- 1Department of Radiology, Dianjiang People’s Hospital of Chongqing, Chongqing, China
- 2Department of Pharmacy, Dianjiang People’s Hospital of Chongqing, Chongqing, China
- 3Department of Medical Imaging, School of Basic Medical Sciences, Xinjiang Medical University, Urumqi, China
Intercostal artery (ICA) injury during CT-guided percutaneous transthoracic needle biopsy (PTNB) is a rare but potentially severe complication. This case report describes a cautious approach for detecting and managing suspected ICA injury using a coaxial needle system. During PTNB in a 71-year-old male with lung cancer, ICA injury was detected through blood aspiration during needle withdrawal. Management involved immediate cessation of withdrawal, slight needle advancement for mechanical hemostasis, and serial monitoring, achieving hemostasis without requiring additional invasive interventions. Literature review of cases from 2018 to 2024 revealed that current management approaches vary based on severity, with a 30% mortality rate among reported cases. Most ICA injuries are detected post-procedurally rather than intraoperatively. Traditional interventions range from conservative treatment to transcatheter arterial embolization (TAE) or thoracotomy. This approach suggests a potential stepwise method for managing suspected ICA injury that might reduce complications and minimize the need for invasive interventions. As a single case report representing hypothesis-generating evidence, this observation requires further validation through collaborative experience from other operators when similar circumstances arise. The case demonstrates an exploratory approach for managing ICA injury during PTNB, particularly relevant in resource-limited settings where interventional radiology services may not be immediately available.
1 Introduction
Increased lung cancer screening recommendations using low-dose CT have amplified demand for percutaneous transthoracic needle biopsy (PTNB). While PTNB is generally safe, intercostal artery (ICA) injury remains a rare but potentially severe complication (1, 2). Given the substantial volume of PTNB procedures performed annually, even rare complications may affect a substantial number of patients. This case describes an exploratory approach for detecting and managing ICA injury during PTNB using a coaxial needle system. The Institutional Review Board (IRB) waived ethical approval requirements for this retrospective case report.
2 Case report
2.1 Patient information
A 71-year-old male presented with worsening cough, sputum production, and chest pain for 3 days. His medical history included chronic cough and sputum production for over 10 years. He had no history of allergies or bleeding disorders. Laboratory tests showed an elevated squamous cell carcinoma antigen level of 17.3 (reference value <3), with other tumor markers within normal ranges. Due to the patient’s severe emphysema with multiple large bullae, pulmonary function tests were not performed to avoid potential pneumothorax risk. Clinical assessment suggested severe obstructive ventilatory dysfunction.
2.2 Clinical findings and pre-procedure planning
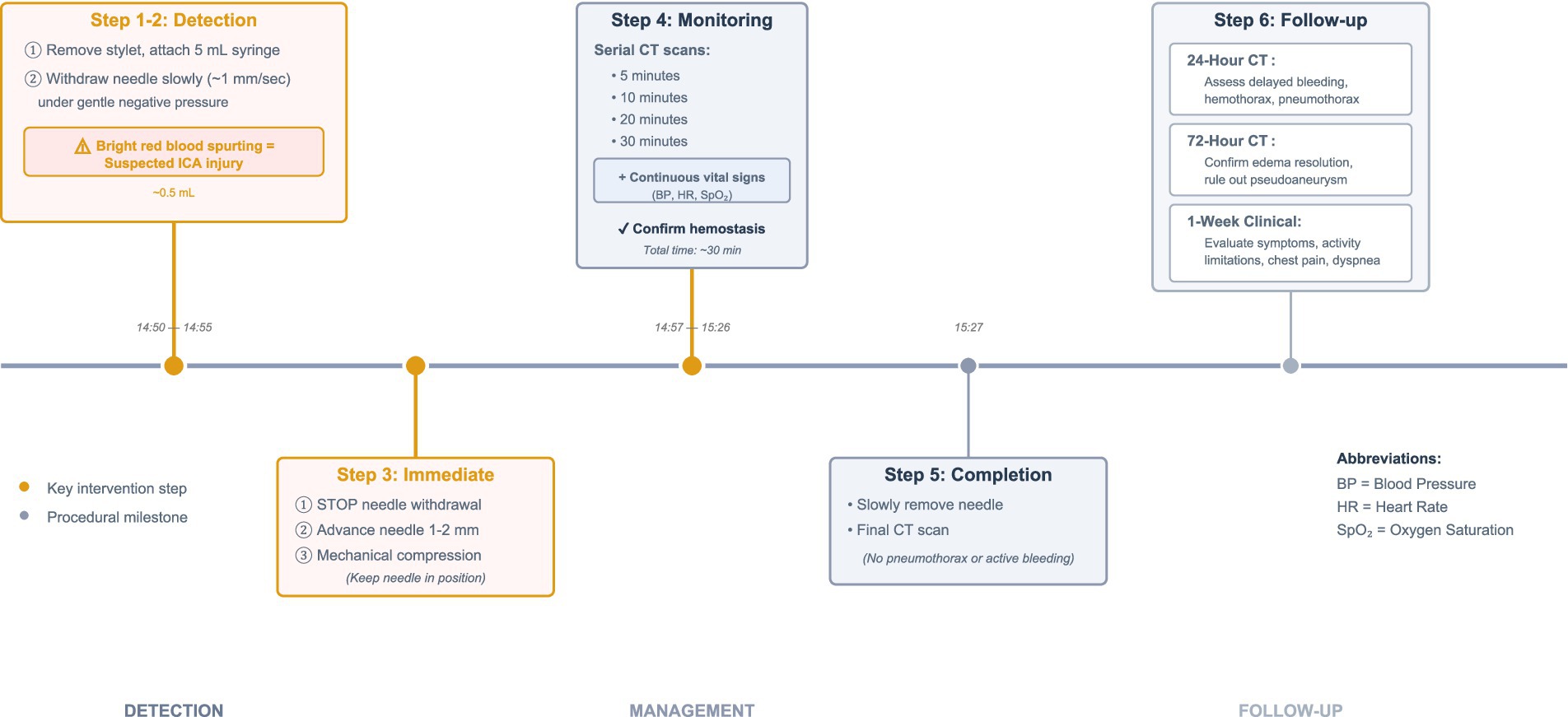
Initial contrast-enhanced chest CT revealed an oval soft tissue density mass in the right lower lobe adjacent to the spine. The scan also demonstrated severe emphysema with multiple bullae in both lungs. Notably, an ICA was observed coursing along the posterior margin of the mass (Figures 1A,B).
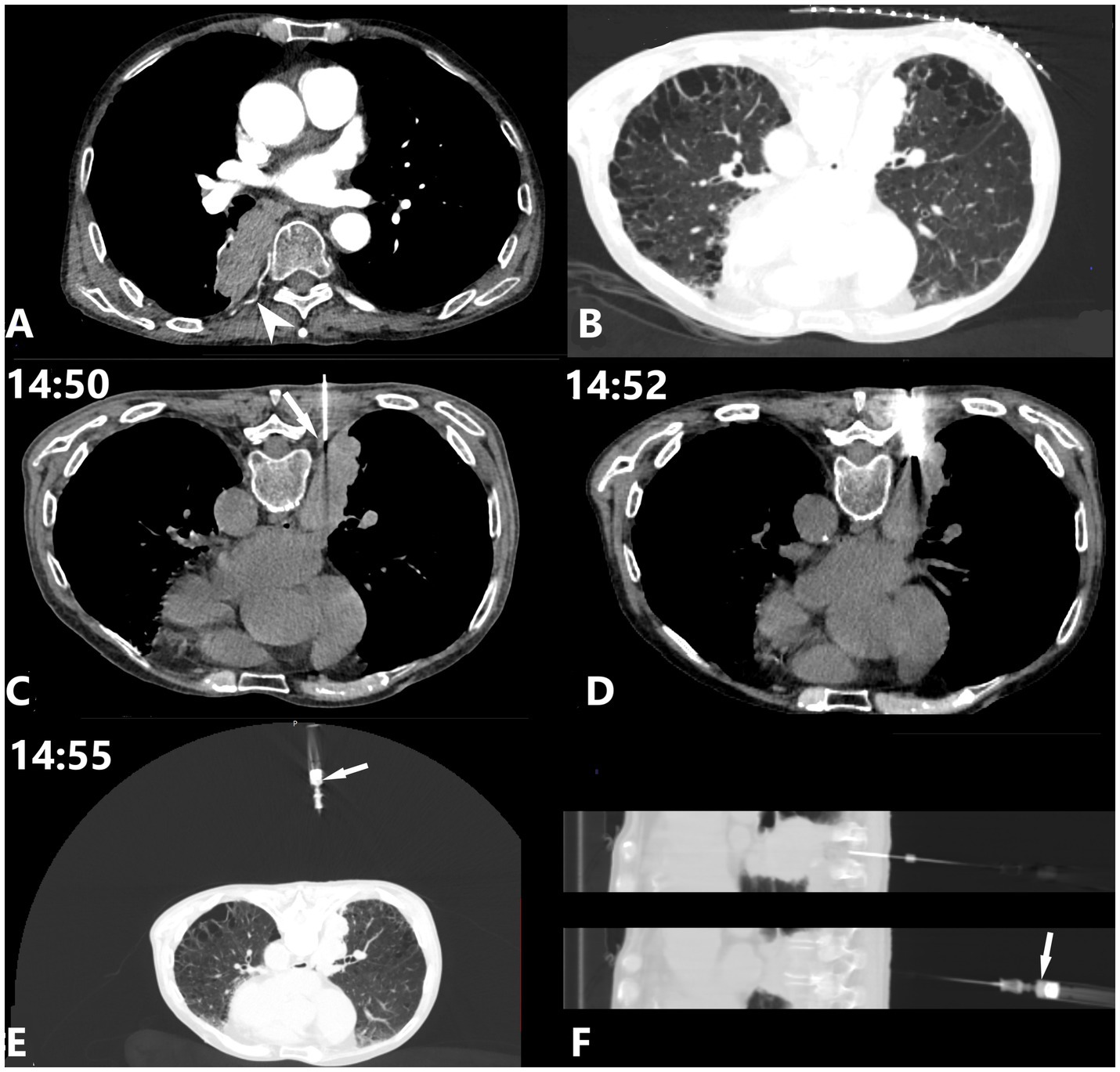
Figure 1. A 71-year-old male with a 10+ year history of recurrent cough and sputum production was admitted due to worsening symptoms and chest pain for 3 days. (A,B) Chest CT scan demonstrates emphysema with multiple bullae in both lungs, and an oval soft tissue density mass (approximately 3.0 × 6.0 cm) in the right lower lobe adjacent to the spine. An ICA (white arrowhead) courses along the posterior margin of the right lung mass. (C) To minimize the risk of pneumothorax, the puncture path was planned to avoid areas of emphysema and lung bullae. The coaxial puncture needle reaches the extrapleural pleura, with its medial edge adjacent to the origin segment of the ICA (white arrow). (D) Four tissue samples were obtained, each measuring 2.2 cm in length. (E,F) Bright red blood rapidly spurted into the 5 mL syringe (white arrow), with an approximate volume of 0.5 mL.
This case presented a challenging clinical decision due to competing risk factors: severe emphysema with multiple bullae increasing pneumothorax risk, and proximity of the target lesion to a large-caliber proximal ICA. Considering the patient’s poor pulmonary function and the relatively low reported incidence of ICA injury, the intervention team chose a posterior approach near the spine, bypassing the emphysematous areas while maintaining increased vigilance throughout the procedure.
2.3 Procedure description
CT-guided PTNB was performed using an 18G coaxial needle system (Monopty 1816B Bard, USA) with the patient in prone position under local anesthesia with 1% lidocaine. Initial CT scan showed the coaxial needle reaching the extrapleural space. At this point, 1 mL of 1% lidocaine was administered for local anesthesia to minimize pleural reaction during subsequent transpleural advancement. A large ICA origin segment was observed at the medial edge of the needle path (Figure 1C). The needle then reached the target mass, and four 2.2-cm-long pathological specimens were obtained (Figure 1D).
After specimen collection, needle withdrawal began. Given the proximity to the spine where the ICA is typically larger at its origin, and considering the CT image findings, the operator maintained increased vigilance for potential ICA injury. The stylet was removed, and a 5 mL syringe was attached. During slow withdrawal (approximately 1 mm/s) with slight negative pressure, 0.5 mL of bright red blood rapidly spurted into the syringe, consistent with ICA injury (Figures 1E,F).
2.4 Management steps
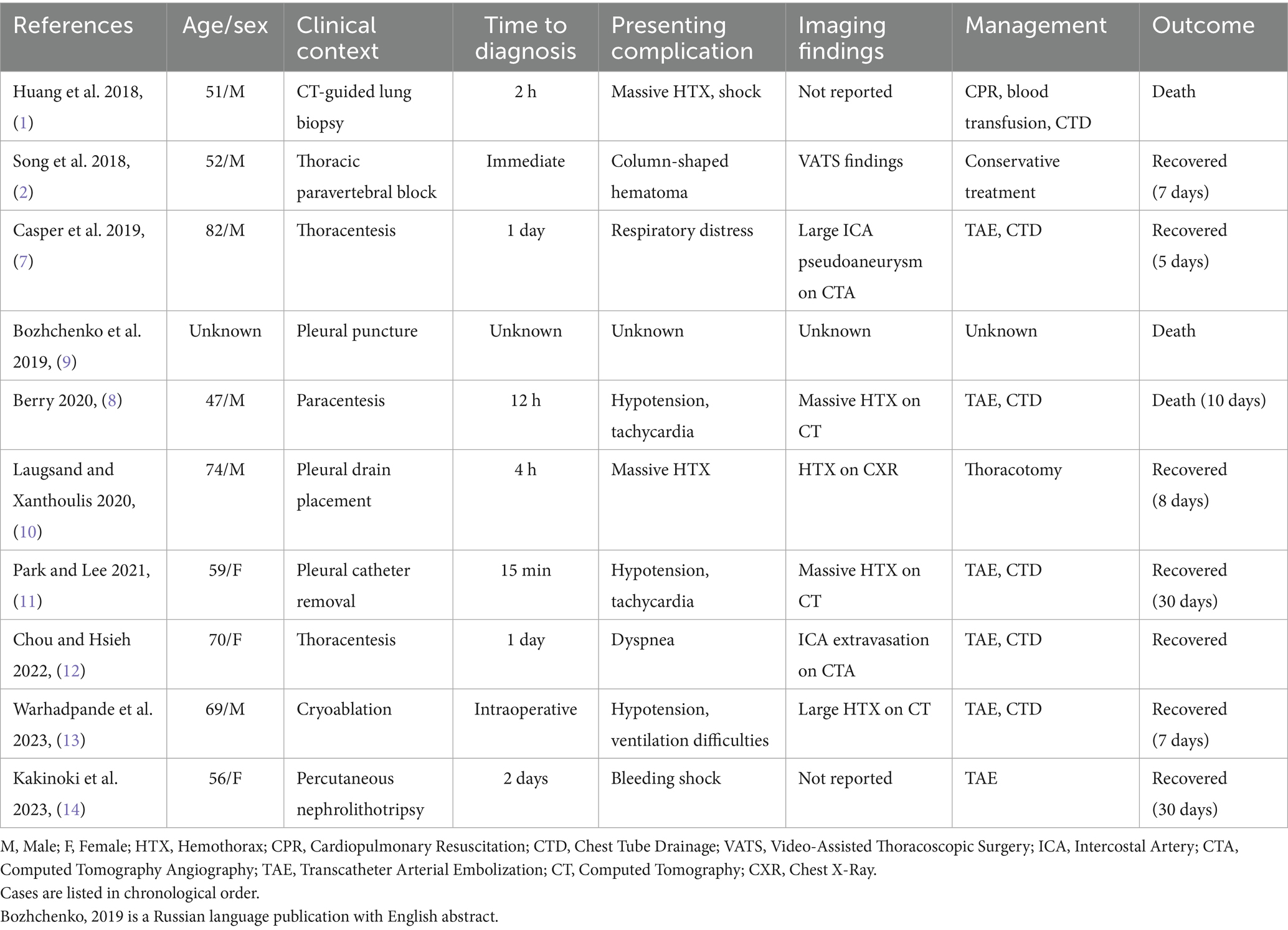
The following management steps were undertaken (Figures 2A–D): (1) Immediate cessation of needle withdrawal and slight advancement of the coaxial needle by 1–2 mm. No additional blood was aspirated, and subsequent CT scan showed no visible hematoma or hemothorax; (2) Serial CT monitoring at regular intervals. The final scan showed no evidence of active bleeding after complete needle withdrawal and no pneumothorax.
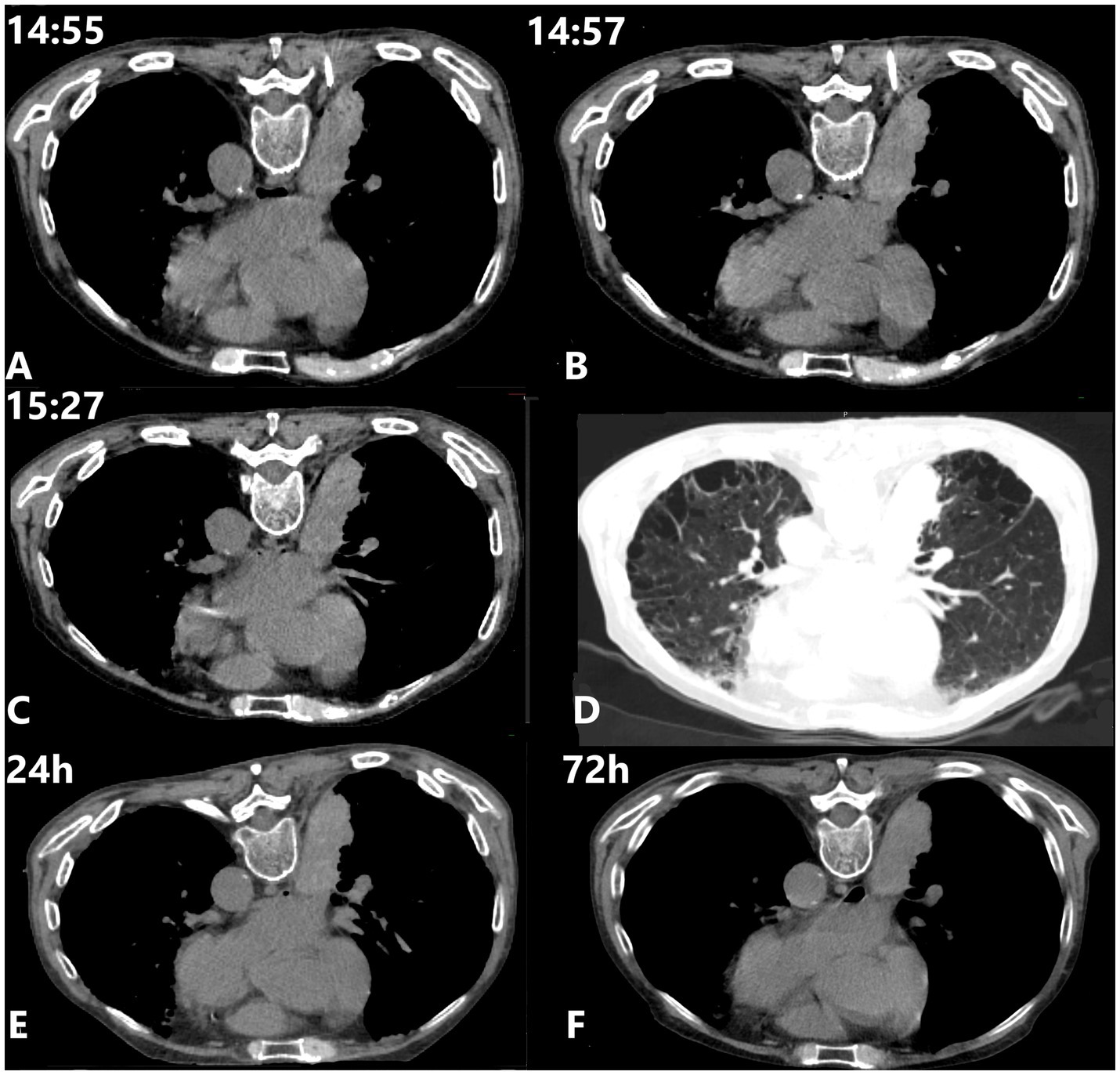
Figure 2. Intervention and evaluation. (A) Mechanical hemostasis was initiated. No visible hematoma or hemothorax was observed. The 5 mL syringe attached to the needle hub caused a slight tilt in the puncture needle. (B) No apparent signs of active bleeding were visible. (C,D) Following complete needle withdrawal, no apparent signs of active bleeding or pneumothorax were observed. (E,F) Follow-up CT scan images obtained at 24 and 72 h post-procedure.
2.5 Follow-up and outcomes
Throughout the procedure, vital signs remained stable, and the patient reported no discomfort. CT scans performed during the hemostasis process revealed slight edema and thickening of the soft tissue surrounding the injured ICA compared to the contralateral side, with no progressive worsening or signs of active bleeding. Follow-up CT scans at 24 and 72 h post-procedure showed no evidence of pneumothorax or new hemorrhage, with gradual resolution of mild local soft tissue edema (Figures 2E,F). The procedural timeline and management sequence are summarized in Figure 3.
Pathological examination confirmed well-differentiated squamous cell carcinoma (Figure 4). The patient subsequently initiated appropriate treatment. During the week-long follow-up period, the patient reported no biopsy-related pain, activity limitations, or complications.
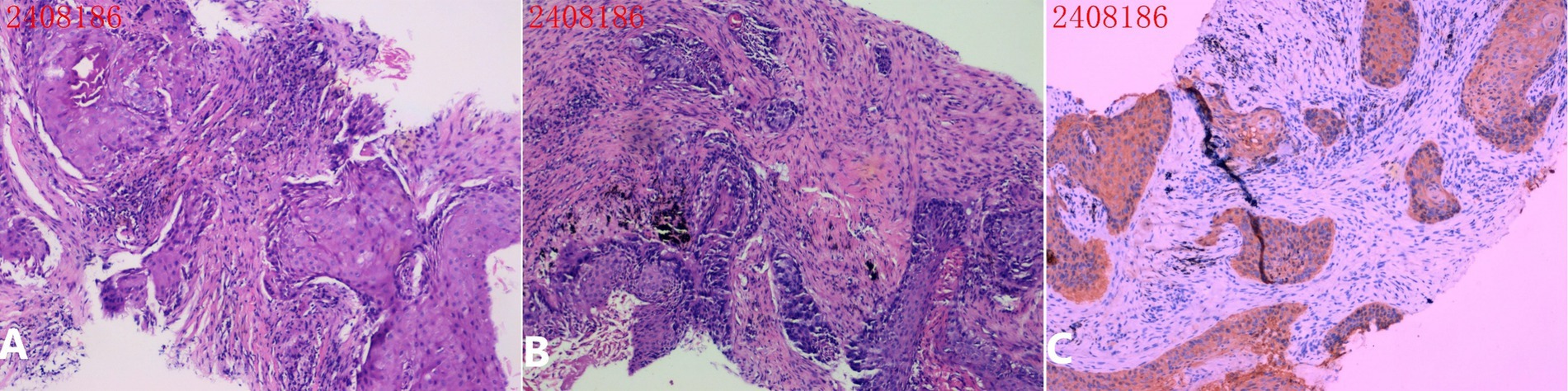
Figure 4. Pathological examination. (A,B) H&E stained pathological section: The biopsy tissue shows chronic inflammation with multiple squamous cell nests, accompanied by keratinization and incomplete keratinization. Mitotic figures are rare, and the cells appear well-differentiated. (C) Immunohistochemistry results: CK7 (−), TTF-1 (−), NapsinA (−), p63 (+), CK5/6 (2+), P40 (+), Ki-67 (3+, 20%).
3 Literature review
A systematic review of literature from 2018 to 2024 was conducted using PubMed database. Search terms included “intercostal artery injury,” “intercostal artery pseudoaneurysm,” and “hemothorax biopsy lung.” Studies reporting iatrogenic ICA injuries in thoracoabdominal procedures and hemothorax complications in PTNB were included.
3.1 Current management and outcomes
Literature review findings (Tables 1, 2) revealed varying management approaches for ICA injuries based on their severity. Detection timing typically ranges from intraoperative discovery to early postoperative periods, not exceeding 24 h post-procedure. Among the reviewed cases, the mortality rate was 30% (3/10), with deaths occurring between the day of injury and up to 10 days later. For surviving patients, recovery periods varied from 5 to 30 days. Currently, most ICA injuries are detected after rather than during the procedure. Management strategies depend on severity: mild cases presenting with hemothorax or local hematoma typically receive conservative treatment, while progressive or severe hemothorax may require more invasive interventions such as transcatheter arterial embolization (TAE), chest tube drainage, blood transfusion, or even thoracotomy. The consensus among reviewed studies emphasizes maintaining high suspicion for ICA injury and considering early intervention to reduce morbidity and mortality, though potential reporting bias may lead to overrepresentation of severe cases.
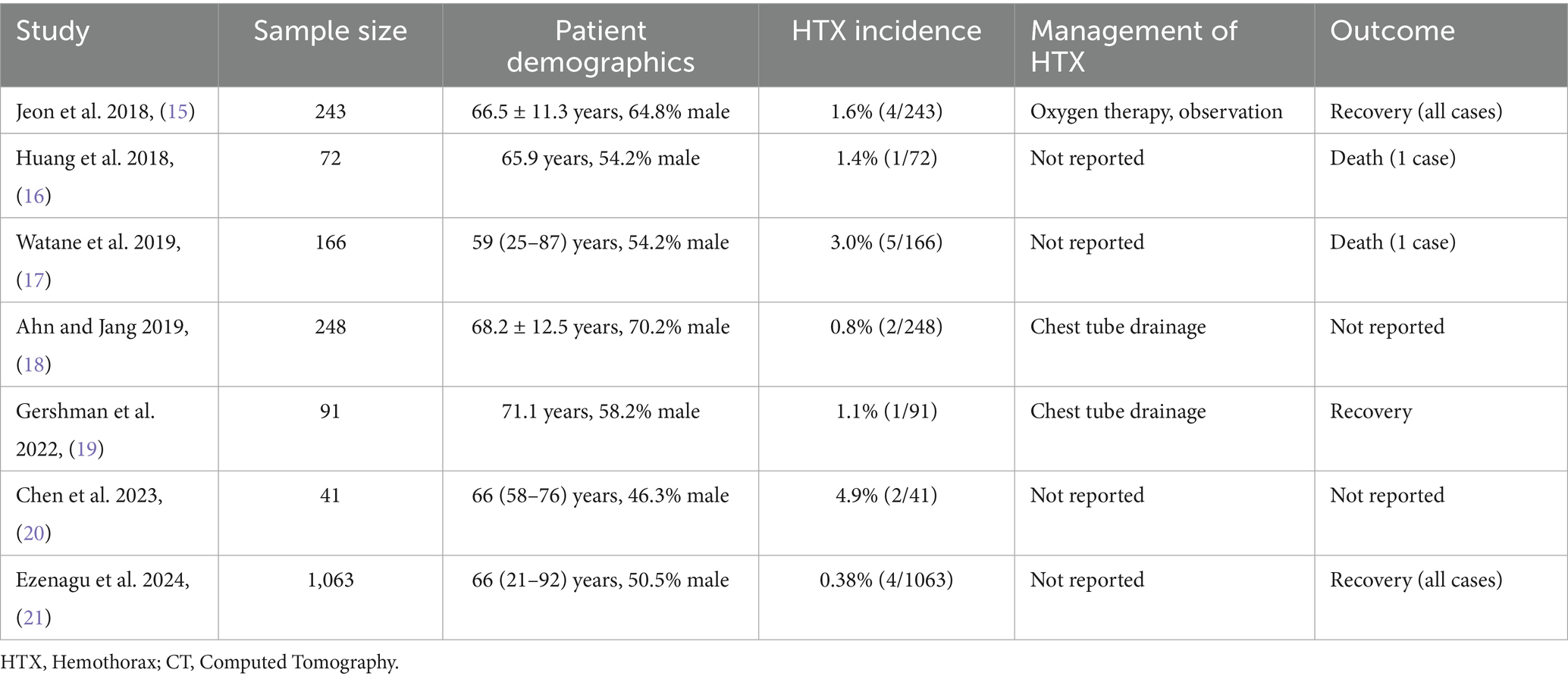
Table 2. Incidence and management of hemothorax in CT-guided PTNB: a review of original research (2018–2024) (15–21).
4 Discussion
This improvised intraoperative management decision was formulated based on two factors: (1) preoperative imaging demonstrating ICA proximity and intraoperative CT findings suggesting potential complications, and (2) adaptation of detection techniques from CT-guided percutaneous transhepatic biliary drainage, extended to include therapeutic needle repositioning for hemostasis. In biliary procedures, when a coaxial needle inadvertently penetrates through the bile duct wall, the established protocol involves removing the stylet, attaching a 5 mL syringe to the needle hub, and slowly withdrawing the needle under slight negative pressure. Bile aspiration confirms when the needlepoint is within the duct, thus facilitating subsequent guidewire insertion. This diagnostic approach parallels established clinical practice protocols, where indirect procedural evidence guides decision-making. A comparable example is the routine use of pre-injection aspiration to prevent inadvertent intravascular lidocaine administration and its associated adverse effects—a standard safety measure based on aspiration results rather than direct vascular visualization. The coaxial needle appeared to provide dual hemostatic functions: (1) mechanical compression of the injured vessel, promoting vasoconstriction and thrombus formation, and (2) coagulation stimulation through foreign body-induced platelet aggregation and fibrin formation (3, 4).
Recent studies report hemothorax incidence rates ranging from 0.38 to 4.9%, higher than earlier reported rates (5). In 2019, Tamburini et al. reported that among 30 cases of ICA injuries managed with TAE at two institutions over 16 months, iatrogenic injuries accounted for 37% (11/30) (6). When faced with ICA injury during PTNB, outcomes can vary widely, ranging from patient recovery with conservative treatment to rapid deterioration and death (1, 7, 8). This case suggests a potential stepwise approach for managing suspected ICA injury that might reduce treatment time and minimize complications while decreasing the need for more invasive interventions. In resource-limited settings where interventional radiology services may not be immediately available, having alternative management options could be valuable.
Several important limitations must be acknowledged. The diagnosis of ICA injury was based primarily on clinical observation and imaging findings, without angiographic confirmation. Additionally, as a single case report representing the lowest level of clinical evidence, this observation should be considered hypothesis-generating and requires further validation. Given that the rarity of this complication limits opportunities for single-center validation, publication of this case report serves to enable other operators to evaluate this approach when similar circumstances arise, thereby facilitating the necessary collaborative validation. The applicability of this method may be influenced by various factors, including vessel size, injury severity, and operator experience in detecting and responding to injury signs.
4.1 Patient perspective
The patient expressed satisfaction with the procedure and appreciated the prompt management of the complication. He reported minimal discomfort during and after the procedure, and was particularly relieved to have avoided both pneumothorax and additional invasive interventions such as chest tube placement.
5 Conclusion
This case describes a cautious approach for managing suspected ICA injury during PTNB that may serve as one potential management option for consideration in similar high-risk scenarios.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Patient clinical data is protected under medical privacy regulations and institutional policies. Raw clinical data cannot be shared publicly due to patient confidentiality requirements. The literature review data are publicly available through the cited references. Summary data and analysis results are presented within the manuscript tables and text. Requests to access these datasets should be directed to Hao Zhang, cGx1dG95ZV83QGhvdG1haWwuY29t.
Ethics statement
The studies involving humans were approved by The Institutional Review Board of Dianjiang People’s Hospital of Chongqing. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant for the publication of this case report.
Author contributions
HZ: Writing – original draft, Writing – review & editing. LL: Methodology, Project administration, Writing – review & editing. DL: Investigation, Supervision, Writing – review & editing. JX: Methodology, Writing – review & editing. HL: Visualization, Writing – review & editing. XL: Investigation, Writing – review & editing. CZ: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the Chongqing medical scientific research project (Joint project of Chongqing Health Commission and Science and Technology Bureau) (grant number 2025MSXM166) and Dianjiang Science and Technology Bureau (grant number: djkjxm2024shmskjcxyw016).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Huang, WM, Lin, HC, Chen, CH, Chen, CW, Wang, CH, Huang, CY, et al. Massive hemothorax after computed tomography-guided lung tumor biopsy: an unusual but disastrous complication. Thorac Cancer. (2018) 9:892–6. doi: 10.1111/1759-7714.12769
2. Song, L, Zhou, Y, and Huang, D. Inadvertent posterior intercostal artery puncture and haemorrhage after ultrasound-guided thoracic paravertebral block: a case report. BMC Anesthesiol. (2018) 18:196. doi: 10.1186/s12871-018-0667-5
3. Kizhakkedathu, JN, and Conway, EM. Biomaterial and cellular implants: foreign surfaces where immunity and coagulation meet. Blood. (2022) 139:1987–98. doi: 10.1182/blood.2020007209
4. Al-Amer, OM. The role of thrombin in haemostasis. Blood Coagul Fibrinolysis. (2022) 33:145–8. doi: 10.1097/MBC.0000000000001130
5. Tomiyama, N, Yasuhara, Y, Nakajima, Y, Adachi, S, Arai, Y, Kusumoto, M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. (2006) 59:60–4. doi: 10.1016/j.ejrad.2006.02.001
6. Tamburini, N, Carriel, N, Cavallesco, G, Molins, L, Galeotti, R, Guzmán, R, et al. Technical results, clinical efficacy and predictors of outcome of intercostal arteries embolization for hemothorax: a two-institutions' experience. J Thorac Dis. (2019) 11:4693–9. doi: 10.21037/jtd.2019.10.27
7. Casper, KP, Sanchirico, PJ, and Pfeiffer, DC. Intercostal artery pseudoaneurysm following thoracentesis: multi-modal imaging and treatment. BMC Med Imaging. (2019) 19:31. doi: 10.1186/s12880-019-0333-5
8. Berry, AC. Hemorrhagic complications of paracentesis: aberrant anatomy versus aberrant technique. Cureus. (2020) 12:e8827. doi: 10.7759/cureus.8827
9. Bozhchenko, AP, Tolmachev, IA, and Belykh, AN. Nastuplenie letal'nogo iskhoda vsledstvie iatrogennogo povrezhdeniia vetvi mezhrebernoĭ arterii pri provedenii plevral'noĭ punktsii [occurrence of a lethal outcome due to iatrogenic damage of an intercostal vessel during a pleural puncture procedure]. Sud-Med Ekspert. (2019) 62:58–62. doi: 10.17116/sudmed20196206158
10. Laugsand, EA, and Xanthoulis, A. Management of a life-threatening intercostal artery bleeding, difficult to visualize in open surgery: a case report. J Surg Case Rep. (2020) 2020:rjaa444. doi: 10.1093/jscr/rjaa444
11. Park, C, and Lee, J. Massive hemothorax due to intercostal arterial bleeding after percutaneous catheter removal in a multiple-trauma patient: a case report. World J Clin Cases. (2021) 9:9942–7. doi: 10.12998/wjcc.v9.i32.9942
12. Chou, CH, and Hsieh, HJ. Haemothorax due to intercostal artery injury after thoracentesis. Respirol Case Rep. (2022) 10:e0950. Published 2022 Apr 15. doi: 10.1002/rcr2.950
13. Warhadpande, S, Liles, A, and Kirkpatrick, D. Intercostal artery laceration after adrenal mass cryoablation. Semin Intervent Radiol. (2023) 40:286–9. doi: 10.1055/s-0043-1769766
14. Kakinoki, H, Yamaguchi, Y, Yukimoto, M, Kakinoki, Y, Udo, K, Tobu, S, et al. A case of bleeding shock induced by injury of the intercostal artery following percutaneous nephrolithotripsy. IJU Case Rep. (2023) 7:18–21. doi: 10.1002/iju5.12657
15. Jeon, MC, Kim, JO, Jung, SS, Park, HS, Lee, JE, Moon, JY, et al. CT-guided percutaneous transthoracic needle biopsy using the additional laser guidance system by a pulmonologist with 2 years of experience in CT-guided percutaneous transthoracic needle biopsy. Tuberc Respir Dis (Seoul). (2018) 81:330–8. doi: 10.4046/trd.2017.0123
16. Huang, WM, Chen, CH, Liang, SH, Huang, CY, Cheng, SM, Sheu, CY, et al. Multiplanar reconstruction technique for difficult computed tomography-guided lung biopsy: improved accuracy and safety. Thorac Cancer. (2018) 9:1333–7. doi: 10.1111/1759-7714.12835
17. Watane, GV, Hammer, MM, and Barile, MF. CT-guided Core-needle biopsy of the lung is safe and more effective than fine-needle aspiration biopsy in patients with hematologic malignancies. Radiol Cardiothorac Imaging. (2019) 1:e180030. doi: 10.1148/ryct.2019180030
18. Ahn, JH, and Jang, JG. Initial experience in CT-guided percutaneous transthoracic needle biopsy of lung lesions performed by a pulmonologist. J Clin Med. (2019) 8:8. doi: 10.3390/jcm8060821
19. Gershman, E, Vaynshteyn, I, Freidkin, L, Pertzov, B, Rosengarten, D, and Kramer, MR. Marked safety and high diagnostic yield of freehand ultrasound-guided core-needle biopsies performed by pulmonologists. Thorac Cancer. (2022) 13:1577–82. doi: 10.1111/1759-7714.14413
20. Chen, LC, Yang, SM, Malwade, S, Chang, HC, Chang, LK, Chung, WY, et al. Cone-beam computed-tomography-derived augmented fluoroscopy-guided biopsy for peripheral pulmonary nodules in a hybrid operating room: a case series. Diagnostics (Basel). (2023) 13:1055. Published 2023 Mar 10. doi: 10.3390/diagnostics13061055
Keywords: intercostal artery injury, percutaneous transthoracic needle biopsy, coaxial needle, hemostasis, case report
Citation: Zhang H, Li L, Lan D, Xu J, Leng H, Liao X and Zhang C (2025) A cautious approach for detecting and managing intercostal artery injury during CT-guided lung biopsy: a case report and literature review. Front. Med. 12:1709713. doi: 10.3389/fmed.2025.1709713
Edited by:
Giuseppe Fiorentino, Colli Hospital, ItalyReviewed by:
Yang Jiao, Second Military Medical University, ChinaTin Nadarević, Clinical Hospital Centre Rijeka, Croatia
Copyright © 2025 Zhang, Li, Lan, Xu, Leng, Liao and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Zhang, cGx1dG95ZV83QGhvdG1haWwuY29t; Chi Zhang, Y2hpemhhbmcyMDA3QGhvdG1haWwuY29t
 Hao Zhang
Hao Zhang Lin Li2
Lin Li2