- 1Department of Health Informatics, School of Public Health, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Birhan, Ethiopia
- 2Department of Health Informatics, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 3Department of Public Health, College of Medicine and Health Sciences, Arsi University, Asella, Ethiopia
- 4Department of Health Informatics, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
Background: Maternal and child health remains a global public health issue, particularly in low- and middle-income countries where maternal and child mortality are extremely high. The World Health Organization estimates that close to 287,000 women die annually due to pregnancy and childbirth complications, and the majority of these deaths occur where skilled birth attendants are not readily available. Reducing the prevalence of home delivery is a key strategy for lowering the maternal mortality rate. Although several studies have explored home delivery and antenatal care (ANC) utilization independently, limited evidence exists on predicting home delivery after ANC visits using machine-learning approaches in East Africa.
Methods: This study utilized a community-based, cross-sectional design with data from the most recent Demographic and Health Surveys conducted between 2011 and 2021 in 12 countries in East Africa countries. A total weighted sample of 44,123 women was analyzed using Python version 3.11. Nine supervised machine-learning algorithms were applied, following Yufeng Guo's steps for supervised learning. The random forest (RF) model, selected as the best-performing algorithm, was used to predict home delivery after ANC visits. A SHapley Additive exPlanations analysis was conducted to identify key predictors influencing home delivery decisions.
Results: Home delivery after ANC visits was most prevalent in Malawi (17.88%), Uganda (15.38%), and Kenya (11.3%), and was low in Comoros (2.38%). Living in rural areas and late ANC initiation (second trimester) increased the likelihood of home delivery. In contrast, factors such as higher household income, husband’s level of primary and secondary education, contraceptive use, shorter birth intervals, absence of distance-related barriers to healthcare, and attending more than four ANC visits were associated with a lower likelihood of home delivery.
Conclusion: The study demonstrates that home delivery after ANC visits was high. The RF machine-learning algorithm effectively predicts home delivery. To reduce home deliveries, efforts should improve early ANC initiation, enhance healthcare quality, and expand facility-based services. Policymakers should prioritize increasing health facility accessibility, promoting media-based health education, and addressing financial barriers for women with low incomes. Strengthening these areas is crucial for improving maternal and neonatal health outcomes in East Africa.
Introduction
A home birth after an antenatal care (ANC) visit is described as a delivery that occurs at home without the presence of a skilled birth attendant, despite the mother having received ANC care (1). Maternal health remains a top priority on the global health agenda (2). Every minute, women around the world die due to problems related to pregnancy and childbirth, most of which are preventable (3). In 2017 alone, approximately 295,000 women died from pregnancy- and childbirth-related issues (3).
Maternal and child mortality remain major global health challenges, with sub-Saharan Africa accounting for 70% of global maternal deaths. In East Africa, home delivery remains prevalent, particularly in Malawi, Uganda, and Kenya, due to rural residence, cultural practices, and limited access to healthcare (3). Despite efforts to enhance ANC utilization, many women still deliver at home, increasing health risks to them and their newborns (4).
Pregnancy- and childbirth-related complications tend to be the reason for the deaths and disabilities that occur worldwide. The main reasons for death include infection, prolonged or obstructed labor, complications from a surgical abortion, hemorrhage, malaria during pregnancy, and anemia (5). The use of professional care during childbirth remains significantly lower in sub-Saharan Africa and South/Southeast Asia, with the exception of a few countries such as Benin, Namibia, Zimbabwe, and Vietnam. In Ethiopia, home delivery is especially prevalent in the Afar and Somali regions, where 89.5% and 81.7% of women, respectively, gave birth at home, compared with just 3.3% of women living in Addis Ababa (6).
Studies have identified a range of statistically significant predictors of home delivery after an ANC visit. These include the women’s educational status (7–13), cultural factors (8, 9, 13, 14), geographic region (7), parity (7), limited access to healthcare facilities (8, 9), poor quality of care (8, 9), lack of transportation (4, 8, 9), maternal age (6, 11, 12, 14, 15), marital status (4), environment (13, 16), distance to health facilities (3, 4, 7, 9, 10, 17), source of health information (3, 4, 7, 10), antenatal care visits (3, 7–9, 18), birth order (7, 8), household wealth index (7, 8, 11, 19), place of residence (3, 6, 7, 9, 12, 18), religion (7, 8, 14), employment status of the woman and her husband (6), knowledge about place of delivery (3, 11, 12, 18), unplanned pregnancy (10), and decision-making regarding the place of delivery (3, 11, 13).
Home delivery poses significant health risks, increasing the likelihood of pregnancy-related complications and neonatal illness or death (20). Studies have shown that perinatal mortality rates are 21% higher for home births compared with deliveries in healthcare facilities, and home births are associated with infections and other adverse outcomes for both mothers and newborns (10).
Home delivery after an ANC visit remains a major public health concern. Reducing the prevalence of home deliveries is one of the most effective ways for lowering maternal mortality rates (3). This study is important when prioritizing the establishment of public health measures because it uses weighted pooled DHS data from 12 countries in East Africa, providing adequate power to accurately detect predictors of home delivery after ANC visits. Existing studies on home delivery rely on traditional statistical methods, which often fail to capture complex interactions among determinants. However, this study fills the gap by using machine learning (ML) to enhance predictive accuracy. A SHapley Additive exPlanations (SHAP) analysis is applied to identify the most influential predictors of women's delivery choices. This research is significant for African policymakers and global health researchers as it enhances predictive modeling for maternal health, provides data-driven insights for targeted interventions, and supports evidence-based policies to improve institutional deliveries (7). Therefore, the aim of this study was to predict home delivery after ANC visits among women of reproductive age in East Africa using supervised machine-learning algorithms.
Methods and materials
Study design and study setting
A community-based cross-sectional study was conducted to predict home delivery after ANC visits among women aged 15–49 years using recent DHS data from East African countries, collected between 2011 and 2021. East Africa comprises 19 countries: Rwanda, Seychelles, Somalia, Tanzania, Uganda, Zambia, South Sudan, Zimbabwe, Burundi, Comoros, Djibouti, Ethiopia, Eritrea, Kenya, Madagascar, Malawi, Mauritius, Mozambique, and Sudan (21). However, only 14 of these countries have DHS data available, whereas five countries (Djibouti, Somalia, South Sudan, Seychelles, and Mauritius) lack DHS datasets. Among the 14 countries with data, Eritrea has restricted DHS data and Sudan’s dataset dates back to 1989–1990. Thus, this study included 12 countries with recent publicly available DHS datasets (Burundi, Ethiopia, Comoros, Uganda, Rwanda, Tanzania, Mozambique, Madagascar, Zimbabwe, Kenya, Zambia, and Malawi).
Enumeration areas (EA) were selected independently within each sampling stratum using probability sampling proportional to EA size. Households were then systematically selected from each chosen EA. The DHS report included a comprehensive description of the sampling methodology (22, 23).
Data source and sampling technique
The study was conducted using publicly available datasets based on the Demographic and Health Surveys (DHS). Different datasets, such as those for men, women, children, births, individuals, and households, are included in each country's survey; for this study, we used the Individual Record (IR) file. DHS used the Population and Housing Census (PHC) as a sampling frame for a two-stage stratified cluster sampling technique.
Populations
We extracted the data of 75,047 women of reproductive age in the study. However, after going through the data (excluding women who did not have an ANC visit, missing values, and unknown responses), a total weighted sample of 44,123 respondents was included in the study for further analysis.
Study variables
The outcome variable, home delivery after ANC visit, is defined as a woman who gives birth at home despite having attended at least one ANC visit during her pregnancy. It was measured as a binary variable (1 = home delivery, 0 = facility-based delivery) (24). Independent variables for this study included maternal age, number of ANC visits, area of residence, birth interval, level of education of the mother and her husband, marital status, household wealth index, media exposure, sex of household head, previous contraceptive use, the timing of ANC visits, and health facility issues (Supplementary Table S1).
Data management and analysis
As recommended by the DHS, the data were weighted using the primary sampling unit, sampling weight, and strata to restore representativeness and account for the complex sampling design, ensuring accurate statistical analysis. Sampling statisticians determined the appropriate sample size for each stratum.
A total of 75,047 actual samples with selected variables were extracted using STATA software version 17 and exported as a CSV file. Further analysis was conducted in Jupyter Notebook version 3.11. Preprocessing steps included explanatory data analysis, missing value management, data discretization, outlier detection, target feature balancing, and feature selection. Finally, the dataset was split into training (80%) and test (20%) subsets, and only features that passed the selection process were used for modeling.
This study used the following nine supervised machine-learning algorithms to predict home delivery among East African women of reproductive age after an ANC visit: Support Vector Machine (SVM), Ada Boost (AdB), Gaussian naïve Bayes (GNB), Multi-Layer Perception (MLP), Decision Tree (DT), Logistic Regression (LR), K Nearest Neighbors (KNN), Extreme Gradient Boosting (XG Boost), and Random Forest (RF) (25–28).
Models training used tenfold cross-validation. A total of 12 recent DHS datasets from East African countries were analyzed. Performance was evaluated using accuracy, precision, recall, F1-score, and area under the curve (AUC) to identify the best-performing model, whose hyperparameters were subsequently adjusted. To identify the best-performing model, we followed a systematic approach that included model evaluation, comparison, and selection based on the metrics. In statistical analyses, packages were applied, including imblearn (29) to handle imbalanced datasets through resampling techniques, sklearn (30) for implementing machine-learning algorithms and model evaluation, and SHAP (31) to interpret model predictions by explaining the contribution of each feature.
SHAP was used to determine feature importance, offering insights into how each variable influenced the prediction of home delivery after an ANC visit. Numerous studies have used SHAP as a feature selection method, demonstrating that incorporating SHAP values into machine-learning models works better in terms of classification performance and model explainability. By plotting the total Shapley value of each feature, it is easier to understand the influence of individual predictors on the likelihood of home delivery after an ANC visit (27, 32).
In addition, the contributions of each feature to the prediction of the positive class (home delivery) were explained using a waterfall plot (27). In this plot, the x-axis represents the probability that a sample will be assigned to the “home delivery” class, while the y-axis lists the independent variables and their corresponding values for each sample. Each horizontal bar reflects each feature's contribution. Positive contributions (red bars) indicate that the feature increases the probability of home delivery, whereas negative contributions (blue bar) suggest a decreased likelihood of this outcome. The complete workflow methodology is presented in Figure 1.
Results
Characteristics of the study respondents
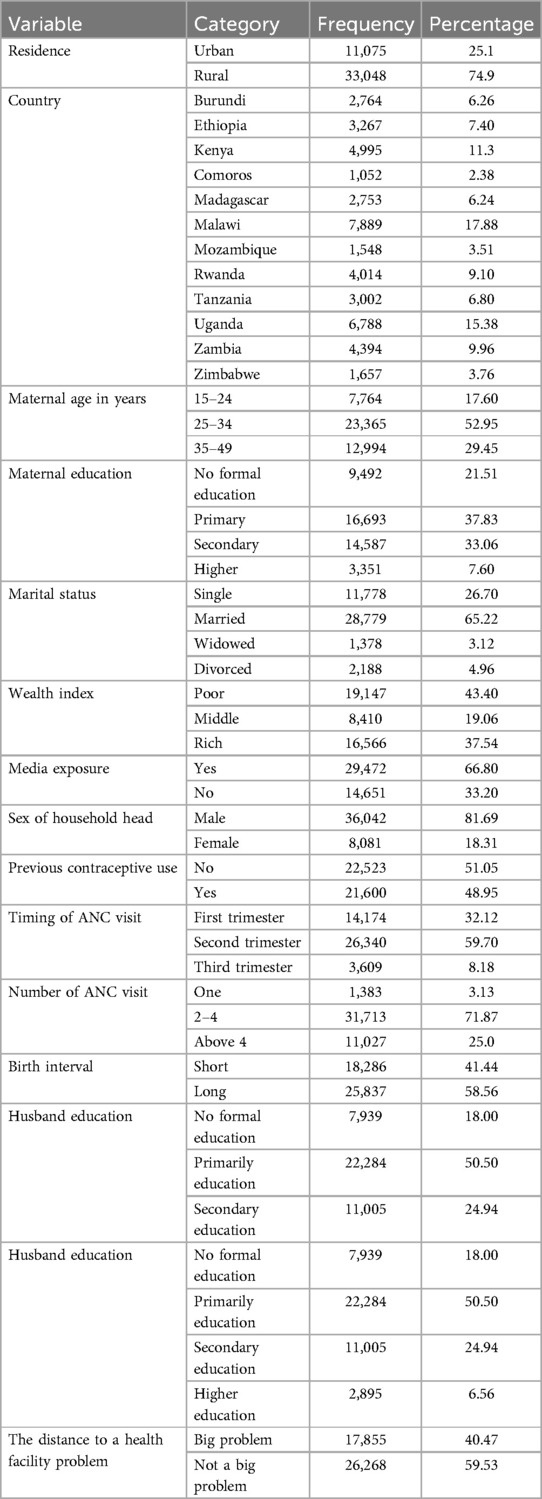
The mean age of the participants was 28.41 years. Of the study participants, 33,048 (74.9%) were from rural areas. In total, 7,889 (17.88%) were from Malawi and 2.38% were from Comoros. Of the participants, 16,693 (37.83%) had attained primary education, 19,147 (43.40%) had a low wealth index, 28,779 (65.22%) were married, 29,472 (66.80) were exposed to media, and 31,713 (71.87%) had attended two to four ANC visits. Of the participants, 26,268 (59.53%) had no issues with the distance to health facilities (Table 1).
Machine-learning analysis of home delivery after ANC visit
Data balancing
To improve model reliability, synthetic minority oversampling technique (SMOTE) oversampling created 13,590 synthetic observations for the minority class. The total distribution of home deliveries after ANC visits was modified from 12,060 home deliveries and 25,650 non-home deliveries to 25,650 in each class (Figure 2).
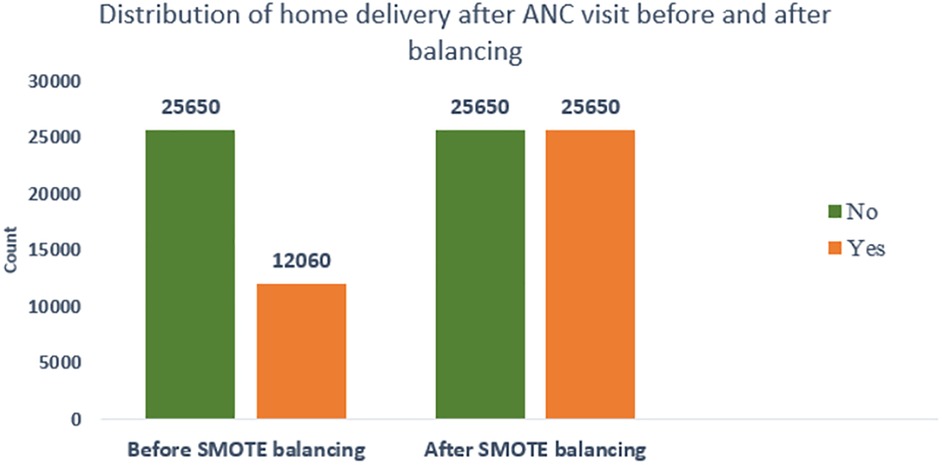
Figure 2. SMOTE balancing of home deliveries after ANC visits among women of reproductive age in East Africa, DHS 2011–2021.
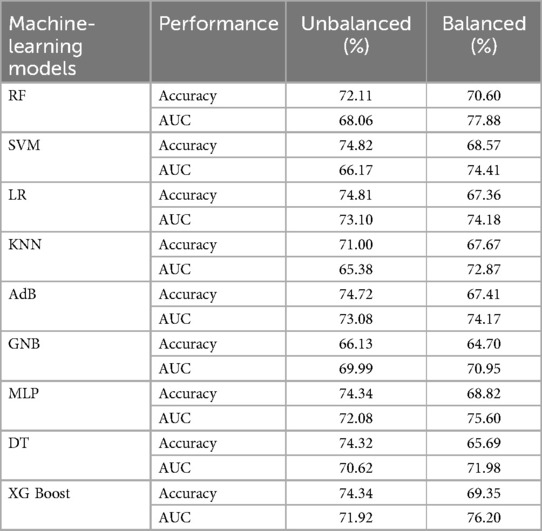
Model performance comparison
Among the classifiers assessed using imbalanced training data with stratified tenfold cross-validation, the Support Vector Machine proved the most effective, achieving an accuracy of 74.82% and an area under the receiver operating characteristic (ROC) curve of 66.17%. However, after applying the SMOTE oversampling technique to balance the training data, the Random Forest model was the best predictive model, with an accuracy of 70.60% and a higher AUC of 77.88% (Table 2).
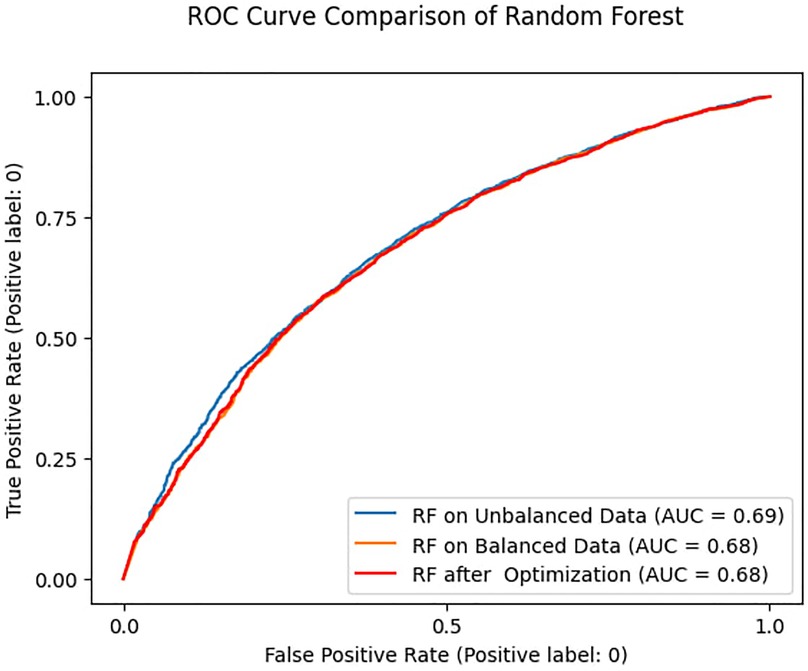
When tested on unseen data, the Random Forest model produced an AUC of 0.69 and 0.68 for the balanced and unbalanced training datasets, respectively. In addition, after hyperparameter tuning, the Random Forest model predicted an AUC of 0.68 (Figure 3).
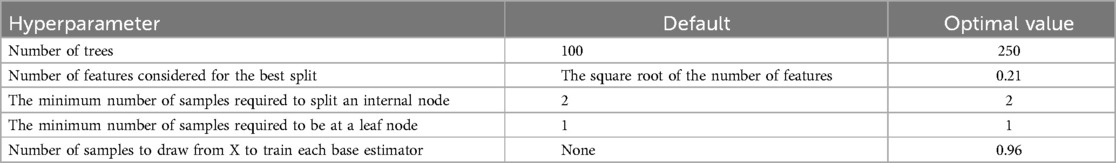
Hyperparameter tuning of RF
A Random Forest model developed with optimized hyperparameters and evaluated using tenfold cross cross-validation on balanced training data achieved an accuracy of 79% and an AUC of 0.78 (Table 3).
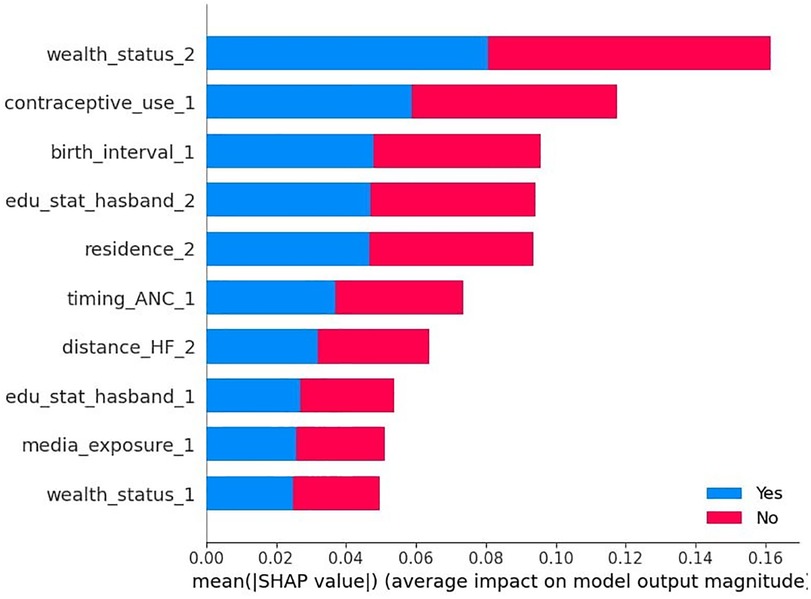
Important feature selection using RF
According to the optimized Random Forest model with test data, the SHAP global importance scores identified the top 10 predictors of home delivery after an ANC visit. These predictors are ranked in descending order according to their mean absolute SHAP values, indicating their influence on the outcome variable. The five most important predictors were: belonging to a rich household (wealth_status = 2), contraceptive use (contraceptive_use = 1), short birth interval (birth_interval = 1), husband’s level of secondary education (edu_status_husband = 2), and residing in rural areas (residence = 2). Other significant predictors included ANC in the second trimester (timing_ANC = 1), difficulty with distance to a healthcare facility (distance_HF = 2), husband’s level of primary education (edu_status_husband = 1), media exposure (media_exposure = 1), and middle household income (wealth_status = 1). As shown in Figure 4, the red and blue colors occupy half of the horizontal rectangles for each class, indicating that each variable has an equal impact on both home delivery after ANC visit (label = yes) and institutional delivery after ANC visit (label = no) outcomes.
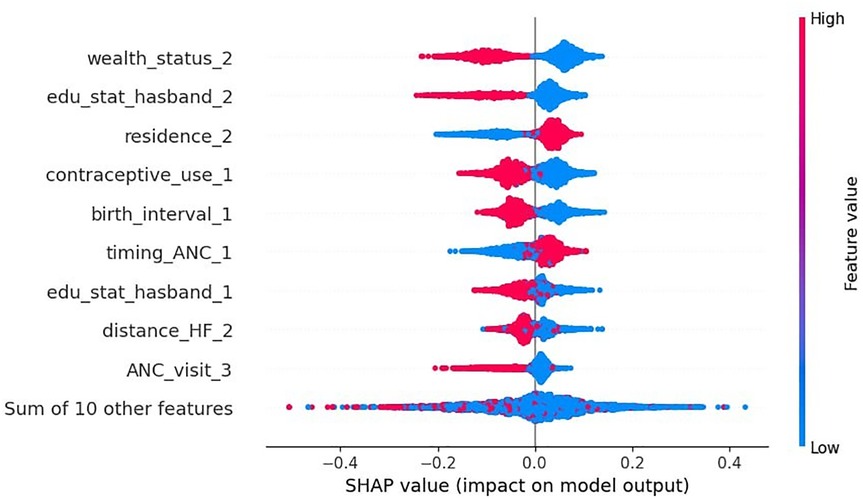
Model interpretation/explanation
According to the beeswarm plot, the points that are to the right of the vertical line (0 SHAP value) increase the likelihood of home delivery after the ANC visit, while those on the left decrease it. The red line represents higher feature values (coded as 1) and the blue line represents lower values (coded as 0). Accordingly, being a rural resident (residence = 2) and attending ANC visits in the second trimester (timing_ANC = 1) increase the likelihood of a home delivery. In contrast, belonging to a rich household (wealth_status = 2), husband’s level of secondary education (edu_status_husband = 2), contraceptive use (contraceptive_use_1), short birth interval (birth_interval = 1), husband’s level of primary education (edu_status_husband = 1), having no difficulties with distance to health facilities (distance_HF = 2), and attending more than four ANC visits (ANC_visit = 3) were factors that decreased the likelihood of a home delivery in East Africa (Figure 5).
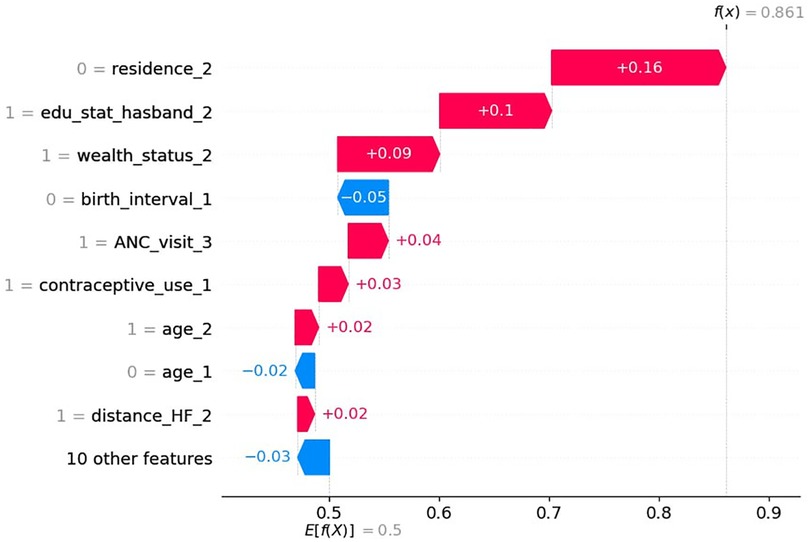
Waterfall plot
The waterfall plots begin with the expected value of the model output on the x-axis {E[f(X)] = 0.5}, which represents the initial prediction for the given sample before considering any feature contributions. For a given observation, model outputs above this value {E[f(X)]} correspond to a positive class (i.e., home delivery), whereas outputs below this value correspond to a negative class (“no home delivery”). Figure 6 demonstrates how the combination of positive (in red) and negative contributions (in blue) adjusts the expected value output to a final model output [f(x) = 0.86], classified as positive class (home delivery after ANC visit).
Accordingly, not being from rural areas (0 = rural resident of women), husband’s level of secondary education (1 = secondary educational level of the husband), high household income (1 = rich household income), attending more than four ANC visits (1 = having above four ANC visits), contraceptive use (1 = contraceptive use), woman's age of 35–49 years (1 = women's age between 35 and 49), and having no difficulties with distance to health facilities (1 = having no problems of distance to health facility) increases the probability of having a home delivery after ANC visits, whereas, no short birth interval (0 = short birth interval) and woman's age not between 25 and 34 years (0 = age between 25 and 34) drives down the probability of having a home delivery after ANC visits for this particular woman (Figure 6).
Discussion
This study aimed to assess the prediction of home delivery after ANC visits in East Africa using a supervised machine-learning algorithm. In the early stages of predictive modeling using unbalanced training data, the SVM model outperformed other classifiers. In the second stage of model prediction on balanced training data, the random forest (RF) model performed better.
The SHAP analysis based on the RF model showed that high household income, contraceptive use, short birth interval, husband’s level of primary and secondary education, residing in rural areas, attending ANC visits in the second trimester, difficulties with distance to health facilities, media exposure, and middle household income were important predictors of home delivery after ANC visits in East Africa.
Women who lived in rural areas had an increased likelihood of home delivery after ANC visits. This finding was in line with previous studies (7, 33–35). A possible explanation could be that women residing in rural areas are often far from healthcare facilities. Although services are widely accessible inside the community, transporting an ambulance in East Africa is challenging due to the region's topography and infrastructure. As a result, even though they follow the antenatal care services, women choose to deliver at home (7).
High household income decreased women's likelihood of home delivery after ANC visits. This implies that home deliveries after ANC visits were higher among women with a lower socioeconomic status compared to those who were wealthier. This finding was supported by previous studies (5–7, 11). This could be because the woman’s low income limited her from affording transport and food-related costs (36). Furthermore, it might be that most wealthy women in East Africa live in urban areas. As a result, those women have easier access to healthcare and transportation, leading to fewer home births (37).
Women who attended ANC visits in their second trimester had an increased likelihood of home delivery after ANC visits. This might be related to the level of care given throughout the ANC visit. Even with advancements over the previous 10 years, there remains a serious shortage of medical experts and unstable drug and equipment supplies (7). This result contradicts an earlier Ethiopian study that found that women who had their first ANC visit in the third trimester were less likely to give birth at home than women who had their first ANC visit in the first trimester. Thus, further study is needed to confirm this (38).
Lower levels of husband’s primary and secondary education were associated with an increased likelihood of women delivering at home after ANC visits. This finding is supported by previous studies (39–41). A possible explanation is that education is a key strategy for increasing the utilization of healthcare services; however, in the absence of universal access to education, there would be a huge disparity in the understanding of those who did and did not have difficulties in labor and delivery, as well as the risks associated with unattended deliveries (10). In addition, husbands’ knowledge improves and enables women to make decisions about where to give birth and to communicate to others (42).
Contraceptive use reduced the number of home deliveries after an ANC visit. This finding is in line with previous studies. This suggests that women who have used contraceptives will place importance on delivering in a healthcare facility. Furthermore, using contraceptives allows women to get more medical counseling, which may substantially reduce the rate of home births (7, 10, 24). Short birth intervals reduced the number of home deliveries after ANC visits. This suggests that women with short childbirth intervals were more likely to use health facilities for delivery. This could be explained by the fact that during pregnancy, women learn more about the possible risks of having frequent preterm births at ANC visits. They also help mothers develop an effective birth plan, which could reduce the possibility of the woman giving birth at home (43, 44).
Women who had no difficulties with distance to health facilities experienced a decrease in home deliveries after ANC visits. A possible explanation for this could be that, even with the lack of other options for transportation, women who live close to medical facilities are more willing to walk there. However, walking far while in labor is difficult and gets worse if labor starts at night. As a result, women choose home births (10).
Attending more than four ANC visits reduced the number of women's home deliveries after ANC visits. The number of ANC visits was also significantly associated with home delivery after ANC visits. This finding was in line with previous studies (10, 24, 45). A reason for this could be the rising number of ANC visits with medical experts, which increases the likelihood of receiving a health consultation regarding place of delivery, birth preparedness, and the value of professional birth attendants. On the other hand, women who attended fewer than four ANC visits did not communicate with medical professionals effectively and decided to deliver at home (36).
Implications of the study
Theoretically, this study highlights the importance of sociodemographic associations in shaping maternal health outcomes. It underscores the need for multi-level interventions that address both socioeconomic factors and barriers to healthcare access. It also highlights the value of predictive modeling, particularly machine-learning algorithms, in identifying key risk factors for home delivery after ANC visits. This helps public health professionals target interventions more effectively. Overall, these findings emphasize that both healthcare system strengthening and social interventions are essential for reducing home deliveries and improving maternal and neonatal health outcomes.
Practically, this study highlights the need for targeted policy interventions to address the identified associations of home delivery. Specifically, improving access to healthcare in rural areas through mobile clinics, better transportation, and expanding healthcare facilities can significantly reduce home births. In addition, financial support and transportation subsidies are crucial to overcome wealth barriers, ensuring that women with low incomes have access to facility-based deliveries. Promoting early ANC visits through outreach programs is vital for improving maternal health outcomes and reducing home deliveries. Engaging husbands, particularly those with lower levels of education, through targeted educational campaigns can also positively impact maternal health decisions. Finally, strengthening family planning services will allow women to better plan pregnancies, ultimately reducing the likelihood of home births.
Limitations and strengths of the study
The primary strength of this study was the use of large sample sizes and nationally representative data. The use of a sophisticated and suitable statistical method (machine-learning technique), which revealed previously undiscovered relationships and patterns in the field, was also another key point. Although machine-learning results limit the interpretation between predictors and outcome variables due to their black-box nature, this study employed the SHAP analysis to ascertain how predictors increased or decreased home delivery after ANC visits with respective predictors.
The limitation of this study was that the DHS rely on self-reported data, which may be subject to recall bias, as participants were asked to recall prior events. In addition, the cross-sectional study design limits the ability to determine causality—it only revealed relationships between factors and home births after ANC visits. Moreover, the different survey years introduce heterogeneity and future studies should consider subgroup analyses.
Conclusion
This study found that the number of home deliveries after ANC visits was highest in Malawi, Uganda, and Kenya. The Random Forest model demonstrated the strongest predictive power of all the machine-learning models used in this study to predict home delivery after ANC visits in East Africa. The beeswarm plot of the SHAP analysis based on the RF model showed that residing in a rural area and attending ANC visits in the second trimester increases the likelihood of a home delivery after an ANC visit. In contrast, high household income, husband’s level of primary and secondary education, contraceptive use, short birth interval, having no difficulties with distance to health facilities, and attending more than four ANC visits reduced the number of women's home deliveries after ANC visits in East Africa.
As a result, this study recommends that women attend antenatal care services early and often throughout their pregnancies to ensure quality care from a qualified practitioner. In addition, education and women's empowerment are important components of programs aimed at reducing mother and infant mortality by improving the quality of health institution service utilization, especially in rural areas. Developing health facilities, promoting media health education, and encouraging women to obtain adequate information on healthcare services are essential, especially in Malawi, Uganda, and Kenya. Finally, healthcare policies should support women from low-income households.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: www.measuredhs.com.
Ethics statement
This study utilized publicly available secondary data from the Demographic and Health Surveys (DHS) conducted in 12 East African countries: Burundi, Ethiopia, Comoros, Uganda, Rwanda, Tanzania, Mozambique, Madagascar, Zimbabwe, Kenya, Zambia, and Malawi. The datasets were obtained through formal online requests submitted to the DHS Program website (http://www.dhsprogram.com), and permission letters were granted upon approval. Each country’s DHS was reviewed and approved by its respective national ethics committee and the Institutional Review Board (IRB) of ICF International. Informed consent was obtained from all participants during the original data collection. The data were fully anonymized and contained no personally identifiable information. The DHS Program waived the need for additional ethical clearance for this secondary analysis. All methods were carried out by the ethical standards of the DHS Program. For detailed information on country specific ethical procedures, readers are encouraged to consult the respective DHS final reports.
Author contributions
AW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SK: Conceptualization, Funding acquisition, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. JA: Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. DM: Conceptualization, Data curation, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to the MEASURE DHS program that provides permission with data access authorization to enable us to conduct the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1461475/full#supplementary-material
Abbreviations
ANC, antenatal care visit; AUC, area under the curve; DHS, Demographic and Health Survey; LR, logistic regression; ML, machine learning; RF, random forest; ROC, receiver operating characteristic; SHAP, SHapley Additive exPlanations; SMOTE, synthetic minority oversampling technique; WHO, World Health Organization.
References
1. Ganle JK, Mahama MS, Maya E, Manu A, Torpey K, Adanu R. Understanding factors influencing home delivery in the context of user-fee abolition in Northern Ghana: evidence from 2014 DHS. Int J Health Plann Manage. (2019) 34(2):727–43. doi: 10.1002/hpm.2731
2. Smith SL, Shiffman J. Setting the global health agenda: the influence of advocates and ideas on political priority for maternal and newborn survival. Soc Sci Med. (2016) 166:86–93. doi: 10.1016/j.socscimed.2016.08.013
3. Nigatu AM, Gelaye KA, Degefie DT, Birhanu AY. Spatial variations of women’s home delivery after antenatal care visits at Lay Gayint district, northwest Ethiopia. BMC Public Health. (2019) 19(1):1–14. doi: 10.1186/s12889-019-7050-4
4. Scott NA, Henry EG, Kaiser JL, Mataka K, Rockers PC, Fong RM, et al. Factors affecting home delivery among women living in remote areas of rural Zambia: a cross-sectional, mixed-methods analysis. Int J Women’s Health. (2018) 10:589. doi: 10.2147/IJWH.S169067
5. Devkota B, Maskey J, Pandey AR, Karki D, Godwin P, Gartoulla P, et al. Determinants of home delivery in Nepal–A disaggregated analysis of marginalised and non-marginalised women from the 2016 Nepal Demographic and Health Survey. PLoS One. (2020) 15(1):e0228440. doi: 10.1371/journal.pone.0228440
6. Chernet AG, Dumga KT, Cherie KT. Home delivery practices and associated factors in Ethiopia. J Reprod Infertil. (2019) 20(2):102.31058055
7. Tessema ZT, Tiruneh SA. Spatio-temporal distribution and associated factors of home delivery in Ethiopia. Further multilevel and spatial analysis of Ethiopian Demographic and Health Surveys 2005–2016. BMC Pregnancy Childbirth. (2020) 20:1–16. doi: 10.1186/s12884-020-02986-w
8. Tiruneh SA, Lakew AM, Yigizaw ST, Sisay MM, Tessema ZT. Trends and determinants of home delivery in Ethiopia: further multivariate decomposition analysis of 2005–2016 Ethiopian Demographic Health Surveys. BMJ Open. (2020) 10(9):e034786. doi: 10.1136/bmjopen-2019-034786
9. Yebyo H, Alemayehu M, Kahsay A. Why do women deliver at home? Multilevel modeling of Ethiopian National Demographic and Health Survey data. PLoS One. (2015) 10(4):e0124718. doi: 10.1371/journal.pone.0124718
10. Kasaye HK, Endale ZM, Gudayu TW, Desta MS. Home delivery among antenatal care booked women in their last pregnancy and associated factors: community-based cross sectional study in Debremarkos town, North West Ethiopia, January 2016. BMC Pregnancy Childbirth. (2017) 17(1):1–12. doi: 10.1186/s12884-017-1409-2
11. Mrisho M, Schellenberg JA, Mushi AK, Obrist B, Mshinda H, Tanner M, et al. Factors affecting home delivery in rural Tanzania. Trop Med Int Health. (2007) 12(7):862–72. doi: 10.1111/j.1365-3156.2007.01855.x
12. Abdella M, Abraha A, Gebre A, Reddy PS. Magnitude and associated factors for home delivery among women who gave birth in last 12 months in Ayssaita, Afar, Ethiopia-2016. A community based cross sectional study. Glob J Fertil Res. (2017) 2(1):030–9. doi: 10.17352/gjfr.000009
13. Ramezani Siakhulake F, Tabatabaei SM, Mohammadi M, Behmanesh Pour F. Home delivery practices among pregnant women in southeast of Iran and associated factors after the implementation of the health transformation plan: a case-control study. Women’s Health Bulletin. (2021) 8(3):142–51. doi: 10.30476/whb.2021.91277.1122
14. Abubakar S, Adamu D, Hamza R, Galadima JB. Determinants of home delivery among women attending antenatal care in Bagwai town, Kano Nigeria. Afr J Reprod Health. (2017) 21(4):73–9. doi: 10.29063/ajrh2017/v21i4.8
15. Idris S, Gwarzo U, Shehu A. Determinants of place of delivery among women in a semi-urban settlement in Zaria, northern Nigeria. Ann Afr Med. (2006) 5(2):68–72. Available at: https://www.ajol.info/index.php/aam/article/view/8376
17. Simfukwe ME. Factors contributing to home delivery in Kongwa District, Dodoma-September 2008. Dar Es Salaam Medi Students’ J. (2011) 18(1):13–22. Available at: https://www.ajol.info/index.php/dmsj/article/view/71001
18. Abebe F, Berhane Y, Girma B. Factors associated with home delivery in Bahirdar, Ethiopia: a case control study. BMC Res Notes. (2012) 5(1):1–6. doi: 10.1186/1756-0500-5-653
19. Ogolla JO. Factors associated with home delivery in West Pokot County of Kenya. Adv Public Health. (2015) 2015. doi: 10.1155/2015/493184
20. Bang RA, Bang AT, Reddy MH, Deshmukh MD, Baitule SB, Filippi V. Maternal morbidity during labour and the puerperium in rural homes and the need for medical attention: a prospective observational study in Gadchiroli, India. BJOG. (2004) 111(3):231–8. doi: 10.1111/j.1471-0528.2004.00063.x
21. Raru TB, Ayana GM, Zakaria HF, Merga BT. Association of higher educational attainment on antenatal care utilization among pregnant women in east Africa using Demographic and Health Surveys (DHS) from 2010 to 2018: a multilevel analysis. Int J Women’s Health. (2022) 14:67–77. doi: 10.2147/IJWH.S350510
22. Tesema GA, Teshale AB, Tessema ZT. Incidence and predictors of under-five mortality in east Africa using multilevel Weibull regression modeling. Arch Public Health. (2021) 79:1–13. doi: 10.1186/s13690-021-00727-9
24. Muluneh AG, Animut Y, Ayele TA. Spatial clustering and determinants of home birth after at least one antenatal care visit in Ethiopia: Ethiopian Demographic and Health Survey 2016 perspective. BMC Pregnancy Childbirth. (2020) 20(1):97. doi: 10.1186/s12884-020-2793-6
25. Kebede SD, Sebastian Y, Yeneneh A, Chanie AF, Melaku MS, Walle AD. Prediction of contraceptive discontinuation among reproductive-age women in Ethiopia using Ethiopian Demographic and Health Survey 2016 dataset: a machine learning approach. BMC Med Inform Decis Mak. (2023) 23(1):1–17. doi: 10.1186/s12911-023-02102-w
26. Mamo DN, Yilma TM, Fekadie M, Sebastian Y, Bizuayehu T, Melaku MS, et al. Machine learning to predict virological failure among HIV patients on antiretroviral therapy in the University of Gondar Comprehensive and Specialized Hospital, in Amhara Region, Ethiopia, 2022. BMC Med Inform Decis Mak. (2023) 23(1):75. doi: 10.1186/s12911-023-02167-7
27. Kebede SD, Mamo DN, Adem JB, Semagn BE, Walle AD. Machine learning modeling for identifying predictors of unmet need for family planning among married/in-union women in Ethiopia: evidence from performance monitoring and accountability (PMA) survey 2019 dataset. PLOS Digital Health. (2023) 2(10):e0000345. doi: 10.1371/journal.pdig.0000345
28. Demsash AW, Chereka AA, Walle AD, Kassie SY, Bekele F, Bekana T. Machine learning algorithms’ application to predict childhood vaccination among children aged 12–23 months in Ethiopia: evidence 2016 Ethiopian Demographic and Health Survey dataset. PLoS One. (2023) 18(10):e0288867. doi: 10.1371/journal.pone.0288867
30. Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, et al. Scikit-learn: machine learning in python. J Mach Learn Res. (2011) 12:2825–30.
31. Lundberg SM, Lee S-I. A unified approach to interpreting model predictions. Adv Neural Inf Process Syst. (2017) 30. Available at: https://proceedings.neurips.cc/paper/2017/hash/8a20a8621978632d76c43dfd28b67767-Abstract.html
32. Gebreyesus Y, Dalton D, Nixon S, De Chiara D, Chinnici M. Machine learning for data center optimizations: feature selection using Shapley Additive exPlanation (SHAP). Future Internet. (2023) 15(3):88. doi: 10.3390/fi15030088
33. Habte F, Demissie M. Magnitude and factors associated with institutional delivery service utilization among childbearing mothers in Cheha district, Gurage zone, SNNPR, Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. (2015) 15(1):1–12. doi: 10.1186/s12884-015-0716-8
34. Doctor HV, Nkhana-Salimu S, Abdulsalam-Anibilowo M. Health facility delivery in sub-Saharan Africa: successes, challenges, and implications for the 2030 development agenda. BMC Public Health. (2018) 18:1–12. doi: 10.1186/s12889-018-5695-z
35. Huda TM, Chowdhury M, El Arifeen S, Dibley MJ. Individual and community level factors associated with health facility delivery: a cross sectional multilevel analysis in Bangladesh. PLoS One. (2019) 14(2):e0211113. doi: 10.1371/journal.pone.0211113
36. Ayalew HG, Liyew AM, Tessema ZT, Worku MG, Tesema GA, Alamneh TS, et al. Spatial variation and factors associated with home delivery after ANC visit in Ethiopia; spatial and multilevel analysis. PLoS One. (2022) 17(8):e0272849. doi: 10.1371/journal.pone.0272849
37. Wagle RR, Sabroe S, Nielsen BB. Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth. (2004) 4:1–10. doi: 10.1186/1471-2393-4-8
38. Tariku M, Enyew DB, Tusa BS, Weldesenbet AB, Bahiru N. Home delivery among pregnant women with ANC follow-up in Ethiopia; evidence from the 2019 Ethiopia Mini Demographic and Health survey. Front Public Health. (2022) 10:862616. doi: 10.3389/fpubh.2022.862616
39. Nduka I, Nduka E. Determinants of noninstitutional deliveries in an urban community in Nigeria. J Med Invest Pract. (2014) 9(3):102.
40. Mengesha ZB, Biks GA, Ayele TA, Tessema GA, Koye DN. Determinants of skilled attendance for delivery in Northwest Ethiopia: a community based nested case control study. BMC Public Health. (2013) 13(1):1–6. doi: 10.1186/1471-2458-13-130
41. Feyissa TR, Genemo GA. Determinants of institutional delivery among childbearing age women in Western Ethiopia, 2013: unmatched case control study. PLoS One. (2014) 9(5):e97194. doi: 10.1371/journal.pone.0097194
42. Dickson KS, Adde KS, Amu H. What influences where they give birth? Determinants of place of delivery among women in Rural Ghana. Int J Reprod Med. (2016) 2016:7203980. doi: 10.1155/2016/7203980
43. Ejigu AG, Yismaw AE, Limenih MA. The effect of sex of last child on short birth interval practice: the case of northern Ethiopian pregnant women. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4110-x
44. Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci. (2014) 24:93–104. doi: 10.4314/ejhs.v24i0.9S
Keywords: machine learning, home delivery, ANC visit, East Africa, prediction
Citation: Walle AD, Kebede SD, Adem JB and Mamo DN (2025) Machine-learning algorithm to predict home delivery after antenatal care visit among reproductive age women in East Africa. Front. Glob. Women's Health 6:1461475. doi: 10.3389/fgwh.2025.1461475
Received: 16 July 2024; Accepted: 2 May 2025;
Published: 5 June 2025.
Edited by:
Sarosh Iqbal, Forman Christian College, PakistanReviewed by:
Kanchan Thapa, Noble Shivapuri Research Institute, NepalAdauto Barbosa, Fluminense Federal University, Brazil
Copyright: © 2025 Walle, Kebede, Adem and Mamo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Agmasie Damtew Walle, YWdtYXNpZTg5QGdtYWlsLmNvbQ==
 Agmasie Damtew Walle
Agmasie Damtew Walle Shimels Derso Kebede
Shimels Derso Kebede Jibril Bashir Adem
Jibril Bashir Adem Daniel Niguse Mamo
Daniel Niguse Mamo