- 1National Health Command Center, Ministry of Health, Riyadh, Saudi Arabia
- 2Global Center of Mass Gatherings Medicine, Ministry of Health, Riyadh, Saudi Arabia
- 3Ministry of Health, Riyadh, Saudi Arabia
Over 98% of the world's greenhouse gas emissions in 2014 came from carbon dioxide (CO2), methane, and nitrous oxide. Over one century, CO2 emissions increased from 3.09 to 37.12 billion metric tons. The healthcare sector is one of the major sources of greenhouse gas emissions. The carbon footprint of a country's healthcare system is influenced by its domestic economy, healthcare expenditure, and energy system. The aim of this study is to present a concise of the present status of carbon emissions within the healthcare sectors on a global scale, as well as the forthcoming endeavors to mitigate these emissions. A narrative review of studies on climate change, carbon emissions, and greenhouse gases in the healthcare sector was conducted using Medline PubMed, Web of Science, Scopus and Google Scholar databases from 2005 to April 2023. According to the data, several countries emit more carbon per capita than others. The Conference of the Parties on Climate Change (COP26) recently encompassed extensive efforts culminating in releasing initiatives toward zero-carbon healthcare sectors. Efforts in some medical practices, smart technology to save energy, digital health, artificial intelligence technology, and monitoring have contributed to reducing carbon emissions. In conclusion, the healthcare sector with zero carbon emissions must be sustainable, adaptable, and efficient while delivering safe, high-quality care. Addressing the sector's carbon footprint requires innovative strategies, a multisector approach, health professionals' participation, community engagement, and regular monitoring of emissions and performance indicators to ensure patient service quality and low carbon emissions in the healthcare sector.
Introduction
Climate change is a long-term, gradual variation in temperature and weather patterns influenced by human activities (World Health Organization, 2022). These factors entail variations in the amount of solar radiation the earth receives, oceanic processes (such as oceanic circulation), plate tectonics, forest fires, volcanic explosions, greenhouse gases (GHGs) intensification, and aerosol formation (Balato et al., 2013; Yue and Gao, 2018). In 2014, over 98% of the world's greenhouse gas emissions came from CO2, methane, and nitrous oxide (Edenhofer, 2015; OECD, 2017a). CO2 emissions have escalated from 3.09 to 37.12 billion metric tons between 1921 and 2021 (Ritchie et al., 2020). Recent analysis has found that the three primary sources of CO2 release are the combustion of fuels associated with transportation, CO2 emissions from power generation units, and construction and industrial sector operations (Udara Willhelm Abeydeera et al., 2019). Considering its widespread influence on society and the economy, the healthcare sector is one of the major sources of greenhouse gas emissions (Teghammar et al., 2019).
On average, member countries of the Organization for Economic Co-operation and Development (OECD) spent 9% of their gross domestic product on healthcare in 2021 (OECD, 2017b). Healthcare expenditures have skyrocketed over the past few decades, and healthcare-seeking increased due to aging populations, demographic shifts, and the prevalence of non-communicable diseases. However, despite its relatively low carbon effusions, the healthcare sector significantly contributes to the national CO2 footprint. Each year, the healthcare sector globally produces GHG emissions equal to 514 coal-fired power plants. Members of the OECD, including China and India, have accorded 5% CO2 from their healthcare sector to their national CO2 footprint. In 2014, the average per capita health carbon ranged from 0.06t CO2 in India to 1.51t CO2 in the U.S. The carbon footprint of a country's healthcare system is influenced by its domestic economy, healthcare expenditure, and energy system (Pichler et al., 2019). A study revealed that hospital care (36%), physicians and clinical services (12%), and prescription drugs (10%) are the healthcare services with the biggest carbon footprints (Eckelman and Sherman, 2016).
Recently, the Climate Change Conference (COP26) was launched in Glasgow, UK, by the World Health Organization, United Nations (U.N.) and collaborators in November 2021, aimed to develop sustainable and resilient climate change and low-carbon health systems (United Nations, 2022). However, efforts to mitigate carbon emissions in the health sector still need more (The Lancet Planetary Health, 2021). This paper aims to provide a brief overview of the current state of carbon emissions in the healthcare sector globally and future mitigation efforts. Furthermore, this study demonstrates the digital technologies employed for monitoring carbon emissions in health facilities in the Kingdom of Saudi Arabia, serving as a groundbreaking initiative that garnered commendation from numerous professionals in the field.
Methodology
A narrative review was conducted via the Medline PubMed, Web of Science, Scopus and Google Scholar databases using the keywords following the search terms with the term “health sector” or “healthcare sector” in combination with each of the following terms: “climate change,” “carbon emissions,” “carbon footprint,” and “greenhouse gases.” Studies published in the period between 2005 and April 2023 were included to identify the most recent evidence. English studies were included as the most common language in the scientific literature.
In addition, World Health Organization (WHO) and COP26 publications relating to the healthcare sector and search terms were also included. Additional studies were identified and included among the references cited from the included studies. Duplicate articles were excluded. Three public health experts screened the titles and abstracts and identified the most relevant papers according to the search criteria.
Results
Global healthcare carbon footprint figures
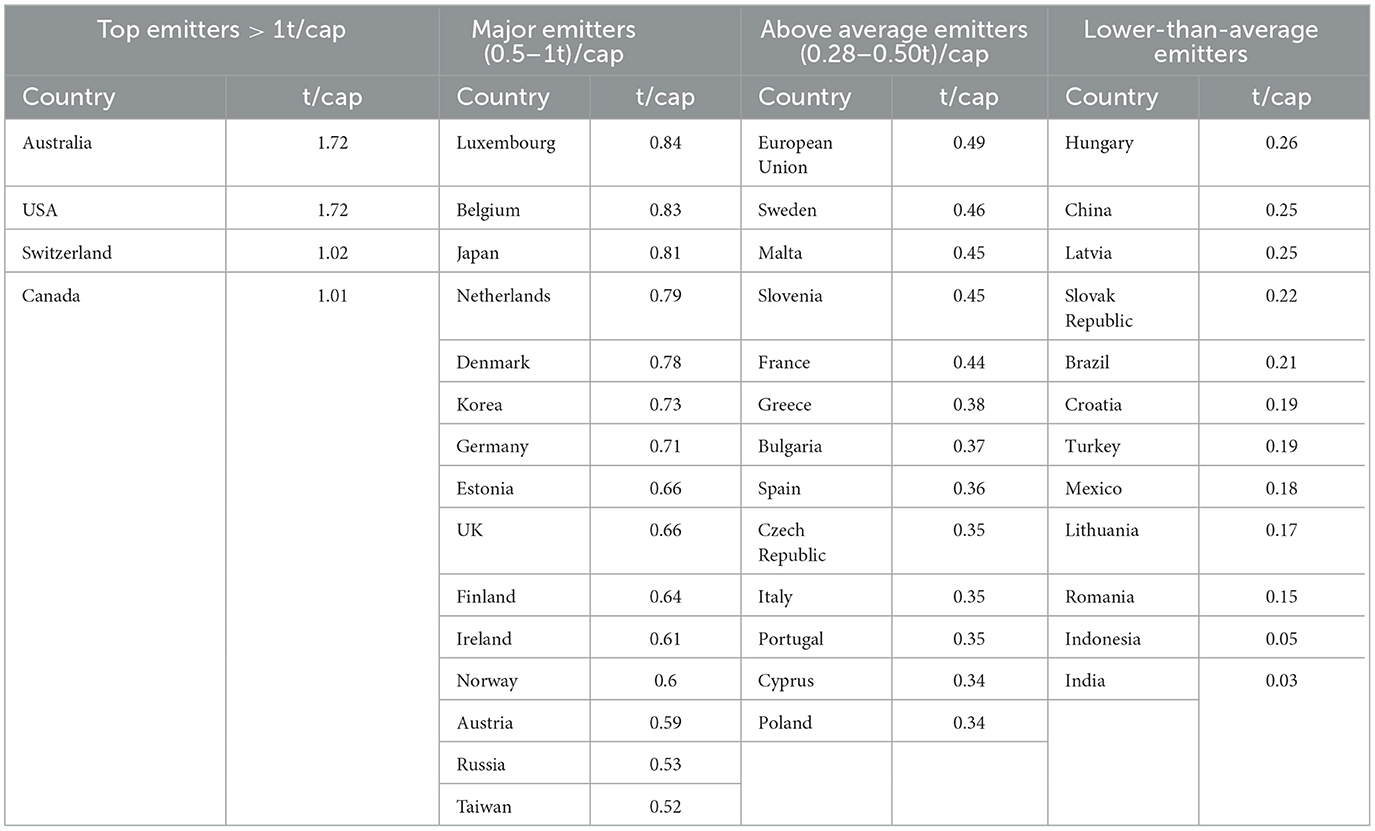
The global carbon footprint of healthcare has established a discernible pattern among lower-middle-income, upper-middle-income, low and middle-income, and high-income countries. A recent analysis has reported high carbon discharge among lower middle-income and low and middle-income, compared to upper-middle-income and high-income countries. A cumulative screening of 7 lower-middle-income and 24 Low and middle-income countries rendered an average CO2 intensity of 1.44 and 1.03 kgCO2e/$, respectively. In contrast, 17 Upper middle income and 37 High-income countries marked an average of 0.87 and 0.38 kgCO2e/$, respectively (Rasheed et al., 2021). On the other hand, a Health Care Without Harm (HCWH) report found that certain high-income countries have exceptionally high levels of health-related carbon emissions per person. The U.S. contributed 27% of all GHG emissions in the healthcare sector globally, followed by China with 17%, the European Union with 12%, Japan with 5%, Russia with 4%, India, Brazil, South Korea, Canada, and Australia each contributing 2% independently, and the remaining 25% coming from other countries (Karliner et al., 2019) (Table 1).
Scopes of healthcare-associated carbon emissions
Different nations worldwide contribute varying amounts of GHGs while providing medical care (Lenzen et al., 2020), which involves products, services, technologies, and instruments befalling the emission of high carbon to the environment. Significant sources of healthcare-associated GHGs are transport, energy consumption, product manufacturing, use, and disposal (Corvalan et al., 2020). About 40% of emissions have been attributed to electricity, heating, cooling, or gas distribution (Royal Society, 2023). Thirteen per cent of operational emissions were documented, followed by 11% from other manufacturing components (elemental metal, foods, textile, etc.), 9% from agricultural origins, 8% from other sectors and services, 7% from transport, 5% from pharmaceutical products, and 7% from minor categories such as waste treatment, rubber and plastic products, primary industries, and electronic equipment (Karliner et al., 2019).
Future initiatives for mitigating carbon emissions in the healthcare sector
International endeavors to reduce carbon emissions
HCWH and the Alliance of Nurses for Healthy Environments (ANHE) sought to inform, implement, and influence the impact of the healthcare sector on the environment. HCWH are a collaboration of 52 countries that offer ecologically safe alternatives to global perilous healthcare practice (Ballard, 2008). A programme called Practice Green Health aims to limit chemical and hazardous waste, eliminate mercury waste, reduce the amount of trash generated by the healthcare industry, and avoid pollution in general (Practice Green health, 2023). ANHE advocate for the integration of environmental health into nursing tasks by giving nurses educational forums abroad. The association supports environmental health through instruction, practice, research, and policy modifications to encourage the integration of environmentalism into nursing education and the greening of nursing facilities (ANHE, 2023).
Several organizations have devised plans to achieve measurable outcomes. In 2009, the US EPA (Environmental Protection Agency) established standards for disposing of infectious waste in healthcare facilities to minimize the emission of greenhouse gases and other harmful substances (Roberts, 2015). The United Kingdom National Health Service (NHS) pioneered a sustainable development unit in 2008 with the goal of meeting the government's commitment under the U.K. Climate Change Act. It examined the NHS's carbon footprint that same year. These assessments are frequently updated and improved to quantify GHG emissions from healthcare sectors and are pivotal to analysis on national grounds (Tennison et al., 2021). In the last decade, the World Health Organization drafted seven elements for healthy hospitals, the planet, and people (World Health Organization, 2010) (Box 1). Additionally, HCWH outlined seven high-impact actions on the path toward “zero emissions” while maintaining climate resilience and health equity across the healthcare sector (Karliner et al., 2021) (Box 2). In a recent COP26 conference, the Health Programme aimed to enhance the emphasis on health and the level of ambition within the framework of COP26. The COP26 Health Programme encompassed various initiatives toward net-carbon emissions in the healthcare sectors (World Health Organisation, 2021) (Box 3).
Box 1. Seven elements of a climate-friendly hospital (World Health Organization, 2010).
1. Energy efficiency Reduce hospital energy consumption and costs through efficiency and conservation measures.
2. Green building design Build hospitals that are responsive to local climate conditions and optimized for reduced energy and resource demands.
3. Alternative energy generation Produce and/or consume clean, renewable energy onsite to ensure reliable and resilient operation.
4. Transportation Use alternative fuels for hospital vehicle fleets; encourage walking and cycling to the facility; promoting staff, patient and community use of public transport; site healthcare buildings to minimize the need for staff and patient transportation.
5. Food Provide sustainably grown local food for staff and patients.
6. Waste Reduce, reuse, recycle, compost; employ alternatives to waste incineration.
7. Water Conserve water; avoid bottled water when safe alternatives exist.
Box 2. Seven high-impact actions on the path toward net zero.
1. Power healthcare with 100% clean, renewable electricity.
2. Invest in zero-emissions buildings and infrastructure.
3. Transition to zero-emissions sustainable travel and transport.
4. Provide healthy, sustainably grown food.
5. Incentivise and produce low-carbon pharmaceuticals.
6. Implement circular health care and sustainable health care waste management.
7. Establish greater health system effectiveness.
Box 3. The five key health priorities for COP26.
1. Building climate resilient health systems.
2. Developing low carbon sustainable health systems.
3. Adaptation Research for Health.
4. The inclusion of health priorities in Nationally Determined Contributions.
5. Raising the voice of health professionals as advocates for stronger ambition on climate change.
The Saudi Arabia national health command and control centre's novel role in controlling carbon emissions
The National Health Command and Control Centre (NHCC) within Saudi Arabia's Ministry of Health (MoH) is an interdisciplinary command center with the ability to continuously and thoroughly assess health system performance through 11 operations centers. NHCC is designed to ensure the effectiveness and efficiency of the health system, identify and detect substandard services and events, and respond to these items. In addition, NHCC leverages advanced analytics tools, such as simulation models and artificial intelligence, to predict and produce reports that inform health system decision-making.
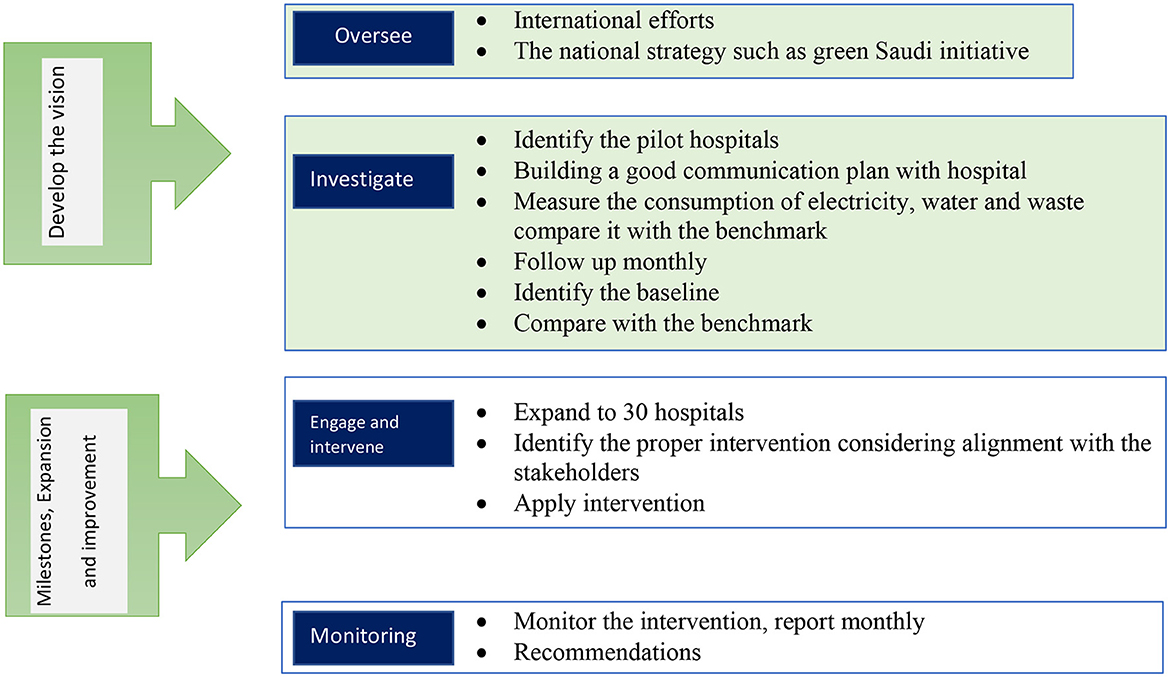
The NHCC started an initiative to reduce carbon emissions from MoH hospitals. This initiative follows the NHCC framework, which has four phases: oversee, investigate, intervene, and monitor. In the “oversee” phase, the initiative began by reviewing international efforts to measure and reduce emissions across various health sectors. Alignment with national strategies, such as the Saudi Green initiative, was established in this phase as well. The NHCC then identified pioneer hospitals to set a comparison benchmark, created appropriate initial key performance indicators (KPIs), and determined the criteria for the selection of appropriate pilot hospitals (i.e., hospitals with at least 400 beds). Seven pilot hospitals were selected to provide a sense of their carbon emission baseline, starting with three domains: electricity, water, and waste. In the Investigation phase, carbon emissions from electricity, water and non-medical waste were measured in each pilot hospital. Emission patterns are investigated monthly through KPIs. The pilot hospitals understood the scope of the initiative, building a strong focal point through the regional health command center, thereby creating an effective communication strategy for increased engagement and collaboration. In the intervention phase, the NHCC will suggest areas for improvement, intervention activities, and emission reduction targets, along with supporting the facilities in intervention implementation. In the monitoring phase, the NHCC will follow up and evaluate this intervention by using tools (e.g., ticketing system) to detect the low performance and respond and intervene accordingly. In the monitoring phase, performance will be reported using the NHCC dashboard for more engagement and support from the decision-makers (Figures 1, 2).
Pilot phase
• Seven hospitals have been chosen as pilots (all have at least 400 hospital beds)
- King Salman Hospital in Riyadh
- Prince Mohammed bin Abdulaziz Hospital in Riyadh
- King Fahad medical city in Riyadh
- King Fahad Central Hospital in Jazan
- King Khalid Hospital in Najran
- Asser Central Hospital in Asser
- King Fahad Hospital in Qassim
• Selection of initial KPIs for reporting
Reporting on monthly electricity and water consumption, as well as waste production on the carbon emissions dashboard
- Average electricity consumption (kW/month). Per bed, per employee, per square meter
- Average water consumption (liter/month). Per bed, per employee, per square meter
- Average waste production (kg/month)
• Calculating the carbon emissions from electricity and water consumption, as well as waste production, using the U.S. conversion factor
- Stakeholder alignment
• Gained alignment through discussions with the MoH Climate Change Committee and MoH Facility Management
• Benchmarking with a selection of NHS Trusts
Applied benchmarks from seven NHS trusts enabling comparison per square meter, employee, patient visit, and bed:
- Leeds Teaching Hospital
- King's College Hospital
- Manchester University Hospital
- Cambridge University Hospital
- University College London Hospital
- Guys and St Thomas Hospital
- Imperial College Hospital
• Initiation of monthly reporting in seven hospital facilities
• Continued data gathering and reporting
Closing data gaps for square meters, patient visits, and waste production for the 7 MoH facilities. Data are being uploaded to the Net Zero dashboard to be presented to the decision-makers in MoH.
Different perspectives to reduce carbon emissions
Several methods have been documented and internationally practiced to minimize carbon in the healthcare sector. The U.S. has employed energy-cutting stratagems by switching-off electronic devices on inoperative timings. This facilitates carbon emission reductions in a convenient, rapid manner (Sadler and Guenther, 2015; Frumkin, 2018). Hospitals are the chief biohazard waste-producing centers globally (Padmanabhan and Barik, 2019; Kenny and Priyadarshini, 2021). Disposal processes involve high carbon production (Rizan et al., 2021). This can be mitigated by identifying waste areas and providing specialized training to the staff on using the National Institute for Health and Care Excellence (NICE) “do not do” recommendation database and “Choosing Wisely” list of low-value interventions. Carbon emissions can be further reduced by embracing support initiatives in clinical leadership skill development and in clinical settings to minimize carbon waste. Curtailing the disposal of viable pharmaceutical products is a feasible indirect approach (Tong et al., 2011; The Academy of Medical Royal Colleges, 2014). In addition, NHS should ensure that products are being prepared under environmental sustainability regulations (NHS Supply Chain, 2012; Samuel and Lucassen, 2022). Public awareness sessions are equally important to convey the extent of environmental severity (Edwards and Roberts, 2009; Capstick et al., 2015; Rahimi, 2020). Telemedicine should be encouraged, and face-to-face consultations should be justifiably called, as telemedicine has evinced potentially high scores in reducing carbon consumption (Holmner et al., 2014; Tsagkaris et al., 2021; Lokmic-Tomkins et al., 2022; Maria et al., 2022; Morcillo Serra et al., 2022; Patel et al., 2023). According to a study by Holmner et al., carbon emissions have decreased by 40–70 times because of people using telemedicine instead of commuting to medical facilities (Holmner et al., 2014). Another study showed that an autonomous A.I. could reduce GHG emissions by 80% but only compared marginal GHG emissions from one additional diabetic eye exam (Wolf et al., 2022).
McAlister et al. assessed the carbon footprint of hospital diagnostic imaging in Australia. Clinicians can reduce diagnostic imaging carbon emissions by ordering less imaging, employing low-impact imaging (X-ray and U.S.) instead of MRI and C.T. scans where clinically appropriate, turning off scanners, when possible, to reduce standby power emissions; reducing scan impact enhances resource efficiency (McAlister et al., 2022a). Another study by Heye et al. (2020) showed that the energy consumption of MRI and C.T. was about 4% of the total energy consumed in the hospital and found that MRI consumed fifth times energy than C.T. devices. Potential energy and cost savings could be achieved during unproductive inactivity and system downtime patterns (Heye et al., 2020). Friedericy et al. (2019) noted that carbon emissions could be mitigated in operating rooms by using sustainable energy and turning off the heating, ventilation, and air conditioning after hours. Anesthetists can significantly minimize the carbon footprint of the operating room by using intravenous anesthesia instead of inhalation anesthesia. Circular procurement, choosing reusable vs. disposable materials, and recycling can all help to reduce the operating room's indirect carbon emissions and waste generation (Friedericy et al., 2019). Furthermore, empowering patients can facilitate fewer rehospitalisations and relatively fewer hospital visits, which will eventuate in the use of less carbon (Charmel and Frampton, 2008). Several studies have found that using metered dose inhalers in people with respiratory diseases increases carbon emissions over time (Wilkinson et al., 2019; Janson et al., 2020; Panigone et al., 2020; Kponee-Shovein et al., 2022; Wichers and Pieters, 2022). When possible, using alternatives such as powder-free inhalers or soft mist inhalers can reduce carbon emissions (Pernigotti et al., 2021).
Discussion
This study sheds light on global carbon emissions in the health sector and efforts to mitigate greenhouse gases. Globally, the figures showed higher carbon emissions per capita from the health sector in some countries than others (Pichler et al., 2019). The efforts of countries to reduce these figures in the future contribute greatly to the health of the environment and the health of society in the first place due to the known harmful effects of carbon emissions. In the scope of community health, the effects of carbon emissions reduction influence health benefits and decrease disability-adjusted life years (Gavurova et al., 2021). Climate change fatalities are estimated to be approximately 250,000 deaths annually between 2030 and 2050 (Burch et al., 2022). Moreover, climate change can potentially result in the geographical dissemination of infectious diseases (Bhandari et al., 2020). Unfortunately, delaying carbon footprint reduction could affect the health and quality of life in the next few years.
The global figures for carbon emissions in the health sector are expected to be three times higher in the year 2050 (Karliner et al., 2019). International collaboration in reducing carbon emissions benefits all countries and is not limited to a host country as an effect of climate change and purely global health security (Yellapu et al., 2022). Efforts are ongoing to find solutions to reduce carbon emissions and need more (Yao et al., 2022). The most important step is commitment and performance monitoring of carbon emissions (McAlister et al., 2022b), as tangible results from reducing carbon emissions need a long time, but in the short-term, avoiding damage from warming impacts (Sun et al., 2022).
In summary of recommendations of this study to mitigate carbon footprint in the healthcare sectors:
- Developing innovative strategies with specific goal targets and indicators for each health facility to enhance reducing carbon emissions, commencing from health centers and extending to hospitals.
- Monitoring performance indicators for each health facility and periodically verifying these indicators are essential practices.
- Promoting research and studies focusing on carbon emissions reduction within the health sector.
- Implementing intelligent technological systems in the healthcare sector that resulted in significant and expeditious transformations, including, for instance, energy-efficient lighting solutions, smart air conditioning, and intelligent occupancy sensors for energy savings.
- Involving healthcare professionals in mitigating carbon footprint by minimizing unnecessary medical procedures that can be conducted with minimal environmental impact.
- Engaging the community in utilizing contemporary technologies such as telemedical consultations.
- Implementation of renewable energy sources in establishing new health facilities, alongside promoting health facilities that exclusively rely on clean energy.
- Recognizing and capitalizing on new methods of energy efficiency.
- Enhancing community engagement to actively participate in the pursuit of carbon emission reduction targets within the healthcare sector.
- Encouraging multisector collaboration between health and other stakeholders.
This study effectively elucidates the fundamental objective, albeit it possesses some limitations. The scope of the search was limited to articles in the English language. Moreover, it is important to acknowledge that the scope of our search was constrained using certain search terms and a specific period from 2003 to the present. Consequently, relevant publications may have been overlooked. Moreover, CO2 emissions in some nations have been founded in estimation numbers, offering an overview of the issue. However, it is important to note that these estimates should not be solely relied upon for precise figures.
Conclusion
Ensuring the healthcare sector's longevity, adaptability, and sustainability with zero carbon footprint and facing imminent and continuous challenges while simultaneously delivering safe, high-quality, and efficient healthcare poses a considerable challenge for policymakers, healthcare providers, and individuals seeking healthcare services. In addition, more creative approaches are needed to reduce the healthcare sector's carbon footprint without jeopardizing patient service quality. Community engagement and healthcare workers' contributions should be engaged in the action plan to reduce carbon emissions. Finally, monitoring carbon emissions and performance indicators on a periodic basis prompts the health sector to work collectively to achieve the desired goals.
Author contributions
DM and MB: Conceptualization. MB, FA, AAA, YA, and SA: Methodology and participation in writing the original and final draft. MB, SA, AA, NA, and AK: Data collection. MKA: Participation in writing the final draft and supervision and review. All authors reviewed and approved the submission.
Acknowledgments
We would like to thank all healthcare workers who contributed to providing Data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
FA declared that they were an editorial board member of Frontiers, at the time of submission.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
OECD, Organization for Economic Co-operation and Development; GDP, Gross domestic product; HCWH, Health care without harm; ANHE, Alliance of Nurses for Healthy Environments; NHCC, The National Health Command Center; MoH, Ministry of Health; GHG, Green House Gases; CO2, Carbon dioxide; HCS, Health care sector; EPA, Environmental Protection Agency; NHS, National Health Service; Cap, capita; KPI, key performance indicator; NICE, National Institute for Health and Care Excellence; CT, Computed tomography; MRI, Magnetic resonance imaging.
References
ANHE (2023). Alliance of Nurses for Healthy Environments (ANHE). Available online at: https://envirn.org/ (accessed February 27, 2023).
Balato, N., Ayala, F., Megna, M., Balato, A., and Patruno, C. (2013). Climate change and skin. Giornale Italiano di Dermatologia e Venereologia. 148, 135–146.
Ballard, K. A. (2008). Nurses as environmental health activists. Am. J. Nurs. 108, 69–72. doi: 10.1097/01.NAJ.0000318004.85657.fe
Bhandari, D., Bi, P., Sherchand, J. B., Dhimal, M., and Hanson-Easey, S. (2020). Climate change and infectious disease research in Nepal: are the available prerequisites supportive enough to researchers? Acta. Trop. 204:105337. doi: 10.1016/j.actatropica.2020.105337
Burch, H., Beaton, L. J., Simpson, G., Watson, B., Maxwell, J., and Winkel, K. D. (2022). A planetary health–organ system map to integrate climate change and health content into medical curricula. Med. J. Aust. 217, 469–473. doi: 10.5694/mja2.51737
Capstick, S., Whitmarsh, L., Poortinga, W., Pidgeon, N., and Upham, P. (2015). International trends in public perceptions of climate change over the past quarter century. WIREs Clim. Change 6, 35–61. doi: 10.1002/wcc.321
Charmel, P. A., and Frampton, S. B. (2008). Building the business case for patient-centered care. Healthc. Financ. Manage. 62, 80–85.
Corvalan, C., Villalobos Prats, E., Sena, A., Campbell-Lendrum, D., Karliner, J., Risso, A., et al. (2020). Towards climate resilient and environmentally sustainable health care facilities. Int. J. Environ. Res. Public Health. 17:8849. doi: 10.3390/ijerph17238849
Eckelman, M. J., and Sherman, J. (2016). Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE. 11:e0157014. doi: 10.1371/journal.pone.0157014
Edenhofer, O. (2015). Climate Change 2014: Mitigation of Climate Change. Vol. 3. New York, NY: Cambridge University Press.
Edwards, P., and Roberts, I. (2009). Population adiposity and climate change. Int. J. Epidemiol. 38, 1137–1140. doi: 10.1093/ije/dyp172
Friedericy, H. J., Sperna Weiland, N. H., van der Eijk, A. C., and Jansen, F. W. (2019). [Steps for reducing the carbon footprint of the operating room]. Ned. Tijdschr Geneeskd. 163:D4095.
Frumkin, H. (2018). The U.S. health care sector's carbon footprint: stomping or treading lightly? Am. J. Public Health 108, S56–S57. doi: 10.2105/AJPH.2017.304160
Gavurova, B., Rigelsky, M., and Ivankova, V. (2021). Greenhouse gas emissions and health in the countries of the European Union. Front. Public Health 9:756652. doi: 10.3389/fpubh.2021.756652
Heye, T., Knoerl, R., Wehrle, T., Mangold, D., Cerminara, A., Loser, M., et al. (2020). The energy consumption of radiology: energy- and cost-saving opportunities for C.T. and MRI operation. Radiology 295, 593–605. doi: 10.1148/radiol.2020192084
Holmner, Å., Ebi, K. L., Lazuardi, L., and Nilsson, M. (2014). carbon footprint of telemedicine solutions - unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE. 9:e105040. doi: 10.1371/journal.pone.0105040
Janson, C., Henderson, R., Löfdahl, M., Hedberg, M., Sharma, R., Wilkinson, A. J. K., et al. (2020). Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax. 75, 82–84. doi: 10.1136/thoraxjnl-2019-213744
Karliner, J., Roschnik, S., Boyd, R., Ashby, B., and Steele, K. (2021). Global Road Map for Health Care Decarbonization. A Navigational Tool for Achieving Zero Emissions With Climate Resilience and Health Equity. Health Care Without Harm and Arup.
Karliner, J., Slotterback, S., Boyd, R., Ashby, b., and Steele, K. (2019). Health Care Climate Footprint Report. Health Care Without Harm. Available online at: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed February 10, 2023).
Kenny, C., and Priyadarshini, A. (2021). Review of current healthcare waste management methods and their effect on global health. Healthcare 9:284 doi: 10.3390/healthcare9030284
Kponee-Shovein, K., Marvel, J., Ishikawa, R., Choubey, A., Kaur, H., Ngom, K., et al. (2022). Impact of choice of inhalers for asthma care on global carbon footprint and societal costs: a long-term economic evaluation. J. Med. Econ. 25, 940–953. doi: 10.1080/13696998.2022.2088196
Lenzen, M., Malik, A., Li, M., Fry, J., Weisz, H., Pichler, P. P., et al. (2020). The environmental footprint of health care: a global assessment. Lancet Planet Health 4:e271–e279. doi: 10.1016/S2542-5196(20)30121-2
Lokmic-Tomkins, Z., Davies, S., Block, L. J., Cochrane, L., Dorin, A., von Gerich, H., et al. (2022). Assessing the carbon footprint of digital health interventions: a scoping review. J. Am. Med. Inform. Assoc. 29, 2128–2139. doi: 10.1093/jamia/ocac196
Maria, M. S., Silvia, A. N., Beatriz, D. G., Andrew, D., and Guillermo, P. F. (2022). Health care in rural areas: proposal of a new telemedicine program assisted from the reference health centers, for a sustainable digitisation and its contribution to the carbon footprint reduction. Heliyon 8:e09812. doi: 10.1016/j.heliyon.2022.e09812
McAlister, S., McGain, F., Petersen, M., Story, D., Charlesworth, K., Ison, G., et al. (2022a). The carbon footprint of hospital diagnostic imaging in Australia. Lancet Reg. Health West Pac. 24:100459. doi: 10.1016/j.lanwpc.2022.100459
McAlister, S., Morton, R. L., and Barratt, A. (2022b). Incorporating carbon into health care: adding carbon emissions to health technology assessments. Lancet Planet Health 6, e993–e999. doi: 10.1016/S2542-5196(22)00258-3
Morcillo Serra, C., Aroca Tanarro, A., Cummings, C. M., Jimenez Fuertes, A., and Tomás Martínez, J. F. (2022). Impact on the reduction of CO2 emissions due to the use of telemedicine. Sci. Rep. 12, 12507. doi: 10.1038/s41598-022-16864-2
NHS Supply Chain (2012). Code of Conduct Policy. Available online at: https://wwwmedia.supplychain.nhs.uk/media/AHR-231-Code-of-Conduct-Policy.pdf (accessed February 27, 2023).
OECD (2017a). A System of Health Accounts 2011. Available online at: https://www.oecd.org/publications/a-system-of-health-accounts-2011-9789264270985-en.htm (accessed February 27, 2023).
OECD (2017b). Health Expenditure. Available online at: https://www.oecd.org/health/health-expenditure.htm (accessed February 27, 2023).
Padmanabhan, K. K., and Barik, D. (2019). “Health hazards of medical waste and its disposal,” in Energy from Toxic Organic Waste for Heat and Power Generation (Elsevier), 99–118. doi: 10.1016/B978-0-08-102528-4.00008-0
Panigone, S., Sandri, F., Ferri, R., Volpato, A., Nudo, E., Nicolini, G., et al. (2020). Environmental impact of inhalers for respiratory diseases: decreasing the carbon footprint while preserving patient-tailored treatment. BMJ Open Respir. Res. 7:e000571. doi: 10.1136/bmjresp-2020-000571
Patel, K. B., Gonzalez, B. D., Turner, K., Alishahi Tabriz, A., Rollison, D. E., Robinson, E., et al. (2023). Estimated carbon emissions savings with shifts from in-person visits to telemedicine for patients with cancer. JAMA Netw. Open. 6:e2253788. doi: 10.1001/jamanetworkopen.2022.53788
Pernigotti, D., Stonham, C., Panigone, S., Sandri, F., Ferri, R., Unal, Y., et al. (2021). Reducing carbon footprint of inhalers: analysis of climate and clinical implications of different scenarios in five European countries. BMJ Open Respir. Res. 8:e001071. doi: 10.1136/bmjresp-2021-001071
Pichler, P. P., Jaccard, I. S., Weisz, U., and Weisz, H. (2019). International comparison of health care carbon footprints. Environ. Res. Lett. 14, 064004. doi: 10.1088/1748-9326/ab19e1
Practice Green health (2023). Join Practice Greenhealth. Available online at: https://practicegreenhealth.org/about (accessed February 27, 2023).
Rahimi, M. (2020). Public awareness: what climate change scientists should consider. Sustainability 12:8369. doi: 10.3390/su12208369
Rasheed, F. N., Baddley, J., Prabhakaran, P., de Barros, E. F., Reddy, K. S., Vianna, N. A., et al. (2021). Decarbonising healthcare in low and middle income countries: potential pathways to net zero emissions. BMJ 375:n1284. doi: 10.1136/bmj.n1284
Ritchie, H., Roser, M., and Rosado, P. (2020). CO2 and Greenhouse Gas Emissions. Available online at: https://ourworldindata.org/co2-and-greenhouse-gas-emissions (accessed February 25, 2023).
Rizan, C., Bhutta, M. F., Reed, M., and Lillywhite, R. (2021). The carbon footprint of waste streams in a U.K. hospital. J. Clean Prod. 286:125446. doi: 10.1016/j.jclepro.2020.125446
Roberts, D. (2015). Environmental requirements related to patient care and the team working to ensure compliance. U.S. Army Med. Dep. J. 25–31.
Royal Society (2023). Climate Change: Science and Solutions. Available online at: https://royalsociety.org/topics-policy/projects/climate-change-science-solutions/ (accessed February 27, 2023).
Sadler, B. L., and Guenther, R. (2015). Ten rules for 21st century healthcare: a U.S. perspective on creating healthy, healing environments. Future Hosp. J. 2, 22–27. doi: 10.7861/futurehosp.15.009
Samuel, G., and Lucassen, A. M. (2022). The environmental sustainability of data-driven health research: a scoping review. Digit. Health 8:20552076221111296. doi: 10.1177/20552076221111297
Sun, X., Wang, P., Ferris, T., Lin, H., Dreyfus, G., Gu, B. H., et al. (2022). Fast action on short-lived climate pollutants and nature-based solutions to help countries meet carbon neutrality goals. Adv. Clim. Change Res. 13, 564–577. doi: 10.1016/j.accre.2022.06.003
Teghammar, A., Sand Lindskog, H., Fagerberg, B., and Berko, L. (2019). [Climate impact of healthcare]. Lakartidningen. 116.
Tennison, I., Roschnik, S., Ashby, B., Boyd, R., Hamilton, I., Oreszczyn, T., et al. (2021). Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health 5, e84–92. doi: 10.1016/S2542-5196(20)30271-0
The Academy of Medical Royal Colleges (2014). The Academy of Medical Royal Colleges fom.ac.uk. Available online at: http://www.fom.ac.uk/wp-content/uploads/AoMRC-FOM-Core-Guidance-on-Supporting-Information-for-Revalidation-June14.pdf (accessed February 25, 2023).
The Lancet Planetary Health (2021). COP26 in review. Lancet Planet Health 5, e851. doi: 10.1016/S2542-5196(21)00320-X
Tong, A. Y. C., Peake, B. M., and Braund, R. (2011). Disposal practices for unused medications around the world. Environ. Int. 37, 292–298. doi: 10.1016/j.envint.2010.10.002
Tsagkaris, C., Hoian, A. V., Ahmad, S., Essar, M. Y., Campbell, L. W., et al. (2021). Using telemedicine for a lower carbon footprint in healthcare: a twofold tale of healing. J. Clim. Change Health 1:100006. doi: 10.1016/j.joclim.2021.100006
Udara Willhelm Abeydeera, L. H., Wadu Mesthrige, J., and Samarasinghalage, T. I. (2019). Global research on carbon emissions: a scientometric review. Sustainability 11:3972. doi: 10.3390/su11143972
United Nations (2022). COP26: Together for Our Planet. Available online at: https://www.un.org/en/climatechange/cop26 (accessed August 20, 2023).
Wichers, I. M., and Pieters, L. I. (2022). [Environmental impact of inhalers in the Netherlands and worldwide: the facts at a glance]. Ned Tijdschr Geneeskd. 166:D6718.
Wilkinson, A. J. K., Braggins, R., Steinbach, I., and Smith, J. (2019). Costs of switching to low global warming potential inhalers. an economic and carbon footprint analysis of NHS prescription data in England. BMJ Open 9:e028763. doi: 10.1136/bmjopen-2018-028763
Wolf, R. M., Abramoff, M. D., Channa, R., Tava, C., Clarida, W., Lehmann, H. P., et al. (2022). Potential reduction in healthcare carbon footprint by autonomous artificial intelligence. NPJ Digit Med. 5, 62. doi: 10.1038/s41746-022-00605-w
World Health Organisation (2021). COP26 Special Report on Climate Change and Health: The Health Argument For Climate Action. Geneva: World Health Organization.
World Health Organization (2010). Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Health Care Settings: Discussion Draft. Geneva: WHO.
World Health Organization (2022). Climate Change and Health. Available online at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed February 27, 2023).
Yao, L., Tan, S., and Xu, Z. (2022). Towards carbon neutrality: what has been done and what needs to be done for carbon emission reduction? Environ. Sci. Pollut. Res. 30, 20570–20589. doi: 10.1007/s11356-022-23595-4
Yellapu, V., Malan, S., Merkert, B., Kharecha, H., Alam, A., Stawicki, P. S., et al. (2022). “Impact of climate change on international health security: an intersection of complexity, interdependence, and urgency,” in Contemporary Developments and Perspectives in International Health Security - Volume 3. IntechOpen. doi: 10.5772/intechopen.96713
Keywords: climate change, global health, carbon emission, environmental health, public health, health management, healthcare sector carbon footprint, digital practice
Citation: Mominkhan D, Alamri FA, Balharith M, Alharbi M, Alshebli A, Alshareef SY, Khairaldain A, Almutairi N, Abusit A, Almuzaini Y, Alahmari AA and Alabdulaali MK (2023) The current state and potential evolution of carbon emissions in the healthcare sector: a narrative review article. Front. Sustain. Energy Policy 2:1230253. doi: 10.3389/fsuep.2023.1230253
Received: 02 June 2023; Accepted: 26 October 2023;
Published: 15 December 2023.
Edited by:
Presley Kaybe Wesseh Jr., Xiamen University, ChinaReviewed by:
Ridwan Ibrahim, University of Lagos, NigeriaCopyright © 2023 Mominkhan, Alamri, Balharith, Alharbi, Alshebli, Alshareef, Khairaldain, Almutairi, Abusit, Almuzaini, Alahmari and Alabdulaali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fahad A. Alamri, ZmFhYmFsYW1yaUBtb2guZ292LnNh
 Dalia Mominkhan1
Dalia Mominkhan1 Fahad A. Alamri
Fahad A. Alamri Manea Balharith
Manea Balharith Yasir Almuzaini
Yasir Almuzaini Ahmed A. Alahmari
Ahmed A. Alahmari