- 1Department of Internal Medicine, Yale School of Medicine, New Haven, CT, United States
- 2Department of Pediatrics, Yale School of Medicine, New Haven, CT, United States
- 3Department of Pathology, Yale School of Medicine, New Haven, CT, United States
- 4Department of Radiology, Yale School of Medicine, New Haven, CT, United States
- 5Department of Internal Medicine, Yale Center for Genome Analysis, New Haven, CT, United States
- 6Department of Neurology, Yale School of Medicine, New Haven, CT, United States
- 7Department of Cellular and Molecular Physiology, Yale University, New Haven, CT, United States
Background: Gaucher disease (GD) is characterized by significant phenotypic heterogeneity, even among patients with identical GBA1 genotypes, suggesting the role of genetic and/or epigenetic modifiers. The enzymatic defect and pathological accumulation of glucosylceramide (GlcCer) lead to chronic metabolic inflammation, providing ample opportunities for interaction with other biological pathways to influence disease expression. Herein, we developed a model of precision medicine in this prototype single-gene disorder.
Methods: This study leveraged a well-characterized, longitudinally followed cohort of GD patients from a major tertiary care center, integrating whole-exome sequencing (WES) with detailed clinical information. We applied a precision medicine framework centered on four components—clinical reasoning, deep phenotyping, genomic integration, and individualized therapy—to a subset of patients (n = 17) who presented with complex phenotypes deviating from the classical GD presentation and/or were a priori suspected of harboring a second genetic disorder.
Results: Of 275 patients, 17 (6.2%) presented with atypical phenotypes not fully explained by GD. WES revealed additional genetic diagnoses, including hereditary hemochromatosis-associated variants (n = 5), familial Mediterranean fever (n = 4), homozygous MSH6 mutation-associated hereditary cancer predisposition (n = 2), and autosomal dominant polycystic kidney disease (ADPKD) (n = 2).
Conclusion: The presence of concurrent genetic disorders in a subset of GD patients has the potential to modify clinical presentation, impact disease trajectory, and introduce additional complexities in clinical management. This study contributes to advancing precision medicine strategies that aim to optimize patient outcomes. Future research into genetic and epigenetic modifiers of GD will further refine this framework and enhance individualized therapeutic approaches.
1 Introduction
Gaucher disease (GD) is a prototype lysosomal storage disorder caused by biallelic mutations in the GBA1 gene. These mutations lead to a deficiency of the lysosomal enzyme acid β-glucosidase (Grabowski et al., 2021). The enzymatic defect results in the accumulation of bioactive lipids, glucosylceramide (GlcCer), and glucosylsphingosine (GlcSph). Consequently, there is a generalized dysfunction of the lysosomal system, immune activation, and metabolic inflammation. The hallmark of GD pathology is the multisystemic buildup of lipid-laden macrophages, known as Gaucher cells. GD is broadly classified into three phenotypes: type 1 (GD1) (non-neuronopathic, lacking childhood-onset neurodegenerative disease) and the childhood-onset neuronopathic forms, type 2 (GD2) (acute, infantile onset) and type 3 (GD3) (chronic) (Mistry et al., 2011). While some genotype–phenotype correlations exist—such as the association of the p.Leu483Pro homozygous mutation with neuronopathic disease (nGD) and the p.Asn409Ser mutation with type 1 GD—phenotypic variability remains striking (Grabowski et al., 2019). Even among individuals with identical GBA1 genotypes or among affected siblings, there can be profound differences in disease severity and presentation, challenging the traditional genotype–phenotype model (Sidransky, 2012).
While GD is a monogenic disorder, this variability suggests that additional factors, including genetic, epigenetic, or environmental modifiers, may play significant roles in shaping the clinical manifestations of the disease. By modulating penetrance, expressivity, and pleiotropy, such modifiers can intricately adjust cellular and organismic responses to GBA1 mutations, thereby sculpting the clinical landscape of GD beyond the confines of traditional genotype–phenotype correlations. These modifiers may influence critical pathways, such as immune regulation, inflammation, and lysosomal function, further complicating disease expression. However, genotype–phenotype studies in GD have been limited by its rarity and extreme heterogeneity, making it difficult to draw robust conclusions from small cohorts. Some researchers have approached GD as a phenotypic continuum, ranging from asymptomatic GD1 to severe GD2 (Sidransky, 2004). Genome-wide association studies (GWAS) and candidate gene studies have offered insights, but much remains unexplained (Zhang et al., 2012; Velayati et al., 2011; Lo et al., 2011).
We posit that a phenotype-first approach has broad utility in GD for investigating the impact of genomic background and modifier genes underlying the phenotypic heterogeneity observed among patients with identical GBA1 mutations. This approach not only helps elucidate disease variability but also contributes to the development of a precision medicine model for GD. Notably, significant advances have been made using this strategy in patients with GD who develop Parkinson’s disease (Blauwendraat et al., 2023).
Our long-term goal has been to understand the genomic basis of phenotypic diversity in GD (Zhang et al., 2012). To achieve this, our cohort underwent deep phenotyping and whole-exome sequencing (WES) as part of a systematic investigation into disease variability. Here, we focused on a subset of 17 patients who deviated from the classical GD phenotype due to multiple molecular diagnoses and/or were a priori suspected of harboring a second genetic disorder based on family history. Our objective was to evaluate the utility of WES in Gaucher patients with atypical presentations to investigate the genomic basis of phenotypic variability, and to develop a precision medicine framework for individualized patient care. Leveraging this approach, we examined the WES data from this subset to correlate genetic findings with their respective phenotypes. The cases described highlight key pillars of precision medicine as applied to a single-gene disease order, namely, deep phenotyping, longitudinal natural history, clinical reasoning, genomic data, and individualized therapy for holistic disease management.
2 Materials and methods
2.1 Study design and cohort
The Yale Gaucher Disease Center is a destination center for GD patients who undergo comprehensive evaluations 1–2 times per year. Our cohort (n = 275) has been followed for up to 26 years (range: 7 months to 26 years), with systematic collection of clinical, genetic (WES), and laboratory data. All patients were confirmed to have GD based on low acid β-glucosidase activity in peripheral blood leucocytes and biallelic GBA1 mutations. For precise GBA1 genotyping, we employed a combination of PacBio long-read sequencing, WES, and Sanger sequencing to ensure accurate variant detection (Drelichman et al., 2021).
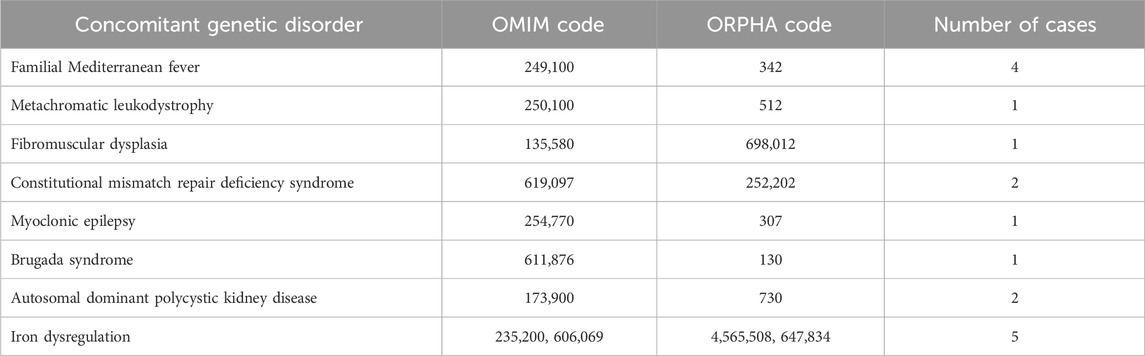
We employ a phenotype-first approach to investigate the genetic basis of phenotypic variability in GD. Here, we focused on a subset of 17 patients who exhibited unusual phenotypes in GD. The concept for our study is depicted in Figure 1, which illustrates the spectrum of atypical phenotypic features observed in our cohort that signaled the presence of additional genetic diagnoses beyond Gaucher disease. By mapping clinical “red flags” across musculoskeletal, hematologic/visceral, neurologic, oncologic, and cardiovascular domains, the figure highlights how seemingly incongruent findings such as recurrent febrile serositis, florid proximal myopathy, iron overload with high ferritin and saturation, early onset malignancies, or renal cystic disease should prompt clinicians to move beyond a monogenic framework and pursue genomic evaluation. This approach highlights the central premise of our study: that GD, despite its single-gene basis, can present with blended or expanded phenotypes due to concurrent genetic disorders or modifier variants. Recognizing these phenotypic outliers is essential for precision medicine as it allows tailoring of diagnostic work-up and therapy to the full spectrum of a patient’s molecular diagnoses, thereby refining prognosis and management. Supplementary Table S1 lists each of the 17 patients, their GBA1 genotype, age at GD diagnosis, therapy (ERT or substrate reduction therapy (SRT)), second diagnosis, and age of second diagnosis.
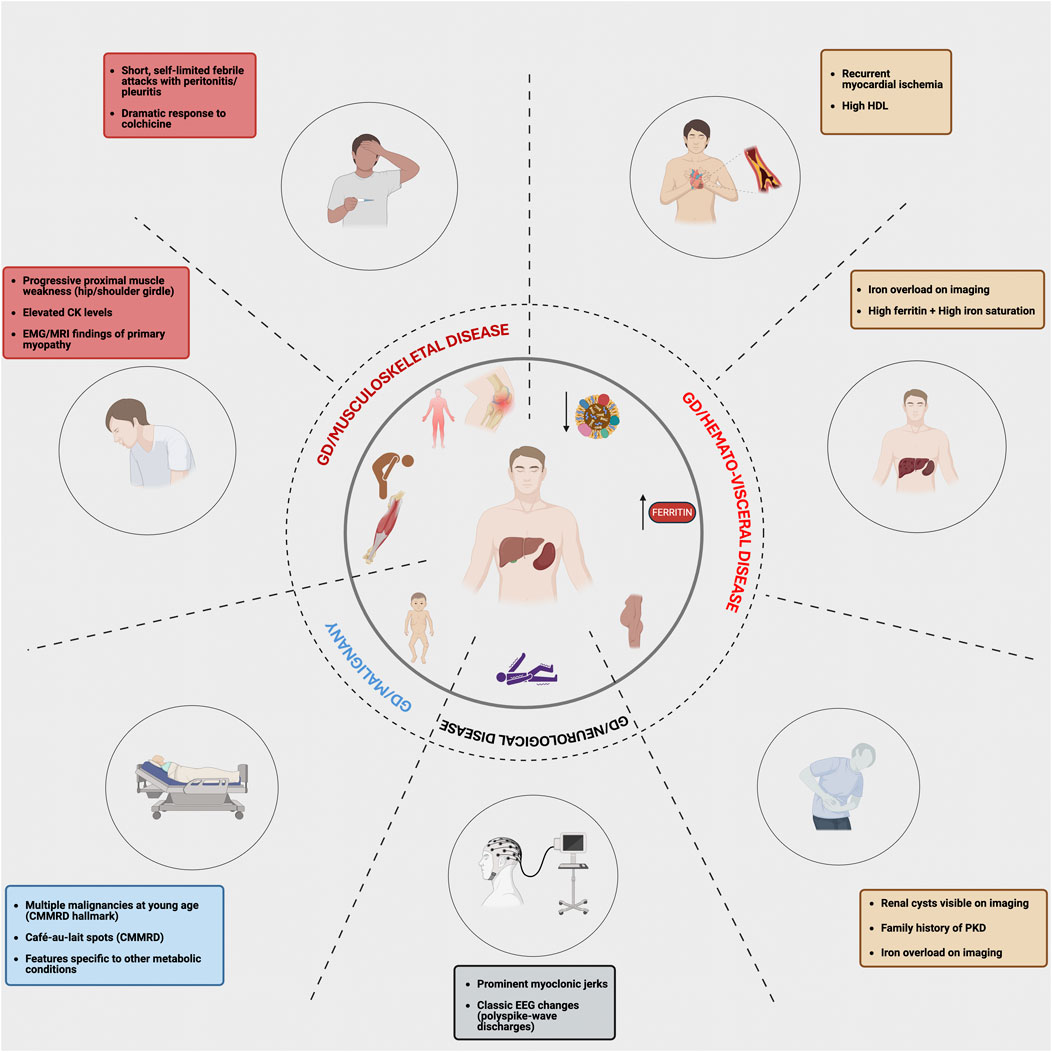
Figure 1. Atypical features in Gaucher disease that prompt evaluation for multiple molecular diagnoses. This figure maps organ system findings in Gaucher disease that should trigger genomic review. Recognizing these phenotypic red flags in distinct clinical domains may prompt clinicians to move beyond a “single gene-single disease” model and consider the presence of a second genetic diagnosis or a potential modifier.
2.2 Longitudinal deep phenotyping
Deep phenotyping included assessments of organ volumes, bone disease indicators, and extensive laboratory testing, including GD biomarkers. This longitudinal approach provided a robust dataset to capture the natural history of GD across various phenotypes.
2.3 Whole-exome sequencing (WES) and analysis
WES was performed as described previously, with additional modifications outlined in Supplementary Materials S1 (Lo et al., 2012). We integrated clinicopathological correlations with genetic data to investigate potential interactions between GD and other disease pathways. Variants in genes encoding proteins involved in key cellular pathways were analyzed and classified according to American College of Medical Genetics (ACMG) guidelines for pathogenicity. This integrative approach facilitated structured clinical reasoning to identify potential correlations between specific genetic variations and the complex phenotypic presentations observed in this subset of patients.
2.4 Ethical considerations
This study adhered to all relevant ethical guidelines and was approved by the Institutional Review Board at Yale University. All participants provided informed consent and written informed consent, including explicit permission for the publication of de-identified genetic data.
3 Results
We focused on 17 patients, including 16 with GD1 and 1 with GD3, who exhibited expanded phenotypes that deviated from the typical presentation of GD, prompting further evaluation for potential concurrent genetic disorders (Tables 1, 2) (Figure 1). The classical phenotypic spectrum of GD1 includes varying degrees of hepatosplenomegaly, cytopenia, and skeletal disease. However, the selected patients displayed atypical manifestations, including symptoms that were either unusually severe, unexplained by known GD pathology, or suggestive of additional systemic involvement. These atypical features warranted WES to investigate potential genetic modifiers or coexisting genetic conditions.
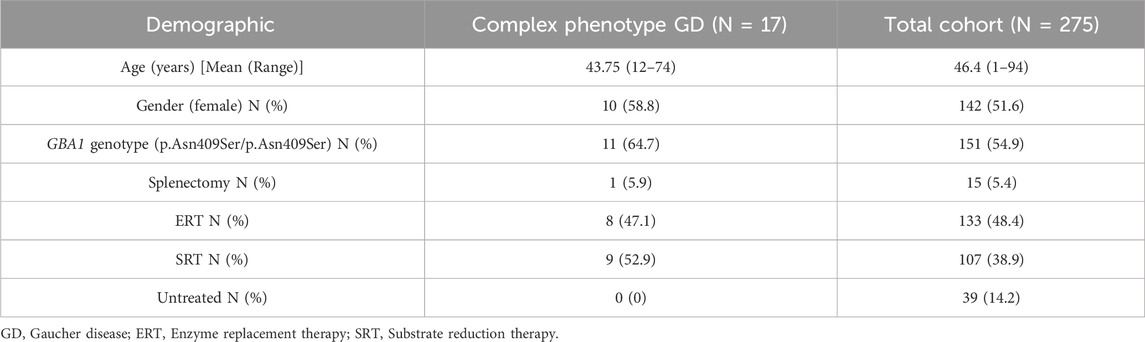
Table 2. Demographic details of our cohort of patients with complex phenotype GD. This table highlights the demographic and clinical characteristics of GD patients at our center, comparing those with complex phenotypes (N = 17) to our total cohort (N = 275).
The identified cases broadly fell into six categories:
1. Unusual inflammatory symptoms due to concurrent familial Mediterranean fever (FMF) in GD1 (n = 4).
2. Myopathy, unexpectedly severe osteoporosis in childhood in a patient homozygous for the p.Asn409Ser mutation, and debilitating chronic fatigue in GD1.
3. Complex phenotypes arising from another rare genetic disease (n = 5, GD1).
4. Autosomal dominant polycystic kidney disease (ADPKD) (n = 2, GD1).
5. Myoclonic epilepsy (n = 1, GD3).
6. Hyperferritinemia and iron overload (n = 5, GD1).
WES was analyzed to identify candidate genes, and the selected variants were annotated using ClinVar, sorting intolerant from tolerant (SIFT), minor allele frequency (MAF), and PolyPhen. Given that approximately 90% of our cohort is of Ashkenazi Jewish ancestry, allele frequencies were specifically examined in our entire cohort and in the broader population datasets in the public domain (Table 3).
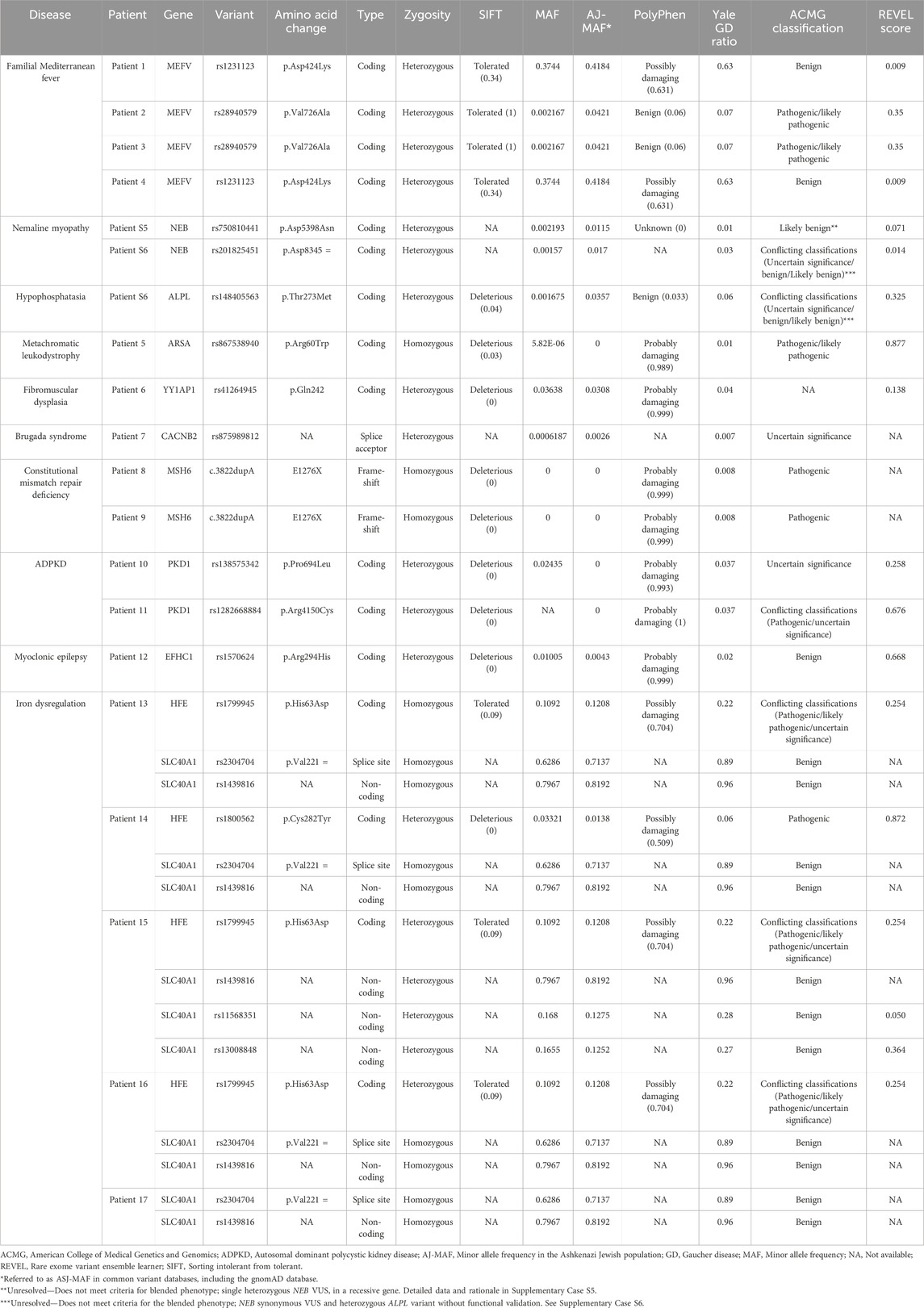
Table 3. Genetic variants detected in our cohort of 17 patients. This table depicts the genetic variants detected in 17 patients with GD in our cohort. For each variant, we report the associated disease, affected gene, variant designation (SNP/coding change), variant type, zygosity status, amino acid change, SIFT prediction score, MAF in the general population, AJ-specific MAF, PolyPhen predicted functional impact, Yale GD ratio, ACMG classification, and rare exome variant ensemble learner (REVEL) score. SIFT scores range from 0 to 1, with scores ≤0.05 considered deleterious. PolyPhen and REVEL scores also range from 0 to 1, with higher scores indicating greater functional impact. The Yale GD ratio represents the relative frequency of variants in these 17 patients compared to our entire cohort of GD patients at Yale. AJ-MAF refers to the minor allele frequency in the Ashkenazi Jewish population.
Below, we present selected cases to illustrate the GD phenotype, clinical reasoning process, therapeutic decision-making, and the diagnostic approach leading to the identification of multiple molecular diagnoses. These cases highlight the application of precision medicine in a single-gene disorder, demonstrating how individualized management was informed by deep phenotyping, longitudinal follow-up, and genomic insights.
3.1 Unusual inflammatory symptoms due to concurrent FMF
Patient 1: A 42-year-old man presented with mild splenomegaly, thrombocytopenia, and osteopenia and was diagnosed with GD1 due to homozygosity for the p.Asn409Ser GBA1 mutation. He experienced recurrent severe serous pericarditis despite colchicine therapy, necessitating repeated hospitalizations and steroid treatment. Despite imiglucerase enzyme replacement therapy (ERT) for GD, recurrent pericarditis persisted, warranting a pericardiectomy. Pericarditis has been previously described in GD; hence, we expected an improvement in symptoms on ERT, but there was no improvement (Harvey et al., 1969; Benbassat et al., 1968). Episodes of recurrent pericarditis continued six or more times each year for more than 2 decades, requiring steroids. Finally, he transitioned to eliglustat substrate reduction therapy (SRT). His response to SRT was striking, with a sustained remission of pericarditis. The patient was able to discontinue colchicine, and there has been no recurrence of pericarditis for the past 6 years on SRT. WES, focusing on genes underlying inflammatory diseases, revealed a heterozygous p.Asp424Glu variant in the MEFV gene (The International FMF Consortium, 1997).
Patient 2: A woman presented at age 25 due to fatigue and bone pain. Genetic testing revealed homozygosity for the p.Asn409Ser GBA1 mutation. Symptoms of fatigue, joint pain, and bone pain were debilitating. While the patient had elevated markers of GD, the severity of symptoms was disproportionate to the findings of GD markers. WES revealed a heterozygous p.Val726Ala variant in the MEFV gene previously reported to be associated with FMF (Aksentijevich et al., 1999). Initiation of eliglustat SRT and colchicine resulted in significant amelioration of symptoms.
Patient 3: An adult woman with a history of thrombocytopenia, easy bruising, and recurrent mucosal bleeding was diagnosed with GD1 at age 39 due to homozygosity for the p.Asn409Ser GBA1 mutation. She developed hepatosplenomegaly, cytopenia, and osteopenia, along with debilitating ankle and abdominal pain. WES revealed a heterozygous p.Val726Ala variant in the MEFV gene. Her symptoms improved with eliglustat SRT and colchicine.
Patient 4: A 25-year-old woman presented with an unusual constellation of symptoms. The patient complained of abdominal distension, pain, nausea, malaise, polyarthralgia, and splenomegaly. An abdominal magnetic resonance imaging (MRI) revealed splenomegaly, while lab testing showed normal blood counts. She was subsequently diagnosed with GD based on low leucocyte acid β-glucosidase activity. Based on the severity of her symptoms, treatment was initiated with eliglustat SRT, which resulted in a reduction in GlcSph level to normal (<1 ng/mL), but the patient continued to complain of frequent episodes of fever, night sweats, persistent abdominal pain, and mouth sores. WES analysis revealed the p.Asp424Glu variant in the MEFV gene. The patient reported significant improvement in symptoms on a combination of eliglustat and colchicine.
3.2 Myopathy, osteoporosis, and chronic fatigue
While mild myopathy has been described in GD1, it is rarely severe enough to cause profound limb-girdle weakness or secondary osteoporosis (Tsai et al., 2008). Two additional patients (Table 3) exhibited neuromuscular phenotypes with variants of uncertain significance; both remain unresolved and are detailed in Supplementary Cases S5, S6.
3.3 Complex phenotypes arising from another rare genetic disease
In a subset of patients with GD, atypical phenotypes were observed that could not be fully explained by the GBA1 genotype or the known clinical spectrum of GD. In these individuals, WES identified additional rare genetic variants consistent with second diagnoses. These concurrent conditions contributed to expanded or overlapping phenotypes that, in some cases, may have interacted with GD pathophysiology or complicated clinical management. These findings underscore the utility of WES in refining diagnoses, uncovering potential genetic contributors to phenotypic variability, and informing more individualized treatment strategies.
3.3.1 Patient 5: metachromatic leukodystrophy (MLD)
A male child presented with increased tone and developmental regression in his first year of life. By 16 months, he had developed spasticity and ataxia with reduced mobility and loss of speech. Brain MRI showed diffuse white matter abnormality. MLD was diagnosed based on low leucocyte arylsulfatase A activity and abnormal urinary sulfatides. At age 4, he was noted to have thrombocytopenia and elevated liver enzymes. WES revealed compound heterozygous GBA1 mutations, p.Asn409Ser and 84GinsG, consistent with GD1. Additionally, he was homozygous for the p.Arg60Trp variant in the ARSA gene that encodes arylsulfatase, known to cause late infantile MLD (Rabin et al., 2024). A recent study demonstrated a frequency of 1 in 1554 or 0.06% in the Ashkenazi Jewish population (Rabin et al., 2024).
The patient received ERT and supportive care. Unfortunately, he was not a candidate for a bone marrow transplant as his disease was deemed too advanced to offer meaningful benefits and unacceptable risks.
3.3.2 Patients 6 and 7: fibromuscular dysplasia (FMD) and Brugada syndrome
Two patients in our cohort, homozygous for the GBA1 p.Asn409Ser mutation, had cardiovascular disease. Cardiovascular complications are recognized in type 3c GD due to a homozygous p.Asp448His mutation (Wang et al., 2024). Cardiovascular disease is uncommon in GD1, with a lower prevalence of atherosclerotic complications compared to the general population, likely due to the typically low LDL cholesterol levels observed in these patients (Stein et al., 2011). However, in rare instances, GD1 patients may develop vascular or cardiac abnormalities, particularly when additional genetic factors are present. The following cases illustrate unique cardiovascular manifestations that occurred in two patients, highlighting the importance of considering the role of concurrent genetic conditions in shaping disease burden.
Patient 6: A 60-year-old woman presented at age 21 with massive splenomegaly and thrombocytopenia and was found to be compound heterozygous for the GBA1 mutations p.Asn409Ser and p.Val433Leu. ERT with alglucerase (later imiglucerase) reversed her organomegaly and cytopenia. Subsequently, she transitioned to eliglustat SRT and maintained good control of her GD. At age 56, she had a spontaneous coronary artery dissection (SCAD) resulting in a non-ST elevation myocardial infarction (NSTEMI) with systolic cardiomyopathy. Cardiac catheterization showed increased tortuosity in distal coronary arteries without occlusion. Positron emission tomography (PET) and computed tomography angiography (CTA) imaging of the abdomen and pelvis revealed a beaded appearance in the right renal and external iliac arteries, suggesting FMD. WES revealed a c.724C>T (p.Gln242*) nonsense variant in the YY1AP1 gene, previously implicated in Grange syndrome and FMD-like syndrome, which involves vascular abnormalities (Guo et al., 2017). While recognizing the possibility of this being a rare adverse effect of eliglustat, it is important to note that structural cardiovascular abnormalities have not been reported as a consequence of eliglustat SRT, and the patient was dosed pharmacologically with attention to drug–drug interactions, proven to ensure safety (Peterschmitt et al., 2019; Ain et al., 2025).
Patient 7: An adult man, who initially presented at age 14 with splenomegaly and thrombocytopenia, was diagnosed with GD1 due to homozygosity for the p.Asn409Ser GBA1 mutation and commenced ERT. A routine EKG during screening for the eliglustat trial revealed a type I Brugada pattern in leads V1-V2. WES, focusing on genes associated with Brugada syndrome, revealed he was heterozygous for g.15206G>T splice acceptor variant in the CACNB2 gene (Garcia-Elias and Benito, 2018). There were no variants in SCN5A, which is classically associated with Brugada syndrome; however, the CACNB2 gene defects also result in Brugada syndrome (Garcia-Elias and Benito, 2018).
3.3.3 Patients 8 and 9: constitutional mismatch repair deficiency (CMMRD) syndrome
Patients with GD have an increased risk of malignancies, particularly hematologic cancers, with epidemiologic studies suggesting an elevated incidence of multiple myeloma and lymphoma (Rosenbloom et al., 2022). However, these malignancies are predominantly observed in older adults, and cancer is rarely reported in pediatric GD patients. The following cases describe two siblings with GD1 who developed T-cell acute lymphoblastic lymphoma (T-ALL) at a young age, highlighting the potential contribution of an additional genetic predisposition.
Two siblings with GD1, born to non-consanguineous parents, developed T-ALL, previously reported by us (Lo et al., 2012). Both children presented with splenomegaly and mediastinal mass. Bone marrow aspirate revealed the presence of T-ALL as well as Gaucher cells. Exome analysis in these siblings revealed homozygosity for a novel GD mutation (p.Asp137Asn) in the GBA1 gene and a homozygous c.3822dupA/c.3822dupA variant in the MSH6 mismatch repair (MMR) gene (Lo et al., 2012).
3.4 ADPKD
Recognizing cases of GD with a family history of ADPKD is particularly important as dysregulation of GlcCer has been implicated in ADPKD pathogenesis. Studies suggest that SRT, including eliglustat, has been investigated as a potential therapeutic approach for ADPKD (Natoli et al., 2010). The following cases illustrate the coexistence of GD and ADPKD, underscoring the importance of considering the potential mechanistic interplay between lysosomal dysfunction and cystic kidney disease when managing these patients.
Patient 10: An adult woman with a known family history of polycystic kidney disease (PKD) was found to have hepatosplenomegaly and cytopenia at age 33. She was homozygous for the p.Asn409Ser mutation in the GBA1 gene and was started on ERT. WES, focusing on genes associated with PKD, revealed heterozygosity for the p.Pro694Leu variant in the PKD1 gene. Her GD has been well-controlled on ERT, and there has been no progression of her PKD, indicated by preserved renal function and no increase in renal cysts during 32 years of follow-up.
Patient 11: An adolescent male child was diagnosed with GD1 at the age of 2.5 years through family screening because his sibling was known to be affected. There was also a positive family history of PKD, and he was found to be affected by ultrasound. Exome analysis confirmed a diagnosis of ADPKD, revealing heterozygosity for the p.R4150C variant in the PKD1 gene. During regular follow-up, he had up-trending indicators of GD activity and an increasing number of renal cysts, although his renal function was normal. At age 16, he was started on eliglustat SRT.
3.5 Myoclonic epilepsy
Epilepsy is a recognized neurological feature of GD3, often presenting as generalized or focal seizures (Tylki-Szymańska et al., 2010). However, the devastating form of myoclonic epilepsy, which can significantly impact quality of life and disease progression, is uncommon in GD3 (Park et al., 2003). The following case describes a patient with GD3 who developed severe myoclonic epilepsy, highlighting the potential contribution of additional genetic factors to seizure susceptibility.
Patient 12: A 17-year-old woman was diagnosed with GD3 at the age of 20 months when she presented with pancytopenia, hepatosplenomegaly, developmental delay, and horizontal gaze palsy. A bone marrow biopsy revealed Gaucher cells, and subsequent investigations identified compound heterozygous GBA1 mutations, p.Leu363Pro and Gly416Ser. Treatment was initiated with a combination of imiglucerase and miglustat. At age 16, she experienced subtle myoclonic jerks in her fingers, which evolved into episodes of generalized tonic-clonic seizures and myoclonic epilepsy requiring multiple anti-epileptic drugs. WES focusing on epilepsy genes revealed a heterozygous EFHC1 variant, p.Arg294His, previously implicated in myoclonic epilepsy (Suzuki et al., 2004; de Nijs et al., 2012).
3.6 Hyperferritinemia and iron overload
Hyperferritinemia with normal iron saturation is a well-recognized feature of GD, often occurring as part of chronic inflammation rather than true iron overload (Motta et al., 2024). However, it is uncommon for GD patients to exhibit both elevated ferritin and iron saturation, with definitive evidence of iron overload on imaging and/or liver biopsy (Stein et al., 2010). The following cases illustrate rare instances where GD coexists with genetic predispositions to iron overload, highlighting the potential interplay between GD pathophysiology and iron metabolism.
Patient 13: Patient 13 is the same patient with GD and myopathy who is also described as Supplementary Case S5. She presented with splenomegaly, thrombocytopenia, and elevated ferritin at age 20. Initially diagnosed with chronic liver disease, her liver biopsy revealed Gaucher cells and hepatocyte siderosis. She was found to have low leukocyte acid β-glucosidase activity, and she was homozygous for the p.Asn409Ser GBA1 mutation. Her symptoms improved on ERT. A routine MRI was performed to assess GD, which revealed iron overload in the liver and the bone marrow (Stein et al., 2010). She underwent phlebotomy to reverse iron overload. WES analysis revealed a homozygous p.His63Asp variant in the HFE gene (Yassin et al., 2014). Additionally, the patient exhibited homozygosity for both the c.44-24G>C and synonymous p.Val221= (alters the splice site) single-nucleotide polymorphisms (SNPs) in the SLC40A1 gene, which have been linked to iron overload syndromes (Duca et al., 2022).
Patient 14: A male child presented with massive splenomegaly and avascular necrosis of the hips, and he was diagnosed with GD1. He underwent splenectomy at age 6 years and started ERT at age 23 years. He was homozygous for the p.Asn409Ser GBA1 mutation. Later, he developed pain and swelling in his proximal interphalangeal joints and knee chondrocalcinosis. He was found to have hyperferritinemia and high iron saturation. MRI of the liver showed hepatic iron overload. WES revealed a heterozygous p.Cys282Tyr variant in the HFE gene. Additionally, the patient was homozygous for the c.44-24G>C and p.Val221 = SNPs in the SLC40A1 gene (Duca et al., 2022). He is undergoing regular phlebotomies to manage the iron overload and recently switched to SRT due to persistent GD activity on ERT.
Patient 15: An adult woman of Italian ancestry presented at age 48 with thrombocytopenia and was diagnosed with GD1 due to a homozygous p.Asn409Ser GBA1 mutation. Despite responding well to ERT, she had persistently elevated ferritin and splenic iron overload on MRI (Figure 2). WES revealed a heterozygous p.His63Asp variant in the HFE gene (Hanson et al., 2001). Additionally, she was homozygous for the c.44-24G>C and synonymous p.Val221 = SNPs in the ferroportin gene, SLC40A1.
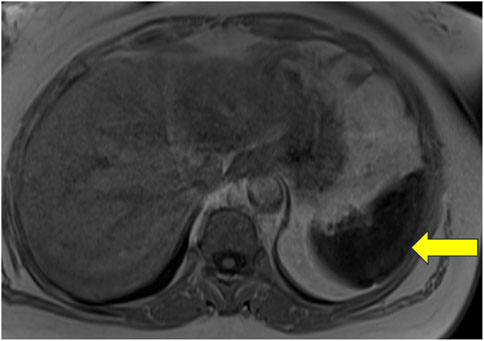
Figure 2. Non-contrast MRI of the abdomen of a patient with Gaucher disease and iron overload. This image represents a T1-weighted image with a uniformly hypointense spleen, which was associated with a signal dropout on the in-phase gradient echo sequence with a longer time to echo (TE), suggestive of diffuse iron deposition.
Patient 16: A routine physical exam in an adult man at age 22 revealed elevated ferritin, thrombocytopenia, elevated liver function tests, and splenomegaly. Liver biopsy revealed hepatocyte siderosis as well as Gaucher cells. Leukocyte acid β-glucosidase activity was low, and he was found to be compound heterozygous for p.Asn409Ser and c.115 + 1G>A GBA1 mutations. Despite a satisfactory response to ERT, he had persistent hyperferritinemia. Abdominal MRI revealed hepatic and splenic iron overload. WES revealed a heterozygous p.His63Asp HFE variant. He was also found to have the SNPs c.44-24G>C, UTR c.C98G, and UTR c.G8C in the SLC40A1 gene. The latter two SNPs have been reported in Brazilian patients with primary iron overload (Santos et al., 2011).
Patient 17: Patient 17 was a male child who presented at age 48 with thrombocytopenia and hyperferritinemia and was diagnosed with GD1 due to a homozygous p.Asn409Ser GBA1 mutation. He was started on ERT and later switched to eliglustat SRT. Despite a good response to therapy, he had persistent hyperferritinemia and marked splenic iron overload on MRI. WES revealed homozygosity for the c.44-24G>C and p.Val221 = variants in the SLC40A1 gene.
4 Discussion
GD, though monogenic in origin, exhibits remarkable phenotypic heterogeneity that cannot be fully explained by the GBA1 genotype alone. Our study expands this framework by demonstrating that, in approximately 6% of patients, atypical clinical features were attributable to multiple molecular diagnoses—supporting the growing recognition that multi-locus inheritance and blended phenotypes are not uncommon, with prior exome studies suggesting similar patterns in up to 5% of individuals undergoing genomic evaluation (Posey et al., 2017).
Building on prior reports showing that multiple molecular diagnoses can clarify atypical presentations and guide patient care, we applied a similar approach in GD (Malhotra et al., 2025; Kurolap et al., 2016). Importantly, this work moves beyond the enumeration of multiple molecular diagnoses to show how integrated genomic analysis can illuminate the underlying basis of unexplained clinical variation in GD. The accumulation of GlcCer and GlcSph in GD activates diverse downstream pathways, including inflammasome signaling, iron dysregulation, autophagy defects, and oxidative stress, which provide a plausible biological context for interaction with other rare disorders (Boddupalli et al., 2022; V et al., 2016).
Taken together, our findings highlight the value of combining deep phenotyping with genomic investigation to refine diagnoses, recognize potential clinically meaningful gene–gene interactions, and tailor therapeutic strategies. This integrated approach is particularly essential when clinical features deviate from the expected trajectory based on GBA1 genotype or age at onset, reinforcing the role of precision medicine in optimizing care for patients with rare, multisystem diseases (Mistry et al., 2002). We focused on 17 patients with GD as a model to illustrate how precision medicine can be applied to rare monogenic disorders. By integrating deep phenotyping, longitudinal natural history, and genomic analysis, we were able to refine diagnoses and optimize therapeutic strategies in cases with atypical presentations. The classical phenotype of GD1 encompasses variable degrees of hepatosplenomegaly, cytopenia, and skeletal disease. However, in some individuals, concurrent genetic conditions appeared to amplify or distort these features in unexpected ways—prompting further investigation. For example, while hyperferritinemia is common in GD, iron overload, characterized by elevated iron saturation and hepatic iron deposition, is unusual and was observed in multiple patients with coexisting variants in iron metabolism genes (Stein et al., 2010). Similarly, although cancer risk is elevated in GD, pediatric malignancy is rare. The identification of homozygous MSH6 variants in two siblings with GD and T-cell acute lymphoblastic lymphoma (T-ALL) highlights the importance of considering hereditary cancer predisposition syndromes in such contexts (Lo et al., 2012). Lastly, while mild muscle involvement is recognized in GD, the presentation of florid limb-girdle myopathy in one patient and disuse osteoporosis led to the identification of variants in the NEB gene associated with nemaline myopathy (Tsai et al., 2008).
In other cases, the presence of dual diagnoses was suspected a priori based on family history, as seen in patients with GD and ADPKD. Recognizing such co-occurrences is clinically important, particularly given emerging evidence linking GlcCer dysregulation to cystogenesis in ADPKD and the potential role of substrate reduction therapy (SRT) in modulating disease progression (Natoli et al., 2010). Similarly, while cardiovascular complications are typically confined to GD3c and are uncommon in GD1—likely due to the characteristically low LDL cholesterol levels—two GD1 patients in our cohort developed vascular and cardiac abnormalities associated with additional pathogenic variants in genes linked to fibromuscular dysplasia and Brugada syndrome, respectively (Wang et al., 2024; Stein et al., 2011). Finally, one patient was diagnosed with coexisting MLD and GD, which are two distinct lysosomal storage disorders. This case exemplifies how comprehensive phenotypic and genomic evaluation can reveal blended phenotypes and supports the rationale for including patients with atypical GD presentations in broader diagnostic frameworks.
4.1 Precision medicine in GD
This study outlines a practical framework for implementing precision medicine in the context of a single-gene disorder like GD. We identify three essential pillars that collectively support individualized care:
• Integrated clinical assessment—A comprehensive evaluation that combines clinical reasoning and longitudinal deep phenotyping. This approach uses long-term follow-up data, family history, phenotype, and disease trajectory to recognize when a patient’s presentation deviates from classical GD, prompting further genomic investigation.
• Genomic integration—Application of WES to uncover variants that explain atypical clinical features, refine diagnoses, and guide targeted interventions.
• Therapeutic individualization—Adaptation of treatment based on the presence of concurrent genetic conditions, such as using eliglustat in patients with inflammatory phenotypes or incorporating phlebotomy in cases of iron overload.
4.2 Genetic background and dual diagnoses
While some concurrent disorders may arise by chance, recurrent patterns across genetically defined populations suggest potential mechanistic or ancestral relevance. The co-occurrence of GD and FMF in individuals of Ashkenazi Jewish descent is particularly striking, given the high carrier frequency of both GBA1 and MEFV variants in this population (Stirnemann et al., 2017; LIDAR et al., 2010). Historical genomic data from medieval Ashkenazi Jewish individuals have identified the presence of both the GBA1 p.N370S and MEFV p.Val726Ala variants, suggesting a possible shared evolutionary background (Waldman et al., 2022).
Although heterozygous MEFV variants such as p.Val726Ala are typically associated with reduced penetrance, they may produce FMF-like symptoms in some carriers. Their potential role as modifiers of GD-related inflammation or disease expression remains a compelling but unresolved question (Booty et al., 2009; Berkun et al., 2012).
4.3 Pathway interactions and clinical implications
Finally, the convergence of GD with other genetic conditions in this cohort raises important questions about shared and intersecting biological pathways. In patients with GD and FMF, both disorders involve inflammasome activation, which may synergistically amplify systemic inflammation and upregulate GlcCer synthesis (Nair et al., 2015; Pandey and Grabowski, 2013; Pandey et al., 2017). This could explain the enhanced clinical response observed with glucosylceramide synthase (GCS) inhibitors like eliglustat compared to ERT. Similarly, in cases of GD with coexisting myopathy, chronic inflammation and metabolic stress may compound neuromuscular dysfunction, suggesting a mechanistic interaction between lysosomal and muscle structural pathways (González-Jamett et al., 2022). In patients with GD and iron overload, the unusual finding of hepatic iron deposition points to potential dysregulation of macrophage iron handling, possibly involving ferroportin-hepcidin signaling, an interaction not typically seen in isolated GD (Stein et al., 2010; Lefebvre et al., 2018). Finally, while seizures are known in GD3, the presence of disabling myoclonic epilepsy in one patient raises the possibility that additional genetic variants, such as those in EFHC1, may modify neuronal excitability and contribute to this rare phenotype (Thounaojam et al., 2017). A previous study implicated variants in the SCARB2 gene in type 3 GD complicated by myoclonic epilepsy (Velayati et al., 2011). Together, these observations support a model in which concurrent genetic variants may modulate GD pathophysiology via shared immune, metabolic, or neuroinflammatory pathways, with implications for personalized therapeutic strategies.
4.4 Study limitations
Our study is limited by its single-center nature and the rarity of GD, which may limit generalizability. The heterogeneity of GD and varying depths of phenotyping across centers make replication difficult. In particular, variants of uncertain significance or single heterozygous variants in recessive disease genes, such as those observed in Patients 5 and 6, should not be over-interpreted as blended phenotypes; rather, they highlight the interpretive limits of current genomic analysis and the need for functional validation. Emerging evidence suggests that synonymous variants may still impact gene expression, mRNA stability, and translation efficiency (Kesner et al., 2023). WES excludes most non-coding regions, making it challenging to detect complex alleles. Additionally, WES is less reliable for identifying copy number variants (CNVs) or mosaicism due to its inherent limitations in read depth, coverage, and difficulty capturing structural variants.
While we describe only a small subset of our patients, these cases highlight a potential paradigm for precision medicine in GD. In some cases, the concurrent genetic disorders appear stochastic, for example, GD and myopathy or GD and iron overload. Genetic population structure may also play a role, as most of our patients are Ashkenazi Jewish. Thus, the co-occurrence of GD and FMF should be considered in atypical patients, especially in Ashkenazi Jewish patients, due to the ancestral relationship between MEFV and GD variants. However, stochastic co-occurrence is not confined to Ashkenazi Jewish patients; it can also be seen in non-Jewish patients, illustrated by the two children with GD and ALL.
While our cases suggest potential mechanistic links, they remain hypothesis-generating, necessitating larger multicenter studies to confirm our observations. Future research should leverage rare disease consortia (e.g., NORD Centers of Excellence) to validate these findings in broader populations.
5 Conclusion
This study reframes the search for a singular genetic modifier in GD, instead highlighting the intricate interplay of multiple genetic and phenotypic factors that shape disease expression. By integrating longitudinal deep phenotyping, rigorous clinical reasoning, and comprehensive genomic analysis, we demonstrate how precision medicine can be operationalized in the management of a rare monogenic disorder. This approach not only refines diagnosis and enhances therapeutic decision-making but also uncovers biologically plausible interactions between GD and coexisting genetic conditions. Our findings further suggest that standard GD therapies, especially SRT, may exert ancillary benefits on coexisting genetic disorders such as FMF, likely through shared biological pathways. As genomic technologies become increasingly accessible, this framework offers a path forward for individualized care in GD and provides a model for applying precision medicine across the broader landscape of rare diseases.
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding author at cHJhbW9kLm1pc3RyeUB5YWxlLmVkdQ==.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Yale University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
AS: Writing – original draft, Writing – review and editing, Conceptualization, Formal Analysis, Investigation, Methodology, Visualization. NA: Writing – original draft, Writing – review and editing. JR: Writing – original draft, Writing – review and editing, Data curation, Formal Analysis, Methodology, Software. MK: Writing – original draft, Writing – review and editing. DJ: Writing – original draft, Writing – review and editing. GI: Writing – original draft, Writing – review and editing. SM: Software, Writing – original draft, Writing – review and editing. NB: Writing – original draft, Writing – review and editing. SN: Writing – original draft, Writing – review and editing. PM: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors declare that this study received funding from Sanofi. AS and NUA are recipients of the Rare Lysosomal Disease Fellowship (Sanofi). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgements
We extend our deepest gratitude to our patients, whose trust and willingness to participate made this study possible. We also thank our clinical and research teams for their dedicated support throughout this work. AS and NA were recipients of the Rare Lysosomal Fellowship from Sanofi, and we acknowledge their valuable contribution to this research. The Yale HPC cluster was used for preliminary sequencing data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2025.1553036/full#supplementary-material
References
Ain, N. U., Saith, A., Ruan, A., Yang, R., Burton, A., and Mistry, P. K. (2025). Eliglustat and cardiac comorbidities in gaucher disease: a pharmacogenomic approach to safety and efficacy. Front. Med. (Lausanne) 12, 1535099. doi:10.3389/fmed.2025.1535099
Aksentijevich, I., Torosyan, Y., Samuels, J., Centola, M., Pras, E., Chae, J. J., et al. (1999). Mutation and haplotype studies of Familial Mediterranean fever reveal new ancestral relationships and evidence for a high carrier frequency with reduced penetrance in the Ashkenazi Jewish population. Am. J. Hum. Genet. 64 (4), 949–962. doi:10.1086/302327
Benbassat, J., Bassan, H., Milwidsky, H., Sacks, M., and Groen, J. J. (1968). Constrictive pericarditis in Gaucher’s disease. Am. J. Med. 44 (4), 647–652. doi:10.1016/0002-9343(68)90067-3
Berkun, Y., Eisenstein, E., and Ben-Chetrit, E. (2012). FMF - clinical features, new treatments and the role of genetic modifiers: a critical digest of the 2010-2012 literature. Clin. Exp. Rheumatol. 30 (3), S90–S95.
Blauwendraat, C., Tayebi, N., Woo, E. G., Lopez, G., Fierro, L., Toffoli, M., et al. (2023). Polygenic parkinson’s disease genetic risk Score as risk modifier of parkinsonism in gaucher disease. Mov. Disord. 38 (5), 899–903. doi:10.1002/mds.29342
Boddupalli, C. S., Nair, S., Belinsky, G., Gans, J., Teeple, E., Nguyen, T. H., et al. (2022). Neuroinflammation in neuronopathic Gaucher disease: role of microglia and NK cells, biomarkers, and response to substrate reduction therapy. Elife 11, e79830. doi:10.7554/eLife.79830
Booty, M. G., Chae, J. J., Masters, S. L., Remmers, E. F., Barham, B., Le, J. M., et al. (2009). Familial mediterranean fever with a single MEFV mutation: where is the second hit? Arthritis Rheum. 60 (6), 1851–1861. doi:10.1002/art.24569
de Nijs, L., Wolkoff, N., Coumans, B., Delgado-Escueta, A. V., Grisar, T., and Lakaye, B. (2012). Mutations of EFHC1, linked to juvenile myoclonic epilepsy, disrupt radial and tangential migrations during brain development. Hum. Mol. Genet. 21 (23), 5106–5117. doi:10.1093/hmg/dds356
Drelichman, G. I., Fernández Escobar, N., Soberon, B. C., Basack, N. F., Frabasil, J., Schenone, A. B., et al. (2021). Long-read single molecule real-time (SMRT) sequencing of GBA1 locus in Gaucher disease national cohort from Argentina reveals high frequency of complex allele underlying severe skeletal phenotypes: collaborative study from the Argentine Group for Diagnosis and Treatment of Gaucher Disease. Mol. Genet. Metab. Rep. 29, 100820. doi:10.1016/j.ymgmr.2021.100820
Duca, L., Granata, F., Di Pierro, E., Brancaleoni, V., Graziadei, G., and Nava, I. (2022). Associated effect of SLC40A1 and TMPRSS6 polymorphisms on iron overload. Metabolites 12 (10), 919. doi:10.3390/metabo12100919
Garcia-Elias, A., and Benito, B. (2018). Ion channel disorders and sudden cardiac death. Int. J. Mol. Sci. 19 (3), 692. doi:10.3390/ijms19030692
González-Jamett, A., Vásquez, W., Cifuentes-Riveros, G., Martínez-Pando, R., Sáez, J. C., and Cárdenas, A. M. (2022). Oxidative stress, inflammation and connexin hemichannels in muscular dystrophies. Biomedicines 10 (2), 507. doi:10.3390/biomedicines10020507
Grabowski, G. A., Kolodny, E. H., Weinreb, N. J., Rosenbloom, B. E., Prakash-Cheng, A., Kaplan, P., et al. (2019). “Gaucher disease: phenotypic and genetic variation,” in The online metabolic and molecular bases of inherited disease. Editors D. Valle, S. Antonarakis, A. Ballabio, A. Beaudet, and G. Mitchell (McGraw-Hill Education). Available online at: https://ommbid.mhmedical.com/content.aspx?bookid=2709§ionid=225546386 (Accessed December 9, 2024).
Grabowski, G. A., Antommaria, A. H. M., Kolodny, E. H., and Mistry, P. K. (2021). Gaucher disease: basic and translational science needs for more complete therapy and management. Mol. Genet. Metab. 132 (2), 59–75. doi:10.1016/j.ymgme.2020.12.291
Guo, D. chuan, Duan, X. Y., Regalado, E. S., Mellor-Crummey, L., Kwartler, C. S., Kim, D., et al. (2017). Loss-of-Function mutations in YY1AP1 lead to grange syndrome and a fibromuscular dysplasia-like vascular disease. Am. J. Hum. Genet. 100 (1), 21–30. doi:10.1016/j.ajhg.2016.11.008
Hanson, E. H., Imperatore, G., and Burke, W. (2001). HFE gene and hereditary hemochromatosis: a HuGE review. Human Genome Epidemiology. Am. J. Epidemiol. 154 (3), 193–206. doi:10.1093/aje/154.3.193
Harvey, P. K., Jones, M. C., and Anderson, E. G. (1969). Pericardial abnormalities in Gaucher’s disease. Heart 31 (5), 603–606. doi:10.1136/hrt.31.5.603
Kesner, J. S., Chen, Z., Shi, P., Aparicio, A. O., Murphy, M. R., Guo, Y., et al. (2023). Noncoding translation mitigation. Nature 617 (7960), 395–402. doi:10.1038/s41586-023-05946-4
Kurolap, A., Orenstein, N., Kedar, I., Weisz Hubshman, M., Tiosano, D., Mory, A., et al. (2016). Is one diagnosis the whole story? Patients with double diagnoses. Am. J. Med. Genet. A 170 (9), 2338–2348. doi:10.1002/ajmg.a.37799
Lefebvre, T., Reihani, N., Daher, R., de Villemeur, T. B., Belmatoug, N., Rose, C., et al. (2018). Involvement of hepcidin in iron metabolism dysregulation in Gaucher disease. Haematologica 103 (4), 587–596. doi:10.3324/haematol.2017.177816
Lidar, M., Kedem, R., Berkun, Y., Langevitz, P., and Livneh, A. (2010). Familial mediterranean fever in Ashkenazi jews: the mild end of the clinical spectrum. J. Rheumatol. 37 (2), 422–425. doi:10.3899/jrheum.090401
Lo, S. M., Liu, J., Chen, F., Pastores, G. M., Knowles, J., Boxer, M., et al. (2011). Pulmonary vascular disease in gaucher disease: clinical spectrum, determinants of phenotype and long-term outcomes of therapy. J. Inherit. Metab. Dis. 34 (3), 643–650. doi:10.1007/s10545-011-9313-9
Lo, S. M., Choi, M., Liu, J., Jain, D., Boot, R. G., Kallemeijn, W. W., et al. (2012). Phenotype diversity in type 1 gaucher disease: discovering the genetic basis of gaucher disease/hematologic malignancy phenotype by individual genome analysis. Blood 119 (20), 4731–4740. doi:10.1182/blood-2011-10-386862
Malhotra, A., Thorpe, E., Coffey, A. J., Rajkumar, R., Adjeman, J., Naa Adjeley Adjetey, N. D., et al. (2025). Multiple molecular diagnoses identified through genome sequencing in individuals with suspected rare disease. Hum. Genet. Genomics Adv. 6 (3), 100430. doi:10.1016/j.xhgg.2025.100430
Mistry, P. K., Sirrs, S., Chan, A., Pritzker, M. R., Duffy, T. P., Grace, M. E., et al. (2002). Pulmonary hypertension in type 1 Gaucher’s disease: genetic and epigenetic determinants of phenotype and response to therapy. Mol. Genet. Metab. 77 (1-2), 91–98. doi:10.1016/S1096-7192(02)00122-1
Mistry, P. K., Cappellini, M. D., Lukina, E., Ozsan, H., Mach Pascual, S., Rosenbaum, H., et al. (2011). A reappraisal of gaucher Disease—Diagnosis and disease management algorithms. Am. J. Hematol. 86 (1), 110–115. doi:10.1002/ajh.21888
Motta, I., Delbini, P., Scaramellini, N., Ghiandai, V., Duca, L., Nava, I., et al. (2024). Enzyme replacement therapy improves erythropoiesis and iron dysregulation in gaucher disease. Ann. Hematol. 103 (12), 5113–5121. doi:10.1007/s00277-024-05918-2
Nair, S., Boddupalli, C. S., Verma, R., Liu, J., Yang, R., Pastores, G. M., et al. (2015). Type II NKT-TFH cells against Gaucher lipids regulate B-cell immunity and inflammation. Blood 125 (8), 1256–1271. doi:10.1182/blood-2014-09-600270
Natoli, T. A., Smith, L. A., Rogers, K. A., Wang, B., Komarnitsky, S., Budman, Y., et al. (2010). Inhibition of glucosylceramide accumulation results in effective blockade of polycystic kidney disease in mouse models. Nat. Med. 16 (7), 788–792. doi:10.1038/nm.2171
Pandey, M. K., and Grabowski, G. A. (2013). Immunological cells and functions in gaucher disease. Crit. Rev. Oncog. 18 (3), 197–220. doi:10.1615/CritRevOncog.2013004503
Pandey, M. K., Burrow, T. A., Rani, R., Martin, L. J., Witte, D., Setchell, K. D., et al. (2017). Complement drives glucosylceramide accumulation and tissue inflammation in Gaucher disease. Nature 543 (7643), 108–112. doi:10.1038/nature21368
Park, J. K., Orvisky, E., Tayebi, N., Kaneski, C., Lamarca, M. E., Stubblefield, B. K., et al. (2003). Myoclonic epilepsy in gaucher disease: Genotype-Phenotype insights from a rare patient subgroup. Pediatr. Res. 53 (3), 387–395. doi:10.1203/01.PDR.0000049515.79882.94
Peterschmitt, M. J., Freisens, S., Underhill, L. H., Foster, M. C., Lewis, G., and Gaemers, S. J. M. (2019). Long-term adverse event profile from four completed trials of oral eliglustat in adults with Gaucher disease type 1. Orphanet J. Rare Dis. 14 (1), 128. doi:10.1186/s13023-019-1085-6
Posey, J. E., Harel, T., Liu, P., Rosenfeld, J. A., James, R. A., Coban Akdemir, Z. H., et al. (2017). Resolution of disease phenotypes resulting from multilocus Genomic variation. N. Engl. J. Med. 376 (1), 21–31. doi:10.1056/NEJMoa1516767
Rabin, R., Hirsch, Y., Booth, K. T. A., Hall, P. L., Yachelevich, N., Mistry, P. K., et al. (2024). ARSA variant associated with late infantile metachromatic leukodystrophy and carrier rate in individuals of Ashkenazi Jewish ancestry. Am. J. Med. Genet. A 197, e63919. doi:10.1002/ajmg.a.63919
Rosenbloom, B. E., Cappellini, M. D., Weinreb, N. J., Dragosky, M., Revel-Vilk, S., Batista, J. L., et al. (2022). Cancer risk and gammopathies in 2123 adults with gaucher disease type 1 in the international gaucher Group gaucher Registry. Am. J. Hematol. 97 (10), 1337–1347. doi:10.1002/ajh.26675
Santos, PCJL, Cançado, R. D., Pereira, A. C., Schettert, I. T., Soares, R. A. G., Pagliusi, R. A., et al. (2011). Hereditary hemochromatosis: mutations in genes involved in iron homeostasis in Brazilian patients. Blood Cells Mol. Dis. 46 (4), 302–307. doi:10.1016/j.bcmd.2011.02.008
Sidransky, E. (2004). Gaucher disease: complexity in a “simple” disorder. Mol. Genet. Metab. 83 (1-2), 6–15. doi:10.1016/j.ymgme.2004.08.015
Sidransky, E. (2012). Gaucher disease: insights from a rare Mendelian disorder. Discov. Med. 14 (77), 273–281.
Stein, P., Yu, H., Jain, D., and Mistry, P. K. (2010). Hyperferritinemia and iron overload in type 1 Gaucher disease. Am. J. Hematol. 85 (7), 472–476. doi:10.1002/ajh.21721
Stein, P., Yang, R., Liu, J., Pastores, G. M., and Mistry, P. K. (2011). Evaluation of high density lipoprotein as a circulating biomarker of Gaucher disease activity. J. Inherit. Metab. Dis. 34 (2), 429–437. doi:10.1007/s10545-010-9271-7
Stirnemann, J., Belmatoug, N., Camou, F., Serratrice, C., Froissart, R., Caillaud, C., et al. (2017). A review of gaucher disease pathophysiology, clinical presentation and treatments. Int. J. Mol. Sci. 18 (2), 441. doi:10.3390/ijms18020441
Suzuki, T., Delgado-Escueta, A. V., Aguan, K., Alonso, M. E., Shi, J., Hara, Y., et al. (2004). Mutations in EFHC1 cause juvenile myoclonic epilepsy. Nat. Genet. 36 (8), 842–849. doi:10.1038/ng1393
The International FMF Consortium (1997). Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. Cell 90 (4), 797–807. doi:10.1016/S0092-8674(00)80539-5
Thounaojam, R., Langbang, L., Itisham, K., Sobhani, R., Srivastava, S., Ramanujam, B., et al. (2017). EFHC1 mutation in Indian juvenile myoclonic epilepsy patient. Epilepsia Open 2 (1), 84–89. doi:10.1002/epi4.12037
Tsai, L., Chien, Y., Yang, C., and Hwu, W. (2008). Myopathy in Gaucher disease. J. Inherit. Metab. Dis. 31 (S3), 489–491. doi:10.1007/s10545-007-0795-4
Tylki-Szymańska, A., Vellodi, A., El-Beshlawy, A., Cole, J. A., and Kolodny, E. (2010). Neuronopathic Gaucher disease: demographic and clinical features of 131 patients enrolled in the International Collaborative Gaucher Group Neurological Outcomes Subregistry. J. Inherit. Metab. Dis. 33 (4), 339–346. doi:10.1007/s10545-009-9009-6
Vardi, A., Zigdon, H., Meshcheriakova, A., Klein, A. D., Yaacobi, C., Eilam, R., et al. (2016). Delineating pathological pathways in a chemically induced mouse model of Gaucher disease. J. Pathol. 239 (4), 496–509. doi:10.1002/path.4751
Velayati, A., DePaolo, J., Gupta, N., Choi, J. H., Moaven, N., Westbroek, W., et al. (2011). A mutation in SCARB2 is a modifier in gaucher disease. Hum. Mutat. 32 (11), 1232–1238. doi:10.1002/humu.21566
Waldman, S., Backenroth, D., Harney, É., Flohr, S., Neff, N. C., Buckley, G. M., et al. (2022). Genome-wide data from medieval German Jews show that the Ashkenazi founder event pre-dated the 14th century. Cell 185 (25), 4703–4716.e16. doi:10.1016/j.cell.2022.11.002
Wang, J. S., Koch, R. L., Kenney-Jung, D., Huggins, E., Sodhi, S. S., Landstrom, A. P., et al. (2024). Gaucher disease type 3c: expanding the clinical spectrum of an ultra-rare disease. JIMD Rep. 65 (5), 313–322. doi:10.1002/jmd2.12440
Yassin, M. A., Soliman, A. T., Desanctis, V., Abusamaan, S., Elsotouhy, A., and Aldewik, N. (2014). Hereditary hemochromatosis in an adult due to H63D mutation: the value of estimating iron deposition by MRI T2* and dissociation between Serum Ferritin concentration and hepatic iron overload. Blood 124 (21), 4891. doi:10.1182/blood.V124.21.4891.4891
Zhang, C. K., Stein, P. B., Liu, J., Wang, Z., Yang, R., Cho, J. H., et al. (2012). Genome-wide association study of N370S homozygous gaucher disease reveals the candidacy of CLN8 gene as a genetic modifier contributing to extreme phenotypic variation. Am. J. Hematol. 87 (4), 377–383. doi:10.1002/ajh.23118
Keywords: Gaucher disease, modifier genes, complex phenotypes, longitudinal deep phenotyping, whole-exome sequencing
Citation: Saith A, Ain NU, Ruan J, Kasaiyan M, Jain D, Israel G, Mehta S, Bamford NS, Nair S and Mistry PK (2025) Precision genomic profiling in Gaucher disease: insights from atypical presentations. Front. Genet. 16:1553036. doi: 10.3389/fgene.2025.1553036
Received: 02 January 2025; Accepted: 01 October 2025;
Published: 07 November 2025.
Edited by:
Pilar Giraldo, University of Zaragoza, SpainReviewed by:
Patrick Deegan, Cambridge University Hospitals NHS Foundation Trust, United KingdomHagit Baris Feldman, Tel Aviv Sourasky Medical Center, Israel
Barry Rosenbloom, Cedars Sinai Medical Center, United States
Copyright © 2025 Saith, Ain, Ruan, Kasaiyan, Jain, Israel, Mehta, Bamford, Nair and Mistry. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pramod K. Mistry, cHJhbW9kLm1pc3RyeUB5YWxlLmVkdQ==
†These authors have contributed equally to this work
 Armaan Saith
Armaan Saith Noor Ul Ain
Noor Ul Ain Jiapeng Ruan
Jiapeng Ruan Maniya Kasaiyan
Maniya Kasaiyan Dhanpat Jain3
Dhanpat Jain3 Sameet Mehta
Sameet Mehta Nigel S. Bamford
Nigel S. Bamford Shiny Nair
Shiny Nair