- 1Wissenschaftliches Institut der TK für Nutzen und Effizienz im Gesundheitswesen (WINEG), Hamburg, Germany
- 2Department of Psychology & Methods, Jacobs University Bremen, Bremen, Germany
Introduction
As stated by the Institute of Medicine: “It is widely believed that health IT, when designed, implemented, and used appropriately, can be a positive enabler to transform the way care is delivered. Designed and applied inappropriately, health IT can add an additional layer of complexity to the already complex delivery of health care, which can lead to unintended adverse consequences, for example dosing errors, failure to detect fatal illnesses, and delayed treatment due to poor human–computer interactions or loss of data” (Institute of Medicine, 2012). In fact, health information technologies (HIT) have the potential to increase the performance of delivered services, increase health care quality, save costs and involve patients as effective partners of their own health care. One recent example that aims at providing such a technology is EHDViz, a clinical dashboard development using open-source technology integrating high-frequency health and wellness data streams using interactive and real-time data visualization and analytics modalities (Badgeley et al., 2016). By providing such collaborative data visualizations, wellness trend predictions, risk estimation, proactive activity status monitoring, and knowledge of complex disease indicators, EHDViz proved to be an essential prototype of implementing data-driven precision medicine to improve the quality of affordable health care delivery (Badgeley et al., 2016).
However, thorough implementation and monitoring of HIT that have proven effective into regular health care delivery is a central concern of patient safety research. If not implemented and monitored correctly, HIT have the potential to pose a severe threat to the patient's health with a chance for lethal consequences due to implementation failure. Implementation failure is defined as failure to deliver a program as intended, which can result in failure to achieve the intended intervention effects or even adverse intervention effects (e.g., due to lack of acceptance) (Campbell et al., 2000; Rychetnik et al., 2002; Craig et al., 2008; Katz et al., 2013). Besides concrete harm for the patient due to implementation failure, additional risks are frustration and demoralization of staff as well as time loss which impede team performance in the delivery of care and, as a result, can also impact successful implementation (Ash et al., 2004; Harrison et al., 2007; Friedberg et al., 2014). Though studies predominantly report positive consequences on patient safety parameters when using HIT (e.g., reduction of adverse events), a few studies also report on negative consequences (e.g., increase in mortality due to adverse events) which could have been avoided with thorough implementation and monitoring resulting in lives saved (Han et al., 2005; Brenner et al., 2016).
Ongoing digital transformation in the health care system (e.g., machine learning, big data) further highlights the importance to incorporate HIT thoroughly into settings and routines. A recent publication by Shameer et al. (2017) highlighted the benefits of translational, integrative bioinformatics as a driver for data-driven precision medicine and wellness care, but also mention the need for a “… seamless integration of data from clinical evaluations and biomedical investigations with genomics and other physiological profiling to characterize an individual patient's disease progression. Implementing precision medicine practices in clinical settings requires coordinated efforts to integrate data from both healthy and disease states in individuals.” The authors propose the consolidated individualome data model which integrates environmental, person health related, and clinical data repositories and see electronic model records as a potential vehicle to centralize biomedical and health care data via real-time data streams (Shameer et al., 2017).
Health Information Technologies are Complex Interventions
However, implementing and monitoring HIT while also considering patient safety as a central aim of digital transformation in health care is often easier said than done. By nature, HIT follow the principle rules of complex interventions which have an impact on several parts of organizational and team structures ranging from IT infrastructures to the point of care. As change agents, HIT affect health care delivery in predictable (e.g., reorganization of processes) and unpredictable ways (e.g., interrupt care delivery) (Drummond et al., 2009).
They do so by covering several dimensions of complexity: (1) Number of and interactions between components; (2) Number and difficulty of behaviors required by those delivering or receiving the intervention; (3) Number of groups or organizational levels targeted by the intervention; (4) Number and variability of outcomes; (5) Degree of flexibility or tailoring of the intervention permitted (Rychetnik et al., 2002). Therefore, complex interventions not only call for thorough implementation, but also evaluation methods to display and understand if and how different parts of complex interventions work in different contexts, and how these parts might be improved to facilitate overall success of the implementation of HIT and their effectiveness. As a result, complex interventions may work best if tailored to local circumstances rather than being completely standardized. According to Craig et al. (2008) it is best practice to develop complex interventions systematically by using the best available evidence and theory, followed by a series of pilot studies to target key uncertainties in the design, an explorative and a definitive evaluation. The evaluations' results are to be disseminated as widely and persuasive as possible, with additional research to assist and monitor the process of implementation (Craig et al., 2008).
Implementing Complex Health Information Technologies in High Reliability Health Care Organizations
As health care organizations can be described as high reliability organizations (HRO) special emphasize needs to be put on the implementation of complex interventions to avoid implementation failure and potential harm to the patient. HROs in health care can be described by the following characteristics: (1) Preoccupation with failure; (2) Reluctance to simplify; (3) Sensitivity to operations; (4) Deference of expertise; (5) Commitment to resilience. According to the Agency for Healthcare Research and Quality, “the principles of high reliability go beyond standardization; high reliability is better described as a condition of persistent mindfulness within an organization. High reliability organizations cultivate resilience by relentlessly prioritizing safety over other performance pressures” (Agency for Healthcare Research and Quality, 2012).
To ensure quality and increase effectiveness of health care in HROs, implementation science provides the necessary repository of ideas and instruments to facility implementation and monitoring of HIT. Implementation science is defined as “the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services” (Eccles and Mittman, 2006). Therefore, increasing patient safety by improving quality and effectiveness of delivered health care go hand in hand with a major goal of implementation science. One of such instruments is the Consolidated Framework for Implementation Research (CFIR) as a pragmatic meta-theoretical framework (Damschroder et al., 2009). The CFIR represents the synthesis of 19 theories associated with implementation science to summarize potential barriers and facilitators of implementation, and to ensure consistent use of constructs across studies and support their comparability. These constructs are broadly subsumed under five domains: (1) Intervention characteristics; (2) Outer setting; (3) Inner setting; (4) Characteristics of individuals; (5) Process. These domains and their corresponding constructs (see Table 1) can complement the proposed key elements of the development and evaluation process of complex interventions by Craig et al. (2008) as displayed in the modified model for complex HIT interventions (see Figure 1) (Craig et al., 2008; Damschroder et al., 2009).
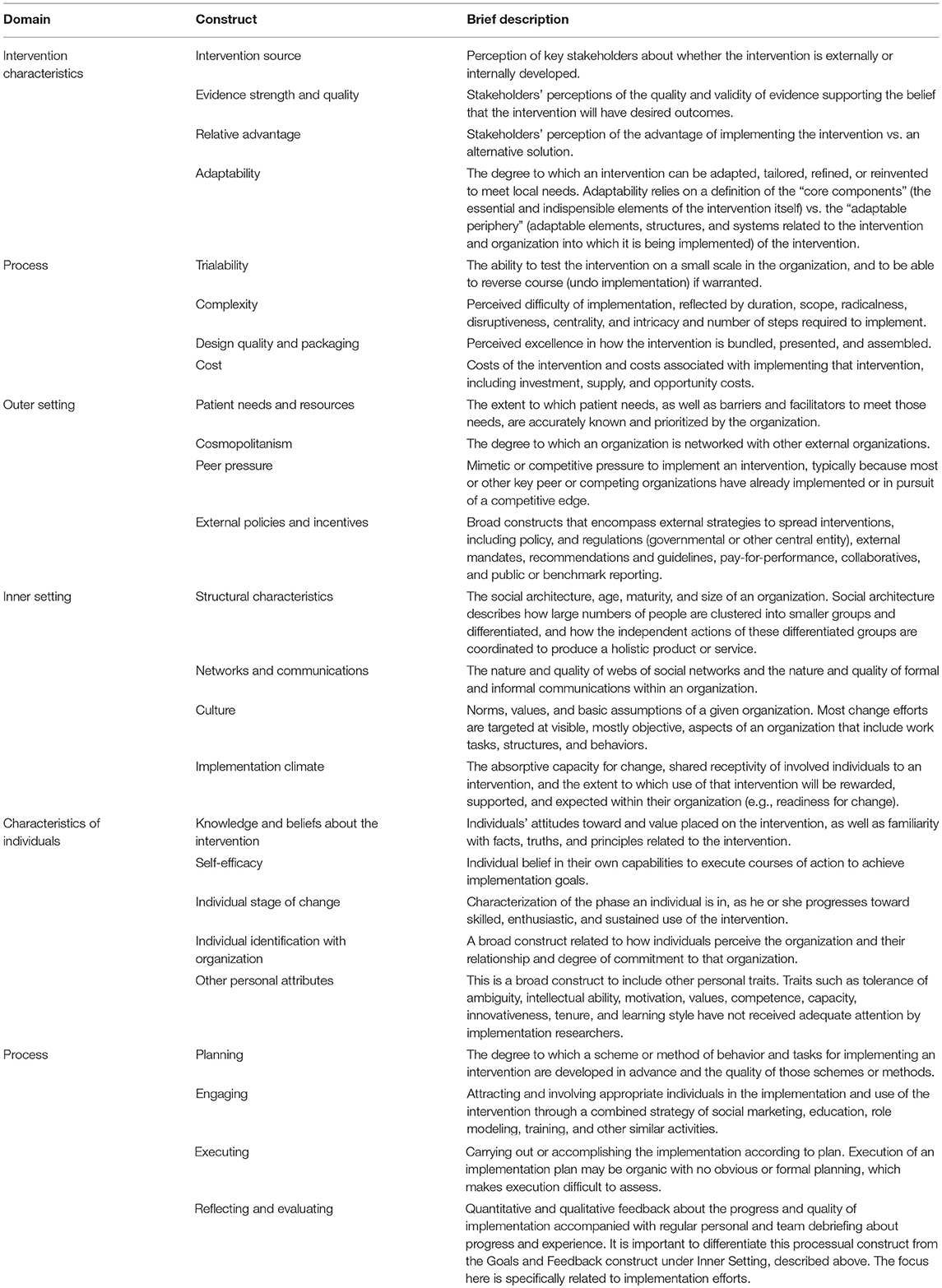
Table 1. Domains, constructs, and their brief descriptions as displayed in Damschroder et al. (2009).
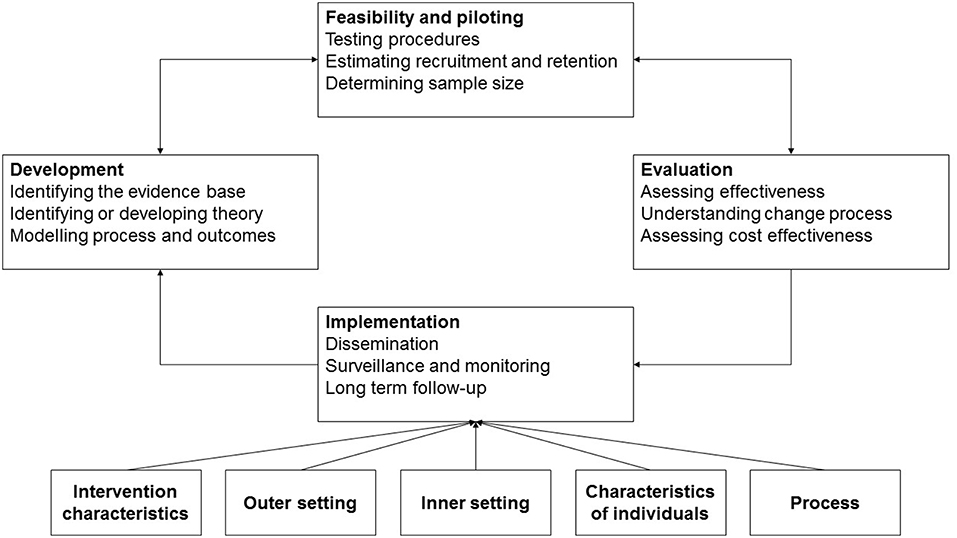
Figure 1. Key elements of the development and evaluation process of complex HIT interventions based on Craig et al. (2008) and Damschroder et al. (2009).
A Patient Safety Example for Implementation Failure of Complex Health Information Technologies
One particular example is a study by Han et al. (2005) which reported an unexpected increase in mortality after implementing a computerized physician order entry system (CPOE) in children who are transported for specialized care to an intensive care unit (ICU). Though implementing the CPOE had the opposite intent (i.e., to reduce mortality), the authors report that observed mortality nearly doubled, increasing from 2.80 to 6.57% (Han et al., 2005). In non-survivors, the CPOE was used more often (48.0 vs. 27.4%; P < 0.001) and was an independent predictor of mortality in the final logistic regression model (OR = 3.28; 95% CI 1.94–5.55; P < 0.001). The authors describe in detail the restructured processes after the CPOE was implemented, highlighting diverse problems such as delay of care due to a complex ordering process which can only start when the patient is fully registered, communication bandwidth problems using wireless communication due to increased overall traffic in the hospital computer system, dislocation of medical personal as one physician was now needed to place orders for the first 15 to 60 min if a patient arrived in extremis, and the removal of a satellite medication dispenser for critical medication from the ICU as all medication now had to be located at the central pharmacy. Furthermore, medical staff at the ICU were logged out when a pharmacist accessed the placed order for further processing, delaying additional order entries.
Though the displayed problems might not be exhaustive, they still underline the importance of thorough implementation of HIT as complex interventions. Referring to Figure 1, the authors reported on problems that emerged regarding intervention characteristics (e.g., external intervention source which was poorly adapted to the needs of the ICU and not tested on a small scale to identify potential problems, despite the potential to increase complexity of health care delivery in the ICU), the outer setting (i.e., not considering the patient needs for immediate care and treatment sufficiently), and process (poor planning of the implementation with no simulations or practice sessions for ICU staff or incremental implementation of parts of the intervention which might have provided important information at an early stage as well as a poor reflection and subsequent adaptation at an early stage of the implementation due to a lack of such “dry runs”). The majority of the reported problems might have transpired because the CPOE was externally developed, tested for feasibility and evaluated, and was not well-implemented in the ICU, resulting in an increase in mortality. An implementation failure happened that would have likely cost lives.
Conclusion
Though this current opinion piece can be seen as a first step in understanding HIT as complex interventions, the example highlights that it can help guide their development, implementation, and evaluation. Special emphasize needs to be placed on the successful implementation of HIT to ensure high quality of care and patient safety with the aim of avoiding potential harm to patients. The proposed blended model introduced in this opinion piece can help to identify potential elements for implementation failure or to understand the adverse effects of HIT interventions by drawing on key elements of complex interventions, with a special emphasize on the implementation by including the CFIR.
Future studies that attend to the field of patient safety and HIT should (a) be aware of the complex nature of HIT and consider this branch of research to enhance the understanding of working and non-working mechanisms in clinical settings by (b) drawing on insights from implementation science to avoid a failure of implementation with potential harm for patients. Additionally, relying on the CFIR and its' definition of domains and related constructs can also increase transparency regarding implementation effort and comparability with other studies.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Funding
The publication of this article was possible due to the Frontiers Waiver Program. The author would like to thank Frontiers for supporting this publication. No other funding can be reported.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Agency for Healthcare Research Quality (2017). High Reliability. Available online at: https://psnet.ahrq.gov/primers/primer/31/high-reliability (accessed July 19, 2018).
Ash, J. S., Berg, M., and Coiera, E. (2004). Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J. Am. Med. Inform. Assoc. 11, 104–112. doi: 10.1197/jamia.M1471
Badgeley, M. A., Shameer, K., Glicksberg, B. S., Tomlinson, M. S., Levin, M. A., McCormick, P. J., et al. (2016). EHDViz: clinical dashboard development using open-source technologies. BMJ Open 6:e010579. doi: 10.1136/bmjopen-2015-010579
Brenner, S. K., Kaushal, R., Grinspan, Z., Joyce, C., Kim, I., Allard, R. J., et al. (2016). Effects of health information technology on patient outcomes: a systematic review. J. Am. Med. Inform. Assoc. 23, 1016–1036. doi: 10.1093/jamia/ocv138
Campbell, M., Fritzpatrick, R., Haines, A., Kinmonth, A. L., Sandercock, P., Spiegelhalter, D., et al. (2000). Framework for design and evaluation of complex interventions to improve health. BMJ 321:694. doi: 10.1136/bmj.321.7262.694
Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., and Petticrew, M. (2008). Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. London: Medical Research Council. Available online at: https://mrc.ukri.org/documents/pdf/complex-interventions-guidance (accessed April 29, 2019).
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., and Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Imp. Sci. 4:50. doi: 10.1186/1748-5908-4-50
Drummond, W. H., Ferranti, J. M., Lehmann, C. U., and Lighter, D. E. (2009). “Complexity in healthcare information technology systems,” in Pediatric Informatics—Computer Applications in Child Health, eds C. U. Lehmann, G. R. Kim, and K. B. Johnson (New York, NY: Springer), 83–117. doi: 10.1007/978-0-387-76446-7_8
Eccles, M. P., and Mittman, B. S. (2006). Welcome to implementation science. Imp. Sci. 1:1. doi: 10.1186/1748-5908-1-1
Friedberg, M. W., Chen, P. G., Van Busum, K. R., Aunon, F., Pham, C., Caloyeras, J., et al. (2014). Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: RAND Corporation. Available online at: https://www.rand.org/content/dam/rand/pubs/research_reports/RR400/RR439/RAND_RR439.pdf (accessed April 29, 2019).
Han, Y. Y., Carcillo, J. A., Venkataraman, S. T., Clark, R. S., Watson, R. S., Nguyen, T. C., et al. (2005). Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 116, 1506–1512. doi: 10.1542/peds.2005-1287
Harrison, M. I., Koppel, R., and Bar-Lev, S. (2007). Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J. Am. Med. Inform. Assoc. 14, 542–549. doi: 10.1197/jamia.M2384
Institute of Medicine (2012). Health IT and Patient Safety. Building Safer Systems for Better Care. Washington, DC: National Academies Press.
Katz, J., Wandersman, A., Goodman, R. M., Griffin, S., Wilson, D. K., and Schillaci, M. (2013). Updating the FORECAST formative evaluation approach and some implications for ameliorating theory failure, implementation failure, and evaluation failure. Eval. Program. Plann. 39, 42–50. doi: 10.1016/j.evalprogplan.2013.03.001
Rychetnik, L., Frommer, M., Hawe, P., and Shiell, A. (2002). Criteria for evaluating evidence on public health interventions. J. Epidemiol. Commun. Health 56, 119–127. doi: 10.1136/jech.56.2.119
Keywords: patient safety, complex interventions, implementation failure, health information technology, health care
Citation: Wienert J (2019) Understanding Health Information Technologies as Complex Interventions With the Need for Thorough Implementation and Monitoring to Sustain Patient Safety. Front. ICT 6:9. doi: 10.3389/fict.2019.00009
Received: 05 September 2018; Accepted: 08 April 2019;
Published: 17 May 2019.
Edited by:
Sandra C. Buttigieg, University of Malta, MaltaReviewed by:
Shameer Khader, Northwell Health, United StatesDalia Kriksciuniene, Vilnius University, Lithuania
Copyright © 2019 Wienert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julian Wienert, ZHIuanVsaWFuLndpZW5lcnRAZ21haWwuY29t
 Julian Wienert
Julian Wienert