- 1Department of Psychological & Brain Sciences, Washington University in St. Louis, St. Louis, MO, United States
- 2School of Humanities, Central South University, Changsha, China
- 3Xiangya Hospital, Central South University, Changsha, China
- 4Center for Clinical Pharmacology, Third Xiangya Hospital, Central South University, Changsha, China
Artificial Intelligence (AI) is increasingly being adopted across many industries including healthcare. This has brought forth the development of many new independent ethical frameworks for responsible use of AI within institutions and companies. Risks associated with the application of AI in healthcare have high stakes for patients. Further, the existence of multiple frameworks may exacerbate these risks due to potential differences in interpretation and prioritization in said frameworks. Resolving these risks requires an ethical framework that is both broadly adopted in healthcare settings and applicable to AI. Here, we examined whether a framework consisting of the 4 well-established principles of biomedical ethics (i.e., Beneficence, Non-Maleficence, Respect for Autonomy, and Justice) can serve as a foundation for an ethical framework for AI in healthcare. To this end, we conducted a scoping review of 227 peer-reviewed papers using semi-inductive thematic analyses to categorize patient-related ethical issues in healthcare AI under these 4 principles of biomedical ethics. We found that these principles, which are already widely adopted in healthcare settings, were comprehensively and internationally applicable to ethical considerations concerning use of AI in healthcare. The existing four principles of biomedical ethics can provide a foundational ethical framework for applying AI in healthcare, grounding other Responsible AI frameworks, and can act as a basis for AI governance and policy in healthcare.
1 Introduction
The potential of Artificial Intelligence (AI) to improve healthcare (e.g., automate tasks, improve diagnoses and treatment) has led to its widespread adoption. In a 2022 international systematic review, AI usage by medical students and physicians was reported to be between 10% and 30% (1). By 2023, a separate survey found that nearly 38% of physicians in America were already using AI in practice, with nearly two-thirds stating they recognized its potential advantages (2). However, this rapid integration of AI also introduces novel ethical risks (e.g., explainability) across healthcare research and clinical settings (3–5).
In 2022, 75% of Americans believed healthcare providers would adopt AI too quickly before fully understanding risks for patients (6). Concerns among the public are founded on more than simple technological aversion. Indeed, ethical issues and unknowns raised by involvement of AI in healthcare are evolving as quickly as the technology itself, while regulatory governance currently lags behind (e.g., explicit permission to use patient data for training AI models) (7–9). To address these challenges, a new area of study referred to as “Responsible AI” (RAI) has emerged, defined as “the practice of developing, using, and deploying [AI] systems in a way that is ethical, transparent, and accountable” (10–13).
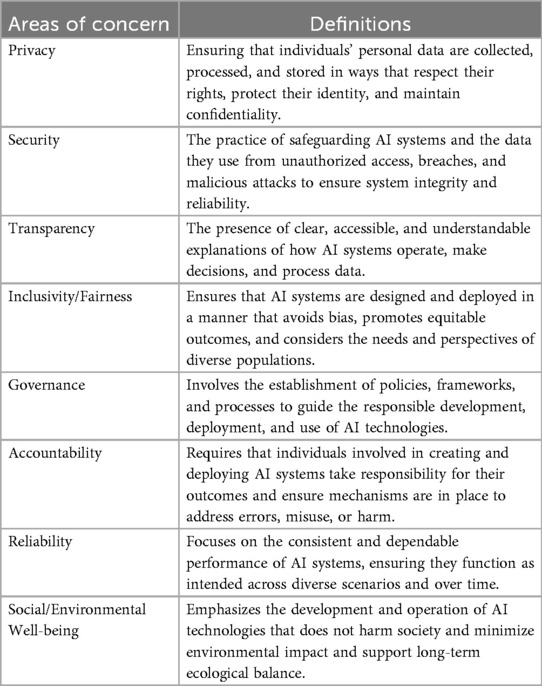
To date, numerous frameworks for RAI have been suggested by both governmental (14–20) and non-governmental organizations (e.g., technology companies) (21–26) (see Tables 1, 2 for common areas of concern in RAI and how they correspond to healthcare issues). However, these frameworks feature noticeable limitations which are especially relevant in healthcare, where use of AI has significant implications for patients (27). Such limitations include but are not limited to the abstract nature of these frameworks (28). For example, several frameworks include the concept of “fairness”. However, fairness in AI and fairness in healthcare do not always align. Fairness may variously describe: the impact of class imbalances in AI model training data (29), poor generalizability of AI models (30), expected patient outcomes from AI-produced recommendations (31), and/or focus on inappropriate metrics (e.g., focusing on accuracy over clinical utility) (32). Further, emerging RAI frameworks vary widely in content, such that no one framework could necessarily claim to be comprehensive. Indeed, the very nature of having a variety of frameworks to choose from may lead to a focus on compliance for the sake of compliance (33). Finally, beyond general RAI principles, specific ethical considerations for healthcare need to be considered (34, 35). As adoption of healthcare AI continues to accelerate, there is a need for RAI frameworks for healthcare to be grounded in foundational principles that are already widely accepted and applied in healthcare around the world.
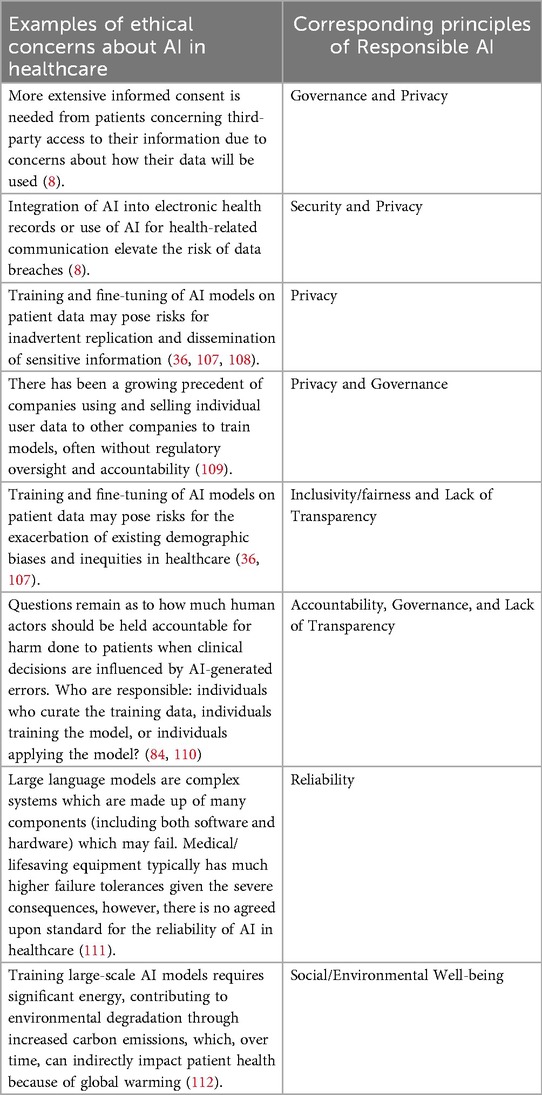
Table 2. Examples of ethical concerns about AI in healthcare and their corresponding Responsible AI principles.
A recent literature review by Ong and colleagues (36) proposed the four principles of biomedical ethics by Beauchamp and Childress (37, 38) as an ideal standard to guide use of large language models in medicine. In doing so, the authors called upon a classical health ethics framework with a well-established history across cultures, time, and technology as a potential unifying framework for ethical evaluation of AI in healthcare. Beauchamp and Childress's framework emerged in 1979 as part of an international wave of biomedical ethics reform and is used to this day (37). The framework encompasses the following four principles: Beneficence (to take positive action to enhance the welfare of patients and to minimize potential for harm); Non-Maleficence (not to inflict harm on patients); Respect for Autonomy (to respect the capacities of patients to hold their own views, make choices, and act based on their values and beliefs); and Justice (to distribute healthcare benefits appropriately and fairly).
Although some authors have speculated about the utility of these principles as a foundational framework for assessing ethical implications of AI in healthcare (36, 39), there has been limited effort to systematically examine how research and commentary in current peer-reviewed literature on AI in healthcare maps onto these four well established biomedical principles. In this scoping review, we aim to map ethical discussion from current peer-reviewed literature about AI in healthcare onto the four principles, to demonstrate their utility as a concise, foundation for RAI in healthcare that has already been internationally adopted in healthcare settings. We demonstrate this by using said principles to identify, categorize, and examine emerging patient-related ethical implications of AI in healthcare. Finally, we discuss how leveraging these well-established principles as a foundational framework can help expedite regulatory governance of RAI in healthcare.
2 Materials and methods
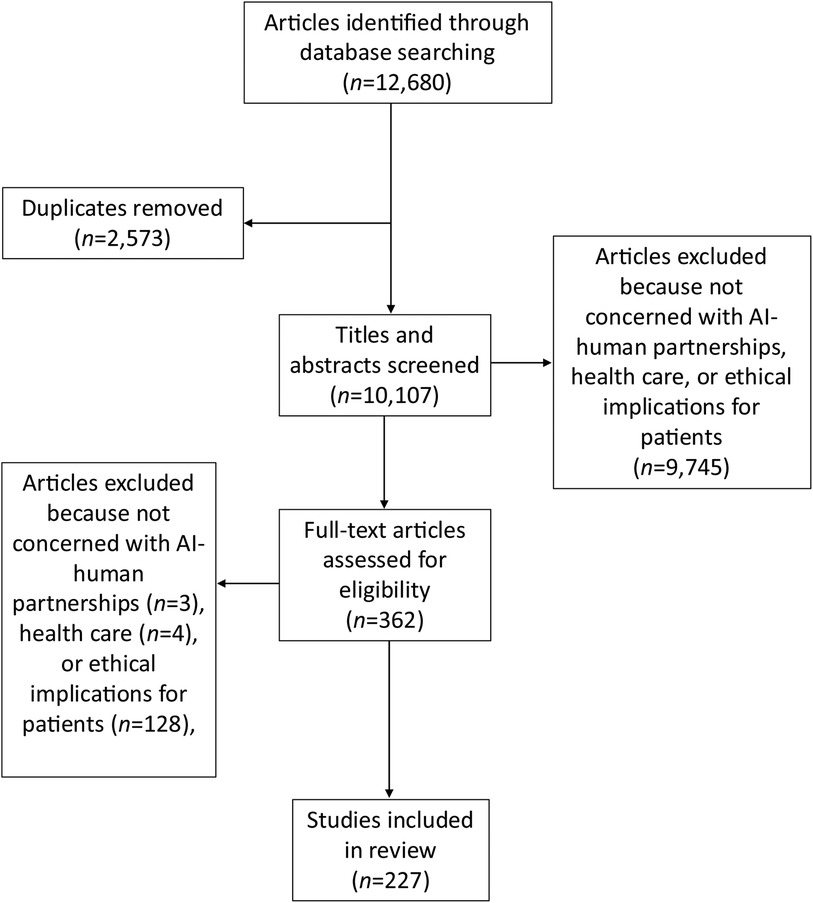
Our scoping review was conducted using criteria outlined by Mak and Thomas (40) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (see Supplementary Appendix 1) (41).
2.1 Search strategy
PubMed and EMBASE databases were searched for articles on the use of AI in healthcare. The search strategy and rationale as well as search terms are provided in Supplementary Appendix 2. The final search, which included any articles published from database inception to February 17, 2024, after removal of duplicates, yielded 10,107 articles for abstract screening.
2.2 Eligibility criteria
Studies included in our review were required to be published or in press in a peer-reviewed journal or conference proceeding in English or have an accompanying English translation and mention AI in healthcare settings in the context of human input or oversight. Broadly, we conceptualized AI in healthcare as a partner to human activity and oversight rather than a sole agent operating independently. In accordance with the qualitative nature of our research question, articles were not required to be empirical in nature; editorials, reviews, and conference proceedings with content more substantial than single-paragraph abstracts were included in the review. To focus our findings on direct ethical implications for patients, we excluded articles that focused only on AI involvement in research paper writing and publishing, clinician education and training, or research that did not involve human participants.
Finally, articles were only selected if they substantively referenced the ethical implications of healthcare AI with respect to patients. To be considered “substantive,” ethical content in abstracts had to either use a broad, inclusive term such as “ethics” or “ethical implications” or at least two phrases referencing ethical issues relating to patients such as “improving patient care,” “data privacy,” “bias,” “informed consent,” “health equity,” “transparency of data use,” or “[sociodemographic] representativeness of training data”.
2.3 Screening, data extraction, and synthesis
The full text of articles passing title and abstract screening [conducted by authors JH and AG using Rayyan (42)] was reviewed by a team of 4 coders (authors ML, JW, YR, LY) who extracted and synthesized relevant data. A study eligibility guide based on the Population/Concept/Context framework (43), was developed to train reviewers and referred to in both title/abstract screening and full-text review (Supplementary Appendix 3).
2.3.1 Study eligibility: reviewer calibration and evaluation of consistency
During an initial training phase, a batch of 900 (roughly 9% of total) abstracts were screened by JH and AG independently during initial training to resolve differences through consensus and iteratively refine study eligibility criteria applied to various types of content covered by abstracts. To achieve calibration between the two reviewers following training, a second batch of 870 (roughly 9% of total) abstracts were screened independently by both reviewers, and 93% agreement was achieved, exceeding the minimum of 90% agreement recommended by Mak and Thomas (40). Differences across both batches of 900 and 870 articles respectively were resolved through consensus, and the remainder of abstracts were divided between the two calibrated reviewers until completion of title-and-abstract screening.
Following abstract screening, authors ML and JW underwent an initial training phase for full-text screening, during which both authors independently conducted screening, data extraction, and data synthesis for a preliminary batch of 40 articles (approximately 11% of total articles included after abstract screening). Any differences were resolved by consensus. Authors YR and LY then completed screening, extraction, and synthesis for a second batch of 40 (roughly 11% of total) articles under independent individual supervision by authors ML and JW, and any differences were again resolved by consensus. For each batch of 40 through the remainder of articles, each of the four reviewers completed screening, extraction, and synthesis for 10 articles. To ensure ongoing calibration, a random number generator was used to select one article from each batch of 40 that was then independently reviewed by all four authors. Any differences in the randomly selected calibration articles were resolved through ongoing consensus. Finally, all synthesized data were reviewed by author ML for consistency. Articles were excluded after data extraction and full-text screening if they did not meet eligibility criteria.
2.3.2 Data extraction
Data extraction involved reading each article in full and charting key summary information, including citation information; country of origin; article aims; study population and intervention (if applicable); findings; and ethical considerations discussed (see Supplementary Appendix 4 for details).
2.3.3 Thematic analysis
Data from all articles included after full-text screening was synthesized using semi-inductive thematic analysis in NVivo 12 for analysis of mixed methods research (44). This approach was informed by Fereday and Muir-Cochrane (45), who described thematic analysis that uses a hybrid approach between deductively applying a predetermined framework to data and inductively allowing for additional information to emerge from the data in the process of analysis (46). We used this approach due to our aim to discover emerging ethical implications of AI and examine their relevance to the four principles.
In the process of thematic analysis, we followed the six stages outlined by Fereday and Muir-Cochrane (45). In Stage 1, we developed an initial codebook of four codes, using the principles of biomedical ethics as a deductive theoretical framework to guide our analysis. We established definitions for each of these four main codes based on their definitions from Beauchamp and Childress (37). In Stage 2, we tested the applicability of codes to the data by comparing the application of these four main codes during the aforementioned training phase in which authors ML and JW both coded data from the same batch of 40 articles. In Stage 3, we used the process of data extraction to summarize the data and identify sub-codes that represented emerging ethical implications for patients related to healthcare AI. Sub-codes were defined, discussed, and revised through iterative discussion with the whole research team. In Stage 4, once a final codebook was established, the codes were applied to all articles in the review with the intention of identifying meaningful units of text for the synthesis of themes (see Table 3 for a comprehensive list of all codes included in the final codebook, grouped by theme, with representative coded excerpts). In Stage 5, once all articles were coded, excerpts representing each code were compared and connected to synthesize themes. In Stage 6, themes were scrutinized to ensure that they were accurate summaries of the coded ethical implications that emerged from the data, resulting in our final narrative summary of the results. Finally, as a post-hoc analysis, once all themes were generated, they were then mapped to the RAI principles identified in Table 1.

Table 3. Main findings organized by ethical principles, Responsible AI principles, themes, and sub-codes with representative excerpts.
3 Results
After abstract and full-text screening of all 10,107 unique articles, 227 articles (2.25%) met criteria for inclusion (Figure 1; Supplementary Appendix 4). The majority of included articles were editorials (n = 96; 42%), review articles (n = 73; 32%), or empirical articles (n = 46; 20%) with the remaining (n = 12, 5%) being composed of other article types (e.g., workshop reports, case studies, etc.) (see Supplementary Appendix 5 for details). Publication dates of articles were concentrated between 2020 and 2024 (n = 203/227; full date range: 2007–2024). Articles originated across 33 countries (first author's country of affiliation), with the vast majority (n = 91; 40%) coming from the US (Figure 2).
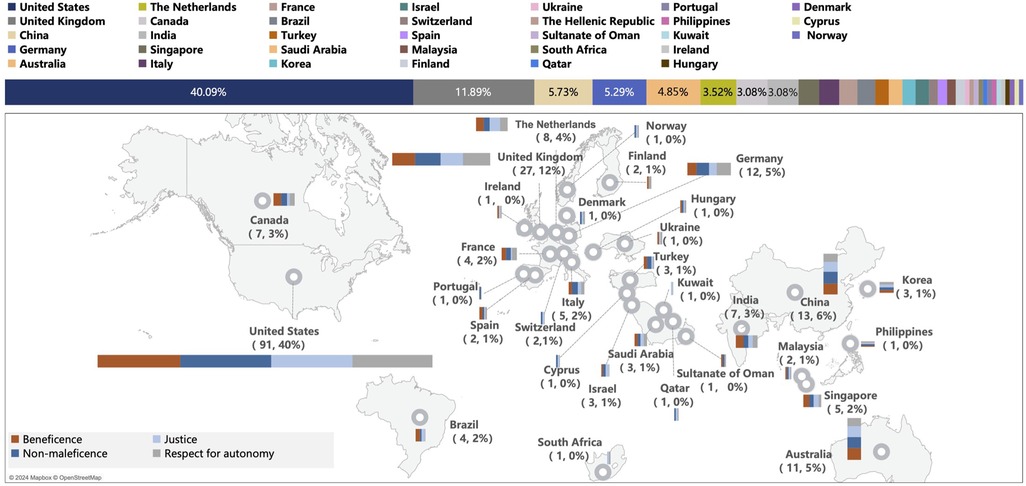
Figure 2. Articles included in review and discussion of issues related to the four principles, by country. Map data from Mapbox and OpenStreetMap.
In Supplementary Appendix 6, we present a non-exhaustive list of example phrases that were considered representative of each principle during abstract screening, highlighting the relevance of each principle to ethical issues in healthcare AI. Semi-inductive thematic analysis revealed that researchers' discussion of ethical considerations of AI use in healthcare spanned across the four principles. Numbers of articles discussing topics related to each of the four principles were quite comparable, including: Beneficence (n = 136), Non-maleficence (n = 148), Respect for Autonomy (n = 130), and Justice (n = 136). Word clouds showing further findings on words mentioned at the highest frequency within coded text for each principle are presented in Supplementary Appendix 7.
A total of 29 more specific ethical issues were identified and treated as sub-codes to the four principles in our analysis. Issues discussed by the highest number of articles included “privacy and data protection” (sub-code to Non-Maleficence; n = 107), “transparency and understandability” (sub-code to Respect for Autonomy; n = 93), “bias and discrimination” (sub-code to Justice; n = 80), “accuracy and efficiency” (sub-code to Beneficence; n = 75), and “equity and fairness” (sub-code to Justice; n = 54). Findings on the four principles and 29 sub-codes were consolidated into themes, summarized below. A list of all themes and sub-codes pertaining to each principle are included in Table 3.
3.1 Narrative summary: relevance of the principle of beneficence
3.1.1 Theme 1: health service quality: accuracy, efficiency, and safety
Articles in our review stated that AI holds promise for addressing human errors and managing escalating healthcare workloads (47–49). It can also be utilized to promote more personalized treatment (50) by tailoring treatment methods based on the specific characteristics and risk status of each patient (51, 52). However, some articles in our review questioned the accuracy and efficiency of AI chatbots, with potentially harmful consequences for patients (53).
3.1.2 Theme 2: patient experience and doctor-patient relationship
The presence of AI will introduce a third party with a shared role in diagnosis, management, and prediction of disease. Some articles suggested that this third party may complicate the traditional healthcare relationship (54) or reduce face-to-face communication, while other articles highlighted how AI can generate comprehensive summaries of patients' medical information and handle other documentation, thus allowing clinicians to spend more time with their patients (52).
3.1.3 Theme 3: social and humanistic dimensions of health services
Several articles in our review emphasized the possibility of incorporating empathy, patient values, and patient preferences into AI-assisted care delivery and decision-making (55). Others suggested that because AI functions based on algorithms, it cannot truly show empathy of the same nature as human providers (56). Particularly in mental healthcare, some articles argued that AI may exacerbate social isolation by inadequately substituting human connection (57, 58).
3.2 Relevance of the principle of non-maleficence
3.2.1 Theme 1: data quality: accuracy, reliability and generalizability
The hazards and risks of AI can be influenced by a variety of factors, including data quality. For example, one article noted that during COVID-19, unreliable data and algorithms led to inaccurate outbreak tracking and predictions (59). Other examples in radiology demonstrated that AI accuracy is influenced by the quality of the data (60).
3.2.2 Theme 2: patient privacy and data protection
Healthcare AI, especially chatbots, collect and use sensitive patient data, posing risks for data leaks and in turn compromising patient security (61, 62). Additionally, the healthcare sector faces higher AI related cyber-attack rates than other industries, with AI systems being exploited to expose vulnerabilities (63). While privacy is a fundamental right, it must often be balanced with public health benefits, such as improved care and research. Notably, large datasets and AI make re-identifying de-identified individuals easier, intensifying ethical concerns (64). Experts call for stricter data regulations, stakeholder education on secure practices, and tighter oversight of AI developers and data users (65–67).
3.2.3 Theme 3: other technology risks and regulatory issues
There is a risk of human overreliance on AI in medicine, with clinicians experiencing “alert fatigue” from excessive information input, such as automated notifications (63). Overuse can harm users' mental health, foster technology addiction, and reduce trust in healthcare (68–70). It was also noted that currently, there is a dearth of regulation concerning many AI models, such as Multimodal Large Language Models, raising safety and ethical concerns (71). There was a consistent message across articles that stronger regulatory frameworks are needed, but developing them requires navigating technical, legal, and ethical challenges (72–74).
3.3 Relevance of the principle of respect for autonomy
3.3.1 Theme 1: patients' right to informed consent
Informed consent in AI-assisted healthcare ensures patients know how their data is used (75). For true informed consent, clinicians, developers, and researchers must explain AI's roles, limitations, and data use implications (62, 76). Current consent procedures are often either overly simple or overly complex, with lengthy terms of service (57). Given the ubiquity of AI integration, patients may unknowingly interact with AI without clarity on data storage and usage (47). Dynamic consent processes are needed, allowing patients to manage and withdraw data sharing at any time (75, 77, 78).
3.3.2 Theme 2: transparency or understandability
The “black-box” nature of algorithms can erode trust when decisions cannot be validated or security risks arise (79). Many articles argued that improving algorithm traceability, reducing bias, and making AI decisions understandable are essential to fostering trust among clinicians and patients (61, 80, 81).
3.3.3 Theme 3: shared decision-making in healthcare
Shared decision-making involves collaboration between clinicians and patients, balancing information, risks, and preferences. AI facilitates this process by analyzing data to identify risks and assist decisions (82). AI-assisted algorithms can aid medical decisions, using large amounts of health data (83). But while AI can leverage big data to guide decisions, it is currently unclear how AI-derived suggestions can be applied more flexibly to account for the dynamic nature of human autonomy and decision-making.
3.4 Relevance of the principle of justice
3.4.1 Theme 1: responsibility and accountability for health service quality
Articles highlighted how AI in healthcare complicates accountability for service quality. Responsibility lies with developers, clinicians, and agencies, requiring clear governance frameworks. Some articles posited that clinicians must always make final decisions, as they are directly accountable, but noted that shared human-AI actions create an “accountability gap,” especially with “black-box” systems (84). Current ethical and legal norms inadequately address responsibility for failures (85). Proposed strategies include clearer guidelines, defining AI's role, and ensuring clinicians retain ultimate responsibility (86). However, health-related AI regulations are still evolving, leaving gaps in accountability for errors (87).
3.4.2 Theme 2: affordability and accessibility of health services
Healthcare AI could significantly improve the accessibility and convenience of medical services by providing remote diagnosis, intelligent assisted diagnosis and treatment, and other new means of healthcare that could enable more patients to receive timely and effective assistance; particularly patients in rural or underserved areas (53, 88). During the COVID-19 outbreak, AI-based services offered patients alternatives to face-to-face visits, saving time, transportation costs, and infection risks (89).
3.4.3 Theme 3: diversity, equity, and inclusion in the context of health
AI bias and discrimination were noted as major concerns, with LLM responses reflecting societal biases in training data, amplifying disparities in healthcare (61, 90). Bias often affects minoritized groups due to underrepresentation in training datasets (81). Addressing this requires more diverse, representative data. Some articles also explored AI's emerging role in equitably allocating scarce public health resources (91, 92).
4 Discussion
The rapid expansion of AI in healthcare has led to the development of numerous, sometimes overlapping or contradictory frameworks (14–26). In this scoping review of 227 articles, we found that the four well-established principles of biomedical ethics (Beneficence, Non-Maleficence, Respect for Autonomy, and Justice) can provide a useful foundational framework for ethical application of AI in healthcare. Our analysis demonstrated that all ethical considerations of the 227 articles mapped onto one or more of the four ethical principles, and consequently their derived themes (see Table 3). Additionally, many of the identified themes corresponded to one or more concerns highlighted by the general principles from Responsible AI (RAI) (Table 1), such as security, inclusivity/fairness, governance, accountability, social/environmental well-being, and transparency (see Table 3 and Narrative Summary in Supplementary Appendix 8 for details). However, in the thematic analysis, two of the themes identified for the principle of Beneficence did not map onto these general RAI principles but are common to healthcare (i.e., 1) patient experience and clinician-patient relationship and 2) social and humanistic dimensions of health services). Collectively, our findings suggest that the four widely accepted principles of biomedical ethics provide a relevant foundation to build upon for ethical evaluation of AI in healthcare and could be used to ground interpretation and prioritization of other RAI frameworks for specific uses in healthcare. While various newer RAI frameworks may offer more specific ethics-related language relevant to applying AI to modern healthcare (93), our findings suggest that the four bio-medical ethical principles can ground existing RAI frameworks by helping to bridge, clarify, and prioritize existing RAI principles while also offering a “safety net” to ensure that foundational healthcare-specific ethical concerns are addressed (94).
Using a classical, widely accepted ethical framework like the four principles presents an opportunity for government bodies and regulatory agencies to establish more straightforward, consistent, and streamlined guidelines for the governance of AI in healthcare. As can be observed by the international spread of articles (33 countries) that met inclusion criteria for our review (see Figure 2), the ethical issues surrounding application of AI in healthcare are a subject of global discourse. This approach allows for evolution of existing policies based on these principles which have both withstood the test of time and have already shaped existing policies in biomedicine. Thus, rather than the creation of completely new guidelines for regulation of AI in healthcare, government and regulatory agencies can instead focus on building upon these foundational biomedical ethical principles and applying them to the current technological moment. In addition to simplifying development of regulations, this would promote universally recognized ethical standards for integration of AI technologies in the healthcare sector. Enabling broad coverage, in turn, will allow for current and future RAI frameworks in healthcare to be as prescriptive as needed and to evolve with technology while maintaining the same foundational four bio-medical ethical principles.
When mapping the literature on AI in healthcare onto the four principles, we found that, similarly to how various areas of RAI overlap (see Table 2), multiple ethical principles are often simultaneously implicated in addressing AI-related issues in healthcare. We believe in some cases this highlights the complementary nature of the four principles in examining different sides of an issue, while in others, it may highlight ethical dilemmas involving tensions between two or more principles. Still other cases may call for prioritizing application of one or more principles over the others.
For example, ethical issues related to use of patient data in AI can be understood to involve all four principles in a manner that encourages examination of various sides of data-related issues (52, 95). When AI models are handling vast amounts of sensitive patient information, ensuring data security becomes paramount (96), and the principle of Non-Maleficence is implicated in the potential for data breaches, as sensitive health information leaks may lead to personal privacy damage, information abuse, identity theft, and other harms (97, 98). In terms of the principle of Respect for Autonomy, data sharing in AI training and analysis raises need for new forms of informed consent (75, 99). Third, the principle of Beneficence underscores the positive potential to use data to improve healthcare and patient outcomes, as well as the need for benefits to individuals and society to outweigh the risks. Lastly, the principle of Justice is invoked when ensuring that data collection and use do not disproportionately burden or benefit particular groups (56, 100).
In other cases, different principles may conflict, raising ethical dilemmas. Rather than nullifying the applicability of the four principles, such cases highlight that the original intention of the four principles was not to stand alone as a comprehensive moral theory but rather to provide a normative framework as a starting point for ethical practice. In addition, the long history of the four principles offers established methods for resolving ethical conflicts and dilemmas, such as the rule of double effect (RDE). The RDE is invoked to justify claims that a single act, which has one or more good effects and one or more harmful effects (such as death), is not always morally prohibited (101). Classical formulations of the RDE identify four conditions or elements (the nature of the act, the agent's intention, the distinction between means and effects, and proportionality between the good effect and the bad effect) that must be satisfied for an act with a double effect to be justified (102). The RDE may serve as a helpful framework when the need arises to judge single instances of apparent contradictions between the potential benefits of applying AI to healthcare (such as improved efficiency and quality of medical services) and its potential negative effects (such as risks of harmful errors and data breaches).
Finally, in some healthcare applications of AI, one or more principles may be especially salient. For example, when considering effects of AI on the patient experience, the principle of Beneficence becomes prominent. Humanistic care emphasizes the need to develop treatment plans that are tailored to the individual needs of patients (56, 103). Future advancements in AI models are needed to enable deeper understanding of contextual nuances of specific patients' situations and to address subtle differences in individual and societal contexts, fostering a more holistic and patient-centered approach to healthcare (55).
This review has several limitations. Firstly, our use of two databases (PubMed and EMBASE) and constrained search terms may have missed relevant papers. Secondly, due to our focus on mapping our results onto an ethical framework and our inclusion of non-empirical studies and the limited empirical literature in this area, it was beyond the scope of this study to evaluate the quality of existing empirical literature on healthcare AI. Finally, AI research is evolving at a rapid pace, necessitating a dynamic dialogue around its advancements and implications. Our review, which by nature is a static summary based on past literature, represents only a snapshot of existing knowledge up to this point, potentially lagging behind the most recent developments in the field, which future studies should continue to address.
In conclusion, risks associated with the application of AI in healthcare may be high stakes (104, 105). Medical decisions directly impact the quality of life, health, and safety of patients, meaning that any technical errors or ethical misconduct can have serious consequences. Given the already extensive adoption and evolving use cases of AI in healthcare—from using AI to generate research questions, to diagnostic assistance and personalized treatment planning, to patient monitoring—ensuring technological reliability and ethical protections has become particularly critical. Our research suggests that the four widely accepted principles of biomedical ethics (Beneficence, Non-Maleficence, Respect for Autonomy, and Justice) provide a relevant foundation for ethical evaluation of AI engagement in healthcare to build upon and can be used to ground interpretation and prioritization in other Responsible AI Frameworks. These four principles can be an organizing framework to address gaps that may exist in current policies and regulations, in addition to bridging, clarifying, prioritizing, while also offering a “safety net” for handling healthcare specific ethical concerns. By grounding emerging regulatory mechanisms in these established ethical guidelines, we can better construct a comprehensive governance system that promotes the responsible application of AI in the healthcare sector.
Author contributions
AG: Investigation, Visualization, Conceptualization, Writing – review & editing, Writing – original draft, Methodology, Validation, Data curation, Formal analysis. ML: Conceptualization, Validation, Investigation, Data curation, Writing – review & editing, Writing – original draft, Software, Methodology, Visualization. JH: Visualization, Writing – original draft, Validation, Writing – review & editing, Data curation, Supervision, Investigation, Conceptualization, Methodology. JW: Investigation, Conceptualization, Software, Writing – original draft, Methodology, Data curation. YR: Data curation, Writing – original draft, Methodology, Conceptualization, Software, Investigation. LY: Writing – original draft, Methodology, Software, Investigation, Data curation, Conceptualization. XZ: Validation, Supervision, Writing – review & editing. XL: Validation, Supervision, Writing – review & editing. XW: Supervision, Methodology, Validation, Conceptualization, Visualization, Writing – review & editing, Formal analysis, Data curation. RB: Writing – review & editing, Validation, Supervision, Methodology. BC: Validation, Writing – review & editing, Supervision, Methodology.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. AG was supported by NSF DGE-213989. ML was supported by the Fundamental Research Funds for the Central Universities of Central South University (grant number CX20240157). JH was supported by T32AG000030-47. XW was supported by the Scientific Research Project of Health Commission of Hunan Province (grant number B202315018734) and by the General Project of Hunan Provincial Social Science Foundation (project number 24YBA036).
Acknowledgments
The authors would like to thank Heyun Lee, Yichen Zhang, Tanish Sathish, Alaivrya Theard, Ruohan Yang, and Annabelle Winssinger for their assistance in verifying data for tables and figures.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2025.1662642/full#supplementary-material
References
1. Chen M, Zhang B, Cai Z, Seery S, Gonzalez MJ, Ali NM, et al. Acceptance of clinical artificial intelligence among physicians and medical students: a systematic review with cross-sectional survey. Front Med (Lausanne). (2022) 9:990604. doi: 10.3389/fmed.2022.990604
2. American Medical Association. AMA Augmented Intelligence Research. Chicago, IL: American Medical Association (2023).
3. Maleki Varnosfaderani S, Forouzanfar M. The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering (Basel). (2024) 11(4):337. doi: 10.3390/bioengineering11040337
4. Alanazi A. Using machine learning for healthcare challenges and opportunities. Inform Med Unlocked. (2022) 30:100924. doi: 10.1016/j.imu.2022.100924
5. LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. (2015) 521(7553):436–44. doi: 10.1038/nature14539
6. Funk AT, Pasquini G, Spencer A, Cary F. 60% of Americans Would Be Uncomfortable With Provider Relying on AI in Their Own Health Care. Washington, DC: Pew Research Center (2023). Available online at: https://www.pewresearch.org/science/2023/02/22/60-of-americans-would-be-uncomfortable-with-provider-relying-on-ai-in-their-own-health-care/ (Accessed July 31, 2024).
7. Mennella C, Maniscalco U, De Pietro G, Esposito M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon. (2024) 10(4):e26297. doi: 10.1016/j.heliyon.2024.e26297
8. Liaw ST, Liyanage H, Kuziemsky C, Terry AL, Schreiber R, Jonnagaddala J, et al. Ethical use of electronic health record data and artificial intelligence: recommendations of the primary care informatics working group of the international medical informatics association. Yearb Med Inform. (2020) 29(1):51–7. doi: 10.1055/s-0040-1701980
9. Arora RK, Wei J, Hicks RS, Bowman P, Quinonero-Candela J, Tsimpourlas F, et al. HealthBench: Evaluating Large Language Models Towards Improved Human Health.
10. IBM. What is AI Ethics? (2021). Available online at: https://www.ibm.com/think/topics/ai-ethics (Accessed December 18, 2024).
12. The IEEE Global Initiative on Ethics of, Autonomous and Intelligent Systems. Ethically Aligned Design: A Vision for Prioritizing Human Well-being with Autonomous and Intelligent Systems, Version 2. Piscataway, NJ: IEEE (2017). (Intelligent Systems, Control and Automation: Science and Engineering). Available online at: http://link.springer.com/10.1007/978-3-030-12524-0_2 (Accessed December 18, 2024).
13. OECD. AI Principles. Available online at: https://www.oecd.org/en/topics/ai-principles.html (Accessed December 18, 2024).
14. The White House. Blueprint for an AI Bill of Rights | OSTP. Available online at: https://www.whitehouse.gov/ostp/ai-bill-of-rights/ (Accessed August 4, 2024).
15. National Institute of Standards and Technology (NIST). Trustworthy and Responsible AI. Gaithersburg, MD: NIST (2022). Available online at: https://www.nist.gov/trustworthy-and-responsible-ai (Accessed August 4, 2024).
16. Ministry of Science and Technology of the People’s Republic of China. Ethical Code for the New Generation of Artificial Intelligence. Available online at: https://www.most.gov.cn/kjbgz/202109/t20210926_177063.html (Accessed November 3, 2024).
17. Office of the Central Cyberspace Affairs Commission, a division under the Cyberspace Administration of China (CAC). Global AI Governance Initiative_Office of the Central Cyberspace Affairs Commission. Available online at: https://www.cac.gov.cn/2023-10/18/c_1699291032884978.htm (Accessed November 3, 2024).
18. Ministry of Industry and information Technology of the People’s Republic of China. Guidelines for the Construction of National Artificial Intelligence Industry Comprehensive Standardization System (2024 Edition). Available online at: https://www.gov.cn/zhengce/zhengceku/202407/content_6960720.htm (Accessed November 6, 2024).
19. General Office of the CPC Central Committee and the General Office of the State Council. Opinions on Strengthening the Governance of Science and Technology Ethics. Available online at: https://www.gov.cn/gongbao/content/2022/content_5683838.htm (Accessed November 6, 2024).
20. Oniani D, Hilsman J, Peng Y, Poropatich RK, Pamplin JC, Legault GL, et al. Adopting and expanding ethical principles for generative artificial intelligence from military to healthcare. npj Digit Med. (2023) 6(1):1–10. doi: 10.1038/s41746-023-00965-x
21. National Academy of Medicine. Health Care Artificial Intelligence Code of Conduct. Available online at: https://nam.edu/programs/value-science-driven-health-care/health-care-artificial-intelligence-code-of-conduct/ (Accessed August 4, 2024).
22. Hill B. CHAI Releases Draft Responsible Health AI Framework for Public Comment. Washington, DC: CHAI - Coalition for Health AI (2024). Available online at: https://chai.org/chai-releases-draft-responsible-health-ai-framework-for-public-comment/ (Accessed August 4, 2024).
23. LCFI - Leverhulme Centre for the Future of Intelligence. Leverhulme Centre for the Future of Intelligence. Available online at: https://www.lcfi.ac.uk (Accessed August 4, 2024).
24. Home | Stanford HAI. (2024). Available online at: https://hai.stanford.edu/ (Accessed August 4, 2024).
25. UKRI Trustworthy Autonomous Systems Hub. Available online at: http://tas.ac.uk/ (Accessed August 4, 2024).
26. Ethics and Governance of Artificial Intelligence for Health: WHO Guidance. Geneva: World Health Organization (2021).
27. EU Artificial Intelligence Act. Up-to-Date Developments and Analyses of the EU AI Act. (2024). Available online at: https://artificialintelligenceact.eu/ (Accessed December 18, 2024).
28. Sadek M, Kallina E, Bohné T, Mougenot C, Calvo RA, Cave S. Challenges of responsible AI in practice: scoping review and recommended actions. AI Soc. (2025) 40(1):199–215. doi: 10.1007/s00146-024-01880-9
29. Japkowicz N, Stephen S. The class imbalance problem: a systematic study1. Intell Data Anal. (2002) 6(5):429–49. doi: 10.3233/IDA-2002-6504
30. Gohil V, Dev S, Upasani G, Lo D, Ranganathan P, Delimitrou C. The importance of generalizability in machine learning for systems. IEEE Comput Arch Lett. (2024) 23(1):95–8. doi: 10.1109/LCA.2024.3384449
31. Dixon D, Sattar H, Moros N, Kesireddy SR, Ahsan H, Lakkimsetti M, et al. Unveiling the influence of AI predictive analytics on patient outcomes: a comprehensive narrative review. Cureus. (2024) 16(5):e59954. doi: 10.7759/cureus.59954
32. Whittlestone J, Nyrup R, Alexandrova A, Cave S. The role and limits of principles in AI ethics: towards a focus on tensions. Proceedings of the 2019 AAAI/ACM Conference on AI, Ethics, and Society. Honolulu, HI, USA: ACM (2019). p. 195–200. Available online at: https://dl.acm.org/doi/10.1145/3306618.3314289 (Accessed May 7, 2025).
33. Narayanan M, Schoeberl C. A Matrix for Selecting Responsible AI Frameworks. Washington, DC: Center for Security and Emerging Technology (2023). Available online at: https://cset.georgetown.edu/publication/a-matrix-for-selecting-responsible-ai-frameworks/ (Accessed May 17, 2025).
34. Schiff GD. AI-driven clinical documentation—driving out the chitchat? N Engl J Med. (2025) 392(19):1877–9. doi: 10.1056/NEJMp2416064
35. Sîrbu CL, Mercioni MA. Fostering trust in AI-driven healthcare: a brief review of ethical and practical considerations. 2024 International Symposium on Electronics and Telecommunications (ISETC) (2024). p. 1–4. Available online at: https://ieeexplore.ieee.org/document/10797264 (Accessed July 24, 2025).
36. Ong JCL, Chang SYH, William W, Butte AJ, Shah NH, Chew LST, et al. Medical ethics of large language models in medicine. NEJM AI. (2024) 1(7):AIra2400038. doi: 10.1056/AIra2400038
37. Beauchamp TL. In: Childress JF, editor. Principles of Biomedical Ethics. New York: Oxford University Press (1979).
38. Beauchamp TL. The ‘four Principles’ approach to health care ethics. In: Ashcroft RE, Dawson A, Draper H, McMillan JR, editors 1st ed. Principles of Health Care Ethics. Hoboken, NJ: Wiley (2006). p. 3–10.
39. Farhud DD, Zokaei S. Ethical issues of artificial intelligence in medicine and healthcare. Iran J Public Health. (2021) 50(11):i–v.
40. Mak S, Thomas A. Steps for conducting a scoping review. J Grad Med Educ. (2022) 14(5):565–7. doi: 10.4300/JGME-D-22-00621.1
41. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
42. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5(1):210. doi: 10.1186/s13643-016-0384-4
43. Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC, et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. (2023) 21(3):520–32. doi: 10.11124/JBIES-22-00123
44. NVivo. Lumivero (2017). Available online at: http://www.lumivero.com
45. Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. (2006) 5(1):80–92. doi: 10.1177/160940690600500107
46. Roberts K, Dowell A, Nie JB. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med Res Methodol. (2019) 19:66. doi: 10.1186/s12874-019-0707-y
47. Nazir A, Wang Z. A comprehensive survey of ChatGPT: advancements, applications, prospects, and challenges. Meta-Radiology. (2023) 1(2):100022. doi: 10.1016/j.metrad.2023.100022
48. Hua D, Petrina N, Young N, Cho JG, Poon SK. Understanding the factors influencing acceptability of AI in medical imaging domains among healthcare professionals: a scoping review. Artif Intell Med. (2024) 147:102698. doi: 10.1016/j.artmed.2023.102698
49. Koski E, Murphy J. AI in healthcare. In: Honey M, Ronquillo C, Lee T-T, Westbrooke L, editors. Nurses and Midwives in the Digital Age. Amsterdam: IOS Press (2021). p. 295–9. Available online at: https://ebooks.iospress.nl/doi/10.3233/SHTI210726 (Accessed November 9, 2024).
50. Etienne H, Hamdi S, Le Roux M, Camuset J, Khalife-Hocquemiller T, Giol M, et al. Artificial intelligence in thoracic surgery: past, present, perspective and limits. Eur Respir Rev. (2020) 29(157):200010. doi: 10.1183/16000617.0010-2020
51. Gauss T, Perkins Z, Tjardes T. Current knowledge and availability of machine learning across the spectrum of trauma science. Curr Opin Crit Care. (2023) 29(6):713–21.37861197
52. Ahmed MN, Toor AS, O’Neil K, Friedland D. Cognitive computing and the future of health care cognitive computing and the future of healthcare: the cognitive power of IBM Watson has the potential to transform global personalized medicine. IEEE Pulse. (2017) 8(3):4–9. doi: 10.1109/MPUL.2017.2678098
53. Bernstein IA, Zhang YV, Govil D, Majid I, Chang RT, Sun Y, et al. Comparison of ophthalmologist and large language model chatbot responses to online patient eye care questions. JAMA Netw Open. (2023) 6(8):e2330320. doi: 10.1001/jamanetworkopen.2023.30320
54. Li LT, Haley LC, Boyd AK, Bernstam EV. Technical/algorithm, stakeholder, and society (TASS) barriers to the application of artificial intelligence in medicine: a systematic review. J Biomed Inform. (2023) 147:104531. doi: 10.1016/j.jbi.2023.104531
55. Dankwa-Mullan I, Weeraratne D. Artificial intelligence and machine learning technologies in cancer care: addressing disparities, bias, and data diversity. Cancer Discov. (2022) 12(6):1423–7. doi: 10.1158/2159-8290.CD-22-0373
56. Li W, Ge X, Liu S, Xu L, Zhai X, Yu L. Opportunities and challenges of traditional Chinese medicine doctors in the era of artificial intelligence. Front Med (Lausanne). (2023) 10:1336175. doi: 10.3389/fmed.2023.1336175
57. Zhu J, Shi K, Yang C, Niu Y, Zeng Y, Zhang N, et al. Ethical issues of smart home-based elderly care: a scoping review. J Nurs Manag. (2022) 30(8):3686–99. doi: 10.1111/jonm.13521
58. Bickmore TW. Relational agents in health applications: leveraging affective computing to promote healing and wellness. In: Calvo R, D’Mello S, Gratch J, Kappas A, editors. The Oxford Handbook of Affective Computing. Oxford: Oxford University Press (2015). p. 537–46.
59. Zhao IY, Ma YX, Yu MWC, Liu J, Dong WN, Pang Q, et al. Ethics, integrity, and retributions of digital detection surveillance systems for infectious diseases: systematic literature review. J Med Internet Res. (2021) 23(10):e32328. doi: 10.2196/32328
60. Mese I, Taslicay CA, Sivrioglu AK. Improving radiology workflow using ChatGPT and artificial intelligence. Clin Imaging. (2023) 103:109993. doi: 10.1016/j.clinimag.2023.109993
61. Jeyaraman M, Ramasubramanian S, Balaji S, Jeyaraman N, Nallakumarasamy A, Sharma S. ChatGPT in action: harnessing artificial intelligence potential and addressing ethical challenges in medicine, education, and scientific research. World J Methodol. (2023) 13(4):170–8. doi: 10.5662/wjm.v13.i4.170
62. Diaz-Asper C, Hauglid MK, Chandler C, Cohen AS, Foltz PW, Elvevåg B. A framework for language technologies in behavioral research and clinical applications: ethical challenges, implications, and solutions. Am Psychol. (2024) 79(1):79–91. doi: 10.1037/amp0001195
63. González-Gonzalo C, Thee EF, Klaver CCW, Lee AY, Schlingemann RO, Tufail A, et al. Trustworthy AI: closing the gap between development and integration of AI systems in ophthalmic practice. Prog Retinal Eye Res. (2022) 90:101034. doi: 10.1016/j.preteyeres.2021.101034
64. Goodman KW. Ethics in health informatics. Yearb Med Inform. (2020) 29(1):26–31. doi: 10.1055/s-0040-1701966
65. Coventry L, Branley D. Cybersecurity in healthcare: a narrative review of trends, threats and ways forward. Maturitas. (2018) 113:48–52. doi: 10.1016/j.maturitas.2018.04.008
66. Lam K, Abràmoff MD, Balibrea JM, Bishop SM, Brady RR, Callcut RA, et al. A Delphi consensus statement for digital surgery. NPJ Digit Med. (2022) 5(1):100. doi: 10.1038/s41746-022-00641-6
67. Luu VP, Fiorini M, Combes S, Quemeneur E, Bonneville M, Bousquet PJ. Challenges of artificial intelligence in precision oncology: public-private partnerships including national health agencies as an asset to make it happen. Ann Oncol. (2024) 35(2):154–8. doi: 10.1016/j.annonc.2023.09.3106
68. Kretzschmar K, Tyroll H, Pavarini G, Manzini A, Singh I, Neurox Young People’s Advisory Group. Can your phone be your therapist? young people’s ethical perspectives on the use of fully automated conversational agents (Chatbots) in mental health support. Biomed Inform Insights. (2019) 11:1178222619829083. doi: 10.1177/1178222619829083
69. Grote T, Berens P. How competitors become collaborators-bridging the gap(s) between machine learning algorithms and clinicians. Bioethics. (2022) 36(2):134–42. doi: 10.1111/bioe.12957
70. Burr C, Taddeo M, Floridi L. The ethics of digital well-being: a thematic review. Sci Eng Ethics. (2020) 26(4):2313–43. doi: 10.1007/s11948-020-00175-8
71. Meskó B. The impact of multimodal large language models on health care’s future. J Med Internet Res. (2023) 25:e52865. doi: 10.2196/52865
72. Paladugu PS, Ong J, Nelson N, Kamran SA, Waisberg E, Zaman N, et al. Generative adversarial networks in medicine: important considerations for this emerging innovation in artificial intelligence. Ann Biomed Eng. (2023) 51(10):2130–42. doi: 10.1007/s10439-023-03304-z
73. Alhasan K, Raina R, Jamal A, Temsah MH. Combining human and AI could predict nephrologies future, but should be handled with care. Acta Paediatr. (2023) 112(9):1844–8. doi: 10.1111/apa.16867
74. Arshad HB, Butt SA, Khan SU, Javed Z, Nasir K. ChatGPT and artificial intelligence in hospital level research: potential, precautions, and prospects. Methodist Debakey Cardiovasc J. (2023) 19(5):77. doi: 10.14797/mdcvj.1290
75. Stogiannos N, Malik R, Kumar A, Barnes A, Pogose M, Harvey H, et al. Black box no more: a scoping review of AI governance frameworks to guide procurement and adoption of AI in medical imaging and radiotherapy in the UK. Br J Radiol. (2023) 96(1152):20221157. doi: 10.1259/bjr.20221157
76. Alfano L, Malcotti I, Ciliberti R. Psychotherapy, artificial intelligence and adolescents: ethical aspects. J Prev Med Hyg. (2024) 64(4):E438.38379752
77. Batlle JC, Dreyer K, Allen B, Cook T, Roth CJ, Kitts AB, et al. Data sharing of imaging in an evolving health care world: report of the ACR data sharing workgroup, part 1: data ethics of privacy, consent, and anonymization. J Am Coll Radiol. (2021) 18(12):1646–54. doi: 10.1016/j.jacr.2021.07.014
78. Borgstadt JT, Kalpas EA, Pond HM. A qualitative thematic analysis of addressing the why: an artificial intelligence (AI) in healthcare symposium. Cureus. (2022) 14(3):e23704.35510027
79. Fisher S, Rosella LC. Priorities for successful use of artificial intelligence by public health organizations: a literature review. BMC Public Health. (2022) 22:2146. doi: 10.1186/s12889-022-14422-z
80. Halm-Pozniak A, Lohmann CH, Zagra L, Braun B, Gordon M, Grimm B. Best practice in digital orthopaedics. EFORT Open Rev. (2023) 8(5):283–90. doi: 10.1530/EOR-23-0081
81. Di Nuovo A. Letter to the editor: “how can biomedical engineers help empower individuals with intellectual disabilities? The potential benefits and challenges of AI technologies to support inclusivity and transform lives”. IEEE J Transl Eng Health Med. (2023) 12:256–7. doi: 10.1109/JTEHM.2023.3331977
82. Hariharan V, Harland TA, Young C, Sagar A, Gomez MM, Pilitsis JG. Machine learning in spinal cord stimulation for chronic pain. Oper Neurosurg (Hagerstown). (2023) 25(2):112–6. doi: 10.1227/ons.0000000000000774
83. Arnold MH. Teasing out artificial intelligence in medicine: an ethical critique of artificial intelligence and machine learning in medicine. J Bioeth Inq. (2021) 18(1):121. doi: 10.1007/s11673-020-10080-1
84. Joda T, Zitzmann NU. Personalized workflows in reconstructive dentistry-current possibilities and future opportunities. Clin Oral Investig. (2022) 26(6):4283–90. doi: 10.1007/s00784-022-04475-0
85. Kellmeyer P. Artificial intelligence in basic and clinical neuroscience: opportunities and ethical challenges. Neuroforum. (2019) 25(4):241–50. doi: 10.1515/nf-2019-0018
86. Li W, Fu M, Liu S, Yu H. Revolutionizing neurosurgery with GPT-4: a leap forward or ethical conundrum? Ann Biomed Eng. (2023) 51(10):2105–12. doi: 10.1007/s10439-023-03240-y
87. Dzobo K, Adotey S, Thomford NE, Dzobo W. Integrating artificial and human intelligence: a partnership for responsible innovation in biomedical engineering and medicine. OMICS. (2020) 24(5):247–63. doi: 10.1089/omi.2019.0038
88. Mese I. Letter to the editor—leveraging virtual reality-augmented reality technologies to complement artificial intelligence-driven healthcare: the future of patient–doctor consultations. Eur J Cardiovasc Nurs. (2024) 23(1):e9–10. doi: 10.1093/eurjcn/zvad043
89. Bhardwaj A. Promise and provisos of artificial intelligence and machine learning in healthcare. J Healthc Leadersh. (2022) 14:113–8. doi: 10.2147/JHL.S369498
90. Dixon BE, Holmes JH. Special section on inclusive digital health: notable papers on addressing bias, equity, and literacy to strengthen health systems. Yearb Med Inform. (2022) 31(1):100. doi: 10.1055/s-0042-1742536
91. Sim JZT, Bhanu Prakash KN, Huang WM, Tan CH. Harnessing artificial intelligence in radiology to augment population health. Front Med Technol. (2023) 5:1281500. doi: 10.3389/fmedt.2023.1281500
92. Mollura DJ, Culp MP, Pollack E, Battino G, Scheel JR, Mango VL, et al. Artificial intelligence in low- and middle-income countries: innovating global health radiology. Radiology. (2020) 297(3):513–20. doi: 10.1148/radiol.2020201434
93. Bouderhem R. Shaping the future of AI in healthcare through ethics and governance. Humanit Soc Sci Commun. (2024) 11(1):1–12. doi: 10.1057/s41599-024-02894-w
94. Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. (2021) 30(1):17–28. doi: 10.1159/000509119
95. Ahmed Z, Mohamed K, Zeeshan S, Dong X. Artificial intelligence with multi-functional machine learning platform development for better healthcare and precision medicine. Database (Oxford). (2020) 2020:baaa010. doi: 10.1093/database/baaa010
96. Parker W, Jaremko JL, Cicero M, Azar M, El-Emam K, Gray BG, et al. Canadian association of radiologists white paper on de-identification of medical imaging: part 2, practical considerations. Can Assoc Radiol J. (2021) 72(1):25–34. doi: 10.1177/0846537120967345
97. Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. (2021) 22(1):122. doi: 10.1186/s12910-021-00687-3
98. Matheny ME, Whicher D, Thadaney Israni S. Artificial intelligence in health care: a report from the national academy of medicine. JAMA. (2020) 323(6):509–10. doi: 10.1001/jama.2019.21579
99. Niel O, Bastard P. Artificial intelligence in nephrology: core concepts, clinical applications, and perspectives. Am J Kidney Dis. (2019) 74(6):803–10. doi: 10.1053/j.ajkd.2019.05.020
100. Zidaru T, Morrow EM, Stockley R. Ensuring patient and public involvement in the transition to AI-assisted mental health care: a systematic scoping review and agenda for design justice. Health Expect. (2021) 24(4):1072–124. doi: 10.1111/hex.13299
101. Cavanaugh TA. Double-Effect Reasoning. Oxford: Oxford University Press (2006). (Oxford Studies in Theological Ethics). Available online at: https://global.oup.com/academic/product/double-effect-reasoning-9780199272198 (Accessed November 15, 2024).
102. Uniacke SM. The doctrine of double effect. The Thomist. (1984) 48(2):188–218. doi: 10.1353/tho.1984.0039
103. Pagliari C. Digital health and primary care: past, pandemic and prospects. J Glob Health. (2021) 11:01005. doi: 10.7189/jogh.11.01005
104. Lee D, Yoon SN. Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int J Environ Res Public Health. (2021) 18(1):271. doi: 10.3390/ijerph18010271
105. Secinaro S, Calandra D, Secinaro A, Muthurangu V, Biancone P. The role of artificial intelligence in healthcare: a structured literature review. BMC Med Inform Decis Mak. (2021) 21(1):125. doi: 10.1186/s12911-021-01488-9
106. Papagiannidis E, Mikalef P, Conboy K. Responsible artificial intelligence governance: a review and research framework. J Strat Inf Syst. (2025) 34(2):101885. doi: 10.1016/j.jsis.2024.101885
107. Haltaufderheide J, Ranisch R. The ethics of ChatGPT in medicine and healthcare: a systematic review on large language models (LLMs). npj Digit Med. (2024) 7(1):1–11. doi: 10.1038/s41746-024-01157-x
108. Hartmann V, Suri A, Bindschaedler V, Evans D, Tople S, West R. SoK: Memorization in General-Purpose Large Language Models (2023). arXiv. Available online at: http://arxiv.org/abs/2310.18362 (Accessed December 18, 2024).
109. Longpre S, Mahari R, Obeng-Marnu N, Brannon W, South T, Kabbara J, et al. Data Authenticity, Consent, and Provenance for AI are All Broken: What Will It Take to Fix Them? An MIT Exploration of Generative AI (2024). Available online at: https://mit-genai.pubpub.org/pub/uk7op8zs/release/2 (Accessed November 6, 2024).
110. Habli I, Lawton T, Porter Z. Artificial intelligence in health care: accountability and safety. Bull World Health Organ. (2020) 98(4):251–6. doi: 10.2471/BLT.19.237487
111. Kokolis A, Kuchnik M, Hoffman J, Kumar A, Malani P, Ma F, et al. Revisiting Reliability in Large-Scale Machine Learning Research Clusters (2024). arXiv. Available online at: http://arxiv.org/abs/2410.21680 (Accessed December 18, 2024).
112. Bloomfield P, Clutton-Brock P, Pencheon E, Magnusson J, Karpathakis K. Artificial intelligence in the NHS: climate and emissions✰,✰✰. J Climate Change Health. (2021) 4:100056. doi: 10.1016/j.joclim.2021.100056
113. Forghani R. A practical guide for AI algorithm selection for the radiology department. Semin Roentgenol. (2023) 58(2):208–13. doi: 10.1053/j.ro.2023.02.006
114. Kremer T, Murray N, Buckley J, Rowan NJ. Use of real-time immersive digital training and educational technologies to improve patient safety during the processing of reusable medical devices: Quo Vadis? Sci Total Environ. (2023) 900:165673. doi: 10.1016/j.scitotenv.2023.165673
115. Wong RSY, Ming LC, Raja Ali RA. The intersection of ChatGPT, clinical medicine, and medical education. JMIR Med Educ. (2023) 9:e47274. doi: 10.2196/47274
116. Pashkov VM, Harkusha AO, Harkusha YO. Artificial intelligence in medical practice: regulative issues and perspectives. Wiad Lek. (2020) 73(12 cz 2):2722–7. doi: 10.36740/WLek202012204
Keywords: ethics, Artificial Intelligence, Responsible AI, healthcare, Beneficence, Non-Maleficence, Autonomy, Justice
Citation: Gorelik AJ, Li M, Hahne J, Wang J, Ren Y, Yang L, Zhang X, Liu X, Wang X, Bogdan R and Carpenter BD (2025) Ethics of AI in healthcare: a scoping review demonstrating applicability of a foundational framework. Front. Digit. Health 7:1662642. doi: 10.3389/fdgth.2025.1662642
Received: 9 July 2025; Accepted: 25 August 2025;
Published: 10 September 2025.
Edited by:
Stephen Gbenga Fashoto, Namibia University, NamibiaReviewed by:
Michaela Th. Mayrhofer, Papillon Pathways e.U., AustriaCristina Sirbu, Polytechnic University of Timisoara, Romania
Copyright: © 2025 Gorelik, Li, Hahne, Wang, Ren, Yang, Zhang, Liu, Wang, Bogdan and Carpenter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaomin Wang, eGlhb21pbndhbmdAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Aaron J. Gorelik
Aaron J. Gorelik Mengyuan Li2,†
Mengyuan Li2,† Jessica Hahne
Jessica Hahne Xing Liu
Xing Liu Xiaomin Wang
Xiaomin Wang Ryan Bogdan
Ryan Bogdan