- 1Department of Public Health, Faculty of Medicine Pattimura University, Ambon, Indonesia
- 2National Research and Innovation Agency Republic of Indonesia, Bogor, Indonesia
- 3Faculty of Medicine, Pattimura University, Ambon, Indonesia
- 4Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
- 5Sydney School of Public Health, Faculty of Medicine and Health, Sydney, NSW, Australia
Introduction: Although Indonesia has made significant progress in improving maternal and child health nationally, regional disparities persist, particularly in eastern Indonesia, where maternal and neonatal health outcomes remain suboptimal compared with the western regions. This study examined factors associated with non-use of antenatal care (ANC) in eastern Indonesia.
Methods: We analyzed data from 3,261 mothers with infants under one year of age in eastern Indonesia who were interviewed in the 2023 Indonesia Health Survey. The primary outcome was maternal non-use at ANC during pregnancy with an infant younger than 12 months at the time of the survey. Eighteen potential predictors of non-use of ANC were assessed using a multilevel analysis.
Results: Approximately 5% (95% CI: 4.14–6.09) of the mothers with infants 0–11 months did not seek antenatal care. Non-use was associated with infant age, region, socioeconomic status, health checks, knowledge of stunting, and pregnancy-related complications. Mothers with infants aged 6–11 months were 63% less likely to forgo ANC [adjusted odds ratio (aOR) = 0.63, p = 0.049]. Living in Sulawesi (aOR = 2.66, p = 0.001), Maluku (aOR = 13.76, p < 0.001), and Papua (aOR = 17.72, p < 0.001) increased ANC non-use. The poorest households had 9.90 times higher odds of non-use than the richest households (p < 0.001). Higher non-use was also linked to no prior health checks (aOR = 2.54, p = 0.006), low stunting knowledge (aOR = 2.93, p = 0.004), and no pregnancy complications (aOR = 4.30, p = 0.001).
Conclusions: Socioeconomic and geographic disparities drive non-use of antenatal care in eastern Indonesia. Improving healthcare access, education, and early screening are crucial for reducing regional inequalities and enhancing maternal health.
Introduction
Antenatal care (ANC) has been widely recognized as a key component of reproductive health services that provides a platform for essential healthcare functions to ensure the well-being of both mother and child during pregnancy (1). Regular ANC visits offer a wide range of essential services for pregnant women, including early detection and management of pregnancy-related complications, nutritional support, immunization, and counselling on safe delivery and new-born care (1, 2). Studies showed that the lack of ANC was associated with an increased risk of maternal and neonatal complications that could lead to various adverse outcomes, such as preterm birth, low birth weight, stillbirth, and even neonatal and maternal mortality (3–5).
The World Health Organization (WHO) recommends a minimum of eight ANC visits during pregnancy to optimize maternal and foetal health outcomes (1). Nevertheless, in many low—and middle-income countries, ANC utilization remains suboptimal, with sometimes disparities across regions, particularly in remote and underdeveloped areas where barriers such as limited health infrastructure and geographic inaccessibility usually affect the uptake of the service (6).
The Ministry of Health (MOH) in Indonesia recommends that pregnant women attend at least six antenatal visits during pregnancy: one in the first trimester, two in the second trimester, and three in the third trimester. Although this is fewer than the eight-contact model recommended by the WHO (7), the national guideline represents a progressive shift from the previous standard of four visits, aiming to improve maternal and neonatal outcomes within the context of Indonesia's healthcare capacity and regional disparities. This adaptation balances global recommendations with local feasibility and accessibility constraints, particularly in remote and underdeveloped areas. National data also showed a steady increase in the proportion of women accessing ANC services over time as the proportion of pregnant women receiving at least one ANC visit increased from 95.4% in 2013 (8) to 96.6% in 2023 (9).
However, the national reports showed that the proportion varied considerably across regions (2, 10). The latest 2023 Indonesia Health Survey reported that the proportion of women attending at least one ANC visit in eastern Indonesia was much lower than in western Indonesia. For example, while 99.6% of pregnant women in Bali (Western Indonesia) received at least one ANC visit, only 58.7% of pregnant women in the Papua region (Eastern Indonesia) did so (9). Studies also reported a higher mortality rates including perinatal and infant mortality in the eastern than western region of Indonesia (4, 11). Studies showed that these deaths was also found to be associated with inadequate antenatal care (11, 12). This evidence indicates that despite the significant progress made by the Government of Indonesia to improve maternal and child health status nationally over the past few decades (9, 13), the outcomes remain suboptimal in eastern Indonesia (4, 14).
Numerous studies have reported the role of various factors influencing ANC use, such as maternal knowledge (14), wealth index (2, 4), and access to healthcare facilities (15, 16). Nevertheless, specific variations in healthcare-seeking behavior in eastern Indonesia remain underexplored. Addressing this gap is therefore important for policymakers and program managers to understand the region-specific determinants of ANC use and further design targeted, region-specific interventions.
In 2023, the MOH of the Republic of Indonesia conducted the 2023 Indonesian Health Survey, which assessed key health indicators nationwide (9). This survey provides essential baseline data on maternal and child health, nutrition, and healthcare use to inform national health policies. Using data from this survey, this analysis aimed to identify factors associated with the non-use of ANC in eastern Indonesia. These findings will help inform strategies to enhance ANC coverage and ultimately reduce maternal and neonatal morbidity and mortality in eastern Indonesia and Indonesia in general.
Materials and methods
Data source and survey design
The data used in this analysis were derived from the 2023 Indonesian Health Survey (9), conducted by the MOH, Republic of Indonesia, using a multistage systematic random sampling method. Since 2007, the MOH has conducted a cross-sectional household health survey every five years to establish baseline data and monitor health-related indicators at the district, provincial, and national levels. The 2023 survey sample size was designed to allow for district-level estimations (9). A detailed explanation of the survey methodology has been provided elsewhere (9).
The 2023 Indonesian Health Survey included a representative sample of households from 38 provinces and 514 districts or cities. It covered 345,000 general households for the basic health survey and an additional 104,000 households with children under five years of age for the nutritional survey. These households were selected from 34,500 census blocks.
At the individual level, 1,191,692 participants were interviewed. For this analysis, we used data from 3,261 mothers with infants aged 0–11 months residing in eastern Indonesia. The region classified as eastern Indonesia comprises Nusa Tenggara Barat, Nusa Tenggara Timur, Sulawesi, Maluku, and Papua (Figure 1). The data were accessed on 1 December 2024, for the purposes of the current research.
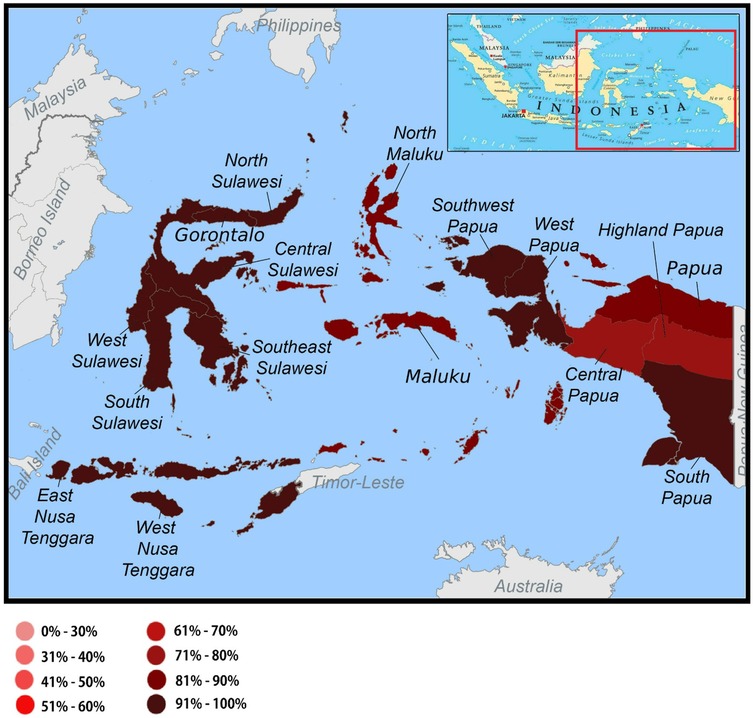
Figure 1. Distribution of the non-use of antenatal care service among mothers with infants aged 0–11 months in the eastern part of Indonesia, the 2023 Indonesia health survey.
Outcome variable
The primary outcome was maternal non-useuse at ANC during the pregnancy in infants younger than 12 months at the time of the survey. The non-use was determined based on the question: “Did you seek ANC from a healthcare provider?” Mothers who did not seek ANC services were assigned a score of 1, while those who attended ANC were assigned a score of 0.
Potential predictors
We included 18 potential predictors of ANC non-use, categorized into five main groups: community factors, household characteristics, parental demographics, maternal exposure to health information and healthcare, and maternal obstetric characteristics. We included the child's age at the time of the survey to account for potential recall bias since mothers of older infants may recall ANC visits less accurately, and to account for contextual differences that may influence ANC use.
Two variables were included in the community characteristics: region (West Nusa Tenggara, East Nusa Tenggara, Sulawesi, Maluku, and Papua) and type of residence (urban or rural). In terms of household characteristics, the number of children under five years old (one, two, or three or more) and the household wealth index (richest, rich, middle, poor, poorest) were included. The household wealth index was constructed using Principal Component Analysis16 based on 16 housing characteristics and assets owned by respondents: (1) predominant wall material, (2) predominant floor material, (3) source of drinking water, (4) type of latrine, (5) method of waste disposal, (6) source of electricity, (7) type of cooking fuel, (8) ownership of a washing machine, (9) ownership of a refrigerator, (10) ownership of a mobile phone, (11) ownership of an air conditioner, (12) ownership of a computer, (13) ownership of a flat-screen television (minimum 30 inches), (14) ownership of a motorcycle, (15) ownership of a car, and (16) ownership of at least 10 grams of gold.
For the parental demographic characteristics, we considered four variables: maternal education (academy or university, completed senior high school, completed junior high school, incomplete elementary school), maternal occupation (housewife or not working outside the home, formal worker, informal worker, or student), paternal education (academy or university, completed senior high school, completed junior high school, incomplete elementary school), and paternal occupation (formal worker, informal worker, or unemployed).
Three variables were included in the group of maternal exposure to health information and care: health-seeking behavior (once or more every six months, once a year or less, never), knowledge and awareness about pregnancy danger signs (high, low), and knowledge and awareness about stunting (high, low). To calculate the respondents' level of knowledge about the danger signs of pregnancy, we used the information from seven questions. These included signs such as vaginal bleeding, swelling of the legs, hands, or face accompanied by headache, high fever, convulsions, early rupture of membranes, reduced or no fetal movement, and persistent vomiting or loss of appetite. The correct response for each question was assigned a score of one. The total knowledge score was calculated, and those scoring above the median were classified as having a high level of knowledge, whereas those scoring at or below the median were categorized as having a low level of knowledge.
The knowledge and awareness of stunting was assessed based on four knowledge groups: definition (nine correct answers), causes (six correct answers), impact (six correct answers), and prevention (eight correct answers) of stunting. The total knowledge score ranged from 0 (all responses were incorrect) to 29 (all correct). Respondents with scores above the median were classified as having a high level of knowledge, whereas those with scores at or below the median were categorized as having a low level of knowledge.
Finally, we included six variables for maternal exposure to health information and care: age at childbirth (<20, 20–29, 30–39, ≥40 years), pregnancy order (first pregnancy, second or third pregnancy, and fourth or more), number of childbirths, history of abortion (yes/no), presence of pregnancy complications (yes or no), and pregnancy intention (yes, no, or only then).
Data analysis
First, descriptive statistical methods were used to examine the distribution of all variables included in the analysis. This was followed by bivariate analyses to explore the distribution of these variables according to ANC attendance status. We then used multilevel analysis with two sequential models that incorporated random intercepts to examine the factors associated with the non-use of ANC.
In the multilevel analysis, a three-level logistic regression model was applied to account for the hierarchical structure of the data, with individuals (Level 1) nested within Primary Sampling Units (PSUs) (Level 2), which were further nested within districts (Level 3) and provinces (Level 4). The null model (also called an empty model), which included no explanatory variables, was constructed to examine the extent to which the primary sampling unit, district, and province levels were associated with ANC attendance without adjusting for individual, household, or community-level predictors. The median odds ratio (MOR) was calculated for each level to quantify its contribution to ANC nonattendance.
Following the null model, we constructed Model 1 by introducing all the explanatory variables. This allowed us to assess the extent to which the explanatory characteristics explained the variation in ANC non-use while accounting for the nested structure of the data. We applied backward elimination to remove factors that were not significantly associated with the outcome, using a significance threshold of 0.05. Four variables— the child's age, region, type of residence (urban or rural), and household wealth index—were selected a priori and retained in the final model regardless of their statistical significance. Adjusted odds ratios (aORs) were used to estimate the association between each potential predictor and the study outcome.
The final model presented adjusted odds ratios (aORs) and 95% confidence intervals (95% CIs) for all predictors. This analysis accounted for the complexity of the sample design. Multilevel models were developed using the Stata/MP software (version 14.2; StataCorp, College Station, TX, USA) with a melogit routine.
Ethical approval and informed consent
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval for the 2023 Indonesia Health Survey was obtained from the Health Research Ethics Committee of the Health Polytechnic of the Ministry of Health Jakarta II (Komisi Etik Penelitian Kesehatan Poltekkes Kemenkes Jakarta II), under reference number LB.02.01/I/KE/L/287/2023.
Results
This analysis used information collected from 3,262 mothers of infants aged 0–11 months residing in eastern Indonesia. Most mothers were from households with only one child under five years of age (68.0%) and had a partner who worked in the informal sector (77.4%). Most mothers were housewives (61.1%), had a low level of awareness of stunting (77.6%), and did not experience any pregnancy complications (83.9%) (Table 1).
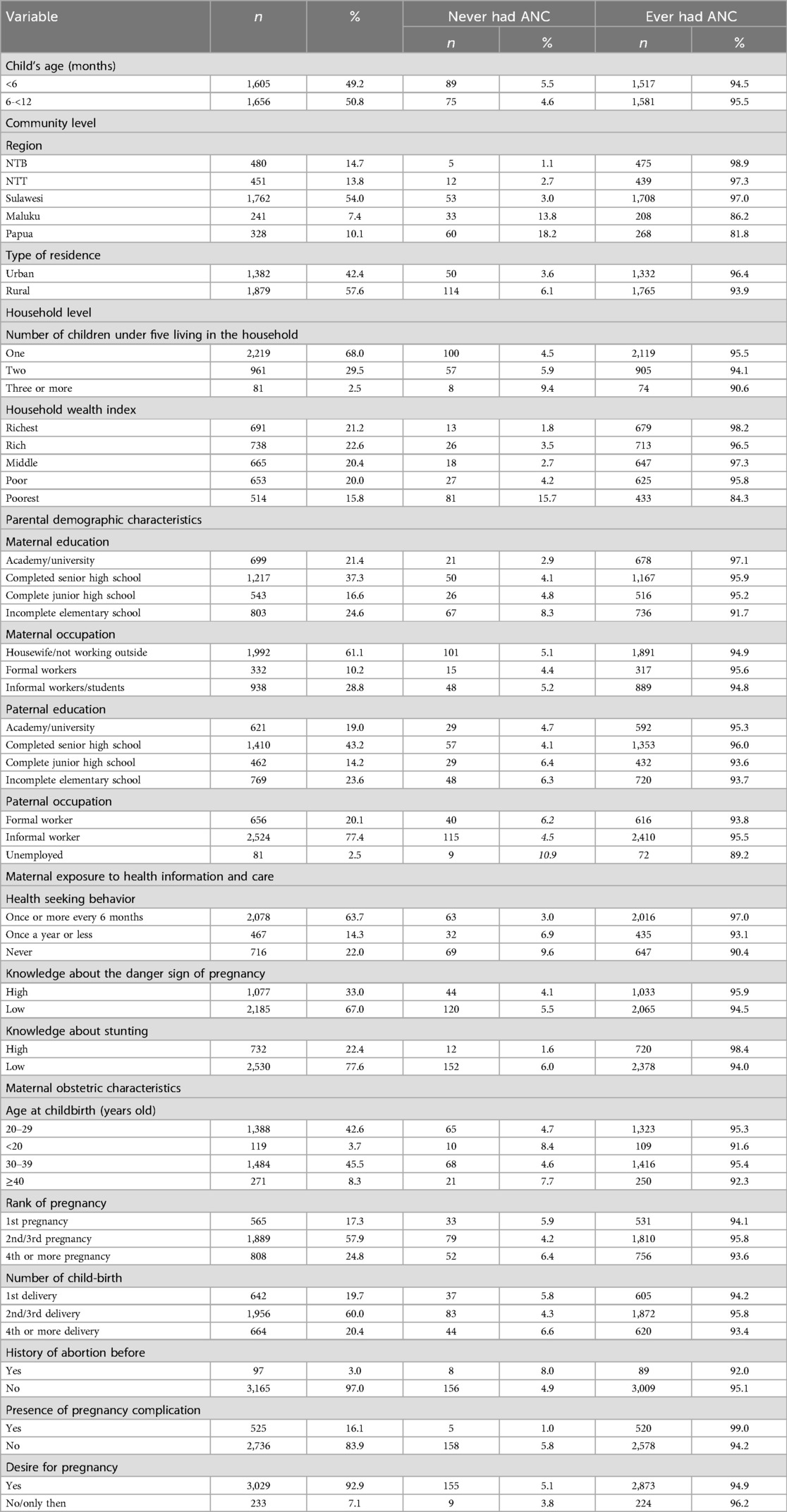
Table 1. Frequency distribution of factors analyzed in this study, the 2023 Indonesia health survey.
Our analysis showed that approximately 5% (95% CI: 4.14–6.09) of the mothers did not seek antenatal care services from healthcare providers. The province of Central Papua had the highest percentage of mothers not attending ANC services (37.2%, 95% CI: 22.9–54.2) (Figure 2). The proportion of ANC non-use by district in each region is presented in Supplementary Figures S1–S5.
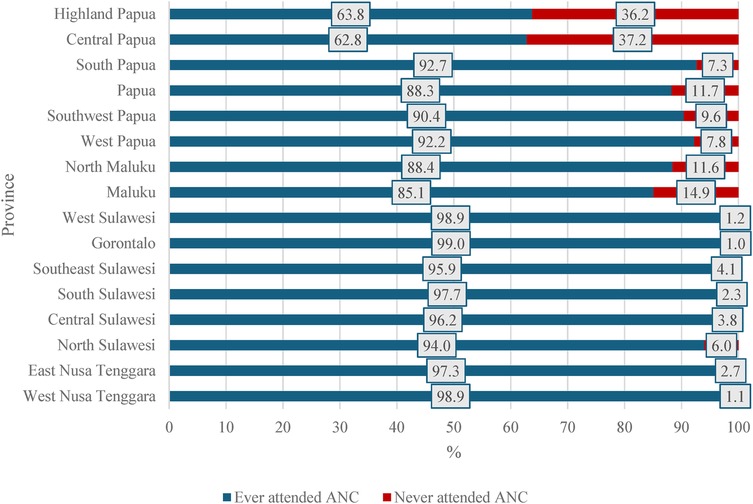
Figure 2. Frequency distribution of antenatal care use by mothers with infants aged 0–11 months in the eastern part of Indonesia, the 2023 Indonesia health survey.
Table 2 shows the multilevel modelling results of the factors associated with the non-use of ANC services. Interestingly, mothers with infants aged 6 to 12 months at the time of the interview were more likely to have attended ANC services during their pregnancy than mothers with younger infants (aged <6 months). This was mirrored by the reduced odds of not attending ANC among mothers of infants aged 6 to <12 months (aOR = 0.63, 95% CI: 0.40–1.00, p = 0.049). Furthermore, mothers residing in Sulawesi (aOR = 2.66, 95% CI: 1.49–4.75, p = 0.001), Maluku (aOR = 13.76 95% CI: 5.79–54.29, p < 0.001), and Papua (aOR = 17.72, 95% CI: 5.79–54.29, p < 0.001) demonstrated significantly higher odds of not attending ANC services compared to those living in Nusa Tenggara Barat region.
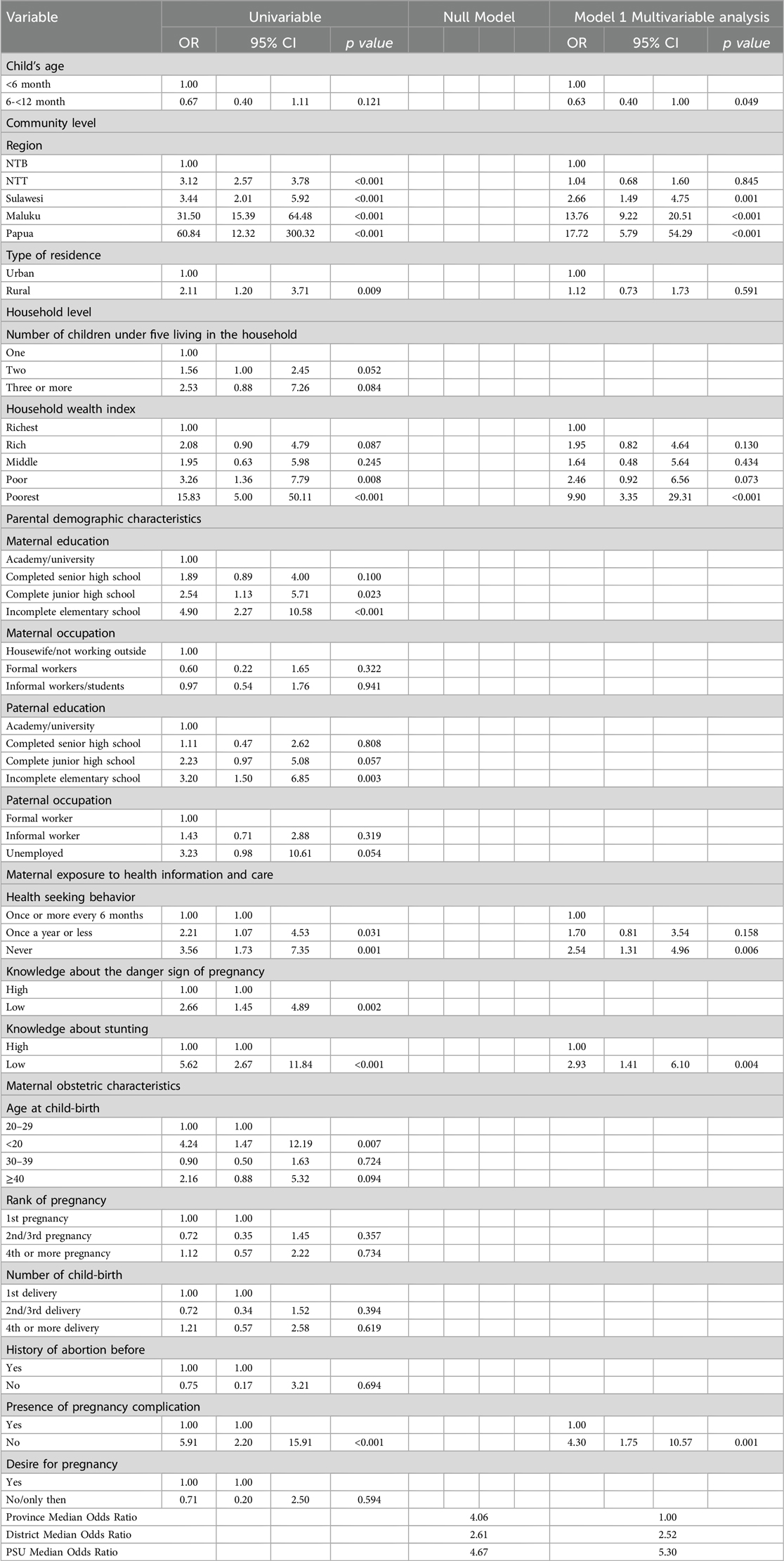
Table 2. Factors associated with the non-use of ANC among mothers with children aged 0–11 months living in the eastern region of Indonesia, the 2023 Indonesia health survey.
At the household level, mothers from the poorest households had significantly higher odds of not attending ANC services than those from the richest households (aOR = 9.90, 95% CI: 3.35–29.31, p < 0.001). As expected, mothers who had never had any health checks were more likely not to attend ANC services than those who underwent health checks regularly at least once every six months (aOR = 2.54, 95%CI:1.31–4.96, p = 0.006). Figure 3 presents the distribution of general health examinations among mothers in eastern Indonesia. The highest percentage of those who had never had any health checks (45.2%) was found in Central Papua Province (95% CI: 29.1–62.3).
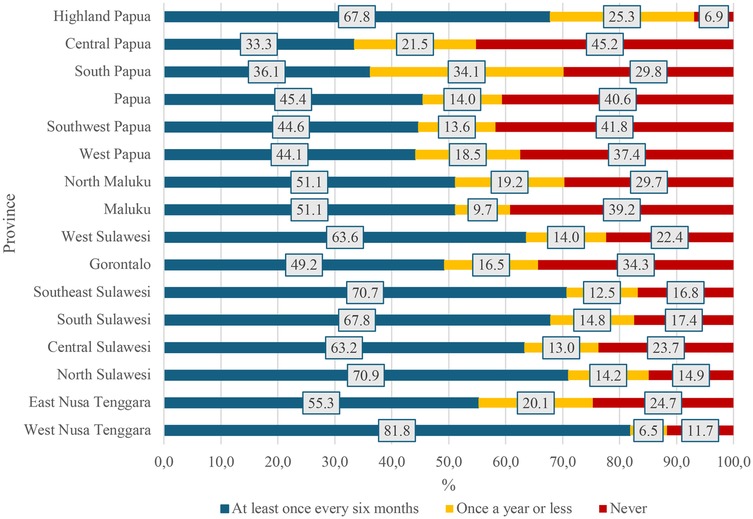
Figure 3. Frequency distribution of general health examination among mothers with infants aged 0–11 months in the eastern part of Indonesia, the 2023 Indonesia health survey.
Moreover, our analysis showed that a low level of maternal knowledge of stunting was also associated with mothers’ non-use at ANC services (aOR = 2.93, 95% CI: 1.41–6.10, p = 0.004). Notably, Central and South Papua had the highest proportion of mothers with a low level of knowledge and awareness about stunting at 91.0% (Figure 4). In addition, the absence of pregnancy complications was significantly associated with non-use at ANC services (aOR = 4.30, 95% CI: 1.75–10.57, p = 0.001).
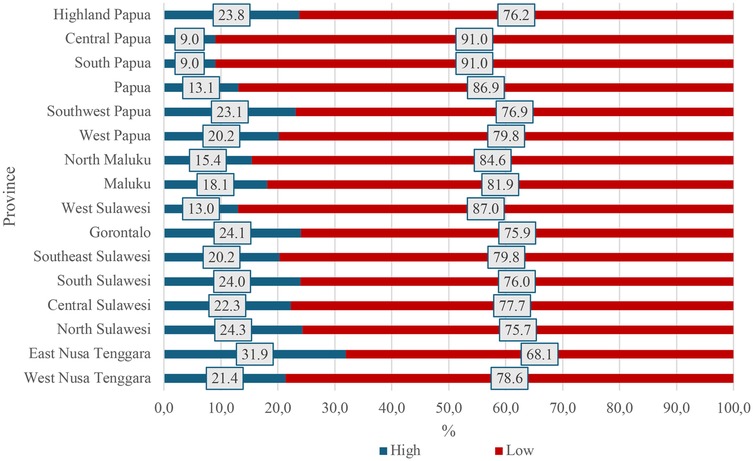
Figure 4. Frequency distribution of the level of knowledge and awareness about stunting among mothers with infants aged 0–11 months in the eastern part of Indonesia, the 2023 Indonesia health survey.
In the null model, the MOR was 4.06 at the province level, 2.61 at the district level, and 4.67 at the PSU level, indicating substantial variation in ANC non-use across all three geographic levels when no explanatory variables were included. After adjusting for all significant predictors in Model 1, the MOR decreased at the provincial level (to 1.00), suggesting that individual characteristics fully explained the variance between provinces. However, the MOR remained relatively unchanged at the district level (2.52) but increased at the PSU level (5.30), indicating substantial variation in average individual characteristics across PSU.
Discussion
Main findings
Our analysis highlighted the role of environmental, household, and maternal factors in ANC non-use among mothers with infants aged 0–11 months residing in eastern Indonesia. ANC attendance was lower among mothers of younger infants (<6 months) than among those of older infants. At the environmental level, the geographic region emerged as a significant predictor of ANC non-use. At the household level, the household wealth index was significantly associated with ANC use, with lower wealth linked to lower service utilization. Among maternal-level factors, limited health-seeking behavior, poor knowledge about stunting, and absence of pregnancy complications were all significantly associated with non-use. These findings underscore the need for targeted, context-specific interventions to improve ANC coverage, especially among the disadvantaged and underserved populations in eastern Indonesia.
Factors associated with ANC non-use in eastern Indonesia
Our findings showed that ANC attendance was lower among mothers with infants aged <6 months than mothers with older infants. This finding may possibly reflect the evolving impact of the Coronavirus Disease 2019 (COVID-19) pandemic. Although we did not have data on the exact timing of pregnancy in relation to the pandemic phases, it is plausible that heightened concern over COVID-19 in early 2022 encouraged greater ANC engagement as a protective health-seeking behavior (9). However, as fear declined by late 2022, care-seeking behavior also appeared to decrease. The transition from emergency to routine health system operations led to the reallocation of resources, staffing shortages, and lingering healthcare worker burnout, which may have disrupted ANC availability (17, 18). The long-term economic effects of the pandemic likely forced some women to deprioritize healthcare visits due to financial constraints (19).
Our study confirmed regional disparities in ANC utilization. Mothers in the Sulawesi, Maluku, and Papua regions were less likely to attend services than those living in Nusa Tenggara Barat. Several potential barriers hinder ANC attendance in these regions, such as geographic isolation, limited health infrastructure, workforce shortages, cultural beliefs, low health literacy, and economic hardship (14, 20). In contrast, it was reported that the Nusa Tenggara Barat benefitted from stronger infrastructure, a well-connected network of community health centers or Puskesmas and hospitals, and targeted maternal programs, supported by better transportation and higher population density (21, 22). We found that ANC attendance in Papua remained among the lowest, which may be attributed to factors such as rugged terrain, dispersed settlements, and a relatively weak health system (22). In particular, Central Papua, a newly established province, and Highland Papua face additional challenges, including administrative and logistical delays in health system development (23). Furthermore, ongoing geopolitical instability and security concerns related to armed conflict in these regions may further limit access to healthcare. In some areas, the presence of extremist groups and intermittent violence has made it unsafe for residents to leave their homes, leading to reluctance to visit primary health centers or other health facilities. These complex barriers likely contribute to the persistently low ANC coverage observed in these provinces. Similarly, women living in Maluku Province might also face challenges related to its archipelagic geography and high inter-island travel costs (24). Our findings showed that even within eastern Indonesia, ANC use varied notably across provinces, indicating that challenges in access are not uniformly experienced. These intra-regional disparities further emphasize the broader gap between eastern and western Indonesia, where the latter benefits from stronger infrastructure and better maternal health outcomes. Addressing these layered inequalities requires locally tailored strategies that respond to both regional and province-specific needs.
The increased likelihood of mothers from the poorest households not attending ANC services indicates the importance of socioeconomic disparities in maternal healthcare access. This is consistent with findings from previous studies conducted in Indonesia and other low- and middle-income countries (10, 14, 25–27). In Indonesia, antenatal care is officially provided free of charge at both integrated health posts, locally known as Pos Pelayanan terpadu or Posyandu, and primary-level facilities, mainly on Puskesmas, particularly the beneficiaries of the Indonesian National Health Insurance (NHI). Despite the high NHI coverage in Indonesia, the uptake among its beneficiaries when accessing health services was reported to be suboptimal (27, 28). This is consistent with our previous study from Maluku Province, which revealed that less than 15% of NHI beneficiaries used NHI when accessing health services.1 Moreover, although ANC services are provided free of charge, other indirect costs, such as transportation, childcare, and lost income due to time off work, could continue to burden low-income households.
Mothers who did not engage in regular health checkups were less likely to use ANC services. This finding aligns with previous studies (29, 30) indicating that the absence of routine interactions with the healthcare system could lead to low awareness, limited familiarity with medical services, and reduced trust in healthcare providers—all of which might discourage ANC attendance (31).
Our study also confirmed the role of maternal knowledge and awareness in ANC uptake, as previously reported (32). We found that mothers with limited knowledge of stunting were also less likely to attend ANC services, potentially due to a lack of understanding of the role of ANC in preventing stunting and promoting child health. A study conducted in West Java, Indonesia, found that improving maternal knowledge significantly increased interest and motivation to use ANC services (11).
Interestingly, mothers without obstetric complications during pregnancy had a reduced likelihood of attending ANC, as reported in previous studies (30, 32, 33). This suggests that women without complications might perceive less need to seek care during pregnancy. Consequently, mothers who did not have any pregnancy complications might perceive their pregnancies as low risk, leading them to underestimate the importance of ANC services. This perception could result in lower ANC attendance, as they might not recognize the role of routine ANC checkups in detecting and preventing potential complications.
Although not explored in this study, cultural values and local wisdom could influence maternal health-seeking behavior in eastern Indonesia, as reported in several qualitative studies (34–36). Traditional beliefs, such as reliance on family elders or traditional birth attendants, could delay or deter ANC visits. Gender roles, trust in modern healthcare, and local norms also shape service uptake. Therefore, further research to understand and integrate these sociocultural factors is essential to improving ANC uptake and ensuring health programs are culturally appropriate (37–40).
The MOR values from our multilevel analysis revealed important insights into the contextual variation in ANC nonattendance across geographic levels. The high MOR in the null model at the province, district, and PSU levels indicated substantial clustering, suggesting that regional and local factors were significantly associated with ANC nonattendance. After adjusting for the significant explanatory variables, the MOR at the provincial level indicated that the explanatory variables largely explained inter-provincial differences. However, MOR remained high at the district level and increased at the PSU level. This shows persistent unexplained variations at more localized levels. These findings suggest that structural, operational, or contextual barriers, such as uneven health facility distribution, staffing shortages, or access issues at the community level, might continue to limit ANC uptake.
Policy implications
Our findings indicate the need for sustained efforts to improve ANC uptake in eastern Indonesia. Raising community knowledge and awareness of the universal benefits of ANC, regardless of perceived pregnancy-related risk, is essential. Various health promotion strategies have been reported to be effective in improving maternal and child health knowledge, both individual and community-based interventions, such as through home visits (24), group counselling (41), and culturally tailored community outreach (42). Furthermore, health workers should use every contact opportunity to educate women and their families about the importance of early and regular ANC and the services available to support a healthy pregnancy.
Efforts to ensure that ANC is financially accessible are also critical. Policies that reduce the financial burden on pregnant women, such as subsidies, conditional cash transfers, or integration of ANC costs into national health insurance schemes, should be considered (27). Additionally, our findings underscore the importance of strengthening mobile health outreach (e.g., mobile clinics, home visits, or temporary outreach posts) to bring services directly to communities (43, 44). The use of telemedicine services (45), provision of incentives for rural health workers (46, 47), and ensuring reliable transportation support (24) could help overcome geographical and logistical barriers that will improve service accessibility. Future preparedness strategies should also ensure uninterrupted access to essential maternal health services during public health crises such as pandemics. This requires strengthening health system resilience and implementing adaptable service delivery models that could continue operating during future public health emergencies (18, 48). Our study also suggests that efforts to improve ANC utilization must extend beyond individual-level interventions and address health system gaps and service delivery challenges at community and sub-district levels.
These findings highlight the need for regionally tailored health policies to address both inter- and intra-regional disparities in ANC access. Localized approaches are crucial to accommodate the diverse geographical and administrative contexts in eastern Indonesia. Strengthening subnational health systems—particularly in provinces like Central Papua and Maluku is essential. Bridging the development gap between eastern and western Indonesia requires equitable resource allocation and stronger oversight of maternal health programs is important to ensure progress toward national health goals.
Strengths and limitations of the study
This study used nationally representative data with a large sample size, enabling a robust analysis of the factors associated with ANC non-use in Indonesia. A key strength is its focus on the eastern region, where access to healthcare is limited. The findings highlight regional disparities and context-specific barriers and offer valuable insights for targeted interventions. The use of multilevel modelling also allowed for a comprehensive assessment of provincial-, district-, and individual-level influences on ANC utilization. However, this study had several limitations. Its cross-sectional design precludes causal inference, and the lack of variables on service access, availability, and affordability limits the analysis. It also lacks qualitative insights into maternal beliefs and perceptions of care. Remote areas may be underrepresented, and reliance on self-reported data may introduce a recall bias.
Conclusions
In conclusion, this study highlights the key factors associated with ANC non-use in eastern Indonesia, where access to care remains limited. ANC nonattendance was associated with regional disparities, socioeconomic status, health-seeking behavior, knowledge of stunting, and perceived pregnancy risks. Additionally, the geographic isolation, economic hardship, and lingering effects of COVID-19 further hindered the community's access to health services. Targeted region-specific strategies, such as mobile health services, telemedicine, transportation support, and community-based education, will help improve uptake. Furthermore, efforts to develop locally tailored policies and health promotion strategies are essential to ensure that no woman is left behind in accessing quality antenatal care, regardless of geography, income, or perceived risk.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval for the 2023 Indonesia Health Survey was obtained from the Health Research Ethics Committee of the Health Polytechnic of the Ministry of Health Jakarta II (Komisi Etik Penelitian Kesehatan Poltekkes Kemenkes Jakarta II), under reference number LB.02.01/I/KE/L/287/2023.
Author contributions
CT: Methodology, Conceptualization, Supervision, Writing – review & editing, Formal analysis. DT: Writing – review & editing, Conceptualization. MM: Resources, Writing – review & editing, Writing – original draft, Conceptualization. IA: Writing – review & editing, Supervision, Data curation, Methodology. RI: Writing – original draft, Resources, Writing – review & editing. SI: Resources, Writing – review & editing. MD: Data curation, Writing – review & editing, Supervision, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We gratefully acknowledge the Ministry of Health, Republic of Indonesia, for granting access to a subset of the 2023 Indonesian Health Survey data used in this analysis. We sincerely thank all enumerators and field personnel for their dedication and efforts in data collection under challenging field conditions. We are also deeply indebted to all the respondents who generously shared their time and information, making this study possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnote
1. ^Titaley CR, Ariawan I, Wahyuningsih W, Iwan RF, Malakauseya MLV, Kimberly VD, et al. The use of Indonesia's national health insurance among its beneficiaries in Maluku, one of the largest archipelagic provinces in the country [manuscript under review]. BMJ Open. (2025).
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1649276/full#supplementary-material
References
1. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. (2016). Available online at: https://www.who.int/publications/i/item/9789241549912 (Accessed March 3, 2025).
2. Simkhada B, van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. (2008) 61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x
3. Geltore TE, Anore DL. The impact of antenatal care in maternal and perinatal health. In: Ray A, editor. Empowering Midwives and Obstetric Nurses. IntechOpen (2021). p. 5. Available online at: https://www.intechopen.com/chapters/77303 (Accessed March 07, 2025).
4. Titaley CR, Mu’asyaroh A, Que BJ, Tjandrarini DH, Ariawan I. Determinants of early neonatal mortality: secondary analysis of the 2012 and 2017 Indonesia demographic and health survey. Front Pediatr. (2024) 12:1288260. doi: 10.3389/fped.2024.1288260
5. Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. (2017) 7(11):e017122. doi: 10.1136/bmjopen-2017-017122
6. Sharma J, O’Connor M, Rima Jolivet R. Group antenatal care models in low- and middle-income countries: a systematic evidence synthesis. Reprod Health. (2018) 15(1):38. doi: 10.1186/s12978-018-0476-9
7. Pristya TYR. Besral. Frequency of antenatal care visits and their impact on low birth weight in Indonesia. Malays J Public Health Med. (2024) 24(1):59–66. Available online at: https://mjphm.org/index.php/mjphm/article/view/2424 (Accessed March 25, 2025).
8. Ministry of Health Republic of Indonesia. National Basic Health Research Report 2013. Badan Penelitian Dan Pengembangan Kesehatan Kementerian Kesehatan RI Tahun 2013. Jakarta: Ministry of Health Republic of Indonesia (2014).
9. Ministry of Health Republic of Indonesia—Board of Health Development Policy. The 2023 Indonesia Health Survey in Numbers. Jakarta: Minstry of Health Republic of Indonesia—Board of Health Development Policy (2024). Available online at: https://www.badankebijakan.kemkes.go.id/ski-2023-dalam-angka/
10. Laksono AD, Rukmini R, Wulandari RD. Regional disparities in antenatal care utilization in Indonesia. PLoS One. (2020) 15(2):e0224006. doi: 10.1371/journal.pone.0224006
11. Misnaniarti , Sariunita N, Idris H. Regional perinatal mortality differences in Indonesia: evidence from Indonesian demographic health survey. Public Health Pract. (2024) 7:100501. doi: 10.1016/j.puhip.2024.100501
12. Sampurna MTA, Handayani KD, Utomo MT, Angelika D, Etika R, Harianto A, et al. Determinants of neonatal deaths in Indonesia: a national survey data analysis of 10,838 newborns. Heliyon. (2023) 9(1):e12980. doi: 10.1016/j.heliyon.2023.e12980
13. Badan_Penelitian_dan-Pengembangan_Kesehatan. Riset Kesehatan Dasar, Riskesdas 2013. (2014). (Badan Penelitian Dan Pengembangan Kesehatan Kementerian Kesehatan Ri Tahun 2013).
14. Titaley CR, Dibley MJ, Roberts CL. Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia demographic and health survey 2002/2003 and 2007. BMC Public Health. (2010) 10(1):485. doi: 10.1186/1471-2458-10-485
15. Vasconcelos A, Sousa S, Bandeira N, Alves M, Papoila AL, Pereira F, et al. Determinants of antenatal care utilization—contacts and screenings—in sao tome & principe: a hospital-based cross-sectional study. Arch Public Health. (2023) 81(1):107. doi: 10.1186/s13690-023-01123-1
16. Hijazi HH, Alyahya MS, Sindiani AM, Saqan RS, Okour AM. Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan: a cross-sectional study. Reprod Health. (2018) 15(1):106. doi: 10.1186/s12978-018-0542-3
17. Randell M, Wahyono TYM, Dynes M, Tinessia A, Li M, Danchin M, et al. Service disruptions, trauma and burnout during the COVID-19 pandemic among healthcare providers delivering immunisation and maternal and child health services in Indonesia. BMJ Glob Health. (2024) 9(6):e014318. doi: 10.1136/bmjgh-2023-014318
18. Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health. (2020) 5(6):e002967. doi: 10.1136/bmjgh-2020-002967
19. UNICEF, UNDP, Prospera, SMERU. The social and economic impact of COVID-19 on households in Indonesia: A second round of surveys in 2022. Jakarta, Indonesia. (2022). Report No.: UNICEF/UN_DSF7197/BEA. Available online at: https://www.unicef.org/indonesia/media/15441/file/The%20social%20and%20economic%20impact%20of%20COVID-19%20on%20households%20in%20Indonesia%20.pdf (Accessed March 3, 2025).
20. Cipta DA, Andoko D, Theja A, Utama AVE, Hendrik H, William DG, et al. Culturally sensitive patient-centered healthcare: a focus on health behavior modification in low and middle-income nations—insights from Indonesia. Front Med. (2024) 11:1353037. doi: 10.3389/fmed.2024.1353037
21. Badan Pusat Statistik (BPS). Badan Pusat Statistik Provinsi Nusa Tenggara Barat. Statistics of Nusa Tenggara Barat Province (Badan Pusat Statistik Provinsi Nusa Tenggara Barat). Available online at: https://ntb.bps.go.id (Accessed March 18, 2025).
22. Ministry of Health Republic Indonesia. Regulation of the Minister of Health of the Republic of Indonesia Number 21 of 2020 Concerning the Strategic Plan of the Ministry of Health for 2020–2024. (2020). Available online at: http://peraturan.bpk.go.id/Details/152564/permenkes-no-21-tahun-2020 (Accessed March 23, 2025).
23. Situmorang HE, Sweet L, Graham K, Grant J. Health care provider’s perceptions of factors that influence infant mortality in Papua Indonesia: a qualitative study. Women Birth. (2022) 35(2):201–9. doi: 10.1016/j.wombi.2021.04.007
24. Leosari Y, Uelmen JA, Carney RM. Spatial evaluation of healthcare accessibility across archipelagic communities of Maluku Province, Indonesia. PLOS Global Public Health. (2023) 3(3):e0001600. doi: 10.1371/journal.pgph.0001600
25. Lukwa AT, Siya A, Odunitan-Wayas FA, Alaba O. Decomposing maternal socioeconomic inequalities in Zimbabwe; leaving no woman behind. BMC Pregnancy Childbirth. (2022) 22(1):239. doi: 10.1186/s12884-022-04571-9
26. Bobo FT, Asante A, Woldie M, Dawson A, Hayen A. Spatial patterns and inequalities in skilled birth attendance and caesarean delivery in sub-Saharan Africa. BMJ Glob Health. (2021) 6(10):e007074. doi: 10.1136/bmjgh-2021-007074
27. Lee JT, McPake B, Putri LP, Anindya K, Puspandari DA, Marthias T. The effect of health insurance and socioeconomic status on women’s choice in birth attendant and place of delivery across regions in Indonesia: a multinomial logit analysis. BMJ Glob Health. (2023) 8(1):e007758. doi: 10.1136/bmjgh-2021-007758
28. Social Security Agency on Health. Active Registered Primary Healthcare Facilities with BPJS. Jakarta: BPJS (2024).
29. Tripathy A, Mishra PS. Inequality in time to first antenatal care visits and its predictors among pregnant women in India: an evidence from national family health survey. Sci Rep. (2023) 13(1):4706. doi: 10.1038/s41598-023-31902-3
30. Tanberika FS, Sansuwito TB, Hassan HC. Knowledge in enhancing antenatal care compliance and improving maternal and neonatal health outcomes. J Angio. (2024) 8(12):1–7. doi: 10.25163/angiotherapy.81210081
31. Barman K, Roy R, Adhikary M, Saha A, Debnath T. Role of demographic and socio-economic factors for influencing on utilization of maternal health care services among the scheduled tribe women: an experience from the EAG states of India. Glob Soc Welf. (2024) 11(1):1–15. doi: 10.1007/s40609-023-00272-z
32. Mwenebanda E, Machado A, Patel AI, Nyondo-Mipando AL, Chiumia IK. Factors influencing antenatal care attendance in the eight contact era policy: a case of selected maternal health service facilities in Blantyre, Malawi. BMC Pregnancy Childbirth. (2024) 24(1):704. doi: 10.1186/s12884-024-06895-0
33. Alemu DA, Zegeye AM, Zeleke LB, Dessie WK, Melese YD, Tarik YD, et al. Pregnancy risk perception and associated factors among pregnant women attending antenatal care at health centers in Jabi Tehnan District, Amhara, Northwestern Ethiopia, 2021. Int J Reprod Med. (2022) 2022:6847867. doi: 10.1155/2022/6847867
34. Damayanti NA, Wulandari RD, Ridlo IA. Maternal health care utilization behavior, local wisdom, and associated factors among women in urban and rural areas, Indonesia. Int J Women’s Health. (2023) 15:665–77. doi: 10.2147/IJWH.S379749
35. Sakti SA, Endraswara S, Rohman A. Revitalizing local wisdom within character education through ethnopedagogy apporach: a case study on a preschool in Yogyakarta. Heliyon. (2024) 10(10):e31370. doi: 10.1016/j.heliyon.2024.e31370
36. Arjaya IBA, Suastra IW, Redhana IW, Sudiatmika AAIAR. Global trends in local wisdom integration in education: a comprehensive bibliometric mapping analysis from 2020 to 2024. IJLTER. (2024) 23(7):120–40. doi: 10.26803/ijlter.23.7.7
37. Agus Y, Horiuchi S, Porter SE. Rural Indonesia women’s traditional beliefs about antenatal care. BMC Res Notes. (2012) 5(1):589. doi: 10.1186/1756-0500-5-589
38. Sumankuuro J, Crockett J, Wang S. Sociocultural barriers to maternity services delivery: a qualitative meta-synthesis of the literature. Public Health. (2018) 157:77–85. doi: 10.1016/j.puhe.2018.01.014
39. Nasir S, Zerihun Kea A, Steege R, Limato R, Tumbelaka P, Datiko DG, et al. Cultural norms create a preference for traditional birth attendants and hinder health facility-based childbirth in Indonesia and Ethiopia: a qualitative inter-country study. Int J Health Promot Educ. (2020) 58(3):109–23. doi: 10.1080/14635240.2020.1719862
40. Adatara P, Strumpher J, Ricks E, Mwini-Nyaledzigbor PP. Cultural beliefs and practices of women influencing home births in rural Northern Ghana. Int J Womens Health. (2019) 11:353–61. doi: 10.2147/IJWH.S190402
41. Heryanto E, Meliyanti F. The relationship between knowledge, occupation, and counselling with family Head’s action in preventing dengue fever (DHF). Lentera Perawat. (2021) 2(1):8–16. doi: 10.52235/lp.v2i1.156
42. Haldane V, Chuah FLH, Srivastava A, Singh SR, Koh GCH, Seng CK, et al. Community participation in health services development, implementation, and evaluation: a systematic review of empowerment, health, community, and process outcomes. PLoS One. (2019) 14(5):e0216112. doi: 10.1371/journal.pone.0216112
43. Grindrod KA, Li M, Gates A. Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR Mhealth Uhealth. (2014) 2(1):e3048. doi: 10.2196/mhealth.3048
44. Choudhury A, Shahsavar Y, Sarkar K, Choudhury MM, Nimbarte AD. Exploring perceptions and needs of Mobile health interventions for nutrition, anemia, and preeclampsia among pregnant women in underprivileged Indian communities: a cross-sectional survey. Nutrients. (2023) 15(17):3699. doi: 10.3390/nu15173699
45. Goldstein CM, Gathright EC, Dolansky MA, Gunstad J, Sterns A, Redle JD, et al. Randomized controlled feasibility trial of two telemedicine medication reminder systems for older adults with heart failure. J Telemed Telecare. (2014) 20(6):293–9. doi: 10.1177/1357633X14541039
46. Dwi Wulandari R, Laksono AD. Education as predictor of the knowledge of pregnancy danger signs in rural Indonesia. Int J Innov Creat Chan. (2020) 13(1):2020. Available online at: www.ijicc.net
47. Laksono AD, Wulandari RD. The barrier to maternity care in rural Indonesia. Zeitschrift fur Gesundheitswissenschaften. (2022) 30(1):135–40. doi: 10.1007/s10389-020-01274-3
Keywords: antenatal care services, maternal health, health care utilization, public health, pregnancy, community health
Citation: Titaley CR, Tjandrarini DH, Malakauseya MLV, Ariawan I, Iwan RF, Istia SS and Dibley MJ (2025) Determinants of non-use of antenatal care services in eastern Indonesia: analysis of the 2023 Indonesia health survey. Front. Glob. Women's Health 6:1649276. doi: 10.3389/fgwh.2025.1649276
Received: 27 June 2025; Accepted: 31 July 2025;
Published: 18 August 2025.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Ni Ketut Aryastami, The National Research and Innovation Agency, IndonesiaUntoro Dwi Raharjo, Universitas Jenderal Achmad Yani Yogyakarta, Indonesia
Copyright: © 2025 Titaley, Tjandrarini, Malakauseya, Ariawan, Iwan, Istia and Dibley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christiana Rialine Titaley, Y2hyaXN0aWFuYV9yaWFsaW5lQHlhaG9vLmNvbQ==
 Christiana Rialine Titaley
Christiana Rialine Titaley Dwi Hapsari Tjandrarini
Dwi Hapsari Tjandrarini Maxwell Landri Vers Malakauseya3
Maxwell Landri Vers Malakauseya3 Iwan Ariawan
Iwan Ariawan Ressita Fannia Iwan
Ressita Fannia Iwan Michael J. Dibley
Michael J. Dibley