Abstract
Objective:
Kinesiology tape has shown certain effects in treating rotator cuff injuries, but its efficacy remains controversial. This study aims to evaluate the effectiveness of kinesiology tape in treating rotator cuff injuries through a systematic review and meta-analysis.
Methods:
We conducted a search in PubMed, Embase, Web of Science, Cochrane Library, CNKI, Wanfang Data and VIP databases, with the search period ending in August 2025. Randomized controlled trials (RCTs) comparing KT with comparable single rehabilitation interventions, placebos or traditional rehabilitation were included. The outcomes included shoulder pain, range of motion, and upper limb movement.
Results:
A total of 17 studies (959 participants) were included. Kinesiology tape (KT) showed a significant therapeutic effect on the shoulder pain score (MD = −0.94; 95% CI: [−1.27, −0.95], Z = 5.6, p < 0.0001, I2 = 75%). KT significantly increased the shoulder flexion range of motion (MD = 9.24; 95% CI: [3.11, 15.36], Z = 2.96, p < =0.003, I2 = 91%). KT significantly increased the shoulder abduction range of motion (MD = 9.14; 95% CI: [6.99, 11.29], Z = 8.34, p < 0.0001, I2 = 38%). KT significantly improved upper limb function (MD = –4.38; 95% CI: [−5.19, −3.57], Z = 10.64, p < 0.0001, I2 = 19%). Through subgroup analysis based on pain assessment, the differences in therapeutic effects of KT treatment were further explored in different types of control groups, treatment cycles, stimulation areas, and genders.
Conclusion:
The results of this meta-analysis indicate that KT has a significant positive effect in alleviating shoulder pain and upper limb dysfunction in patients with rotator cuff injuries. However, due to the presence of potential risk factors, the therapeutic effect of KT needs to be interpreted with caution.
1 Introduction
Rotator cuff injuries (RCIs) represent a prevalent musculoskeletal disorder affecting approximately 20–30% of the general adult population, with incidence markedly increasing with age (1, 2). These injuries encompass a spectrum of pathologies ranging from tendinopathy and partial-thickness tears to full-thickness tears, frequently resulting in persistent shoulder pain, functional impairment, diminished range of motion (ROM), and significant reductions in quality of life and occupational capacity (3–5). Conventional therapeutic approaches include physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, and surgical intervention (6, 7). However, limitations such as variable efficacy, potential adverse effects of pharmacotherapy, procedural risks associated with injections and surgery, and substantial healthcare costs underscore the ongoing need for effective, accessible, and low-risk adjunctive or alternative treatments.
Kinesiology tape (KT), an elastic therapeutic tape engineered to mimic human skin’s elasticity, has gained widespread empirical and clinical traction over the past two decades, particularly within sports medicine and rehabilitation settings (8, 9). Supporters believe that KT exerts its therapeutic effects through various biomechanical and neurophysiological mechanisms. It can provide proprioceptive feedback to enhance neuromuscular control and the position of the scapula (10, 11). By pulling the skin, it promotes microcirculation and lymphatic drainage (12). Additionally, it regulates pain perception through gating theory, providing subtle support for fatigued or injured muscles while not restricting joint movement (13). Therefore, KT is widely used in the treatment of peripheral nerve injury, with its main goal being to relieve pain, restore functional activity ability, and improve activities of daily living (14, 15).
Although KT has been widely used in clinical practice, its therapeutic effect on rotator cuff injuries remains controversial. Although numerous randomized controlled trials have investigated the impact of KT on pain intensity, shoulder function outcomes, arm, shoulder and hand disability questionnaires or the objective measurements of shoulder pain and dysfunction index, as well as joint range of motion, the results vary (16–18). Some trials report that the group treated with KT shows statistically significant and clinically meaningful improvements, whether as a standalone intervention or as an adjunct to conventional physical therapy (19, 20). In contrast, other well-designed randomized controlled trials indicate that compared with sham ligation, placebo intervention or standard care alone, kinesiology tape has little or no significant benefits (21). This inconsistency may stem from methodological differences in different studies, including ligation techniques, participant characteristics, control intervention measures, outcome measurement standards, and follow-up time.
Although previous systematic reviews and meta-analyses have attempted to synthesize the evidence on KT for shoulder pathologies, significant knowledge gaps persist. Earlier syntheses often included studies with mixed shoulder conditions (e.g., adhesive capsulitis, impingement syndrome alongside RCIs), potentially diluting injury-specific effects (22–25). Others incorporated non-randomized or lower-quality studies, introducing potential bias (26). Critically, several new high-quality RCTs focusing specifically on RCIs have been published in recent years, necessitating an updated and more focused quantitative synthesis. Furthermore, the existing meta-analyses often overlook crucial subgroup analyses, analyses of the effects of different stimulation areas or the duration of fixation, which are of vital importance for guiding evidence-based clinical practice.
2 Materials and methods
This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Ethical approval was not requisite, given that this study constitutes secondary research based on previously published articles. No conflicts of interest were present among the authors.
2.1 Literature search strategy
Two investigators conducted an electronic literature search independently to evaluate the results of the KT treatment for rotator cuff injuries. As of August 2025, the electronic databases included in the search were PubMed, Embase, the Web of Science, the Cochrane Library, the Wanfang Database, the China Journal Full-Text Database (CNKI), and the VIP Database, with the search terms limited to English and Chinese. The following search terms were used: “Kinesio Tape,” “Athletic Tape,” “Tape, Athletic,” “kinesiology tape,” “Orthotic Tape,” “Rotator Cuff Injuries,” “Cuff Injury, Rotator,” “Injury, Rotator Cuff,” “Rotator Cuff Injury,” “Rotator Cuff Tears,” “Tear, Rotator Cuff,” and so forth. Detailed search results can be found in Table 1.
Table 1
| Number | Query | Search details | Results |
|---|---|---|---|
| #7 | #3 AND #6 | ((“Rotator Cuff Injuries”[Mesh]) OR ((((((((((((((((((((Rotator Cuff Injuries) OR (Cuff Injury, Rotator)) OR (Injury, Rotator Cuff)) OR (Rotator Cuff Injury)) OR (Rotator Cuff Tears)) OR (Rotator Cuff Tear)) OR (Tear, Rotator Cuff)) OR (Tears, Rotator Cuff)) OR (Rotator Cuff Tendinitis)) OR (Rotator Cuff Tendinitides)) OR (Tendinitis, Rotator Cuff)) OR (Rotator Cuff Tendinosis)) OR (Rotator Cuff Tendinoses)) OR (Tendinoses, Rotator Cuff)) OR (Tendinosis, Rotator Cuff)) OR (Glenoid Labral Tears)) OR (Glenoid Labral Tear)) OR (Labral Tear, Glenoid)) OR (Labral Tears, Glenoid)) OR (Tear, Glenoid Labral))) AND ((“Athletic Tape”[Mesh]) OR (((((((((Athletic Tape) OR (Tape, Athletic)) OR (Orthotic Tape)) OR (Tape, Orthotic)) OR (Kinesio Tape)) OR (Kinesio Tapes)) OR (Tape, Kinesio)) OR (Tapes, Kinesio)) OR (Kinesiotape))) | 18 |
| #6 | #4 OR #5 | (“Rotator Cuff Injuries”[Mesh]) OR ((((((((((((((((((((Rotator Cuff Injuries) OR (Cuff Injury, Rotator)) OR (Injury, Rotator Cuff)) OR (Rotator Cuff Injury)) OR (Rotator Cuff Tears)) OR (Rotator Cuff Tear)) OR (Tear, Rotator Cuff)) OR (Tears, Rotator Cuff)) OR (Rotator Cuff Tendinitis)) OR (Rotator Cuff Tendinitides)) OR (Tendinitis, Rotator Cuff)) OR (Rotator Cuff Tendinosis)) OR (Rotator Cuff Tendinoses)) OR (Tendinoses, Rotator Cuff)) OR (Tendinosis, Rotator Cuff)) OR (Glenoid Labral Tears)) OR (Glenoid Labral Tear)) OR (Labral Tear, Glenoid)) OR (Labral Tears, Glenoid)) OR (Tear, Glenoid Labral)) | 15,856 |
| #5 | “rotator cuff injuries”[MeSH Terms] OR (“rotator”[All Fields] AND “cuff”[All Fields] AND “injuries”[All Fields]) OR “rotator cuff injuries”[All Fields] OR (“tear”[All Fields] AND “glenoid”[All Fields] AND “labral”[All Fields]) OR “tear, glenoid labral”[All Fields] | (((((((((((((((((((Rotator Cuff Injuries) OR (Cuff Injury, Rotator)) OR (Injury, Rotator Cuff)) OR (Rotator Cuff Injury)) OR (Rotator Cuff Tears)) OR (Rotator Cuff Tear)) OR (Tear, Rotator Cuff)) OR (Tears, Rotator Cuff)) OR (Rotator Cuff Tendinitis)) OR (Rotator Cuff Tendinitides)) OR (Tendinitis, Rotator Cuff)) OR (Rotator Cuff Tendinosis)) OR (Rotator Cuff Tendinoses)) OR (Tendinoses, Rotator Cuff)) OR (Tendinosis, Rotator Cuff)) OR (Glenoid Labral Tears)) OR (Glenoid Labral Tear)) OR (Labral Tear, Glenoid)) OR (Labral Tears, Glenoid)) OR (Tear, Glenoid Labral) | 15,856 |
| #4 | Rotator Cuff Injuries”[MeSH Terms] | “Rotator Cuff Injuries”[Mesh] Sort by: Most Recent | 8,865 |
| #3 | #1 OR #2 | (“Athletic Tape”[Mesh]) OR (((((((((Athletic Tape) OR (Tape, Athletic)) OR (Orthotic Tape)) OR (Tape, Orthotic)) OR (Kinesio Tape)) OR (Kinesio Tapes)) OR (Tape, Kinesio)) OR (Tapes, Kinesio)) OR (Kinesiotape)) | 1,538 |
| #2 | athletic tape[MeSH Terms] OR (“athletic”[All Fields] AND “tape”[All Fields]) OR “athletic tape”[All Fields] OR “kinesiotape”[All Fields] OR “kinesiotaping”[All Fields] | ((((((((Athletic Tape) OR (Tape, Athletic)) OR (Orthotic Tape)) OR (Tape, Orthotic)) OR (Kinesio Tape)) OR (Kinesio Tapes)) OR (Tape, Kinesio)) OR (Tapes, Kinesio)) OR (Kinesiotape) | 1,538 |
| #1 | “Athletic Tape”[MeSH Terms] | Search: “Athletic Tape”[Mesh] Sort by: Most Recent | 997 |
PubMed: session results.
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) Research design: randomized controlled trial; (2) Patient population: rotator cuff injury; (3) Intervention measures: exercise therapy; (4) Control group: placebo, sham therapy or conventional rehabilitation; (5) Outcomes: pain, joint range of motion and function.
Exclusion criteria: (1) Exclude cases from animal experiments; (2) Exclude cases with incomplete data; (3) Exclude cases that received improper intervention measures; (4) Exclude cases from non-randomized controlled trials.
2.3 Literature review and data extraction
The data were independently extracted by two reviewers, while the third reviewer integrated these data. A data extraction form had been pre-designed. The valid extracted data included: (1) research data, such as authors, methods, years and countries; (2) population characteristics, including sample size, gender and age; (3) intervention methods, stimulus range; (4) outcome indicators, extracting average values and standard deviations of pain scores, upper limb function scores, shoulder flexion and abduction range of motion.
2.4 Evaluation of the quality of the literature
Risk of bias assessment across the included studies was performed using the Cochrane Risk of Bias tool. This evaluation systematically appraised potential sources of bias in seven critical domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias.
2.5 Statistical analyses
Statistical analyses were conducted utilizing RevMan 5.3 (The Cochrane Collaboration) and Stata 17.0 (StataCorp LP). Study heterogeneity was evaluated primarily via the Chi-square test. A fixed-effect model was employed for analyses demonstrating low heterogeneity (I2 ≤ 50%). In instances of substantial heterogeneity (I2 > 50%), a random-effects model was implemented. Subsequent investigations into heterogeneity sources were performed through subgroup analyses, sensitivity analyses, and meta-regression. Continuous outcome variables are expressed as mean differences (MD) with corresponding 95% confidence intervals (CI). Statistical significance was established at a two-sided p-value threshold of < 0.05 (27).
3 Results
3.1 Results of the literature search
The literature search and screening process is depicted in Figure 1. Initial searches across relevant databases yielded 151 potentially eligible publications (101 English-language articles: PubMed n = 18, Embase n = 32, Web of Science n = 25, Cochrane Library n = 26; 50 Chinese-language articles: CNKI n = 10, Wanfang n = 30, VIP n = 10). Following import into EndNote software, 62 duplicate records were identified and removed. Subsequent screening of titles and abstracts resulted in the exclusion of a further 72 articles. Ultimately, 17 randomized controlled trials (RCTs) investigating the use of KT for rotator cuff injuries met the inclusion criteria (28–44). No additional relevant articles were identified from other sources. Two researchers independently performed the screening process, with consensus achieved at all stages.
Figure 1

Flowchart of literature screening.
3.2 Basic characteristics and quality assessment of included studies
The characteristics of the included studies are summarized in Table 2. This systematic review incorporated a total of 17 randomized controlled trials (RCTs), comprising 11 (28–38) English-language and 6 (39–44) Chinese-language publications. Data from 959 patients diagnosed with rotator cuff injuries were analyzed (436 males, 523 females). Sample sizes across the studies ranged from 39 to 92 participants. Regarding interventions, KT was applied as the sole intervention in the experimental groups of 6 (28, 31, 32, 36–38) RCTs, while the remaining RCTs combined KT with other physical therapies. For outcome measures, pain was assessed in 15 (28–32, 34, 36–44) studies, shoulder flexion range of motion (FLE) in 12 (29, 31, 34–41, 43, 44) studies, shoulder abduction range of motion (ABD) in 11 (29, 34–41, 43, 44) studies, and the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire was reported in 6 (29, 30, 32, 33, 36, 38) studies. The risk of bias assessment for the included RCTs was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions, evaluating seven specific domains. In the assessment of the risk of bias for 17 studies, 1 (33) study showed a relatively high risk of bias in at least one aspect, while the other 16 (28–32, 34–44) studies indicated that the risk of bias was unclear in at least one aspect. Overall, the risk of bias rating for these studies was “unclear,” due to the insufficiently detailed reporting of the concealment of allocation. Most studies did not mention the relevant details of blinding, resulting in the classification of most studies’ blinding as “unclear.” As shown in Figures 2, 3.
Table 2
| Inclusion study | Yr | Intervention measure | Design | Age | Gender (female/male) | N | Stimulation area | Period | Outcome | Country |
|---|---|---|---|---|---|---|---|---|---|---|
| De Oliveira (20) | 2021 | KT + RET/RET | 2-arm RCT | 30.9 ± 9 29.4 ± 7.5 | 11/15 11/15 |
26/26 | Trapezius, supraspinatus, deltoid muscle | 6WK | VAS, DASH, FLE, ABD | Canada |
| Reynard (31) | 2018 | KT/PB | 2-arm RCT | 59 ± 9 60 ± 10 |
4/16 5/14 |
20/19 | Trapezius, supraspinatus, deltoid muscle | 6WK | VAS, FLE | Switzerland |
| Taik (32) | 2022 | KT/PB | 2-arm RCT | 57.2 ± 6.62 57.12 ± 8.88 |
23/2 23/2 | 25/25 | Supraspinatus, deltoid muscle | 2WK | VAS, DASH | Morocco |
| Bac (33) | 2020 | KT + RET/RET | 2-arm RCT | 45.67 ± 9.29 48.17 ± 10.35 |
15/15 17/13 | 30/30 | Deltoid muscle | 6WK | DASH | Czech |
| Durgut (36) | 2024 | KT/CT | 2-arm RCT | 44 ± 5.64 44.47 ± 7.16 |
14/9 10/13 | 23/23 | Trapezius, supraspinatus, deltoid muscle | 1WK | NRS, DASH, FLE, ABD | Turkey |
| Thelen (37) | 2008 | KT/PB | 2-arm RCT | 21.3 ± 1.7 19.8 ± 1.5 | 2/19 4/17 |
21/21 | Trapezius, supraspinatus, deltoid muscle | 1WK | VAS, FLE, ABD | America |
| Miccinilli (28) | 2018 | KT/PB | 2-arm RCT | 61 ± 12 64 ± 10 |
12/9 10/9 |
21/19 | Deltoid muscle | 1WK | NRS | Italy |
| Martin (35) | 2020 | KT + RET/KT/RET | 3-arm RCT | 46.95 ± 10.74 48.65 ± 10.27 49.2 ± 13.13 | 12/8 14/6 16/4 |
20/20/20 | Trapezius, supraspinatus, deltoid muscle | 2WK | FLE, ABD | Brazil |
| Analay (38) | 2018 | KT/PB | 2-arm RCT | 48.86 ± 10.03 54.15 ± 10.22 | 17/12 18/9 |
29/27 | Deltoid muscle | 1WK | VAS, DASH, FLE, ABD | Turkey |
| ÇiFtçi (30) | 2020 | KT + RET/RET | 2-arm RCT | 59.72 ± 2.94 58.52 ± 5.9 | 39/7 25/21 |
46/46 | Trapezius, supraspinatus, deltoid muscle | 3WK | VAS, DASH | Turkey |
| Nguyen (34) | 2025 | KT + RET/RET | 2-arm RCT | 51.27 ± 12.64 57.6 ± 13.4 | 30/10 29/11 |
40/40 | Deltoid muscle | 2WK | VAS, FLE, ABD | Vietnam |
| Chen (39) | 2020 | KT + RET/RET | 2-arm RCT | 43.28 ± 9.27 46.35 ± 10.85 |
12/19 14/17 |
31/31 | Biceps, deltoid muscles | 4WK | VAS, FLE, ABD | China |
| Bao (40) | 2023 | KT + RET/RET | 2-arm RCT | 49.63 ± 7.6 50.17 ± 8.23 |
10/20 6/24 |
30/30 | Trapezius, deltoid muscles | 4WK | VAS, FLE, ABD | China |
| Yuan (41) | 2024 | KT + RET/RET | 2-arm RCT | 50.6 ± 8.43 53.53 ± 7.45 | 17/13 19/11 |
30/30 | Biceps brachii, supraspinatus muscle, deltoid muscle | 1WK | VAS, FLE, ABD | China |
| Wang (42) | 2019 | KT + RET/RET | 2-arm RCT | 57.1 ± 4.35 56.65 ± 4.02 | 12/8 14/6 |
20/20 | Trapezius, supraspinatus, deltoid muscle | 2WK | VAS | China |
| Jia (43) | 2022 | KT + RET/RET | 2-arm RCT | 53.7 ± 11.14 50 ± 12.63 | 10/10 10/10 |
20/20 | Trapezius, supraspinatus, deltoid muscle | 4WK | VAS, FLE, ABD | China |
| Li (44) | 2022 | KT + RET/RET | 2-arm RCT | 49.63 ± 6.68 51.27 ± 5.54 | 18/22 20/20 |
40/40 | Trapezius, supraspinatus, deltoid muscle | 4WK | VAS, FLE, ABD | China |
The general date of the included studies.
DASH = Disabilities of the Arm, Shoulder and Hand questionnaire; CT = cold therapy; ESWT = Extracorporeal shock wave therapy; PB = Placebo; RET = Rehabilitation treatment; FLE = Flexion; ABD = Abduction; RCT = Randomized Controlled Trial; VAS = Visual Analogue Scale; NRS = Numerical Rating Scale.
Figure 2

Risk of bias graph.
Figure 3

Risk of bias summary.
3.3 Outcome
3.3.1 Pain assessment
Pain outcomes were assessed using the Visual Analogue Scale (VAS) or the Numerical Rating Scale (NRS). The meta-analysis included 17 studies involving 839 patients. Significant heterogeneity was observed among the included studies (I2 = 75%). Consequently, a random-effects model was employed for the analysis. The results demonstrated a significantly greater reduction in pain in the KT group compared to the control group (MD = −0.94; 95% CI: [−1.27, −0.61], Z = 5.6, p < 0.0001 Figure 4). To explore potential sources of heterogeneity, subgroup analyses were performed based on intervention type, intervention duration, participant gender, and anatomical site of application (Table 3). Significant pain relief was observed in all subgroups. However, no statistically significant subgroup effects were identified for any of these variables.
Figure 4

Forest plot for effectiveness of kinesio taping on changes in pain.
Table 3
| Variables | Group (n) | Participant (n) |
MD [95%Cl] | P | I2% | Sub-group difference | |
|---|---|---|---|---|---|---|---|
| x 2 | p | ||||||
| Intervention measure | |||||||
| PB | 5 | 227 | −0.59[−1.02,-0.16] | 0.007 | 20% | 2.89 | 0.09 |
| RET | 10 | 612 | −1.11[−1.54,-0.69] | <0.00001 | 82% | ||
| Period | |||||||
| ≥4WK | 6 | 333 | −0.9[−1.42,-0.39] | 0.0006 | 73% | 0.03 | 0.86 |
| <4WK | 9 | 506 | −0.96[−1.42,-0.51] | <0.00001 | 78% | ||
| Gender | |||||||
| Female > Male | 8 | 464 | −1.07[−1.52,-0.61] | <0.00001 | 79% | 0.97 | 0.32 |
| Female < Male | 6 | 799 | −0.7[−1.26,-0.15] | 0.010 | 74% | ||
| Apply stimulation to the designated area | |||||||
| Through the action of large muscle groups | 9 | 491 | −1.09[−1.64,-0.54] | <0.00001 | 79% | 1.17 | 0.28 |
| Not achieved through the action of large muscle groups | 6 | 348 | −0.74[−1.07,-0.41] | <0.00001 | 58% | ||
Effects of KT on pain scale improvement: subgroup analysis.
MD: mean difference; CI: confidence interval.
3.3.2 Evaluation of shoulder flexion
A total of 12 studies evaluated the shoulder flexion condition, involving 693 patients. Heterogeneity analysis revealed significant differences among the studies (I2 = 91%). After analysis using the random effects model, the results indicated that the KT group showed better improvement in shoulder flexion compared to the control group, and the results were statistically significant (MD = 9.24; 95% CI: [3.11, 15.36], Z = 2.96, p = 0.003). As shown in Figure 5.
Figure 5
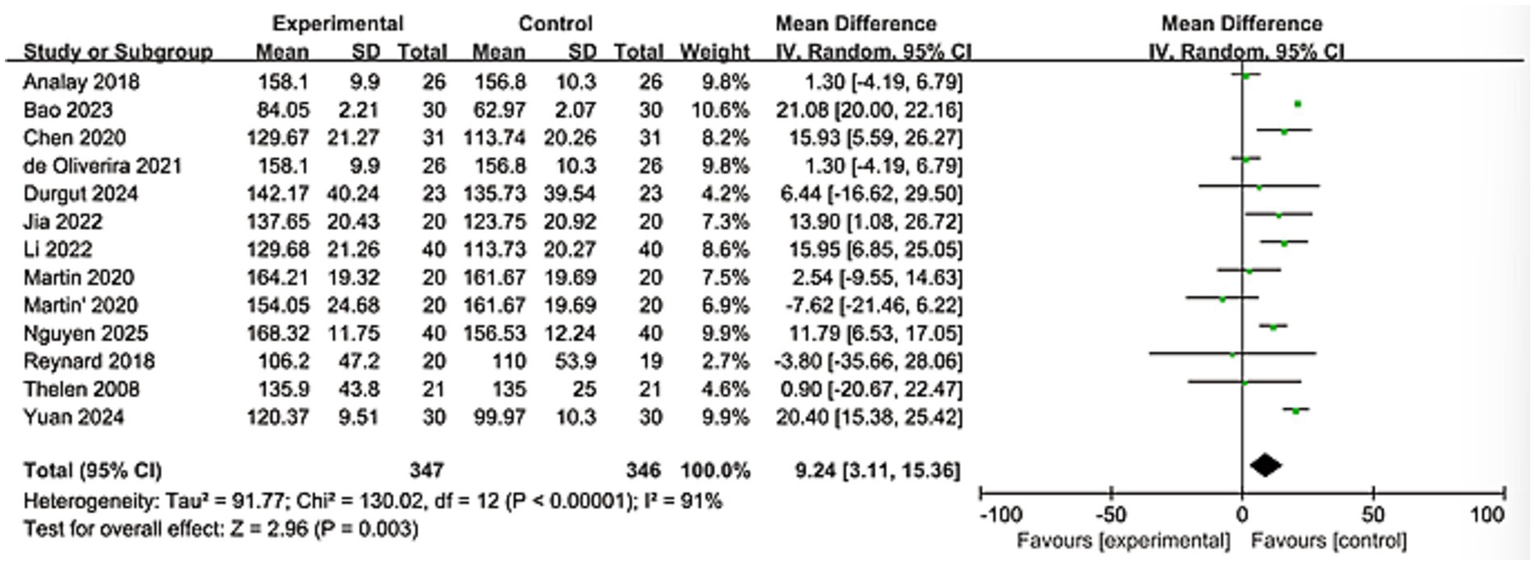
Forest plot of the effectiveness of kinesio tape on forward flexion changes.
3.3.3 Evaluation of shoulder abduction
A total of 11 studies evaluated the shoulder abduction situation, involving 654 patients. Heterogeneity analysis showed significant differences among the studies (I2 = 38%). After analysis using the fixed-effect model, the results indicated that the KT group had better improvement in shoulder abduction compared to the control group, and the results were statistically significant (MD = 9.14; 95% CI: [6.99, 11.29], Z = 8.34, p < 0.0001). As shown in Figure 6.
Figure 6
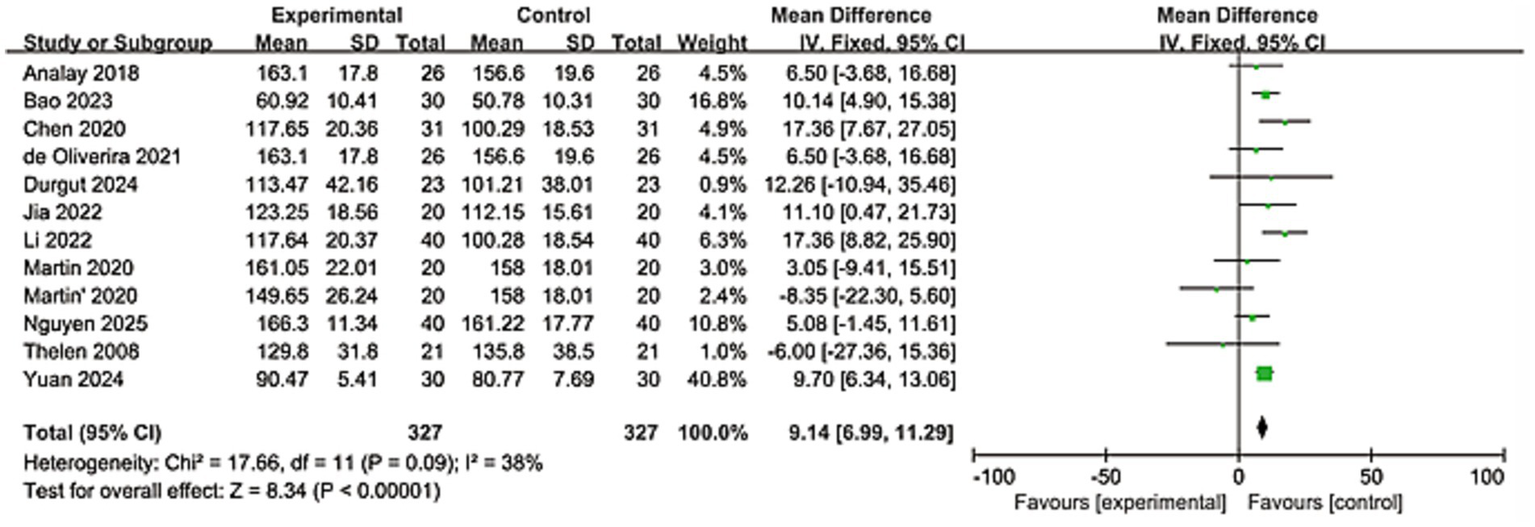
Forest plot showing the effectiveness of the kinesio taping on the external rotation change.
3.3.4 Upper limb function assessment
A total of 6 studies were included in the analysis, involving a total of 356 patients. The evaluation index was the Disabilities of the Arm, Shoulder and Hand score (DASH). Heterogeneity analysis showed significant differences among the studies (I2 = 19%). A fixed-effect model was used for analysis, and the results showed that the improvement in upper limb motor function in the KT group was better than that in the control group, and the results were statistically significant (MD = −4.38; 95% CI: [−5.19, −3.57], Z = 10.64, p < 0.0001). As shown in Figure 7.
Figure 7
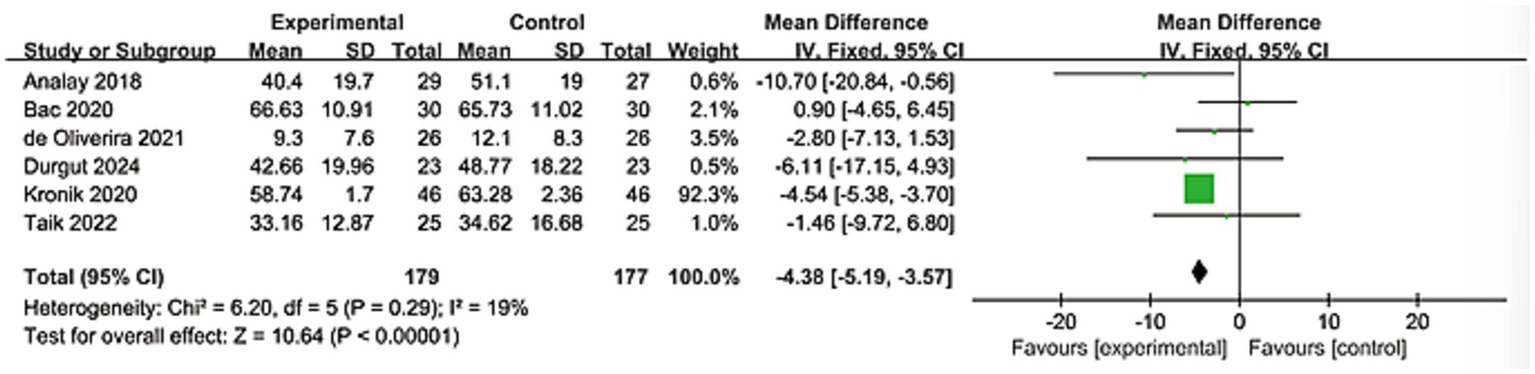
Forest plot showing the effectiveness of the kinesio taping on the changes in shoulder disability.
3.4 Sensitivity analysis
Sensitivity analysis employing the leave-one-out method confirmed the stability of the pooled estimate. Sequential exclusion of individual studies yielded consistently negative 95% confidence intervals, supporting the robustness of the results. No single study significantly altered the magnitude or direction of the pooled effect (Figure 8).
Figure 8

Sensitivity analysis of pain conditions in patients with rotator cuff injuries in the two groups.
3.5 Publication bias
Publication bias was assessed using Egger’s and Begg’s tests for the primary outcome of shoulder pain relief in rotator cuff injury. Both tests indicated no significant publication bias (Egger’s test: p = 0.703; Begg’s test: p = 0.584) (Figures 9, 10).
Figure 9
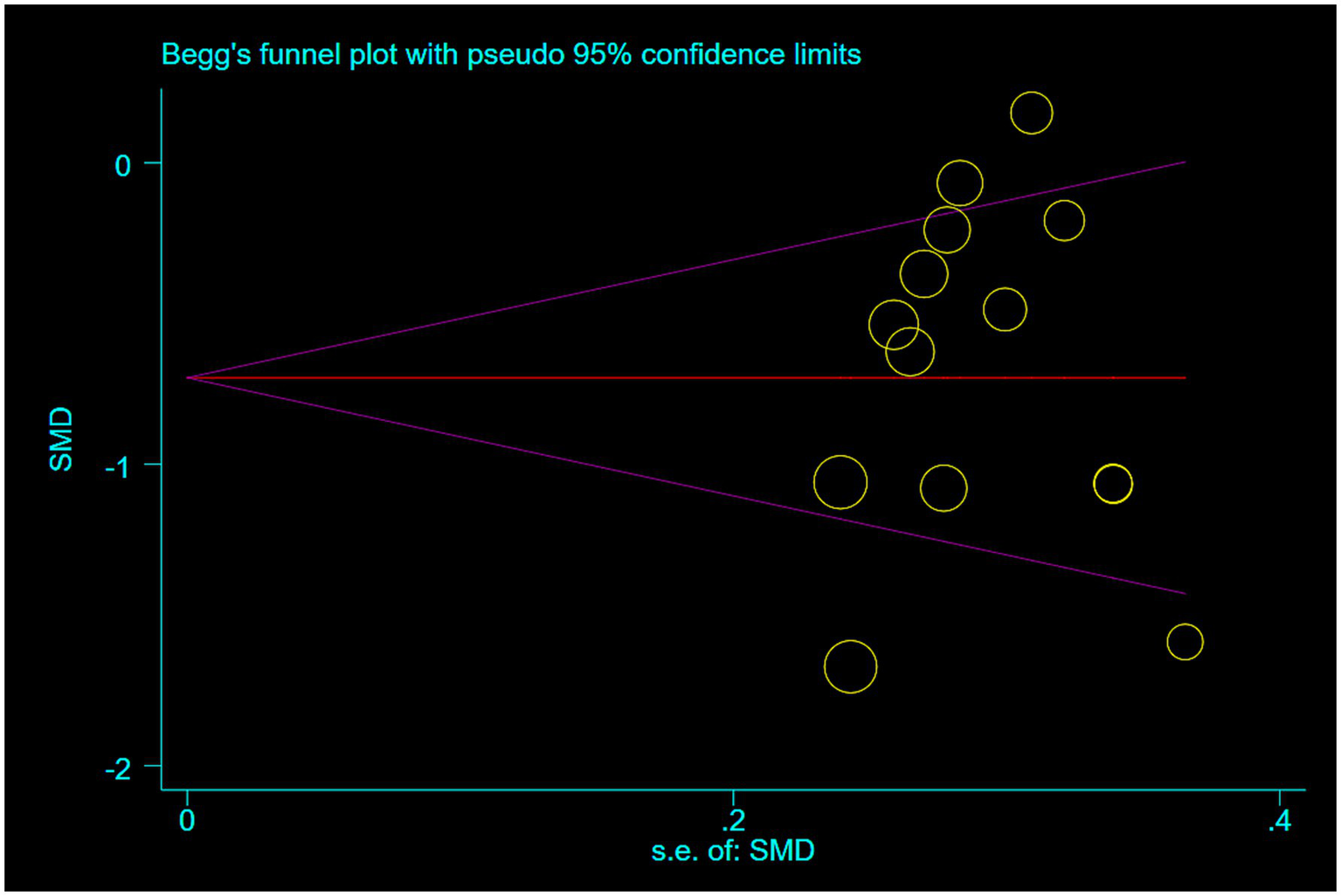
Begg’s funnel plot with pseudo 95% confidence limits.
Figure 10
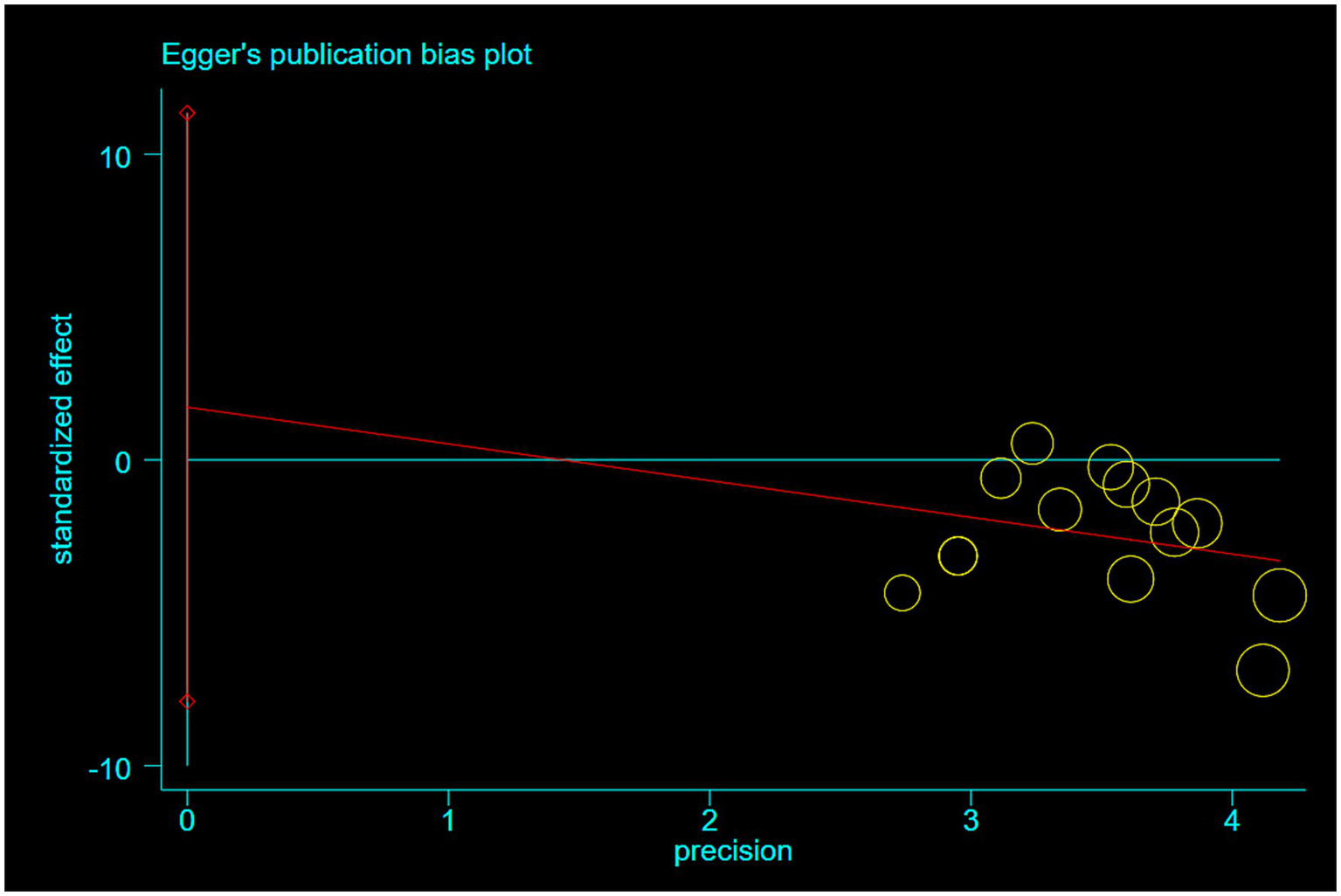
Egger’s publication bias plot.
4 Discussion
The significant pain reduction (MD = −0.94, 95% CI: −1.27 to −0.61; p < 0.0001) approaches the minimal clinically important difference (MCID) for shoulder pain scales (typically 1.0–1.5 points on VAS/NRS), suggesting clinically meaningful relief (45, 46). This aligns with proposed neurophysiological mechanisms of KT, including: Gate control theory modulation: Tactile stimulation from tape may inhibit nociceptive signaling. Proprioceptive enhancement: Improved scapular positioning and neuromuscular control. Microcirculatory effects: Mechanical lift of skin facilitating lymphatic drainage and edema reduction. For functional outcomes, improvements in shoulder flexion (MD = 9.24°) and abduction (MD = 9.14°) exceed reported MCIDs for ROM in RCIs (5°–10°) (47). The greater heterogeneity in flexion (I2 = 91%) versus abduction (I2 = 38%) may reflect methodological variations in ROM assessment or biomechanical complexity of flexion kinematics. The significant differences observed, particularly in terms of pain relief and stretching efficacy, require us to interpret the aggregated results with caution and meticulousness. These differences are likely the result of the combined influence of various clinical and methodological factors. This high degree of heterogeneity indicates that the therapeutic effect of KT varies depending on specific circumstances. Although the consistent direction of the effects in the study supports its general applicability, the magnitude of the specific effects may be modulated by specific implementation methods and patient subgroups. The robust functional improvement DASH (MD = −4.38) further supports KT’s role in restoring daily activities, though its magnitude falls below the DASH MCID (10–15 points), warranting cautious interpretation (48, 49). These findings collectively present a nuanced clinical picture. The proximity of the pain reduction to the MCID threshold, coupled with the sub-MCID improvement in the DASH score, necessitates a careful distinction between statistical significance and clinical importance. The potential for publication bias was statistically assessed using Egger’s and Begg’s tests. The results indicated no significant evidence of small-study effects for the primary outcomes of pain. This meta-analysis synthesizes evidence from 17 randomized controlled trials, demonstrating that kinesiology tape (KT) significantly alleviates pain, improves shoulder mobility (flexion and abduction), and enhances upper limb function in patients with rotator cuff injuries (RCIs). The consistency of these effects across diverse outcome measures strengthens the clinical relevance of KT as a therapeutic adjunct. Yet this efficacy exists in tension with persistent methodological heterogeneity and unresolved questions regarding its mechanistic interface with the underlying pathoanatomy of rotator cuff pathology. Reconciling this duality demands a critical appraisal of KT’s action within the intricate biological and biomechanical landscape of tendon degeneration.
The subgroup analyses reveal a critical consensus: KT consistently alleviates pain across diverse clinical scenarios, with no statistically significant moderating effects observed for intervention type, treatment duration, gender distribution, or taping mechanism. The type of intervention and the duration of treatment directly influence the clinical decisions regarding how and for how long to apply KT. There was no significant gender-related modulation effect, although this needs to be interpreted with caution as it is an assessment at the research level. However, it initially suggests that the analgesic effect of KT may be generally applicable across different patient populations. This highlights its potential as a flexible intervention measure that can adapt to various clinical needs without reducing efficacy. The considerable statistical heterogeneity (I2 = 75%) prompts a more nuanced interpretation. The absence of significant subgroup effects suggests that the observed variability is likely attributable to subtler methodological and clinical distinctions rather than the predefined high-level factors. This heterogeneity may arise from a confluence of sources, such as specific technical applications of taping, the spectrum of comparator interventions (from pure placebo to active controls), and underlying clinical diversity in patient populations. Consequently, while the direction of the treatment effect is consistently positive, the high heterogeneity implies that the precise magnitude of pain relief afforded by KT is context-dependent. This underscores that the finding represents a robust trend rather than a uniform effect size and highlights the imperative for standardized reporting in future research to better delineate its optimal application. Notably, the directionality of certain trends warrants mechanistic consideration. The numerically greater pain reduction in studies with female-dominant cohorts may reflect sex-based differences in cutaneous mechanoreceptor density or central pain processing, though this requires validation via stratified RCTs. Similarly, the trend toward superior efficacy when targeting large muscle groups versus localized neuromodulation aligns with biomechanical principles: scapulothoracic stabilization fundamentally modifies rotator cuff load transmission, whereas focal sensory input primarily modulates peripheral nociception.
The pathophysiological cascade in rotator cuff injuries involves a self-perpetuating cycle: initial collagen fiber microtrauma disrupts force transmission, precipitating compensatory scapular dyskinesia and subacromial impingement. This mechanical dysfunction fuels neurogenic inflammation and nociceptor sensitization, culminating in pain-mediated movement inhibition and functional decline (50, 51). KT’s therapeutic efficacy stems from its ability to interrupt this deleterious loop through neuromodulatory and biomechanical pathways. By enhancing cutaneous proprioceptive feedback, KT refines cortical representation of scapular position, facilitating normalized recruitment of rotator cuff musculature and mitigating aberrant joint loading patterns that perpetuate tissue stress (52). For pain relief, the continuous sensory input from the tape is thought to modulate pain perception through the pain-gate theory, reducing the central transmission of nociceptive signals (53). Concurrently, its elastic recoil creates subtle subdermal convolutions, potentially augmenting lymphatic drainage and venous return within the peritendinous space, thereby dampening local inflammatory mediators (54). This mechanistic profile clarifies KT’s strength in delivering rapid symptomatic relief, similar to the transient anti-inflammatory action of corticosteroids. However, it simultaneously reveals KT’s inherent limitation: as an external biomechanical modulator, KT cannot directly resolve the core pathology of chronic rotator cuff injuries, including tendon matrix disorganization, fatty infiltration, and the intrinsic deficit in healing capacity (55, 56).
The translation of KT’s symptomatic efficacy into clinical practice thus necessitates strategic integration within a broader therapeutic paradigm. Its profound value lies not as a monotherapy aimed at structural restoration, but as a catalyst for functional engagement during the critical early phases of rehabilitation. By effectively reducing pain inhibition and improving movement confidence, KT creates a vital window of opportunity to initiate and sustain mechanoactive interventions—particularly progressive tendon-loading exercises—which are indispensable for driving collagen realignment and tensile strengthening through mechanotransduction (57, 58). This synergistic relationship explains why combined KT and exercise regimens frequently outperform either approach in isolation. Furthermore, KT’s exceptional safety profile, characterized predominantly by minor cutaneous reactions, positions it as a low-risk adjunct in contexts where corticosteroid injections pose unacceptable risks of tendon atrophy or where surgical intervention is premature or contraindicated (59). However, the persistent heterogeneity observed across trials, unmitigated even by rigorous subgroup analyses, serves as a potent reminder that KT’s application is not universally algorithmic. Its efficacy is intrinsically context-dependent, modulated by variables such as tear morphology (partial versus full-thickness), baseline kinematic deficits, and individual pain thresholds, demanding a precision-based approach rather than protocolized uniformity.
Current evidence remains limited by unresolved heterogeneity and insufficient long-term data. Furthermore, the inconsistency in the measurement results, the characteristics of the samples, and the differences in the KT application techniques may have certain impacts on this meta-analysis. To advance KT’s clinical translation, future studies must establish standardized application protocols through biomechanical modeling, while prioritizing longitudinal designs that integrate quantitative imaging biomarkers (e.g., tendon elastography, fat fraction MRI) with real-world functional outcomes. This integrated approach will ultimately clarify KT’s capacity to modify structural progression and inform precision rehabilitation strategies for rotator cuff injuries.
5 Conclusion
In conclusion, this meta-analysis provides evidence that KT application significantly reduces shoulder pain, improves shoulder flexion and abduction range of motion, and enhances upper limb function in patients with rotator cuff injuries in the short term. While substantial heterogeneity exists, particularly for pain and flexion outcomes, the direction of effect is consistently positive, and findings are robust to sensitivity analysis. KT represents a viable, low-risk therapeutic option. Future research should focus on standardizing protocols, understanding long-term effects, and identifying patient subgroups most likely to benefit.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LZ: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Writing – original draft, Writing – review & editing. ZT: Data curation, Investigation, Project administration, Software, Supervision, Writing – review & editing. LC: Data curation, Formal analysis, Investigation, Software, Writing – review & editing. DZ: Conceptualization, Data curation, Investigation, Writing – review & editing. HH: Conceptualization, Data curation, Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AbbreviationsABD, Abduction; CI, Confidence Interval; CNKI, China National Knowledge infrastructure; CT, cold therapy; DASH, Disabilities of the Arm, Shoulder and Hand; FLE, Flexion; KT, Kinesiology tape; MCID, Minimal clinically important difference; MD, Mean difference; NRS, Numerical Rating Scale; NSAID, Non-steroidal anti-inflammatory drugs; PB, Placebo; RET, Rehabilitation treatment; RCI, Rotator cuff injurie; RCT, Randomized Controlled Trial; ROM, Range of motion; VAS, Visual Analogue Scale; VIP, Weipu.
References
1.
Barros EDM Finizola Costa Junior E Matsunaga FT Pompilio Da Silva M Dobashi ET Tamaoki MJS . Effectiveness of oral medications in the perioperative period of rotator cuff injuries - systematic review. Acta ortop bras. (2025) 33:e286067. doi: 10.1590/1413-785220253302e286067
2.
Quan X Wu J Liu Z Li X Xiao Y Shu H et al . Outcomes after double-layer repair versus En masse repair for delaminated rotator cuff injury: a systematic review and Meta-analysis. Orthop J Sports Med. (2023) 11:23259671231206183. doi: 10.1177/23259671231206183
3.
Gupta A Migliorini F Maffulli N . Management of rotator cuff injuries using allogenic platelet-rich plasma. J Orthop Surg Res. (2024) 19:165. doi: 10.1186/s13018-024-04657-4
4.
Kucirek NK Confino JE Feeley B Davies MR . Evaluation and Management of Rotator Cuff Tears Following Shoulder Dislocation. Curr Rev Musculoskelet Med. (2025) 18:323–30. doi: 10.1007/s12178-025-09970-x
5.
Liu A Zhang B Lai T Wang M Wu G Liu S et al . Comparison of functional outcomes following early and delayed arthroscopic repair for traumatic and non-traumatic rotator cuff injuries. J Orthop Surg Res. (2024) 19:368. doi: 10.1186/s13018-024-04858-x
6.
Xiao P Zhang G Wu W Huang Y Guan B Tang X . Knowledge, attitudes, and practices toward postoperative rehabilitation among females with rotator cuff injury: a cross-sectional study. J Orthop Surg Res. (2025) 20:516. doi: 10.1186/s13018-025-05928-4
7.
Wang Z-Y Zhang Y Pei H Wang C He B-J . Electroacupuncture combined with rehabilitation techniques for patients with rotator cuff injury. World J Clin Cases. (2025) 13:13. doi: 10.12998/wjcc.v13.i17.98692
8.
Erdeo F Uca AU Çankaya M Yılmaz NA . Does kinesio taping affect balance in individuals with multiple sclerosis?Neurol Sci. (2025) 46:3183–90. doi: 10.1007/s10072-025-08115-9
9.
Lu J Liu J Chen Y Sheng Y Chen L He F et al . Effects of Kinesio taping and extracorporeal shock wave therapy in combination with exercise in sarcopenic older adults: a study protocol of a double-blinded, randomized controlled trial. BMC Geriatr. (2025) 25:560. doi: 10.1186/s12877-025-06251-7
10.
Liu R Liu Y Zhou L Qian L Chen C Wan X et al . Muscle synergy and kinematic synergy analyses during sit-to-stand motions in hallux valgus patients before and after treatment with Kinesio taping. Biomed Eng Online. (2024) 23:74. doi: 10.1186/s12938-024-01268-2
11.
Comuk Balci N Anuk Ince D Ecevit A Erdoğan B Doğan IE Turan O et al . Impact of Kinesio taping on Oral feeding and swallowing functions: acoustic analysis of swallowing sounds in late preterm infants—a randomized clinical trial. Children. (2025) 12:369. doi: 10.3390/children12030369
12.
Opara JA Fiałkowski T . The effect of kinesiology taping on posture, balance, and gait in patients suffering from low Back pain. Diagnostics. (2024) 14:2506. doi: 10.3390/diagnostics14222506
13.
Cheng L Jiang Y He B . Effects of vibration training combined with kinesio taping on delayed onset muscle soreness of athletes’ knee joints post-DOMS induction: a randomised controlled trial. Front Bioeng Biotechnol. (2025) 13:1561309. doi: 10.3389/fbioe.2025.1561309
14.
Lin X Zhang J Wu M Li J Song W Zhu L . The effect of Kinesio taping on motor function in children with cerebral palsy: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. (2025) 16:1527308. doi: 10.3389/fneur.2025.1527308
15.
Abd-Eltawab AE Ameer MA . Effect of Kinesio taping versus mechanical cervical traction combined with physiotherapy program on chronic neck pain in young female university students. Hong Kong Physiother J. (2024) 44:69–78. doi: 10.1142/S1013702524500082
16.
Ager AL De Oliveira FCL Roy J-S Borms D Deraedt M Huyge M et al . Effects of elastic kinesiology taping on shoulder proprioception: a systematic review. Braz J Phys Ther. (2023) 27:100514. doi: 10.1016/j.bjpt.2023.100514
17.
Huxel Bliven KC Picha KJ . Improvements in shoulder research and rehabilitation. J Sport Rehabil. (2019) 28:217–8. doi: 10.1123/jsr.2019-0028
18.
Nie S Qin H Tan H Zhao P Yan W Zhou A et al . Suture tape anchors for enhancing healing in rotator cuff tears: a retrospective cohort study. BMC Musculoskelet Disord. (2025) 26:470. doi: 10.1186/s12891-025-08728-3
19.
Leong HT Ng GY Fu SN . Effects of scapular taping on the activity onset of scapular muscles and the scapular kinematics in volleyball players with rotator cuff tendinopathy. J Sci Med Sport. (2017) 20:555–60. doi: 10.1016/j.jsams.2016.10.013
20.
De Oliveira FCL Pairot De Fontenay B Bouyer LJ Roy J-S . Immediate effects of kinesiotaping on acromiohumeral distance and shoulder proprioception in individuals with symptomatic rotator cuff tendinopathy. Clin Biomech. (2019) 61:16–21. doi: 10.1016/j.clinbiomech.2018.11.005
21.
Zanca GG Grüninger B Mattiello SM . Effects of Kinesio taping on scapular kinematics of overhead athletes following muscle fatigue. J Electromyogr Kinesiol. (2016) 29:113–20. doi: 10.1016/j.jelekin.2015.06.005
22.
Smith M Sparkes V Busse M Enright S . Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: is there imbalance and can taping change it?Phys Ther Sport. (2009) 10:45–50. doi: 10.1016/j.ptsp.2008.12.002
23.
Kul A Ugur M . Comparison of the efficacy of conventional physical therapy modalities and Kinesio taping treatments in shoulder impingement syndrome. Eurasian J Med. (2019) 51:138–43. doi: 10.5152/eurasianjmed.2018.17421
24.
Tudini F Jordon M Levine D Healy M Cathey S Chui K . Evaluating the effects of two different kinesiology taping techniques on shoulder range of motion and proprioception in patients with hypermobile Ehlers–Danlos syndrome: a randomized controlled trial. Front Rehabil Sci. (2024) 5:1383551. doi: 10.3389/fresc.2024.1383551
25.
Gianola S Iannicelli V Fascio E Andreano A Li LC Valsecchi MG et al . Kinesio taping for rotator cuff disease. Cochrane Database Syst Rev. (2021) 8:CD012720. doi: 10.1002/14651858.CD012720.pub2
26.
Williams S Whatman C Hume PA Sheerin K . Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med. (2012) 42:153–64. doi: 10.2165/11594960-000000000-00000
27.
Luo Y Chen X Shen X Chen L Gong H . Effectiveness of Kinesio tape in the treatment of patients with patellofemoral pain syndrome: a systematic review and meta-analysis. Medicine. (2024) 103:e38438. doi: 10.1097/MD.0000000000038438
28.
Miccinilli S Bravi M Morrone M Santacaterina F Stellato L Bressi F et al . A triple application of Kinesio taping supports rehabilitation program for rotator cuff tendinopathy: a randomized controlled trial. Ortop Traumatol Rehabil. (2018) 20:499–505. doi: 10.5604/01.3001.0012.9707
29.
De Oliveira FCL Pairot De Fontenay B Bouyer LJ Desmeules F Roy J-S . Kinesiotaping for the rehabilitation of rotator cuff–related shoulder pain: a randomized clinical trial. Sports Health. (2021) 13:161–72. doi: 10.1177/1941738120944254
30.
Çi̇Ftçi̇ R Köse E Canbolat M Yilmaz N Çuğlan S Yoloğlu S et al . Assessment of the effects of kinesio-taping in addition to conventional physiotherapy methods on upper extremity functions, quality of life and emotional state in patients with chronic rotator cuff syndrome. Med Records. (2020) 2:14–9. doi: 10.37990/medr.749448
31.
Reynard F Vuistiner P Léger B Konzelmann M . Immediate and short-term effects of kinesiotaping on muscular activity, mobility, strength and pain after rotator cuff surgery: a crossover clinical trial. BMC Musculoskelet Disord. (2018) 19:305. doi: 10.1186/s12891-018-2169-5
32.
Taik FZ Karkouri S Tahiri L Aachari I Moulay Berkchi J Hmamouchi I et al . Effects of kinesiotaping on disability and pain in patients with rotator cuff tendinopathy: double-blind randomized clinical trial. BMC Musculoskelet Disord. (2022) 23:90. doi: 10.1186/s12891-022-05046-w
33.
Bac A Wróbel M Ogrodzka-Ciechanowicz K Michalik E Ścisłowska-Czarnecka A . The influence of the Kinesio taping on selected ultrasonography measurements, and quality of life in patients with rotator cuff lesions. Sci Rep. (2020) 10:18539. doi: 10.1038/s41598-020-75701-6
34.
Nguyen TNA Nguyen NH Vu DK Cu LTN . Short-term effects of Kinesiotaping combined with a rehabilitation program for rotator cuff-related shoulder pain: a randomized, assessor-blinded clinical trial. J Manual Manipulat Therapy. (2025) 33:112–21. doi: 10.1080/10669817.2024.2387913
35.
Martins Da Silva L Maciel Bello G Chuaste Flores B Silva Dias L Camargo P Fernando Mengue L et al . Kinesio tape in shoulder rotator cuff tendinopathy: a randomized, blind clinical trial. Muscle Ligaments Tendons J. (2020) 10:364. doi: 10.32098/mltj.03.2020.03
36.
Durgut E Gurses HN Bilsel K Alpay K Hosbay Z Uzer G et al . Short-term effects of cold therapy and Kinesio taping on pain relief and upper extremity functionality in individuals with rotator cuff tendonitis: a randomized study. Medicina. (2024) 60:1188. doi: 10.3390/medicina60081188
37.
Thelen MD Dauber JA Stoneman PD . The clinical efficacy of Kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. J Orthop Sports Phys Ther. (2008) 38:389–95. doi: 10.2519/jospt.2008.2791
38.
Analay Akbaba Y Kaya Mutlu E Altun S Celik D . Does the patients’ expectations on kinesiotape affect the outcomes of patients with a rotator cuff tear? A randomized controlled clinical trial. Clin Rehabil. (2018) 32:1509–1519. doi: 10.1177/0269215518779645
39.
Chen S Xue Z Chen J . Clinical observation on the treatment of rotator cuff injuries with ultrasound combined with muscle spasticity inhibiting plasters. Medical Diet Therapy and Health. (2020) 9:2.
40.
Bao J Feng Y Guo Y . Clinical efficacy study of kinesiology taping combined with Maitland joint mobilization techniques in patients after rotator cuff tear surgery.Ningxia. Medical Journal. (2023) 45:1101. doi: 10.1362/j.1001-5949.2023.12.1101
41.
Yuan H Li J Li Y . The effect of kinesiology tape combined with intradermal therapy on shoulder joint pain and range of motion after rotator cuff injury at night. Chinese Trad Med Emerg Treatment. (2024) 33:1248–50. doi: 10.3969/j.issn.1004-745X.2024.07.030
42.
Wang W Zhang J . Observation on the effect of kinesiology tape in the rehabilitation treatment of rotator cuff injuries. J PLA Medical Univ. (2019) 8:776–80. doi: 10.3969/j.issn.2095-5227.2019.08.017
43.
Jia P Zhang J Lu B Cheng H . Observation on the therapeutic effect of shoulder muscle group training combined with kinesio taping in the treatment of rotator cuff injuries. Chin Rehabil. (2022) 37:289–92. doi: 10.3870/zgkf.2022.05.008
44.
Li W . The clinical efficacy of extracorporeal shock wave therapy combined with intramuscular kinesio taping in the treatment of patients with rotator cuff injury. Med Equip. (2022) 35:49–52.
45.
Todd KH Funk KG Funk JP Bonacci R . Clinical significance of reported changes in pain severity. Ann Emerg Med. (1996) 27:485–9. doi: 10.1016/S0196-0644(96)70238-X
46.
Todd KH Funk JP . The minimum clinically important difference in physician–assigned visual analog pain scores. Acad Emerg Med. (1996) 3:142–6. doi: 10.1111/j.1553-2712.1996.tb03402.x
47.
Kim DM Kim TH Kholinne E Park JH Shin MJ Kim H et al . Minimal clinically important difference, substantial clinical benefit, and patient acceptable symptomatic state after arthroscopic rotator cuff repair. Am J Sports Med. (2020) 48:2650–9. doi: 10.1177/0363546520943862
48.
Louwerens JKG Van Den Bekerom MPJ Van Royen BJ Eygendaal D Van Noort A Sierevelt IN . Quantifying the minimal and substantial clinical benefit of the constant-Murley score and the disabilities of the arm, shoulder and hand score in patients with calcific tendinitis of the rotator cuff. JSES Int. (2020) 4:606–11. doi: 10.1016/j.jseint.2020.05.001
49.
Smith-Forbes EV Howell DM Willoughby J Pitts DG Uhl TL . Specificity of the minimal clinically important difference of the quick disabilities of the arm shoulder and hand (QDASH) for distal upper extremity conditions. J Hand Ther. (2016) 29:81–8. doi: 10.1016/j.jht.2015.09.003
50.
Goulart LT Matsunaga FT Belloti JC Netto NA Paim TS Tamaoki MJS . Effectiveness of sub-acromial injections in rotator cuff injuries: a systematic review and meta-analysis. World J Orthop. (2025) 16:102856. doi: 10.5312/wjo.v16.i2.102856
51.
Dan F . Arthroscopic treatment for rotator cuff injury and frozen shoulder with concomitant rotator cuff injury: analysis of efficacy and factors influencing prognosis. Am J Transl Res. (2024) 16:864–72. doi: 10.62347/QLMC4456
52.
Bocchino G Grassa D Bove A Salvini M Kaplan R Di Gialleonardo E et al . The effects of Kinesio tape on acute ankle sprain: a systematic review. JCM. (2025) 14:1440. doi: 10.3390/jcm14051440
53.
Dehghan F Fouladi R Martin J . Kinesio taping in sports: a scoping review. J Bodyw Mov Ther. (2024) 40:1213–23. doi: 10.1016/j.jbmt.2023.05.008
54.
Skwiot M . Effectiveness of Kinesio taping for lymphedema in the post-mastectomy patient: a systematic review of randomized controlled trials. JCM. (2025) 14:1700. doi: 10.3390/jcm14051700
55.
Seo Y Lee Y Son S Lee J Park J Lee D et al . Does Kinesio taping enhance exercise performance and recovery in healthy males under heat stress?JCM. (2025) 14:2631. doi: 10.3390/jcm14082631
56.
Bagheri R Pourahmadi MR Sarmadi AR Takamjani IE Torkaman G Fazeli SH . What is the effect and mechanism of kinesiology tape on muscle activity?J Bodyw Mov Ther. (2018) 22:266–75. doi: 10.1016/j.jbmt.2017.06.018
57.
Song S Lee S-K Ahn S-H . The effect of kinesio taping on joint range of motion and balance in total knee replacement patients. J Exerc Rehabil. (2024) 20:131–6. doi: 10.12965/jer.2442254.127
58.
Mei T Shuai Y Wu D Yu H . Effects of kinesio taping in patients undergoing knee or hip arthroplasty: a systematic review and meta-analysis of randomized controlled trials. JRM. (2025) 57:jrm40784. doi: 10.2340/jrm.v57.40784
59.
Skedros JG Adondakis MG Knight AN Pilkington MB . Frequency of shoulder corticosteroid injections for pain and stiffness after shoulder surgery and their potential to enhance outcomes with physiotherapy: a retrospective study. Pain Ther. (2017) 6:45–60. doi: 10.1007/s40122-017-0065-6
Summary
Keywords
rotator cuff injuries, kinesiology tape, systematic review, meta-analysis, pain
Citation
Luo Y, Zhang L, Tang Z, Chen L, Zhou D and Huang H (2025) The efficacy of kinesiology tape for rotator cuff injuries: a meta-analysis of randomized trials. Front. Med. 12:1695350. doi: 10.3389/fmed.2025.1695350
Received
29 August 2025
Accepted
13 October 2025
Published
10 November 2025
Volume
12 - 2025
Edited by
Yoshihiro Noguchi, Gifu Pharmaceutical University, Japan
Reviewed by
Elif Durgut, Bezmialem Vakıf University, Türkiye
Thomas Erwin Christian Junus Huwae, Universitas Brawijaya, Indonesia
Updates
Copyright
© 2025 Luo, Zhang, Tang, Chen, Zhou and Huang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liyue Zhang, 357805715@qq.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.