- 1Corewell Health William Beaumont University Hospital Eye Institute, Corewell Health, Royal Oak, MI, United States
- 2Department of Ophthalmology, New York University (NYU) Langone Health, New York, NY, United States
- 3Kahana Oculoplastic and Orbital Surgery, Livonia, MI, United States
Orbital arteriovenous fistulas are exceedingly rare and present a unique challenge due to difficulties with access. We report a case of a patient with an acute progressive direct orbital arteriovenous fistula causing orbital compartment syndrome and compressive optic neuropathy. He underwent medial orbital decompression followed immediately by direct cannulation of the vascular anomaly, through which two separate fistulas were embolized under fluoroscopic guidance.
Introduction
Orbital arteriovenous fistulas are rare, high-flow vascular malformations characterized by a direct connection between the ophthalmic artery and one of the draining ophthalmic veins. They may arise spontaneously or in association with trauma (1). They are distinguished from orbital arteriovenous malformations by the lack of a central nidus (2). Given the rarity of this entity and the limited number of case reports published on its management, no standard treatment approach has been established. Herein, we review the literature and present a case of a rapidly progressive orbital arteriovenous fistula causing compressive optic neuropathy that was successfully treated with medial orbital decompression followed immediately by direct-access embolization of multiple independent fistula tracks using intraoperative catheter repositioning. The collection and evaluation of protected patient health information were Health Insurance Portability and Accountability Act (HIPAA)-compliant and adhered to the tenets of the Declaration of Helsinki.
Case presentation
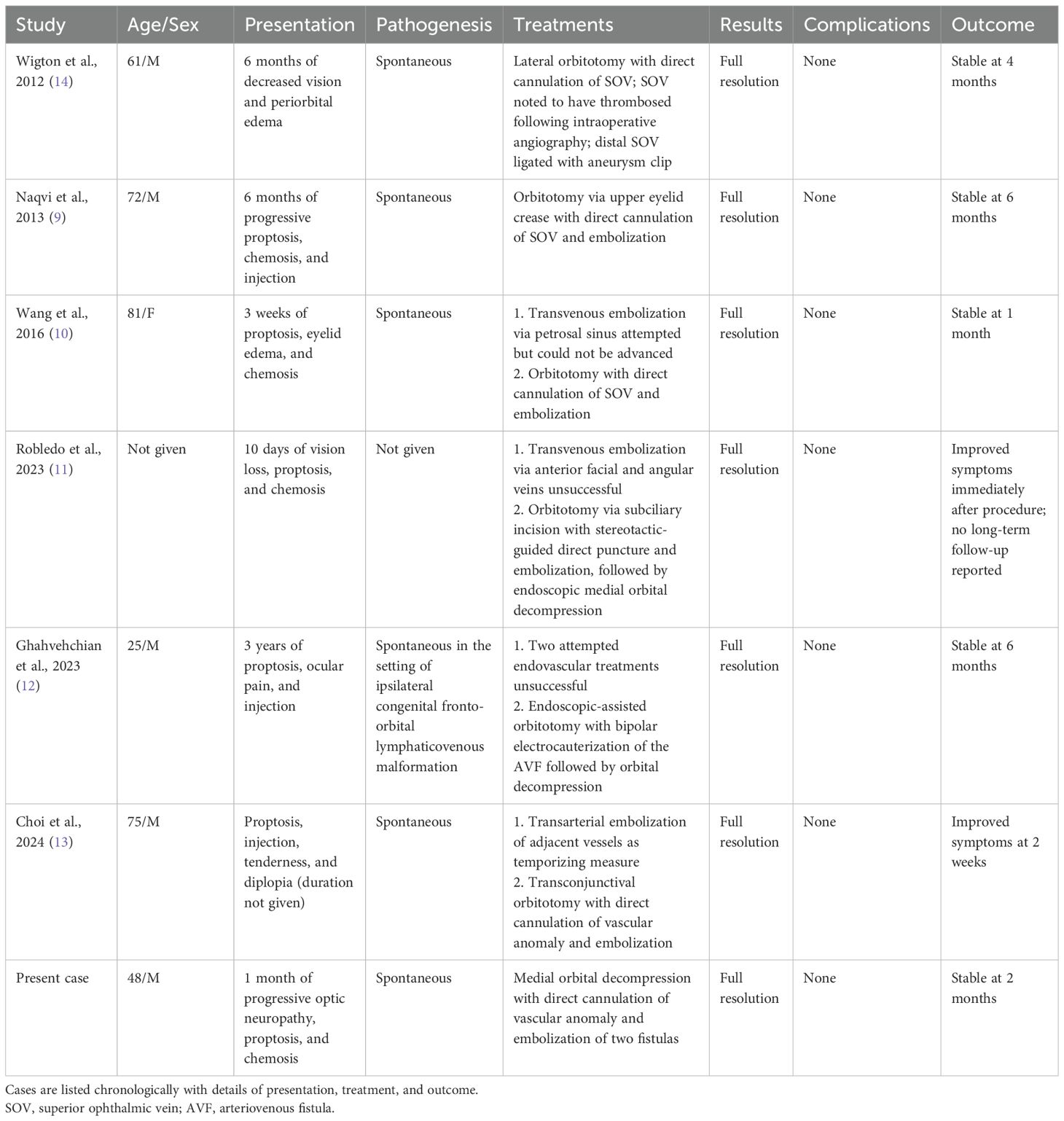
A 48-year-old man presented with 1 month of blurry vision in the left eye without a history of trauma. His past medical history was significant for thyroid cancer in remission and hypothyroidism. On presentation to outside ophthalmology, he was noted to have left optic neuropathy with decreased vision (20/100), poor color vision, relative afferent pupillary defect, restricted extraocular motility, chemosis, eyelid edema, and elevated intraocular pressure. He had 5 mm of left-sided relative proptosis on Hertel exophthalmometry. Imaging, both CT and MRI, was initially read as a varix (Figure 1). He was treated for possible orbital cellulitis and possible thyroid eye disease with intravenous antibiotics and intravenous methylprednisolone, respectively, with no improvement. His proptosis and visual function worsened rapidly (Figure 2), and he was referred to our practice. Reassessment of his imaging raised doubts regarding the diagnosis, and an urgent angiogram was recommended. He was admitted, and six-vessel angiography demonstrated a left orbital arteriovenous fistula fed by three direct branches of the left ophthalmic artery with drainage to the superior ophthalmic vein (SOV) and no communication with the cavernous sinus (Figures 3, 4). MRI of the brain and orbits, and magnetic resonance angiography (MRA) and magnetic resonance venography (MRV) of the brain, demonstrated no evidence of vessel thrombosis or any previous connection to the cavernous sinus or other vasculature. Given the origin of the feeding arterioles off the proximal ophthalmic artery, an arterial approach was deemed to be high risk. Since the venous component of the fistula did not communicate with the cavernous sinus, this approach was not possible. A transvenous approach through the facial vein was also considered, but the indirect access would have made it difficult to guarantee occlusion at the fistula site or sites.
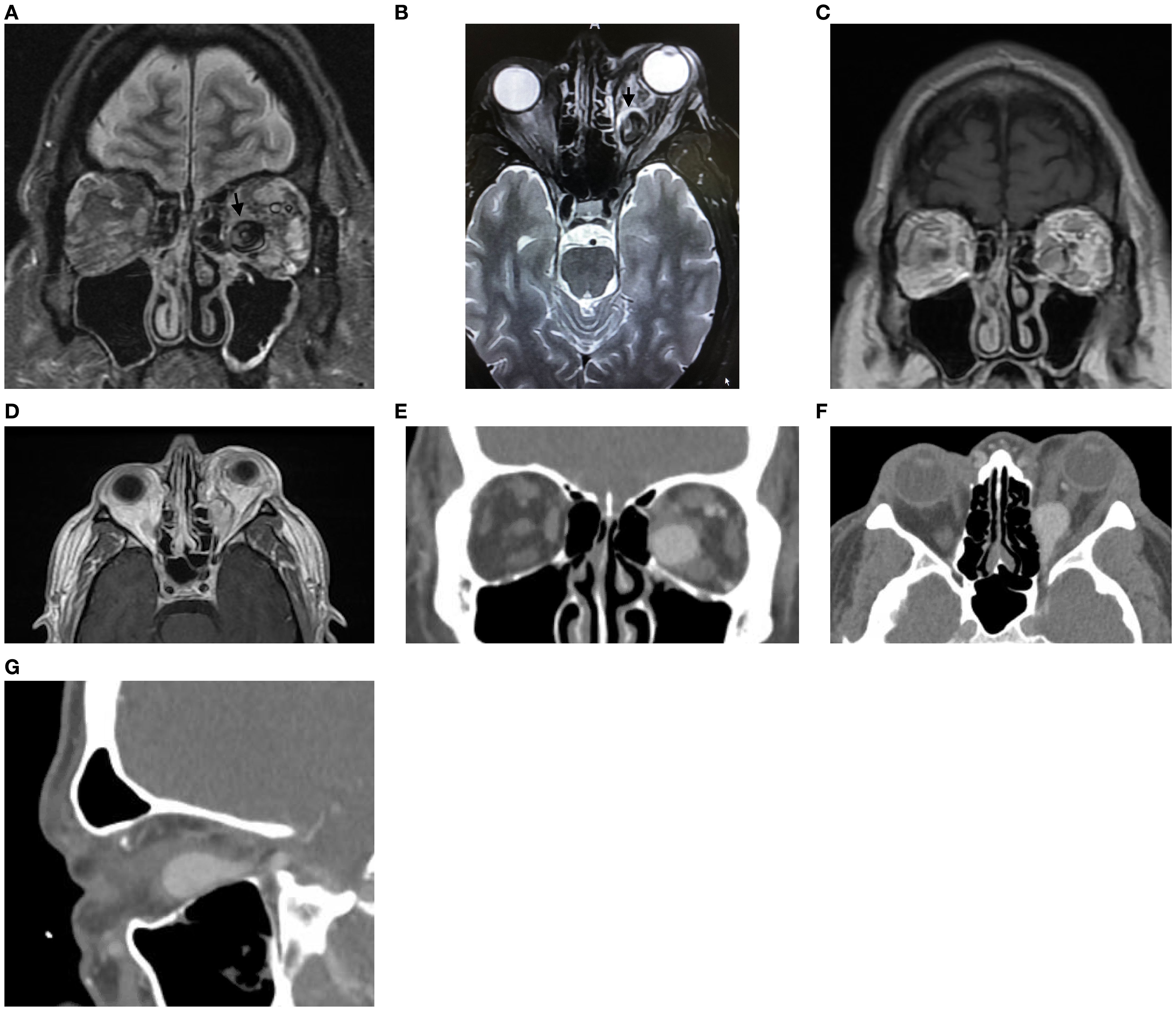
Figure 1. (A) Coronal transverse relaxation time short tau inversion recovery magnetic resonance image demonstrating a large venous aneurysm in the inferomedial left orbit. (B) Axial transverse relaxation time short tau inversion recovery magnetic resonance image demonstrating a dilated venous aneurysm in the posterior medial left orbit (arrow) with associated edema of the medial and lateral rectus muscles. (C, D) Longitudinal relaxation time post-gadolinium magnetic resonance coronal (C) and axial (D) images demonstrating enhancement of the venous aneurysm in the inferomedial left orbit. (E–G) Computed tomography angiography with intravenous contrast in coronal (E), axial (F), and sagittal (G) views demonstrating enhancement of the venous aneurysm, which extends to the orbital apex.

Figure 2. Pre-operative external photograph of the left eye demonstrating significant orbital congestion and chemosis. Photograph was taken on the day of intervention.
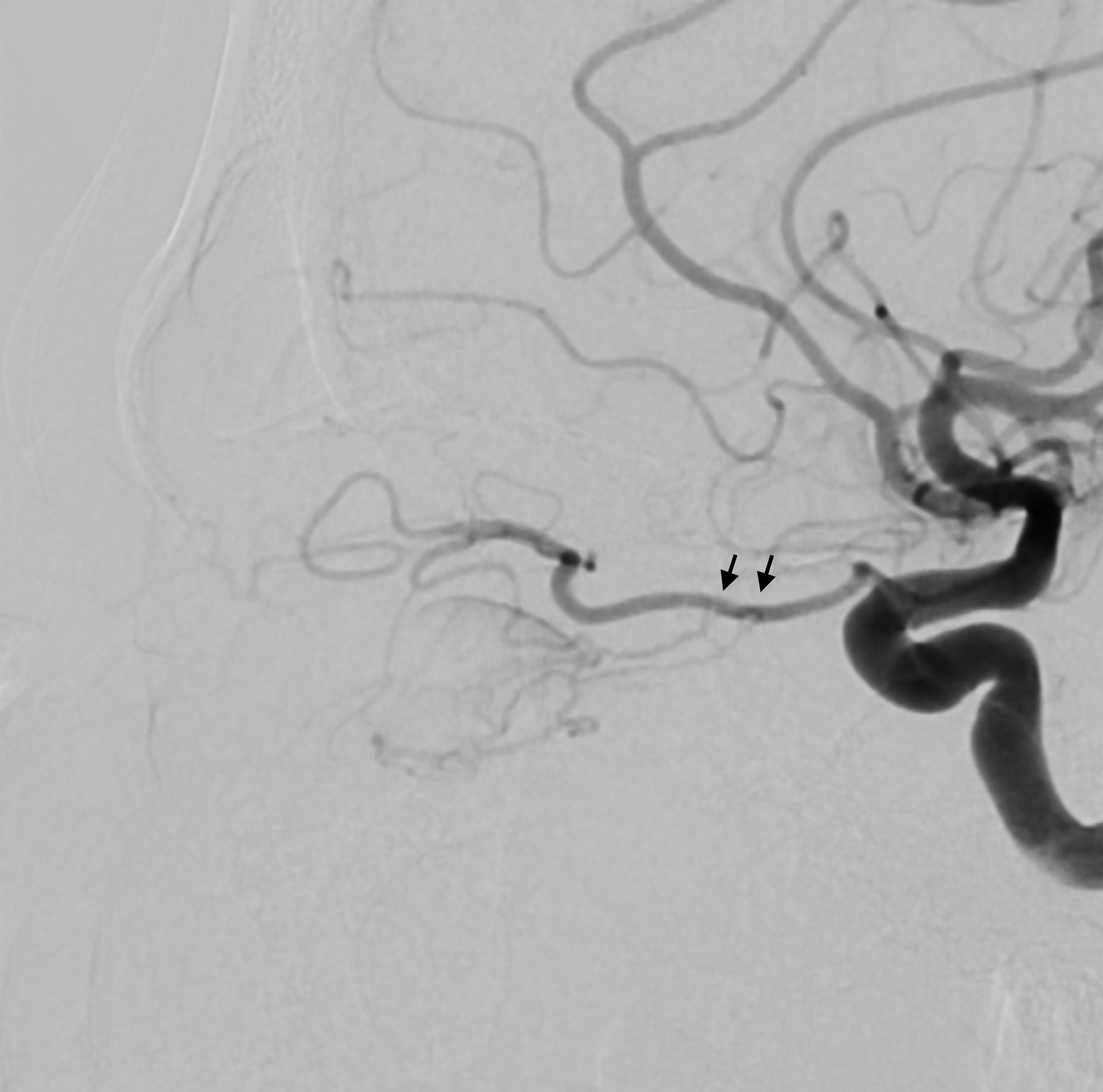
Figure 3. Lateral view of the angiogram after internal carotid artery injection demonstrating feeding arterioles off the proximal ophthalmic artery (arrows).
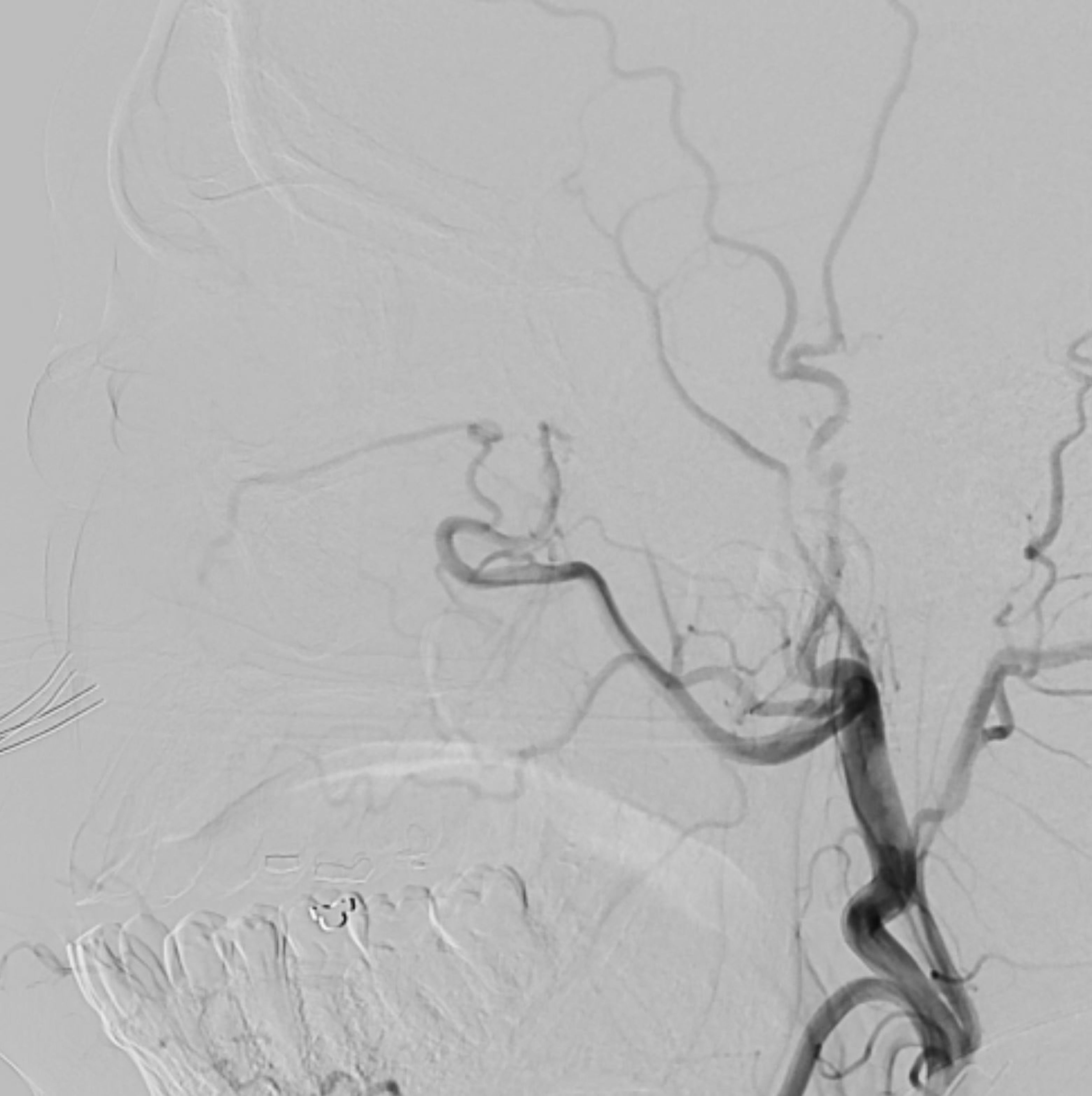
Figure 4. Lateral view of the angiogram after external carotid artery injection demonstrating no feeding of the venous aneurysm.
A multi-disciplinary surgical plan was developed. The patient underwent left medial orbital decompression to decompress the optic nerve, decongest the orbit, and provide access to the venous bulb of the fistula. This was followed immediately by cannulation of the venous anomaly in the operating room using a 5-French micropuncture sheath under direct intraoperative observation (Figure 5), followed by transfer to the fluoroscopy suite. With intraoperative angiography providing a “road map”, the venous outflow channel to the SOV was embolized with 20 coils, revealing a second outflow channel. The orbital catheter was manipulated and repositioned to access the second channel, which was then embolized with another 18 coils. At this point, the venous component was noted to have venous stasis (Figure 6), which would promote clotting followed by involution of the venous anomaly. The SOV was preserved and patent. Given the potential for a compartment syndrome, a lateral canthotomy and a cantholysis were performed preemptively to preserve normal intraocular and intraorbital pressure in the immediate post-operative period.
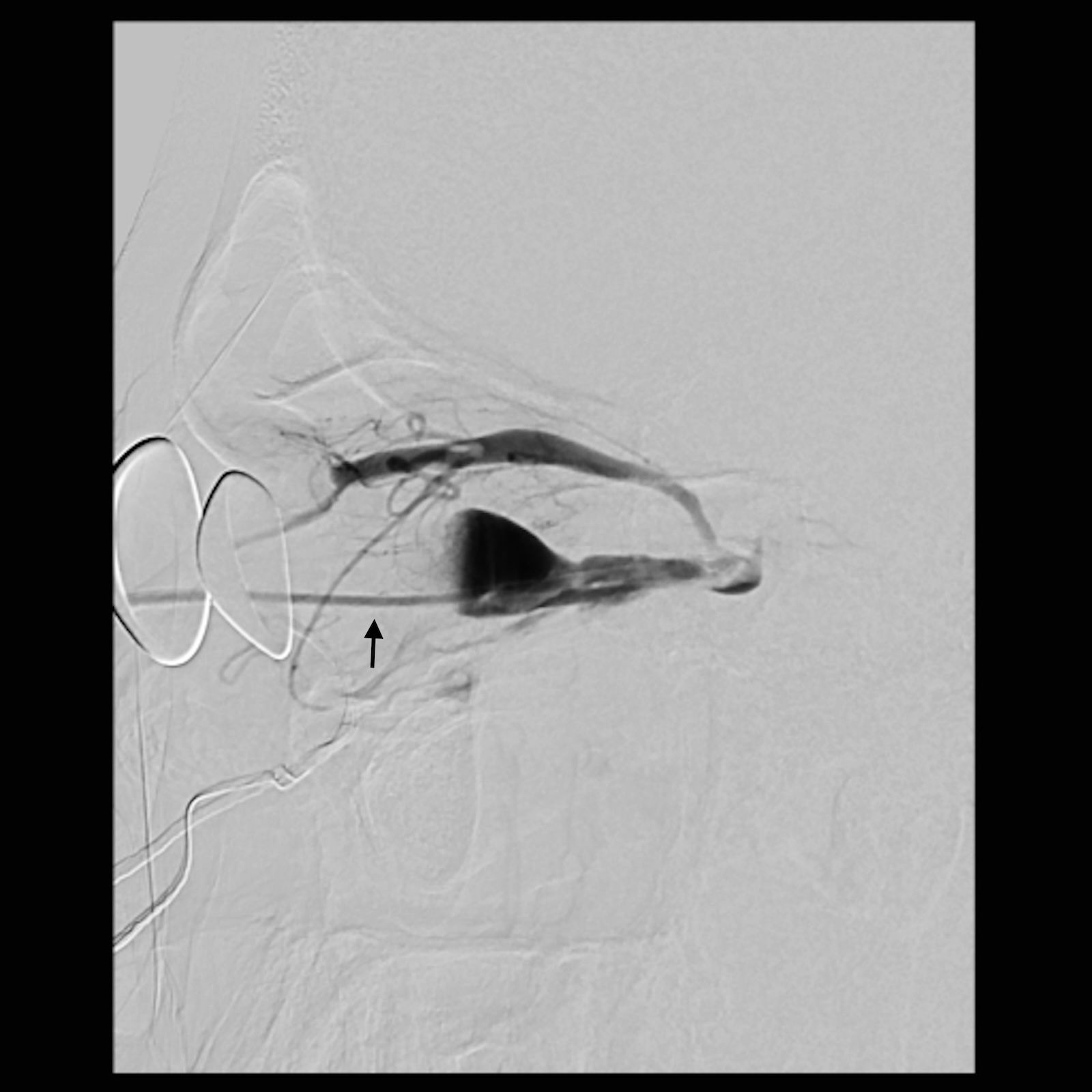
Figure 5. Lateral view of the angiogram demonstrating a percutaneously placed catheter (arrow) in the dilated venous aneurysm of the fistula. There is contrast outflow superficially without direct connection to the cavernous sinus.
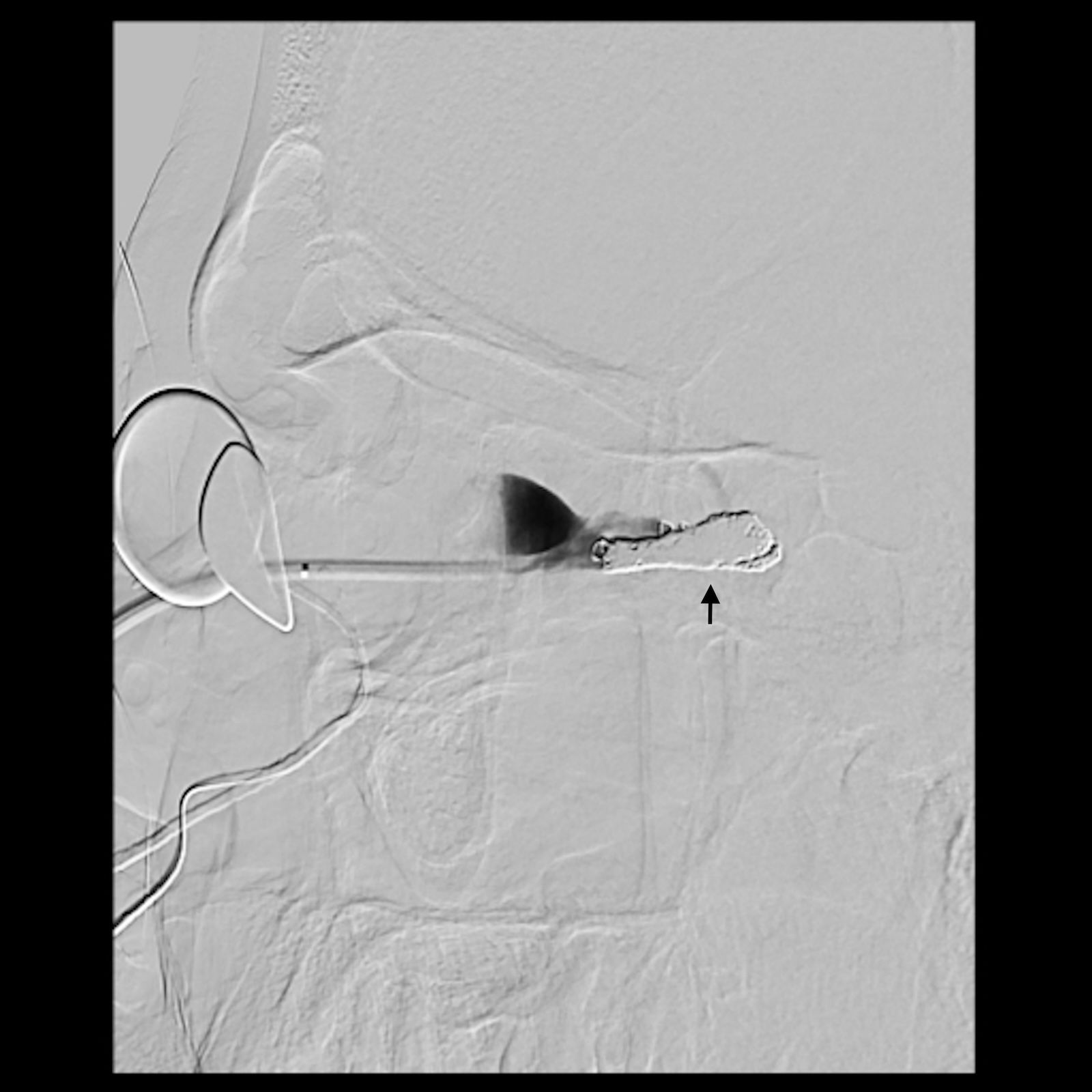
Figure 6. Lateral view of the angiogram after coiling of the venous outflow tracts of the fistula demonstrating complete occlusion of the outflow tracts. Arrow indicates location of coils.
The patient was admitted to the intensive care unit (ICU) for 24 hours and recovered well in the first few days following surgery. At 1 week post-operatively, he was found to have severe swelling and congestion of the orbit with more than 2 cm of proptosis and mild optic disc edema, but intraocular pressure was only mildly elevated to 24 mmHg. He was started on an oral prednisone taper. At 3 weeks post-operatively, he was recovering well with resolved disc edema, improved proptosis, visual acuity of 20/30, improved extraocular motility, and a trace afferent pupillary defect. At long-term follow-up, his visual acuity was restored with normal color vision, no afferent pupillary defect, and no proptosis.
Discussion
Orbital arteriovenous fistulas can cause vision-threatening compartment syndrome, leading to compressive optic neuropathy and ophthalmoplegia. Clinical presentation is characterized by signs and symptoms of orbital venous congestion and may mimic that of an orbital varix, carotid-cavernous fistula, orbital tumor, orbital cellulitis, or thyroid eye disease. The most commonly reported presenting symptoms include proptosis, chemosis, double vision, and vision loss (3). Definitive diagnosis is made by cerebral angiography, which is also essential for treatment planning (1, 4). The decision to obtain an angiogram requires a high level of suspicion and familiarity with the differential diagnosis. A team of neuro-radiologists and orbital specialists is key to achieving diagnostic accuracy.
Most recently, Pathuri et al. published a review of the literature on this subject, organized by treatment modality, and Krylova and Hauck published a review of the literature on this subject, including dural arteriovenous fistulas (2, 5). The authors performed a literature search of PubMed from 1978 to August 2025 for cases of pure intraorbital arteriovenous fistulas with documented intervention and outcome. Dural arteriovenous fistulas and arteriovenous malformations were excluded. Among 29 identified cases, including the present case, 14/29 (48%) were treated with transvenous embolization alone (2, 3, 6–8), 7/29 (24%) were treated with orbitotomy combined with direct fistula treatment (9–14), 4/29 (14%) were treated with craniotomy (15–18), and 4/29 (14%) were treated with transarterial embolization (18–21). Cases in which orbitotomy was performed are summarized in Table 1. In addition, we noted 18 reported cases of spontaneous resolution spanning a variety of etiologies (2, 18), although 5/18 (28%) cases had reported visual decline. Given the limited published experience with this rare entity, clear indications for observational management are yet to be defined.
With the advancement of endovascular techniques over the past two decades, transvenous embolization has become the preferred method of management, when possible (22). When transvenous embolization fails or is not anatomically possible, direct surgical exposure can allow an alternative venous access for embolization (2, 9–13, 17). Notably, orbital decompression combined with direct surgical access for the transvenous management of orbital arteriovenous fistula has been described in three previous cases with successful treatment outcomes (2, 11, 12).
In the present case, given the high-risk location of the three arterial feeding branches, the degree of orbital congestion and optic neuropathy, and the rapidity of progression, the surgical plan was designed for the best chances of safe, effective, and definitive management of the fistula combined with rapid relief of the compressive optic neuropathy. The surgical decompression of the orbital apex prior to embolization provided several benefits: 1) it reduced pressure on the optic nerve, 2) it improved venous outflow to reduce congestion, 3) it provided additional space for the surgical exploration of the arteriovenous fistula, and (4) it accounted for the anticipated increase in orbital inflammation and congestion following a surgical procedure and vessel embolization. Following the procedure, prophylactic lateral canthotomy and superior and inferior cantholysis were performed to further reduce the effects of post-operative congestion. One week after the procedure, the patient had particularly pronounced orbital edema that may have been similar to the phenomenon of “paradoxical worsening” observed to follow thrombosis or embolization of arteriovenous malformations contiguous with the cavernous sinus (23). The multidisciplinary approach adopted in this case resulted in rapid resolution of the compressive optic neuropathy and associated proptosis as well as the maintenance of safe intraocular pressures throughout the post-operative course, without complications. In certain cases, combining surgical decompression with endovascular embolization may provide the best chance of a good outcome in treating the rare direct orbital arteriovenous fistula.
Author contributions
OC: Writing – review & editing, Writing – original draft. SC: Writing – review & editing. JW: Writing – review & editing. AK: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yazici B, Yazici Z, Erdogan C, and Rootman J. Intraorbital arteriovenous fistula secondary to penetrating injury. Ophthalmic Plast Reconstr Surg. (2007) 23:275–8. doi: 10.1097/IOP.0b013e3180686e7e
2. Pathuri SC, Johnson WC, Russell KLP, Robledo A, Albuquerque FC, Kan P, et al. Treatment of intraorbital arteriovenous fistulas with direct puncture: a case series and review of treatments since 1978. J NeuroIntervent Surg. (2024) 16:1250–6. doi: 10.1136/jnis-2023-020967
3. Tsutsumi S, Oishi H, Nonaka S, Okura H, Suzuki T, Yasumoto Y, et al. Orbital arteriovenous fistula coexistent with an arteriovenous hemangioma: A rare occurrence and review of literature. World Neurosurg. (2019) 122:287–92. doi: 10.1016/j.wneu.2018.11.003
4. de Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit. (2003) 22:121–42. doi: 10.1076/orbi.22.2.121.14315
5. Krylova M and Hauck EF. Intraorbital arteriovenous fistulas: illustrative case. J Neurosurg Case Lessons. (2025) 9:CASE24857. doi: 10.3171/CASE24857
6. Hirano Y, Ono H, Shojima M, Abe M, Tanishima T, Tamura A, et al. Orbital arteriovenous fistula causing only visual impairment due to compression of the optic nerve by the dilated superior ophthalmic vein. Asian J Neurosurg. (2023) 18:679–83. doi: 10.1055/s-0043-1771322
7. Vaithialingam B, Gopal S, and Sohrab M. Catheter embolization of an orbital arteriovenous fistula in a patient with wyburn-mason syndrome. Cureus. (2023) 15:e36949. doi: 10.7759/cureus.36949
8. Péchiné C, Agard E, and Holay Q. Pure intraorbital arteriovenous fistula. Am J Ophthalmol. (2025) 271::e1. doi: 10.1016/j.ajo.2024.10.020
9. Naqvi J, Laitt R, Leatherbarrow B, and Herwadkar A. A case of a spontaneous intraorbital arteriovenous fistula: clinico-radiological findings and treatment by transvenous embolisation via the superior ophthalmic vein. Orbit. (2013) 32:124–6. doi: 10.3109/01676830.2013.764444
10. Wang CY, Wei LC, Tsuei YS, Chen WH, and Shen YC. Intraorbital arteriovenous fistula of the ophthalmic vein-embolization using the thombosed superior ophthalmic vein approach. Can J Ophthalmol. (2016) 51:e34–37. doi: 10.1016/j.jcjo.2015.10.001
11. Robledo A, Frank TS, Karas PJ, Shaltoni H, O’Leary S, Darling R, et al. Stereotactic-guided direct orbital puncture for treatment of orbital arteriovenous fistula. J neurointerv Surg. (2023) 16:429. doi: 10.1136/jnis-2023-020145
12. Ghahvehchian H, Karimi N, Kashkouli MB, Ramadan M, Ghamari K, and Aghili S. Endoscopic-assisted orbitotomy for obliteration of orbital arteriovenous fistula refractory to endovascular techniques. Ophthalmic Plast Reconstr Surg. (2023) 39:e188–92. doi: 10.1097/IOP.0000000000002435
13. Choi BJ, Thacker IC, and Vrcek I. Surgical treatment of a spontaneous intraorbital arteriovenous fistula with direct embolization via transconjunctival orbitotomy. Proc (Bayl Univ Med Cent). (2024) 37:330–3. doi: 10.1080/08998280.2023.2299764
14. Wigton EH, Wells JR, Harrigan MR, Long JA, and Vicinanzo MG. Diagnosis and management of an intraorbital vascular fistula. Ophthalmic Plast Reconstr Surg. (2012) 28:e39–41. doi: 10.1097/IOP.0b013e31821971bf
15. Abuallut I, AlOtaibi YA, AlKhalifah R, and Mohana AJ. Thrombosis of intraorbital arterio-venous fistula. Neurosci (Riyadh). (2023) 28:48–52. doi: 10.17712/nsj.2023.1.20220012
16. Byeon HJ, Park KY, Yoon JS, and Ko J. Orbital venous malformation accompanied by arteriovenous fistula. Korean J Ophthalmol. (2020) 34:343–5. doi: 10.3341/kjo.2020.0043
17. Hamada Ji, Morioka M, Kai Y, Sakurama T, and Kuratsu Ji. Spontaneous arteriovenous fistula of the orbit: case report. Surg Neurology. (2006) 65:55–7. doi: 10.1016/j.surneu.2005.03.043
18. Su X, Song Z, Chen Y, Ye M, Zhang H, Ma Y, et al. Intraorbital arteriovenous fistulas: case series and systematic review. Oper Neurosurg. (2024) 27:23–30. doi: 10.1227/ons.0000000000001055
19. Konstas AA, Rootman DB, Quiros PA, and Ross IB. Transarterial embolization of a spontaneous intraorbital arteriovenous fistula with n-BCA glue. Ophthalmic Plast Reconstr Surg. (2017) 33:e63–4. doi: 10.1097/IOP.0000000000000753
20. Diaz R, Rodriguez R, Almeida P, and Ferrer G. Spontaneous intra-orbital arteriovenous fistula: A rare cause of proptosis. Cureus. (2019) 11:e5984. doi: 10.7759/cureus.5984
21. Minakawa S, Hirano M, Takahashi K, Imamura Y, and Watanabe T. A rare case of compression neuritis due to intraorbital arteriovenous fistula (IOAVF) mimicking retrobulbar optic neuritis. Acta Med Okayama. (2025) 79:59–64. doi: 10.18926/AMO/68363
22. Lv X, Li W, Liu A, Lv M, and Jiang C. Endovascular treatment evolution for pure intraorbital arteriovenous fistula: Three case reports and literature review. Neuroradiol J. (2017) 30:151–9. doi: 10.1177/1971400917692163
Keywords: orbital arteriovenous fistula, intraorbital arteriovenous fistula, orbital decompression, direct orbital arteriovenous fistula, orbital vascular lesions
Citation: Cheng OT, Chung SY, Wilseck JM and Kahana A (2025) Intravascular embolization of a direct orbital arteriovenous fistula: case report and review of the literature. Front. Ophthalmol. 5:1666024. doi: 10.3389/fopht.2025.1666024
Received: 15 July 2025; Accepted: 21 October 2025;
Published: 07 November 2025.
Edited by:
Farzad Pakdel, Tehran University of Medical Sciences, IranReviewed by:
Ashish Kulhari, HCA Midwest Health, United StatesAli Mokhtarzadeh, University of Minnesota Twin Cities, United States
Copyright © 2025 Cheng, Chung, Wilseck and Kahana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olivia T. Cheng, b3RjMkBjYXNlLmVkdQ==; Alon Kahana, YWthaGFuYUBtaW9jdWxvcGxhc3RpY3MuY29t
 Olivia T. Cheng
Olivia T. Cheng Stella Y. Chung
Stella Y. Chung Jeffrey M. Wilseck1
Jeffrey M. Wilseck1 Alon Kahana
Alon Kahana