- Division of Population Health and Applied Health Sciences, Faculty of Medicine, Memorial University of Newfoundland, St. John’s, NL, Canada
Public debate in Canada often diagnoses a simple “shortage of family physicians,” yet system indicators point to a more complex access problem. In 2023, 17% of adults reported no regular primary care provider, only 26% obtained same/next-day appointments, and about 15% of emergency department visits were potentially primary-care-manageable—over half potentially manageable virtually. Meanwhile, average weekly physician work hours have declined by 6.9 h since the late 1980’s and the average number of patients seen per family physician fell from 1,746 (2013) to 1,353 (2021), alongside a shift away from comprehensive community practice. Drawing on comparative evidence that stronger primary care architecture is associated with better performance and that primary health care averages ∼13% of current health spending across OECD countries, this Perspective reframes Canada’s challenge across four dimensions: effective capacity (not just headcount); demand—complexity, time, and continuity; maldistribution and loss of comprehensive care; and system entry-point design. We then organize solutions in three groups: system-level (investment floors, enrollment/rostering and after-hours obligations, payment aligned to continuity and team-based comprehensiveness), organizational-level (interdisciplinary teams, task-sharing with NPs/pharmacists/PAs, operationalized continuity), and data & research (effective-FTE and continuity metrics, complexity-adjusted panel targets, rigorous evaluation of entry-point and scope reforms). Recasting the problem from headcount to capacity-and-design clarifies actionable levers for timely attachment and sustained relational continuity.
1 Introduction
Public debate in Canada often reduces primary care access problems to a simple “shortage of family physicians (FPs).” Yet system monitoring shows persistent access gaps: in 2023, 17% of adults reported no regular primary care provider; only 26% reported same- or next-day appointments; and 15% of emergency department visits (April 2023–March 2024) were for conditions potentially manageable in primary care, over half of which could potentially have been managed virtually (1). These indicators suggest a complex access problem that is experienced by the public as “shortage.”
At the same time, supply-side signals complicate a headcount narrative. Average weekly physician work hours have declined by 6.9 h since the late 1980’s (2), and the average number of patients seen per FP per year fell from 1,746 in 2013 to 1,353 in 2021 (3). In parallel, a growing share of physicians practice outside traditional community-based primary care (4). Together, these patterns indicate that the public’s experience of “shortage” reflects multiple interacting dynamics rather than a single deficit in headcount.
Comparative evidence underscores different dimensions access to primary care. Across OECD countries, primary health care averages about 13% of current health spending, and stronger primary care architecture is linked to better access and system performance (5). Canada’s access metrics point to a need to reconsider how we define and target the problem the public experiences as “shortage.”
This Perspective paper builds on prior isolated analyses of family physician shortage by integrating supply/demand, and structure/process frameworks to identify and discuss four complementary dimensions that can guide the analysis without presupposing a single cause (Figure 1).
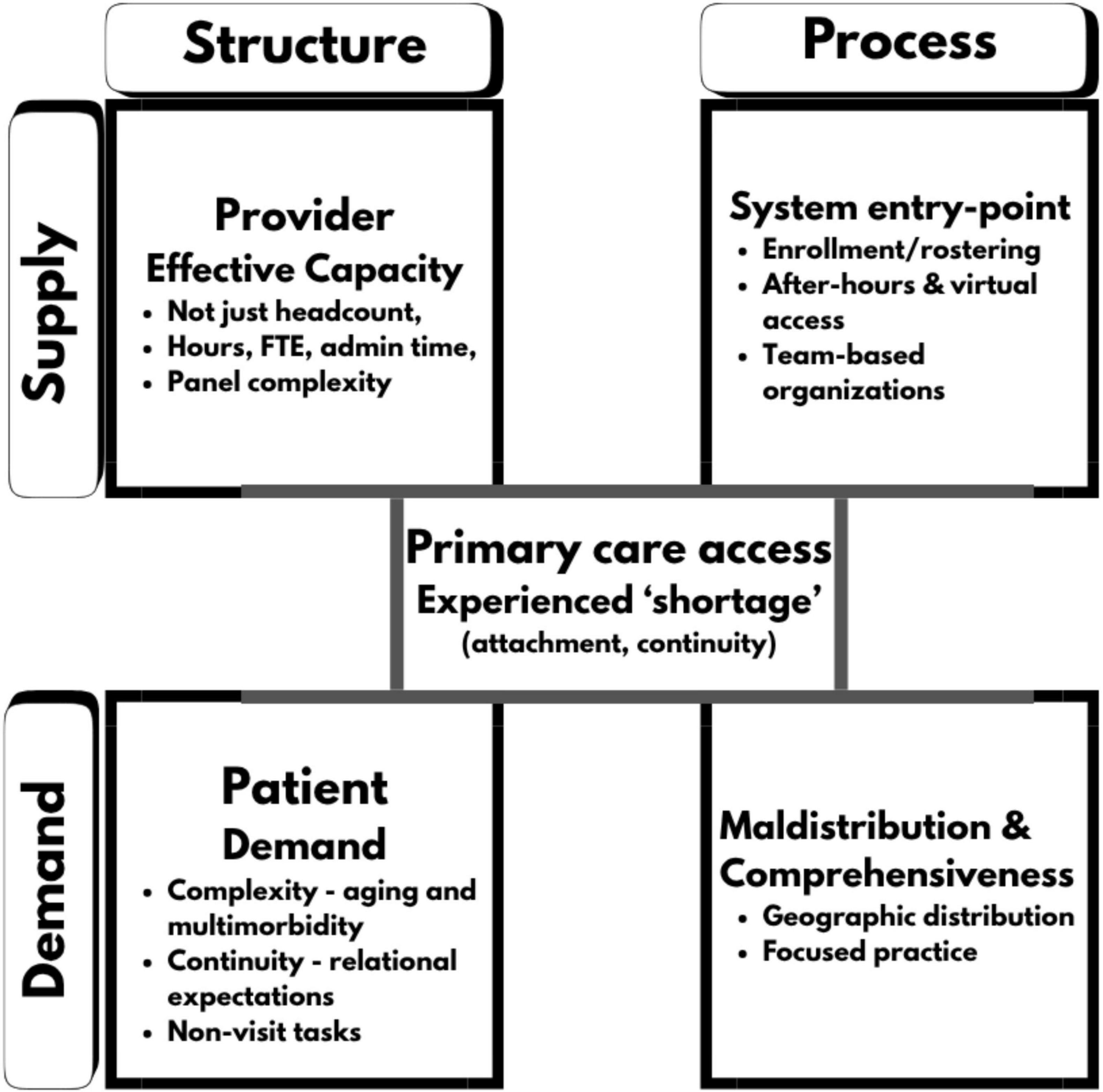
Figure 1. Four dimensions of primary care access in Canada on supply/demand and structure/process domains.
These dimensions are intended to structure policy discussion and guide measurement for solutions that the public will recognize as improved access.
2 Dimensions
2.1 Effective capacity, not just headcount
Counting physicians is a weak proxy for the volume and continuity of care delivered. Over the last three decades, average weekly physician work hours in Canada declined by about 6.9 h—from 52.8 (1987–1991) to 45.9 (2017–2021)—with the decline concentrated among male physicians (2). Parallel analyses emphasize that planning should consider full-time equivalent (FTE) supply rather than absolute counts, because aging populations and changing hours both alter the true service capacity available (6).
Beyond hours, practice intensity has shifted. A cross-provincial study showed that while FP counts grew (e.g., Ontario + 35.3%; Alberta + 48.7% between 2005/06 and 2017/18), annual service days per FP declined (−10.6% Ontario; −5.9% Alberta) (7). Nationally, CIHI reports that the average number of patients seen per FP per year fell from 1,746 to 1,353 between 2013 and 2021 (3). Together these data indicate that time per patient, administrative load, and coordination demands are squeezing the number of encounters an FP can provide—reducing effective capacity even if headcount rises.
Crucially, “optimal” panel size is not a single magic number; it depends on continuity, team supports, patient complexity, and organizational model. Evidence from Ontario suggests nuanced relationships between panel size and quality, underscoring that policies to expand attachment must guard continuity and comprehensiveness rather than chase a uniform target (8).
2.2 Demand, complexity, time, and continuity
In primary care, what patients feel as “shortage” often reflects a dynamic gap: ΔDemand exceeds ΔEffective supply. Demand has grown along four fronts—demography, multimorbidity/complexity, relational demand for continuity, and non-visit tasks—while effective supply (clinician time that converts into longitudinal care) has not proportionally expanded.
Demography change and multimorbidity expand clinical time needs. Canada is aging: by 1 July 2023, 18.9% of the population was 65+, and the share will continue to rise (with very old age growing fastest) (9). Aging brings multimorbidity and polypharmacy that lengthen visits and coordination needs. A systematic review finds patients with multimorbidity require longer consultation times than those without, directly compressing the number of encounters a clinician can provide per day (10). CIHI’s newest international survey of older adults further shows lower timely access in Canada versus peers, consistent with demand outpacing available appointment capacity (11).
Continuity of care can also be viewed as relational demand, not just a quality metric. Patients do not only seek a slot; they seek ongoing relationships with a clinician/team that knows them. Evidence shows patients value continuity (e.g., seeing the same primary care doctor) for trust, not repeating histories, and comfort—and systems that deliver continuity achieve better reported experiences (12). Continuity is also outcome-relevant: a landmark systematic review across multiple settings associates higher continuity with lower mortality (13). When large numbers of people lack a regular provider—86% of adults had one in 2023 (down from 93% in 2016), leaving roughly 4 million without—unmet relational demand accumulates and is perceived as shortage, particularly among higher-need groups (1). Among older adults (65+), 8% still report no regular source of care—highest among 10 countries surveyed—illustrating how the continuity gap is itself part of demand (11).
Finally, complexity extends beyond diagnoses: tasks and coordination consume time. Administrative and coordination tasks (forms, information chasing, prior approvals, e-mails, inbox management) absorb millions of clinician hours annually in Canada, contributing to burnout and reducing effective clinical supply (14). Critical reviews catalog these burdens (compliance, learning, psychological costs) and their crowd-out of direct care (15). In short, even if headcount holds, task inflation increases demand on clinician time, narrowing appointment availability.
2.3 Maldistribution and loss of comprehensiveness
Another driver of “shortage” is where and how FPs practice. CIHI documents a marked shift of FPs toward focused roles outside traditional community-based comprehensive care. Nearly 30% of Canada’s FPs now practice predominantly outside primary care (e.g., emergency medicine or psychiatry), up from about 26% in 2019 to 28.3% in 2022 (3). This shift reduces the pool of clinicians available for longitudinal attachment and first-contact care, even if total FP numbers appear stable.
Population-level analyses from Ontario sharpen this picture. From 1993/94 to 2021/22, the proportion of FPs in focused practice rose from 7.7% to 19.2%, while the number of comprehensive FPs per 100,000 residents fell (16). More recently, growth in the comprehensive FP workforce stagnated post-2019 (9,377 in 2019 vs. 9,375 in 2022), with an increasing share near retirement; patients attached to near-retirement FPs are older and have higher chronic disease burdens, raising transition risks (17, 18).
Maldistribution also includes urban–rural and intra-urban patterns: growth in FP counts has tended to be greater in urban areas, while service days per FP have dropped across geographies, amplifying access gaps in smaller communities (7). Combined with fewer comprehensive FPs and rising patient complexity, these spatial and scope shifts feel like a “shortage” at the point of care—even where nominal FP supply has grown.
2.4 System entry point
In systems where primary care is the front door, how patients are attached, how they enter, and how teams are organized strongly shape experienced “shortage.” Canada continues to post the lowest same/next-day access and among the lowest after-hours access of 10 peer countries—signals of entry-point design as much as raw headcount (1). Countries with near-universal attachment typically combine enrolment/rostering with a clear general-practice “home,” robust after-hours arrangements, and interdisciplinary teams (5, 19).
Canada has piloted many of these organizational levers—but with uneven results. Ontario’s patient-enrolment models (e.g., blended capitation with formal rostering and after-hours obligations) and funded interprofessional teams transformed local primary care, yet early evaluations found mixed gains on access and attachment despite strong intent, underscoring that design details and implementation fidelity matter (20, 21). Meanwhile, at least six provinces have used centralized waiting lists to broker attachment for “orphan” patients; evaluations in Québec show CWLs can attach patients but performance varies by local design and resourcing (22–24).
Peer systems illustrate how entry-point architecture supports continuity and equity. Denmark’s list-based GP registration and gatekeeping model delivers high continuity and coordinated access across sectors—features repeatedly linked to better outcomes (25, 26). The lesson for Canada is not to copy-paste, but to commit to enrolment-first models with dependable after-hours access and team capacity, and to use CWLs as a bridge—not a substitute—for stable longitudinal attachment.
3 Policy solution discussion
Building on the four diagnostic dimensions, solutions can be placed in the following three categories: the system level, the organizational level, and data and research.
System-level change: At the system level, the first lever is to set—and protect—an explicit investment floor for primary care and tie new dollars to measurable improvements in attachment, same/next-day access, after-hours access,. and continuity OECD benchmarking shows primary health care averages roughly 13% of current health spending across member countries, and peer systems with stronger primary-care architecture achieve better attachment and timely access (5, 19). A second lever is to make enrolment/rostering the default point of entry so that demand flows through a longitudinal home rather than episodic settings; countries such as Denmark combine list-based registration, gatekeeping, and after-hours arrangements to channel urgent needs without fragmenting care (19, 27). Centralized Waiting Lists (CWLs) should be used as a bridge—not a substitute—for attachment, with design features (triage by complexity, real-time capacity, feedback loops) that evaluations have linked to better performance (23). Payment policy should align with this managed entry point: evidence from Ontario links funding models to variation in ambulatory-care-sensitive hospitalizations, and recent commentary argues that blended contracts should explicitly measure and reward continuity, after-hours access, and team-delivered comprehensiveness (28, 29). Finally, shrinking administrative drag is a system responsibility: standardized forms, delegated documentation, and EMR usability targets can reclaim clinician time and reduce burnout, converting funding into effective capacity (14).
Organizational-level change: Within organizations, interdisciplinary teams should be funded and staffed with clear roles, shared goals, and local implementation supports (leadership, co-location, panel management, and huddles). Systematic reviews and Canadian scoping reviews indicate that well-implemented teams improve access and comprehensiveness, although effects depend on design fidelity (30, 31). Task-sharing and clinical substitution are central: high-quality evidence shows that nurses (including nurse practitioners) can deliver care comparable to physicians for many conditions with equal or higher patient satisfaction (32). Pharmacist prescribing for minor ailments—now expanded in Ontario and being monitored at scale in British Columbia—has been found safe and effective and can offload low-acuity demand (33–35). Physician assistants also contribute meaningfully to first-contact capacity where funding rules and supervision are clear; Canadian data show high supervising-physician satisfaction but highlight the need for stable organizational funding (36). Crucially, continuity must be operationalized inside teams—e.g., a “named clinician” within a “named team,” explicit continuity metrics, and protected follow-up—because relational continuity is consistently associated with better outcomes, including lower mortality (13, 37).
Data and research: A data strategy should mirror the problem’s reframing and make indicator construction transparent. First, a pan-Canadian effective capacity dashboard should report not only headcount but effective FTE by geography and model (clinical hours, scope, panel complexity, and administrative time), while stating how each indicator is built. For example, CIHI’s “patients seen per family physician” is derived from National Physician Database billing/claims by fiscal year; it is not roster/panel size and can be influenced by alternative payment plans and shadow billing, with recent series excluding some jurisdictions (e.g., Québec, PEI, New Brunswick, territories), which limits comparability (3, 4). Estimates of physician hours commonly rely on Statistics Canada’s Labour Force Survey and reflect self-reported “usual weekly hours” across professional activities (clinical plus administrative), rather than direct patient-contact time (2). Second, analyses should attend to provincial heterogeneity: primary care reforms and workforce trends vary by jurisdiction; cross-provincial comparisons should present stratified estimates and document operational definitions (e.g., “service day” thresholds in claims-based studies) to support valid aggregation (7). Third, attachment and continuity should be core performance indicators, with routine public reporting of usual-provider continuity (UPC) and team continuity indices, given the consistent association between continuity and outcomes, including lower mortality (13, 37). Fourth, demand should be defined and weighted by tracking age structure, multimorbidity, and social complexity to create complexity-adjusted panel targets, reflecting evidence that multimorbidity lengthens consultations and compresses throughput (10). Fifth, entry-point reforms and scope expansions (enrolment/rostering with after-hours obligations; payment alignment; expanded roles for NPs, pharmacists, and PAs) should be evaluated with rigorous designs—stepped-wedge rollouts, difference-in-differences, and interrupted time series—with pre-specified outcomes (attachment, continuity, primary-care-sensitive ED use, ACSC hospitalizations, equity), noting current gaps where evidence remains heterogeneous or observational (28, 35). Finally, administrative burden should be measured and reduced via explicit provincial targets (form elimination, inbox delegation, EMR usability), with linkage to reclaimed clinical time, patients seen, and attachment gains (1, 14).
Implementing the proposed agenda will face predictable barriers. Governance and financing are fragmented across provinces and territories, creating variable readiness for enrolment and rostering, after-hours obligations, and payment alignment. Payment reform is path-dependent and may encounter stakeholder resistance such as concerns about risk selection, administrative load, or perceived loss of autonomy, unless continuity and equity safeguards are explicit. Scaling team-based care requires stable funding, role clarity, and workforce pipelines for NPs, pharmacists, and PAs, alongside regulatory alignment on scope of practice. Data infrastructure remains uneven: alternative payments and shadow billing complicate measurement; common definitions, privacy-respecting data linkages, and real-time evaluation capacity are prerequisites. Finally, rural and underserved settings will need tailored supports such as funding, recruitment incentives, virtual care and after-hours networks to avoid widening inequities during transition.
4 Conclusion
Canada’s primary care crisis is best understood not as a simple headcount gap but as the interaction of effective capacity, demand (complexity, time, continuity), maldistribution and loss of comprehensive care, and system entry-point design—the forces that produce what patients experience as “shortage.” Accordingly, solutions must align at three levels: system (adequate investment, managed enrolment, and incentives that reward continuity and team-delivered comprehensiveness), organizational (well-implemented interprofessional teams and task-sharing), and data/research (measuring effective FTE, attachment, continuity, and evaluating reforms rigorously). If governments, organizations, and researchers act on these levers together, Canadians should see tangible gains in timely attachment and relational continuity.
Data availability statement
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MN: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Canadian Institute for Health Information (CIHI). Access to Primary Care: Many Canadians Face Challenges. (2024). Available online at: https://www.cihi.ca/en/primary-and-virtual-care-access-emergency-department-visits-for-primary-care-conditions/access-to-primary-care-many-canadians-face-challenges
2. Kralj B, Kantarevic J. Long-term trends in the work hours of physicians in Canada. CMAJ. (2024) 196:E369-77. Available online at: https://www.cmaj.ca/content/196/11/E369 (accessed October 28, 2025).
3. Canadian Institute for Health Information (CIHI). Health Workforce: Practice Patterns (State of the Health Workforce in Canada). (2024). Available online at: https://www.cihi.ca/en/the-state-of-the-health-workforce-in-canada-2023/health-workforce-practice-patterns (accessed October 28, 2025).
4. Canadian Institute for Health Information (CIHI). Primary and Virtual Care Access: Emergency Department Visits for Primary Care Conditions; Emergency Department Crowding: Beyond Primary Care Access. (2024). Available online at: https://www.cihi.ca/en/primary-and-virtual-care-access-emergency-department-visits-for-primary-care-conditions (accessed October 28, 2025).
5. Organisation for Economic Co-operation and Development (OECD). Health at a Glance 2023: OECD Indicators. Paris: OECD Publishing (2023). Available online at: https://www.oecd.org/en/publications/2023/11/health-at-a-glance-2023_e04f8239/full-report/health-expenditure-on-primary-healthcare_bf72cd24.html (accessed October 28, 2025).
6. Islam R, Kralj B, Sweetman A. Physician workforce planning in Canada: the importance of accounting for population aging and changing physician hours of work. CMAJ. (2023) 195:E335-40. doi: 10.1503/cmaj.221239
7. McDonald T, Baillie C, Taylor C, Wong ST, McGrail K. Family physician count and service provision in Ontario and Alberta between 2005/06 and 2017/18: a cross-sectional study. CMAJ Open. (2023) 11:E1102-12. doi: 10.9778/cmajo.20220201
8. Dahrouge S, Hogg W, Younger J, Muggah E, Russell G, Glazier RH. Primary care physician panel size and quality of care: a population-based study in Ontario, Canada. Ann Fam Med. (2016) 14:26-33. doi: 10.1370/afm.1864
9. Tadeu ACR, Falcão IV, Medeiros AMC. Multimorbidity and consultation time: a systematic review. Fam Med Prim Care Rev. (2020) 22:246-52. Available online at: https://pubmed.ncbi.nlm.nih.gov/32723303/ (accessed October 28, 2025).
10. Statistics Canada. The Older People Are All Right. (2024). Available online at: https://www.statcan.gc.ca/o1/en/plus/7059-older-people-are-all-right (accessed October 28, 2025).
11. Canadian Institute for Health Information (CIHI). Older Adults in Canada Report Growing Challenges in Accessing Primary Care in International Survey. (2025). Available online at: https://www.cihi.ca/en/news/older-adults-in-canada-report-growing-challenges-in-accessing-primary-care-in-international-survey?utm_source=chatgpt.com (accessed October 28, 2025).
12. Pratiwi AB, Ramdani M, Fahyuni EF. Patients’ values regarding primary health care: a systematic review. BMC Health Serv Res. (2023) 23:1540. doi: 10.1186/s12913-023-09394-8
13. Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors and mortality: a systematic review. BMJ Open. (2018) 8(6):e021161. doi: 10.1136/bmjopen-2017-021161
14. Canadian Medical Association (CMA). Administrative Burden is Driving Physician Burnout, and Puts Access to Care at Risk. (2025). Available online at: https://www.cma.ca/our-focus/administrative-burden/facts (accessed October 28, 2025).
15. Storseth O, Goncalves-Bradley D, McDonald R, Straus S. Administrative burden in primary care: a critical review. Healthc Policy. (2025) 20:1-12. Available online at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12264525/ (accessed October 28, 2025).
16. Ansari H, Green ME, Schultz SE, Frymire E, Kiran T. Family physicians in focused practice in Ontario, Canada: a population-level study of trends from 1993/1994 through 2021/2022. Ann Fam Med. (2025) 23:181-8. doi: 10.1370/afm.240377
17. Premji K, Schultz SE, Cadarette SM, Kiran T. Trends colliding: aging comprehensive family physicians and the growing complexity of their patients. Can Fam Physician. (2025) 71:406-10. Available online at: https://www.cfp.ca/content/71/6/406 (accessed October 28, 2025).
18. ICES. Trends Colliding: Aging Comprehensive Family Physicians and the Growing Complexity of their Patients. (2025). Available online at: https://www.ices.on.ca/publications/journal-articles/trends-colliding-aging-comprehensive-family-physicians-and-the-growing-complexity-of-their-patients/ (accessed October 28, 2025).
19. Shahaed H, Glazier RH, Anderson M, Barbazza E, Bos VLLC, Saunes IS, et al. Primary care for all: lessons for Canada from peer countries with high primary care attachment. CMAJ. (2023) 195:E1628-36. doi: 10.1503/cmaj.221824
20. Hutchison B, Levesque J-F, Strumpf E, Coyle N. Ontario’s primary care reforms have transformed the local care landscape, but a plan is needed for ongoing improvement. Health Aff (Millwood). (2013) 32:695-703. doi: 10.1377/hlthaff.2012.1087
21. Glazier RH, Kopp A, Schultz SE, Kiran T, Henry DA. All the right intentions but few of the desired results: lessons on access to primary care from Ontario’s patient enrolment models. Healthc Q. (2012) 15:17-21. doi: 10.12927/hcq.2013.23041
22. Breton M, Brousselle A, Boivin A, Loiselle M, Luc M, Touati N. Evaluation of the implementation of centralized waiting lists for patients without a family physician and their effects across Québec. Healthc Policy. (2014) 10:108-21. doi: 10.1186/s13012-014-0117-9
23. Breton M, Gagnon D, Touati N, Couture M, Lamothe L, Lévesque J-F. Assessing the performance of centralized waiting lists for unattached patients in primary healthcare. BMC Health Serv Res. (2017) 17:133. doi: 10.1186/s12913-017-2007-8
24. Breton M, Smithman MA, Brousselle A, Lévesque J-F. Attaching patients in primary care through centralized waiting lists: seven Canadian provinces in comparative perspective. Health Reform Observer. (2019) 9:35-48. doi: 10.13162/hro-ors.v7i1.3773
25. Prior A, Vestergaard CH, Ribe AR, Sandbæk A, Bro F, Vedsted P, et al. Chronic care services and variation between Danish general practices: a nationwide cohort study. Br J Gen Pract. (2022) 72:e285-92. doi: 10.3399/BJGP.2021.0419
26. Rimestad DE, Ahnfeldt-Mollerup P, Kristensen T. Patient characteristics and degrees of discontinuity of care in Danish general practice: a cohort study. Br J Gen Pract. (2025) 75:e509-17. doi: 10.3399/BJGP.2024.0570
27. Laschke ADL, Blaakær J, Jensen CF, Larsen MB. Danish general practitioners as gatekeepers for gynaecological patients in regions with different density of resident specialists in gynaecology: in which situations and to whom do they refer? A cross-sectional study. Scand J Prim Health Care. (2023) 41:52-60. doi: 10.1080/02813432.2023.2165085
28. Somé NH, et al. Primary care payment models and avoidable hospitalizations in Ontario, Canada: a multivalued treatment-effects analysis. Health Econ. (2024) 33:2288-305. doi: 10.1002/hec.4872
29. Wranik WD, Price S, Haydt SM, Edwards J, Hatfield K, Weir J, et al. Implications of interprofessional primary care team characteristics for health services and patient health outcomes: a systematic review with narrative synthesis. Health Policy. (2019) 123:550-63. doi: 10.1016/j.healthpol.2019.03.015
30. McCracken RK, Lavergne MR, Hedden L. Will blended family physician payment models revive primary care in Canada? Can Fam Physician. (2025) 71:377-9. doi: 10.46747/cfp.7106377
31. Frikha Y, Gagnon M-P, Breton M. Transformation of primary care settings implementing a co-located team-based care model: a scoping review. BMC Health Serv Res. (2024) 24:890. doi: 10.1186/s12913-024-11291-7
32. Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. (2018) 7:CD001271. doi: 10.1002/14651858.CD001271.pub3
33. Ontario College of Pharmacists. Minor Ailments—Expanded Scope of Practice. (2023). Available online at: https://www.ocpinfo.com/practice-education/expanded-scope-of-practice/minor-ailment/ (accessed October 28, 2025).
34. Government of British Columbia. Pharmacists Prescribing for Minor Ailments and Contraception—Monitoring & Evaluation. (2025). Available online at: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/initiatives/sop/monitoring-evaluation-ppmac (accessed October 28, 2025).
35. Nakhla N, Leung V, Schwartz KL. Expansion of pharmacist prescribing could help improve health care access and quality. Can Fam Physician. (2024) 70:441-3. doi: 10.46747/cfp.700708441
36. Burrows K, Nickell L, Krueger P. Physician assistants working in primary care in Canada: findings from a national survey. Healthc Manage Forum. (2025) 38:456-63. doi: 10.1177/08404704251347908
Keywords: primary care (PC), access, family physician (FP), family physician shortage, Canada
Citation: Najafizada M (2025) Beyond headcount: four dimensions of Canada’s primary care access crisis and a three-level agenda for action. Front. Med. 12:1695409. doi: 10.3389/fmed.2025.1695409
Received: 29 August 2025; Accepted: 28 October 2025;
Published: 20 November 2025.
Edited by:
Waseem Jerjes, Imperial College London, United KingdomReviewed by:
Ricardo De Moraes E. Soares, Naval School, PortugalCopyright © 2025 Najafizada. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maisam Najafizada, bW5hamFmaXphZGFAbXVuLmNh
 Maisam Najafizada
Maisam Najafizada