Abstract
Background:
Total hip arthroplasty (THA) is an effective treatment for end-stage hip disease, which can significantly relieve pain, rebuild joint function, and improve patients’ quality of life. Early post-operative functional exercises are essential to promote the recovery of hip function and minimize complications. However, some patients are afraid of exercise due to the risk of pain or dislocation of the prosthesis, resulting in poor adherence to rehabilitation exercises. Kinesiophobia has now become a key factor hindering the rehabilitation process and leading to poor functional recovery. Therefore, early identification of high-risk groups and implementation of targeted interventions are essential to improve patient prognosis.
Objectives:
To construct and validate a risk prediction model for post-operative kinesiophobia in total hip arthroplasty (THA) patients.
Methods:
This study is a single-center cross-sectional study with only internal validation. Through the convenience sampling method, 205 patients who underwent total hip arthroplasty (THA) at the Second Affiliated Hospital of Shandong First Medical University from October 2024 to May 2025 were selected as the study subjects. Independent predictors associated with the occurrence of kinesiophobia were screened by univariate analysis and multifactorial logistic regression analysis. A nomogram risk prediction model was constructed using R software, and the Hosmer-Lemeshow test, receiver operating characteristic (ROC) curve, area under the curve (AUC), calibration curves, and decision analysis curves (DCA) were used to evaluate the model’s goodness-of-fit, discriminability, calibration, and clinical utility, respectively. The Bootstrap method was used to perform 1,000 repeated samplings for internal validation of the model.
Results:
A total of 126 out of 205 post-operative THA patients developed kinesiophobia, and the incidence of kinesiophobia was 61.5%. Logistic regression showed that pain history duration, anxiety, hip function, coping style, and rehabilitation self-efficacy were the influencing factors for the development of kinesiophobia in post-operative patients with THA (P < 0.05). The AUC value of the constructed model was 0.947 (95% CI 0.919∼0.975), the specificity was 0.873, and the sensitivity was 0.911. The Hosmer-Lemeshow test (χ2 = 2.287, P = 0.971) and the calibration curve showed that the predicted probability of the model was consistent with the probability of the actual occurrence, and the model predicted the effect well; the DCA curve indicates that the model has good clinical utility. Internal validation using the Bootstrap method yielded an AUC value of 0.912 (95% CI 0.875–0.949).
Conclusion:
THA patients with a pain history duration (> 1 year), anxiety, poor hip function, low active coping, and poor rehabilitation self-efficacy are more likely to develop kinesiophobia after surgery. The constructed model has good predictive efficacy, which is helpful for early clinical identification of high-risk patients and provides a reference for developing individualized interventions.
1 Introduction
Total hip arthroplasty (THA) is the replacement of diseased or dysfunctional hip joints with artificial prosthesis, which can effectively alleviate pain, rebuild joint function, and improve the quality of life of patients, and it is currently the most effective treatment for end-stage hip joint diseases (1, 2). With the aging of the population and the advancement of medical technology, the number of THA surgeries continues to climb, and according to statistics, about 2 million patients worldwide undergo hip replacement surgery every year (3). The key to the success of surgery lies not only in the precise implantation of the prosthesis, but also in whether the patient can maximize the recovery of joint function after surgery. Studies have shown that (4) the degree of recovery of hip joint function after surgery is closely related to the rehabilitation exercise of patients after surgery, and early functional exercise can promote the recovery of hip joint function, shorten the hospitalization time, and reduce the occurrence of post-operative complications. However, some patients developed kinesiophobia after surgery, resulting in poor compliance with rehabilitation exercises.
Kinesiophobia is a common psychological problem in post-operative patients with THA, which refers to excessive and irrational fear of physical movement or physical activity due to pain or fear of secondary injury (5). It has been found (6) that kinesiophobia is a key factor affecting the prognosis of THA patients. This fear is not simply pain avoidance, but rather a misperception developed by the patient that activity will inevitably lead to loosening of the prosthesis, dislocation, increased pain, or even catastrophic consequences (7). This misperception will cause patients to develop a “fear-avoidance” behavior: even if they have the ability to move, they will actively limit the range of activities, reduce the intensity of rehabilitation training, prolong the bedtime, and even refuse the necessary early functional exercises due to fear, which will ultimately slow down the process of rehabilitation and affect the effect of joint recovery (8). Therefore, early prediction of the risk of post-operative kinesiophobia in THA patients is crucial for improving patients’ compliance with rehabilitation exercises and improving prognosis.
In recent years, kinesiophobia has gradually gained attention in the field of clinical research. However, there are obvious limitations in current studies, most of which focus on the investigation of the current status of kinesiophobia in THA patients and the analysis of its influencing factors. Moreover, the lack of in-depth understanding of the occurrence of kinesiophobia in THA patients after surgery has led to limited clinical assessment capabilities and difficulties in carrying out effective interventions. Therefore, it is necessary to improve the ability to recognize high-risk groups. In existing studies, there is a relative paucity of content related to risk prediction models for post-operative kinesiophobia in THA patients, and there is a lack of effective and convenient tools to predict the risk of post-operative kinesiophobia in THA patients. The nomogram risk prediction model has significant advantages as a commonly used risk assessment tool in clinical practice. It is able to achieve individualized and visualized prediction of the risk of adverse events by assigning values to risk factors and transforming them into graphical form. The model has been successfully applied to individualized kinesiophobia occurrence risk prediction in patients with lung cancer (9), lumbar disk herniation (10), and after coronary intervention (11). Therefore, in this study, we analyzed the influencing factors of post-operative kinesiophobia in THA patients with whether or not kinesiophobia occurs in THA patients as the dependent variable, constructed a nomogram risk prediction model, which is conducive to the early identification of high-risk patients by healthcare professionals, and provided a reference for the development of targeted intervention strategies to break the vicious circle of “fear-braking-functional deterioration,” and improve the long-term prognosis of patients.
Previous studies have shown that the degree and duration of pain, anxiety, and depression status, level of social support, self-efficacy, coping styles, and hip function are all closely related to the occurrence of kinesiophobia after THA (12–16). Among these factors, pain affects patients’ psychological state and willingness to recover, and when the degree of pain experienced by patients is heavier and lasts longer, the motor fear generated within them tends to be more intense. This is due to the fact that pain causes patients to subconsciously associate exercise with pain, thus instinctively resisting exercise and further hindering the recovery process (17). Whereas anxiety and depression will enhance the stress response of the patient’s body and affect the coordination and flexibility of the muscles around the hip joint, when the patient performs rehabilitation exercises, more discomfort will be generated due to the limited muscle function. This discomfort will further aggravate the patients’ psychological burden, causing them to worry about the effect of the surgery and lack confidence in the recovery of their own body functions, which in turn reduces their acceptance of exercise (18). In addition, a strong social support network consisting of family members, friends, and healthcare professionals can effectively promote functional recovery, emotional stability, and the ability to live independently in the long term; conversely, a lack of support may impede the recovery process and lead to poor post-operative outcomes (19). At the same time, demographic information such as age, gender, education level, and healthcare payment method is similarly associated with the development of kinesiophobia (20). When identifying patients with possible kinesiophobia after THA, all of these types of factors should be considered in order to more fully and accurately assess the patient’s condition.
The biopsychosocial model (BPS) is a model proposed by Engel for describing the behavioral and psychological processes of individuals, emphasizing the interrelationships between mind, body, physiology, and psychology, which suggests that an individual’s physical and mental health is closely related to biological factors (e.g., personal background, current status of the disease), psychological factors (e.g., emotion, cognition), and social factors (social support, economic status, etc.) (21). Based on the theoretical framework of the bio-psycho-social model, this study selected research variables from four dimensions, namely, physiology and disease (pain level and duration, hip function), cognition and beliefs (rehabilitation self-efficacy, coping styles), emotion (anxiety, depression), and society and environment (social support, demographic and sociological factors), to explore the risk factors for the development of kinesiophobia in post-operative patients with THA and to construct a nomogram prediction model, through which high-risk patients can be identified early and intervened in a timely manner, so as to reduce the incidence of post-operative kinesiophobia in THA, help patients to recover joint function early and improve their quality of life.
2 Materials and methods
2.1 Study design and target population
This is a single-center cross-sectional study, which facilitated the selection of 205 patients who underwent THA treatment in the Second Affiliated Hospital of Shandong First Medical University from October 2024 to May 2025, and the patients were categorized into kinesiophobia and non-kinesiophobia groups according to whether or not they developed kinesiophobia after surgery. Inclusion criteria: first-time THA surgery; age ≥ 18 years old; clear consciousness, expression ability is OK; voluntary participation in this study, and signed the informed consent. Exclusion criteria: patients with psychiatric history or cognitive impairment; patients with other important organ injuries, whose conditions may change at any time; patients with other diseases that limit lower limb activities.
In this study, the sample size was calculated using the Events Per Variable (EPV) method (22), and 18 study variables were finally selected in this study after combining the literature review, clinical practice experience, and group discussion, with an EPV ≥ 5 set to ensure the stability of the results. Based on the prevalence of kinesiophobia after total hip arthroplasty (THA) in a previous study (23), which was 58.7%, and taking into account the 20% loss to follow-up rate, the sample size was calculated to be at least (18 × 5/0.587)/0.8 = 192 cases. 205 valid questionnaires were finally recovered in this study.
2.2 Data collection
In this study, two uniformly trained researchers worked together to collect data and initially screened eligible THA patients through the electronic medical record system based on pre-established inclusion and exclusion criteria. Before the formal data collection, the researchers will fully communicate with the patients and their families, informing them in detail about the purpose, content, and process of the study, and promising to strictly protect the privacy of the patients and never disclose any personal information, and signing the informed consent form after obtaining the understanding of the patients and their families. General information was extracted directly through the hospital information technology platform, and other information was collected using a paper version of the scale when the patients’ post-operative vital signs were stable and their mental status was good. Before filling in the scale, the researchers used a unified instruction to explain the requirements and precautions for filling in the scale. For patients with dyslexia or those who were unable to complete the scale independently for other reasons, the researchers would adopt an objective and neutral way of expression, explaining the content of the scale one by one and avoiding inducing questions, and assisting the patients in completing the scale in the form of questions and answers. After the completion of the questionnaire, the researchers collected the questionnaires on the spot, evaluated and reviewed the questionnaires, and excluded the questionnaires with obvious errors. All data were entered independently by two researchers and double-checked to ensure the accuracy of the final data.
2.3 Measures
2.3.1 General information questionnaire
Self-designed questionnaire through literature review and group discussion, where demographic information included gender, age, place of residence, marital status, monthly household income, literacy level, and healthcare payment method. Disease information included BMI, pain level (visual analog scale), years of pain, and presence of comorbid chronic diseases.
2.3.2 Tampa scale for kinesiophobia
The Tampa Scale for Kinesiophobia was developed by Miller et al. (24) and Chineseized by Hu (25), using a four-point Likert scale, with scores of 1–4 indicating “completely oppose, oppose, agree, and completely agree,” and a total of 17 entries, of which four entries (entries 4, 8, 12, and 16) were reverse scored. There were 17 entries, four of which (entries 4, 8, 12, 16) were reverse scored, with total scores ranging from 17 to 68, and >37 points were recognized as kinesiophobia. The Cronbach’s alpha coefficient of this scale was 0.894 in this study.
2.3.3 Simplified coping style questionnaire
The Simplified Coping Style Questionnaire was compiled by Xie (26), using a four-point Likert scale, with scores of 0–3 as “do not take, occasionally take, sometimes take, and often take,” respectively. A total of 20 entries were divided into two dimensions: positive coping (entries 1–12) and negative coping (entries 13–20), and the dimension with the higher score was the coping style that the patients preferred to adopt. The Cronbach’s alpha coefficients of the positive coping and negative coping dimensions of this scale were 0.880 and 0.858, respectively, in this study.
2.3.4 Social support rating scale
The Social Support Rating Scale was developed by Xiao (27), with a total of 10 entries, including three dimensions of subjective support (entries 1, 3, 4, and 5), objective support (entries 2, 6, and 7), and utilization of support (entries 8, 9, and 10), and a four-point Likert scale was used, i.e., 1 point was assigned to option (1), and four points were assigned to option (4), where 6 and 7 were assigned 0 points on a scale of 0–9, and 0 points were assigned to option 7, which was assigned “no source.” Four points, of which questions 6 and 7 were scored on a scale of 0–9, with A scored 0, I scored 9, and question 7 scored 0 for “no source.” A total score of <20 means low social support, a total score between 20 and 30 means some social support, and a score of 30 or more means satisfactory social support. The Cronbach’s alpha coefficient of this scale was 0.893 in this study.
2.3.5 Hospital anxiety and depression scale
The hospital anxiety and depression scale was compiled by Zigmond et al. (28) and consists of 14 entries, including two subscales of anxiety and depression, where the odd-numbered entries are for anxiety and the even-numbered entries are for depression, and a Likert four-point scale was used, with each entry scored from 0 to 3, and a dimensional score of >7 indicating that the patient suffers from anxiety or depression. The Cronbach’s coefficients of the anxiety and depression sub-scales were 0.869 and 0.870, respectively, in this study.
2.3.6 Self-Efficacy for rehabilitation outcome scale
The Self-Efficacy for Rehabilitation Outcome Scale was developed by Waldrop et al. (29) and Chineseized by Wang et al. (30), with a total of 12 entries and a Likert-11 scale, with scores ranging from 0 to 10, which indicate “cannot at all” to “do not have any difficulty,” respectively. A total of 12 entries were scored on a Likert-11 scale from 0 to 10, indicating “no difficulty at all” and “no difficulty at all,” respectively, with a total score of 120 points, and the higher the score, the more confident the patient is in rehabilitation training. The Cronbach’s alpha coefficient of this scale was 0.907 in this study.
2.3.7 Harris Hip Scoreing System
Harris Hip Scoreing System was compiled by Harris (31), the higher the score indicates that the patient’s hip function is better, the scale mainly includes four aspects of pain (44 points), function (47 points), deformity (four points), mobility (five points), the total score of 100 points, of which 90–100 points is excellent, 80–89 points is good, 70–79 was classified as fair, and ≤ 69 was classified as poor. The Cronbach’s alpha coefficients for this scale ranged from 0.830 to 0.910.
2.4 Statistical analysis
Data were statistically analyzed using SPSS 29.0 and R4.4.2 software. Normally distributed quantitative data were expressed as mean ± SD, and qualitative data were expressed as frequency and percentage (%); comparisons between groups were made using two independent samples t-test and chi-square test. Quantitative data that did not conform to the normal distribution were expressed as median and quartiles [M(P25, P75)], and the Mann-Whitney rank-sum - sum test was used for comparison between groups. Qualitative data were described by the number of cases and percentage (%), and the χ2-test, Fisher’s exact probability method, and rank-sum test were used for comparison between groups. Variables that were statistically significant in the one-way analysis were included in the multifactor Logistic regression analysis, and the stepwise forward-backward method was used to screen the independent predictors, while the multicollinearity between the predictor variables was checked by the Variance Inflation Factor (VIF), which indicated the existence of multicollinearity between the variables when the VIF was ≥5; finally, the predictive model was constructed using the R software, and the nomogram was drawn. The predictive ability of the model was evaluated using the Hosmer-Lemeshow goodness-of-fit test and the Area Under the Curve (AUC) of the receiver operating characteristic (ROC) curve, and the AUC value was close to 1, which indicated that the model had good predictive ability. The calibration and clinical utility value of the model were evaluated by the calibration curve and Decision Curve Analysis (DCA). And the model was also internally validated by repeated sampling 1,000 times using the Bootstrap method with a sample size of 205 cases per sampling to assess the stability of the model. The difference was considered statistically significant at two-sided P < 0.05.
2.5 Ethical considerations
The study followed the Declaration of Helsinki and was approved by the Ethics Committee of the Second Affiliated Hospital of Shandong First Medical University (2024-H-053).
3 Results
3.1 Current status of post-operative kinesiophobia in THA patients
The 205 THA patients were categorized into kinesiophobic and non-kinesiophobic groups according to whether or not they developed kinesiophobia postoperatively, of which 126 developed kinesiophobia postoperatively, with a kinesiophobia incidence rate of 61.5%.
3.2 Univariate analysis of factors influencing post-operative kinesiophobia in THA patients
The results of the univariate analysis of the two groups of patients showed statistically significant differences in gender, age, place of residence, monthly household income, presence of comorbid chronic diseases, pain history duration, anxiety, depression, social support, coping styles, rehabilitation self-efficacy, and hip function (P < 0.05), as shown in Table 1.
TABLE 1
| Variables | Non-kinesiophobic group (N = 79) | Kinesiophobia group (N = 126) | Statistics | P-value |
|---|---|---|---|---|
| Gender (%) | 23.3801 | <0.001 | ||
| Male | 51 (64.60) | 38 (30.20) | – | – |
| Female | 28 (35.40) | 88 (69.80) | – | – |
| Current address (%) | 13.2401 | <0.001 | ||
| Urban | 39 (49.40) | 31 (24.60) | – | – |
| Rural | 40 (50.60) | 95 (75.40) | – | – |
| Educational level (%) | 0.3071 | 0.989 | ||
| Primary school and below | 21 (26.60) | 31 (24.60) | – | – |
| Middle school | 33 (41.80) | 52 (41.30) | – | – |
| High school/technical secondary school | 12 (15.20) | 19 (15.10) | – | – |
| Junior college | 7 (8.90) | 12 (9.50) | – | – |
| University and above | 6 (7.60) | 12 (9.50) | – | – |
| Marital status (%) | 0.7381 | 0.691 | ||
| Widowed | 0 (0.00) | 1 (0.80) | – | – |
| Unmarried | 1 (1.30) | 1 (0.80) | – | – |
| Married | 78 (98.70) | 124 (98.40) | – | – |
| Medical payment methods (%) | 5.5601 | 0.062 | ||
| Urban and rural residents’ medical insurance | 47 (59.50) | 72 (57.10) | – | – |
| Urban workers’ medical insurance | 17 (21.50) | 15 (11.90) | – | – |
| Out-of-pocket expenses | 15 (19.00) | 39 (31.00) | – | – |
| Monthly household income (%) | 59.3951 | <0.001 | ||
| <3,000 | 9 (11.40) | 76 (60.30) | – | – |
| 3,000–5,000 | 44 (55.70) | 45 (35.70) | – | – |
| ≥5,000 | 26 (32.90) | 5 (4.00) | – | – |
| Presence of comorbid chronic diseases (%) | 33.2011 | <0.001 | ||
| No | 58 (73.40) | 39 (31.00) | – | – |
| Yes | 21 (26.60) | 87 (69.00) | – | – |
| Number of years of pain (%) | 168.2161 | <0.001 | ||
| >1 | 14 (17.70) | 97 (77.00) | – | – |
| ≤1 | 65 (82.30) | 29 (23.00) | – | – |
| Age | 58.85 ± 11.66 | 68.44 ± 11.61 | −5.7462 | <0.001 |
| BMI | 24.71 ± 3.67 | 24.61 ± 3.84 | 0.2012 | 0.841 |
| Pain numeric score | 1.42 ± 1.64 | 1.59 ± 1.63 | −0.7252 | 0.469 |
| Anxiety | 2.86 ± 1.91 | 8.91 ± 3.81 | 13.1202 | <0.001 |
| Depression | 3.95 ± 4.27 | 8.37 ± 4.50 | −6.9702 | <0.001 |
| Social support score | 51.38 ± 5.33 | 36.16 ± 8.13 | 14.7602 | <0.001 |
| Rehabilitation self-efficacy score | 99.52 ± 4.93 | 75.10 ± 14.72 | 14.2402 | <0.001 |
| Active coping style score | 29.73 ± 2.87 | 16.50 ± 6.30 | 17.5502 | <0.001 |
| Passive coping style score | 7.65 ± 2.50 | 13.93 ± 4.70 | −10.9302 | <0.001 |
| Harris hip function score | 66.29 ± 9.29 | 43.89 ± 11.91 | 14.2202 | <0.001 |
Univariate analysis of post-operative development of kinesiophobia in total hip arthroplasty patients.
1Is the χ2-value. 2Is the t-value.
3.3 Logistic regression analysis of factors influencing post-operative kinesiophobia in THA patients
The occurrence of kinesiophobia was used as the dependent variable (yes = 1, no = 0), and the variables that were statistically significant in the univariate analysis were used as the independent variables. Logistic regression (stepwise forward-backward method) was chosen to screen for independent predictors, and a table of the independent variable assignments is shown in Table 2. Variance Inflation Factor (VIF) tests were performed, and all variables had VIF values < 2, indicating no covariance and good model fit. The results showed that pain history duration, anxiety, positive coping styles, rehabilitation self-efficacy, and Harris hip function were the most important predictors of the occurrence of THA in patients with predictors of kinesiophobia, see Table 3.
TABLE 2
| Variables | Assignment of values |
|---|---|
| Gender | Male = 0, female = 1 |
| Current address | Urban = 0, rural = 1 |
| Monthly household income | <3,000 = 0, 3,000–5,000 = 1, ≥5,000 = 2 |
| Presence of comorbid chronic diseases | No = 0, yes = 1 |
| Pain history duration | >1 = 0, ≤1 = 1 |
| Age | Substituting the original value into |
| Anxiety | Substituting the original value into |
| Depression | Substituting the original value into |
| Social support score | Substituting the original value into |
| Rehabilitation self-efficacy score | Substituting the original value into |
| Coping style score | Substituting the original value into |
| Harris hip function score | Substituting the original value into |
Assignment of independent variables.
TABLE 3
| Variables | β | SE | Wald χ2 | OR (95% CI) | P |
|---|---|---|---|---|---|
| Constant | 56.311 | 24.91 | 5.11 | – | 0.024 |
| Pain history duration1 | −5.426 | 2.507 | 5.147 | 0.004 (0.000–0.599) | 0.030 |
| Anxiety | 1.928 | 0.849 | 5.822 | 6.876 (1.302–36.308) | 0.023 |
| Rehabilitation self-efficacy | −0.331 | 0.168 | 3.483 | 0.718 (0.517–0.998) | 0.049 |
| Active coping style | −1.159 | 0.450 | 6.444 | 0.314 (0.130–0.758) | 0.010 |
| Harris hip function | −0.204 | 0.097 | 3.787 | 0.815 (0.674–0.986) | 0.036 |
Logistic regression of factors influencing the development of post-operative kinesiophobia in total hip arthroplasty (THA) patients.
1The reference for the pain history duration is >1 year.
3.4 Construction of a nomogram prediction model for post-operative kinesiophobia in THA patients
According to the logistic regression results of the post-operative kinesiophobia prediction model for THA patients plotted with the R software, each predictor is located on the left side of the Nomogram, and the corresponding scores are obtained by making a vertical line upward from them, and these scores are added to obtain the total score, and the predicted probability of the patient’s development of kinesiophobia in the post-operative period can be obtained by making a vertical line downward from the coordinate axis of the total score (Figure 1). For example, a patient who underwent THA surgery with a pain history duration of more than 1 year has an anxiety score of 12, a rehabilitation self-efficacy score of 50, an active coping score of 10, and a hip function score of 30. In the Nomogram, each variable has a corresponding score. Thus, pain history duration of more than 1 year corresponds to a score of 19, anxiety status corresponds to a score of 42, rehabilitation self-efficacy corresponds to a score of 69, active coping corresponds to a score of 82, and hip function corresponds to a score of 30. The predicted probability of kinesiophobia in a post-operative patient with THA was obtained by summing the scores for each variable to obtain a total score of 242, and then drawing a vertical line at the total score. Thus, the Nomogram model predicted the probability of kinesiophobia in this patient after surgery was 85%.
FIGURE 1
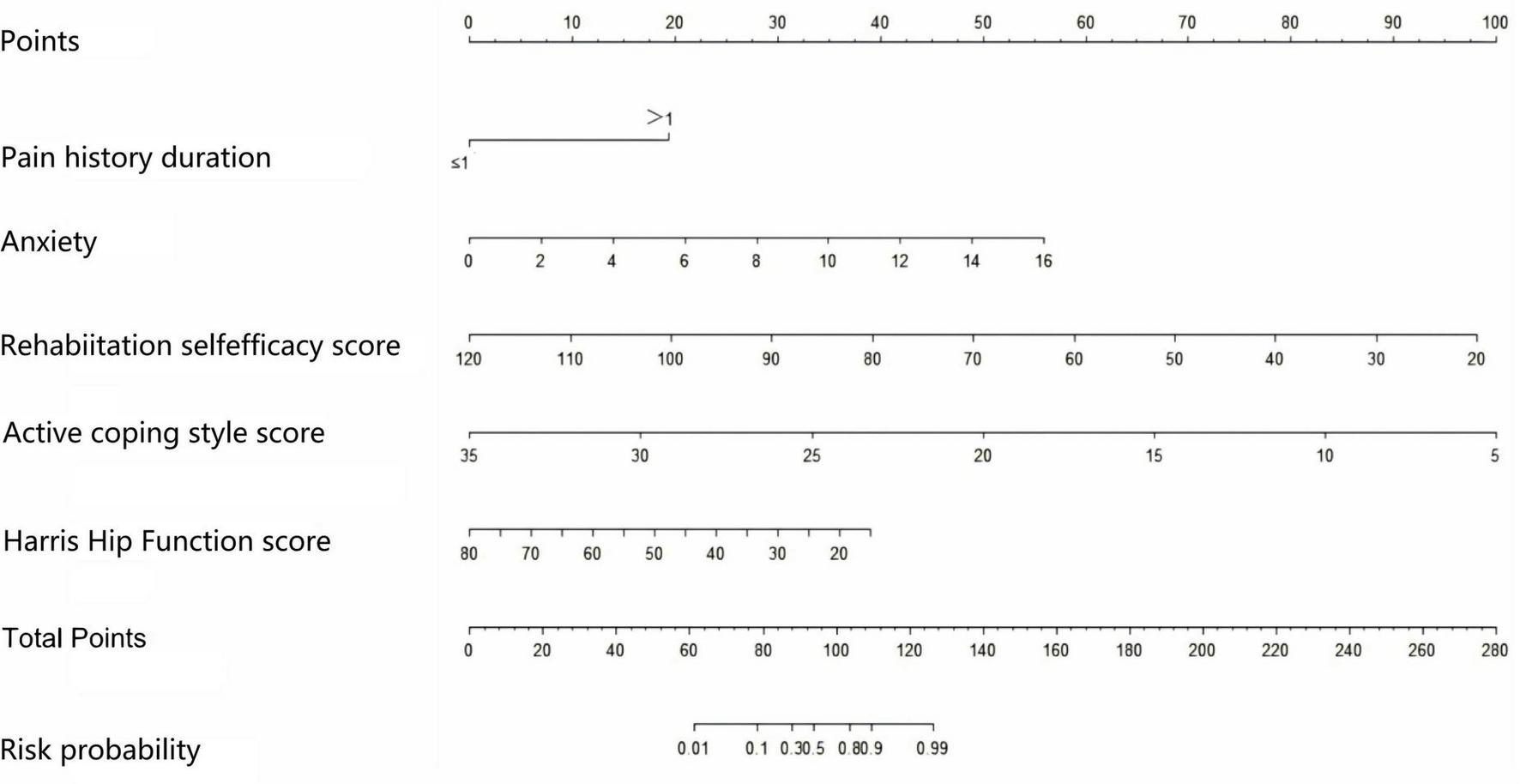
Nomogram risk prediction model for fear of movement after total hip arthroplasty (THA) surgery.
3.5 Evaluation and validation of a nomogram prediction model for post-operative kinesiophobia in THA patients
The ROC curve of this study (Figure 2) shows that the AUC value of the model is 0.947 (95% CI 0.919∼0.975), the specificity is 0.873, the sensitivity is 0.911, and the Hosmer-Lemeshow test χ2 = 2.287, P = 0.971, which suggests that the model has a better differentiation, fit, and prediction ability. The horizontal coordinate of the calibration curve is the probability of the event predicted by the model, and the vertical coordinate is the probability of the event actually observed. When the calibration curve is closer to the 45° diagonal, it indicates that the predicted probability is closer to the actual probability. The calibration curve in this study is close to the ideal curve (Figure 3A), indicating that there is consistency between the predicted and actual values.
FIGURE 2
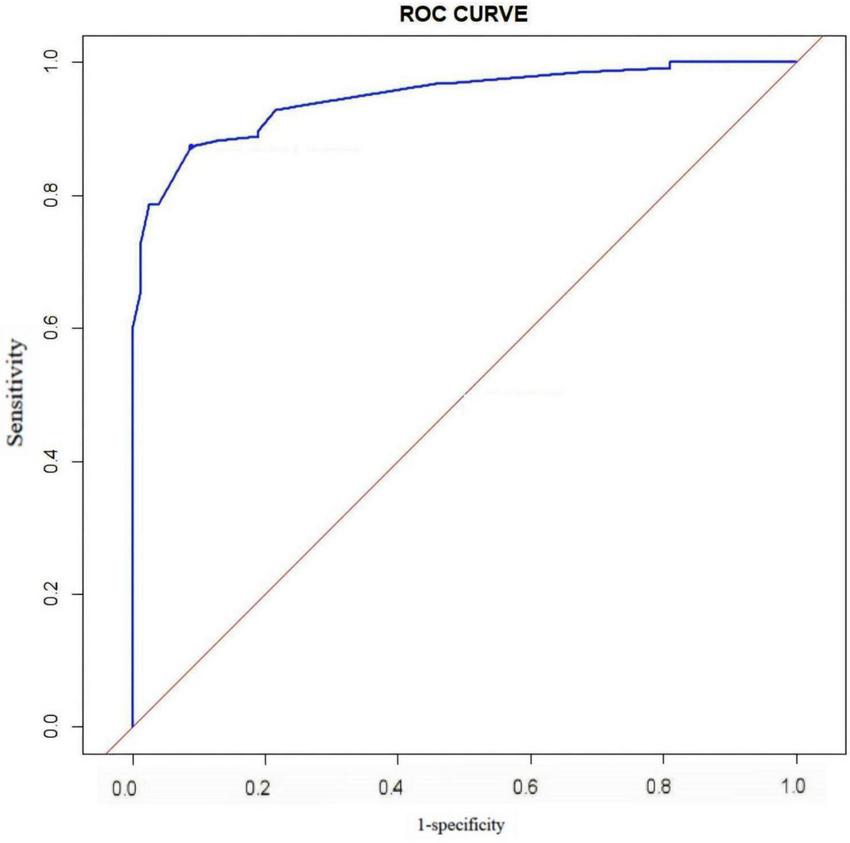
Receiver operating characteristic (ROC) curve of the predictive model for the risk.
FIGURE 3
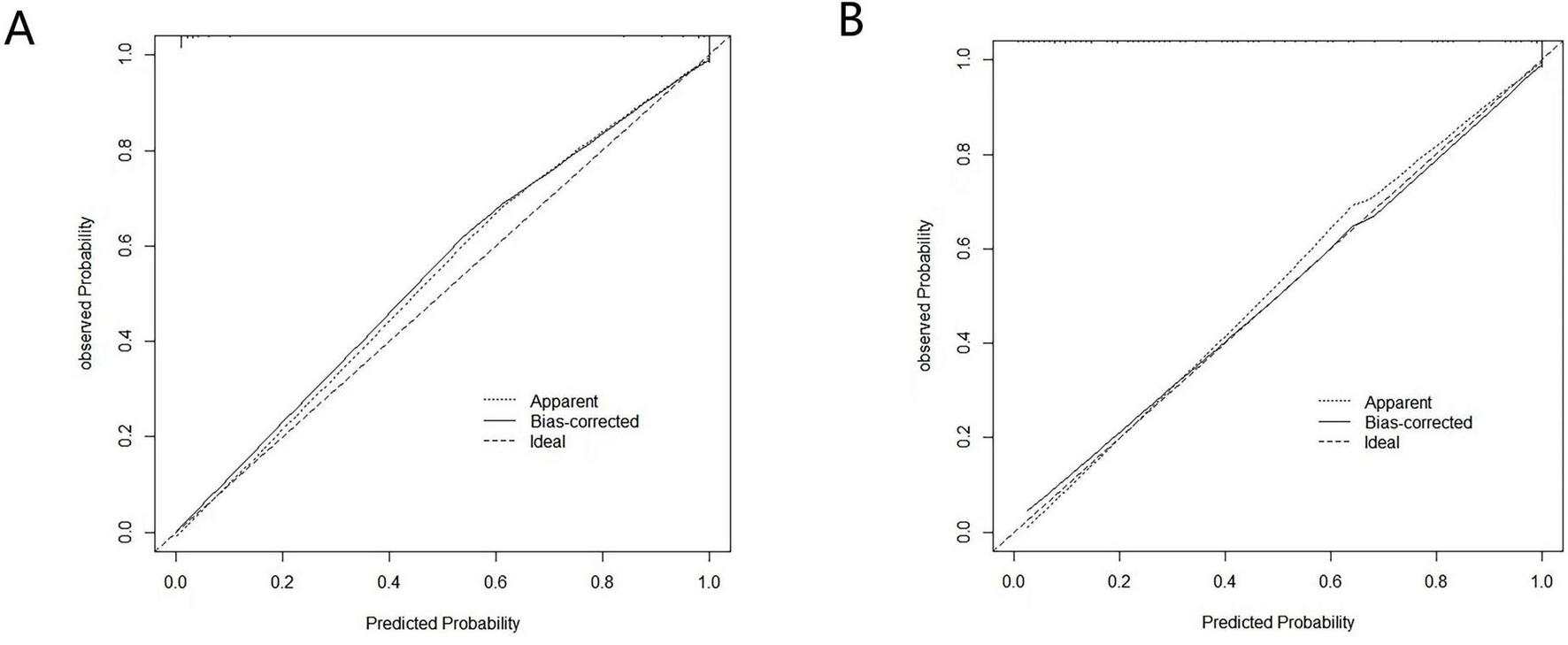
Calibration curve of the predictive model. (A) Calibration curve of the original model. (B) Calibration curve after 1,000 bootstrap resamples for internal validation.
The model was internally validated using the Bootstrap method with 1,000 repeated samples. The result yielded an AUC value of 0.912 (95% CI 0.875–0.949), and the calibration curve fitted well with the ideal curve (Figure 3B), indicating that the model had a good predictive effect.
The decision analysis curve (DCA) is a tool for assessing the utility and clinical application value of clinical predictive models by plotting decision curves to compare the clinical benefits of different predictive models at different therapeutic decision thresholds. The horizontal axis of the curve represents the threshold probability, and the vertical axis represents the net benefit. The solid black line refers to no therapeutic intervention for any patient, the dashed black line refers to therapeutic intervention for all patients, and the blue curve refers to the overall net benefit of that predictive model over the entire range of thresholds. In the threshold range at the bottom of the horizontal axis, the net gain of the predictive model is higher than both the ALL line and the None line, indicating that the model has practical value; when the blue curve is very close to or coincides with the two extreme lines, the ALL line and the None line, it indicates that the model may be of less value for application. The blue curves in this study were between the thresholds 0–1, and the curves were all above the reference line, indicating that the model has a high net benefit and good clinical utility (Figure 4).
FIGURE 4
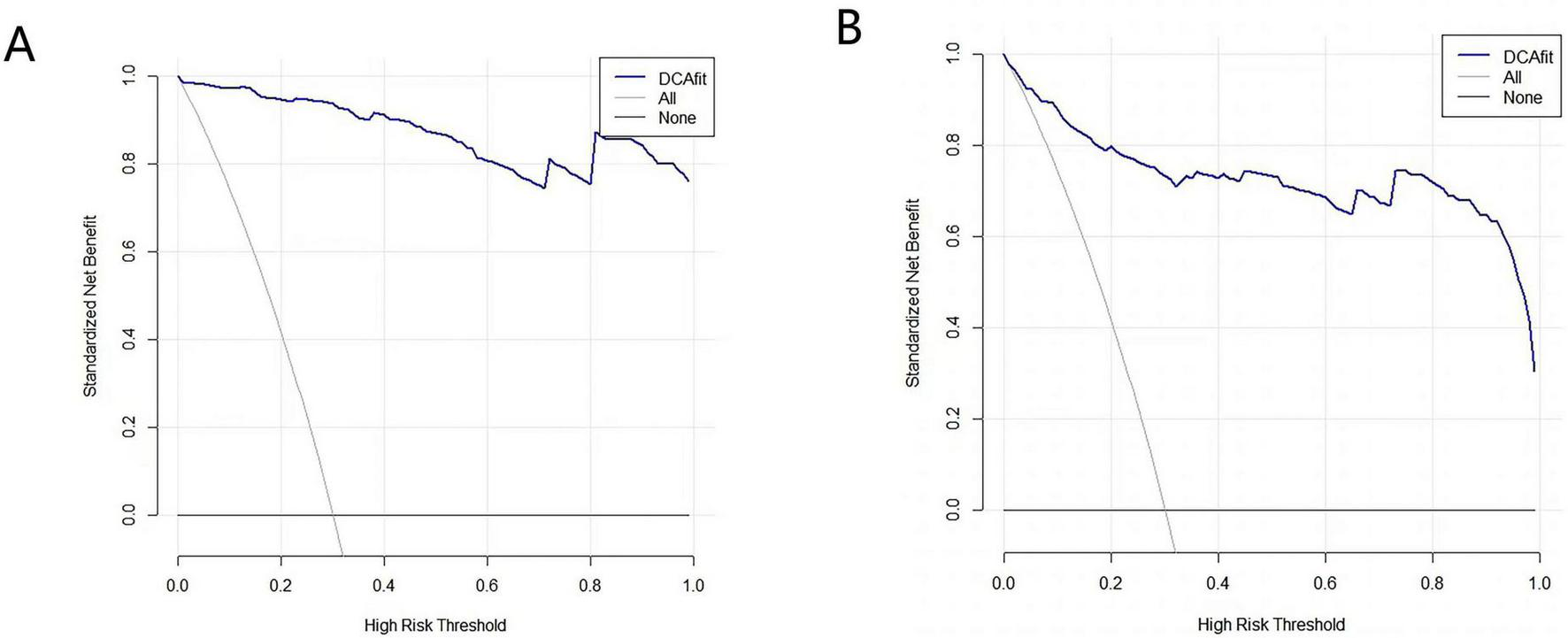
Clinical decision curve of the predictive model. (A) Decision analysis curves (DCA) of the original model. (B) DCA after 1,000 bootstrap resamples for internal validation.
4 Discussion
4.1 Current status of the occurrence of post-operative kinesiophobia in THA patients
The results of this study showed that the incidence of post-operative kinesiophobia in THA patients was 61.5%, which was similar to the findings of Huang Li et al. (23) (58.7%) and higher than the findings of Lai et al. (32) (43.78%), and the reasons for this analysis may be due to the fact that the age of the population included in the present study is on the high side, which may affect the patients’ psychological tolerance and the degree of their fear of post-operative rehabilitation and exercise; and secondly, there are differences in the various studies differed in the time of assessment of kinesiophobia, and the physical recovery and psychological state of patients differed at different post-operative time nodes, which may lead to fluctuations in the assessment of the incidence of kinesiophobia; in addition, the geographical environment is an important factor. There are differences in medical conditions, cultural backgrounds, and patients’ cognitive levels of diseases in different regions, which may have an impact on the occurrence of post-operative exercise phobia among patients. Kinesiophobia, as a kind of excessive fear of pain or injury, will cause patients to avoid necessary activities and functional exercises, which will hinder the recovery of joint function and delay the post-operative rehabilitation process (33). And some studies have shown (34) that the effects of kinesiophobia on patients may last for several years or even accompany patients throughout their lives. Therefore, early identification and intervention of kinesiophobia is essential to improve the prognosis of patients.
4.2 Analysis of factors influencing the occurrence of kinesiophobia in THA patients after surgery
4.2.1 Pain history duration
This study showed that a pain history of more than 1 year was a risk factor for the occurrence of kinesiophobia in THA patients after surgery, which was consistent with the findings of Wen et al. (35), that patients enduring a longer period of pain preoperatively had a greater risk of developing kinesiophobia after surgery. The reason for this analysis may be that with the development of the accelerated recovery surgery concept (ERAS) and the advancement of pain management techniques, perioperative pain management in THA has achieved remarkable results, and the post-operative pain level of patients is generally at a relatively low and stable level, and the effect of the difference in the pain level on kinesiophobia may be weakened. In contrast, pain chronology indicates the duration of pain, reflecting patients’ long-term experience of pain and the long-lasting effects of chronic pain. Studies have shown (36, 37) that long-term chronic pain may lead to increased sensitivity of the central nervous system to pain signals, and that even mild post-operative pain may be perceived by the patient as severe pain, which induces fear and avoidance behaviors. In addition, patients with long years of pain may have developed negative expectations and catastrophizing thinking about pain and are more likely to develop false perceptions of the disease (38, 39). Therefore, the impact of long-term chronic pain may go beyond the pain itself, suggesting that healthcare professionals need to pay attention to the duration and degree of preoperative pain while focusing on the patients’ post-operative pain management, and to conduct more detailed psychological assessments and interventions for patients experiencing longer periods of preoperative pain.
4.2.2 Anxiety
This study shows that patients with high anxiety levels are at a higher risk of developing kinesiophobia after surgery. This is due to the fact that higher levels of anxiety activate the sympathetic nervous system, causing increased heart rate and muscle tension, which exacerbate exercise avoidance behaviors, creating a vicious cycle of “anxiety-avoidance” (40). Patients usually have more negative expectations of pain and functional exercise, are more sensitive to pain and discomfort, and easily perceive functional exercise as a potential threat to aggravate pain, and misinterpret minor discomfort during rehabilitation as a worsening of the condition, leading to fear and avoidance of rehabilitation exercises (41). In addition, patients’ concerns about prognostic outcomes and the presence of post-operative complications can further exacerbate their anxiety. Therefore, in clinical practice, the assessment and management of anxiety can be incorporated into the prevention and intervention strategies of kinesiophobia to help patients effectively alleviate anxiety, reduce the risk of post-operative kinesiophobia, and improve patient prognosis.
4.2.3 Rehabilitation self-efficacy
The results of this study showed that patients with higher rehabilitation self-efficacy scores were less likely to develop kinesiophobia. Rehabilitation self-efficacy, which refers to a patient’s specific confidence and beliefs about functional recovery after surgery, is one of the most important predictors of patient prognostic outcomes and an important influence on functional recovery in THA patients (42). Previous studies have shown (43) that self-efficacy is a key variable in predicting fearful avoidance behavior and plays a mediating role between an individual’s fearful emotions and avoidance behavior. Patients with low rehabilitation self-efficacy tend to lack confidence in various post-operative motor exercises and are more prone to feelings of helplessness and fear, and this negative psychological state will make them tend to avoid rehabilitation training, which in turn will affect the physical recovery process. In addition, a longitudinal study showed that rehabilitation self-efficacy can reduce patients’ fear of anticipated activities and better predict the long-term outcomes of post-operative THA patients (44). Therefore, improving rehabilitation self-efficacy is crucial for reducing the risk of kinesiophobia and improving prognosis, and healthcare professionals can help patients build confidence and improve self-efficacy by setting small achievable goals, providing positive feedback, and encouraging patients to share their successes.
4.2.4 Active coping styles
The results of this study showed that a low active coping score was a risk factor for the development of kinesiophobia in THA patients after surgery. Coping styles refer to the cognitive and behavioral strategies that individuals adopt when facing stressful events (45). It has been shown (46) that positive coping styles are significantly and negatively associated with kinesiophobia. Patients who adopt positive coping styles usually have better psychological resilience and are better able to adapt to the challenges they face during the rehabilitation process, such as pain and joint discomfort. These patients are optimistic about the disease and the recovery process, and tend to actively seek support from the outside world and explore solutions to their problems. Before surgery, they are fully aware of the risks and expected outcomes, which reduces their uncertainty about the surgery and recovery process. In the post-operative period, they were able to actively participate in post-operative rehabilitation training, and their uneasiness and fear of rehabilitation exercises were relatively low. It has also been shown (47) that coping styles play a partial mediating role between self-efficacy and kinesiophobia, and that positive coping styles enhance patients’ self-efficacy and make them believe that they can safely perform rehabilitation exercises, which they will regard as an effective way to restore their health, rather than as a source of triggering fear. This positive perception and attitude will help patients face the rehabilitation process more comfortably and reduce the risk of kinesiophobia. Therefore, healthcare professionals should carefully observe patients’ emotional changes, provide them with timely psychological guidance and health education, guide them to adopt positive coping styles, encourage them to take the initiative to participate in rehabilitation training, improve their cognitive ability regarding the disease and exercise compliance, and provide them with support and assistance when necessary.
4.2.5 Harris hip function
The results of this study show that patients with poorer hip function are more likely to develop kinesiophobia. The reason for this may be analyzed because the success of the surgery allowed patients who had been suffering from long-term pain due to hip disease to regain hip function and have their pain relieved. When patients do not suffer from significant pain during exercise, they are less likely to be fearful of exercise. In addition, the improvement of joint mobility and daily living ability will enhance patients’ self-confidence and self-efficacy, which will make them participate more actively in rehabilitation training and reduce their fear and avoidance behaviors toward exercise. On the contrary, patients with limited function may have a fear of exercise due to the psychological burden exacerbated by repeated frustration. In addition, patients with better hip joint function are usually able to complete rehabilitation training earlier and more smoothly, and earlier rehabilitation training also facilitates the recovery of post-operative joint function, forming a virtuous circle and thus effectively preventing the occurrence of kinesiophobia (48). This suggests that we can start rehabilitation training as early as possible under the premise of ensuring safety in the clinic and formulate an individualized rehabilitation plan to gradually improve the joint mobility and muscle strength of patients and promote functional recovery. At the same time, we should regularly assess the patients’ hip function as an important indicator for monitoring the rehabilitation process and predicting the risk of kinesiophobia, and timely adjust the rehabilitation program according to the changes in scores.
4.3 Scientificity and significance of constructing a nomogram prediction model for post-operative kinesiophobia in THA patients
In this study, five predictors were screened using Logistic regression (stepwise forward-backward method), and the nomogram prediction model was plotted to transform the complex regression equations into visualized graphs. The predictive model demonstrated excellent performance in terms of the evaluation metrics of the model. The area under the ROC curve of the prediction model was 0.947, the specificity was 0.873, the sensitivity was 0.911, and the Hosmer-Lemeshow test χ2 = 2.287, P = 0.971, and internal validation using the Bootstrap method yielded a ROC value of 0.912, which suggests that the prediction model has good post-operative kinesiophobia in THA patients with good predictive performance and accuracy. The calibration curves of both the model and internal validation showed consistency between predicted and actual values, and the DCA curves all indicated that the model had good clinical utility. Constructing a nomogram can help healthcare professionals to more intuitively understand the risk probability of a particular indicator occurring (49). By comprehensively assessing the impact of multiple factors on the risk of kinesiophobia, it is possible to more accurately predict which patients belong to the high-risk group, which is conducive to healthcare personnel taking targeted preventive and intervention measures according to the differences in different patient groups, to reduce the incidence of post-operative kinesiophobia, and to improve the long-term prognosis of patients.
In addition, as the predictors included in this model encompassed biological, psychological and behavioral dimensions, and the study subjects were all patients who underwent THA for the first time in the same hospital, the relative homogeneity of the study subjects reduced the interference of irrelevant variation on the results to a certain extent, resulting in the AUC values of the present study being higher than 0.9. However, despite the results of the internal validation supporting the good robustness of the model, in view of the limitations of the present limitations of study, the very high performance of the model still needs to be further validated by multicenter external studies in the future to ensure the general applicability and reliability of the model in a wider range of clinical settings.
4.4 Limitations and innovations of this study
Although the predictive model constructed in this study showed excellent performance, there are some limitations. Firstly, this study was a cross-sectional study, and all data were collected at the same post-operative time point; patients were not followed up. Secondly, the nomogram prediction model constructed in this study was not externally validated, and its external adaptability is not yet clear. Moreover, with the use of single-center convenience sampling, the representativeness of the sample may be affected by the level of diagnosis and treatment of a specific healthcare institution, the regional culture, and the characteristics of the patient group, which limits the generalizability of the results of the study to a certain degree and puts some constraints on its generalization and application. It is suggested that future studies may conduct longitudinal surveys, as well as enhance the external validity of the model through multi-center, random sampling research methods, and external validation to make the results more generalizable. In addition, this study used a biopsychosocial model to select the different dimensions of the study variables and visualized the complex predictive model in the form of a nomogram. This provides a convenient tool for individualized risk assessment in the clinic. In the future, the model can also be combined with the Accelerated Rehabilitation Surgical Theory (ERAS), which can be utilized to rapidly screen people at high risk for kinesiophobia, thus initiating multidisciplinary interventions at an early stage, and ultimately accelerating the patient’s recovery process.
5 Conclusion
The incidence of post-operative kinesiophobia in THA patients is high, and patients with a pain history duration of more than 1 year, poor hip function, low active coping, and poor rehabilitation self-efficacy are more likely to develop kinesiophobia in the post-operative period. The risk prediction model constructed in the present study has a good predictive efficacy, and it can serve as an effective tool for the early prediction of the risk of post-operative kinesiophobia in patients with THA in the clinical setting.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Review Committee of the Second Affiliated Hospital of Shandong First Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SD: Data curation, Methodology, Writing – original draft, Investigation, Writing – review & editing. XG: Data curation, Writing – original draft, Writing – review & editing, Supervision, Formal analysis. YZ: Formal analysis, Writing – review & editing, Investigation, Software. YC: Formal analysis, Software, Writing – review & editing, Methodology. CW: Data curation, Resources, Visualization, Writing – review & editing. SP: Writing – review & editing, Validation, Project administration, Formal analysis, Supervision. LW: Formal analysis, Conceptualization, Writing – review & editing, Software. WH: Conceptualization, Writing – review & editing, Funding acquisition, Visualization. WL: Funding acquisition, Writing – review & editing, Supervision, Resources, Project administration, Conceptualization.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This research was supported by the Research Foundation for Doctoral Talents of Anhui University of Chinese Medicine (approval number: 2024rcyb022), and the Shandong Province Medical and Health Science and Technology Project (approval number: 202404070508).
Acknowledgments
We thank all the participants and researchers in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Alnahhal A Aslam-Pervez N Sheikh HQ . Templating hip arthroplasty.Open Access Maced J Med Sci. (2019) 7:672–85. 10.3889/oamjms.2019.088
2.
Ferguson RJ Palmer AJ Taylor A Porter ML Malchau H Glyn-Jones S . Hip replacement.Lancet. (2018) 392:1662–71. 10.1016/S0140-6736(18)31777-X
3.
Wu YJ Wang JW Zhang YM Pei Q Wang T . Comparison of the efficacy of total hip arthroplasty for femoral neck fracture between SuperPATH approach and Moore approach.Chin Remedies Clin. (2020) 20:262–4. 10.11655/zgywylc2020.02.043
4.
Wainwright TW Gill M McDonald DA Middleton RG Reed M Sahota O et al Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. (2020) 91:3–19. 10.1080/17453674.2019.1683790
5.
Li ZW Feng LJ Yang J Yuan Q . A scoping review of assessment tools for fear of movement.J Nurs. (2024) 39:124–9. 10.3870/j.issn.1001-4152.2024.20.124
6.
Bullock GS Sell TC Zarega R Bennett C Ambegaonkar JP Butler C et al Kinesiophobia, knee self-efficacy, and fear avoidance beliefs in people with ACL injury: a systematic review and meta-analysis. Sports Med. (2022) 52:3001–19. 10.1007/s40279-022-01739-3
7.
Sergooris A Verbrugghe J De Baets L Timmermans A Vereecken S . Arecontextual factors associated with activities and participation after total hip arthroplasty? A systematic review.Ann Phys Rehabil Med. (2023) 66:101712. 10.1016/j.rehab.2022.101712
8.
Peduzzi P Concato J Feinstein AR Holford TR . Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates.J Clin Epidemiol. (1995) 48:1503–10. 10.1016/0895-4356(95)00048-8
9.
Li HY Ding X Yang Y Yang Y . Influencing factors of exercise phobia in elderly patients after radical resection of lung cancer and construction of its risk prediction nomogram model.Pract J Card Cereb Pneum Vasc Dis. (2025) 33:20–4. 10.12114/j.issn.1008-5971.2025.00.141
10.
Li KX Wang Q Shao YR . Construction and validation of a prediction model for panic disorder during rehabilitation in patients undergoing surgery for lumbar disc herniation.Mod. Nurse. (2024) 31:68–73. 10.19792/j.cnki.1006-6411.2024.29.015
11.
Wang HZ Zhou LL Cheng PF Ke S Song Y Wu R et al Construction and validation of a predictive model for kinetophobia in patients after percutaneous coronary intervention. Chin J Nurs. (2024) 59:2108–15. 10.3761/j.issn.0254-1769.2024.17.009
12.
Sharif-Nia H Nazari R Hajihosseini F Froelicher E Osborne J Taebbi S et al The relationship of fear of pain, pain anxiety, and fear-avoidance beliefs with perceived stress in surgical patients with postoperative kinesiophobia. BMC Psychol. (2025) 13:420. 10.1186/s40359-025-02743-8
13.
Marmouta P Marmouta L Tsounis A Tzavara C Malliarou M Fradelos E et al Effect of kinesiophobia and social support on quality of life after total hip arthroplasty. Healthcare. (2025) 13:1366. 10.3390/healthcare13121366
14.
Alsaleem MK Alkhars AM Alalwan HA Almutairi A Alonayzan A AlYaeesh IA . Kinesiophobia post total hip arthroplasty: a retrospective study.Cureus. (2021) 13:e15991. 10.7759/cureus
15.
Li LL Song H Sun Q . A survey on the current status and influencing factors of early exercise fear in patients with femoral head necrosis after total hip arthroplasty.Psychol Month. (2025) 20:213–5. 10.19738/j.cnki.psy.2025.12.063
16.
Zhang L Zhang ZR Zhang CL Fu J . Latent profile analysis and influencing factors of early postoperative kinesiophobia in elderly patients with total hip arthroplasty.Chin J Mod Nurs. (2024) 30:4002–8. 10.3760/cma.j.cn115682-20231116-02107
17.
Chen YQ. Analysis of the Status and Influencing Factors of Kinesiophobia in Patients Undergoing Total Hip Arthroplasty in Changsha city. Changsha: Springer (2020). 10.27137/d.cnki.ghusu.2020.001840
18.
Wang Y Zhang ZY Wang LY . Influencing factors of patients developing exercise fear after total hip arthroplasty.Mod Med Health Res Electron J. (2025) 9:133–7. 10.3969/j.issn.2096-3718.2025.06.043
19.
Kamp T Stevens M Van Beveren J Rijk P Brouwer R Bulstra S et al Influence of social support on return to work after total hip or total knee arthroplasty: a prospective multicentre cohort study. BMJ Open. (2022) 12:e059225. 10.1136/bmjopen-2021-059225
20.
Morri M Venturini E Franchini N Ruisi R Culcasi A Ruggiero A et al Is kinesiophobia a predictor of early functional performance after total hip replacement? A prospective prognostic cohort study. BMC Musculoskelet Disord. (2020) 21:724. 10.1186/s12891-020-03748-7
21.
Engel G . The need for a new medical model: a challenge for biomedicine.Science. (1977) 196:129–36. 10.3109/13561828909043606
22.
Zheng Q Lu PL Wang YM He MT Lu TT . Analysis of risk factors of kinesiophobia after total hip arthroplasty.Nurs Pract Res. (2021) 18:3176–80. 10.3969/j.issn.1672-9676.2021.21.004
23.
Huang L Yang X Li FF Zheng QY Zhou JL Cao J . Current status and influencing factors of kinesiophobia in patients after hip arthroplasty or knee arthroplasty.Chin J Bone Joint Surg. (2023) 16:1001–7. 10.3969/j.issn.2095-9958.2023.11.05
24.
Miller MB Roumanis MJ Kakinami L Dover GC . Chronic pain patients’ kinesiophobia and catastrophizing are associated with activity intensity at different times of the day.J Pain Res. (2020) 13:273–84. 10.2147/JPR.S230039
25.
Hu W. Cultural Adaptation of the Simplified Chinese Version of TSK and FABQ Scales and its Application in Degenerative Low Back and Leg Pain. Shanghai: Second Military Medical University (2012).
26.
Xie YN . A preliminary study of the reliability and validity of the Simple Coping Style Scale.Chin J Clin Psychol. (1998) 2:53–4.
27.
Xiao SY . Theoretical basis and research application of the Social Support Rating Scale.J Clin Psychiatry. (1994) 2:98–100.
28.
Zigmond AS Snaith RP . The hospital anxiety and depression scale.Acta Psychiatr Scand. (1983) 67:361–70. 10.1111/j.1600-0447.1983.tb09716.x
29.
Waldrop D Lightsey OR Jr. Ethington CA Woemmel CA Coke AL . Self-efficacy, optimism, health competence, and recovery from orthopedic surgery.J Couns Psychol. (2001) 48:233–8. 10.1037/0022-0167.48.2.233
30.
Wang HY Xu YL Hu SL Zhou L Qian Y Qian HJ . Evaluation of the reliability and validity of the Chinese version self-efficacy for rehabilitation outcome scale.Chin J Mod Nurs. (2014) 20:268–70. 10.3760/cma.j.issn.1674-2907.2014.03.007
31.
Harris WH . Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation.J Bone Joint Surg Am. (1969) 51:737–55.
32.
Lai T Wu ML Hu KL Zhou XK Hu JX . Analysis of the current situation and influencing factors of motion phobia in patients after total hip arthroplasty.Orthop Surg. (2024) 15:258–62. 10.3969/j.issn.1674-8573.2024.03.012
33.
Liu T Ma YR Qin YJ Fan X Liu B . Influence of education and exposure intervention in patients with irrational fear of movement after total hip arthroplasty.J Nurs. (2023) 38:22–6. 10.3870/j.issn.1001-4152.2023.10.022
34.
Filardo G Roffi A Merli G Marcacci T Kon E Perdisa F . Patient kinesiophobia affects both recovery time and final outcome after total knee arthroplasty.Knee Surg Sports Traumatol Arthrosc. (2016) 24:3322–8. 10.1007/s00167-015-3898-8
35.
Wen Y Zhao SX Luo Y Wang QC Yan XY Zuo XL et al Factors associated with kinesiophobia after total knee arthroplasty. Chin J Orthop Surg. (2023) 31:413–7. 10.3977/j.issn.1005-8478.2023.05.06
36.
Sun L Peng C Joosten E Billet B Vanneste S . Spinal cord stimulation and treatment of peripheral or central neuropathic pain: mechanisms and clinical application.Neural Plast. (2021) 2021:5607898. 10.1155/2021/5607898
37.
Quesada C Kostenko A Ho I Hatcher C Ackerley R Wartolowska K . Human surrogate models of central sensitization: a critical review and practical guide.Eur J Pain. (2021) 25:1389–428. 10.1002/ejp.1768
38.
Mun CJ Beitel M Oberleitner L Oberleitner DE Madden LM Bollampally P . Pain catastrophizing and pain acceptance are associated with pain severity and interference among methadone-maintained patients.J Clin Psychol. (2019) 75:2233–47. 10.1002/jclp.22842
39.
Sousa CRA Arsati YBOL Velly AM Silva CALD Arsati F . Catastrophizing is associated with pain-related disability in temporomandibular disorders.Braz Oral Res. (2023) 37:e070. 10.1590/1807-3107bor-2023.vol37.0070
40.
Li C Zhang L Lin YB Guo XR Lin KX Lu YY et al Influencing factors of kinesiophobia in lung cancer patients after thoracoscopic surgery. J Nurs. (2025) 40:39–43. 10.3870/j.issn.1001-4152.2025.07.039
41.
Zhang SL Wang JQ Zhao J Yang HY Xing L Fan HJ et al Status of postoperative kinesiophobia among breast cancer patients and its influencing factors. J Nurs. (2020) 35:24–7. 10.3870/j.issn.1001-4152.2020.19.024
42.
Zhang LF Zhang MF Xiao P Wang WH . Study on self-efficacy and related factors of rehabilitation exercise in elderly patients after total hip replacement.J Nurs Adm. (2017) 17:717–9. 10.3969/j.issn.1671-315X.2017.10.012
43.
Farley H . Promoting self-efficacy in patients with chronic disease beyond traditional education: a literature review.Nurs Open. (2019) 7:30–41. 10.1002/nop2.382
44.
Tu CY Shields N Gill SD Tacey M Lindner C Hill KD . Longitudinal changes in physical activity levels and fear of falling after hip fracture.Physiother Res Int. (2021) 26:e1884. 10.1002/pri.1884
45.
Cao EF Wang YT Li P Duan KX Ge WJ Wang J . Current status of acute stress disorder in patients with acute myocardial infarction after PCI and its relationship with illness perception and coping strategies.Nurs Res. (2024) 38:37–42. 10.12102/j.issn.1009-6493.2024.01.006
46.
Qin JW Xiong JJ Chen C Wang X Gao Y Zhou Y et al Influencing factors of kinesiophobia in older patients with chronic heart failure: a structural equation model. Clin Cardiol. (2023) 46:729–36. 10.1002/clc
47.
Shi HN Chen L Zhou LJ Wang L . Mediating effect of positive coping style between self-efficacy and kinesophobia among postoperative breast cancer patients.Milit Nurs. (2023) 40:59–62. 10.3969/j.issn.2097-1826.2023.03.014
48.
Wang WH Zhang LF Li XX Zhang MF . Joint function and its influencing factors in patients who underwent hip arthroplasty.Chin J Nurs. (2017) 52:649–53. 10.3761/j.issn.0254-1769.2017.06.002
49.
Pang YH Zhang HJ Liu T Jiang ZQ Shi XP Bi T et al Mediating effect of self-efficacy on the relationship between kinesiophobia and physical activity among female elderly osteoporosis patients. Chin Public Health. (2020) 36:628–31. 10.11847/zgggws1121618
Summary
Keywords
total hip arthroplasty, kinesiophobia, influencing factors, risk prediction mode, nomogram
Citation
Dong S, Guo X, Zhou Y, Chen Y, Wang C, Peng S, Wu L, Han W and Liu W (2025) Construction and validation of a predictive model for post-operative kinesiophobia in total hip arthroplasty patients. Front. Med. 12:1699157. doi: 10.3389/fmed.2025.1699157
Received
04 September 2025
Revised
15 October 2025
Accepted
06 November 2025
Published
24 November 2025
Volume
12 - 2025
Edited by
Tomasz Reysner, Poznan University of Medical Sciences, Poland
Reviewed by
Wanying Su, Hunan Provincial People’s Hospital, China
Grzegorz Kowalski, Uniwersytet Medyczny im. Karola Marcinkowskiego w Poznaniu, Poland
Updates
Copyright
© 2025 Dong, Guo, Zhou, Chen, Wang, Peng, Wu, Han and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiting Liu, liuweiting1213@126.com
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.