- 1Department of Medicine, Division of Gastroenterology and Hepatology, MASLD Research Center, University of California San Diego, San Diego, CA, United States
- 2Department of Medicine, School of Medicine, California University of Science and Medicine, Colton, CA, United States
- 3Department of Medicine, University of California San Diego, San Diego, CA, United States
- 4Herbet Wertheim School of Public Health, University of California San Diego, San Diego, CA, United States
Background: Social determinants of health (SDOH) and transplant center characteristics have been associated with access to liver transplantation (LT) for Hispanic individuals. The aim of this study was to identify waitlist characteristics and correlates of odds of LT and waitlist removal by Hispanic ethnicity.
Methods: This was a single-center cohort study of adults listed for LT between January 2018–December 2020. Demographic, clinical, and SDOH were analyzed using logistic regression.
Results: 375 patients were included. 52.5% (N = 197) were Hispanic. At time of listing, Hispanic patients had significantly higher BMI, prevalence of diabetes and metabolic dysfunction associated steatohepatitis. Rates of substance use were significantly lower and time of last drink to listing was significantly longer (641 vs. 391 days, p = 0.0007) in Hispanic adults. Rates of LT and waitlist removal did not significantly differ by Hispanic ethnicity (46.9% vs. 46.1% and 35% vs. 36.5%, respectively). Hepatocellular carcinoma (OR 3.28) was associated with odds of LT whereas employment status predicted waitlist removal.
Conclusions: Distribution on the waitlist, LT and waitlist removal did not differ by Hispanic ethnicity. Hispanic patients had significantly longer time from last drink to listing, suggesting referral bias. Public health interventions to optimize LT referral are needed to increase health equity.
Background
The Hispanic population is one of the fastest growing in the United States (US), accounting for approximately 20% of the population (1). Hispanic adults are disproportionately impacted by chronic liver disease, with the most pronounced disparities noted in prevalence of metabolic dysfunction–associated steatotic liver disease (MASLD) and its more aggressive subtype metabolic dysfunction–associated steatohepatits (MASH) (2). Despite this increased prevalence in liver disease with associated risk of need for liver transplantation (LT), prior studies have demonstrated lower rates of referral for LT, LT listing and rates of LT for Hispanic individuals (3–6). The mechanisms underlying these disparities in LT access are multifactorial and also involve intersectionality of several SDOH factors disproportionately impacting the Hispanic community in the US.
Access to healthcare is one SDOH that contributes strongly to disparities throughout the medical system, including LT. Patients with public forms of insurance have lower likelihood of referral for LT, and Hispanic individuals are less likely to have private insurance (7, 8). Both implicit and explicit biases and other forms of structural racism also impact referral and overall care management in chronic disease. From a liver transplant perspective, this manifests most strongly in forms of liver disease associated with health behaviors including alcohol-associated liver disease (ALD) (9, 10). Once referred and listed, several factors have been identified as impacting differences in rates of LT and waitlist removal for minority populations. Low socioeconomic status, public insurance or lack of insurance, and rural locality, factors that commonly impact Hispanic populations, have been independently associated with lower likelihood of LT and higher LT waitlist mortality (6, 11–14).
While current literature, including analyses of large databases such as the Scientific Registry of Transplant Recipients (SRTR), has shown racial and ethnic disparities in LT referral, listing, LT rates and waitlist outcomes, results specific to these outcomes for Hispanic individuals have been discordant across studies. For example, analysis of 24,595 LT from the National Inpatient Sample (NIS) found that Hispanic individuals had increased rates of LT compared to White patients [adjusted odds ratio (aOR) 1.16] (14). The specific factors identified as playing a causal role in disparities for Hispanic patients in need of LT have also been inconsistent in the literature. Therefore, the aim of this study was to identify factors impacting LT access including waitlist characteristics, correlates of odds of LT and waitlist removal by Hispanic ethnicity in a large, ethnically diverse academic transplant center database in which more detailed assessment of psychosocial and SDOH factors was available for analysis.
Material and methods
Study population and design
This retrospective cohort study included adults age 18 or older listed for LT between January 2018 and December 2020 at an academic transplant center in an ethnically diverse setting. Exclusion criteria included those listed as status 1A and patients who underwent prior LT. Our center utilizes a variety of grafts including donation after circulatory (DCD) and brain death (DBD) as well as living donors and extended criteria donors (ECDs) with graft acceptance evaluated by transplant surgery in consultation with transplant hepatology based on individual recipient characteristics. All data elements analyzed in the study were obtained through structured review of our EMR system. Demographic, clinical, psychosocial, and SDOH data were gathered through a retrospective review of electronic medical records. Data extracted from chart review consisted of past medical history, family history, social history, multidisciplinary pre-transplant workup, post-transplant follow-up notes, imaging, laboratory and other diagnostic testing results and information regarding removal from waitlist, death, or LT. Cardiac parameters, including ejection fraction and right ventricular systolic pressure (RVSP), were primarily obtained from transthoracic echocardiogram (TTE) performed as part of routine pre-transplant cardiovascular evaluation to reflect potential cardiopulmonary contributors to listing and transplantation decisions. Heart catheterization data was conducted in select cases when indicated based on initial screening. Psychiatric and substance use history included history of failed rehabilitation, time (in days) between last drink and listed for transplant, Alcohol Use Disorders Identification Test (AUDIT) score, history of mental health conditions, marijuana use, other substance use, tobacco use, and Stanford Integrated Psychosocial Assessment Tool (SIPAT). Karnofsky scores, used to assess functional status, were collected as well. SDOH included annual household income, education level, current employment status, marital status, and whether the patient had private insurance. Annual income was categorized as <$25,000, $25–50,000, $50–100,000, and >$100,000. Education level was classified as less than high school, completed high school, some college or associates degree, college graduate, or advanced degree. Current employment status included employed vs. unemployed. Marital status was defined as either married/in a long-term partnership or not. Ethics approval for this study was provided by our Institutional Review Board.
Statistical analysis
Chi-squared analysis was used to compare demographic, clinical, psychosocial, and SDOH between Hispanic and non-Hispanic candidates at time of listing. Univariate and multivariate logistic regression analyses were conducted to examine characteristics associated with odds of LT and waitlist removal. Statistical analysis was performed using STATA software, with statistical significance defined as p < 0.05.
Results
Patient characteristics at time of LT listing
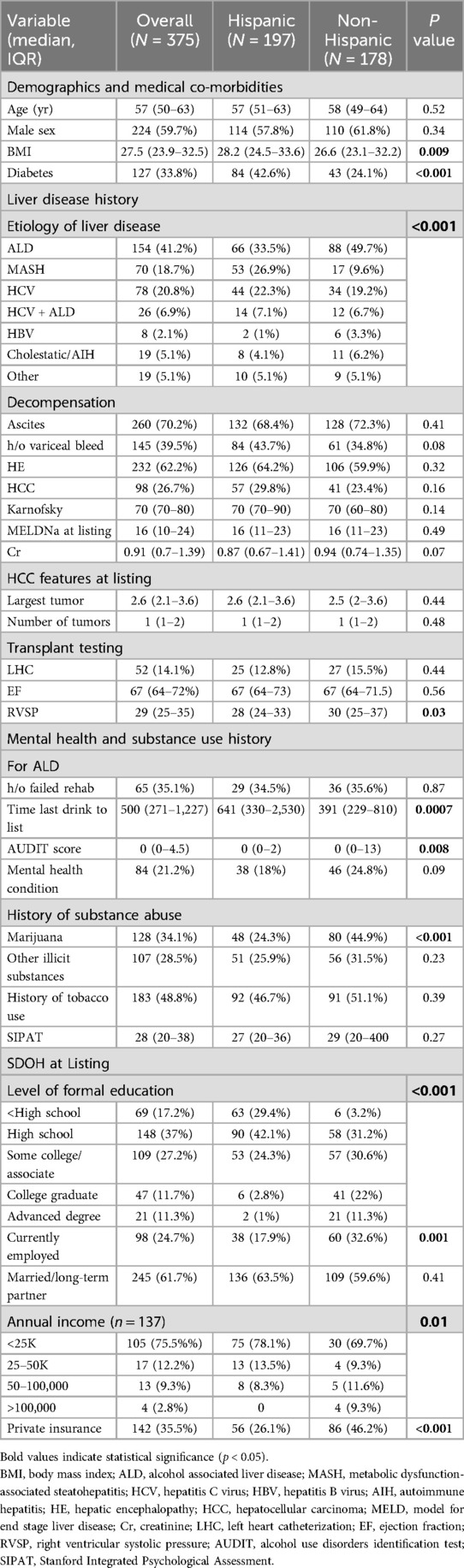
A total of 375 patients listed for LT were included in this study, of whom 52.5% (N = 197) were Hispanic. The non-Hispanic cohort (N = 178) consisted of 76.4% (N = 136) White, 4.5% (N = 8) Black, 9.5% (N = 17) Asian, and 9.5% (N = 17) other race (including American Indian, Alaska Native, Native Hawaiian or other Pacific Islander and mixed race not including Hispanic). The cohort consisted of 224 males (59.7%) with a median age of 57 [interquartile range (IQR) 50–63], median body mass index (BMI) of 27.5 with 24% having type II diabetes (Table 1). The most common etiologies of liver disease were ALD (41.2%), hepatitis C virus (HCV) 20.8% and MASH (18.7%). Median model of end stage liver disease (MELD) Na at time of listing was 16 (IQR 10–24). At time of listing, Hispanic patients had higher BMI (28.2 vs. 26.2 kg/m2, p = 0.009), percentage of diabetes (42.6% vs. 24.1%, p = <0.001), and MASH as indication for LT (26.9% vs. 9.6%, p = <0.001). There were no statistically significant differences in MELDNa at listing, hepatocellular carcinoma (HCC), forms of decompensation or functional status as assessed by Karnofsky score between Hispanic and non-Hispanic candidates. From a cardiac perspective, Hispanic patients had significantly lower right ventricular systolic pressure.
Time of LT listing psychosocial factors and SDOH
Prevalence of mental health conditions were similar between the two groups. From a substance use perspective, Hispanic patients had significantly lower rates of marijuana use (24.3% vs. 44.9%, p = <0.001) and similar rates of use of tobacco and other illicit substances compared to non-Hispanic individuals. SIPAT scores were similar between Hispanic and non-Hispanic candidates. Among patients listed for ALD, Hispanic patients had significantly lower Alcohol Use Disorder Identification Test (AUDIT) scores and had significantly longer duration from time to last drink to listing (641 days vs. 391 days, p = 0.007). SDOH substantially differed by Hispanic ethnicity with Hispanic patients having fewer years of formal education (p = <0.001), rates of employment (17.9% vs. 32.6%, p = 0.001), annual household income (p = 0.01), and private insurance (26.1% vs. 46.2%), p < 0.001).
Transplantation and waitlist removal
Rates of transplantation did not significantly differ by Hispanic ethnicity (46.9% vs. 46.1%, p = 0.98) (Figure 1). Similarly, time from listing to transplant did not vary based on Hispanic ethnicity (214 days in Hispanic vs. 184.5 days in non-Hispanic candidates, p = 0.12). No significant differences in multiorgan transplantation, use of DCD or high-risk donor organs were noted between Hispanic and non-Hispanic candidates. The majority of grafts were DBD donors. Two living donor grafts were performed in this cohort. LT recipients in the Hispanic cohort were less often male (54.9% vs. 74.4%, p = 0.008), more commonly transplanted for MASH, and had lower biologic MELDNa at time of LT (18 vs. 24, p = 0.003) in the setting of higher HCC indications (40% vs. 23.2%, p = 0.003). Removal from the waitlist also did not significantly differ by Hispanic ethnicity (35% vs. 36.5%, p = 0.87). Indications for removal from the waitlist did not statistically significantly differ, though 60.9% of Hispanic patients were removed due to death or being too sick compared to 44.6% of non-Hispanic patients (p = 0.04, Figure 1).
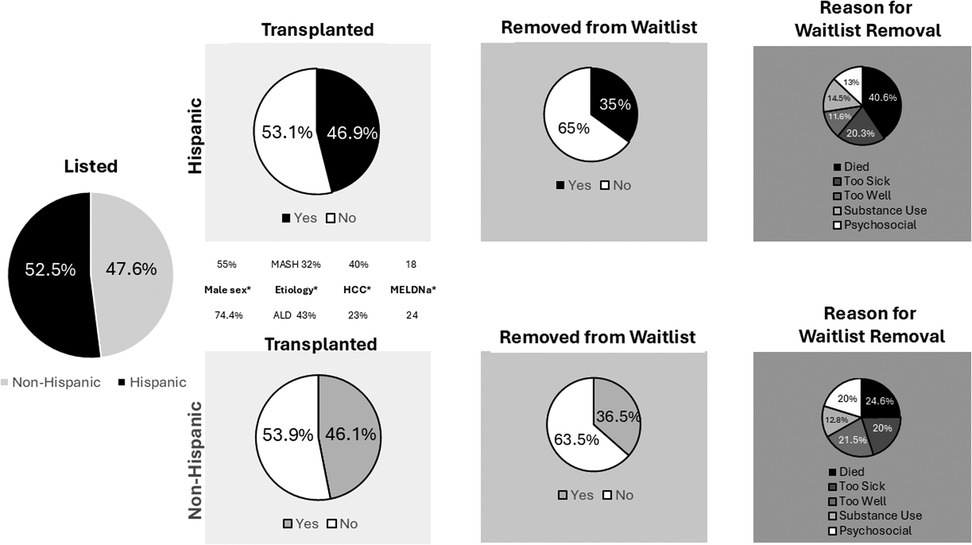
Figure 1. Listing, transplantation and removal from LT waitlist by Hispanic ethnicity. *denotes statistically significant difference in variable between groups.
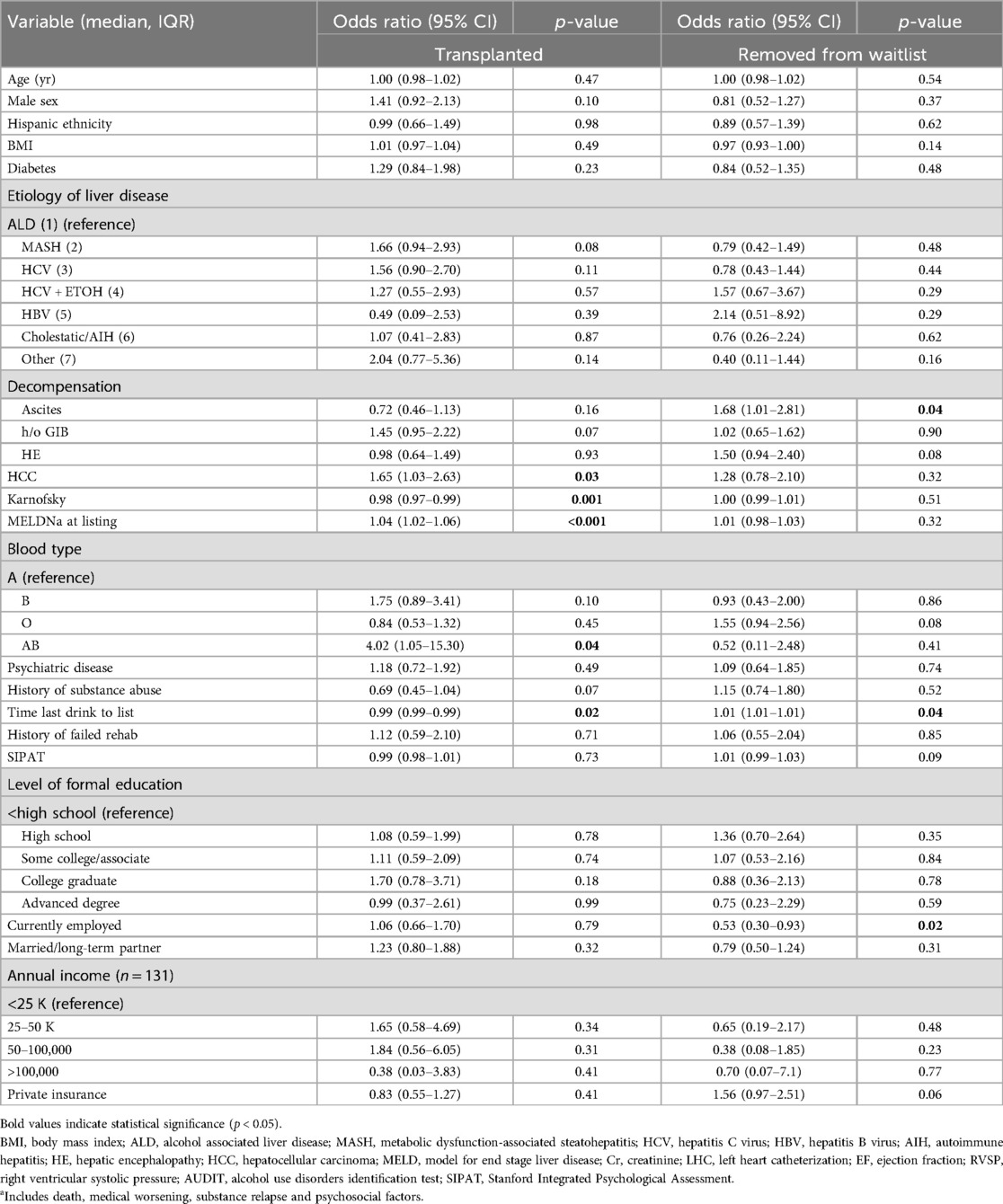
On univariate logistic regression, several characteristics were significantly associated with odds of transplantation (Table 2). The presence of HCC [odds ratio (OR) 1.65, 95% confidence interval (CI) 1.03–2.63], MELDNa at listing (OR 1.04, 95% CI 1.02–1.06), and AB blood type (OR 4.02, 95% CI 1.05–15.3) were all associated with higher odds of LT. Of note, Karnofsky scores were also associated with odds of transplant (OR 0.98, 95% CI 0.97–0.99). The only psychosocial factor associated with odds of LT was time from last drink to listing (OR 0.99, 95% CI 0.99–0.99). For odds of removal from the waitlist, history of ascites (OR 1.68, 95% CI 1.01–2.81), time from last drink to listing (OR 1.01, 95% CI 1.01–1.01) and current employment status (OR 0.53, 95% CI 0.30–0.93) were the only significant factors. On multivariate logistic regression, HCC (OR 10.2, 95% CI 1.15–90.44) was associated with increased odds of transplant (Table 3). The only factor independently associated with odds of removal from the waitlist on multivariate analysis when accounting for baseline differences in the Hispanic vs. non-Hispanic cohorts was employment status.
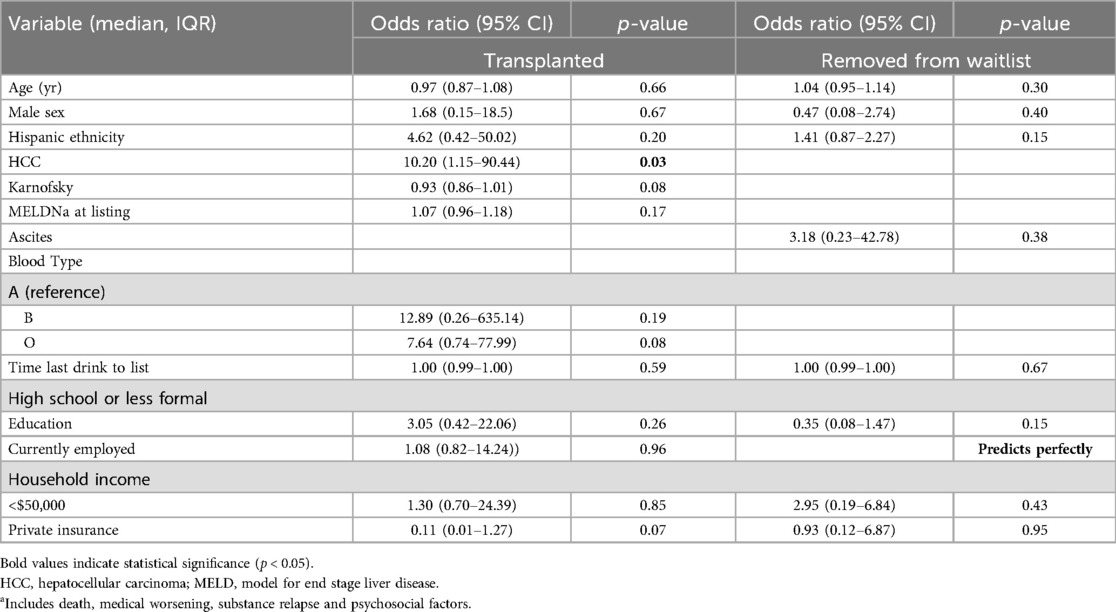
Table 3. Multivariate analysis of correlates of transplant or removal from waitlista including SDOH differences in table 1 by Hispanic ethnicity.
Discussion
Main findings
Analysis of patients listed for LT at a large, academic transplant center with a high density of Hispanic/Latino patients in its referral area demonstrated no significant differences in rates of LT and removal from the LT waitlist for Hispanic compared to non-Hispanic patients. This was despite the Hispanic cohort having statistically significantly higher rates of medical co-morbidities (higher BMI, type II diabetes) and SDOH factors that have been associated with lower access to LT (fewer years of formal education, lower annual income, lower rates of employment and less private insurance). The finding of equitable distribution on the LT waitlist, rates of LT and removal from the waitlist despite these potentially challenging medical and SDOH factors may in part be explained by the protective psychosocial factors noted in the Hispanic group. Further, these comparable findings between Hispanic and non-Hispanic patients despite identified SDOH found among the Hispanic cohort could possibly be explained by the strategic structure of our health system designed to mitigate barriers to access. Studies have shown that the effects of SDOH can vary by region, reflecting differences in local healthcare delivery models, referral patterns, and transplant center practices (15, 16). The single center used for this study has established community outreach programs as well as culturally tailored services, which may explain the apparent attenuation of disparities generally seen in broader national datasets. These services include the use of bilingual navigators, interpreter services, and expedited virtual consult pathways that support earlier and more equitable access to evaluation. Our findings highlight the importance of examining healthcare delivery models that may reduce the effects of SDOH and identifying which specific interventions within this health network have been most impactful, potentially serving as models for broader implementation.
Important differences in referral patterns were noted impacting access to LT, specifically significantly longer duration of time from last drink to listing for Hispanic candidates, highlighting potential biases and SDOH factors contributing to delay in referral for this population or lack of up to date knowledge regarding LT protocols for ALD for referring providers. On multivariate analysis, only HCC predicted odds of transplant whereas only SDOH factors, employment status, predicted odds of removal from the LT waitlist.
In context with current literature
Our findings build on the existing literature by addressing discordant findings regarding distribution on the LT waitlist, rates of LT and removal from the LT waitlist between Hispanic and non-Hispanic LT candidates. Discrepancies in results, particularly of analyses from larger nationwide databases, may reflect lack of more detailed assessments of psychosocial and SDOH factors impacting health equity. Differences in results across studies may also be impacted by comparator groups used with some studies comparing only to non-Hispanic White participants and others having non-Hispanic of any other race/ethnicity as the comparator. In this study, the non-Hispanic cohort consisted of 76% White individuals, with the remaining including Black. Asian and other race/ethnicity. We opted to keep participants from other non-Hispanic ethnicities in the comparator group to enhance power and to ascertain the impact of variables on outcomes of interest by Hispanic ethnicity alone. Our analyses outlined relevant factors that may impact LT candidacy that ultimately were not reflected in significant differences in SIPAT scores. Potential biases in psychosocial assessments and global LT listing patterns were shown in a recent study that found that Hispanic candidates were more likely to be denied listing due to psychosocial concerns compared to non-Hispanic white patients (10).
Implications for clinical care and research
Given the rising burden of MASLD, particularly among Hispanic populations, the implications of our findings warrant further consideration. While this study was not designed to stratify outcomes by liver disease etiology, prior work by our group demonstrated that patients with MASH had similar rates of liver transplantation and waitlist removal compared to other etiologies, but experienced higher waitlist mortality (17). The higher prevalence of MASLD among Hispanic patients may contribute to observed disparities in access and outcomes. These findings underscore the importance of addressing MASLD-related social determinants of health and ensuring equitable transplant evaluation.
Once contributors to health disparities across groups are identified, it is critical to identify pragmatic, actionable interventions to address these factors to improve health equity. Several LT centers have designed programs focused on LT for Hispanic individuals with goals of increasing referral, listing, LT rates and improving long-term clinical outcomes. One such program in Texas resulted in increases in referral for LT, though the proportion of Hispanic patients undergoing LT dropped due to financial barriers (18). Our center does not have any restrictions on accepting public insurance, including Medicaid, in an effort to obviate potential disparities seen in regards to access to transplant and waitlist maintenance. Additionally, our center has implemented a systemwide initiative designed to identify barriers to access and to improve equity. Barriers to access were found to be multifactorial, including both patient-level factors and structural factors within the healthcare system including delays in referral triage, language barriers, inconsistent navigation of the healthcare system, and limited appointment flexibility. As a result, our center has implemented several interventions including virtual expedited consult clinics, self-scheduling portals, expanded interpreter services, and provider-to-provider e-consults that allow primary care physicians to initiate specialty evaluation without requiring in-person visits. These system-level changes have led to measurable improvements in specialty care access at our center and highlight the importance of addressing healthcare delivery, in addition to addressing patient-level factors. Current literature indicates that while some centers have implemented similar initiatives, there is limited research evaluating their effectiveness in significantly increasing transplantation rates among the Hispanic population.
Therefore, these models highlight the potential for transplant centers to identify and systematically address barriers to care and the need to evaluate the effectiveness of such interventions.
From an outcomes viewpoint, these disparities have significant implications as prior studies have shown better post-LT patient and graft survival in Hispanics compared to non-Hispanic LT recipients (5, 19). Similarly, a lower rate of biochemical alcohol relapse has been documented in Hispanic patients compared to White patients, further suggesting disparity in the referral and selection process (20). Future studies are needed to determine whether these better outcomes are secondary to unidentified protective factors in this patient population that may have implications on transplant selection. From a public health viewpoint, it is necessary to identify interventions to not only increase referrals for LT but mechanisms targeted at minimizing SDOH factors impeding LT listing and maintenance on the waitlist.
Strengths and limitations
A main strength of this study is the detailed assessment of both potential risk and beneficial factors impacting LT and waitlist removal. Specifically, we were able to abstract relevant psychosocial and SDOH factors that are frequently excluded or minimally captured in larger databases. Through this methodology we were able to highlight key differences in referral patterns for patients with ALD in Hispanic compared to non-Hispanic patients. An inherent limitation of any retrospective study results from potential missingness in data capture as a result of differential level of detail documented for each patient that was available for abstraction. The overall missingness for each variable of interest was minimal however given the comprehensive chart review performed by experienced research staff who are practitioners in liver transplant. Our transplant program has data from time of referral regarding listing and transplantation status. This was also a single center study from a diverse, large academic transplant center, and thus our findings may not be reflective of other transplant centers with more homogeneous patient populations. Given the high density of Hispanic individuals in our referral area, our center provided an ideal setting to investigate the outcomes of interest for this patient population. Our sample size was modest however, and this may impact the statistical power to detect differences across groups.
Conclusions
In conclusion, in a large, ethnically diverse academic liver transplant center, rates of LT and waitlist removal did not differ by Hispanic ethnicity. Hispanic patients did appear to have delays in referral for ALD compared to non-Hispanic counterparts. Both risk and protective factors were identified in the Hispanic cohort that impact odds of LT. SDOH, particularly employment status, predicted removal from the waitlist, and was more common among Hispanic candidates. Given the increasing burden of MASLD, especially among Hispanic populations, and its strong association with socioeconomic and lifestyle factors, these findings highlight the importance of addressing SDOH that impact transplant access. Tailored, culturally sensitive programs aimed at increasing referral and listing for LT have shown promise for Hispanic patients, though downstream benefits of increased rates of transplantation have thus far remained works in progress. Designing programs that both mitigate risk factors and enhance the benefits of protective characteristics may advance progress towards health equity for Hispanic patients in need of LT.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by UCSD Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because secondary analysis of de-identified data.
Author contributions
MT: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. JP: Writing – review & editing. FD: Data curation, Project administration, Writing – review & editing. KT: Data curation, Writing – review & editing. DA: Data curation, Writing – review & editing. MM: Writing – review & editing. IV: Data curation, Writing – review & editing. VA: Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. MT is supported by the National Cancer Institute of the National Institutes of Health (U54CA285117 and U54CA2851) and ACTRI voucher funding. VA is supported by NIDDK (K23DK119460) and ACTRI voucher funding (UL1TR001442).
Acknowledgments
This manuscript was presented at the American Transplant Congress in June 2024 as a poster Abstract.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction Note
A correction has been made to this article. Details can be found at: 10.3389/frtra.2025.1720964.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. U.S. Census Bureau. Releases 2023 Population Estimates by Demographic Characteristics. U.S. Census Bureau (2024). Available online at: https://www.census.gov/newsroom/press-releases/2024/population-estimates-characteristics.html (Accessed August 19, 2024).
2. Tesfai K, Pace J, El-Newihi N, Martinez ME, Tincopa M, Loomba R. Disparities for Hispanic adults with metabolic dysfunction-associated steatotic liver disease in the United States: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. (2024) 23(2):236–49. doi: 10.1016/j.cgh.2024.06.038
3. Nephew LD, Serper M. Racial, gender, and socioeconomic disparities in liver transplantation. Liver Transpl. (2021) 27(6):900–12. doi: 10.1002/lt.25996
4. Park C, Jones MM, Kaplan S, Koller FL, Wilder JM, Boulware LE, et al. A scoping review of inequities in access to organ transplant in the United States. Int J Equity Health. (2022) 21(1):22. doi: 10.1186/s12939-021-01616-x
5. Goyes D, Danford CJ, Nsubuga JP, Bonder A. Waitlist mortality and transplant free survival in Hispanic patients listed for liver transplant using the UNOS database. Ann Hepatol. (2021) 23:100304. doi: 10.1016/j.aohep.2021.100304
6. Warren C, Carpenter AM, Neal D, Andreoni K, Sarosi G, Zarrinpar A. Racial disparity in liver transplantation listing. J Am Coll Surg. (2021) 232(4):526–34. doi: 10.1016/j.jamcollsurg.2020.12.021
7. Nguyen GC, Segev DL, Thuluvath PJ. Racial disparities in the management of hospitalized patients with cirrhosis and complications of portal hypertension: a national study. Hepatology. (2007) 45(5):1282–9. doi: 10.1002/hep.21580
8. Bryce CL, Angus DC, Arnold RM, Chang CC, Farrell MH, Manzarbeitia C, et al. Sociodemographic differences in early access to liver transplantation services. Am J Transplant. (2009) 9(9):2092–101. doi: 10.1111/j.1600-6143.2009.02737.x
9. Yilma M, Kim NJ, Shui AM, Tana M, Landis C, Chen A, et al. Factors associated with liver transplant referral among patients with cirrhosis at multiple safety-net hospitals. JAMA Netw Open. (2023) 6(6):e2317549. doi: 10.1001/jamanetworkopen.2023.17549
10. Deutsch-Link S, Bittermann T, Nephew L, Ross-Driscoll K, Weinberg EM, Weinrieb RM, et al. Racial and ethnic disparities in psychosocial evaluation and liver transplant waitlisting. Am J Transplant. (2023) 23(6):776–85. doi: 10.1016/j.ajt.2023.01.011
11. Quillin RC 3rd, Wilson GC, Wima K, Hohmann SF, Sutton JM, Shaw JJ, et al. Neighborhood level effects of socioeconomic status on liver transplant selection and recipient survival. Clin Gastroenterol Hepatol. (2014) 12(11):1934–41. doi: 10.1016/j.cgh.2014.05.020
12. Ross K, Patzer RE, Goldberg DS, Lynch RJ. Sociodemographic determinants of waitlist and posttransplant survival among end-stage liver disease patients. Am J Transplant. (2017) 17(11):2879–89. doi: 10.1111/ajt.14421
13. Robinson A, Hirode G, Wong RJ. Ethnicity and insurance-specific disparities in the model for end-stage liver disease score at time of liver transplant waitlist registration and its impact on mortality. J Clin Exp Hepatol. (2021) 11(2):188–94. doi: 10.1016/j.jceh.2020.07.011
14. Mansour MM, Fard D, Basida SD, Obeidat AE, Darweesh M, Mahfouz R, et al. Disparities in social determinants of health among patients receiving liver transplant: analysis of the national inpatient sample from 2016 to 2019. Cureus. (2022) 14(7):e26567. doi: 10.7759/cureus.26567
15. Yilma M, Dalal N, Wadhwani SI, Hirose R, Mehta N. Geographic disparities in access to liver transplantation. Liver Transplant. (2023) 29(9):987–97. doi: 10.1097/LVT.0000000000000182
16. Zhou K, Lit A, Kuo LS, Thompson LK, Dodge JL, Mehta N, et al. Neighborhood-level social determinants of health and waitlist mortality for liver transplantation: the liver outcomes and equity index. Transplantation. (2024) 108(7):1558–69. doi: 10.1097/TP.0000000000004888
17. Torosian K, Delebecque F, Arellano D, Vodkin I, Ajmera V, Tincopa M. Association of clinical, psychosocial, and social determinants of health factors and liver transplantation and waitlist removal for MASH. Transplant Direct. (2025) 11(5):e1791. doi: 10.1097/TXD.0000000000001791
18. Kodali S, Mobley CM, Brombosz EW, Lopez A, Graves R, Ontiveros J, et al. Effect of a Hispanic outreach program on referral and liver transplantation volume at a single center. Transpl Immunol. (2024) 84:102034. doi: 10.1016/j.trim.2024.102034
19. Thuluvath PJ, Amjad W, Zhang T. Liver transplant waitlist removal, transplantation rates and post-transplant survival in Hispanics. PLoS One. (2020) 15(12):e0244744. doi: 10.1371/journal.pone.0244744
Keywords: health equity, Hispanic, mortality, cirrhosis, referral
Citation: Tincopa M, Pace JL, Delebecque F, Torosian K, Arellano D, Martinez ME, Vodkin I and Ajmera V (2025) Disparities in liver transplant waitlist characteristics and outcomes among Hispanic compared to non-Hispanic adults. Front. Transplant. 4:1592516. doi: 10.3389/frtra.2025.1592516
Received: 12 March 2025; Accepted: 30 July 2025;
Published: 20 August 2025;
Corrected: 21 October 2025.
Edited by:
Giovanni A. Roldan, University of Minnesota Health Sciences, University of Minnesota Medical Center, United StatesReviewed by:
Paolo De Simone, University of Pisa, ItalyDavid Cobourn Mulligan, Yale University, United States
Deborah Verran, Consultant, Sydney, Australia
Copyright: © 2025 Tincopa, Pace, Delebecque, Torosian, Arellano, Martinez, Vodkin and Ajmera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Monica Tincopa, bXRpbmNvcGFAaGVhbHRoLnVjc2QuZWR1
 Monica Tincopa
Monica Tincopa Jordan L. Pace
Jordan L. Pace Fanny Delebecque1
Fanny Delebecque1 Maria Elena Martinez
Maria Elena Martinez