- 1Faculty of Medicine, Rural Clinical School, University of Queensland, Toowoomba, QLD, Australia
- 2Faculty of Medicine, Rural Clinical School, University of Queensland, Theodore, QLD, Australia
- 3Keele Medical School, Keele University, Keele, United Kingdom
- 4Ukwanda Center for Rural Health, Department of Global Health, Stellenbosch University, Cape Town, South Africa
- 5Medical Education and Human Resources Center, Faculty of Medicine, Menoufia University, Shibin el Kom, Egypt
- 6Family Medicine Practitioner, DOC24 Family Practice Clinic, Ghaziabad, India
- 7Ghana College of Physicians and Surgeons, Accra, Ghana
- 8Department of Family Medicine and Community Health, Duke University, Durham, NC, United States
- 9Planning and Quality Management Unit, Base Hospital, Panadura, Sri Lanka
- 10Center for Rural Health Studies, Memorial University of Newfoundland, St. John's, NL, Canada
- 11College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia
Background: There is an urgent need to scale up global action on rural workforce development. This World Health Organization-sponsored research aimed to develop a Rural Pathways Checklist. Its purpose was to guide the practical implementation of rural workforce training, development, and support strategies in low and middle-income countries (LMICs). It was intended for any LMICs, stakeholder, health worker, context, or health problem.
Method: Multi-methods involved: (1) focus group concept testing; (2) a policy analysis; (3) a scoping review of LMIC literature; (4) consultation with a global Expert Reference Group and; (5) field-testing over an 18-month period.
Results: The Checklist included eight actions for implementing rural pathways in LMICs: establishing community needs; policies and partners; exploring existing workers and scope; selecting health workers; education and training; working conditions for recruitment and retention; accreditation and recognition of workers; professional support/up-skilling and; monitoring and evaluation. For each action, a summary of LMICs-specific evidence and prompts was developed to stimulate reflection and learning. To support implementation, rural pathways exemplars from different WHO regions were also compiled. Field-testing showed the Checklist is fit for purpose to guide holistic planning and benchmarking of rural pathways, irrespective of LMICs, stakeholder, or health worker type.
Conclusion: The Rural Pathways Checklist provides an agreed global conceptual framework for the practical implementation of “grow your own” strategies in LMICs. It can be applied to scale-up activity for rural workforce training and development in LMICs, where health workers are most limited and health needs are greatest.
Introduction
Poor access to healthcare has major implications for the health and well-being of millions of people. Globally, countries with the highest proportion of rural residents correlate with poorest access. In countries where rural populations exceed 70%, only 16% of the population has access to universal health coverage (1). The most affected people are those in rural communities of LMICs (2). More than 90 per cent of people of low-income countries have no access to basic health care (3).
A critical issue for increasing universal health coverage is addressing the availability of a skilled rural health workforce (4, 5). The International Labor Organization (ILO) estimates that there is a current global shortfall of 10.3 million health workers needed to ensure provision of quality health services (3). Further, the World Health Organization (WHO) suggests that, based on increasing healthcare demand, ~18 million health workers are needed by 2030, mainly in LMIC (6).
To increase access to rural and remote health workers worldwide, the WHO released its evidence-based global recommendations of effective strategies in 2010 (7). These focus on four areas of intervention: rural education, regulatory, financial, and personal and professional support. Of these strategies, investing in “grow your own” educational approaches (selecting and training health workers in rural areas) are considered as a mainstay. They particularly play a role in achieving a skilled and satisfied rural workforce, over relying on regulatory strategies like obligatory rural service requirements (8–14). However, educational strategies are some of the most complicated to translate into practice because they involve multiple stakeholders and complex actions at different systems levels. Compared with financial or regulatory strategies which can be enacted through a change in central government policy or legislation, to be successful, rural educational strategies involve a holistic package of linked interventions that are managed over a longer-term cycle. Further, they rely on tailoring to different rural places, training systems, types of health workers, and health system infrastructure. This makes their implementation relatively complicated, particularly for LMICs where there are many competing healthcare priorities to address within restricted resources.
Effective translation of the WHO recommendations into practice is also challenging because there are no known practical tools which integrate the WHO “rural education” and “personal and professional support” strategies into a package for implementation. This is important as rural education, unless backed up with ongoing development and support, is likely to fail as a longer-term workforce development strategy. The availability of practical tools like Checklists, may help to integrate rural training and professional development and support actions, tailored to different LMICs and rural and remote settings.
Implementing training and development strategies in rural locations, apart from improving access to healthcare, has a significant role in addressing rural social and economic development. This approach rebalances the range of training and practice resources, skills, and jobs that are typically concentrated in cities, to be available in rural communities. The WHO High-Level Commission identifies the links between health and health sector jobs, in rural communities and social, economic, and health outcomes (15). The urgent need for more health workers in LMICs over the next 15 years presents a significant global challenge, but by addressing this challenge through fostering more rural-based health worker training and development interventions, it is possible also to generate economic growth where it is most needed (15). Developing more rural training and development also reinforces the United Nations' Sustainable Development Goals, by improving access to rural quality education and work, they reduce poverty, improve gender equality, build community partnerships, and promote health and well-being in rural places (16).
There is no globally agreed and LMIC-sensitive terminology that addresses the training, development, and support strategies needed to grow the rural workforce. Colloquially, the term “grown your own” and “rural training” only picks up on elements related to training. “Rural pipelines” is also often used, however, it purveys being stuck in a rigid structure “pipeline.” The term “rural pathways” has the potential to better reflect the choice of the trainee/worker to participate at each stage of their development and ongoing work, as a continuum of experience toward being skilled and supported for ongoing work in rural communities.
Our research aimed to confirm whether rural pathways terminology was appropriate, and describe what it entailed. Secondly, we aimed to design a Rural Pathways Checklist (Checklist) as a tool to guide the implementation of rural pathways in LMICs contexts. Finally, we intended to disseminate and test the application of the Checklist, assessing whether it addressed its purpose.
Methods
This project was sponsored by the WHO and had ethics approval from Monash University, Victoria, Australia (Project number 17636) ratified by the University of Queensland (Project number 2019002437). At project commencement, we engaged 13 experienced rural pathways implementers/rural health researchers from around the world, in a Steering Committee (October—December 2018). This group had experience of LMIC settings in different WHO regions and oversaw all aspects of project governance, quality, decision-making, and engagement. The Steering Committee, in consultation with the WHO, firstly agreed a clear vision, principles, and methods for the Checklist. These are outlined below.
Focus Groups
Two focus groups were held face-to-face with LMIC participants at the World Rural Health Conference (run by Rural WONCA—the Working Party on Rural Practice of the World Organization of Family Doctors) in 2018. These aimed to test LMIC concepts and terminology for “rural pathways,” “training,” “recruitment,” and “professional support.” Participants were trained primary healthcare workers and rural educators. They participated in open discussion with facilitators, where group comments were noted on a whiteboard, printed out and shared with the research team for analysis and informing the next stages of a policy and scoping review.
Policy Review
A desktop review of existing LMIC rural health workforce policies aimed to describe the progress and outcomes of rural focused policies and programs in LMIC settings, based on concepts and terminology from the focus groups. This was considered an important background for interpreting rural pathways strategies and describing the context of implementation. Articles or reports were accessed via key websites, sourced by the Steering Committee and Expert Reference Group or identified from published papers about LMIC human resource and rural pathways policies (by-products of the scoping which is described below).
Scoping Review
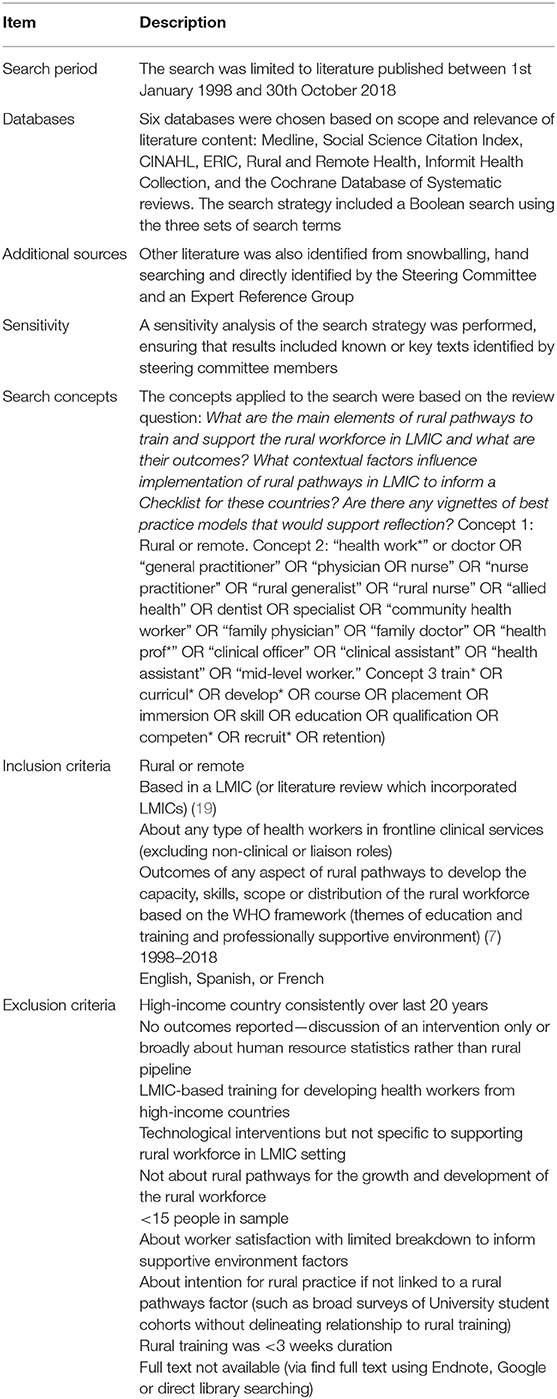
A scoping review was done using the five stage Arksey and O'Malley process (17, 18). The research question was to identify the extent, range and nature of LMIC rural pathways evidence and identify any exemplars. The search strategy and inclusion criteria (Table 1) were iteratively developed and informed by the LMICs concepts/terminology emerging from the focus groups, Steering Committee discussions and other global workforce reports (7, 20). In order to identify material and activity occurring in Latin-American and Francophone countries, English, French, and Spanish articles were included.
Consultation
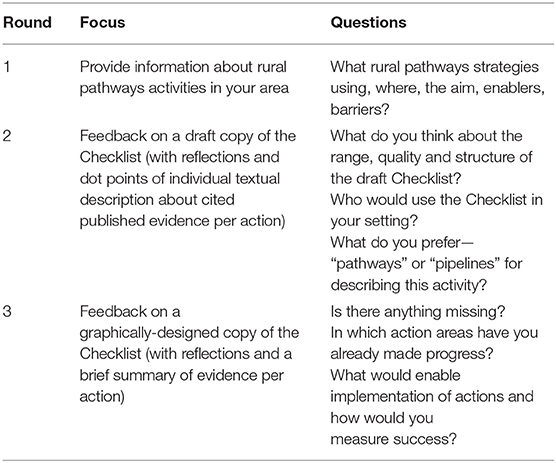
Consultation with an Expert Reference Group aimed to test and refine the Checklist with practical users, including stakeholders involved in rural workforce development in LMICs as well as personnel in high income countries (HICs) with knowledge of LMICs rural contexts and training systems. The Expert Reference Group included 70 rural pathways implementers who were part of the global rural health policy and practice community associated with Rural WONCA. Participants covered a range of health disciplines, countries and WHO regions, 42 (60%) were from LMICs. Consultation occurred over three stages, via tailored Qualtrics surveys sent by Email using Rural WONCA's regular Email list (covering all countries, rural stakeholders, and health worker types). The first round sought to gather general information about rural pathways activity for informing Checklist development. The 2nd and 3rd rounds sought feedback about the draft Checklist (Table 2).
Dissemination, Engagement, and Field-Testing
Dissemination, engagement, and field-testing of the Checklist occurred between January 2019 and February 2020. To aid distribution and access to the materials, a short version of the Checklist which was translated into 12 languages: Arabic, Bengali, Burmese, Chinese, French, Hindi, Indonesian, Portuguese, Russian, Spanish, Swahili, and Thai. The Checklist and translated materials were then provided on the Rural WONCA website and sent by email circulation to the global rural health policy and practice network associated with Rural WONCA and other experts these people identified. The materials were also provided to the Expert Reference Group. The Checklist was then presented at six international primary care conference workshops in 5 locations (Kyoto, Bratislava, Darwin, Uganda, Albuquerque), and at key workforce planning networks that the Steering Committee members were involved in.
The field-testing process followed and aimed to test whether the Checklist addressed its intended purpose, including being applicable to a range of LMICs countries and rural and remote contexts, health workers, stakeholders, and rural health problems, for its planned purpose of benchmarking and planning rural pathways implementation. To do this, interactive workshops were held, inclusive of a mix of stakeholders at conferences. Further, direct meetings were held with Expert Reference Group members from LMICs who nominated an interest in the Checklist and a willingness to test its application to their situation.
To aid data collection from meetings and workshops, a self-assessment tool, which was an adaptation of the Checklist, was applied to field-testing. This was developed by changing the reflective questions of the Checklist action areas into a series of 4–6 statements representing components of the action. A copy of this tool and the Checklist was provided to participants in advance of field-testing workshops or meetings.
For field-testing, the Checklist and its intended purpose was firstly explained. Then individuals were asked to consider a problem in their own rural community and the types of health workers they needed to support it. Following this, participants were asked to apply the self-assessment tool to rate their progress on actions for this issue (from 0 to 4 as “nil” to “strong”). The sum of progress scores on each item was then calculated giving participants an overall benchmark score of their progress in each Checklist action area. The process took ~40 min to complete and was followed by 20 min of discussion and reflection, whereby a facilitator recorded participant feedback. When the session concluded, the completed self-assessment tools were collected as data. In addition to this, participants were encouraged to take a copy of the Checklist and materials and apply them to real-world planning in their own communities and submit more detailed feedback via email.
Results
The agreed vision for the Checklist was to inform the implementation of all levels of action required for effectively training and supporting health workers in LMICs to improve the capacity, skills, scope, distribution, and retention of qualified rural generalist teams, adaptable for different rural, and remote communities. For impact, the focus was not just on the quantity of health workers, but also on their quality and relevance to the community (21).
The Checklist principles were also agreed: the Checklist would be informed by the literature about successful LMICs strategies; easy to use; based on universally understood terminology; able to promote reflection and learning; and applicable for planning tailored action for different LMICs, stakeholders, health workers, and community problems/contexts, at any stage of rural pathways development.
Focus Groups
From the focus groups, LMICs stakeholders identified that the term “rural pathways” covered broad strategies encompassing recruitment, education, training, professional support, and retention. In their context, bridging courses and step-wise qualifications were commonly used. Producing fit for purpose generalist teams of rural health workers was agreed to include people with certified skills. Trained or untrained health workers with only basic general qualifications were not considered to meet the criteria, nor support rural equity, or quality care.
Policy Review
Over 350 articles or reports were accessed in relation to LMIC policies. Substantial variation of rural workforce policy development was apparent for different LMICs and WHO regions. Few countries had strong national-scale rural health or rural workforce strategies. If they did, the strategic directions were often confined to one health worker type or targeted at a particular community health issue like maternal health (22, 23). The evidence of integrated rural pathways strategies was most developed in Thailand and the Philippines for medical doctors, including at University and early graduate levels (24–28). There were also examples of step-wise models included Community Health Worker training in Ethiopia (29, 30) and international partnerships to boost intelligence and resources for building rural pathways (31). However, there was limited evidence of holistic planning for training and supporting the range of skilled health workers needed by rural communities (32–34). This highlighted the potential value of a Checklist as a systems framework.
Scoping Review
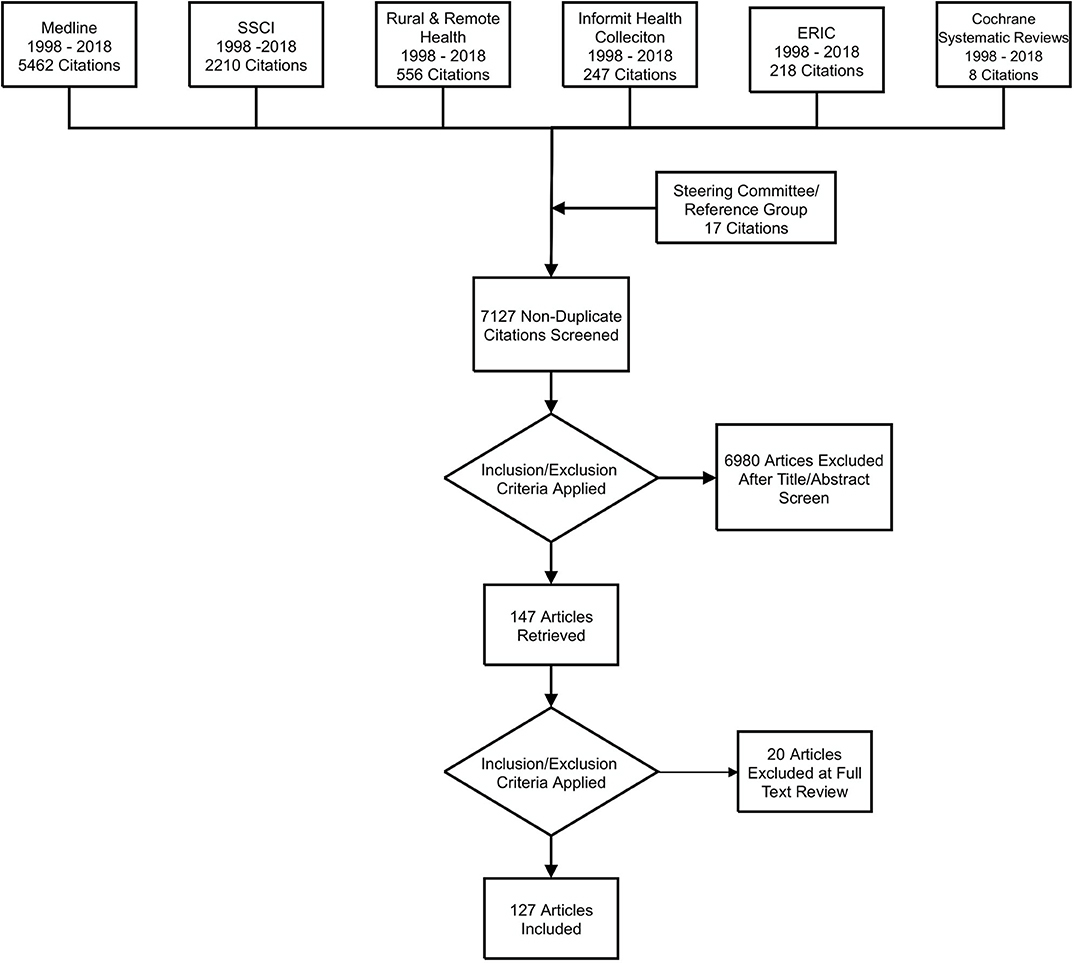
The scoping review identified 7,127 articles (Figure 1). After screening titles and abstracts, 97 empirical studies (83 from the literature search and 14 identified by the Steering Committee and Expert Reference Group) and 30 literature reviews (27 from the literature search and 3 from the Steering Committee) were included. After full text screening, data extraction was done using an Excel spreadsheet based on criteria that had been iteratively developed to ascertain material relevant to the scoping review question.
Most of the evidence was published since 2010. Empirical studies were from Africa (n = 45); Southeast Asia (25); Western Pacific (14); South or Central America (12), and Eastern Mediterranean regions (2) as formally defined WHO regions (35). Of the 97 empirical articles, 63 were about doctors/physicians; 28 were about other primary health care workers, mainly Community Health Workers, Health Extension Workers, Mid-Level Health Workers, Health Assistants, and Auxiliary Midwives. There were also two studies about other disciplines: Radiographers and Nutritionists/Physiotherapists/Speech Therapists/Occupational Therapists. Three other studies focused on Midwives, Nurse Practitioners, and Nurses, respectively. A single study concerned Rural Health Service Managers.
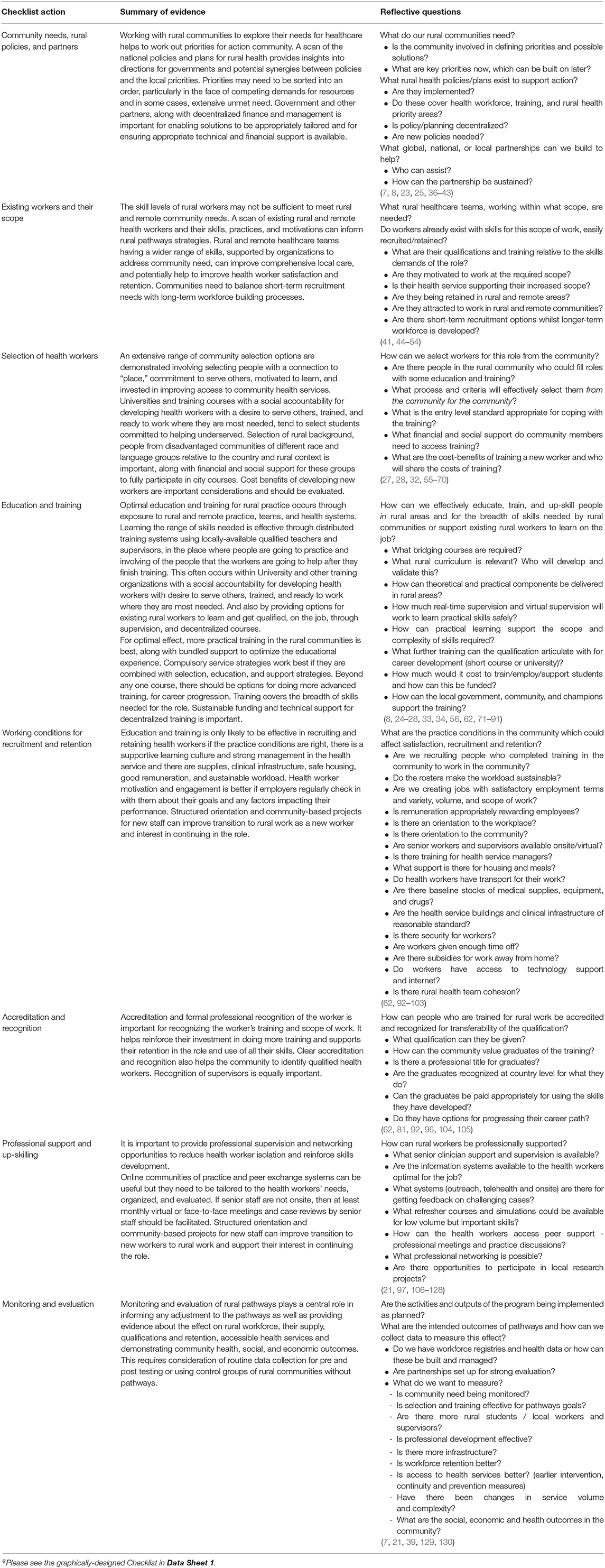
The literature was firstly charted according to broad training and personal/professional support categories based on the strategy areas of the 2010 WHO global recommendations for Increasing access to health workers in remote and rural areas through improved retention (7). Inductive thematic analysis was then applied to progressively layer and reorganize material into key themes related to guiding implementation without any pre-existing coding framework. This resulted in a draft framework of rural pathways actions that was discussed and refined based on feedback from the Steering Committee, Expert Reference Group, and staff at the WHO. Eventually the draft Checklist comprised eight equally balanced actions, presented in a Microsoft Word document (shown in Table 3 before being applied as the graphically-designed Checklist in Data Sheet 1). These actions were: establishing community needs, policies, and partners; exploring existing workers and their scope; selecting health workers; education and training; considering working conditions for recruitment and retention; accreditation and recognition of qualified workers; professional support and up-skilling and; monitoring and evaluation. For each action area, reflective questions underpinned by supporting evidence (individual references to research and what it showed) was developed. This design specifically aimed to address the objective of stimulating reflection and learning for implementing each action specific to the LMICs context.
Consultation
The consultation with the Expert Reference Group at round 2 (Table 2), suggested that the draft Checklist was well-structured and comprehensive—applicable to any LMICs, stakeholder, health worker, context, or health problem, regardless of the starting point. The reflective questions were considered useful:
“In resource poor settings, a checklist of basic tools/equipment for the workers being trained is an important practical aspect for reflection”.
“Reflective questions fit our setting which is poorly resourced (human and material)”.
The stakeholders gave feedback that they preferred that the evidence was provided in summary references only. Further, some respondents indicated that the Checklist may be more successful if there was more consideration as to the context of implementation. To address this, the Steering Committee decided it was relevant to develop a stakeholder map to accompany the Checklist, which could represent the partners in relation to implementing the 8 Checklist actions (Data Sheet 2). Also, a series of rural pathways implementation exemplars was developed. These were based on the highest quality examples of rural pathways activities that had been identified by the policy, scoping review and consultation phases, targeting coverage of different WHO regions (Data Sheet 3) (35, 131). Round 2 feedback confirmed that the term “rural pathways” was preferred over terms like “rural pipelines.” Respondents noted the former was easier to translate in all LMIC languages and encompassed different entry points, iterative lifelong learning and progression through training and development events, rather sealed and inflexible routes.
The round 3 feedback from the Expert Reference Group related to the graphically-designed version of the Checklist (131) (Data Sheet 1). This unanimously confirmed that the Checklist was comprehensive and complete:
“It's very well structured and is the way forward for any country”
“This graphic display presents the key elements very clearly”
“…I think it can be used at many different levels of the healthcare system and planning processes… to identify gaps.”
This feedback also identified that the priorities and the degree of progress with rural pathways implementation across the 8 actions was highly variable by country. Respondents reported that a key enabler for implementing actions were a government commitment to rural health, formalized in policy, and through sustained investment. They also mentioned that health service engagement and using coordinators who could assist to broker pathways and relevant partnerships may be helpful. The key barriers to implementation in LMICs included: time and funding; sharing resources with rural communities and; embedding the value of rural work and learning into policy action.
Dissemination, Engagement, and Field-Testing
Dissemination, engagement, and field-testing provided a range of positive feedback about the Checklist and no major changes were suggested. Participants unanimously noted that the tool was highly applicable as a practical resource for implementing rural pathways in HICs (reaching beyond the intended purpose). The self-assessment tool (Data Sheet 4) was used to test the Checklist's application. Overall 56 participants from 20 countries participated in this process. Of these, 38 worked in rural areas, 21 were from LMICs—Brazil, Liberia, Guatemala, Malawi, India, Papua New Guinea, Latin America, Philippines and Uganda, and 35 were from HIC—Canada, Australia, United Kingdom, and United States of America (5 of whom were serving LMICs– Haiti, Kyrgyzstan, Syria, Iraq, Thailand, Asia, and Africa). Participants represented various stakeholders (director to student/community levels) from a range of organizations including universities, trainers/educators, global and rural health programs and researchers, overseas missions, policy and planning institutes, health services, and community boards.
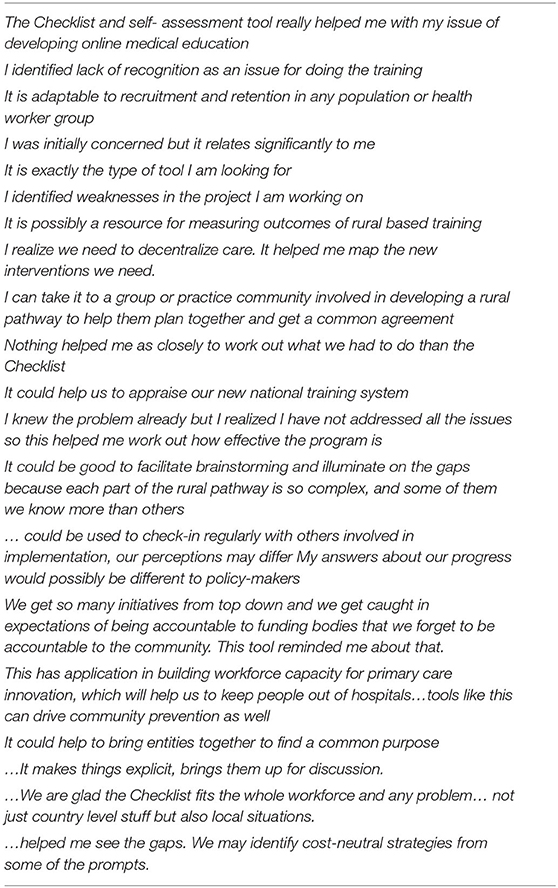
Participants identified a wide range of real-world rural health problems and health workforce challenges for which the Checklist was considered relevant. The data from the self-assessment tool also showed that the Checklist was effective for any type of stakeholder to self-identify gaps in their rural pathway actions for specific rural health workers they were trying to train, develop, and support. Stakeholders suggested that it helped them to see gaps in the pathway that they needed to discuss with other stakeholders, so they could work out jointly agreed strategies to address these. Some considered that the Checklist and associated materials could be valuable to use with different rural pathways implementers in the one training sub-system, for example during collaborative meetings, to agree on community needs, stakeholder actions, and responsibilities, thereafter checking in regularly to refine action. The self-assessment tool was also considered applicable to support regular planning over the long-term rural pathways implementation cycle. This includes when reflexive action may be needed based on changing conditions. A summary participant's reflections is outlined (Table 4). Beyond the field-testing meetings, selected stakeholders applied the Checklist to real-world planning in their countries. One such study is published to date, finding the Checklist was applicable for developing strategies to expand rural healthcare workforce in Kyrgyzstan (132).
With respect to HIC use, stakeholders noted that the state of progress toward rural pathways implementation was fairly strong, but the Checklist particularly applied to them as they noted their rural pathways were complicated by extensive numbers of stakeholders, professional competition, and workforce regulations which sometimes detracted from addressing community goals.
Discussion
This project involved developing an agreed terminology and framework to support practical implementation of rural pathways in LMICs. The resulting Rural Pathways Checklist evolved from a breadth of methods including reviewing evidence, consultation, and engagement and field-testing to ensure it was both evidence-based and pragmatic, for greatest utility in LMICs. The Checklist is a step forward in achieving a globally-agreed conceptual framework and language which integrates eight training and personal/professional support actions to train, develop, and support rural health workers under a continuous quality improvement cycle. Building on the 2010 WHO recommendations for increasing access to health workers, the Checklist actions are focused on a community goal. They attempt to drive more comprehensive rural pathways interventions through long-term effort of many stakeholders, rather than through discrete or siloed strategies. We note from our consultation, that for LMICs to achieve holistic rural pathways implementation, relies on political commitment to decentralize training and resources to rural communities over the long-term. The Checklist may be a tool that LMICs can use to advocate for clear rural training/professional support strategies and more rural investment.
Developed with LMICs evidence as the reference point, the Checklist is the first of its type to be sensitive to countries with the most extreme healthcare needs and most significant shortages of health workers. Although HICs found the Checklist useful and applicable to their own setting, its application may have the most benefit in LMICs given the outstanding levels of socio-economic and health disadvantage, extreme geographical isolation, and poverty. Starting the process of implementing rural pathways in this context has the greatest potential to alleviate global poverty by increasing access to rural work and health, enabling universal health coverage. Critically, it may also bolster local health workers trained for the problems in the community who are more likely to be retained in their community of origin. By increasing trained health workers, local health services are able to cope with the volume of presentations locally and diversify their service platform, supporting rural social, and economic development goals. The demands for a skilled and stable rural health workforce have been particularly notable during the COVID-19 pandemic. The pandemic situation has placed extensive strain on a small number of rural health workers to work at a broad scope, often without the training and professional support they may need. The Checklist may be a way to navigate out of this situation and build self-reliant rural communities with sufficient skilled health workers.
The project identified that countries, districts, and communities are at different starting points with respect to rural pathways implementation and have different health needs, but the Checklist may be a viable reference point for planning and evaluating action regardless. As opposed to other tools that are discipline, stakeholder or country specific, the Checklist may aid as a resource that is applicable to diverse countries, rural locations, and workforce issues and help to break down siloed profession-based workforce planning, in vertical disease areas. Such effort does not address holistic rural community need in LMICs. The self-assessment tool provides a means of regularly evaluating progress with rural pathways implementation in the complex dynamic environment of rural communities, where changes are common and adjustment is regularly needed. Regular use of the self-assessment tool may increase the potential for timely identification and response to emerging challenges.
Our project has some limitations. The scoping review identified 127 relevant studies from LMICs, applicable to the Checklist but as more evidence emerges, the Checklist may need to be updated. We only commenced the process of collecting exemplars from different WHO regions in this project. Yet there is great potential to build on this and foster global communities of practice in this area, including through online exchanges. This may help with information-sharing and mitigate professional isolation that many rural pathways implementers may face in their own countries or regions. The Checklist has the potential to support more comparative multi-national research about rural pathways. Its utility may also be facilitated if further work was done to marry this with a suite of other global tools to guide action for improving universal health coverage worldwide. The field-testing we did was limited to a convenience sample covering diverse rural contexts, but further research could usefully test the applicability of the Checklist to a set of rural pathways stakeholders of individual countries such as some studies are starting to do (132). Finally, our research explored whether the Checklist applied to all types of health workers needed in rural areas, but it may be pertinent to test how well it applies to particular primary health cadres across a sub-set of LMICs, to gather more data about its reliability.
Conclusion
Our study developed a Rural Pathways Checklist to support practical implementation of integrated rural training, development, and support strategies for health workers in LMICs rural areas. Through diverse methods which drew on both theory and practice, we identified eight actions, reflective questions, and additional resources. Together, these support a continuous, connected and sustained effort for rural pathways implementation in LMICs. Although this Checklist requires further validation, it is possible that it can produce real improvements in access to health workers, fit for the needs of LMICs communities worldwide, as a key step for addressing major inequalities in rural health and sustainable development in rural places.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by This study had ethics approval from Monash University, Victoria, Australia (Project Number 17636) ratified by the University of Queensland (Project Number 2019002437). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
BO'S led the conceptual design, ethics, data collection, field-testing, analysis, and writing. BC and JW-J led the establishment of the global and expert steering groups and the concept testing phase. AB assisted with the scoping review, expert reference group surveys, and field-testing protocol. All authors contributed to design, data collection, analysis, and writing and agreed on the final manuscript and Checklist materials for publication. The WHO approved the Checklist and final manuscript for submission for peer review publication.
Funding
This work was funded by the World Health Organization (WHO).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was done in collaboration with the World Organization of Family Doctors (WONCA) through the WONCA Working Party on Rural Practice (Rural WONCA). We acknowledge the substantial feedback and advice of a Steering Committee and an Expert Reference Group along with input and testing of the Checklist by rural pathways implementers from around the world. The views and opinions expressed in this article are those of the author(s).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2020.594728/full#supplementary-material
Data Sheet 1. Graphically-designed Checklist.
Data Sheet 2. Stakeholder map.
Data Sheet 3. Exemplars from WHO regions.
Data Sheet 4. Self-assessment tool.
References
1. International Labour Organization. Social Protection: Inequity in Health Protection: Rural/Urban Divide. Available online at: https://www.social-protection.org/gimi/gess/ShowTheme.action?lang=EN&id=4066 (accessed 14 October, 2019).
2. World Bank. The World Bank Data Washington: World Bank (2018). Available online at: https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS (accessed November 06, 2020).
3. International Labour Organization. World Social Protection Report: Building Economic Recovery, Inclusive Development And Social Justice. Geneva: ILO (2014). p. 1–364.
4. United Nations. Universal Health Coverage, New York, NY (2020). Available online at: https://www.un.org/pga/73/event/universal-health-coverage/
5. World Health Organization. Health Workforce 2030: A Global Strategy on Human Resources for Health. Geneva: WHO (2018).
6. World Health Organization. Health Workforce. Geneva: WHO (2018). Available online at: https://www.who.int/hrh/education/en/ (accessed November 06, 2020).
7. World Health Organization. Increasing Access to Health Workers in Remote and Rural Areas Through Improved Retention: Global Policy Recommendations. Geneva: WHO (2010). p. 1–80.
8. da Silva EN, Ramos MC, Santos W, Rasella D, Oliveira A, Pacheco Santos LM. Cost of providing doctors in remote and vulnerable areas: Programa Mais Medicos in Brazil. Rev Panam Salud Publica. (2018) 42:e11. doi: 10.26633/RPSP.2018.11
9. Frehywot S, Mullan F, Payne PW, Ross H. Compulsory service programmes for recruiting health workers in remote and rural areas: do they work? Bullet World Health Organ. (2010) 88:364–70. doi: 10.2471/BLT.09.071605
10. Russell D, Humphreys JS, McGrail M, Cameron WI, Williams PJ. The value of survival analyses for evidence-based rural medical workforce planning. Human Resour Health. (2013) 11:1–9. doi: 10.1186/1478-4491-11-65
11. McGrail M, Humphreys J, Joyce C, Scott A. International medical graduates mandated to practise in rural Australia are highly unsatisfied: results from a national survey of doctors. Health Policy. (2012) 108:133–9. doi: 10.1016/j.healthpol.2012.10.003
12. McGrail M, O'Sullivan B, Russell D. Rural training pathways: the return rate of doctors to work in the same region as their basic medical training. Human Resour Health. (2018) 16:1–10. doi: 10.1186/s12960-018-0323-7
13. Straume K, Shaw DM. Effective physician retention strategies in Norway's northernmost county. Bullet World Health Organ. (2010) 88:390–4. doi: 10.2471/BLT.09.072686
14. O'Sullivan B, McGrail M, Russell D, Walker J, Chambers H, Major L, et al. Duration and setting of rural immersion during the medical degree relates to rural work outcomes. Med Educ. (2018) 52:803–15. doi: 10.1111/medu.13578
15. World Health Organization. High-Level Commission on Health Employment and Economic Growth. Geneva: WHO (2018). Available online at: https://www.who.int/hrh/com-heeg/en/ (accessed November 06, 2020).
16. United Nations. Sustainable Development Goals. New York, NY (2018). Available online at: https://sdgs.un.org/goals (accessed November 06, 2020).
17. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
18. Culquhoun HL, Levac D, O'Brien KK, Strausd S, Tricco AC, Perrierd L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. (2014) 67:1291–4. doi: 10.1016/j.jclinepi.2014.03.013
19. Country Classifications by Income Level: 2017-2018. Washington, DC: World Bank (2018). Available online at: https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2017-2018 (accessed November 06, 2020).
20. Dolea C, Stormont L, Braichet J-M. Evaluated strategies to increase attraction and retention of health workers in remote and rural areas. Bulletin World Health Organ. (2010) 88:379–85. doi: 10.2471/BLT.09.070607
21. World Health Organization. Transforming and Scaling Up Health Professionals' Education and Training: World Health Organization Guidelines 2013. Geneva: WHO (2018).
22. Nadan D. National rural health mission: turning into reality. Indian J Commun Med. (2010) 35:453–4. doi: 10.4103/0970-0218.74338
23. Nagarajan S, Paul VK, Yadav N, Gupta S. The National Rural Health Mission in India: its impact on maternal, neonatal, and infant mortality. Semin Fetal Neonatal Med. (2015) 20:315–20. doi: 10.1016/j.siny.2015.06.003
24. Yi Y, Chongsuvivatwong V, Sriplung H, Rueanarong C. CPIRD: a successful Thai programme to produce clinically competent medical graduates. F1000research. (2015) 4:158. doi: 10.12688/f1000research.6638.1
25. Pagaiya N, Kongkam L, Sriratana S. Rural retention of doctors graduating from the rural medical education project to increase rural doctors in Thailand: a cohort study. Human Resour Health. (2015) 13:10. doi: 10.1186/s12960-015-0001-y
26. Putthasri W, Suphanchaimat R, Topothai T, Wisaijohn T, Thammatacharee N, Tangcharoensathien V. Thailand special recruitment track of medical students: a series of annual cross-sectional surveys on the new graduates between 2010 and 2012. Human Resour Health. (2013) 11:47. doi: 10.1186/1478-4491-11-47
27. Halili SB Jr., Cristobal F, Woolley T, Ross SJ, Reeve C, et al. Addressing health workforce inequities in the Mindanao regions of the Philippines: tracer study of graduates from a socially-accountable, community-engaged medical school and graduates from a conventional medical school. Med Teacher. (2017) 39:859–65. doi: 10.1080/0142159X.2017.1331035
28. Siega-Sur JL, Woolley T, Ross SJ, Reeve C, Neusy AJ. The impact of socially-accountable, community-engaged medical education on graduates in the Central Philippines: Implications for the global rural medical workforce. Med Teacher. (2017) 39:1084–91. doi: 10.1080/0142159X.2017.1354126
29. Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. (2012) 12:352. doi: 10.1186/1472-6963-12-352
30. World Health Organization. Case study: Scaling Up Education and Training of Human Resources for Health in Ethiopia: Moving Towards Achieving the MDGs. Geneva: WHO (2010). p. 1–36.
31. Derbew M, Animut N, Talib ZM, Mehtsun S, Hamburger EK. Ethiopian medical schools' rapid scale-up to support the government's goal of universal coverage. Acad Med. (2015) 89:1–6. doi: 10.1097/ACM.0000000000000326
32. Iputo JE. Faculty of Health Sciences, Walter Sisulu University: training doctors from and for rural South African Communities. Medic Rev. (2008) 10:25–9. doi: 10.37757/MR2008.V10.N4.6
33. Kwizera EN, Iputo J. Addressing social responsibility in medical education: the African way. Med Teacher. (2011) 33:649–53. doi: 10.3109/0142159X.2011.590247
34. Woolley T, Cristobal F, Siega-Sur JJ, Ross S, Neusy AJ, Halili SD, et al. Positive implications from socially accountable, community engaged medical education across two Philippines regions. Rural Remote Health. (2018) 18:1–10. doi: 10.22605/RRH4264
35. World Health Organization. About WHO: WHO Regional Offices. Geneva: WHO (2018). Available online at: https://www.who.int/about/regions/en/ (accessed November 06, 2020).
36. Cho S, Lee H, Yoon S, Kim Y, Levin PF, Kim E. Community health needs assessment: a nurses' global health project in Vietnam. Int Nursing Rev. (2018) 65:505–14. doi: 10.1111/inr.12443
37. Dawe R, Stobbe K, Pokharel YJ, Shrestha S. Capacity building in Nepal. Canad Med Educ J. (2016) 7:e51–3. doi: 10.36834/cmej.36847
38. World Health Organization. Task Shifting : Rational Redistribution of Tasks Among Health Workforce Teams : Global Recommendations and Guidelines. Geneva: WHO (2008). p. 1–96.
39. World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva: WHO (2016). p. 1–64.
40. Javanparast S, Baum F, Labonte R, Sanders D, Rajabi Z, Heidari G. The experience of community health workers training in Iran: a qualitative study. BMC Health Serv Res. (2012) 12:291. doi: 10.1186/1472-6963-12-291
41. Li X, Liu J, Huang J, Qian Y, Che L. An analysis of the current educational status and future training needs of China's rural doctors in (2011). Postgraduate Med J. (2013) 89:202–8. doi: 10.1136/postgradmedj-2012-131094
42. Versteeg M, du Toit L, Couper I. Building consensus on key priorities for rural health care in South Africa using the Delphi technique. Global Health Action. (2013) 6:119–26. doi: 10.3402/gha.v6i0.19522
43. Kumar P, Kumar R. Rural health scenario – role of family medicine: Academy of Family Physicians of India position paper. J Fam Med Primary Care. (2018) 7:1157–62. doi: 10.4103/jfmpc.jfmpc_254_18
44. Capati J, Crichton A, Louw M, Smalley S, Tshabalala Z. Clinical Associate Training and Profession - Current Successes and Future Steps. South Africa: Report of the Clinical Associate National Task Team 2017 (2018). p. 1–74.
45. Goliath C, Mukinda FK, Dudley L. Capacity-building needs assessment of rural health managers: the what and the how. African Health Profess Educ. (2015) 7(1 Suppl. 1):92–7. doi: 10.7196/AJHPE.510
46. Salehi Zalani G, Bayat M, Shokri A, Mirbahaeddin SE, Rasi V, Alirezaei S, et al. Affecting factors on the performance of community health workers in Iran's rural areas: a review article. Iran J Public Health. (2016) 45:1399–410.
47. Shelley KD, Belete YW, Phiri SC, Musonda M, Kawesha EC, Muleya EM, et al. Implementation of the Community Health Assistant (CHA) Cadre in Zambia: a process evaluation to guide future scale-up decisions. J Commun Health. (2016) 41:398–408. doi: 10.1007/s10900-015-0110-5
48. Couper I, Ray S, Blaauw D, Ng'wena G, Muchiri L, Oyungu E, et al. Curriculum and training needs of mid-level health workers in Africa: a situational review from Kenya, Nigeria, South Africa and Uganda. BMC Health Serv Res. (2018) 18:553. doi: 10.1186/s12913-018-3362-9
49. Reid SJ, Couper ID, Volmink J. Educational factors that influence the urban-rural distribution of health professionals in South Africa: a case-control study. S Afr Med J. (2011) 101:29–33. doi: 10.7196/SAMJ.4342
50. Fathima FN, Raju M, Varadharajan KS, Krishnamurthy A, Ananthkumar SR, Mony PK. Assessment of ‘Accredited Social Health Activists’—A NationalCommunity Health Volunteer Scheme in Karnataka State, India. J Health Policy Nutrit. (2015) 33:1–9.
51. Sánchez Del Hierro G, Remmen R, Verhoeven V, Van Royen P, Hendrickx K. Are recent graduates enough prepared to perform obstetric skills in their rural and compulsory year? A study from Ecuador. BMJ Open. (2014) 4:e005759–e. doi: 10.1136/bmjopen-2014-005759
52. Abera M, Tesfaye M, Belachew T, Hanlon C. Perceived challenges and opportunities arising from integration of mental health into primary care: a cross-sectional survey of primary health care workers in south-west Ethiopia. BMC Health Serv Res. (2014) 14:1–10. doi: 10.1186/1472-6963-14-113
53. Allen CW, Jeffery H. Implementation and evaluation of a neonatal educational program in rural Nepal. J Trop Pediatrics. (2006) 52:218–22. doi: 10.1093/tropej/fmi106
54. Luo EM, Opare-Ado HS, Adomako J, Danso KA, Peltzman T, Anderson FWJ. Completing the Maternal Care Team: OB/GYN expertise at rural district hospitals in ghana, a qualitative study. Mater Child Health J. (2018) 22:1085–91. doi: 10.1007/s10995-018-2492-3
55. Newman DE, Shapiro MC. Obstacles faced by general practitioners in Loreto Department, Peru in pursuing residency training. Rural Remote Health. (2010) 10:1256.
56. Husum H, Gilbert M, Wisborg T. Training pre-hospital trauma care in low-income countries: the ‘Village University’ experience. Med Teacher. (2003) 25:142–8. doi: 10.1080/0142159031000092526
57. Tani K, Exavery A, Baynes CD, Pemba S, Hingora A, Manzi F, et al. Unit cost analysis of training and deploying paid community health workers in three rural districts of Tanzania. BMC Health Serv Res. (2016) 16:237. doi: 10.1186/s12913-016-1476-5
58. Phiri SC, Prust ML, Chibawe CP, Misapa R, van den Broek JW, Wilmink N. An exploration of facilitators and challenges in the scale-up of a national, public sector community health worker cadre in Zambia: a qualitative study. Human Resour Health. (2017) 15:40. doi: 10.1186/s12960-017-0214-3
59. Morgan C, Teshome M, Crocker-Buque T, Bhudia R, Singh K. Medical education in difficult circumstances: analysis of the experience of clinical medical students following the new innovative medical curriculum in Aksum, rural Ethiopia. BMC Med Educ. (2018) 18:119. doi: 10.1186/s12909-018-1199-x
60. Van Heng Y, Davoung C, Husum H. Non-doctors as trauma surgeons? A controlled study of trauma training for non-graduate surgeons in rural Cambodia. Prehosp Disast Med. (2008) 23:483–9. doi: 10.1017/S1049023X00006282
61. Knettel BA, Slifko SE, Inman AG, Silova I. Training community health workers: an evaluation of effectiveness, sustainable continuity, and cultural humility in an educational program in rural Haiti. Int J Health Promot Educ. (2017) 55:177–88. doi: 10.1080/14635240.2017.1284014
62. Zimmerman M, Shah S, Shakya R, Sundar Chansi B, Shah K, Munday D, et al. A staff support programme for rural hospitals in Nepal. Bullet World Health Organ. (2016) 94:65–70. doi: 10.2471/BLT.15.153619
63. Tumbo JM, Couper ID, Hugo JFM. Rural-origin health science students at South African universities. S Af Med J. (2009) 99:54–6.
64. Hamm J, Bodegraven PV, Bac M, Louw JM. Cost effectiveness of clinical associates: A case study for the Mpumalanga province in South Africa. Af J Prim Health Care Fam Med. (2016) 8:e1–6. doi: 10.4102/phcfm.v8i1.1218
65. Leon BK, Riise Kolstad J. Wrong schools or wrong students? The potential role of medical education in regional imbalances of the health workforce in the United Republic of Tanzania. Human Resour Health. (2010) 8:3. doi: 10.1186/1478-4491-8-3
66. Pei H, Sun Y, Bai Z, Yu Z, Chang C, Qiu C, et al. Selective admission policy of medical undergraduates in western China: applicants' real attitudes to the choice of a rural medical career. Rural Remote Health. (2018) 18:1–12. doi: 10.22605/RRH4519
67. Hayes BW, Butterworth K, Neupane BD. Nepal's general practitioners - factors in their location of work. Middle East J Fam Med. (2007) 6:17–21.
68. Ross AJ, Couper I. Rural scholarship schemes: a solution to the human resource crisis in rural district hospitals? S Af Fam Pract. (2004) 46:05–6. doi: 10.1080/20786204.2004.10873025
69. Ross A, MacGregor G, Campbell L. Review of the Umthombo Youth Development Foundation scholarship scheme, 1999–2013. Af J Prim Health Care Fam Med. (2015) 7:1–6. doi: 10.4102/phcfm.v7i1.739
70. Mapukata NO, Couper ID, Dreyer AR, Mlambo M. Health sciences students' contribution to human resources for health strategy: a rural health careers day for grade 12 learners in the North West Province of South Africa. Af Jo Health Profes Educ. (2017) 9:92–3. doi: 10.7196/AJHPE.2017.v9i3.856
71. Budhathoki SS, Zwanikken PAC, Pokharel PK, Scherpbier AJ. Factors influencing medical students' motivation to practise in rural areas in low-income and middle-income countries: a systematic review. BMJ Open. (2017) 7:e013501. doi: 10.1136/bmjopen-2016-013501
72. Crampton PES, McLachlan JC, Illing JC. A systematic literature review of undergraduate clinical placements in underserved areas. Med Educ. (2013) 47:969–78. doi: 10.1111/medu.12215
73. Farmer J, Kenny A, McKinstry C, Huysmans RD. A scoping review of the association between rural medical education and rural practice location. Human Resour Health. (2015) 13:27. doi: 10.1186/s12960-015-0017-3
74. Wilson NW, Couper ID, De Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. (2009) 9:1060.
75. Verma P, Ford JA, Stuart A, Howe A, Everington S, Steel N. A systematic review of strategies to recruit and retain primary care doctors. BMC Health Serv Res. (2016) 16:126. doi: 10.1186/s12913-016-1370-1
76. Mlambo M, Dreyer A, Dube R, Mapukata N, Couper I, R C. Transformation of medical education through decentralised training platforms: a scoping review. Rural Remote Health. (2018) 18:4337. doi: 10.22605/RRH4337
77. Doherty JE, Couper I. Strengthening rural health placements for medical students: lessons for South Africa from international experience. S Af Med J. (2016) 106:524–7. doi: 10.7196/SAMJ.2016.v106i5.10216
78. Couper ID, Thurley JD, Hugo JFM. The neonatal resuscitation training project in rural South Africa. Rural Remote Health. (2005) 5:459.
79. Alebachew A, Waddington C. Improving Health System Efficiency: Ethiopia Human Resources for Health Reforms. Geneva: WHO (2015) p. 1–28.
80. Tilahun D, Hanlon C, Araya M, Davey B, Hoekstra RA, Fekadu A. Training needs and perspectives of community health workers in relation to integrating child mental health care into primary health care in a rural setting in sub-Saharan Africa: a mixed methods study. Int J Mental Health Syst. (2017) 11:15. doi: 10.1186/s13033-017-0121-y
81. Mung'omba B, Botha ADH. Core competencies of radiographers working in rural hospitals of KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med. (2017) 9:e1–8. doi: 10.4102/phcfm.v9i1.1389
82. Hu G, Yi Y. Is a decentralized continuing medical education program feasible for Chinese rural health professionals? J Educ Evaluat Health Profess. (2016) 13:18. doi: 10.3352/jeehp.2016.13.18
83. Kibore MW, Daniels JA, Child MJ, Nduati R, Njiri FJ, Kinuthia RM, et al. Kenyan medical student and consultant experiences in a pilot decentralized training program at the University of Nairobi. Educ Health. (2014) 27:170–6. doi: 10.4103/1357-6283.143778
84. Kizito S, Baingana R, Mugagga K, Akera P, Sewankambo NK. Influence of community-based education on undergraduate health professions students' decision to work in underserved areas in Uganda. BMC Res Notes. (2017) 10:726. doi: 10.1186/s13104-017-3064-0
85. Bhushan H, Bhardwaj A. Task shifting: a key strategy in the multipronged approach to reduce maternal mortality in India. Int J Gynaecol Obstet. (2015) 131(Suppl. 1):S67–70. doi: 10.1016/j.ijgo.2015.03.016
86. Techakehakij W, Arora R. Rural retention of new medical graduates from the Collaborative Project to Increase Production of Rural Doctors (CPIRD): a 12-year retrospective study. Health Policy Plann. (2017) 32:809–15. doi: 10.1093/heapol/czx026
87. Henderson LN, Tulloch J. Incentives for retaining and motivating health workers in Pacific and Asian countries. Human Resour Health. (2008) 6:18. doi: 10.1186/1478-4491-6-18
88. Theron GB. Improved practical skills of midwives practicing in the Eastern Cape Province of the Republic of South Africa through the study of a self-education manual. J Perinatol. (2000) 20:184–8. doi: 10.1038/sj.jp.7200334
89. Symmons D, Curry C. Rural hospital generalist and emergency medicine training in Papua New Guinea. Emerg Med Austral. (2007) 19:151–4. doi: 10.1111/j.1742-6723.2006.00913.x
90. Stellenbosch University. Report: Driving decentralised training – Adaptive Approaches SUCCEED Preconference SAAHE Workshop Report. Durban: Stellenbosch University (2018). p. 1–15.
91. Velavan J. “The Refer Less Resolve More” initiative: a five-year experience from CMC Vellore, India. J Fam Med Prim Care. (2012) 1:3–6. doi: 10.4103/2249-4863.94439
92. Singh D, Negin J, Otim M, Orach CG, Cumming R. The effect of payment and incentives on motivation and focus of community health workers: five case studies from low- and middle-income countries. Human Resour Health. (2015) 13:58. doi: 10.1186/s12960-015-0051-1
93. Kaye D, Mwanika A, Burnham G, Chang LW, Mbalinda SN, Okullo I, et al. The organization and implementation of community-based education programs for health worker training institutions in Uganda. BMC Int Health Human Rights. (2011) 11(Suppl. 1):S4. doi: 10.1186/1472-698X-11-S1-S4
94. Kok MC, Dieleman M, Taegtmeyer M, Broerse JEW, Kane SS, Ormel H, et al. Which intervention design factors influence performance of community health workers in low- and middle-income countries? A systematic review. Health Policy Plann. (2015) 30:1207–27. doi: 10.1093/heapol/czu126
95. Goel S, Angeli F, Bhatnagar N, Singla N, Grover M, Maarse H. Retaining health workforce in rural and underserved areas of India: what works and what doesn't? A critical interpretative synthesis. Natl Med J India. (2016) 29:212–8.
96. Tshering D, Tejativaddhana P, Briggs D, Wangmo N. Factors affecting motivation and retention of village health workers and recommended strategies: a systematic review from 11 developing countries. Asia Pac J Health Manag. (2018) 13:i137. doi: 10.24083/apjhm.v13i2.13
97. Moran AM, Coyle J, Pope R, Boxall D, Nancarrow SA, Young J. Supervision, support and mentoring interventions for health practitioners in rural and remote contexts: an integrative review and thematic synthesis of the literature to identify mechanisms for successful outcomes. Human Resour Health. (2014) 12:10. doi: 10.1186/1478-4491-12-10
98. Blacklock C, Bradley DCG, Mickan S, Willcox M, Roberts N, Bergstroem A, et al. Impact of contextual factors on the effect of interventions to improve health worker performance in Sub-Saharan Africa: review of randomised clinical trials. PLoS ONE. (2016) 11:e0145206. doi: 10.1371/journal.pone.0145206
99. Van Dormael M, Dugas S, Kone Y, Coulibaly S, Sy M, Marchal B, et al. Appropriate training and retention of community doctors in rural areas: a case study from Mali. Human Resour Health. (2008) 6:25. doi: 10.1186/1478-4491-6-25
100. Vyas R, Zacharah A, Swamidasan I, Doris P, Harris I. Blended distance education program for junior doctors working in rural hospitals in India. Rural Remote Health. (2014) 14:2420.
101. Rennert W, Koop E. Primary health care for remote village communities in Honduras: a model for training and support of community health workers. Fam Med. (2009) 41:646–51.
102. Cavender A, Albán M. Compulsory medical service in Ecuador: the physician's perspective. Soc Sci Med. (1998) 47:1937–46. doi: 10.1016/S0277-9536(98)00335-9
103. Liu J, Zhang K, Mao Y. Attitude towards working in rural areas: a cross-sectional survey of rural-oriented tuition-waived medical students in Shaanxi, China. BMC Med Educ. (2018) 18:91. doi: 10.1186/s12909-018-1209-z
104. Kawasaki R, Sadamori T, Ferreira de Almeida T, Akiyoshi M, Nishihara M, Yoshimura T, et al. Reactions of community members regarding community health workers' activities as a measure of the impact of a training program in Amazonas, Brazil. J Rural Med. (2015) 10:7–19. doi: 10.2185/jrm.2890
105. Rabbani F, Shipton L, Aftab W, Sangrasi K, Perveen S, Zahidie A. Inspiring health worker motivation with supportive supervision: a survey of lady health supervisor motivating factors in rural Pakistan. BMC Health Serv Res. (2016) 16:397. doi: 10.1186/s12913-016-1641-x
106. Thapa KR, Shrestha BK, Bhattarai MD. Study of working experience in remote rural areas after medical graduation. Kathmandu Univ Med J. (2014) 12:121–5. doi: 10.3126/kumj.v12i2.13658
107. Mboineki JF, Zhang W. Healthcare provider views on transitioning from task shifting to advanced practice nursing in Tanzania. Nursing Res. (2018) 67:49–54. doi: 10.1097/NNR.0000000000000259
108. Wangmo S, Suphanchaimat R, Htun WMM, Tun Aung T, Khitdee C, Patcharanarumol W, et al. Auxiliary midwives in hard to reach rural areas of Myanmar: filling MCH gaps. BMC Public Health. (2016) 16:914. doi: 10.1186/s12889-016-3584-x
109. Ludwick T, Turyakira E, Kyomuhangi T, Manalili K, Robinson S, Brenner JL. Supportive supervision and constructive relationships with healthcare workers support CHW performance: use of a qualitative framework to evaluate CHW programming in Uganda. Human Resour Health. (2018) 16:11. doi: 10.1186/s12960-018-0272-1
110. Ndima SD, Sidat M, Give C, Ormel H, Kok MC, Taegtmeyer M. Supervision of community health workers in Mozambique: a qualitative study of factors influencing motivation and programme implementation. Human Resour Health. (2015) 13:63. doi: 10.1186/s12960-015-0063-x
111. Bailey C, Blake C, Schriver M, Cubaka VK, Thomas T, Hilber AM. A systematic review of supportive supervision as a strategy to improve primary healthcare services in Sub-Saharan Africa. Int J Gynecol Obstet. (2016) 132:117–25. doi: 10.1016/j.ijgo.2015.10.004
112. Barnett S, Jones SC, Bennett S, Iverson D, Bonney A. General practice training and virtual communities of practice - a review of the literature. BMC Fam Pract. (2012) 13:87. doi: 10.1186/1471-2296-13-87
113. Van Wieren A, Palazuelos L, Elliott PF, Arrieta J, Flores H, Palazuelos D. Service, training, mentorship: first report of an innovative education-support program to revitalize primary care social service in Chiapas, Mexico. Global Health Action. (2014) 7:25139. doi: 10.3402/gha.v7.25139
114. Dowling S, Last J, Finnigan H, Cullen W. Continuing education for general practitioners working in rural practice: a review of the literature. Educ Prim Care. (2018) 29:151–65. doi: 10.1080/14739879.2018.1450096
115. Curran V, Rourke L, Snow P. A framework for enhancing continuing medical education for rural physicians: a summary of the literature. Med Teacher. (2010) 32:e501–e8. doi: 10.3109/0142159X.2010.519065
116. Mbemba G, Gagnon M-P, Pare G, Cote J. Interventions for supporting nurse retention in rural and remote areas: an umbrella review. Human Resour Health. (2013) 11:1–9. doi: 10.1186/1478-4491-11-44
117. Hoque DME, Arifeen SE, Rahman M, Chowdhury EK, Haque TM, Begum K, et al. Improving and sustaining quality of child health care through IMCI training and supervision: experience from rural Bangladesh. Health Policy Plann. (2014) 29:753–62. doi: 10.1093/heapol/czt059
118. Saab BR, Kanaan N, Hamadeh G, Usta J. Postgraduate educational program for primary care physicians in remote areas in Lebanon. J Contin Educ Health Profes. (2003) 23:168–72. doi: 10.1002/chp.1340230308
119. Ajeani J, Mangwi Ayiasi R, Tetui M, Ekirapa-Kiracho E, Namazzi G, Muhumuza Kananura R, et al. A cascade model of mentorship for frontline health workers in rural health facilities in Eastern Uganda: processes, achievements and lessons. Glob Health Action. (2017) 10:1345497. doi: 10.1080/16549716.2017.1345497
120. Butterworth K, Hayes B, Zimmerman M. Remote and rural: do mentors enhance the value of distance learning continuing medical education? Educ Health. (2011) 24:539.
121. Nqala MO, Rout CC, Aldous CM. Remote clinical support by telephone for rural district hospital medical officers in the Eastern Cape. S Af Fam Pract. (2015) 57:286–90. doi: 10.1080/20786190.2015.1055671
122. Chib A, Tran Khanh P, Si CW, Hway NS. Enabling informal digital guanxi for rural doctors in Shaanxi, China. Chinese J Commun. (2013) 6:62–80. doi: 10.1080/17544750.2013.753500
123. Vyas R, Zachariah A, Swamidasan I, Doris P, Harris I. Integration of academic learning and service development through guided projects for rural practitioners in India. Med Teacher. (2011) 33:e401–e7. doi: 10.3109/0142159X.2011.575900
124. Vyas R, Zachariah A, Swamidasan I, Doris P, Harris I. A networking approach to reduce academic and social isolation for junior doctors working in rural hospitals in India. Educ Health. (2012) 25:70–4. doi: 10.4103/1357-6283.99212
125. Rusatira JC, Tomaszewski B, Dusabejambo V, Ndayiragije V, Gonsalves S, Sawant A, et al. Enabling access to medical and health education in rwanda using mobile technology: needs assessment for the development of mobile medical educator apps. JMIR Med Educ. (2016) 2:e7. doi: 10.2196/mededu.5336
126. Li H, Wang Z, Jiang N, Liu Y, Wen D. Lifelong learning of Chinese rural physicians: preliminary psychometrics and influencing factors. BMC Med Educ. (2015) 15:192. doi: 10.1186/s12909-015-0460-9
127. Li X, Shen JJ, Yao F, Jiang C, Chang F, Hao F, et al. Does exam-targeted training help village doctors pass the certified (assistant) physician exam and improve their practical skills? A cross-sectional analysis of village doctors' perspectives in Changzhou in Eastern China. BMC Med Educ. (2018) 18:107. doi: 10.1186/s12909-018-1211-5
128. Hatcher AM, Onah M, Kornik S, Peacocke J, Reid S. Placement, support, and retention of health professionals: national, cross-sectional findings from medical and dental community service officers in South Africa. Human Resour Health. (2014) 12:14. doi: 10.1186/1478-4491-12-14
129. Bertone MP. Strategies of health workforce retention in rural areas of seven countries of francophone Africa. Sante Publique. (2018) S1:33–43. doi: 10.3917/spub.180.0033
130. World Health Organization. Handbook on Monitoring and Evaluation of Human Resources for Health: With Special Applications for low- and Middle-Income Countries. In: Dal Poz MR, Gupta N, Quaine E, Soucat A, editors. Geneva: WHO (2009).
131. O'Sullivan B, Chater B, Bingham A, Wynn-Jones J, Couper I, Hegazny N, et al. A Report for the World Health Organization: Development of a Checklist for Implementing Rural Pathways to Train and Support Health Workers in Low and Middle Income Countries - Draft for Consultation Bendigo: Monash University and rural WONCA. (2018). Available online at: https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/Groups/Rural%20Practice/19%20implementing%20rural%20pathways.pdf (accessed November 06, 2020).
Keywords: rural workforce, rural health workers, training, education, professional support, implement, LMICs, guide
Citation: O'Sullivan B, Chater B, Bingham A, Wynn-Jones J, Couper I, Hegazy NN, Kumar R, Lawson H, Martinez-Bianchi V, Randenikumara S, Rourke J, Strasser S and Worley P (2020) A Checklist for Implementing Rural Pathways to Train, Develop and Support Health Workers in Low and Middle-Income Countries. Front. Med. 7:594728. doi: 10.3389/fmed.2020.594728
Received: 14 August 2020; Accepted: 30 October 2020;
Published: 27 November 2020.
Edited by:
Sarah Larkins, James Cook University, AustraliaReviewed by:
Torres Woolley, James Cook University, AustraliaHarm Van Marwijk, Brighton and Sussex Medical School, United Kingdom
Copyright © 2020 O'Sullivan, Chater, Bingham, Wynn-Jones, Couper, Hegazy, Kumar, Lawson, Martinez-Bianchi, Randenikumara, Rourke, Strasser and Worley. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Belinda O'Sullivan, YmVsaW5kYS5vc3VsbGl2YW5AdXEuZWR1LmF1
 Belinda O'Sullivan
Belinda O'Sullivan Bruce Chater2
Bruce Chater2 Ian Couper
Ian Couper Viviana Martinez-Bianchi
Viviana Martinez-Bianchi Sankha Randenikumara
Sankha Randenikumara James Rourke
James Rourke Paul Worley
Paul Worley