- 1Department of Psychiatry, Faculty of Medicine Universitas Indonesia—Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 2Doctoral Program in Medical Sciences, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia
- 3Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
- 4Department of Child Health, Faculty of Medicine Universitas Indonesia—Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 5Department of Dermatovenereology, Faculty of Medicine Universitas Indonesia—Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 6Department of Clinical Pathology, Faculty of Medicine Universitas Indonesia—Cipto Mangunkusumo Hospital, Jakarta, Indonesia
- 7Department of Psychiatry, Faculty of Medicine Universitas Padjajaran—Hasan Sadikin Hospital, Bandung, Indonesia
- 8Department of Child Psychiatry, University of Turku, Turku, Finland
Introduction: Transitional-aged youths (17-to-24-years-old) are prone to mental-health problems. Students in higher education, especially medical students, are more exposed to stressors and thus need training to increase resilience. However, there have been limited mental-health strengthening modules specifically developed for medical students of transitional age, and none in Indonesia. This study intends to test the effectiveness of an online mental-health strengthening module in altering resilience.
Methods: A pragmatic randomized trial with repeated measurements was employed to evaluate biopsychosocial outcomes of resilience. The intervention module was delivered in 4 weeks to 105 eligible students. Participants were divided into intervention group (n = 52) and control group (n = 53). Outcomes were measured in the 4th, 8th, and 12th weeks. Primary outcome was resilience level as measured by Connor-Davidson Resilience Scale (CD-RISC). Perceived Stress Scale (PSS), Depression Anxiety Stress Scale (DASS) were utilized to measure stress, depression and anxiety. Knowledge and attitude toward mental-health were also measured through validated questionnaires. Stress levels of participants were measured biologically by measuring salivary cortisol and alpha-amylase levels at the baseline and 12th-week.
Results: Compared to the control group, there were no significant difference in resilience score of the intervention group compared to control group [F(1, 103) = 2.243, P = .137]; however, there was a significant main effect of time [F(3, 309) = 18.191, P < .001] and interaction effect between intervention and time in resilience score [F(3, 309) = 5.056, P = .002]. Additionally, compared to the control group, there were significant increases in knowledge [F(1, 103) = 66.805, P < .001], attitudes and behavior towards mental-health [F(1, 103) = 5.191, P = .025], and a significant decrease in stress perception score [F(1, 103) = 27.567, P < .001]. The mean salivary delta cortisol during pre-test and post-test at week 12 in the intervention group showed significant difference (P < .001). However, there was no significant difference in the mean delta salivary alpha-amylase between pre-test and post-test at week 12, both in the intervention and control groups.
Conclusion: The mental-health strengthening module was accepted and applicable to first-year medical students and was found to be effective in increasing resilience from various biopsychosocial aspects. It is also advisable to have similar modules throughout the medical school to maintain sustainability.
1. Introduction
Transitional-aged youth has been referred to as the population that falls under the period between late adolescents (17-to-19 years old) until early adulthood (21-to-24 years old) (1). In this transitional period to adulthood, youths may face multiple internal and external pressures. Internally, they are processing their self-image, physical and emotional changes. Externally, they might have family, peer, academic, or other life events-related conflicts (1, 2). With all these conditions, adolescents in transitional age are more likely to experience mental health problems (3). In the United States, 50 to 75% of anxiety disorders, mood disorders, and substance abuse disorders start at the age of 14 to 24 (4). Immaturity in managing emotions and solving problems might also lead youths to do high-risk behaviors such as alcohol or substance abuse, unsafe sex, or self-harm practice. Therefore, this period is a critical period for shaping youths' ability to deal with stress and the capacity to regulate emotions (2).
A common major stressor in this age group is entering college or university due to the pressure to change their ways of learning and become more self-directed (3). In Indonesia, among university students aged 16 to 24 years, more than 90% of 393 participants expressed they had financial or academic difficulties, felt lonely, and anxious (5). First-year university students stand at the intersection of physical, psychological, and environmental changes that potentially increase their stress levels (6–10). Mental health problems in university students vary between 10% to 85%, with depression and anxiety as the most common disorders reported (11). Unattended mental health problems can lead to serious consequences that affect youths' ability to live fulfilling lives in the future (12). Therefore, preventing the occurrence of serious mental health difficulties is imperative.
Resilience has been defined as a process of good adaptation to adversity, trauma, tragedy, threats, and significant sources of stress, for example, family or relationship problems, serious health problems, and work or economic environment-related stress (13, 14). Resilience is complex, multidimensional, and dynamic. It is important to note that a healthy adaptation to stress or resilience depends not only on the individual but also on the available sources of support, namely family, friends, groups, or organizations, and depends on culture, religion, community, society, and government (15, 16). Strong resilience has been linked to reduced psychological stress, increased life satisfaction, increased happiness, improved quality of life, reduced anxiety symptoms, and improved overall health (17, 18).
Resiliency training has been conducted for children and adolescents in families, schools, and community-based settings. Programs focusing on transitional youth have been developed in high-income countries and regions such as Finland, Canada, the United States, Australia, Ireland, and Asia-Pacific (19–22). However, it has not been as well researched in low-and-middle-income countries. Furthermore, in Indonesia, a country with a high population of youths, only one large-scale resiliency training program was delivered. It focused more on early adolescents in junior high schools (23). Currently, in Indonesia, no mental strengthening intervention specifically helps late adolescents face life challenges in the transition period to adulthood. Existing mental health strengthening interventions focus more on mental disorders or psychotherapy modules for specific disorders. No mental health strengthening module explicitly prepares adolescents of transition age to enter the higher education environment and the common problems often faced in such settings. With the many pressures faced by youths transitioning to adulthood in university settings, it is important to develop a resilience-based mental health training program embedded in the academic setting.
In Indonesia, medical school programs usually begin right after graduating from high school. Students in medical schools have been found to experience higher levels of stress. The resilience of medical students had been found to be lower than that of the general population in a study from Canada, stating that medical students have higher stress and lower resilience than their peers in the general population (17, 18). Thus, developing and testing the effectiveness of an online mental health strengthening module that promotes resilience in transitional-aged youth medical students is timely. To date, there is no resiliency training module specifically designed for early-year medical students in the Indonesian context. This study aimed to investigate whether a contextually adapted resiliency module delivered through online discussions and self-learning using a website can influence transitional-aged youths' resilience and mental health biopsychosocial outcomes in an Indonesian medical school setting.
2. Materials and methods
2.1. Study design
The study employed a pragmatic randomized trial design with repeated outcome measurements. Participants were divided into two groups: intervention and control groups. Outcomes for both groups were assessed at baseline, immediately at post-intervention (the 4th week), then at follow-up on the 8th and the 12th week. The study was conducted at the Faculty of Medicine, Universitas Indonesia, from August 2021 to January 2022.
2.2. Ethics approval
The study received full ethical approval from the Health Research Ethics Committee, Faculty of Medicine, Universitas Indonesia, with the protocol number Health Research Ethics Committee, Faculty of Medicine, University of Indonesia, numbered 20-05-0538 (KET-527/UN2.F1/ETIK/PPM.00.02/2020).
2.3. Sample size
The sample size was calculated to estimate the difference between the means of two independent groups (24). Based on the results of a previous resiliency-based intervention on transitional-aged youths (25), we expect a difference in means (d) of 7.6 with a standard deviation (σ) of 13. With a 5% level of significance and 80% power, with the formula:
we calculated that a minimum of 46 subjects was required for each group. To anticipate the chance of a 10% drop-out, the minimum number of subjects per group was recalculated, and the minimum target was 52 subjects per group.
2.4. Recruitment and selection
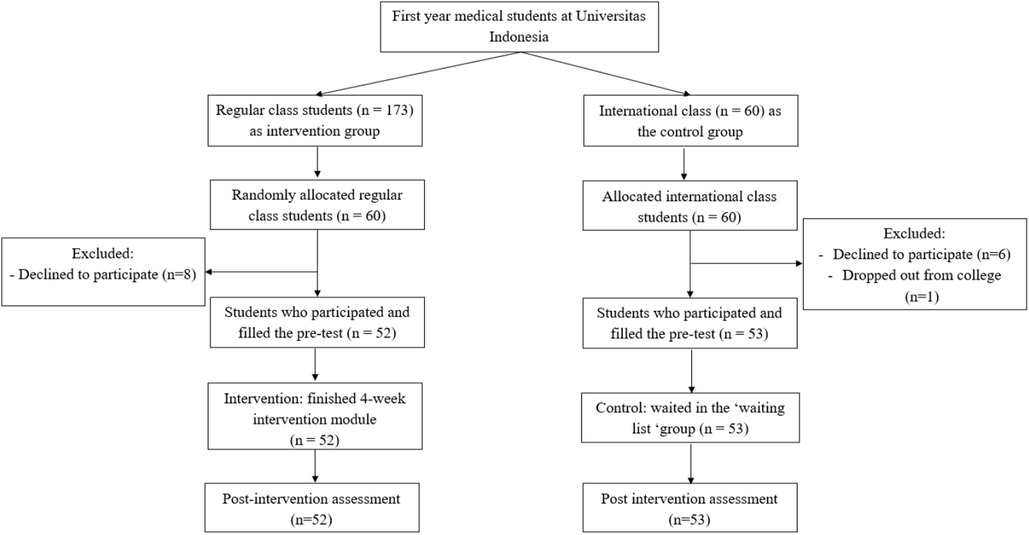
Participants were recruited from the first-year medical students' cohort at Universitas Indonesia. The detailed recruitment process is outlined in Figure 1. There were two classes at the Faculty of Medicine: regular and international. At first, using randomizer.org, the regular class was assigned as the pool to choose participants in the intervention group, while the international class was the pool for the control group. Then, to meet the sample size, 60 students were randomly picked from the 173 students in the regular class to be recruited to join the intervention. Eight students declined; thus, 52 students consented and participated in the intervention group. All 60 students in the international class were recruited to be in the control group, but 1 student dropped out, and 6 students declined. Thus, there were 53 students consented to be in the control group. Reasons for declining include health conditions, feeling unprepared to join an additional activity, or living in another city or country with a different time zone. All other remaining students were invited to join the module after this study had finished.
2.5. Intervention
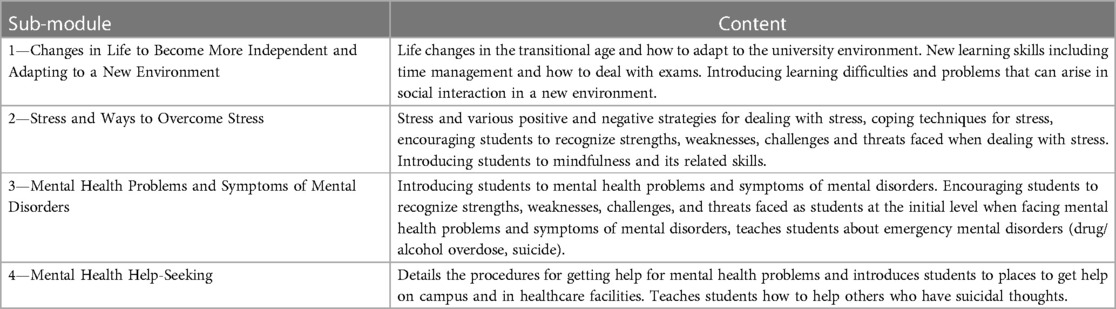
For the intervention group, the participants joined the “Transition and Adaptation towards Resiliency” module. The module was developed through the creation and subsequent adaptations of previous resiliency-based interventions gathered through literature review and qualitative consultations with key experts and the previous cohort of first-year medical students. The qualitative phase of the module development was intended to contextualize the intervention. The content for the module is presented on a website created specifically for the module (https://modultransisi.id/ in Indonesian, a snippet of the module in English is captured in Supplementary Material). Table 1 presents the contents of the module.
The module intervention activities were guided online by five facilitators consulted previously during the module development. The criteria for becoming a facilitator in this module is that of a medical teacher who has been a facilitator in other learning experiences. The facilitators have been given the Module Facilitators Guidebook and access to the module website.
The module is divided into 4 submodules and delivered in 4 weeks. To complete the module, students need to participate in 8 online discussion sessions. They were required to join the online opening session (through Zoom meeting) and subsequent twice-weekly meetings.
In general, the structure and schedules of the activities of each sub-module was as follows:
1. First meeting for 90 min:
- Explaining the general overview of the sub-module topic.
- Explaining self-study techniques.
2. Independent learning through the website for a week.
3. Second meeting after 1 week for 90 min:
- Reflection of participants after participating in independent learning activities in small groups.
- Summary and reinforcement of learning objectives.
Week 1: Opening (first meeting of submodule 1), independent learning submodule 1.
Week 2: Second meeting of Submodule 1, first meeting of submodule 2, independent learning submodule 2.
Week 3: Second meeting of Submodule 2, first meeting of submodule 3, independent learning submodule 3.
Week 4: Second meeting of Submodule 3, first meeting of Submodule 4, independent learning submodule 4.
Week 5: Closing (second meeting of Submodule 4).
The opening of the module was attended by the research team, 52 students, and 5 facilitators. In the opening session, participants were introduced to the overview of the module and how to use the website for self-study by the facilitators. Then they were introduced to the first sub-module content and were divided into 5 groups for small-group discussions of the topic. The facilitators guided the small group discussions to further discuss student experiences on the topics. At the end of the session, they return to the main room to be notified about the self-study task.
The second meeting of each sub-module is held after one week of independent study activities. The activity begins with opening statements in the large group, after which students will enter small group discussions with their respective facilitators. Small group activities take place in breakout rooms in the form of self-reflective discussions and material from the website that students have studied and worked on for the previous week. The facilitators also assess student activity individually and in groups. The group discussion lasted for 45 min. The activity ended with a large group plenary for 35 min to discuss the results of each group's discussion, providing feedback from the facilitators and conclusions.
2.6. Measured outcomes
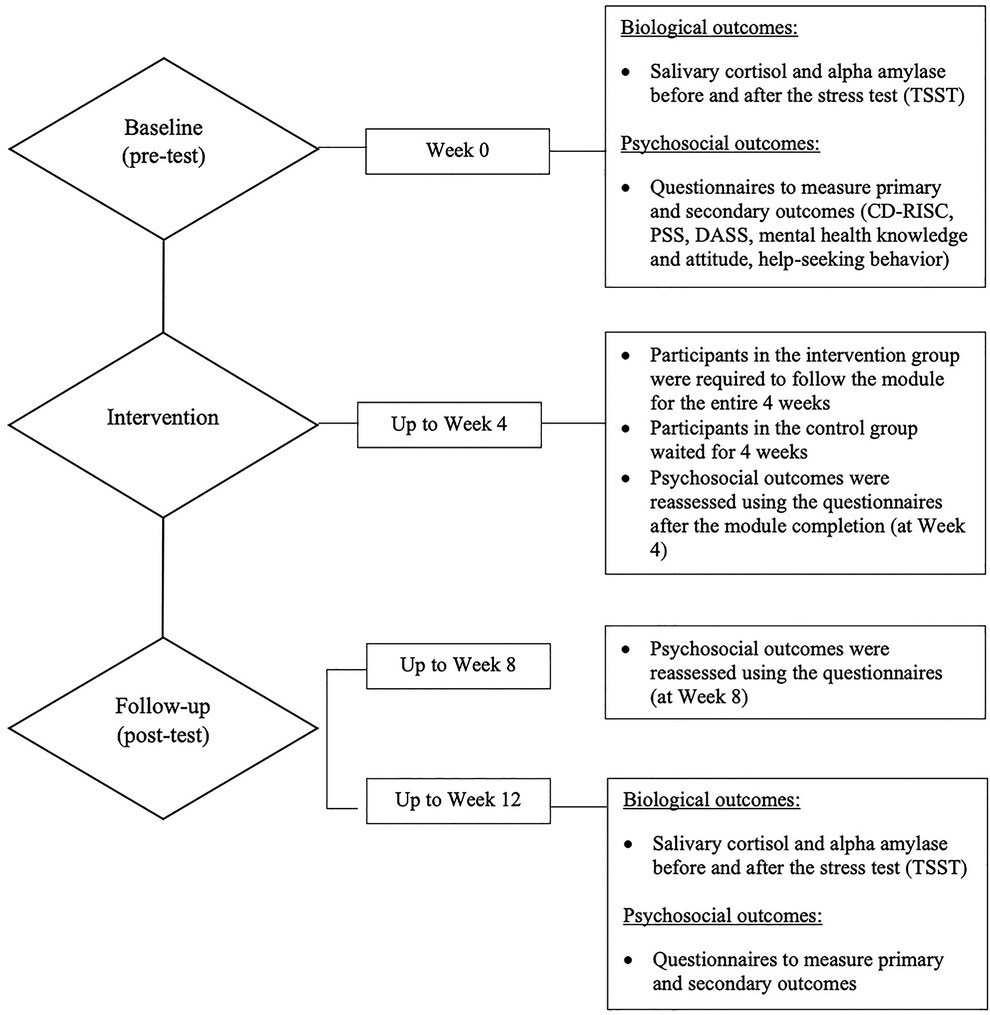
Effectiveness was investigated through pre-and-post biopsychosocial outcomes measurements. Figure 2 will elaborate when and which outcomes were assessed during the trial.
2.6.1. Primary outcome measure
The Connor-Davidson Resilience Scale (CD-RISC) was utilized to measure the participants' resiliency levels (26). The CD-RISC uses a 5-point scale (0 = strongly disagree to 4 = strongly agree) and a higher score indicates a higher resiliency level. For this study, the 10-item version, which has been validated in Indonesian, was used (27).
2.6.2. Secondary outcome measures
The perceived stress scale (PSS), which has been translated and validated in Indonesian, was used to measure the participants' stress perceptions in the last month (28, 29). The PSS has a 5-point scale (0 = never to 4 = very often).
To assess participants' mental health problems, the Depression Anxiety Stress Scale (DASS) was utilized to measure the participants' depression and anxiety symptoms in the past week. The 21-item version has been translated and validated previously in an Indonesian setting (30, 31). The DASS uses a 4-point scale (0 = never to 3 = very often). The depression score is obtained by adding item numbers 3, 5, 10, 13, 16, 17, and 21. The anxiety score is obtained by adding item numbers 2, 4, 7, 9, 15, 19, and 20. Meanwhile, the stress score is obtained from numbers 1, 6, 8, 11, 12, 14, and 18.
The knowledge and attitude toward mental health questionnaires translated, adapted, and validated for the study were used to measure participants' knowledge and attitude toward mental health (32).
To assess stress levels biologically, participants' salivary cortisol and alpha-amylase levels were measured at the baseline (week 0) and at the 12th-week follow-up. Cortisol and alpha-amylase were measured twice in baseline and twice in week 12 by administering a standardized stress test called the Trier Social Stress Test (TSST). Each participant was tasked to perform a presentation task in front of a scientific forum and an arithmetic task (33, 34). Before and after the TSST, the participants collected their saliva samples. The measured baseline cortisol (S1) and alpha-amylase (S1) before the TSST were compared with post-TSST cortisol (S2) and alpha-amylase (S2) to obtain a delta value (S2 – S1) for individual levels after the test.
The Trier Social Stress Test (TSST) and collection of the salivary samples were virtually directed through a video conference platform. All participants received the sampling tools and an instructional video that guides them on collecting and sending their salivary samples. Then, the TSST was conducted by presenting in front of a board of examiners and an arithmetic test for 45 min between 7 AM and 12 PM (local time) considering the natural cortisol cycle. Samples were received and analyzed by the Integrated Laboratory Installation, Clinical Pathology Department, Cipto Mangunkusumo Hospital (RSCM), Jakarta.
2.7. Statistical analysis
Data collected from the results of laboratory tests and questionnaires were analyzed using the SPSS version 20.0 program. Normality tests with Kolmogorov-Smirnov were conducted on all outcome measures. For normal distribution data, repeated measures ANOVA were carried out to analyze difference in mean scores between intervention group and control group across all time points (main effect), and to assess any interaction effect between within-subjects factor (time) and between-subjects factor (intervention). If the normality of data distribution was violated, a non-parametric Friedman test was carried out instead to analyze the main effect. Bonferroni post-hoc analyses between time-points would be conducted if there is significant interaction effect between time and intervention.
3. Results
3.1. Participants' characteristics and baseline measurement
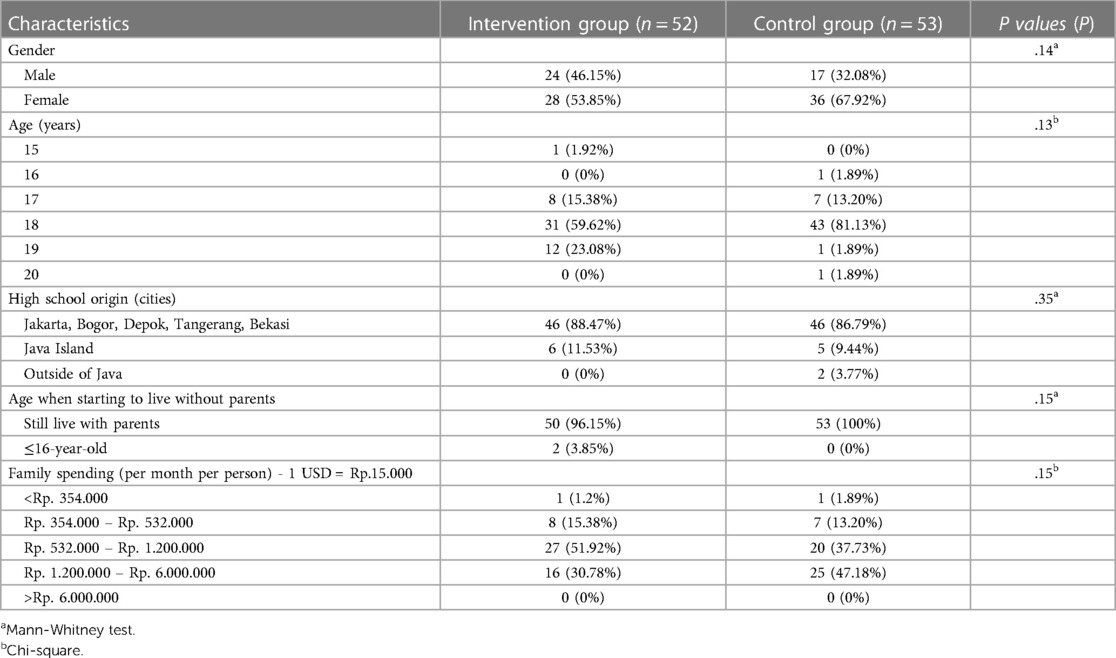
In total, 105 students participated in the study. Analysis of their demographic characteristics (Table 2) revealed no significant differences between the two groups.
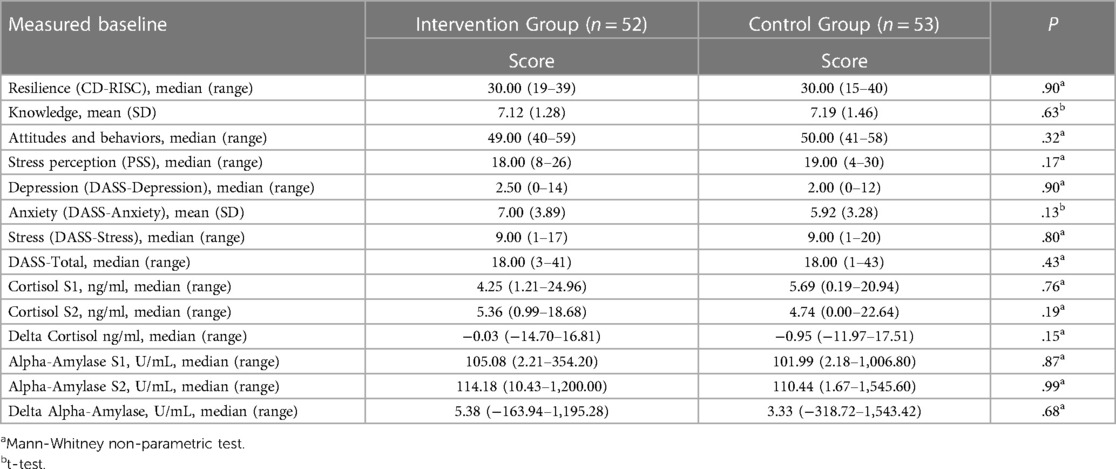
From the baseline data from the pre-test questionnaires, there was no significant difference in biological parameters (cortisol and alpha-amylase), as well as of the primary (CD-RISC) psychosocial parameter and the secondary psychosocial parameters (knowledge, attitude and behavior, stress perception, DASS score) between subjects in the intervention group and the control group. The initial profile of the participants in the intervention and control groups can be seen in Table 3. Only knowledge and DASS-Anxiety variables were normally distributed, presented as mean, and analyzed using t-test; other variables were not normally distributed, presented as median and analyzed with non-parametric test (Mann Whitney test).
3.2. Primary outcome
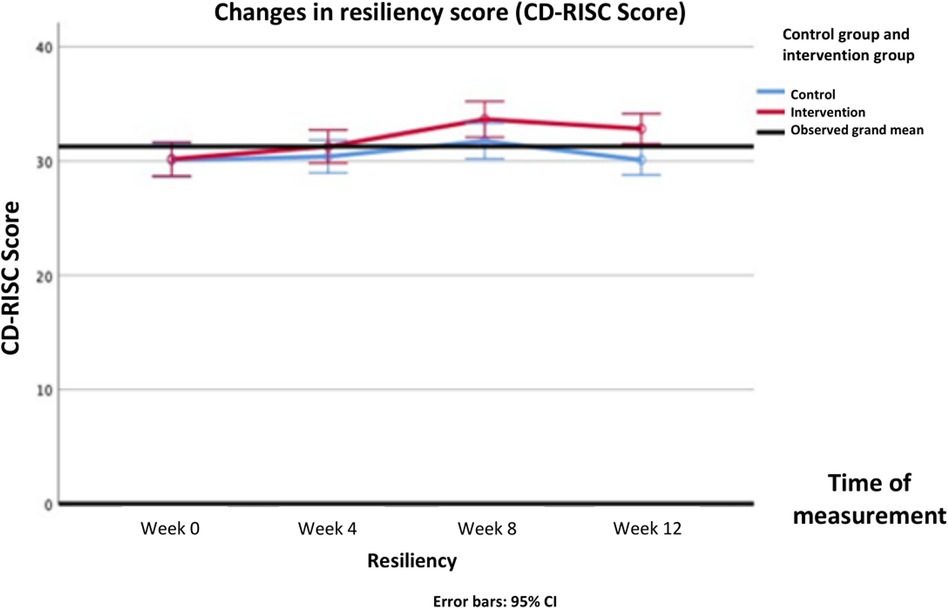
Normality test showed that the data had a normal distribution (P > .05), thus parametric tests were used. Analysis of CD-RISC scores of group main effect using repeated measures ANOVA revealed there was no significant increase in the resilience score in the intervention group (Δ mean [95%CI] = 1.40 [−0.45–3.26]; F(1, 103) = 2.243, P = .137) compared to the control group. However, significant main effect of time [F(3, 309) = 18.191, P < .001] and interaction effect between intervention and time [F(3, 309) = 5.056, P = .002] was observed in the CD-RISC scores. Bonferroni post-hoc analyses of CD-RISC score differences between group in each time-point showed significant difference in week 12 (Δ mean [95%CI] = 2.73 (0.87—4.59); P = .004). The changes in CD-RISC scores from the pre-test to the 12-week follow-up in both groups can be seen in Figure 3 and Table 4.
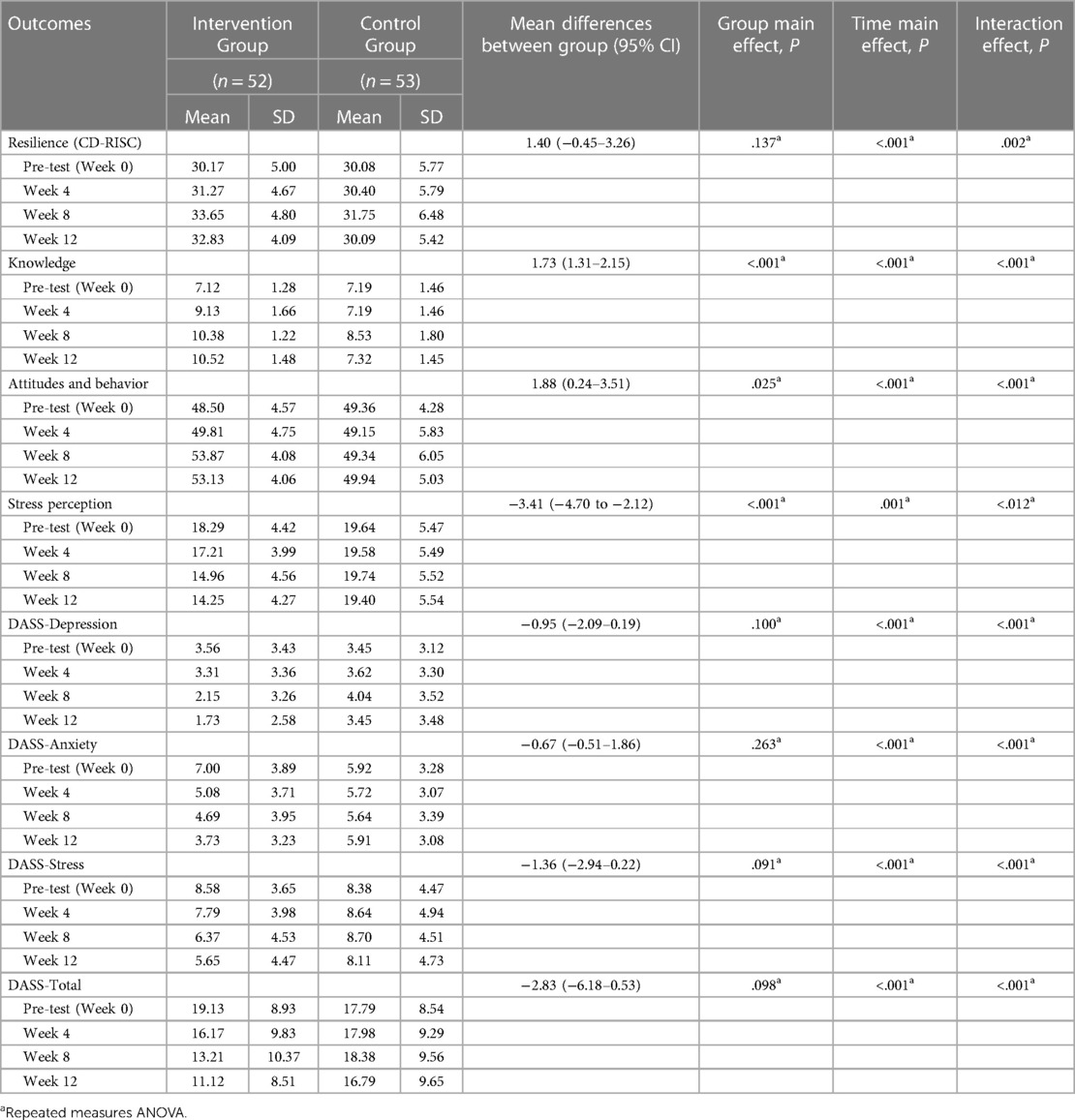
Table 4. Comparison of the psychosocial outcomes of the participants during the pre-test and post-test.
3.3. Secondary outcomes
In all secondary outcome measures, normality tests were conducted and showed that the distribution were normal (P > .05), thus all data are presented in mean and parametric tests were used. Biological parameter analysis of the participants' salivary cortisol and alpha-amylase levels showed there was a significant difference in the mean cortisol delta during the pre-test (Mean 0.12) and post-test (Mean – 3.84) at week 12 (P < .001) in the intervention group. While for the control group, there was no difference in the mean cortisol delta pre-test (Mean −0.82) and post-test (Mean −2.83) (P = .07). For the measurement of alpha-amylase delta biomarker levels, there was no significant difference in the mean at the pre-test and after the 12th week, both in the intervention and control groups. Changes in delta levels of cortisol and alpha-amylase biomarkers during the pre-test and post-test at week 12 can be seen in Figures 4, 5.
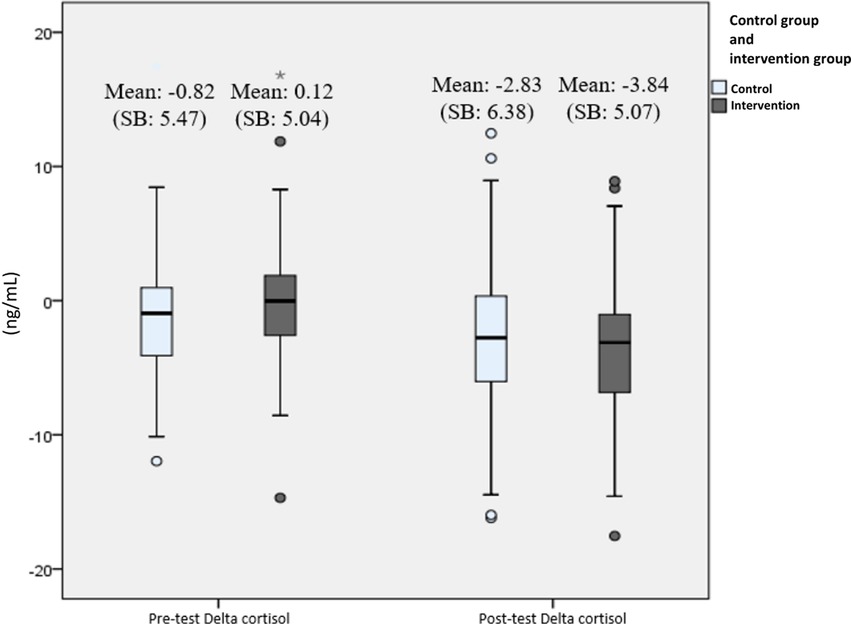
Figure 4. Changes in delta cortisol level (ng/mL) from pre-test to post-test presented with boxplot. The bars represent median and interquartile range, while the tip of the bar represents minimum and maximum value. The spheres represent mild outliers (Q1 – 1.5 * IQR or Q3 + 1.5 * IQR), while the asterisk represent extreme outliers (Q1–3 * IQR or Q3 + 3 * IQR).
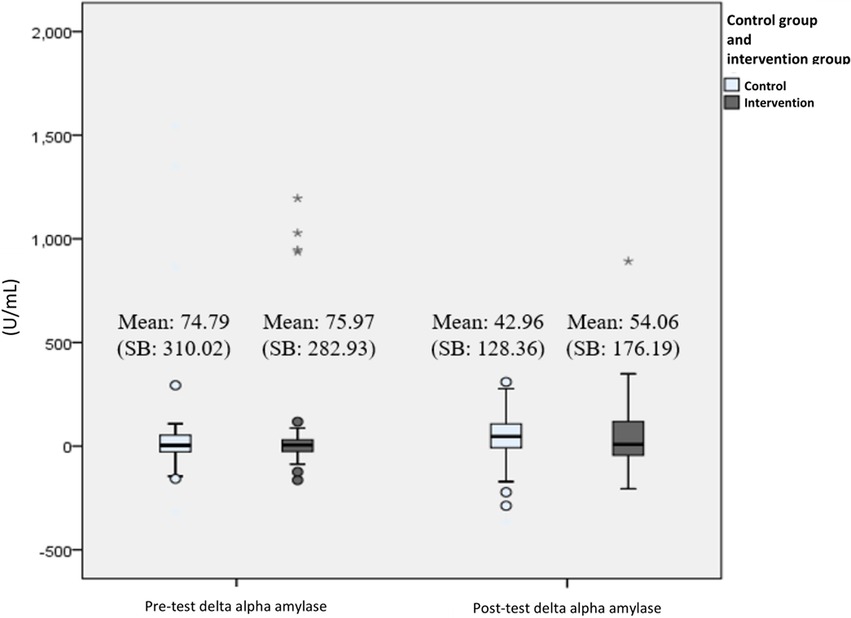
Figure 5. Changes in delta alpha amylase level (U/mL) from pre-test to post-test presented with boxplot. The bars represent median and interquartile range, while the tip of the bar represents minimum and maximum value. The spheres represent mild outliers (Q1–1.5 * IQR or Q3 + 1.5 * IQR), while the asterisk represent extreme outliers (Q1–3 * IQR or Q3 + 3 * IQR).
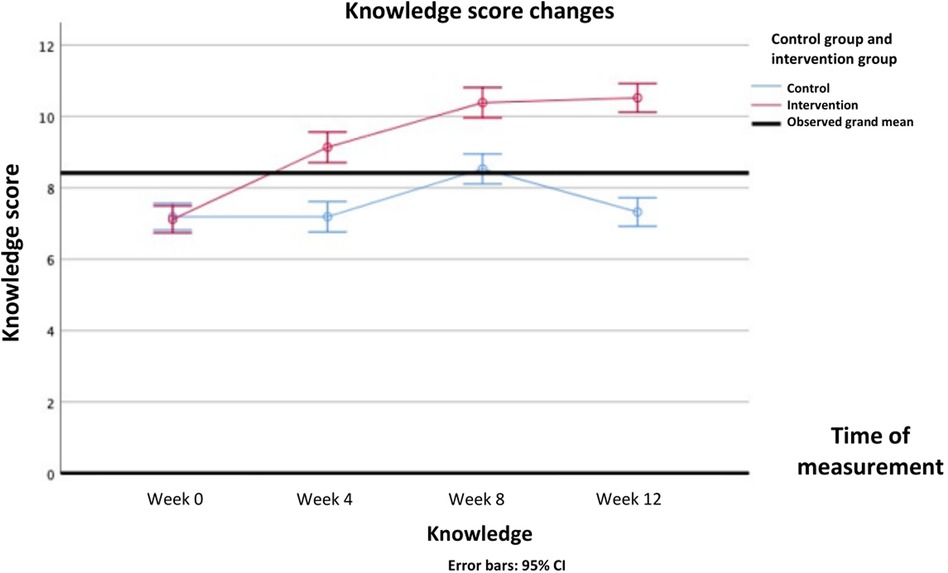
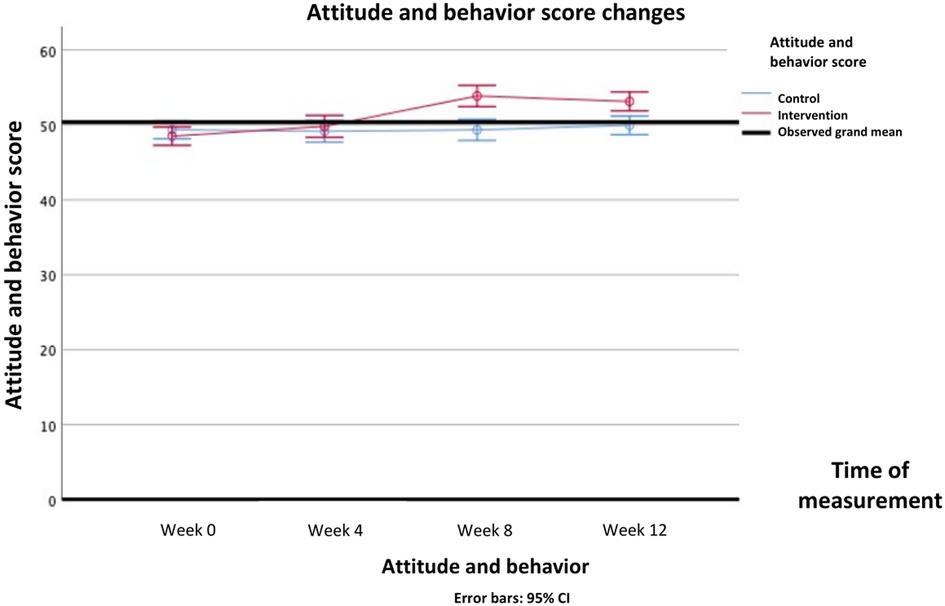
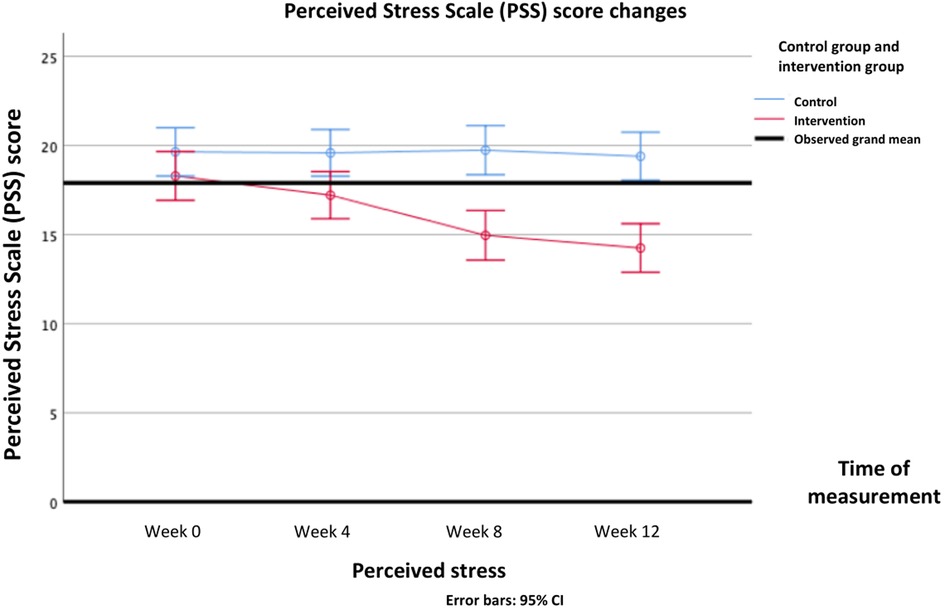
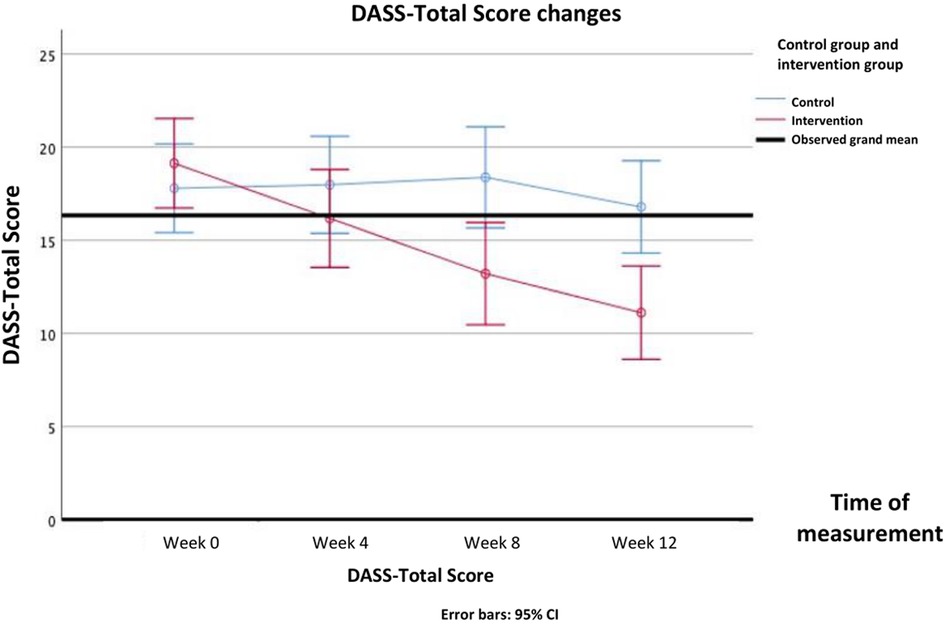
For the psychosocial parameters, analysis using repeated measures ANOVA showed main effects of group on knowledge (Δ mean [95%CI] = 1.73 (1.31—2.15); F(1, 103) = 66.805, P < .001), attitudes and behavior (Δ mean [95%CI] = 1.88 (0.24—3.51); F(1, 103) = 5.191, P = .025), and stress perception (Δ mean [95%CI]=−3.41 (−4.70 to −2.12); F(1, 103) = 27.567, P < .001). Main effects of time were also found on all psychosocial parameters: knowledge [F(3, 309) = 76.459, P < .001], attitudes and behavior [F(3, 309) = 24.908, P < .001], stress perception [F(3, 309)= 5.561, P = .005], DASS-Anxiety [F(3, 309) = 13.729, P < .001], DASS-Depression [F(3, 309) = 7.018, P < .001], DASS-Stress [F(3, 309) = 13.729, P < .001], and DASS-Total [F(3, 309) = 23.515, P < .001].
Interaction effects between intervention and time were found on all secondary psychosocial outcomes: knowledge [F(3, 309) = 83.700, P < .001], attitudes and behavior [F(3, 309) = 36.214, P < .001], stress perception [F(3, 309)= 6.970, P < .001], DASS-Anxiety [F(3, 309) = 33.384, P < .001], DASS-Depression [F(3, 309) = 65.223, P = .012], DASS-Stress [F(3, 309) = 26.595, P < .001], and DASS-Total [F(3, 309) = 39.229, P < .001]. In post-hoc analysis, knowledge scores started to improve significantly after 4th week and forth, while attitude and behavior began to improve after 8th week and forth. Stress perception began to decrease in the 4th week. Mental health problems assessed by DASS questionnaire, namely depression symptoms and stress improved after 8th week, whereas anxiety symptoms improved after 12th week. The DASS-Total score improved after 8th week. All Bonferroni post-hoc analysis of all the secondary psychosocial outcomes score differences between groups in each time point are presented in Table 5.
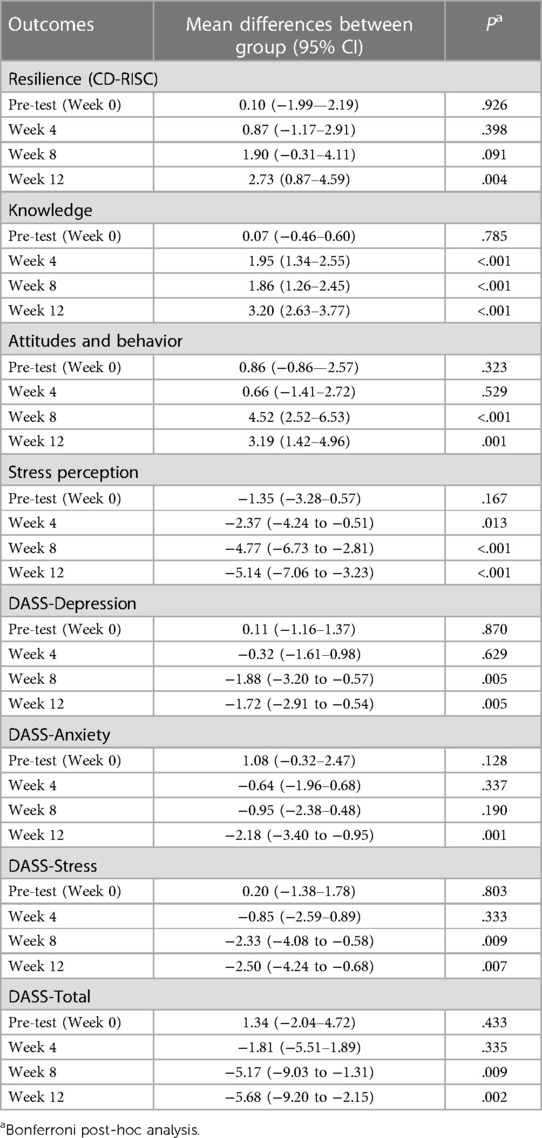
Table 5. Post-hoc analysis of the repeated measures ANOVA of mean score differences between intervention group and control in each time points.
The differences in all resiliency and psychosocial outcomes in the pre-test and post-test in the intervention group and the control group over repeated measurements can be seen in Table 4. The psychosocial profiles of the two groups during the pre-test up to week 12 can be seen in detail in Figures 6–9.
4. Discussion
4.1. Principal results
Improvement in resilience and all secondary psychosocial outcomes (knowledge, attitude and behavior on mental health; stress perception; symptoms of depression, anxiety, and stress from DASS questionnaire; and the DASS-total score) on the intervention group compared to the control group after certain time points. The resilience score between groups was not found to be significantly improved until week 8 and is found to be significantly improved on week 12. All the secondary psychosocial outcomes had a significant improvement between groups by week 12, while almost all secondary psychosocial outcomes (except anxiety symptoms) also had a significant improvement by week 8. This finding implies that the effectiveness of this intervention to improve resilience may be seen after application of the module for a certain duration, which is similar to previous studies.
Two studies by Roig et al. (21) and Sood et al. (35) also showed an increase in resilience eight weeks after intervention. Zare et al. (36), where a 60–90-minute mental health module course set for over six weeks successfully increased knowledge, reduced stigmatization towards mental disorders and encouraged strategies for self-help under challenging situations. Attitude and behavior improvement toward mental health was also observed in Milin et al. (37) and Ventieri et al. (38); however, both studies were conducted on school students. Regarding symptoms of anxiety, depression, and stress, findings in this study were also supported by an RCT in Malaysia by Mohammadzadeh et al. (39), which found that a mental health coaching intervention in teenagers succeeded in reducing the level of depression, anxiety, and stress.
This study also analyzed the change in salivary cortisol levels as a secondary outcome, and it was found that the cortisol levels were significantly reduced after the intervention. This finding showed that it is biologically evident that subjects who received mental health strengthening module intervention had better emotion regulation and perception control of stress elicited by TSST. Other studies also found a significant reduction in salivary cortisol levels after TSST following intervention (40, 41). It is already widely known that cortisol levels are correlated with stress, which activates the hypothalamic-pituitary-adrenal (HPA) axis that eventually secretes cortisol in humans.
However, this study found no significant difference between salivary alpha-amylase levels after the intervention in both groups. The results of available studies regarding the correlation of alpha-amylase with resiliency were still mixed (42–46). Although alpha-amylase is a specific biomarker of stress, many factors might interfere with its secretion, such as decreased saliva production and increased protein levels due to food intake.
This study is the first to develop a mental health strengthening module for transitional-age youths in the first year of medical school. This module effectively increases resilience to stress measured from various biopsychosocial aspects, such as cortisol, resilience, knowledge, attitude and behavior, perception of stress, and symptoms of depression, anxiety, and stress. One similar study which developed an intensive mental health education module for the first-year medical student was conducted in China. The module was done over an 8-week interval with 90 min sessions per week, resulting in a significant decline in psychological distress and academic burnout while increasing life satisfaction levels (47). This study showed that even with a shorter duration (4 weeks), the module could achieve a similar outcome compared to a longer duration module.
4.2. Limitations
This study did not limit the stress exposure experienced by students during the academic schedule while being enrolled in this study. Additionally, by the 12th week of the study, all first-year students were in the final week exam, which might influence the result of the stress biomarker baseline. However, the study outcomes were more contextualized by letting students follow the natural course of university students and take exams as usual. They were closer to the actual setting in which students undergo the adaptation process and face stressors in the university.
5. Conclusion
The four-week online mental health strengthening module was found to have significant effects in improving the resilience of medical students, particularly at the end of the study (week 12), and improving various other psychosocial parameters. The positive results of the intervention require 4–12 weeks to take effect in resilience and all secondary psychosocial parameters. Salivary cortisol levels as a stress biomarker were significantly reduced following the intervention.
In order to maintain the sustainability of this module's effectiveness, it is highly advisable to have a program aiming to increase knowledge and skills to overcome mental health problems throughout the medical school program. It is essential to disseminate any information regarding help-seeking behavior for students to be more independent without experiencing stigma. In addition, students can be more sensitive to mental health problems, signs, and symptoms encountered by their friends. Thus, they can be more assistive and follow the procedures of seeking help following the module.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The datasets presented in this article are not readily available because participants of this study did not agree for their data to be shared publicly. Requests to access further information about the study should be directed to FK,ZnJhbnNpc2thLmthbGlnaXNAdWkuYWMuaWQ=.
Ethics statement
The studies involving humans were approved by Ethical committee of the Universitas Indonesia Faculty of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
FK, RII, TW and SP designed the study questions and methods. WI, HG, MMP, and VP contributed to the study's design and reviewed the data's interpretation. FK carried out the data collection. FK analyzed the data and wrote the draft of the manuscript. FK, CCM, GWN, RI, BP, NC and TW contributed to finalizing the manuscript. SP, WI, HG, MMP, VP and AS contributed to the interpretation of the data and critically reviewed and approved the final draft of the manuscript. All authors agree to accept responsibility for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
The authors acknowledge the funding received for the study through the grant Hibah PUTI Q2 (NKP-1231/UN2/RST/HKP.05.00/2022) from Universitas Indonesia.
Acknowledgments
The authors would like to thank Stan Kutcher, Marjo Kurki, Sonja Gilbert and all the cross-cultural Transition study group for the rich discussion about mental health literacy and digital intervention program for adolescents. In addition, we would also like to thank the dean of medical faculty of Universitas Indonesia, Prof Ari Fachrial Syam, Prof Suhendro and Prof Harrina Rahardjo, coordinator and secretary of doctoral program in medical science, for all the support. Last but not least, thank you for all medical students in Universitas Indonesia who participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fdgth.2023.1207583/full#supplementary-material
References
1. Eyre O, Thapar A. Common adolescent mental disorders: transition to adulthood. Lancet. (2014) 383(9926):1366–8. doi: 10.1016/S0140-6736(13)62633-1
2. Wilens TE, Rosenbaum JF. Transitional aged youth: a new frontier in child and adolescent psychiatry. J Am Acad Child Adolesc Psychiatry Elsevier. (2013) 52(9):887–90. doi: 10.1016/j.jaac.2013.04.020
3. Heinen I, Bullinger M, Kocalevent R-D. Perceived stress in first year medical students—associations with personal resources and emotional distress. BMC Med Educ. (2017) 17:4. doi: 10.1186/s12909-016-0841-8
4. Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the national comorbidity study-adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. (2010) 49(10):980–9. doi: 10.1016/j.jaac.2010.05.017
5. Kaligis F, Ismail RI, Wiguna T, Prasetyo S, Indriatmi W, Gunardi H, et al. Mental health problems and needs among transitional-age youth in Indonesia. Int J Environ Res Public Health Multidisciplinary Digital Pub Inst. (2021) 18(8):4046. doi: 10.3390/ijerph18084046
6. Chambel MJ, Curral L. Stress in academic life: work characteristics as predictors of student well-being and performance. Appl Psych. (2005) 54(1):135–47. doi: 10.1111/j.1464-0597.2005.00200.x
7. Chiauzzi E, Brevard J, Thum C, Decembrele S, Lord S. MyStudentBody-Stress: an online stress management intervention for college students. J Health Commun. (2008) 13(6):555–72. doi: 10.1080/10810730802281668
8. Salanova M, Schaufeli W, Martinez I, Breso E. How obstacles and facilitators predict academic performance: the mediating role of study burnout and engagement. Anxiety Stress Coping. (2010) 23(1):53–70. doi: 10.1080/10615800802609965
9. Shin H, Puig A, Lee J, Lee J, Lee S. Cultural validation of the maslach burnout inventory for Korean students. Asia Pac Educ Rev. (2011) 12:633–9. doi: 10.1007/s12564-011-9164-y
10. Stallman HM, Hurst CP. The university stress scale: measuring domains and extent of stress in university students. Aust Psychol. (2016) 51(2):128–34. doi: 10.1111/ap.12127
11. Marthoenis MI, Fathiariani L, Sofyan H. Prevalence of depression and anxiety among college students living in a disaster-prone region. Alx. J Med Taylor Francis. (2018) 54(4):337–40. doi: 10.1016/j.ajme.2018.07.002
12. Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet Elsevier. (2014) 383(9926):1404–11. doi: 10.1016/S0140-6736(13)62116-9
13. Remschmidt H. Mental health and psychological illness in adolescence. Dtsch Arztebl Int. (2013) 110(25):423–4. doi: 10.3238/arztebl.2013.0423
14. Jaworska N, MacQueen G. Adolescence as a unique developmental period. J Psychiatry Neurosci. (2015) 40(5):291–3. doi: 10.1503/jpn.150268
15. Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. (2004) 59(1):20–8. doi: 10.1037/0003-066X.59.1.20
16. Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. (2012) 338(6103):79–82. doi: 10.1126/science.1222942
17. Saeed AA, Bahnassy AA, Al-Hamdan NA, Almudhaibery FS, Alyahya AZ. Perceived stress and associated factors among medical students. J Family Community Med. (2016) 23(3):166–71. doi: 10.4103/2230-8229.189132
18. Lin YK, Lin C-D, Lin BY-J, Chen D-Y. Medical students’ resilience: a protective role on stress and quality of life in clerkship. BMC Med Educ. (2019) 19(1):473. doi: 10.1186/s12909-019-1912-4
19. Kutcher S, Wei Y, McLuckie A, Bullock L. Educator mental health literacy: a programme evaluation of the teacher training education on the mental health & high school curriculum guide. Adv School Ment Health Promotion Taylor Francis. (2013) 6(2):83–93. doi: 10.1080/1754730X.2013.784615
20. Winzer R, Lindberg L, Guldbrandsson K, Sidorchuk A. Effects of mental health interventions for students in higher education are sustainable over time: a systematic review and meta-analysis of randomized controlled trials. PeerJ. (2018) 6:e4598. doi: 10.7717/peerj.4598
21. Roig AE, Mooney O, Salamanca-Sanabria A, Lee CT, Farrell S, Richards D. Assessing the efficacy and acceptability of a web-based intervention for resilience among college students: pilot randomized controlled trial. JMIR Form Res. (2020) 4(11):e20167. doi: 10.2196/20167
22. Reavley N, Jorm AF. Prevention and early intervention to improve mental health in higher education students: a review. Early Interv Psychiatry. (2010) 4(2):132–42. doi: 10.1111/j.1751-7893.2010.00167.x
23. Departemen Kesehatan Republik Indonesia. Modul pelatihan meningkatkan kesehatan jiwa remaja di sekolah elalui pendidikan kecakapan hidup (life skills education). Jakarta: Depkes RI (2006).
24. Machin D, Campbell MJ, Fayers P, Pinol A. Sample size tables for clinical studies. West Sussex, UK: Blackwell Science (2008). Available at: https://abdn.pure.elsevier.com/en/publications/sample-size-tables-for-clinical-studies (Accessed January 13, 2023) (SBN:978-0-86542-870-6).
25. Rogers D. Does a brief workshop change clinical associate students’ resilience? Afr J Prim Health Care Fam Med. (2016) 8(1):e1–4. doi: 10.4102/phcfm.v8i1.1183
26. Connor KM, Davidson JRT. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18(2):76–82. doi: 10.1002/da.10113
27. Almasyhur AF, Nasrun MW, Kusumadewi I. [The validation study of connor-davidson resilience scale 25 (CD-RISC 25) in Indonesia]. Jakarta: Universitas Indonesia (2021). Available at: https://lib.ui.ac.id/detail?id=20513439&lokasi=lokal (Accessed July 7, 2023).
28. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24(4):385–96. doi: 10.2307/2136404
29. Pin TL. Hubungan Kebiasaan Berolahraga Dengan Tingkat Stres Pada Mahasiswa Fakultas Kedokteran Universitas Sumatera Utara. (2011). Available at: http://repository.usu.ac.id/handle/123456789/31538
30. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd ed Sydney, N.S.W: Psychology Foundation of Australia (1995).
31. Damanik ED. Pengujian reliabilitas, validitas, analisis item dan pembuatan norma depression anxiety stress scale (DASS): Berdasarkan penelitian pada kelompok sampel yogyakarta dan bantul yang mengalami gempa bumi dan kelompok sampel Jakarta dan sekitarnya yang tidak mengalami gempa bumi. Jakarta, Indonesia: Universitas Indonesia (2006). Available at: https://lib.ui.ac.id/detail.jsp?id=94859 (Accessed January 13, 2023).
32. Kaligis F, Ismail RI, Wiguna T, Prasetyo S, Indriatmi W, Gunardi H, et al. Translation, validity, and reliability of mental health literacy and help-seeking behavior questionnaires in Indonesia. Front Psychiatry. (2022) 12:764666. doi: 10.3389/fpsyt.2021.764666 (Accessed January 13, 2023).35115960
33. Rashkova MR, Ribagin LS, Toneva NG. Correlation between salivary alpha-amylase and stress-related anxiety. Folia Med (Plovdiv). (2012) 54(2):46–51. doi: 10.2478/v10153-011-0088-4
34. Birkett MA. The trier social stress test protocol for inducing psychological stress. J Vis Exp. (2011) 56:3238. doi: 10.3791/3238
35. Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: a pilot randomized clinical trial. J Gen Intern Med. (2011) 26(8):858–61. doi: 10.1007/s11606-011-1640-x
36. Zare S, Kaveh MH, Ghanizadeh A, Asadollahi A, Nazari M. Promoting mental health literacy in female students: a school-based educational intervention. Health Education Journal SAGE Publications Ltd. (2021) 80(6):734–45. doi: 10.1177/00178969211013571
37. Milin R, Kutcher S, Lewis SP, Walker S, Wei Y, Ferrill N, et al. Impact of a mental health curriculum on knowledge and stigma among high school students: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2016) 55(5):383–91. doi: 10.1016/j.jaac.2016.02.018
38. Ventieri D, Clarke DM, Hay M. The effects of a school-based educational intervention on Preadolescents’ knowledge of and attitudes towards mental illness. Adv Sch Ment Health Promot. (2011) 4(3):5–17. doi: 10.1080/1754730X.2011.9715632
39. Mohammadzadeh M, Awang H, Ismail S, Shahar HK. Improving emotional health and self-esteem of Malaysian adolescents living in orphanages through life skills education program: a multi-centre randomized control trial. PLOS ONE Public Lib Sci. (2019) 14(12):e0226333. doi: 10.1371/journal.pone.0226333
40. Mikolajczak M, Roy E, Luminet O, de Timary P. Resilience and hypothalamic-pituitary-adrenal axis reactivity under acute stress in young men. Stress. (2008) 11(6):477–82. doi: 10.1080/10253890701850262
41. Gaab J, Blättler N, Menzi T, Pabst B, Stoyer S, Ehlert U. Randomized controlled evaluation of the effects of cognitive-behavioral stress management on cortisol responses to acute stress in healthy subjects. Psychoneuroendocrinology. (2003) 28(6):767–79. doi: 10.1016/S0306-4530(02)00069-0
42. Aguilar-Raab C, Stoffel M, Hernández C, Rahn S, Moessner M, Steinhilber B, et al. Effects of a mindfulness-based intervention on mindfulness, stress, salivary alpha-amylase and cortisol in everyday life. Psychophysiology. (2021) 58(12):e13937. doi: 10.1111/psyp.13937
43. Duchemin A-M, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. J Occup Environ Med. (2015) 57(4):393–9. doi: 10.1097/JOM.0000000000000371
44. Ko CM, Grace F, Chavez GN, Grimley SJ, Dalrymple ER, Olson LE. Effect of seminar on compassion on student self-compassion, mindfulness and well-being: a randomized controlled trial. J Am Coll Health. (2018) 66(7):537–45. doi: 10.1080/07448481.2018.1431913
45. Limm H, Gündel H, Heinmüller M, Marten-Mittag B, Nater UM, Siegrist J, et al. Stress management interventions in the workplace improve stress reactivity: a randomised controlled trial. Occup Environ Med. (2011) 68(2):126–33. doi: 10.1136/oem.2009.054148
46. Rose RD, Buckey JC, Zbozinek TD, Motivala SJ, Glenn DE, Cartreine JA, et al. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav Res Ther. (2013) 51(2):106–12. doi: 10.1016/j.brat.2012.11.003
Keywords: medical students, mental health, online module, resilience, transitional age
Citation: Kaligis F, Ismail RI, Wiguna T, Prasetyo S, Gunardi H, Indriatmi W, Pasaribu MM, Pandia V, Minayati K, Magdalena CC, Nurraga GW, Pramatirta B, Calvin N and Sourander A (2023) Effectiveness of an online mental health strengthening module to build resilience and overcome stress for transitional aged medical students. Front. Digit. Health 5:1207583. doi: 10.3389/fdgth.2023.1207583
Received: 17 April 2023; Accepted: 22 September 2023;
Published: 4 October 2023.
Edited by:
Sylvie Bernaerts, Thomas More University of Applied Sciences, BelgiumReviewed by:
Michael Musker, University of South Australia, AustraliaHazli Zakaria, Alaminda Healthcare, Malaysia
© 2023 Kaligis, Ismail, Wiguna, Prasetyo, Gunardi, Indriatmi, Pasaribu, Pandia, Minayati, Magdalena, Nurraga, Pramatirta, Calvin and Sourander. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fransiska Kaligis ZnJhbnNpc2thLmthbGlnaXNAdWkuYWMuaWQ=
 Fransiska Kaligis
Fransiska Kaligis Raden Irawati Ismail1
Raden Irawati Ismail1 Clarissa Cita Magdalena
Clarissa Cita Magdalena Garda Widhi Nurraga
Garda Widhi Nurraga Billy Pramatirta
Billy Pramatirta