporary pain Management in Elderly Patients after hip Fracture Surgery: cross-sectional analyses at baseline of a randomized controlled trial. Clin J Pain. (2015) 31:788–93. doi: 10.1097/AJP.0000000000000158
67. Abou-Setta, AM, Beaupre, LA, Rashiq, S, Dryden, DM, Hamm, MP, Sadowski, CA, et al. Comparative effectiveness of pain management interventions for hip fracture: a systematic review. Ann Intern Med. (2011) 155:234–45. doi: 10.7326/0003-4819-155-4-201108160-00346
68. Morrison, RS, Meier, DE, Fischberg, D, Moore, C, Degenholtz, H, Litke, A, et al. Improving the management of pain in hospitalized adults. Arch Intern Med. (2006) 166:1033–9. doi: 10.1001/archinte.166.9.1033
69. Zhao, X, Bai, R, and Yang, J. Effect of painless rehabilitation nursing for hip replacement patients. Comput Math Methods Med. (2022) 2022:1–6. doi: 10.1155/2022/5164973
70. Gordon, DB. Pain management in the elderly. J Perianesth Nurs. (1999) 14:367–72. doi: 10.1016/s1089-9472(99)80098-7
71. Oliver, D, Papaioannou, A, Giangregorio, L, Thabane, L, Reizgys, K, and Foster, G. A systematic review and meta-analysis of studies using the STRATIFY tool for prediction of falls in hospital patients: how well does it work? Age Ageing. (2008) 37:621–7. doi: 10.1093/ageing/afn203
72. Brodersen, F, Wagner, J, Uzunoglu, FG, and Petersen-Ewert, C. Impact of preoperative patient education on postoperative recovery in abdominal surgery: a systematic review. World J Surg. (2023) 47:937–47. doi: 10.1007/s00268-022-06884-4
73. Agarwal, N, Feng, T, Maclullich, A, Duckworth, A, and Clement, N. Early mobilisation after hip fracture surgery is associated with improved patient outcomes: a systematic review and meta-analysis. Musculoskeletal Care. (2024) 22:e1863. doi: 10.1002/msc.1863
74. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, and Mulrow, CD. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:71. doi: 10.1136/bmj.n71
75. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
76. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
77. Morrison, SR, Magaziner, J, McLaughlin, MA, Orosz, G, Silberzweig, SB, Koval, KJ, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. (2003) 103:303–11. doi: 10.1016/S0304-3959(02)00458-X
78. Kaye, AD, Urman, RD, Rappaport, Y, Siddaiah, H, Cornett, EM, Belani, K, et al. Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings. J Anaesthesiol Clin Pharmacol. (2019) 35:S40–5. doi: 10.4103/joacp.JOACP_51_18
79. Sharma, V, Morgan, PM, and Cheng, EY. Factors influencing early mobilization after total hip arthroplasty. J Arthroplast. (2009) 24:198–204.
80. Sharma, V, Morgan, PM, and Cheng, EY. Factors influencing early rehabilitation after THA: a systematic review. Clin Orthop Relat Res. (2009) 467:1400–11 doi: 10.1007/s11999-009-0750-9
81. Chou, R, Griffin, JC, Blazina, I, Schwarz, E, Atchison, C, and Mauer, K. Systematic Review on Treatments for Acute Pain: Surveillance Report 3: Literature Update Period: January 22, 2022, through May 6, 2022. 2022 Jun. In: Treatments for Acute Pain: A Systematic Review: Surveillance Reports [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US). (2020)
82. Hara, R, Hiraga, Y, Hirakawa, Y, and Babazono, A. Effects of integrating pain coping strategies into occupational therapy after Total knee arthroplasty: a parallel mixed-method study. Healthcare. (2025) 13:627. doi: 10.3390/healthcare13060627
83. Keswani, A, Tasi, MC, Fields, A, Lovy, AJ, Moucha, CS, and Bozic, KJ. Discharge destination after Total joint arthroplasty: an analysis of Postdischarge outcomes, placement risk factors, and recent trends. J Arthroplast. (2016) 31:1155–62. doi: 10.1016/j.arth.2015.11.044
84. Nijs, J, George, SZ, Clauw, DJ, Fernández-de-Las-Peñas, C, Kosek, E, Ickmans, K, et al. Central sensitisation in chronic pain conditions: latest discoveries and their potential for precision medicine. Lancet Rheumatol. (202) 3:e383–92. doi: 10.1016/S2665-9913(21)00032-1
85. Aprisunadi,, Nursalam N,, Mustikasari M,, Ifadah E,, and Hapsari ED,. Effect of early mobilization on hip and lower extremity postoperative: a literature review. SAGE Open Nurs. (2023) 9:23779608231167825. doi: 10.1177/23779608231167825
86. Grota, T, Betihavas, V, Burston, A, and Jacob, E. Impact of nurse-surgeons on patient-centred outcomes: a systematic review. Int J Nurs Stud Adv. (2022) 4:100086. doi: 10.1016/j.ijnsa.2022.100086
87. Fan, JC, Lo, CK, Kwok, CK, and Fung, KY. Nurse-led orthopaedic clinic in total joint replacement. Hong Kong Med J. (2014) 20:511–8. doi: 10.12809/hkmj134150
88. Sterne, JAC, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
89. Huang, M, Zhang, Y, and Wang, F. Leave-one-out sensitivity testing in rehabilitation meta-analyses. J Rehabil Med. (2021) 53:jrm00267
Keywords: activities of daily living, hip arthroplasty, Meta-analysis, pain-relief nursing, postoperative recovery
Citation: Xie J, Bai R, Lei H, Bi R-L and Chen Y (2025) Effect of pain-relief nursing on activities of daily living in patients following hip arthroplasty: a systematic review and meta-analysis. Front. Med. 12:1680486. doi: 10.3389/fmed.2025.1680486
Edited by:
Luis Manuel Mota de Sousa, Universidade Atlântica, PortugalReviewed by:
Geyslane Pereira Melo de Albuquerque, Universidade de Pernambuco, BrazilPaula Cristina Dias Rocha, Instituto Politecnico de Viseu, Portugal
Sandy Severino, Escola Superior de Saúde Atlântica, Portugal
Copyright © 2025 Xie, Bai, Lei, Bi and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Chen, MTU4Mjc1ODYyODFAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Jun Xie†
Jun Xie† Ying Chen
Ying Chen