- 1Department of Obstetrics and Gynecology, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
- 2Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
Background: Cesarean section (CS) rates are increasing globally, including in the Middle East. While CS can be a lifesaving procedure, unnecessary CS can lead to complications for both mother and child. Understanding factors influencing women’s delivery preferences is crucial for optimizing maternal and child health outcomes.
Methods: This cross-sectional study investigated factors influencing the preferred mode of delivery among 661 pregnant women in Jeddah, Saudi Arabia. Data were collected using a structured questionnaire and analyzed using descriptive statistics and logistic regression.
Results: Multiple factors showed significant associations with CS preference in multivariable analysis. Non-Saudi women had substantially higher odds of preferring CS compared to Saudi nationals (aOR 2.45, 95% CI 1.30–4.60). Urban residency (aOR 2.89, 95% CI 1.45–5.78) and higher income ≥50,000 SAR (aOR 4.15, 95% CI 1.02–16.88) were also strong predictors. Conversely, women aged 31–40 years had significantly lower odds of preferring CS (aOR 0.23, 95% CI 0.07–0.78) compared to those aged 18–24. Women with no prior CS were more likely to prefer spontaneous vaginal delivery, and previous CS in private hospitals significantly increased CS preference for subsequent deliveries.
Conclusion: This study highlights the complex interplay of demographic, socioeconomic, and personal factors influencing women’s delivery preferences. Understanding these factors is crucial for developing targeted interventions to promote informed decision-making and optimize maternal and child health outcomes. Further research is needed to investigate the underlying reasons for these preferences.
1 Introduction
Cesarean section (CS) is the most frequent obstetric operation designed to treat or avoid serious complications that could endanger the lives of the mother or fetus (1). Globally, CS rates have been witnessing a surge due to multiple reasons. In middle- and high-income countries, studies reported an increase in CS rates despite lack of evidence of improvement toward maternal and perinatal mortality and morbidity (2), rather, some data suggest the contrary and propose a greater risk for complications when undergoing CS including maternal mortality, vesical injury, ureteral tract injury and hysterectomy (3–5). Furthermore, unnecessary CS can be associated with increased surgical complications, abnormal placentation in subsequent pregnancies, uterine rupture, and longer recovery times (3–5). In contrast, spontaneous vaginal delivery (SVD) offers several health benefits, including faster maternal recovery, establishment of breastfeeding, transfer of beneficial microbiota to the newborn, and reduced risk of respiratory complications in infants (4, 5). However, while CS is associated with increased maternal morbidity, it may offer benefits in specific contexts including reduced risk of urinary incontinence, pelvic organ prolapses, and avoidance of emergency procedures in complicated labors. A balanced understanding of risks and benefits is essential for shared decision-making (6). Nonetheless, it is important to note that the World Health Organization (WHO) recommends an ideal cesarean section rate of 10–15%, noting that rates above this threshold are not associated with reduced maternal or neonatal mortality.
Regionally, the Middle East has mirrored this global trend with rising CS rates across many countries. Within Saudi Arabia specifically, this pattern is particularly evident, with healthcare research increasingly concentrating on the risks associated with different delivery methods. While CS can be lifesaving in certain circumstances, it carries specific fetal risks including respiratory distress syndrome, iatrogenic prematurity, altered immune development, and increased likelihood of neonatal intensive care unit admission compared to vaginal delivery (7). Studies also highlighted an increase in CS, which is like the global surge, including one study in the United Arab Emirates, which presented a rate of CS exceeding the average global rates (8). Similarly, a single-center study in the densely populated Egypt said that CS contribute more than half of deliveries annually (9). Furthermore, a substantial increase has been observed over a decade in Saudi Arabia for the CS according to public estimates, which reach up to 80% (10). This is echoed by single-center data, which similarly present an increase in the rates of CS (11). Midst these data and the conflicting reports on the outcome of CS, patients’ choices constitute one of the key reasons for unnecessary CS procedures made in the absence of clear medical indications (12). Several studies shed light on factors influencing women and contributing to this decision, which varied between parity history as well as some country-specific characteristics, and others (13–16). Meanwhile, none of them quantitatively summarized the results (13–16).
Giving birth is one of the most important and profound human experiences with high individual significance (7). Women who give birth often express feelings of empowerment, joy, and accomplishment, especially after giving birth naturally without the need for medical assistance (17). Multiple factors influence delivery method preference including maternal age, education, previous delivery experience, cultural beliefs, fear of labor pain, perceptions of safety, and healthcare provider recommendations. Understanding these determinants is crucial for developing appropriate patient education and counseling strategies. Moreover, while previous Saudi studies have documented rising CS rates, few have comprehensively examined the interplay of socioeconomic, obstetric, and psychological factors shaping women’s preferences in the Jeddah region. This study aims to identify modifiable determinants of delivery preference to inform targeted interventions and address the growing CS rate in this specific population.
2 Materials and methods
2.1 Study design and setting
We conducted a cross-sectional exploratory study in Jeddah, Saudi Arabia, following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline (18). The study utilized a multi-center approach across major public and private hospitals between January and December 2024 to investigate patients’ preferences for mode of delivery. We included both pregnant women (≥28 weeks gestation) and postpartum women (within 6 months of delivery) to capture preferences across the perinatal period. Exclusion criteria included multiple current pregnancies, known medical indications for CS (e.g., placenta previa, active genital herpes), fetal congenital anomalies, and women unable to provide informed consent. Participants were stratified by pregnancy status in analysis to account for potential differences in perspective. Data were collected using a structured, pre-validated questionnaire from a heterogeneous sample of 661 participants. The questionnaire was re-validated for our use through expert review by three obstetricians and a psychometrician, pilot testing with 30 women, and demonstrated good internal consistency (Cronbach’s alpha = 0.82). Participants were recruited during routine antenatal visits and through hospital maternity records. Enrolled women were asked their preference for delivery type during the post-delivery period. The questionnaire was distributed via secure WhatsApp links, with reminders sent at 2-week intervals to maximize response rate. To minimize response bias, we employed multiple recruitment strategies across different hospital settings, ensured anonymity of responses, and used standardized neutral language in all survey materials. The response rate was 71%, with no significant differences in basic demographics between responders and non-responders. The primary outcome, preference for mode of delivery, was assessed using the direct question with multiple response options.
2.2 Sampling technique
We adopted a convenience sampling method to ensure a larger cohort is enrolled in the study, with the representation of diverse demographic groups within the society under study. The sample was not restricted to certain age groups to explore potential associations and reduce the probability of confounders. The statistically appropriate sample size was calculated using Raosoft software, with a 95% confidence interval (CI) and <0.05 margin of error. The applied equation was as follows:
where, n = population size, p = prevalence, d = precision (desired margin of error), DEFF = design effect, and Z1 − α/2 = 1.96 for a 95% confidence level. We exceeded the minimum recommended sample size, which was determined at 378 (19).
2.3 Data collection and variables
We obtained data through a 31-item self-administered online survey. Patients’ information was retrieved from the electronic hospital record to ensure the survey was accessible to the targeted population and subsequently contacted. For additional clarification, the first section of the survey included a consent statement explaining the nature of the study and the targeted population. The second section obtained socio-demographic data that included their gender, age, nationality, place and city of residency, marital status (e.g., single, married, divorced, or widow), certain anthropometric measurements (e.g., weight and height), educational level (e.g., uneducated, elementary, middle school, high school, university level, higher education), monthly income in local currency, and current occupation. The third section is about obstetrics and delivery, focused on current pregnancy status, number of previous pregnancies, history of live births, abortions, stillbirths, and prior delivery methods, including CS history and setting (public/private hospital). The fourth section is pain and post-delivery experience evaluated participants’ experiences with postpartum pain, duration of medication use, and perceived community awareness regarding delivery complications.
2.4 Data analysis
Data were cleaned, managed, and coded using Microsoft Excel 2019 (Microsoft Corporation, Redmond, WA). Statistical analysis was performed using R (RStudio, version 1.4.1106; RStudio, Inc). Descriptive analysis included frequency distributions. Cross-tabulations were evaluated using the chi-square test, and odds ratios (OR) with 95% confidence intervals (CI) were calculated. Multivariable logistic regression included covariates selected a priori based on literature review: age, nationality, education, income, parity, previous CS, and source of delivery information. Missing data (<5%) were handled using multiple imputation. Model assumptions were checked using residual analysis and variance inflation factors (all <2.0). A p-value of less than 0.05 was considered statistically significant.
3 Results
3.1 Sociodemographic characteristics
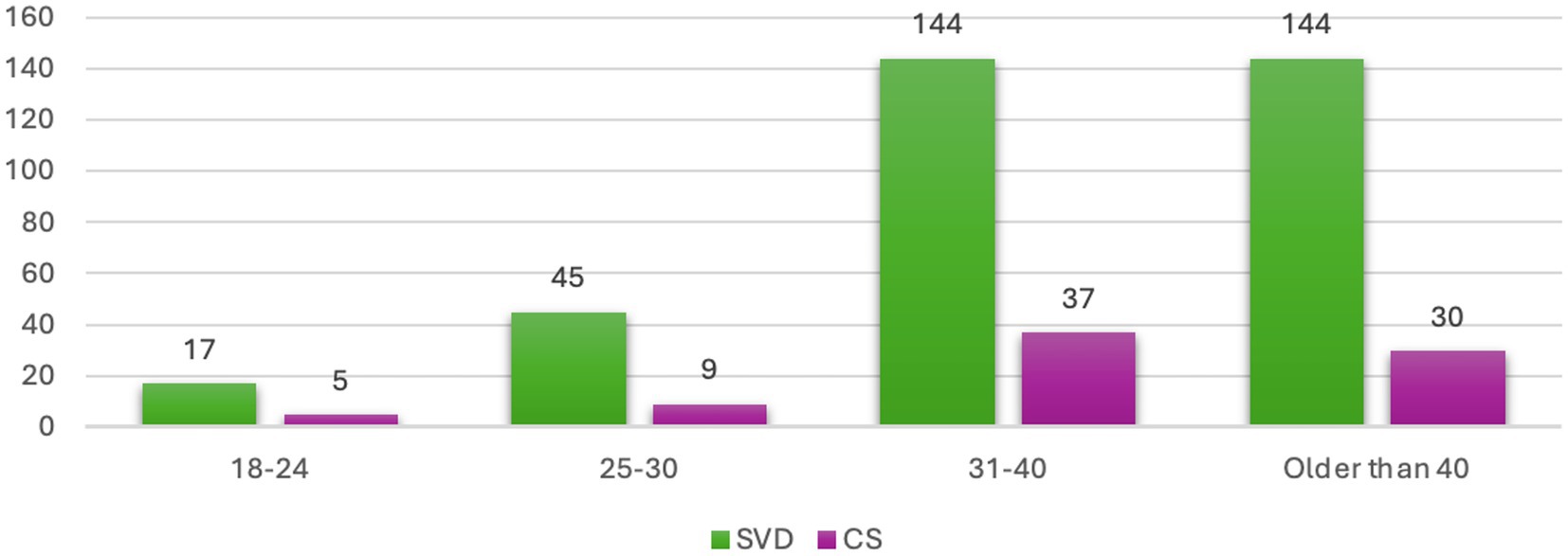
The sociodemographic characteristics of the 661 participants are summarized in Table 1. The cohort was predominantly Saudi (79.4%), married (62.5%), and resided within Saudi Arabia (92.9%), with a majority living in the study city of Jeddah (63.2%). The age distribution was broad, with the largest proportion of participants falling within the 31–40 year age group (29.0%). Education levels were high, as most participants had attained a university degree (61.9%). Nearly half of the participants (49.6%) reported a monthly income of less than 5,000 Saudi Riyals. Regarding anthropometrics, the majority of participants were within the 150–169 cm height range (86.4%) and the 50–69 kg weight category (52.8%; Figure 1). This profile describes a cohort that is broadly representative of an urban patient population in the region.
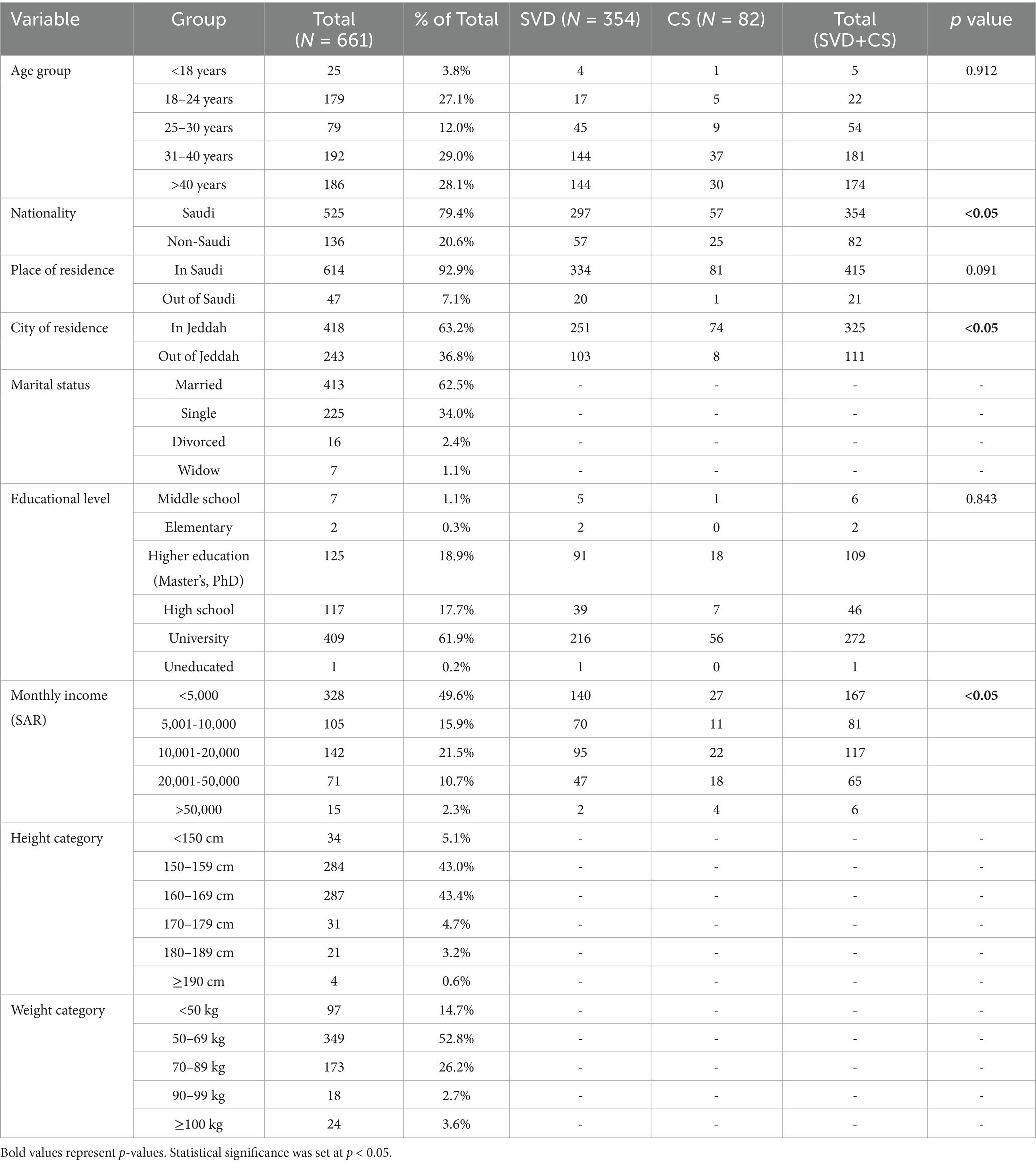
Table 1. Sociodemographic characteristics of participants and association with preferred mode of delivery.
3.2 Factors influencing preferred mode of delivery
The association between participant characteristics and their preferred mode of delivery is presented in Table 1. In the bivariate analysis, several demographic factors showed significant associations with a preference for CS. These included non-Saudi nationality (p < 0.05), residence within Jeddah city (p < 0.05), and higher monthly income (p < 0.05). In contrast, age group (p = 0.912) and educational level (p = 0.843) were not significantly associated with delivery preference.
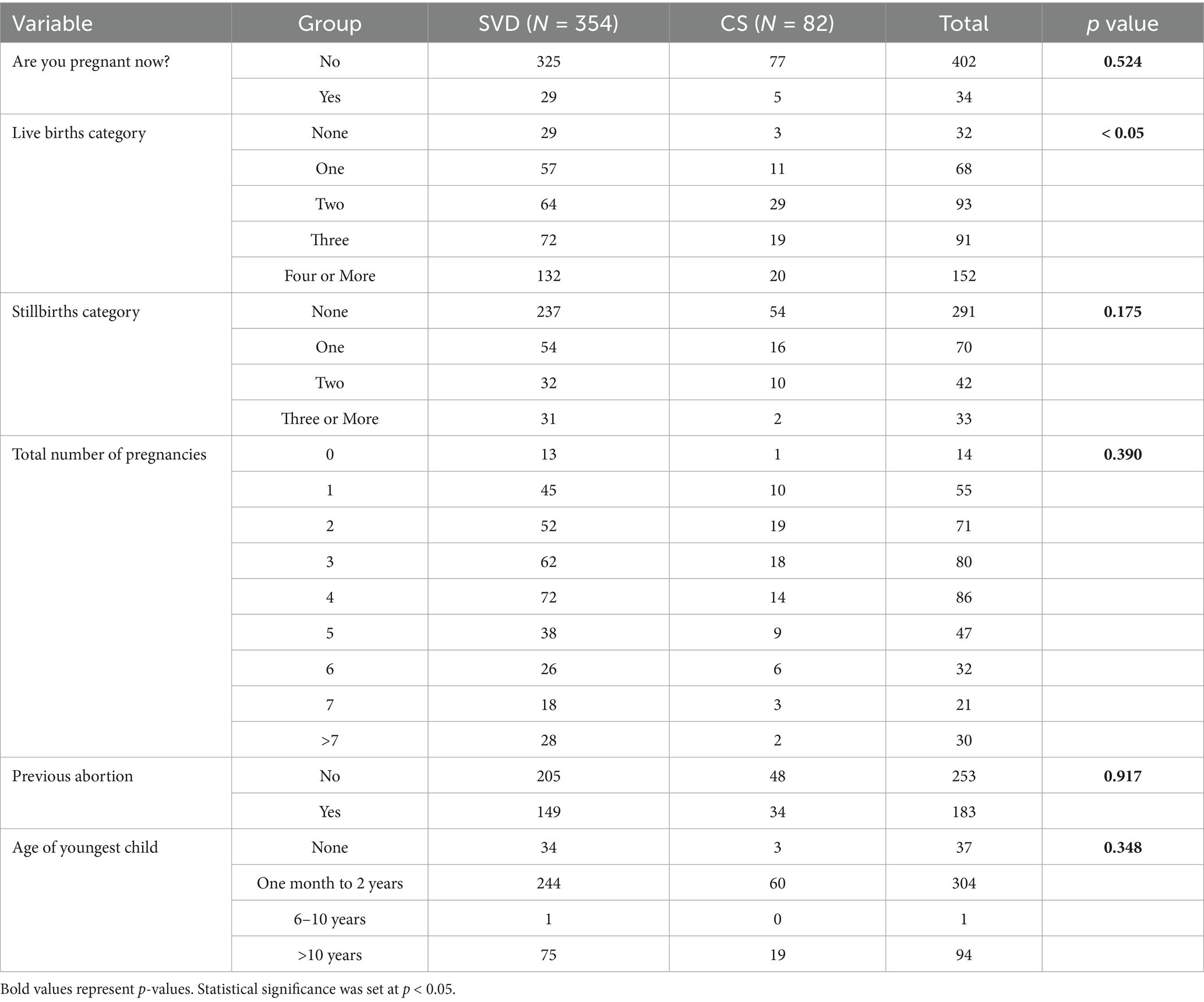
Further analysis of obstetric history, detailed in Table 2, revealed that the number of previous live births was a significant factor (p < 0.05). However, other obstetric factors such as current pregnancy status, history of stillbirth, total number of pregnancies, previous abortion, and the age of the youngest child did not demonstrate a significant influence on the choice between SVD and CS.
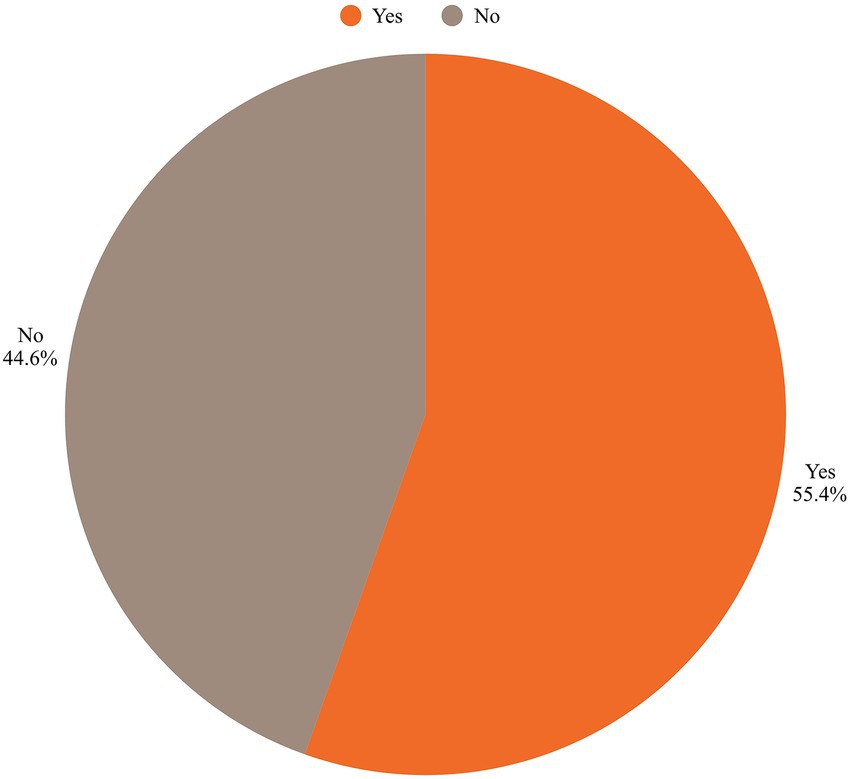
3.3 Impact of CS on delivery mode preferences
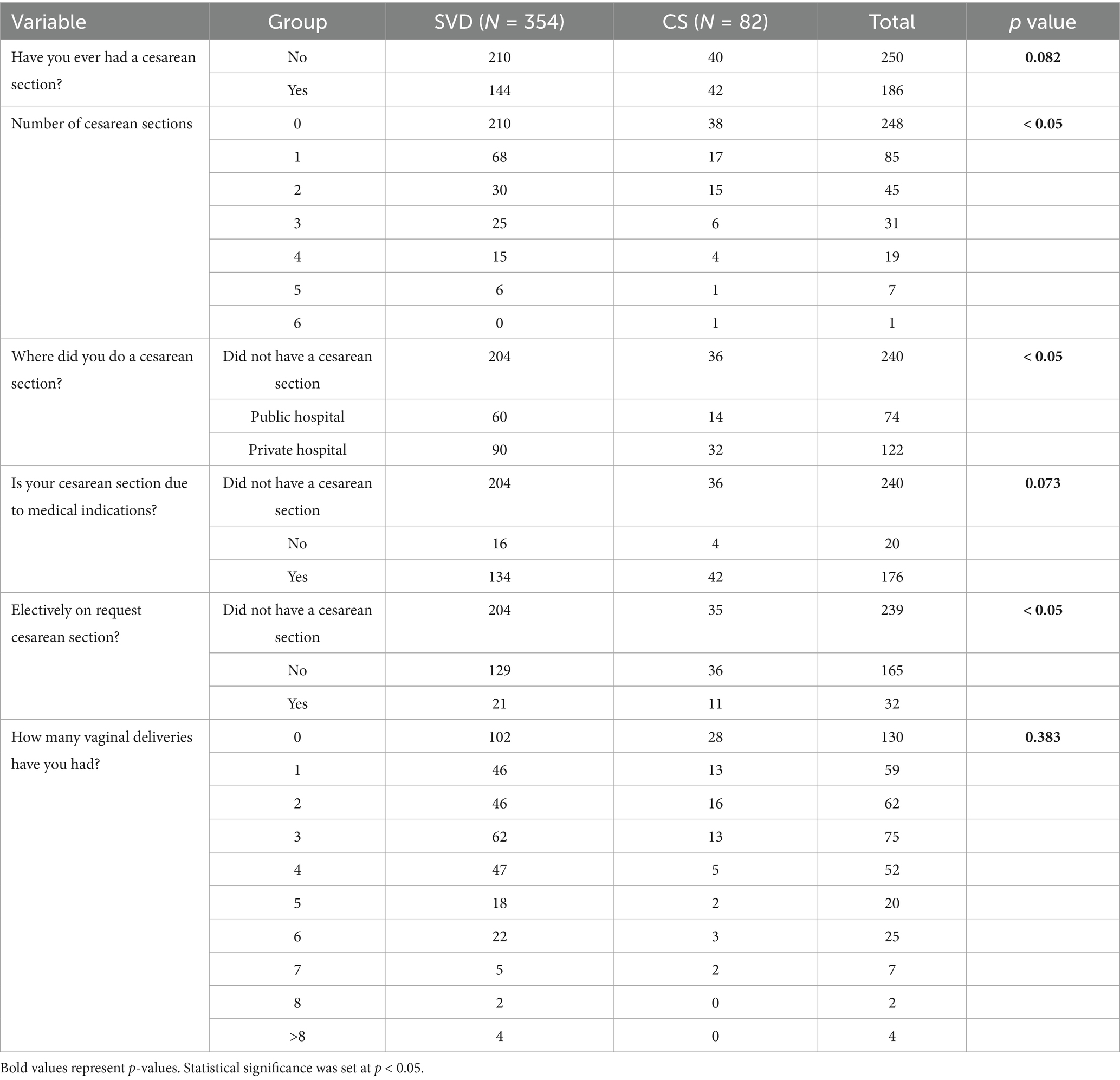
The relationship between CS history and participants’ preferred mode of delivery reveals several significant findings (Table 3). The number of previous CS strongly influenced delivery preferences, with participants who had no prior CS more likely to prefer SVD (p < 0.05). Additionally, those who had CSs in private hospitals were more inclined to choose CS for subsequent deliveries (p < 0.05). Elective CS on request also played a significant role, with participants who opted for elective CS more likely to continue preferring CS (p < 0.05). In contrast, factors such as whether the CS was due to medical indications and the number of previous SVD did not significantly affect delivery preferences (p > 0.05).
3.4 Opinions on mode of delivery and associated factors
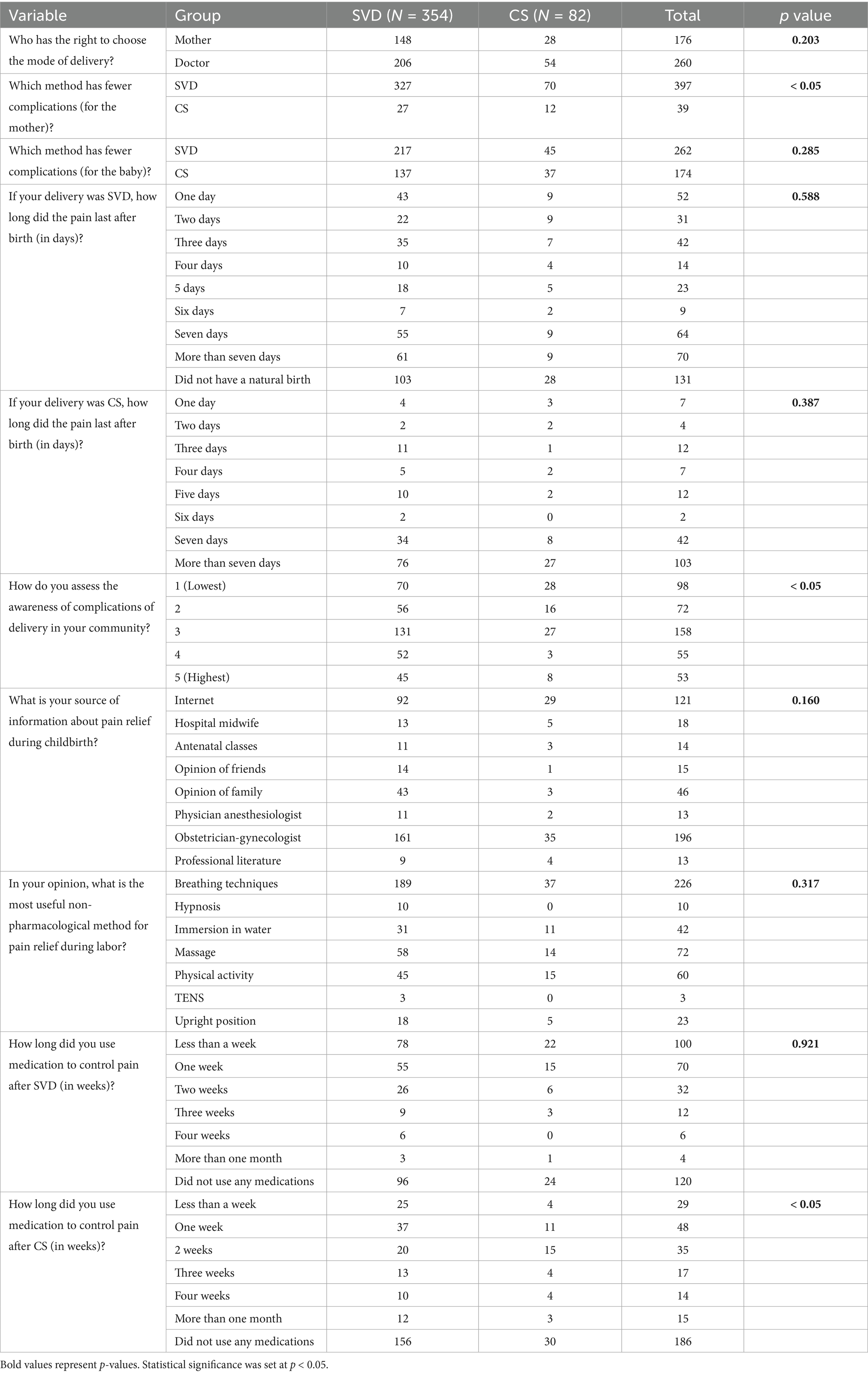
Table 4 presents opinions on the mode of delivery and associated factors among participants who preferred SVD and CS. The decision-making process regarding the mode of delivery was similar between the groups, with mothers and doctors playing key roles (p = 0.203). A significant majority believed that SVD has fewer complications for the mother compared to CS (p < 0.05). However, opinions on complications for the baby did not significantly differ between SVD and CS (p = 0.285).
When assessing post-delivery pain duration, there were no significant differences in how long the pain lasted after SVD or CS (p = 0.59 and p = 0.39, respectively). However, community awareness of delivery complications was perceived as low, with a significant difference noted across groups (p < 0.05). The internet and obstetrician-gynecologists were the most common sources of information about pain relief during childbirth, although this was not statistically significant (p = 0.16). Breathing techniques were the most favored non-pharmacological method for pain relief during labor, with no significant difference observed between the groups (p = 0.32).
Regarding pain management after delivery, the duration of medication use was similar following SVD (p = 0.92), while after CS, there was a significant variation, with some participants requiring medication for more than a month (p < 0.05). These findings reflect the different perspectives and experiences related to SVD and CS, particularly in terms of perceived complications and pain management.
3.5 Significant factors influencing preferred mode of delivery
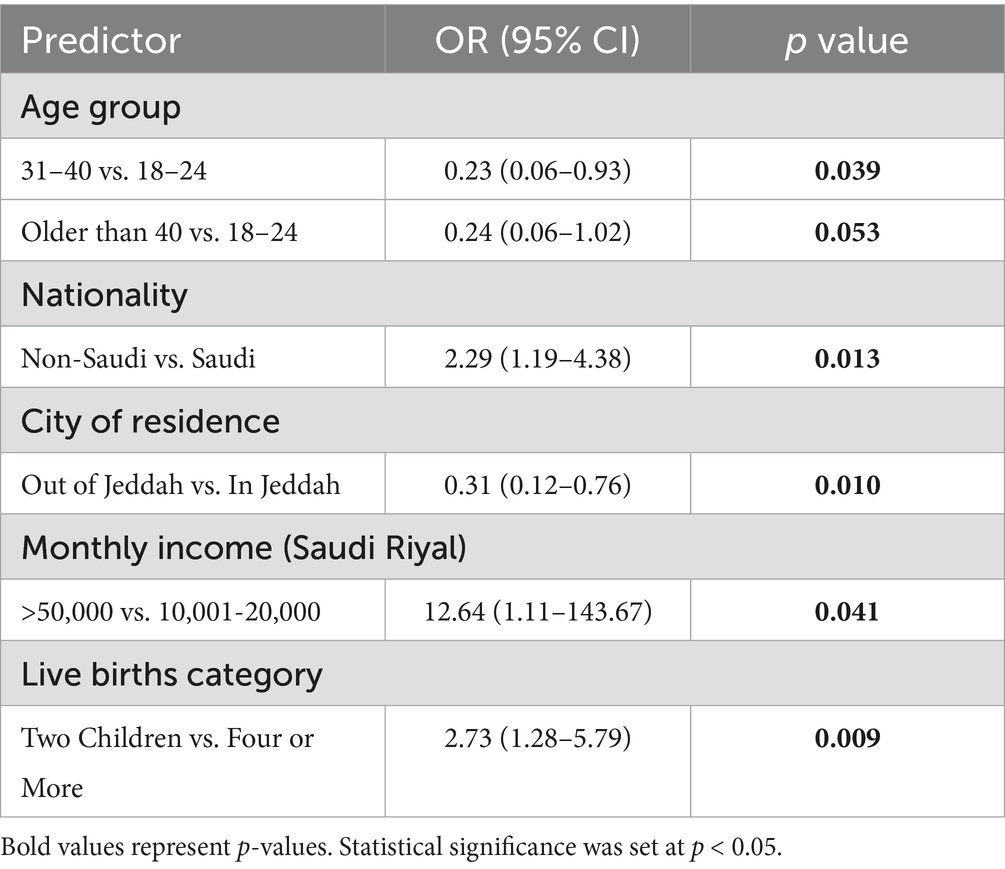
A multivariable logistic regression was performed to identify independent predictors of a preference for Cesarean Section (CS), with the full results detailed in Table 5. The analysis revealed a distinct profile of women with a higher likelihood of preferring CS. Demographically, women aged 31–40 years had significantly lower odds of preferring CS compared to the 18-24-year reference group. Conversely, non-Saudi nationality was a strong predictor, associated with more than double the odds of preferring CS compared to Saudi nationals. Socioeconomic and residential factors were also significant. Residing outside of Jeddah was associated with a substantially lower likelihood of preferring CS. Furthermore, a monthly income exceeding 50,000 SAR was the strongest socioeconomic predictor, significantly increasing the odds of a CS preference. Finally, obstetric history played a role; women with two children had significantly higher odds of preferring CS compared to those with four or more children.
4 Discussion
The study aimed to identify the preferred mode of delivery and factors influencing women preferring CS and SVD in a tertiary care center in Jeddah, Saudi Arabia. The study involved surveying women who were attending antenatal care appointments at our center. After collecting and analyzing the data, several factors and novel findings were presented in this study. Women’s autonomy can lead to a positive birth experience, and it is considered an essential part of quality maternity care (20, 21). During this significant life stage, many women desire autonomy to make their own choices about their healthcare and the well-being of their unborn child, to feel empowered to take an active role in their pregnancy journey, and to make decisions that align with their personal values and beliefs and the expected health outcome for their fetus (22, 23). Therefore, it is important to investigate factors that influence their decision.
4.1 Influence of demographics on delivery preferences
Specific demographic factors were analyzed to evaluate their impact on delivery preferences. Age was found not to be a significant factor in determining the preferred mode of delivery in our study. This result aligns with a previous study conducted in Saudi Arabia, which also found no correlation between age and delivery preference (24). However, a study in Poland reported that older women were more likely to prefer cesarean delivery, with a mean age difference of 1.25 years between those opting for CS and SVD (25).
Nationality emerged as a significant factor, with Saudi women showing a higher preference for SVD, while non-Saudi women preferred CS. This finding corroborates previous research, which also indicated a higher prevalence of CS preference among non-Saudi women (26). Additionally, residents in Jeddah and women with higher incomes were more likely to prefer CS. Notably, a prior study at King Abdulaziz Hospital in Jeddah found a preference for SVD among participants, suggesting a shift in attitudes over the past 2 years (27). As for the income variable, the wide confidence interval suggests caution in interpretation due to limited sample size in this subgroup.
4.2 Impact of CS history on delivery preferences
A significant finding of our study was the influence of previous CS on delivery preferences. Women with no prior CS were more likely to prefer SVD (p < 0.05) as seen in Figure 2. This trend is consistent with a study by Ana-man-Torgbor et al. (28), which found that most women with prior CS preferred SVD, with only 10.4% opting for CS (29). Similarly, research by Gbaranor et al. concluded that SVD was the preferred mode of delivery, with only 2.9% of participants expressing a preference for CS (30). However, a study by Zewude et al. reported a higher prevalence of CS preference (25%), which exceeds the national average (31).
Our study also highlighted the role of private hospital deliveries in shaping future preferences. Women who underwent previous CS in private hospitals were significantly more likely to prefer CS for subsequent deliveries (p < 0.05). This finding aligns with research by Rayhan, which emphasized the role of private healthcare facilities in influencing CS preference due to perceived superior quality of care (32). Similarly, Mazzoni et al. found that women delivering in private hospitals were more likely to opt for CS, even among those who initially preferred SVD (17).
4.3 Logistic regression analysis of factors influencing preferences
Logistic regression analysis identified several factors associated with delivery preference. Women aged 31–40 years had significantly lower odds of preferring CS compared to those aged 18–24 years. This finding contrasts with some literature that reports increased CS preference among older women due to concerns about pregnancy complications (33). The observed pattern in our cohort may reflect unique cultural or generational attitudes toward childbirth in our setting, though the cross-sectional design precludes determination of causal mechanisms.
Nationality also influenced delivery preferences, with non-Saudi women showing a higher likelihood of opting for CS. While previous studies have explored factors contributing to rising CS rates in Saudi Arabia, including educational status and income (34), further research is needed to investigate the specific differences between Saudi and non-Saudi women. Similarly, a study from Bangladesh identified maternal education, previous CS, and socioeconomic status as key determinants of cesarean delivery (35). Our findings regarding CS preferences take on added significance in light of recent evidence on CS-related complications. A recent regional study by Abdulrazzak et al. confirmed high CS prevalence and identified similar demographic risk factors in neighboring populations, reinforcing the regional pattern our study observed (36). Furthermore, the long-term maternal complications associated with CS, including isthmocele and subsequent infertility as highlighted by Al-Ghotani et al., underscore the importance of minimizing non-medically indicated procedures (37). From the neonatal perspective, while rare, serious complications such as portal vein thrombosis following CS delivery, as documented by Haddad et al., contribute to the comprehensive risk–benefit assessment that should inform delivery method decisions (38).
Urban residency and income levels were additional factors influencing preferences. Women residing in urban areas, particularly Jeddah, and those with higher income were associated with greater odds of preferring CS, consistent with patterns observed in other middle-income settings (39). Additionally, this finding aligns with research indicating that urban women have greater access to healthcare facilities and are more exposed to information about delivery options, which may influence their decision-making (31). Higher-income women may also perceive CS as a safer or more convenient option, especially when private healthcare services are readily accessible.
4.4 Sources of information and pain management preferences
Our study also revealed critical insights into women’s sources of information and perceptions. Notably, most participants perceived community awareness of delivery complications as low. The internet and obstetrician-gynecologists were the most common sources of information about pain relief, while breathing techniques were the most favored non-pharmacological method. These findings highlight a significant opportunity to enhance patient education through trusted digital platforms and to integrate training on non-pharmacological pain management, like breathing techniques, into routine antenatal counseling.
4.5 Clinical and policy implications
The findings of this study suggest several actionable strategies for clinical practice and public health policy including targeted education by developing evidence-based educational programs addressing misconceptions about CS, particularly for higher-income women, urban residents, and non-Saudi women. These programs should be delivered through popular channels like digital platforms and reinforced by healthcare providers. Structured antenatal counseling can be valuable by integrating structured discussions of delivery preferences, including a balanced view of risks and benefits for both CS and SVD, into routine antenatal care visits. Also, training healthcare providers in shared decision-making and effective communication is needed to ensure women’s choices are informed and aligned with clinical evidence and the incorporation of training on non-pharmacological pain management methods, such as breathing techniques, into antenatal classes to empower women and reduce fear of SVD.
4.6 Limitations
This study has several limitations that should be considered when interpreting the results. Its cross-sectional design precludes the establishment of causal relationships between the identified factors and delivery preferences. The reliance on self-reported data introduces the potential for recall bias, particularly among postpartum women reflecting on past decisions, and social desirability bias. Although the study utilized a multi-center approach, the use of convenience sampling and its restriction to a major urban center (Jeddah) may limit the generalizability of the findings to rural populations or other regions of Saudi Arabia with different healthcare landscapes and cultural norms. Furthermore, the online, self-administered nature of the survey might have excluded women with lower literacy levels or limited digital access, potentially leading to an underrepresentation of disadvantaged socioeconomic groups.
Despite these limitations, the study possesses notable strengths. The large sample size provides robust statistical power for the analyses conducted. The inclusion of a wide range of socioeconomic, demographic, and obstetric factors allows for a comprehensive exploration of determinants influencing delivery preference. Furthermore, the focus on a specific, understudied urban population in Jeddah yields valuable insights that are directly relevant to local health policy and clinical practice, providing a foundation for targeted interventions to align delivery method choices with evidence-based care,
5 Conclusion
In conclusion, our study identified nationality, income level, urban residence, and previous delivery experience as key determinants of delivery method preference among women in Jeddah. Non-Saudi women, those with higher incomes, and urban residents showed significantly greater preference for cesarean delivery, while women without prior cesarean sections predominantly preferred spontaneous vaginal delivery. These findings highlight the need for targeted educational interventions and shared decision-making approaches in antenatal care to ensure delivery method choices align with clinical evidence and individual patient values.
Data availability statement
The raw data supporting the conclusions of this article are available from the corresponding author upon reasonable request, subject to patient confidentiality considerations.
Ethics statement
The study was approved by Unit of Biomedical Ethics Research Committee (reference number: 35–24) at the Faculty of Medicine, King Abdulaziz University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NA: Conceptualization, Investigation, Supervision, Validation, Writing – original draft, Writing – review & editing. MS: Data curation, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. SB: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. AHA: Data curation, Resources, Writing – original draft, Writing – review & editing. FA: Data curation, Investigation, Writing – original draft, Writing – review & editing. KH: Data curation, Software, Writing – original draft, Writing – review & editing. ASA: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. EJ: Data curation, Visualization, Writing – original draft, Writing – review & editing. RA: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. SA: Data curation, Investigation, Writing – original draft, Writing – review & editing. MA: Conceptualization, Investigation, Supervision, Writing – original draft, Writing – review & editing. MM: Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to express their deep gratitude to all the obstetricians for their valuable time in completing the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Belizán, JM, Althabe, F, and Cafferata, ML. Health consequences of the increasing caesarean section rates. Epidemiology. (2007) 18:485–6. doi: 10.1097/EDE.0B013E318068646A
3. Belizán, JM, Cafferata, ML, Althabe, F, and Buekens, P. Risks of patient choice cesarean. Birth. (2006) 33:167–9. doi: 10.1111/J.0730-7659.2006.0098B.X
4. Betrán, AP, Merialdi, M, Lauer, JA, Bing-Shun, W, Thomas, J, Van Look, P, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. (2007) 21:98–113. doi: 10.1111/J.1365-3016.2007.00786.X
5. Althabe, F, Sosa, C, Belizán, JM, Gibbons, L, Jacquerioz, F, and Bergel, E. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth. (2006) 33:270–7. doi: 10.1111/J.1523-536X.2006.00118.X
6. Keag, OE, Norman, JE, and Stock, SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med. (2018) 15:2494. doi: 10.1371/journal.pmed.1002494
7. Nilsson, L, Thorsell, T, Wahn, EH, and Ekström, A. Factors influencing positive birth experiences of first-time mothers. Nurs Res Pract. (2013) 2013:1–6. doi: 10.1155/2013/349124
8. Abdulrahman, M, Abdullah, SS, Alaani, AFK, AlAbdool, NH, Sherif, FEY, Ahmed, ZS, et al. Exploring obstetrical interventions and stratified cesarean section rates using the Robson classification in tertiary care hospitals in the United Arab Emirates. Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics. (2019) 41:147–54. doi: 10.1055/S-0038-1676524
9. Jadoon, B, Assar, TM, Nucier, AAAR, Raziq, HEA, Abd El-Azym Saad, AS, and Megahed Amer, W. Analysis of the caesarean section rate using the 10-group Robson classification at Benha University Hospital, Egypt. Women Birth. (2020) 33:e105–10. doi: 10.1016/J.WOMBI.2019.03.009
10. Ba’aqeel, HS. Cesarean delivery rates in Saudi Arabia: a ten-year review. Ann Saudi Med. (2009) 29:179. doi: 10.4103/0256-4947.51773
11. Ahmed, AE, and Mohammad, RS. Cesarean sections. Associated factors and frequency at king Abdulaziz Medical City in the central region of the Kingdom of Saudi Arabia. Saudi Med J. (2018) 39:1154–7. doi: 10.15537/SMJ.2018.11.22499
12. Dobson, R. Caesarean section rate in England and Wales hits 21. BMJ. (2001) 323:951. doi: 10.1136/bmj.323.7319.951a
13. Gamble, J, Creedy, DK, McCourt, C, Weaver, J, and Beake, S. A critique of the literature on women’s request for cesarean section. Birth. (2007) 34:331–40. doi: 10.1111/J.1523-536X.2007.00193.X
14. Kingdon, C, Baker, L, and Lavender, T. Systematic review of nulliparous women’s views of planned cesarean birth: the missing component in the debate about a term cephalic trial. Birth. (2006) 33:229–37. doi: 10.1111/J.1523-536X.2006.00108.X
15. Eden, KB, Hashima, JN, Osterweil, P, Nygren, P, and Guise, JM. Childbirth preferences after cesarean birth: a review of the evidence. Birth. (2004) 31:49–60. doi: 10.1111/J.0730-7659.2004.0274.X
16. Gamble, JA, and Creedy, DK. Women’s request for a cesarean section: a critique of the literature. Birth. (2000) 27:256–63. doi: 10.1046/J.1523-536X.2000.00256.X
17. Elgzar, WT, Alshahrani, MS, and Ibrahim, HA-F. Mode of delivery preferences: the role of childbirth fear among nulliparous women. Front Psychol. (2023) 14:1221133. doi: 10.3389/FPSYG.2023.1221133
18. Charan, J, and Biswas, T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. (2013) 35:121–6. doi: 10.4103/0253-7176.116232
19. Salawati, E, Ghamri, R, Amir, A, Alsubaie, M, Abualsaud, R, Bahowarth, S, et al. The magnitude of influence of personal and professional factors on the career choices of medical students. J Med Life. (2024) 17:449–56. doi: 10.25122/JML-2023-0453
20. Tunçalp,, Pena-Rosas, JP, Lawrie, T, Bucagu, M, Oladapo, OT, Portela, A, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. (2017) 124:860–2. doi: 10.1111/1471-0528.14599
21. Antenatal care. London: National Institute for Health and Care Excellence (NICE) (2021). Available online at: https://pubmed.ncbi.nlm.nih.gov/34524750/ (Accessed on January 2, 2025)
22. Bibeau, AM. Interventions during labor and birth in the United States: a qualitative analysis of women’s experiences. Sex Reprod Healthc. (2014) 5:167–73. doi: 10.1016/J.SRHC.2014.10.003
23. Lucas, A. Information for women after CS: are they getting enough? RCM Midwives. (2004) 7:472. Available at: https://pubmed.ncbi.nlm.nih.gov/15612178/
24. Alshammari, RF, Khan, FH, Alkwai, HM, Alenazi, F, Alshammari, KF, Sogeir, EKA, et al. Role of parity and age in cesarean section rate among women: a retrospective cohort study in hail, Saudi Arabia. Int J Environ Res Public Health. (2023) 20:1486. doi: 10.3390/IJERPH20021486
25. Michalik, A, Wojcicka, L, Czerwińska-Osipiak, A, Zdun-Ryżewska, A, Jakitowicz, K, Olszewska, J, et al. Preferences of women with low obstetric risk for cesarean or vaginal birth in Poland: areas for intervention. Birth. (2021) 48:265–73. doi: 10.1111/BIRT.12537
26. Ahmed, AE, and Mohammad, RS. Motives for - and prevalence of - cesarean delivery on maternal request: a survey in Saudi Arabia. Qatar Med J. (2019) 2019:2. doi: 10.5339/QMJ.2019.2/CITE/REFWORKS
27. Yaqoub, RM, Khouj, MA, Alsaif, AA, Eissa, GA, Alhemdi, JA, and Albasri, S. Awareness and knowledge of caesarean section complications among women in Jeddah, Saudi Arabia. Cureus. (2022) 14:52. doi: 10.7759/cureus.32152
28. Anaman-Torgbor, JA, Konlan, KD, Owusu, E, and Gbagbo, B. Factors influencing preference of birth method among pregnant women: a descriptive cross-sectional study in a tertiary health facility in Ghana. J Glob Health Sci. (2022) 4:e11. doi: 10.35500/JGHS.2022.4.E11
29. Karlström, A, Nystedt, A, and Hildingsson, I. A comparative study of the experience of childbirth between women who preferred and had a caesarean section and women who preferred and had a vaginal birth. Sex Reprod Healthc. (2011) 2:93–9. doi: 10.1016/J.SRHC.2011.03.002
30. Gbaranor, KB, Kinako, SE, and Austin-Asomeji,. Preferred method of delivery amongst women of reproductive age in south-South Nigeria. Sch Int J Obs Gynec. (2023) 6:312–5. doi: 10.36348/sijog.2023.v06i07.008
31. Zewude, B, Siraw, G, and Adem, Y. The preferences of modes of child delivery and associated factors among pregnant women in southern Ethiopia. Pragmatic Observational Res. (2022) 13:59–73. doi: 10.2147/POR.S370513
32. Sk, R. Does delivery in private hospitals contribute largely to caesarean section births? A path analysis using generalised structural equation modelling. PLoS One. (2020) 15:e0239649. doi: 10.1371/JOURNAL.PONE.0239649
33. Šťastná, A, Fait, T, Kocourková, J, and Waldaufová, E. Does advanced maternal age comprise an independent risk factor for caesarean section? A population-wide study. Int J Environ Res Public Health. (2023) 20:668. doi: 10.3390/IJERPH20010668/S1
34. Ayman Aljabri, W, Al-Jifree, M, and Abudoraehem, OS. International journal of medicine in developing countries factors that impact favoring cesarean section among women in Saudi Arabia. Dublin: Discover STM. (2021).
35. Hossain, MS, Shuvo, SD, Asha, S, Chodhoury, MR, and Elahi, MT. Cesarean delivery and its determining factors: a hospital-based study in Jashore District, Bangladesh. Public Health Practice (Oxford, England). (2024) 8:100558. doi: 10.1016/j.puhip.2024.100558
36. Abdulrazzak, M, Alshaghel, MM, Alhashemi, M, Mayo, W, Oubari, S, Jamal, BR, et al. Prevalence and risk factors associated with cesarean section in Syria: a cross-sectional study of the two largest health centers. Health Sci Rep. (2025) 8:e70604. doi: 10.1002/hsr2.70604
37. Al-Ghotani, B, Martini, N, Alabdallah, E, Alawad, I, and Hussien, K. A large post-caesarean niche (Isthmocele) with amenorrhea, a symptom that was not reported in the medical literature: a rare case report. Int J Surg Case Rep. (2023) 109:108528. doi: 10.1016/j.ijscr.2023.108528
38. Haddad, S, Haddad, S, Swaid, K, Martini, N, Mansour, M, and Alkouri, L. Portal vein thrombosis in a 10-month-old infant as a complication of neonatal umbilical catheterization: a case report. Annals Med Surgery (2012). (2023) 85:5158–62. doi: 10.1097/MS9.0000000000001173
Keywords: cesarean section, mode of delivery, maternal health, knowledge, opinion
Citation: Aldardeir N, Sulaimani M, Bahowarth SY, Abdulaziz AH, Alghalayini FK, Halabi KW, Alyazidi AS, Jastanieh ES, Alharbi R, Alamoudi ST, Alrumaihi M and Malibary MA (2025) Patients preference for mode of delivery in a Middle Eastern society: a cross-sectional study. Front. Med. 12:1688528. doi: 10.3389/fmed.2025.1688528
Edited by:
Forough Mortazavi, Sabzevar University of Medical Sciences, IranReviewed by:
Sakhawot Hossain, Daffodil International University, BangladeshElie Ouainaty, Notre dame des secours university hospital, Lebanon
Copyright © 2025 Aldardeir, Sulaimani, Bahowarth, Abdulaziz, Alghalayini, Halabi, Alyazidi, Jastanieh, Alharbi, Alamoudi, Alrumaihi and Malibary. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anas S. Alyazidi, YWx5YXppZGkuYW5hc0BnbWFpbC5jb20=
 Nashwa Aldardeir1
Nashwa Aldardeir1 Anas S. Alyazidi
Anas S. Alyazidi