- 1School of Physiotherapy, University of Verona, Verona, Italy
- 2Department of Physiotherapy, Faculty of Medicine, Health and Sports, Universidad Europea de Madrid, Madrid, Spain
- 3Unit of Clinical Epidemiology, IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
- 4Department of Orthopaedics, Duke University, Durham, NC, United States
- 5Duke Clinical Research Institute, Duke University, Durham, NC, United States
- 6Department of Population Health Sciences, Duke University, Durham, NC, United States
- 7Department of Medical Sciences, University of Udine, Udine, Italy
- 8Department of Rehabilitation, Hospital of Merano (SABES-ASDAA), Teaching Hospital of Paracelsus Medical University (PMU), Merano-Meran, Italy
- 9Department of Biomedical and Neuromotor Sciences (DIBINEM), Alma Mater University of Bologna, Bologna, Italy
- 10Unit of Occupational Medicine, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
Introduction: Artificial Intelligence (AI) chatbots, which generate human-like responses based on extensive data, are becoming important tools in healthcare by providing information on health conditions, treatments, and preventive measures, acting as virtual assistants. However, their performance in aligning with clinical practice guidelines (CPGs) for providing answers to complex clinical questions on lumbosacral radicular pain is still unclear. We aim to evaluate AI chatbots' performance against CPG recommendations for diagnosing and treating lumbosacral radicular pain.
Methods: We performed a cross-sectional study to assess AI chatbots' responses against CPGs recommendations for diagnosing and treating lumbosacral radicular pain. Clinical questions based on these CPGs were posed to the latest versions (updated in 2024) of six AI chatbots: ChatGPT-3.5, ChatGPT-4o, Microsoft Copilot, Google Gemini, Claude, and Perplexity. The chatbots' responses were evaluated for (a) consistency of text responses using Plagiarism Checker X, (b) intra- and inter-rater reliability using Fleiss' Kappa, and (c) match rate with CPGs. Statistical analyses were performed with STATA/MP 16.1.
Results: We found high variability in the text consistency of AI chatbot responses (median range 26%–68%). Intra-rater reliability ranged from “almost perfect” to “substantial,” while inter-rater reliability varied from “almost perfect” to “moderate.” Perplexity had the highest match rate at 67%, followed by Google Gemini at 63%, and Microsoft Copilot at 44%. ChatGPT-3.5, ChatGPT-4o, and Claude showed the lowest performance, each with a 33% match rate.
Conclusions: Despite the variability in internal consistency and good intra- and inter-rater reliability, the AI Chatbots' recommendations often did not align with CPGs recommendations for diagnosing and treating lumbosacral radicular pain. Clinicians and patients should exercise caution when relying on these AI models, since one to two-thirds of the recommendations provided may be inappropriate or misleading according to specific chatbots.
Introduction
Large Language Models (LLMs) are deep learning systems capable of producing, understanding, and interacting with human language (1). In the field of LLMs, artificial intelligence (AI) chatbots (e.g., ChatGPT, Google Gemini, Microsoft Copilot) represent emerging tools that use algorithms to predict and generate words and phrases based on provided text input (2, 3). Recently, notable hype involving AI Chatbots has occurred because of their friendly interface that facilitates interaction, thus simplifying user accessibility (4).
This progress is relevant in health care, where patients increasingly use AI chatbots to navigate health-related queries (5). AI chatbots allow patients to inquire about their health conditions, treatment options, and preventive measures by acting as virtual assistants (6). However, the risk of misinformation, prejudices, lack of transparency, and hesitations about privacy and data security are still unresolved issues (7, 8). The AI Chatbots' ability to facilitate patient health literacy underlines the importance of investigating their performance in providing health information, guaranteeing reliability, accuracy, and alignment of their content with the best evidence included in the clinical practice guidelines (CPGs) (9).
Focusing on musculoskeletal pain conditions of the lumbar spine, conflicting evidence emerged when assessing the performance of AI Chatbots agreement with CPGs (10–13). A comparative analysis of ChatGPT's responses to CPGs for degenerative spondylolisthesis revealed a concordance rate of 46.4% for ChatGPT-3.5, while 67.9% for ChatGPT-4 (10). Another study reported a ChatGPT-3.5 accuracy of 65% in generating clinical recommendations for low back pain, which improved to 72% when prompted by an experienced orthopaedic surgeon (12). While assessing recommendations regarding lumbar disk herniation with radiculopathy, Mejia et al. found that ChatGPT-3.5 and ChatGPT-4 provided matched accuracy when compared to the CPGs of 52% and 59% of responses, respectively (11). Recently, ChatGPT-3.5 showed limited word text consistency of responses in terms of low levels of agreement between different parts of a system and percentage match rate with CPGs for lumbosacral radicular pain, presenting agreement of responses (i.e., match rate) in only 33% of recommendations (13).
Despite growing interest in the use of AI chatbots to support patient education in musculoskeletal conditions, current evidence reveals substantial variability in their response accuracy when compared with established CPGs (10–13). Most existing studies have evaluated individual chatbots or outdated versions (e.g., ChatGPT 3.5), without direct comparisons across multiple and updated models (e.g., ChatGPT-4o). Moreover, limited data are available on the performance of newer AI systems, such as Google Gemini, Microsoft Copilot, Claude, and Perplexity, when benchmarked against consistent, evidence-based recommendations for specific conditions like lumbosacral radicular pain. This lack of comprehensive, up-to-date comparison represents a critical gap in the literature, particularly regarding the reliability and accuracy (i.e., match rate) of the information these tools provide in the context of musculoskeletal care (4).
Therefore, the aim of this study was to compare the performance of five emerging AI Chatbots (ChatGPT-4o, Google Gemini, Microsoft Copilot, Claude, and Perplexity) and ChatGPT-3.5 (13) in providing accurate, evidence-based health advice for lumbosacral radicular pain against CPGs. In detail, we assessed (a) the word text consistency of chatbots, (b) intra- and inter-rater reliability of readers, and (c) match rate of each AI Chatbots with CPG recommendations.
Materials and methods
Study design and ethics
We performed an observational cross-sectional study, comparing the recommendations of a systematic review of CPGs (14) with those of AI Chatbots for lumbosacral radicular pain (Figure 1). We followed the Strengthening the Reporting of Observational Studies in Epidemiology guideline (STROBE) (15) and Reporting guideline for the early-stage clinical evaluation of decision support systems driven by artificial intelligence (DECIDE-AI) to achieve high-quality standards for reporting (16). As the units in our investigation were studies and not participants, we did not involve any interaction with human subjects or access to identifiable private information: ethical approval was not considered necessary (17).
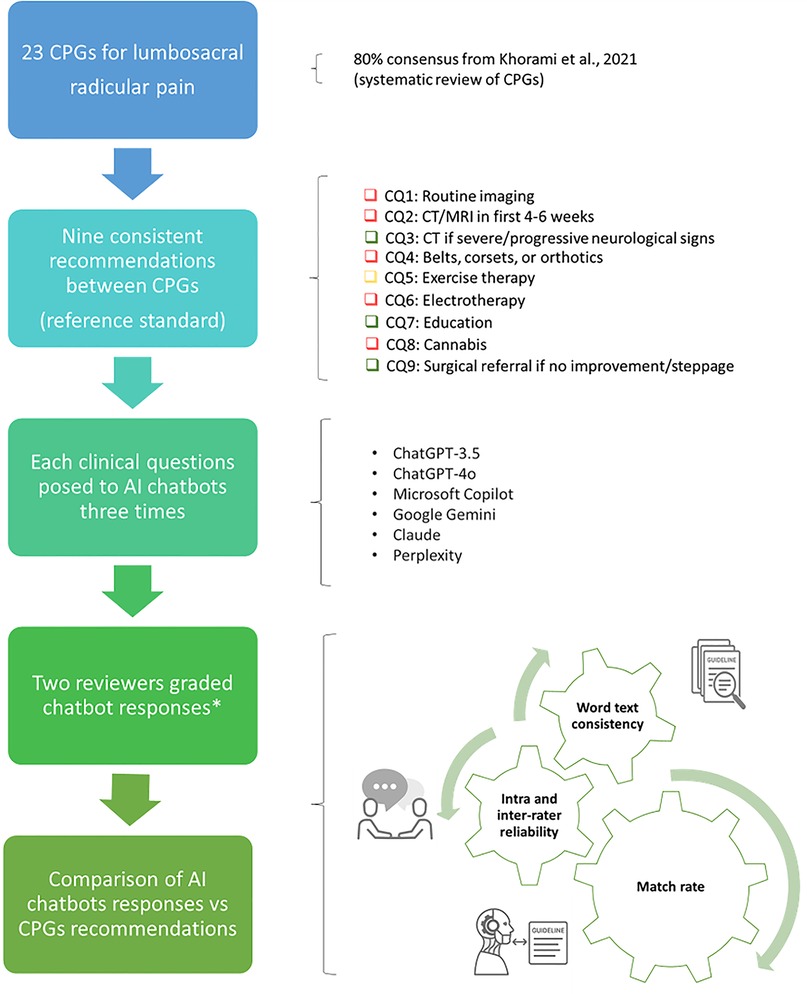
Figure 1. Overview of the study's pipeline. AI, artificial intelligence; CPGs, clinical practice guidelines; CQ, clinical question. *According to criteria for clinical inference adopted by the CPGs review appraisal (14). Green: “should do” (i.e., strong recommendation in favour to intervention); yellow: “could do” (i.e., weak recommendation in favour to intervention); red: “do not do” (i.e., recommendation against intervention); blue: “uncertain” (i.e., direction and strength of recommendation unclear).
Setting
In April 2024, a multidisciplinary group of methodologists, clinicians, and researchers with diverse healthcare backgrounds (e.g., physiotherapy, nursing) and expertise (e.g., musculoskeletal, neurology) coordinated this study. This choice of multiple backgrounds was aimed to ensure clinical expertise and to reflect the systematic appraisal of the recommendations of the Standards for Development of Trustworthy CPGs (18).
Sample
In accordance with our previous study on AI Chatbots (13), we used a sample of 9 CPGs recommendations for patients with lumbosacral radicular pain that emerged from a recent systematic review (14). A typical lumbosacral radicular pain pattern radiates through the path of a spinal nerve. It usually originates from the lumbar (lower back) or sacral (lowermost part of the spine) regions and may spread to the buttocks, thighs, or legs (14).
The nine CPGs recommendations included physical examination and diagnostics, non-invasive interventions, pharmacological interventions, invasive treatments and referral (14). We used these as reference standards, because their strength and direction were consistent across all CPGs for lumbosacral radicular pain (consensus ≥80% CPGs indicating “should do”, “could do”, “do not do”, or “uncertain”) (19). From the nine consistent recommendations, the multidisciplinary group developed nine relative clinical questions that were inputted into the five AI Chatbots (13) (Table 1).
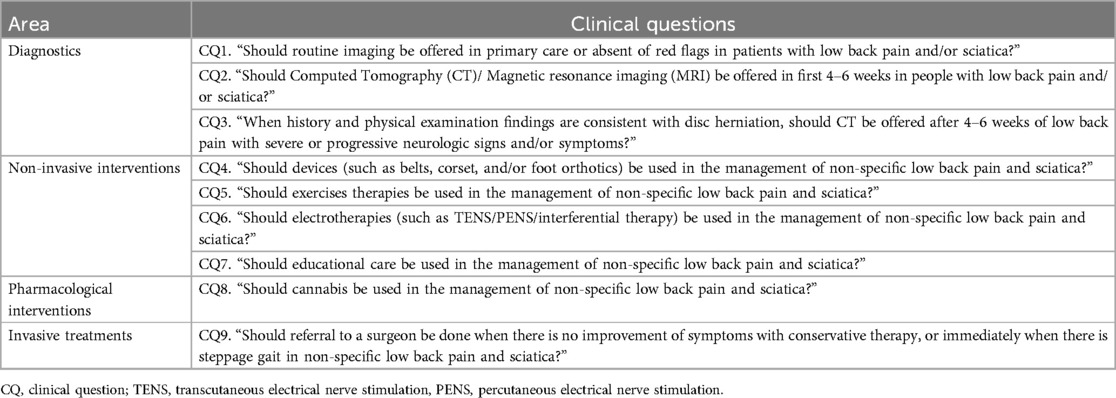
Table 1. Clinical questions obtained from the selected consistent recommendations across multiple clinical practice guidelines (14).
Measurements and variables
We used the latest versions of the AI chatbots that were updated in April 2024, including: ChatGPT-4o (OpenAI Incorporated, Mission District, San Francisco, United States) (20), Microsoft Copilot (Microsoft Corporation, WA, US) (21), Google Gemini (Alphabet Inc., CA, US) (22), Claude (Anthropic PBC, San Francisco, California, U.S.) (23), and Perplexity (Perplexity AI, Inc., San Francisco, California, USA) (24). The CPGs were compared with the responses of the five emerging AI Chatbots (ChatGPT-4o, Google Gemini, Microsoft Copilot, Claude, and Perplexity) and ChatGPT-3.5 (13). We considered the following variables for the analysis: (a) word text consistency of chatbots, (b) intra- and inter-rater reliability of those reading the AI chatbots, and (c) match rate of AI chatbots (13).
Text consistency of responses represents the degree of the interrelatedness among the items (i.e., text words) following the international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes (COSMIN) (25, 26). To measure the word text consistency of the AI chatbot answers, we adopted Plagiarism Checker X (27) to check for overlapping text among the three answers. The software compares the text of two documents side by side and displays the degree of similarity as a percentage (range: 0%–100%). A 0% match indicates no similarity, whereas a 100% match suggests a complete overlap of words and perfect consistency within the document. An example is given in Supplementary File 1, Figure S1.
Intra and inter-rater reliability indicate the level of agreement among independent reviewers in rating the three text responses obtained on the same clinical question (26). Match rate expresses the accuracy of how close a measurement result is to the measure's value, representing a qualitative performance characteristics (28). To measure the match rate as agreement of grading AI chatbot answers against the CPGs recommendations, we compared the frequency of the same judgements between AI chatbots and CPGs recommendations.
Procedure
To avoid prompt engineering influencing the generative output, we standardized the input formats of the nine clinical questions following the Prompt-Engineering-Guide (29). First, we prepared the nine clinical questions in Microsoft Word® by formatting them for proper structure and readability. Then, we manually copied and pasted each question onto the five AI chatbots during a single chat session on April 1, 2024.
The clinical questions were run three times to assess word text consistency, and responses were recorded (13). To minimize learning bias and eliminate the influence of prior interactions, we: (a) created and used a new account, (b) did not provide positive or negative feedback on the answer given, and (c) deleted conversations with the AI chatbots before entering each new question into a new chat (with no previous conversations) (13). To further enhance robustness and reproducibility, we implemented a controlled input/output protocol: all prompts were delivered in isolated, single-turn sessions, and the resulting outputs were copied verbatim, anonymized, and stored offline to prevent contextual contamination or post hoc alteration (13).
To measure intra and inter-rater reliability, two reviewers (SB, SG) with expertise in musculoskeletal disorders and clinical epidemiology (more than 3 years) graded each set of three text responses from the AI chatbot for all clinical questions. Prior to the study, they received 5 h of training. Using the same criteria for clinical inference adopted by the CPGs review appraisal (14), reviewers graded each set of responses as follows: “should do” (i.e., strong recommendation in favour to intervention), “could do” (i.e., weak recommendation in favour to intervention), “do not do” (i.e., recommendation against intervention) or “uncertain” (i.e., direction and strength of recommendation unclear). The terminology used for the grading system can be found in Supplementary File 1, Table S1.
We compared AI Chatbots' text responses to CPGs' recommendations in answering the nine clinical questions to measure their match rate (13). To obtain an unambiguous clinical judgement on AI Chatbot answers for each reviewer, we considered the mode (i.e., how frequently a particular categorial variable occurs) of the three trials of each categorical variable. A final clinical judgement between reviewers was established. We consulted a third reviewer (ZI) if there was any disagreement.
Statistical analyses
STATA/MP 16.1 was used to perform all statistical calculations, while data were plotted using STATA and Python. Categorical data were presented as absolute frequencies and percentages (%). A p-value of <.05 was considered significant. We a priori followed a common rule of thumb for defining word text consistency: ≥90% “excellent”, 80%–90% “good”, 70%–80% “acceptable”, 60%–70% “questionable”, 50%–60% “poor”, and <50% “unacceptable” (30). For intra and inter-rater reliability on AI Chatbot answers, we adopted Fleiss' Kappa (κ) (31). Interpretation of strength of agreement (Kappa-values) was categorized following Landis and Koch suggestions (<0.00 “poor”, 0–0.20 “slight”; 0.21–0.40 “fair”, 0.41–0.60 “moderate”, 0.61–0.80 “substantial”, 0.81–1.00 “almost perfect”) (32). As a measure of match rate, we used the inter-observer agreement obtained from a formula that divides the number of agreements in the grading by the sum of the agreement and disagreement [No. of agreements/(No. of agreements + disagreements) × 100]. A chi-square test was used to ascertain whether the answers differed among all AI chatbots against the CPGs' recommendations. A p-value of <.05 was considered significant. Since we compared six groups/AI chatbots, a Bonferroni adjustment for multiple measures was applied. Raw data are reported in Open Science Framework (OSF) repository available at https://osf.io/8dgrx/.
Ethics
Ethical approval is not applicable as no patients were recruited or involved in this study.
Results
Word text consistency of AI Chatbot answers
The consistency of text responses for each Chatbot in every CQ is highly variable ranging from “unacceptable” (median 26%) to “questionable” (median 68%). Findings for each clinical question are reported in Supplementary File 2, Tables S1–S6.
Reliability of AI Chatbot answers
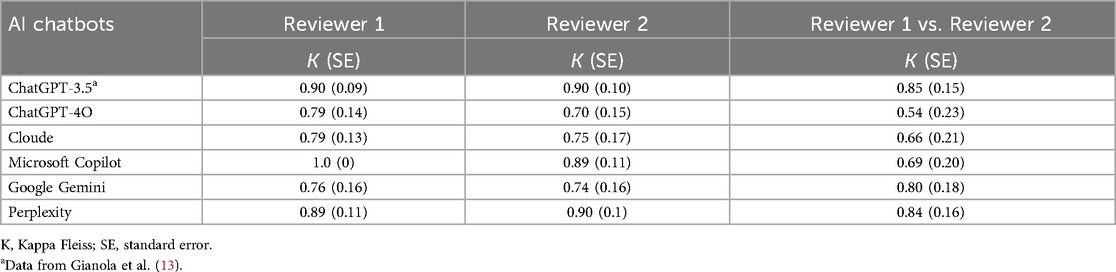
The intra-rater reliability was “almost perfect” for both reviewers considering Microsoft Copilot, Perplexity and ChatGPT-3.5 and “substantial” for ChatGPT-4o, Cloud and Gemini. Out of nine CQ ratings, the inter-rater reliability between the two reviewers was “almost perfect” for Perplexity (0.84, SE: 0.16) and ChatGPT-3.5 (0.85, SE: 0.15), “substantial” for Microsoft Copilot (0.69, SE: 0.20), Cloude (0.66, SE: 0.21) and Google Gemini (0.80, SE: 0.18), and “moderate” for ChatGPT-4o (0.54, SE: 0.23). Table 2 reported the Kappa Fleiss for each chatbot.
Match rate of AI Chatbot answers compared to CPGs recommendations
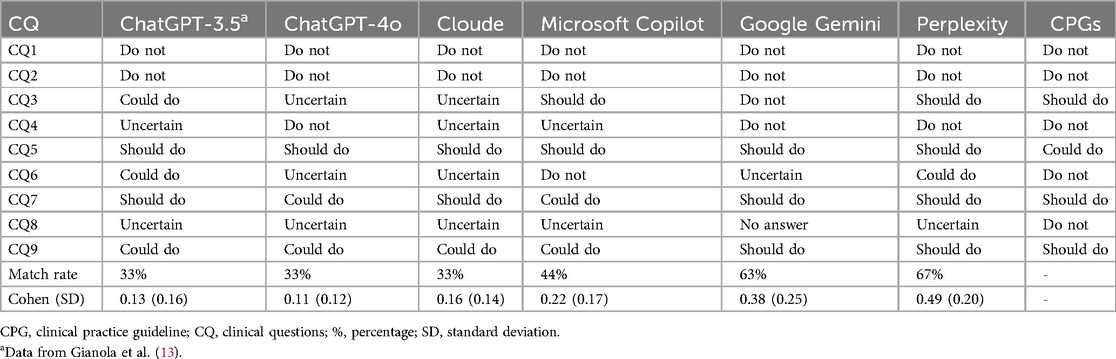
Among the AI Chatbots evaluated, Perplexity exhibited the highest matched rate at 67%, followed by Google Gemini at 63% and Microsoft Copilot at 44%. Conversely, Cloude, ChatGPT-3.5, and ChatGPT-4o demonstrated the lowest match rates with a score of 33% (Figure 2, Table 3).
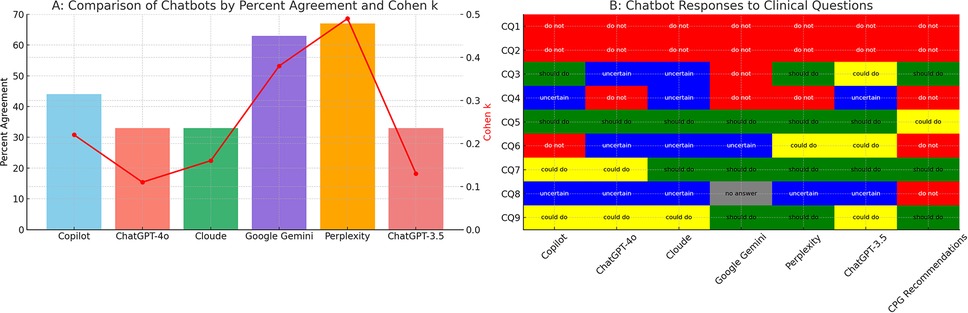
Figure 2. Performance of AI chatbots compared to CPG recommendation. AI, artificial intelligence; CPGs, clinical practice guidelines; CQ, clinical question. (A) Quantitative bar chart representing percentage of agreement (y-axis, left side) of the six chatbots (x-axis). Red points represent Cohen's K value (y-axis, right side). (B) Qualitative table showing the clinical inference for each CQ (y-axis) in each chatbot (x-axis). Chat GPT-3.5 data are from Gianola et al. (13).
Discussion
Main findings
In this study, we compared the performance of five updated AI Chatbots (ChatGPT-4o, Google Gemini, Microsoft Copilot, Claude, and Perplexity) and ChatGPT-3.5 (13) in producing evidence-based health advice against CPGs for radicular lumbosacral pain. As the main finding, no AI chatbots provided advice that was in absolute agreement with CPGs, confirming the results previously found in other lumbar spine pain conditions (10–13). This finding suggests that although AI chatbots have promising potential, they currently do not perform adequately to be recommended for patient use.
Comparison with evidence
Comparing our study with existing literature is a challenge due to the limited amount of research that has examined multiple AI chatbots (e.g., mainly ChatGPT-3.5 and 4) against CPGs (10–13) and that have analysed similar performance metrics (13). We observed that: (a) the word consistency of text responses for each Chatbot was highly variable; (b) the intra-rater reliability ranged from “almost perfect” to “substantial”, whereas the inter-rater reliability varied from “almost perfect” to “moderate”; and (c) the match rate differs notably between AI Chatbots, with Gemini and Perplexity being superior, albeit imperfect.
The findings reveal substantial variability in AI chatbot performance, which likely arises from fundamental differences in model architecture (e.g., decoder-only transformer frameworks), pre-training strategies (e.g., autoregressive language modeling vs. instruction tuning), and the nature of training datasets—often heterogeneous, non-curated, and lacking peer-reviewed medical content (33). Moreover, current LLMs do not exhibit structured clinical reasoning but operate through probabilistic pattern matching, which contributes to recurrent errors such as factual inaccuracies, overgeneralization, contextual misinterpretation, and poor management of clinical ambiguity (34). This is further compounded by the lack of transparency surrounding proprietary algorithms, rendering these models “black boxes” with limited interpretability for the scientific community (11).
Implications for clinical practice
Our results discourage the adoption of AI Chatbots as an information tool for patients with lumbosacral radicular pain. Our experience supports previously documented evidence that AI chatbots tend to provide generic, verbose, incomplete, outdated, or inaccurate information (7, 8). Furthermore, being highly dependent on the quality of the training data, AI Chatbots may be biased (e.g., language, gender, race), which affects their outputs (7, 8). Finally, AI Chatbots suffer from the phenomenon of “artificial hallucination” and may produce confident answers based on fabricated facts without evidence (7, 8).
In an era of digitisation, where patients increasingly search for health information on the web and assume it is reliable and valid (35), AI Chatbots, being user-friendly (5) have the potential to complement existing web tools (e.g., Dr Google, Wikipedia) (36, 37). However, lacking critical analysis and abstract reasoning, as well as the clinician's experience and judgement, AI Chatbots may play the role of threats rather than opportunities (4). For example, in lumbosacral radicular pain, basing their outputs on information retrieved on the web whose quality is poor (38), they could act as a nocebo source capable of spreading negative information and perpetuating an infodemic (39). As a consequence, patients with lumbosacral radicular pain could be harmed, directed towards non-evidence-based treatments, and wasted economic resources (4).
For AI chatbots to be gradually integrated into healthcare systems, clinicians, healthcare organisations, and policy-makers should raise awareness among stakeholders (e.g., patients and laypersons) with public information campaigns to analyse the pros and cons (40). It is essential that AI chatbots are trained to search for information in healthcare databases (e.g., PubMed, Scopus, Web of Science) and assess the methodological quality of the information obtained (10, 11). Accordingly, several healthcare-specific LLMs are being developed (e.g., PMC-LLaMA, Med-LLaMA, Almanac) (41–43), but further studies are needed to assess their feasibility and validity, prior to adoption.
In this evolving context, universities and academic institutions have a crucial role in both managing risks and supporting the responsible use of AI chatbots in healthcare (44). As centers of education and research, they should integrate digital health literacy into healthcare training programs, equipping future clinicians with the skills needed to critically evaluate AI tools (45). Furthermore, through interdisciplinary collaborations, universities can lead the rigorous validation of AI systems and promote the development of ethical and safe digital solutions.
Strengths and limitations
This study is the first to compare the performance of multiple AI Chatbots against CPGs for lumbosacral radicular pain, adopting a transparent methodology that comprises the use of standardized prompts and an objective measure of performance (13). Despite this, there are some limitations that exist. Firstly, we studied five AI Chatbots that although very popular, do not represent the totality of available tools [e.g., DeepSeek (46)]. Secondly, not all the Chatbots considered were available without payment: only five were free (13, 21–24), whereas ChatGPT-4o was available at a fee (20). Given the evolving nature of LLMs, our results may not be extendable to more recent models, as AI Chatbots are continuously developed and improved (12). Thirdly, we investigated the performance of AI chatbots focusing on lumbosacral radicular pain; however, these findings may not be generalisable to other pathologies of the lumbar spine (10–13). Lastly, we did not execute a sentiment analysis on the AI's outputs to identify the quality of the texts' emotional tone (e.g., positive, negative, or neutral) (4).
Thus, while awaiting shared reporting guidelines (47), further research is needed to address the current limitations. This includes evaluating emerging and updated AI chatbot models against CPGs in other musculoskeletal conditions (e.g., upper and lower limbs, cervical and thoracic spine), assessing their interpretability, and examining performance when interpreted by end-users such as patients. Comparative studies involving human clinicians as reference standards are also warranted to determine the clinical utility of these tools. Finally, future work should explore multimodal outputs (e.g., text, visuals) and the integration of AI chatbots into patient-facing digital health platforms to enhance usability and relevance in real-world settings.
Conclusion
In our study, none of the AI chatbots fully matched responses of the CPGs for lumbosacral radicular pain, revealing a high variability in their performance. These findings confirm that currently patients without clinician supervision cannot use AI Chatbots to provide health information.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://osf.io/8dgrx/.
Ethics statement
Ethical approval was not required for the study in accordance with the local legislation and institutional requirements.
Author contributions
GR: Conceptualization, Data curation, Methodology, Project administration, Writing – original draft, Writing – review & editing, Formal analysis, Supervision, Validation. SB: Methodology, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Supervision, Validation. CC: Writing – original draft, Writing – review & editing, Supervision, Validation. SGu: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Methodology. AP: Writing – original draft, Writing – review & editing, Supervision, Validation. LR: Data curation, Writing – original draft, Writing – review & editing, Formal analysis, Methodology. PP: Writing – original draft, Writing – review & editing, Supervision, Validation. AT: Writing – original draft, Writing – review & editing, Supervision, Validation. GC: Formal analysis, Project administration, Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Validation. SGi: Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing, Conceptualization, Validation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors receive funding from the Department of Innovation, Research, University and Museums of the Autonomous Province of Bozen/Bolzano for covering the Open Access Publication costs. SB, SGu, GC and SGi were supported and funded by Italian Ministry of Health.
Acknowledgments
The authors thank the Department of Innovation, Research, University and Museums of the Autonomous Province of Bozen/Bolzano for covering the Open Access publication cost.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2025.1574287/full#supplementary-material
References
1. Thirunavukarasu AJ, Ting DSJ, Elangovan K, Gutierrez L, Tan TF, Ting DSW. Large language models in medicine. Nat Med. (2023) 29(8):1930–40. doi: 10.1038/s41591-023-02448-8
2. Ng JY, Maduranayagam SG, Suthakar N, Li A, Lokker C, Iorio A, et al. Attitudes and perceptions of medical researchers towards the use of artificial intelligence chatbots in the scientific process: an international cross-sectional survey. Lancet Digit Health. (2025) 7(1):e94–102. doi: 10.1016/S2589-7500(24)00202-4
3. Clusmann J, Kolbinger FR, Muti HS, Carrero ZI, Eckardt JN, Laleh NG, et al. The future landscape of large language models in medicine. Commun Med. (2023) 3(1):141. doi: 10.1038/s43856-023-00370-1
4. Rossettini G, Cook C, Palese A, Pillastrini P, Turolla A. Pros and cons of using artificial intelligence chatbots for musculoskeletal rehabilitation management. J Orthop Sports Phys Ther. (2023) 53(12):728–34. doi: 10.2519/jospt.2023.12000
5. Park YJ, Pillai A, Deng J, Guo E, Gupta M, Paget M, et al. Assessing the research landscape and clinical utility of large language models: a scoping review. BMC Med Inform Decis Mak. (2024) 24(1):72. doi: 10.1186/s12911-024-02459-6
6. Choudhury A, Elkefi S, Tounsi A. Exploring factors influencing user perspective of ChatGPT as a technology that assists in healthcare decision making: a cross sectional survey study. PLoS One. (2024) 19(3):e0296151. doi: 10.1371/journal.pone.0296151
7. Dave T, Athaluri SA, Singh S. ChatGPT in medicine: an overview of its applications, advantages, limitations, future prospects, and ethical considerations. Front Artif Intell. (2023) 6:1169595. doi: 10.3389/frai.2023.1169595
8. Gödde D, Nöhl S, Wolf C, Rupert Y, Rimkus L, Ehlers J, et al. A SWOT (strengths, weaknesses, opportunities, and threats) analysis of ChatGPT in the medical literature: concise review. J Med Internet Res. (2023) 25:e49368. doi: 10.2196/49368
9. Wei Q, Yao Z, Cui Y, Wei B, Jin Z, Xu X. Evaluation of ChatGPT-generated medical responses: a systematic review and meta-analysis. J Biomed Inform. (2024) 151:104620. doi: 10.1016/j.jbi.2024.104620
10. Ahmed W, Saturno M, Rajjoub R, Duey AH, Zaidat B, Hoang T, et al. ChatGPT versus NASS clinical guidelines for degenerative spondylolisthesis: a comparative analysis. Eur Spine J. (2024) 33(11):4182–203. doi: 10.1007/s00586-024-08198-6
11. Mejia MR, Arroyave JS, Saturno M, Ndjonko LCM, Zaidat B, Rajjoub R, et al. Use of ChatGPT for determining clinical and surgical treatment of lumbar disc herniation with radiculopathy: a north American spine society guideline comparison. Neurospine. (2024) 21(1):149–58. doi: 10.14245/ns.2347052.526
12. Shrestha N, Shen Z, Zaidat B, Duey AH, Tang JE, Ahmed W, et al. Performance of ChatGPT on NASS clinical guidelines for the diagnosis and treatment of low back pain: a comparison study. Spine. (2024) 49(9):640–51. doi: 10.1097/BRS.0000000000004915
13. Gianola S, Bargeri S, Castellini G, Cook C, Palese A, Pillastrini P, et al. Performance of ChatGPT compared to clinical practice guidelines in making informed decisions for lumbosacral radicular pain: a cross-sectional study. J Orthop Sports Phys Ther. (2024) 54(3):222–8. doi: 10.2519/jospt.2024.12151
14. Khorami AK, Oliveira CB, Maher CG, Bindels PJE, Machado GC, Pinto RZ, et al. Recommendations for diagnosis and treatment of lumbosacral radicular pain: a systematic review of clinical practice guidelines. J Clin Med. (2021) 10(11):2482. doi: 10.3390/jcm10112482
15. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61(4):344–9. doi: 10.1016/j.jclinepi.2007.11.008
16. Vasey B, Nagendran M, Campbell B, Clifton DA, Collins GS, Denaxas S, et al. Reporting guideline for the early-stage clinical evaluation of decision support systems driven by artificial intelligence: DECIDE-AI. Nat Med. (2022) 28(5):924–33. doi: 10.1038/s41591-022-01772-9
18. Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, editors. Washington (DC): National Academies Press (US) (2011). Available at: https:// www.ncbi.nlm.nih.gov/books/NBK209537/ (Accessed June 15, 2025).
19. Gattrell WT, Hungin AP, Price A, Winchester CC, Tovey D, Hughes EL, et al. ACCORD guideline for reporting consensus-based methods in biomedical research and clinical practice: a study protocol. Res Integr Peer Rev. (2022) 7(1):3. doi: 10.1186/s41073-022-00122-0
20. Hello GPT-4o. Available online at: https://openai.com/index/hello-gpt-4o/ (Accessed June 3, 2024).
21. Microsoft Copilot: il tuo AI Companion quotidiano. Microsoft Copilot: il tuo AI Companion quotidiano. Available online at: https://ceto.westus2.binguxlivesite.net/ (Accessed May 4, 2024).
22. Gemini: chatta per espandere le tue idee. Gemini. Available online at: https://gemini.google.com (Accessed May 4, 2024).
23. Claude. Available online at: https://claude.ai/login?returnTo=%2F%3F (Accessed May 4, 2024).
24. Perplexity. Available online at: https://www.perplexity.ai/?login-source=oneTapHome (Accessed May 4, 2024).
25. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. (2010) 63(7):737–45. doi: 10.1016/j.jclinepi.2010.02.006
26. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. 1573–2649 (Electronic).
27. Plagiarism checker X - text similarity detector. Plagiarism checker X. Available online at: https://plagiarismcheckerx.com (Accessed May 4, 2024).
28. Menditto A, Patriarca M, Magnusson B. Understanding the meaning of accuracy, trueness and precision. Accredit Qual Assur. (2007) 12:45–7. doi: 10.1007/s00769-006-0191-z
29. Giray L. Prompt engineering with ChatGPT: a guide for academic writers. Ann Biomed Eng. (2023) 51(12):2629–33. doi: 10.1007/s10439-023-03272-4
30. George D, Mallery M. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 Update. 10th ed. Boston: Pearson (2010).
32. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33(1):159–74. doi: 10.2307/2529310
33. Alhur A. Redefining healthcare with artificial intelligence (AI): the contributions of ChatGPT, Gemini, and co-pilot. Cureus. (2024) 16(4):e57795. doi: 10.7759/cureus.57795
34. Zhang D, Xiaojuan X, Gao P, Jin Z, Hu M, Wu Y, et al. A survey of datasets in medicine for large language models. Intell Robot. (2024) 4:457–78. doi: 10.20517/ir.2024.27
35. Amante DJ, Hogan TP, Pagoto SL, English TM, Lapane KL. Access to care and use of the internet to search for health information: results from the US national health interview survey. J Med Internet Res. (2015) 17(4):e106. doi: 10.2196/jmir.4126
36. Smith DA. Situating Wikipedia as a health information resource in various contexts: a scoping review. PLoS One. (2020) 15(2):e0228786. doi: 10.1371/journal.pone.0228786
37. Lee K, Hoti K, Hughes JD, Emmerton L. Dr Google and the consumer: a qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. J Med Internet Res. (2014) 16(12):e262. doi: 10.2196/jmir.3706
38. Mancuso-Marcello M, Demetriades AK. What is the quality of the information available on the internet for patients suffering with sciatica? J Neurosurg Sci. (2023) 67(3):355–9. doi: 10.23736/S0390-5616.20.05243-1
39. De Angelis L, Baglivo F, Arzilli G, Privitera GP, Ferragina P, Tozzi AE, et al. ChatGPT and the rise of large language models: the new AI-driven infodemic threat in public health. Front Public Health. (2023) 11:1166120. doi: 10.3389/fpubh.2023.1166120
40. Huo B, Calabrese E, Sylla P, Kumar S, Ignacio RC, Oviedo R, et al. The performance of artificial intelligence large language model-linked chatbots in surgical decision-making for gastroesophageal reflux disease. Surg Endosc. (2024) 38(5):2320–30. doi: 10.1007/s00464-024-10807-w
41. Li Y, Li Z, Zhang K, Dan R, Jiang S, Zhang Y. Chatdoctor: a medical chat model fine-tuned on a large language model meta-AI (LLaMA) using medical domain knowledge. Cureus. (2023) 15(6):e40895. doi: 10.7759/cureus.40895
42. Zakka C, Shad R, Chaurasia A, Dalal AR, Kim JL, Moor M, et al. Almanac - retrieval-augmented language models for clinical medicine. NEJM AI. (2024) 1(2). doi: 10.1056/AIoa2300068
43. Wu C, Lin W, Zhang X, Zhang Y, Xie W, Wang Y. PMC-LLaMA: toward building open-source language models for medicine. J Am Med Inform Assoc. (2024) 31(9):1833–43. doi: 10.1093/jamia/ocae045
44. Tortella F, Palese A, Turolla A, Castellini G, Pillastrini P, Landuzzi MG, et al. Knowledge and use, perceptions of benefits and limitations of artificial intelligence chatbots among Italian physiotherapy students: a cross-sectional national study. BMC Med Educ. (2025) 25(1):572. doi: 10.1186/s12909-025-07176-w
45. Rossettini G, Palese A, Corradi F, Pillastrini P, Turolla A, Cook C. Artificial intelligence chatbots in musculoskeletal rehabilitation: change is knocking at the door. Minerva Orthop. (2024) 75:397–9. doi: 10.23736/S2784-8469.24.04517-6
46. DeepSeek. Available online at: https://deep-seek.chat/ (Accessed May 12, 2025).
Keywords: artificial intelligence, physiotherapy, machine learning, musculoskeletal, natural language processing, orthopaedics, ChatGPT, chatbots
Citation: Rossettini G, Bargeri S, Cook C, Guida S, Palese A, Rodeghiero L, Pillastrini P, Turolla A, Castellini G and Gianola S (2025) Accuracy of ChatGPT-3.5, ChatGPT-4o, Copilot, Gemini, Claude, and Perplexity in advising on lumbosacral radicular pain against clinical practice guidelines: cross-sectional study. Front. Digit. Health 7:1574287. doi: 10.3389/fdgth.2025.1574287
Received: 10 February 2025; Accepted: 9 June 2025;
Published: 27 June 2025.
Edited by:
Norberto Peporine Lopes, University of São Paulo, BrazilReviewed by:
Manuela Deodato, University of Trieste, ItalyJoaquín González Aroca, University of La Serena, Chile
Copyright: © 2025 Rossettini, Bargeri, Cook, Guida, Palese, Rodeghiero, Pillastrini, Turolla, Castellini and Gianola. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lia Rodeghiero, bGlhLnJvZGVnaGllcm85NEBnbWFpbC5jb20=
†These authors have contributed equally to this work
‡ORCID:
Giacomo Rossettini
orcid.org/0000-0002-1623-7681
Silvia Bargeri
orcid.org/0000-0002-3489-6429
Chad Cook
orcid.org/0000-0001-8622-8361
Stefania Guida
orcid.org/0000-0002-1809-061X
Alvisa Palese
orcid.org/0000-0002-3508-844X
Paolo Pillastrini
orcid.org/0000-0002-8396-2250
Andrea Turolla
orcid.org/0000-0002-1609-8060
Greta Castellini
orcid.org/0000-0002-3345-8187
Silvia Gianola
orcid.org/0000-0003-3770-0011
 Giacomo Rossettini
Giacomo Rossettini Silvia Bargeri
Silvia Bargeri Chad Cook4,5,6,‡
Chad Cook4,5,6,‡ Alvisa Palese
Alvisa Palese Lia Rodeghiero
Lia Rodeghiero Paolo Pillastrini
Paolo Pillastrini Andrea Turolla
Andrea Turolla Greta Castellini
Greta Castellini Silvia Gianola
Silvia Gianola