- 1Department of Clinical Sciences (Malmö), Lund University, Lund, Sweden
- 2Nutrition and Health Science, Laney Graduate School, Emory University, Atlanta, GA, United States
- 3Adult Psychiatry, Directorate General of Health, Dhaka, Bangladesh
Introduction: Depression and anxiety are leading contributors to the global burden of disease among women yet help-seeking for mental health concerns remains limited in lower-middle-income countries. This study aimed to estimate the prevalence of anxiety, depression, and help-seeking behaviors, and to identify factors associated with the absence of help-seeking among ever-married women of reproductive age in Bangladesh.
Methods: We conducted a cross-sectional analysis using nationally representative data from the 2022 Bangladesh Demographic and Health Survey. Mental health outcomes were assessed using the Generalized Anxiety Disorder-7 and Patient Health Questionnaire-9 screening tools. Help-seeking behavior was defined as any attempt to obtain external support for mental health concerns. Multivariable logistic regression models, accounting for survey design and sampling weights, were used to examine predictors of not seeking help following Behavioral Model of Health Services Use by Andersen and Davidson.
Results: Among 19,987 women aged 15–49 years, 5.1% reported depression, 19.7% reported anxiety, and 20.4% had either condition. Only 20.5% of those with anxiety or depression reported help-seeking, predominantly from informal sources such as family and neighbors. Rural residence, older age, and a professional diagnosis of anxiety were associated with increased help-seeking, while low health autonomy and residence in the Barishal division were linked to lower help-seeking. Formal help-seeking was rare, and significant regional disparities were observed. One in five ever-married women of reproductive age in Bangladesh experiences anxiety or depression, but help-seeking remains low, especially for formal services.
Discussion: Informal networks play a critical role in support. Interventions should address contextual and individual barriers, strengthen social support, and improve access to mental health care, particularly in underserved regions.
1 Introduction
Mental health is foundational to overall well-being, enabling individuals to cope with life's stresses, realize their potential, and contribute to their communities. The etiology of mental disorders is complex, influenced by structural, individual, and community-level factors (1). Despite its importance, mental health remains an often neglected component of global health policy and systems, even though research consistently shows strong connections between mental and physical health. Depression and anxiety—the most prevalent mental disorders—are associated with increased risk for chronic diseases, functional impairment, and all-cause mortality (2–7).
Globally, the burden of mental disorders is higher among women than men, a disparity attributed to biological, psychological, and sociocultural factors, including gender roles and life events such as menstruation, pregnancy, and menopause (5, 8–10). In 2021, the global prevalence of anxiety and depression among women aged 15–49 years was approximately 7% and 6%, respectively (8). Lower-middle-income countries (LMICs) are disproportionately affected, with an estimated 82% of all people living with mental disorders residing in LMICs (5, 11).
In Bangladesh, a South Asian LMIC, mental health challenges are pronounced. The National Mental Health Survey 2019 found that 18.7% of adults had at least one mental disorder, with a higher burden among women compared to men (9). Depressive (7.9%) and anxiety disorders (5.4%) are the most common (8, 9), and women in Bangladesh face additional risks due to higher rates of physical and sexual violence, as well as early marriage, which is associated with elevated depressive symptoms among adolescent and adult women (5, 10, 12–14). Despite these challenges, the treatment gap for mental health in Bangladesh is alarmingly high, with about 90% of adults with mental disorders not receiving appropriate care, mainly due to the predominance of depressive and anxiety disorders (9, 15). Access to formal mental health services is further limited by factors including availability, accessibility, and affordability (16–18). Next to formal help-seeking behavior, it is therefore essential to also understand informal help-seeking behavior within familial and friendship dynamics, its enablers and barriers. This distinction is needed to consider both forms of help-seeking in policy design for women's mental health.
In Bangladesh as in many other LMICs, research on mental health and help-seeking behavior especially among women is limited (19, 20). This poses the risk of creating policies and interventions based on assumption about magnitudes, associations and directionalities that differ to higher income contexts. While some studies have been conducted in the South Asia region (21–25), to our knowledge only two quantitative studies on help-seeking were conducted in Bangladesh, focusing on a rural district, and university students (26, 27). The country-representative National Mental Health Survey 2019 described treatment-seeking for mental health; however, they did not assess associations with sociodemographic factors. Help-seeking behavior was conceptualized differently across studies—as intentions, attitudes or reported past behaviors.
Therefore, understanding formal and informal help-seeking behavior and the predictors of help-seeking behavior among women in Bangladesh is critical to addressing the treatment gap and improving mental health outcomes. The Sustainable Development Goals explicitly address mental health, underscoring its relevance to broader public health and development objectives (3, 28). This study utilizes data from the Bangladesh Demographic and Health Survey (BDHS) 2022 to assess the prevalence of anxiety, depression, and help-seeking behaviors among ever-married women of reproductive age (15–49 years), and to identify factors associated with the absence of help-seeking for mental health problems in this population.
2 Materials and methods
2.1 Data source
The study utilized secondary data from the BDHS 2022, a survey that is nationally representative. The survey employed a two-stage stratified sampling technique to guarantee the representation of the whole population residing in non-institutional households across Bangladesh. The initial phase entailed the selection of 675 enumeration units (clusters) using a probability proportional to size sampling method, succeeded by a comprehensive household listing inside each chosen unit. In the second phase, 45 households from each enumeration area were selected (n = 30,330) and ever-married women aged 15 to 49 were interviewed (19,987, response rate: 98.9%). Ever-married women were those women currently married or married previously, but widowed, divorced or separated at the time of data collection. See Figure 1 for further information on the sample selection. The analytical sample was restricted to the sub-sample of ever-married women aged 15 to 49 years who were screened for anxiety and depression. More information on sampling can be obtained from the official survey report (29).
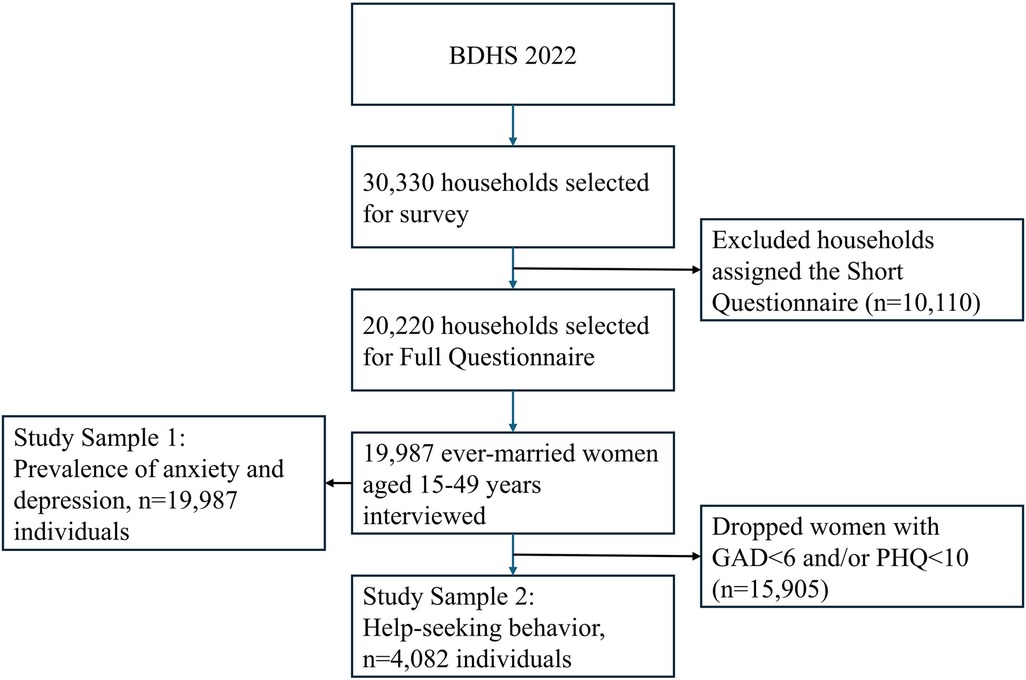
Figure 1. Flow chart presenting the sample selection for the analysis of prevalences of anxiety and depression, and help-seeking behavior using BDHS 2022 data. BHDS, Bangladesh Demographic and health survey; GAD, generalized anxiety Disorder-7; PHQ, patient health questionnaire-9.
2.2 Conceptual model
The study was guided by the Behavioral Model of Health Services Use by Andersen and Davidson (30), which conceptualizes healthcare access as influenced by both individual and contextual factors (Figure 2). These are categorized into predisposing (demographics, social structure, health beliefs), enabling (resources, policies, organizational factors), and need (perceived or evaluated need for care) components. Predisposing and need factors are generally less mutable, whereas enabling factors are more amenable to policy intervention. Based on this framework and prior research, relevant variables from the BDHS 2022 were selected for analysis.
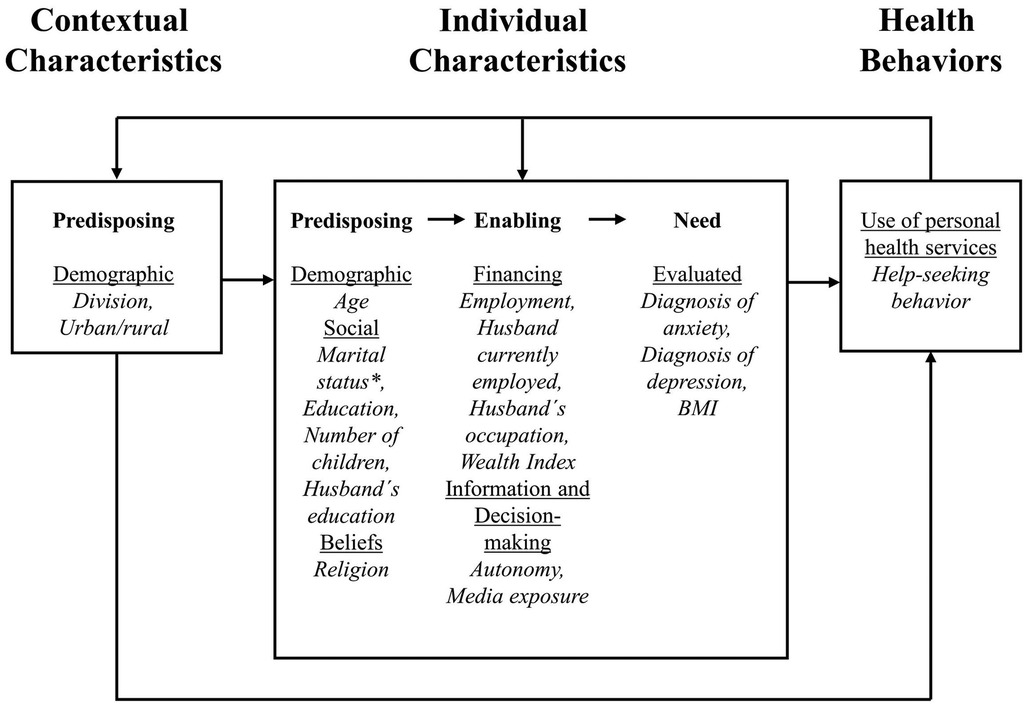
Figure 2. Behavioral model of health services use (30) adapted to seeking help for anxiety and/or depression.
2.3 Variables
2.3.1 Outcome variables
This study examined four outcome variables: anxiety, depression, any anxiety or depression, and help-seeking behavior. For the mental health outcomes of anxiety and depression, cut-offs were selected based on the reviewed literature (22, 23). This increased interpretability of results but did not allow to look at the full spectrum of mental health and may yield different results than clinical diagnoses.
Anxiety was measured using the Generalized Anxiety Disorder-7 (GAD-7) scale (31), a 7-item questionnaire assessing symptoms over the past two weeks, scored from 0 (never) to 3 (always). Scores were classified as mild (0–5), moderate (6–14), and severe (15–49), with a score of 6 or higher indicating anxiety (binary: yes/no).
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) (32), comprising nine items scored 0–3 over the past two weeks. Severity was categorized as minimal/no symptoms (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27). A score of 10 or higher indicated depression (binary: yes/no).
Any anxiety or depression was defined as the presence of either anxiety or depression, or both, vs. neither.
Help-seeking behavior was defined as the attempt to obtain external assistance for mental health concerns. In this study, help-seeking behavior was assessed by self-report of past help-seeking (yes/no). While this simplification was necessary for appropriate analyses and interpretation, the findings do not account for the number of help sources, time spent seeking or receiving help, and success of the help-seeking practice. The sources of help were categorized: formal (doctor/medical personnel, social service organization, social worker, community health worker/fieldworker, NGO) and informal (religious leader, spouse/partner, family member, friend, neighbor).
2.3.2 Independent variables
Variables were classified according to the Andersen model (30) (Figure 2). For contextual predisposing factors, place of residence and division were included. Place of residence was a binary variable (urban, rural), while the variable division was categorized according to the eight administrative divisions in Bangladesh: Barishal, Chattogram, Dhaka, Khulna, Mymensingh, Rajshahi, Rangpur and Sylhet.
Individual characteristics were grouped according to predisposing, enabling and need factors as portrayed by the Andersen model. Predisposing factors were age (15–24, 25–34, 35–49 years), marital status (currently married, widowed/divorced/separated), number of children (none, 1–2, ≥3), woman's and husband's highest education level (no education, primary, secondary, higher), and religion (Islam, others). Education was treated as a predisposing factor due to its low mutability.
Enabling factors were current employment (yes/no), Wealth Index (poorest, poorer, middle, richer, richest), husband's employment status (worked last 7 days: yes/no), husband's occupation (non-manual/manual), women's autonomy in health decisions (respondent alone, joint, husband/other), and media exposure (yes/no). In the BDHS, wealth quintiles were calculated with principal component analysis that each comprises 20% of the population and consider owned consumer goods and housing characteristics. Husband's occupation was categorized as non-manual (not working, professional/technical/managerial, clerical, sales) or manual (agricultural, household/domestic, services, skilled/unskilled manual), following previous BDHS research. Media exposure included radio, newspaper, magazine, internet, or TV (any vs. none).
Need factors were body mass index (BMI) and prior diagnoses of anxiety or depression. BMI was dichotomized using the World Health Organization's (WHO's) Asian criteria: normal (18.5–22.9) and underweight/overweight/obese (<18.5 or >22.9) (33). Diagnoses were based on prior professional assessment by healthcare providers.
2.4 Statistical analysis
Descriptive statistics were presented as frequencies and percentages. Associations between independent and dependent variables were assessed using Pearson's chi-square tests. Bivariate relationships were examined with simple logistic regression, using absence of help-seeking as the reference. Multivariate logistic regression included all significant factors from bivariate analyses, reporting odds ratios (OR), adjusted odds ratios (aOR), 95% confidence intervals (CI), and p-values. Statistical significance was set at α < 0.05. The statistical software automatically excluded collinear variables from adjusted models adjusted models. Analyses were restricted to participants with anxiety (GAD-7 ≥ 6) and/or depression (PHQ-9 ≥ 10). Sensitivity analyses can be obtained in the Supplementary Material. We performed unadjusted and adjusted logistic regressions for the absence of informal help-seeking behavior among the subsample of women seeking only informal help to determine whether this largest source of help was consistent with our main analysis. Additionally, we tested for interaction of selected predictors (highest level of education and autonomy over health decisions) to assess whether associations differed by values of other variables (Supplementary Material). Data were analyzed using Stata/SE 18.0 accounted for sampling weights and survey design to ensure national representativeness (29).
2.5 Ethical considerations
The study utilized publicly available secondary data from the 2022 BDHS. Ethical approval was obtained from the ICF Institutional Review Board and the Bangladesh Medical Research Council (29). All data were anonymized and analyzed at the population level. Respondents with a PHQ-9 score ≥10 or any suicidal ideation were offered mental health services.
3 Results
3.1 Prevalence of anxiety, depression and any depression or anxiety
The sample consisted of 19,987 ever-married women aged 15 to 49 years. Within the sample, 5.1% (n = 1,026) were identified as experiencing depression. Anxiety was reported by 19.7% (n = 3,925) of the participants. The prevalence of either mental condition was 20.4% (n = 4,082) among the participating women.
3.2 Prevalence of help-seeking behavior and predictors of not seeking help
Among women with any anxiety or depression (n = 4,082), 20.5% (n = 836) reported help-seeking behavior. Chi-square analyses indicated that division, current employment, women's autonomy, media exposure, diagnosis of anxiety, and diagnosis of depression were significantly associated with the absence of help-seeking behavior, while no individual predisposing factors showed significant associations (Table 1). In the adjusted regression analysis, several contextual and individual factors were significant predictors of help-seeking (Table 2). A forest plot (Supplementary Figure S1, Supplementary Material) presents an overview of the adjusted regression analysis results. Contrary to common expectations, women residing in rural areas had significantly lower odds of not seeking help compared to those in urban areas (aOR: 0.68; 95% CI: 0.50–0.94). Compared to Barishal, all divisions except Sylhet had lower odds of absence of help-seeking, with Khulna showing the lowest odds (aOR: 0.42; 95% CI: 0.24–0.74). Older age was associated with increased help-seeking, as women aged 35–49 years had significantly lower odds of not seeking help than those aged 15–24 years (aOR: 0.63; 95% CI: 0.41–0.97). Regarding enabling factors, joint health decision-making with a husband was associated with 60% higher odds of not seeking help compared to independent decision-making by the woman (aOR: 1.60; 95% CI: 1.13–2.25). Finally, a professional diagnosis of anxiety was linked to a 67% reduction in the odds of not seeking help (aOR: 0.33; 95% CI: 0.21–0.51).
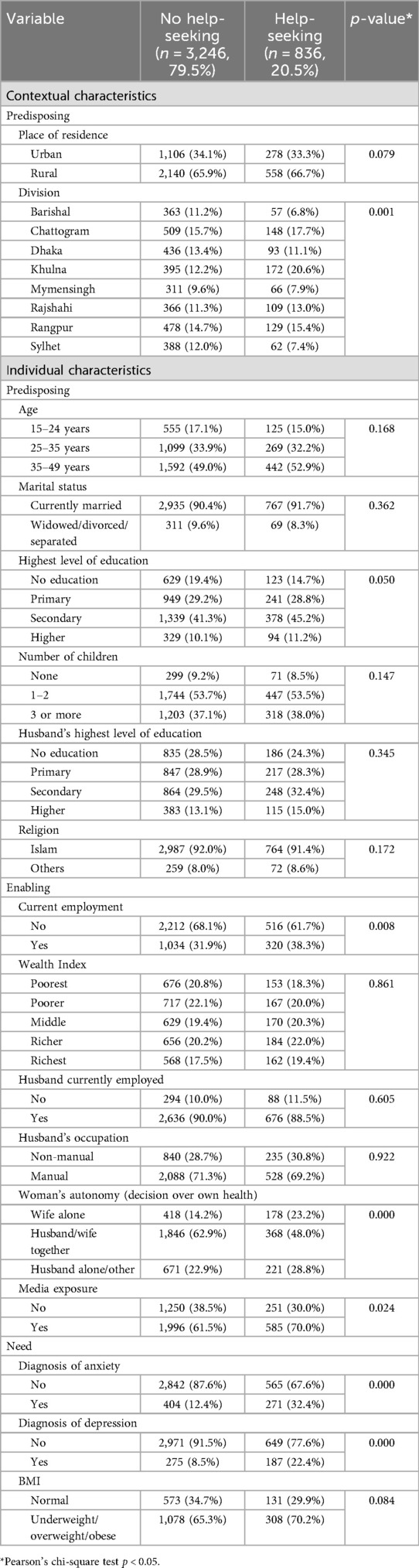
Table 1. Sociodemographic and health-related characteristics by help-seeking behavior among ever-married women aged 15–49 years in Bangladesh.
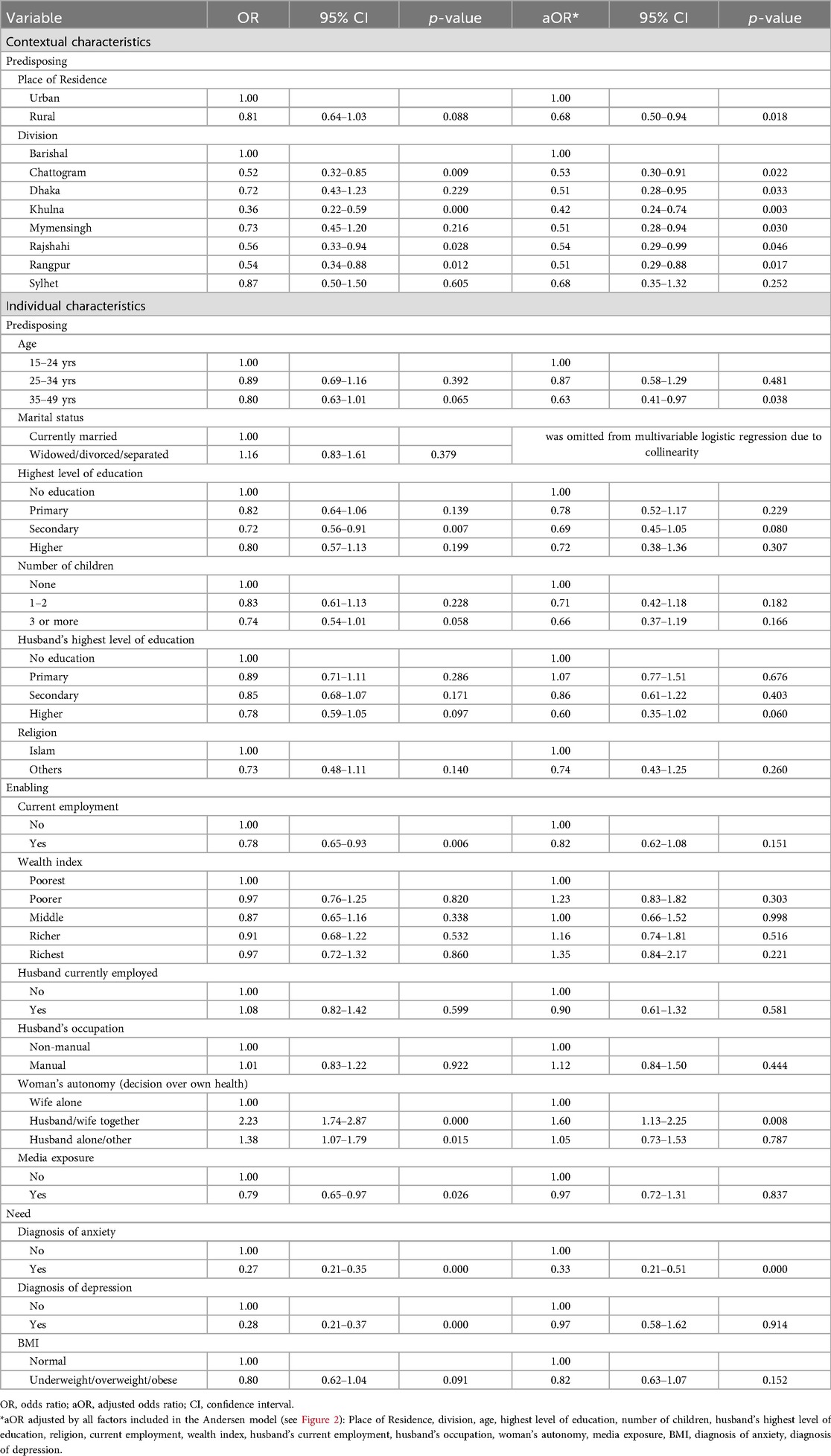
Table 2. Details of univariate and multivariate logistic regressions for the association of sociodemographic and health-related characteristics with the absence of help-seeking behavior among ever-married women aged 15–49 years in Bangladesh with any depression or anxiety.
3.3 Sources for help
Among women with any anxiety or depression who sought help, the majority (87.6%, n = 732) (Figures 3–5) relied on informal sources. Only 3.8% (n = 28) accessed both informal and formal help, and 22.8% of those who sought formal help also used informal sources. Doctors or medical care personnel were the most common formal source (14.0%, n = 117), with formal help-seeking more frequent among women with depression (23.4%) than those with anxiety (13.8%). Other formal sources, such as social service organizations, social workers, community health workers, fieldworkers, and NGOs, were rarely utilized (0.8%, n = 7).
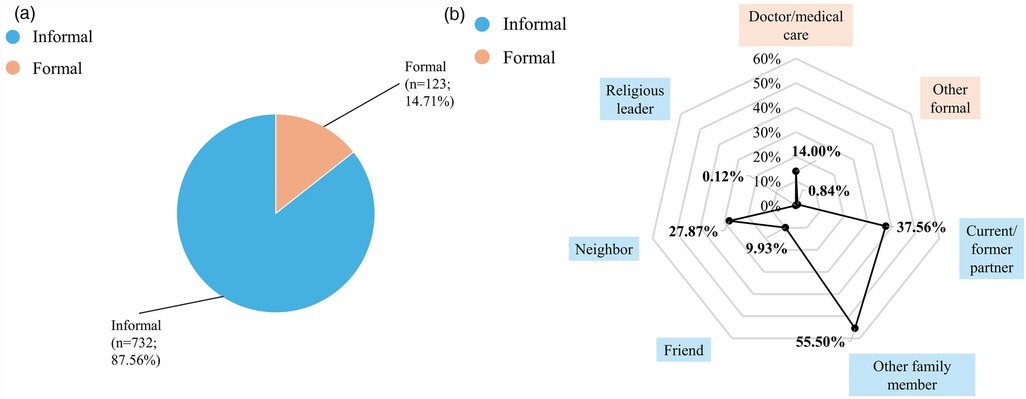
Figure 3. Help-Seeking with any anxiety or depression among ever-married women aged 15–49 years in Bangladesh (n = 836), BDHS 2022. The denominator for percentages entails everyone with any depression or anxiety seeking help. Because multiple sources of help could be selected by respondents, percentages add up to more than 100%. Other formal help-seeking sources include social service organizations, social workers, community health workers and NGOs. (a) Formal and informal help-seeking among ever-married women aged 15–49 years in Bangladesh with any anxiety or depression (n = 836), BDHS 2022. (b) Sources of help sought by ever-married women aged 15–49 years in Bangladesh with any anxiety or depression (n = 836), BDHS 2022.
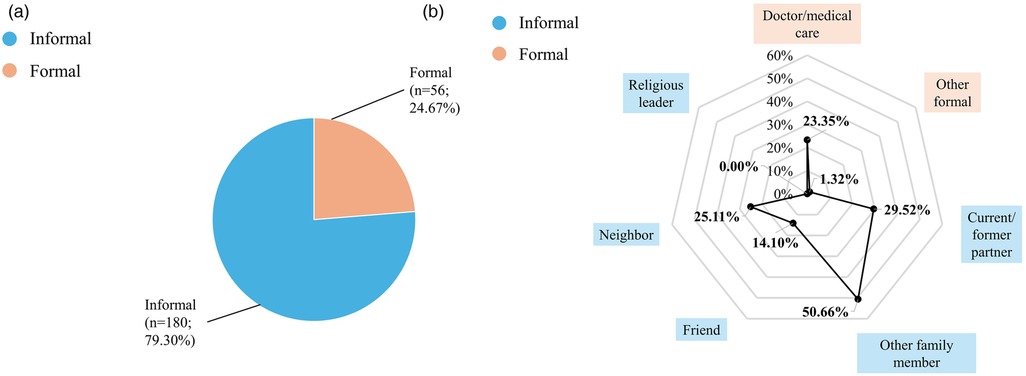
Figure 4. Help-Seeking with depression among ever-married women aged 15–49 years in Bangladesh (n = 227), BDHS 2022. The denominator for percentages entails everyone with anxiety seeking help. Because multiple sources of help could be selected by respondents, percentages add up to more than 100%. Other formal help-seeking sources include social service organizations, social workers, community health workers and NGOs. (a) Formal and informal help-seeking among ever-married women aged 15–49 years in Bangladesh with depression (n = 227), BHDS 2022. (b) Sources of help sought by ever-married women aged 15–49 years in Bangladesh with depression (n = 227), BDHS 2022.
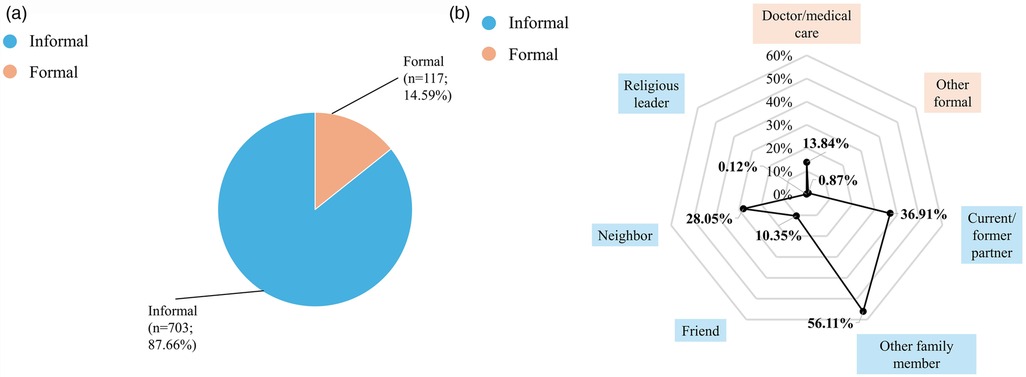
Figure 5. Help-Seeking with anxiety among ever-married women aged 15–49 years in Bangladesh (n = 802), BDHS 2022. The denominator for percentages entails everyone with depression seeking help. Because multiple sources of help could be selected by respondents, percentages add up to more than 100%. Other formal help-seeking sources include social service organizations, social workers, community health workers and NGOs. (a) Formal and informal help-seeking among ever-married women aged 15–49 years in Bangladesh anxiety (n = 802), BDHS 2022. (b) Sources of help sought by ever-married women aged 15–49 years in Bangladesh with anxiety (n = 802), BDHS 2022.
Family members other than a current or former husband/partner were the most frequent source of help overall (55.5%, n = 464) (Figures 3–5). Current or former husbands/partners (37.6%, n = 314) and neighbors (27.9%, n = 233) were also common sources, while friends (9.9%, n = 83) and religious leaders (0.1%, n = 1) were less frequently approached. No major differences in help-seeking sources were observed between women with anxiety and those with depression.
4 Discussion
4.1 Prevalence of anxiety, depression and any depression or anxiety
The prevalence of depression was lower than previously reported in the National Mental Health Survey 2019 for adult women in Bangladesh (7.9%) (9) and the Global Burden of Disease Study 2021 estimates for women aged 15–49 years (8.3%) (8). In contrast, the prevalence of anxiety disorders among our sample (19.6%) was substantially higher than the rates reported in these studies, which found 5.4% (9) for adult women and 5.5% for women aged 15–49 years (8). This discrepancy may be attributed to a stricter multi-stage case identification including diagnoses by trained research psychiatrists for the National Mental Health Survey or reliance on older source data from 1996, 1997 and 2000 in the Global Burden of Disease Study. Furthermore, the use of distinct assessment instruments and varying cutoff points complicates direct comparisons of prevalence rates across studies.
Notably, the overall prevalence of any depression or anxiety in our sample (20.4%) closely aligns with the National Mental Health Survey 2019 finding of 21.5% for mental disorders among women (9). However, that study utilized the Self Reporting Questionnaire to screen for 24 psychotic and non-psychotic mental disorders whereas we only included depression and anxiety. This highlights the heterogeneity in indicator measurement. Our results are consistent with data from a nationally representative survey in Nepal, which reported similar prevalence rates for depression (5.4%) and anxiety (21.9%) among women (34). These findings underscore the importance of methodological consistency and up-to-date data sources when interpreting mental health prevalence estimates across different contexts.
4.2 Help-seeking behavior
We found that help-seeking among women with depression or anxiety in Bangladesh was generally low, consistent with findings from other South Asian countries and LMICs (22, 23, 35). Compared to Nepal, help-seeking was approximately 10% lower in our sample, though differences in sample composition—such as the inclusion of never-married women and those with very mild symptoms in the Nepalese study—may account for some of this disparity (23).
The majority of women who sought help did so through informal channels, primarily family members, friends, and neighbors. This pattern aligns with previous research from Bangladesh and the broader South Asian context, which highlights the central role of families and local networks in providing support for mental health concerns (9, 23, 35–37). The WHO's Situational Assessment on Mental Health in Bangladesh also emphasized the strength of family networks as a resource for mental health support (15). Notably, women in rural areas were more likely to seek help than those in urban settings, a finding that contrasts with some earlier studies attributing higher urban help-seeking rates to better healthcare infrastructure (17). This may be explained by a greater reliance on informal support in rural areas (38), where higher physical proximity and stronger social cohesion facilitate access to help, especially for women engaged primarily in domestic work (36). Women in rural Bangladesh may have lower odds of not seeking help compared to urban women because rural communities often foster stronger social connectivity and support networks that promote interpersonal communications, frequently unrecognized as a kind of help-seeking behavior (39). Though family structures in Bangladesh are changing, women in rural Bangladesh usually still live in joint families which facilitates contact with family members and neighbors (40). Women living in urban areas are more likely to work outside the home which might reduce opportunities for social contacts.
Contrary to some reports, very few women sought help from religious leaders (9, 15), despite the significant role faith and traditional healers play in general health care in Bangladesh. Mental disorders in the country are often attributed to supernatural causes which may lead to a preference for spiritual healers rather than medical professionals (9, 17, 41). However, stigma surrounding mental health may discourage women from seeking help from these sources for mental health issues.
Formal help-seeking, particularly among women with anxiety, was much less common than informal help-seeking (9, 23), and when it occurred, it was mainly from medical professionals such as physicians. Barriers to formal help-seeking can be both person-centric—such as stigma, low health literacy, and cultural beliefs—and system-centric, including a lack of trained professionals, poor service quality, and limited resource distribution (42). These challenges contribute to persistent treatment gaps and low utilization of formal mental health services (9, 18, 36, 38).
Geographical disparities were evident, with women in Barishal division having significantly higher odds of not seeking help compared to other regions. Bangladesh is ranked one of the most climate vulnerable areas globally which affects women's mental health negatively (43, 44). Barishal division is among the most vulnerable regions to climate change in Bangladesh, especially due to its coastal location. Its unique geography exposes it to more frequent cyclones, tidal surges, flooding, salinity intrusion, and water logging compared to other divisions with potential consequences on healthcare accessibility and help-seeking rates (45). This finding is further exacerbated by potential higher levels of anxiety and depression in Barishal division, connected to climate change-related extreme weather events, in particular floodings, which were previously identified for adolescents (46). However, the overall low levels of formal help-seeking suggest that regional differences may also reflect variations in informal support networks or other contextual factors.
The conceptual model highlighted the importance of predisposing contextual elements in influencing help-seeking behavior. In analyzing environmental and systemic factors, it is essential to consider the present public health expenditure on mental health. Notwithstanding the reported high prevalence rates of two significant mental diseases and the Lancet Commission's recommendation to commit a minimum of 5% of health expenditures to mental health (3), in 2020, just approximately 0.05% of total public health expenditure in Bangladesh was dedicated to mental health (15). This highlights a significant disparity between high demand and constrained human, financial, and physical resources, particularly prevalent in LMICs (35). Mental health is currently excluded from social insurance plans, rendering it unaffordable for numerous Bangladeshi women (17, 38). The restricted funding for mental health may lead to low rates of formal help-seeking and significant disparities across divisions (47).
In the fully adjusted models, the only individual predisposing factor that significantly predicted lower odds of not seeking help was being beyond the age of 34. In Nepal, help-seeking was less prevalent among older age groups; however, no significant associations were tested (22), nor was any variation in help-seeking across age groups detected (34). Previous studies indicate that stigma, which hinders help-seeking, is more pronounced among older individuals (41). Mental disorders are being connected to magic and religion and people living with mental disorders are perceived as dangerous, having personal weaknesses, causing family shame and having failed spiritually/morally (41). Nevertheless, the global literature regarding the correlation between age and the propensity to seek mental health assistance remains inconclusive (48). Hypotheses supporting higher help-seeking among older age groups may be increased time availability due to older children, broader social networks among family, friends, and neighbors, or comorbidities that heighten the necessity for overall health assistance.
Low health autonomy was identified as a predictor of the absence of help-seeking behavior. Individuals who collaborate with their spouses in health decision-making or who are entirely uninvolved may encounter various obstacles when contemplating addressing stigmatized mental health issues (49). Jafree et al. (49) point out, that even educated and working women in Bangladesh live in a system, were making autonomous health decisions might make them “fear being shunned, stigmatized, and labeled a “rebel” for assuming health rights independently” (49, p. 56). This shows the interplay of different barriers to help-seeking such as autonomy, stigma and gender dynamics (41). Enhancing social support networks and fostering self-awareness may facilitate increased help-seeking behaviors for mental health issues (42).
Diagnoses of mental disorders can serve as both motivators for seeking assistance and outcomes of the help-seeking process. The bidirectional relationship necessitates careful interpretation of the strong association between a diagnosis of anxiety and help-seeking behavior. It underscores the significance of diagnoses in the process of seeking help for mental health issues. In Bangladesh, individuals must pursue formal medical assistance to obtain a diagnosis. Nonetheless, a limited percentage of individuals with mental health issues seek assistance from qualified professionals capable of making diagnoses (36). This is also associated with the limited availability of human resources. In 2021, the WHO estimated that Bangladesh had 0.16 psychiatrists, 0.4 specialized mental health nurses, and 0.34 psychologists per 100,000 people (15). The integration of mental health services into primary care and the provision of training in mental health care at this level may be significantly pertinent.
Overall, these findings underscore the need for interventions targeting both contextual and individual barriers to mental health care. Effective strategies should build on existing social support networks, reduce stigma, and increase awareness about mental health and available services among both the general population and healthcare providers. Structural changes, including increased financing and integration of mental health into community-level care, are essential, especially in underserved regions such as Barishal. Ensuring that health service structures can reach women in remote areas and address mental health needs is vital for reducing the treatment gap and improving outcomes for women across Bangladesh (50).
4.3 Strengths & limitations
This study utilized cross-sectional data, precluding causal inferences between exposures and mental disorders or help-seeking behavior (51). Given the temporal relationship between mental health problems and help-seeking, there is a risk of sample selection bias. By including only women with current anxiety or depression, the study may have excluded those who previously experienced these conditions, sought help, and recovered, potentially underestimating the effectiveness of certain help sources.
The use of existing secondary data introduced further limitations. Symptom data were collected through interviewer-administered surveys, and stigma surrounding mental health may have led to underreporting, resulting in underestimated prevalence rates (16). Differences in cultural understanding and interpretation of mental health could also affect disclosure and complicate cross-country comparisons (5). Although the BDHS employed validated instruments (GAD-7 and PHQ-9), these tools are screening measures and do not substitute for clinical diagnosis; thus, reported cases should be considered probable rather than confirmed disorders.
Help-seeking behavior was assessed based on self-reported past actions and sources. The dataset did not include information on help-seeking intentions, types of assistance, number of help sources, or time frames, nor did it capture self-help behaviors—areas that warrant further investigation in future research (52, 53).
The variables analyzed were primarily individual-level factors, reflecting data availability. However, broader societal and political determinants such as stigma and mental health literacy also play a critical role in mental health and need to be explored to increase explanatory power of study results and to ultimately inform resource allocation and policy development (44). The selection of variables does not capture the full spectrum of predictors for help-seeking but highlights key factors and groups requiring attention. Comorbidities such as thyroid disease, diabetes and hypertension were excluded due to limited data and lack of statistical significance, as their inclusion would have substantially reduced the analytic sample.
This study is aimed to observe Bangladeshi women's mental-health help seeking behavior using BDHS 2022 survey data, but that survey only considered depression and anxiety, ignoring other common mental-health issues like psychosis, obsessive compulsive disorder, bipolar disorder, post-partum blue, stress disorders, somatic symptom disorders etc. This may limit the overall picture of mental-health help-seeking behavior of Bangladeshi women.
Despite these limitations, the study achieved its objectives, providing new insights into the prevalence of anxiety and depression, as well as help-seeking behavior among ever-married women of reproductive age in Bangladesh. The use of reliable, nationally representative data and validated instruments supports the robustness of the findings. While results may be generalizable to similar populations in South Asia, contextual factors—including physical, social, and political environments—should be considered. The conceptual model employed underscored the importance of both contextual and individual determinants of anxiety, depression, and help-seeking behavior.
5 Conclusion
This study indicated that approximately 20% of women in Bangladesh experienced depression or anxiety. The likelihood of not seeking help was greatest among women lacking a formal anxiety diagnosis, those residing in the Barishal division, and younger women. Approximately 20% of women experiencing anxiety or depression pursued assistance for their mental health. Informal sources of assistance, such as family and neighbors, were more prevalent than formal support systems. To elucidate these differences and formulate policies and interventions aimed at enhancing mental health in Bangladesh at both structural and societal levels, it is essential to consider additional socio-cultural factors.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.dhsprogram.com/Countries/Country-Main.cfm?ctry_id=1&;c=Bangladesh&;Country=Bangladesh&;cn=&;r=4.
Ethics statement
The studies involving human participants were reviewed and approved by ICF Institutional Review Board ethics committee, and Bangladesh Medical Research Council. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in the primary study.
Author contributions
HW: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. MC: Methodology, Validation, Visualization, Writing – review & editing. MA: Conceptualization, Data curation, Writing – review & editing. SF: Conceptualization, Validation, Writing – review & editing. SS: Conceptualization, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We gratefully acknowledge the Demographic and Health Survey (DHS) Program for providing access to the publicly available data used in this study. This article includes parts of the first author’s master’s thesis titled “Predictors of anxiety, depression and help-seeking behavior among women in Bangladesh: An analysis based on the “Bangladesh Demographic and Health Survey” 2022”, submitted to Lund University in 2025. The thesis is not publicly accessible online but can be obtained upon request.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1679141/full#supplementary-material
References
1. World Health Organization. Mental health (n.d.). Available online at: https://www.who.int/health-topics/mental-health#tab=tab_1 (Accessed April 14, 2025).
2. Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. (2015) 28(11):1295–302. doi: 10.1093/ajh/hpv047
3. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The lancet commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
4. Rajan S, McKee M, Rangarajan S, Bangdiwala S, Rosengren A, Gupta R, et al. Association of symptoms of depression with cardiovascular disease and mortality in low-, middle-, and high-income countries. JAMA Psychiatry. (2020) 77(10):1052–63. doi: 10.1001/jamapsychiatry.2020.1351
5. World Health Organization. World Mental Health Report. Geneva: World Health Organization (2022). Available online at: https://iris.who.int/bitstream/handle/10665/356119/9789240049338-eng.pdf?sequence=1 (Accessed April 17, 2025).
6. Huang H, Meng F, Qi Y, Yan X, Qi J, Wu Y, et al. Association of hypertension and depression with mortality: an exploratory study with interaction and mediation models. BMC Public Health. (2024) 24:1068. doi: 10.1186/s12889-024-18548-0
7. World Health Organization. Depression (n.d.). Available online at: https://www.who.int/health-topics/depression#tab=tab_2 (Accessed April 14, 2025).
8. Institute for Health Metrics and Evaluation. GBD Results. Washington: University of Washington (2021). Available online at: https://vizhub.healthdata.org/gbd-results/ (Accessed April 14, 2025).
9. Alam F. National Mental Health Survey 2019. Dhaka: National Institute of Mental Health (2021). Available online at: https://nimh.gov.bd/wp-content/uploads/2021/11/Mental-Health-Survey-Report.pdf (Accessed February, 20 2025).
10. Government of the People’s Republic of Bangladesh. National Mental Health Strategic Plan 2020–2030. Dhaka: Government of the People’s Republic of Bangladesh (2022). Available online at: https://dghs.gov.bd/sites/default/files/files/dghs.portal.gov.bd/notices/e27171cb_a80b_42d4_99ad_40095adef31b/2022-08-16-08-42-af8622e2c4936593dd45601b84f4920f.pdf (Accessed April 11, 2025).
11. Hossain MD, Ahmed HU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry. (2014) 14:216. doi: 10.1186/s12888-014-0216-9
12. Rozario LG, Islam S. Scenario of mental health in Bangladesh: a signature glimpse. Dhaka Univ J Biol Sci. (2022) 30(3):405–16. doi: 10.3329/dujbs.v30i3.59033
13. Khan R, Akter F, Rahman M, Amin N, Rahman M, Winch PJ. Socio-demographic factors associated with mental health disorders among rural women in Mymensingh, Bangladesh. Front Psychiatry. (2025) 16:1446473. doi: 10.3389/fpsyt.2025.1446473
14. UNICEF. Ending Child Marriage: A Profile of Progress in Bangladesh. New York: UNICEF (2020). Available online at: https://www.unicef.org/bangladesh/media/4526/file/Bangladesh%20Child%20Marriage%20report%202020.pdf.pdf (Accessed April 24, 2025).
15. World Health Organization. Bangladesh—WHO Special Initiative for Mental Health: Situational Assessment. Geneva: World Health Organization (2021). Available online at: https://cdn.who.int/media/docs/default-source/mental-health/special-initiative/who-special-initiative-country-report—bangladesh—2020_f746e0ca-8099-4d00-b126-fa338a06ca6e.pdf?sfvrsn=c2122a0e_7 (Accessed March 25, 2025).
16. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. (2019) 21(2):10. doi: 10.1007/s11920-019-0997-0
17. Hasan MT, Anwar T, Christopher E, Hossain S, Hossain MM, Koly KN, et al. The current state of mental healthcare in Bangladesh: part 1—an updated country profile. BJPsych Int. (2021) 18(4):78–82. doi: 10.1192/bji.2021.41
18. Rahman MA, Babaye Y, Bhat A, Collins PY, Kemp CG. Availability of two essential medicines for mental health in Bangladesh, the Democratic Republic of Congo, Haiti, Nepal, Malawi, Senegal, and Tanzania: evidence from nationally representative samples of 7958 health facilities. J Glob Health. (2022) 12:04063. doi: 10.7189/jogh.12.04063
19. Maselko J. Social epidemiology and global mental health: expanding the evidence from high-income to low- and middle-income countries. Curr Epidemiol Rep. (2017) 4(2):166–73. doi: 10.1007/s40471-017-0107-y
20. Roberts T, Miguel Esponda G, Krupchanka D, Shidhaye R, Patel V, Rathod S. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry. (2018) 18:262. doi: 10.1186/s12888-018-1837-1
21. Sajjad A, Shah S, Abbas G, Aslam A, Randhawa F, Khurram H, et al. Treatment gap and barriers to access mental healthcare among women with postpartum depression symptoms in Pakistan. PeerJ. (2024) 12:e17711. doi: 10.7717/peerj.17711
22. Shawon MSR, Hossain FB, Ahmed R, Poly IJ, Hasan M, Rahman MR. Role of women empowerment on mental health problems and care-seeking behavior among married women in Nepal: secondary analysis of nationally representative data. Arch Womens Ment Health. (2024) 27(4):527–36. doi: 10.1007/s00737-024-01433-5
23. Pandey AR, Adhikari B, Bista B, Lamichhane B, Joshi D, KC S, et al. Prevalence, determinants and care-seeking behaviour for anxiety and depression in Nepalese population: a secondary analysis of data from Nepal Demographic and health survey 2022. BMJ Open. (2024) 14(8):e078582. doi: 10.1136/bmjopen-2023-078582
24. Aryal R, Rajbanshi M, Pokhrel S, Regmi S, Mali P, Baskota S. Help-seeking behaviour towards anxiety among undergraduate students of Nepal: a web-based cross-sectional study. Ann Med Surg. (2024) 86:146–52. doi: 10.1097/MS9.0000000000001568
25. Shidhaye R, Lyngdoh T, Murhar V, Samudre S, Krafft T. Predictors, help-seeking behaviour and treatment coverage for depression in adults in Sehore district, India. BJPsych Open. (2017) 3(5):212–22. doi: 10.1192/bjpo.bp.116.004648
26. Uddin MN, Bhar S, Islam FMA. An assessment of awareness of mental health conditions and its association with socio-demographic characteristics: a cross-sectional study in a rural district in Bangladesh. BMC Health Serv Res. (2019) 19(1):562. doi: 10.1186/s12913-019-4385-6
27. World Health Organization Regional Office for Europe. Mental Health. Fact Sheet on Sustainable Development Goals (SDGs): Health Targets. Mental Health. Copenhagen: World Health Organization Regional Office for Europe (2018). Available online at: https://iris.who.int/bitstream/handle/10665/340847/WHO-EURO-2018-2364-42119-58012-eng.pdf?sequence=1 (Accessed April 03, 2025).
28. Sifat MS, Tasnim N, Hoque N, Saperstein S, Shin RQ, Feldman R, et al. Motivations and barriers for clinical mental health help-seeking in Bangladeshi university students: a cross-sectional study. Glob Ment Health. (2022) 9:211–20. doi: 10.1017/gmh.2022.24
29. National Institute of Population Research and Training (NIPORT) and ICF. Bangladesh Demographic and Health Survey 2022: Final Report. Dhaka and Rockville, MD: NIPORT and ICF (2024). Available online at: https://www.dhsprogram.com/pubs/pdf/FR386/FR386.pdf (Accessed February 05, 2025).
30. Andersen RM, Davidson PL. Improving access to care in America. Individual and contextual indicators. In: Andersen RM, Rice TH, Kominski GF, editors. Changing the US Health Care System: Key Issues in Health Services Policy and Management. 3rd ed. San Francisco, CA: Jossey Bass/John Wiley & Sons, Inc (2007). p. 3–31.
31. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166(10):1092–7. doi: 10.1001/archinte.166.10.1092
32. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
33. World Health Organization Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3
34. Shawon MSR, Hossain FB, Hasan M, Rahman MR. Gender differences in the prevalence of anxiety and depression and care seeking for mental health problems in Nepal: analysis of nationally representative survey data. Glob Ment Health. (2024) 11:e46. doi: 10.1017/gmh.2024.37
35. Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low- and middle-income countries. Health Serv Insights. (2017) 10:1178632917694350. doi: 10.1177/1178632917694350
36. Nuri NN, Sarker M, Ahmed HU, Hossain MD, Beiersmann C, Jahn A. Pathways to care of patients with mental health problems in Bangladesh. Int J Ment Health Syst. (2018) 12:39. doi: 10.1186/s13033-018-0218-y
37. Dutta GK, Sarker BK, Ahmed HU, Bhattacharyya DS, Rahman MM, Majumder R, et al. Mental healthcare-seeking behavior during the perinatal period among women in rural Bangladesh. BMC Health Serv Res. (2022) 22(1):310. doi: 10.1186/s12913-022-07678-z
38. Ahmed SM, Alam BB, Anwar I, Begum T, Huque R, Khan JAM, et al. Bangladesh Health System Review. Geneva: World Health Organization (2015). Health systems in transition, 5(3). Available online at: https://iris.who.int/bitstream/handle/10665/208214/9789290617051_eng.pdf?sequence=1 (Accessed February 18, 2025).
39. Rahman H, Swahnberg K. Social Connectivity and Help Seeking Behavior among Abused Women in Rural Bangladesh: A Cross-Cultural Qualitative Study. Kalmar: Linnaeus University (2025). Available online at: https://urn.kb.se/resolve?urn=urn:nbn:se:lnu:diva-137886 (Accessed October 6, 2025).
40. Sultana A, Dey MR, Islam B. Changing family structure in rural Bangladesh: a sociological study in Chandpur District of Bangladesh. Asian J Soc Sci Leg Stud. (2024) 6(4):127–35. doi: 10.34104/ajssls.024.01270135
41. Faruk MO, Khan AH, Chowdhury KUA, Jahan S, Sarker DC, Colucci E, et al. Mental illness stigma in Bangladesh: findings from a cross-sectional survey. Glob Ment Health. (2023) 10:e59. doi: 10.1017/gmh.2023.56
42. Andary S, Bassani J, Burrell G, Cole E, Evans R, Redman E, et al. Barriers and enablers to access and utilization of mental health care services across Southeast Asia: a preliminary scoping review. Asia Pac Psychiatry. (2023) 15(4):e12549. doi: 10.1111/appy.12549
43. Planning Commission, Ministry of Planning, Asian Development Bank. Bangladesh Climate and Disaster Risk Atlas: Hazards—Volume I. Dhaka, Manila: Asian Development Bank (2021). Available online at: https://www.adb.org/sites/default/files/publication/760776/bangladesh-climate-disaster-risk-atlas-volume1-cover-pg29.pdf (Accessed April 25, 2025).
44. Alam F, Hossain R, Ahmed HU, Alam MT, Sarkar M, Halbreich U. Stressors and mental health in Bangladesh: current situation and future hopes. BJPsych Int. (2021) 18(4):91–4. doi: 10.1192/bji.2020.57
45. Huda FA, Mahmood HR, Hossain AT, Khan J, Faruk O, Razzak ZS, et al. Analysis of Health Needs and Health System Response in the Coastal Districts of Bangladesh. Dhaka: icddr,b (2020). Available online at: https://assets.publishing.service.gov.uk/media/5f34f2478fa8f5174ac78f24/icddrb_Final_Study_Report_23_July_2020_DFID.pdf (Accessed April 15, 2025).
46. Goldberg L, Luby S, Sayiara Shuchi N, Sen T, Hossen N, Wong-Parodi G, et al. Adolescent psychological health under chronic climate change-related stress: a mixed-methods cross-sectional study in Bangladesh. Lancet [Preprint]. (2024):36. Available online at: https://ssrn.com/abstract=5037271 (Accessed July 18, 2025).
47. Koly KN, Saba J, Rao M, Rasheed S, Reidpath DD, Armstrong S, et al. Stakeholder perspectives of mental healthcare services in Bangladesh, its challenges and opportunities: a qualitative study. Glob Ment Health. (2024) 11:e37. doi: 10.1017/gmh.2024.30
48. Magaard JL, Seeralan T, Schulz H, Brutt AL. Factors associated with help-seeking behaviour among individuals with major depression: a systematic review. PLoS One. (2017) 12(5):e0176730. doi: 10.1371/journal.pone.0176730
49. Jafree SR, Zakar R, Anwar S. Women's role in decision-making for health care in south Asia. In: Jafree SR, editor. The Sociology of South Asian Women’s Health. Cham: Springer Nature (2020). p. 55–78.
50. Sajib M, Hasan K, Hayder T, Hasan AMR, Rahman MM, Ether S, et al. Reaching the unreachable: a mixed-method evaluation of multidimensional healthcare model addressing the healthcare service gaps in hard-to-reach Northern riverine Bangladesh. Arch Public Health. (2025) 83(1):103. doi: 10.1186/s13690-025-01592-6
51. Aschengrau A, Seage GR. Essentials of Epidemiology in Public Health. 4th ed. Burlington, MA: Jones & Bartlett Learning (2020).
52. Rickwood D, Thomas K. Conceptual measurement framework for help-seeking for mental health problems. Psychol Res Behav Manag. (2012) 5:173–83. doi: 10.2147/PRBM.S38707
Keywords: Women's mental health, Bangladesh, anxiety, depression, help-seeking behavior, health autonomy, informal support, Demographic and Health Survey
Citation: Walter H, Craig ME, Ali M, Faruque S and Saha S (2025) Seeking support: insights into women’s mental health help-seeking behavior in Bangladesh. Front. Glob. Women's Health 6:1679141. doi: 10.3389/fgwh.2025.1679141
Received: 4 August 2025; Accepted: 17 October 2025;
Published: 5 November 2025.
Edited by:
Alina Haines-Delmont, Manchester Metropolitan University, United KingdomReviewed by:
Luca Pingani, University of Modena and Reggio Emilia, ItalyMamunur Rahman, East West University, Bangladesh
Copyright: © 2025 Walter, Craig, Ali, Faruque and Saha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hannah Walter, aGE2ODU1d2Etc0BzdHVkZW50Lmx1LnNl
 Hannah Walter
Hannah Walter Maggie E. Craig
Maggie E. Craig Masum Ali2
Masum Ali2 Sanjib Saha
Sanjib Saha